Professional Documents
Culture Documents
Axelrod and Pomfret
Axelrod and Pomfret
Uploaded by
Amy WooCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Axelrod and Pomfret
Axelrod and Pomfret
Uploaded by
Amy WooCopyright:
Available Formats
EDITORIAL Editorials represent the opinions
of the authors and JAMA and
not those of the American Medical Association.
Race and Sex Disparities
in Liver Transplantation
Progress Toward Achieving Equal Access?
David A. Axelrod, MD, MBA tem contributed to a reduction in the waiting list death rates
from 150 to 125 deaths per 1000 patient-years at risk.1 How-
Elizabeth A. Pomfret, MD, PhD
ever, these waiting list death rates had been declining for
the 5 years before MELD at an even greater rate. Further-
U
NIQUE AMONG MEDICAL SPECIALTIES, THE ORGAN
more, this reduction in waiting list death rates was accom-
transplantation community has the obligation to ex-
plished without a significant deterioration in posttrans-
plicitly allocate a very limited lifesaving resource.
plant survival. The MELD system has also led to a more
Liver transplantation offers the sole hope for long-
objective method for estimating the benefit of transplant and
term survival for patients with end-stage liver disease. Over-
subsequent revision of the allocation system. For relatively
all survival rates for transplantation now routinely exceed 90%
healthy patients (MELD score of ⬍15), liver transplanta-
at 1 year, even among patients with the most advanced liver
tion was found to have no survival benefit and was in fact
failure, the majority of whom would die within months with-
associated with worse survival than remaining on the trans-
out a transplant.1,2 As stewards of a precious resource, the trans-
plant list.5 As a result, the transplant community has re-
plant community has a goal of achieving an equitable, trans-
quired that donated livers be used within a wider geographi-
parent, and efficient system of organ allocation. Meeting these
cal region before being used in the local community if no
goals is crucial for maintaining confidence in the transplant
recipients with a MELD score of more than 15 are waiting
system and encouraging organ donation.
locally.
Before 2002, deceased donor liver allografts were allo-
In this issue of JAMA, Moylan and colleagues6 report that
cated by using a system that was loosely based on severity of
the use of MELD has had another desirable benefit. Retro-
illness and time spent waiting. Review of the national out-
spective analysis of the United Network for Organ Sharing
comes demonstrated that this system consistently failed to
(UNOS) database confirmed prior findings that in the pre-
achieve the goals of equity, transparency, and efficiency.3,4 Liver
MELD era, black patients were more likely to die on the wait-
allocation was perceived to be too arbitrary, too easily ma-
ing list than white patients.7 The article by Moylan et al shows
nipulated, and overly reliant on waiting time. Furthermore,
that following MELD, there were no significant racial or eth-
major regional differences were found in the rates of patient
nic differences in time waiting or waiting list deaths. This
death while on the waiting list. To address these issues, the
finding represents an important improvement in the eq-
Institute of Medicine (IOM) recommended to the US Depart-
uity of the organ allocation system. However, Moylan et al
ment of Health and Human Services that a novel system of
also identified a persistent disparity between women and men
organ allocation be defined based solely on medical criteria.3
in access to liver transplantation.
In response, the transplant community developed and imple-
The reduction in waitlist mortality for black patients is
mented the current system of liver allocation that prioritizes
likely multifactorial and may in fact not guarantee an equal
patients on the basis of severity of illness, as assessed by the
opportunity to obtain a liver transplant. The transplant pro-
Model of End-Stage Liver Disease (MELD) score. The MELD
cess requires a complex pretransplant evaluation. Before
score is calculated by using 3 laboratory test results (creati-
MELD, early referral for evaluation often resulted in more
nine, bilirubin, and international normalized ratio), which are
rapid listing and a correspondingly greater opportunity to
objective measures of the degree of organ dysfunction and risk
accrue waiting time before clinical decompensation. Be-
of death. Under the MELD allocation system, the patient with
cause patients without private health insurance are signifi-
the greatest chance of dying without a transplant is allocated
cantly less likely to be referred for specialist care, they were
the next available organ regardless of the time the patient has
spent on the waiting list. Author Affiliations: Department of Surgery, Dartmouth-Hitchcock Medical Cen-
The clinical benefits of the MELD allocation system have ter, Lebanon, New Hampshire (Dr Axelrod); and Department of Transplantation,
been well documented. Implementation of the MELD sys- Division of Surgery, Lahey Clinic Medical Center, Burlington, Massachusetts
(Dr Pomfret).
Corresponding Author: David A. Axelrod, MD, MBA, Department of Surgery,
See also p 2371. Dartmouth-Hitchcock Medical Center, 1 Medical Center Dr, Lebanon, NH 03756
(david.axelrod@hitchcock.org).
©2008 American Medical Association. All rights reserved. (Reprinted) JAMA, November 26, 2008—Vol 300, No. 20 2425
Downloaded from jama.ama-assn.org at Vanderbilt University on November 7, 2011
EDITORIAL
often evaluated and listed too late. Under MELD, late list- (P⬍ .001).9 This difference directly correlates into a higher
ing does not preclude transplantation as it often did in the death rate on the waiting list. By adjusting for these re-
system based on waiting time. However, as demonstrated gional differences, Moylan et al6 may have diminished the
by Moylan et al, black patients are still listed with higher ongoing disparity in access for black patients who are largely
MELD scores and for a shorter period, suggesting that the concentrated in larger urban areas with longer waiting times.
access barriers remain even under the new system. In ad- It is likely that women, especially those who are often less
dition, black patients continue to have a higher rate of liver able to travel due to other responsibilities and those with-
disease than the national average, but represent a smaller out health insurance, are likewise systematically less able
proportion of transplant recipients. Thus, it is likely that many to access this lifesaving resource.
black patients are never listed due to advanced disease at When compared with the system before 2002, the cur-
presentation as a result of late referral. This problem is out- rent MELD system is clearly a step toward achieving the goal
side of the scope of the allocation system, however, and needs of an equitable, efficient, and transparent organ allocation
a broader solution. system. The MELD system appears to have reduced, but likely
The sex disparity is likely a reflection of several factors, not eliminated, differential access based on race and eth-
including a limitation in the MELD calculation, body and nicity. However, modest differences based on sex persist,
organ size considerations, and potentially differences in the but could be addressed by revisions in the organ allocation
etiology of the underlying liver disease. Because women have policy to ensure that MELD scores are comparable across
less body mass, the inclusion of creatinine rather than weight- sexes. The real challenge facing the liver transplant com-
adjusted glomerular filtration rate in the MELD score is likely munity is to tackle the long-standing disparity of geogra-
to underestimate their degree of renal dysfunction. Thus, phy. If those who can afford to travel can receive organ trans-
MELD scores will be lower in women than in men with the plants at lower MELD scores more rapidly, the system will
same degree of renal failure, decreasing women’s access to remain fundamentally inequitable.10 The current construc-
liver allografts. Women are also smaller, limiting the pool tion of DSAs and UNOS regions is largely an accident of his-
of available organs. Women may wait longer for a size- tory. As recognized by the IOM, achieving the goals of or-
appropriate organ because livers from pediatric donors are gan allocation requires the creation of equivalent size regions
preferentially allocated to children awaiting transplanta- to match supply and demand. The transplant community
tion. In addition, a small organ can be used in a larger in- should be acknowledged for the progress achieved thus far
dividual, but the converse is not always possible. More- in reducing racial and sex disparities, and should be en-
over, women are more likely than men to have autoimmune couraged to take the next difficult step in further reducing
liver diseases, including primary biliary cirrhosis and pri- geographic disparities.
mary sclerosing cholangitis, both of which are less likely than
Financial Disclosures: None reported.
hepatitis C to lead to kidney dysfunction and higher MELD
scores. From the data presented by Moylan et al, it appears
REFERENCES
logical to adjust the MELD score based on sex to ensure that
the risk of death is comparable for men and women who 1. Freeman RB Jr, Steffick DE, Guidinger MK, Farmer DG, Berg CL, Merion RM.
Liver and intestine transplantation in the United States, 1997-2006. Am J Transplant.
have the same MELD score. Consideration should also be 2008;8(4 pt 2):958-976.
given to expanding access to pediatric donors for women 2. Schaubel DE, Sima CS, Goodrich NP, Feng S, Merion RM. The survival benefit
of deceased donor liver transplantation as a function of candidate disease severity
who are less than a certain weight or size. and donor quality. Am J Transplant. 2008;8(2):419-425.
Although MELD has reduced the disparity based on some 3. Organ Procurement and Transplantation. Assessing Current Policies and the
Potential Impact of the DHHS Final Rule: Committee on Organ Procurement and
demographic characteristics, it has not met the IOM direc- Transplantation Policy, Division of Health Sciences Policy, Institute of Medicine.
tive to reduce geographic disparity. Under existing prac- Washington, DC: National Academy Press; 1999.
tice, the nation is divided into 11 regions by UNOS, each of 4. Freeman RB Jr, Wiesner RH, Harper A, et al; UNOS/OPTN Liver Disease Se-
verity Score, UNOS/OPTN Liver and Intestine, and UNOS/OPTN Pediatric Trans-
which is composed of 1 or more donation service areas plantation Committees. The new liver allocation system: moving toward evidence-
(DSAs). These regions vary substantially in terms of popu- based transplantation policy. Liver Transpl. 2002;8(9):851-858.
5. Merion RM, Schaubel DE, Dykstra DM, Freeman RB, Port FK, Wolfe RA. The
lation size and number of deceased donors. In the analysis survival benefit of liver transplantation. Am J Transplant. 2005;5(2):307-313.
by Moylan et al, as well as many other studies, survival with 6. Moylan CA, Brady CW, Johnson JL, Smith AD, Tuttle-Newhall JE, Muir AJ. Dis-
parities in liver transplantation before and after introduction of the MELD score.
end-stage liver disease is determined in large part by where JAMA. 2008;300(20):2371-2378.
the patient lives, not by the patient’s race or sex. As in poli- 7. Reid AE, Resnick M, Chang Y, Buerstatte N, Weissman JS. Disparity in use of
tics, right now, all allocation is local. Patients who live in orthotopic liver transplantation among blacks and whites. Liver Transpl. 2004;
10(7):834-841.
(or have the money to travel to) regions with a higher ratio 8. Pomfret EA, Fryer JP, Sima CS, Lake JR, Merion RM. Liver and intestine trans-
of donors to transplant candidates can receive organ trans- plantation in the United States, 1996-2005. Am J Transplant. 2007;7(5 pt 2):
1376-1389.
plants far earlier and at a lower MELD score.8 The disparity 9. Trotter JF, Osgood MJ. MELD scores of liver transplant recipients according to
is even greater at the DSA level. In small DSAs, the percent- size of waiting list: impact of organ allocation and patient outcomes. JAMA. 2004;
291(15):1871-1874.
age of recipients who receive transplants at low MELD scores 10. Ubel PA, Caplan AL. Geographic favoritism in liver transplantation: unfortu-
(11-18) was 47% compared with only 23% in large DSAs nate or unfair? N Engl J Med. 1998;339(18):1322-1325.
2426 JAMA, November 26, 2008—Vol 300, No. 20 (Reprinted) ©2008 American Medical Association. All rights reserved.
Downloaded from jama.ama-assn.org at Vanderbilt University on November 7, 2011
You might also like
- PHC 6517 Answer Key For Assignment #4: Patient Care PracticesDocument4 pagesPHC 6517 Answer Key For Assignment #4: Patient Care PracticesCarolina ZapataNo ratings yet
- Quiz MicrobiologyDocument65 pagesQuiz MicrobiologyMedShare98% (51)
- The Model For End-Stage Liver DiseaseDocument9 pagesThe Model For End-Stage Liver Diseasegwyneth.green.512No ratings yet
- #x201c Beyond MELD” – Emerging StraDocument12 pages#x201c Beyond MELD” – Emerging StraCláudia SilvaNo ratings yet
- What Matters For Liver Transplant in Severe ACLF - Medpage Today Dec 28 2018-MergedDocument21 pagesWhat Matters For Liver Transplant in Severe ACLF - Medpage Today Dec 28 2018-MergedUKNo ratings yet
- Gait Speed, Grip Strength, and Clinical Outcomes in Older Patients With Hematologic MalignanciesDocument9 pagesGait Speed, Grip Strength, and Clinical Outcomes in Older Patients With Hematologic MalignanciesTícia RanessaNo ratings yet
- FMD Nature Paper s41467-024-45260-9Document13 pagesFMD Nature Paper s41467-024-45260-9davidbearx3No ratings yet
- Comparative Survival and Economic Benefits of Deceased Donor Kidney Transplantation and Dialysis in People With Varying Ages and Co-MorbiditiesDocument9 pagesComparative Survival and Economic Benefits of Deceased Donor Kidney Transplantation and Dialysis in People With Varying Ages and Co-MorbiditieslopovNo ratings yet
- Xenotransplantation - The Current Status and ProspectsDocument10 pagesXenotransplantation - The Current Status and ProspectsSivaNo ratings yet
- Brown 2006Document18 pagesBrown 2006Arif Erdem KöroğluNo ratings yet
- Cardiometabolic Outcomes PDFDocument11 pagesCardiometabolic Outcomes PDFSarah CrausNo ratings yet
- Metastasis Patterns and PrognoDocument17 pagesMetastasis Patterns and Prognosatria divaNo ratings yet
- Associations of Pretransplant Weight and Muscle.32Document11 pagesAssociations of Pretransplant Weight and Muscle.32m.m.tomeh95No ratings yet
- AASLD LTX GuidelinesDocument14 pagesAASLD LTX GuidelineswpolidoNo ratings yet
- 1 s2.0 S1083879120306686 MainDocument2 pages1 s2.0 S1083879120306686 MainCommon JaiswalNo ratings yet
- Biology of Blood and Marrow Transplantation: Sudipto Mukherjee, Dominic Boccaccio, Mikkael A. Sekeres, Edward CopelanDocument9 pagesBiology of Blood and Marrow Transplantation: Sudipto Mukherjee, Dominic Boccaccio, Mikkael A. Sekeres, Edward CopelanFran QuagliarielloNo ratings yet
- Autologous Stem Cell TransplantDocument7 pagesAutologous Stem Cell TransplantgauravsinghalNo ratings yet
- Jamapediatrics Chang 2018 Oi 180059Document8 pagesJamapediatrics Chang 2018 Oi 180059juan lopezNo ratings yet
- NIH Public Access: Author ManuscriptDocument4 pagesNIH Public Access: Author ManuscriptAlex OlahNo ratings yet
- Patient and Graft Survival ImplicationsDocument11 pagesPatient and Graft Survival ImplicationsAnaNo ratings yet
- 2012 Guides Blood TransfusionDocument4 pages2012 Guides Blood TransfusionRandy Mar TagudarNo ratings yet
- Paper 2 Cancer DicoveryDocument18 pagesPaper 2 Cancer DicoverySuraj ShahNo ratings yet
- 6348 FullDocument9 pages6348 FullpakemainmainNo ratings yet
- Cancer Stem Cells: A Review From Origin To Therapeutic ImplicationsDocument9 pagesCancer Stem Cells: A Review From Origin To Therapeutic ImplicationsJoyatideb SinhaNo ratings yet
- 79 BioTek Ebook FINAL - CompressedDocument63 pages79 BioTek Ebook FINAL - CompressedMichelleNo ratings yet
- Targeted Based Drug Delivery System ForDocument12 pagesTargeted Based Drug Delivery System ForElena CaterevNo ratings yet
- J Jacc 2023 01 027Document11 pagesJ Jacc 2023 01 027ERIK EDUARDO BRICEÑO GÓMEZNo ratings yet
- Feasibility and Outcome of Haploidentical Hematopoietic Stem Cell Transplant With Post Transplantation Cyclophosphamide in High Risk Malignancies in ChildrenDocument4 pagesFeasibility and Outcome of Haploidentical Hematopoietic Stem Cell Transplant With Post Transplantation Cyclophosphamide in High Risk Malignancies in ChildrenHerald Scholarly Open AccessNo ratings yet
- CPG Liver Transplantation JHEPAT 5856Document53 pagesCPG Liver Transplantation JHEPAT 5856Jorge AlvarezNo ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofFajar PramaduNo ratings yet
- Cost-Effectiveness in A Flat World - Can Icds Help The United States Get Rhythm?Document3 pagesCost-Effectiveness in A Flat World - Can Icds Help The United States Get Rhythm?Rui FonteNo ratings yet
- Jco 23 00280Document6 pagesJco 23 00280Julio MineraNo ratings yet
- Current Concepts and Future Perspectives of Stem Cell Therapy in Peripheral Arterial DiseaseDocument3 pagesCurrent Concepts and Future Perspectives of Stem Cell Therapy in Peripheral Arterial DiseaseAyushmanNo ratings yet
- Original Article: Saudi Journal of Kidney Diseases and TransplantationDocument5 pagesOriginal Article: Saudi Journal of Kidney Diseases and TransplantationNiponis ChunchunNo ratings yet
- MS Research Proposal Exosomes NDDSDocument8 pagesMS Research Proposal Exosomes NDDSmuhammad wajahatNo ratings yet
- A Novel Waitlist Dropout Score For Hepatocellular Carcinoma - Identifying A Threshold That Predicts Worse Post-Transplant SurvivalDocument9 pagesA Novel Waitlist Dropout Score For Hepatocellular Carcinoma - Identifying A Threshold That Predicts Worse Post-Transplant SurvivalHadi KuriryNo ratings yet
- Sangre FrescaDocument9 pagesSangre FrescaRobinson Trujillo CabanillaNo ratings yet
- Colorectal Cancer Screening: Clinical ApplicationsDocument6 pagesColorectal Cancer Screening: Clinical ApplicationsChâu Khắc ToànNo ratings yet
- How I Treat Acute Myeloid LeukemiaDocument10 pagesHow I Treat Acute Myeloid LeukemiaSutiara Prihatining TyasNo ratings yet
- Resistance After Selective Decontamination 𠄽ocument2 pagesResistance After Selective Decontamination –Kyomukama Racheal ClaireNo ratings yet
- Evidence Based Care For All Patients - AjmDocument3 pagesEvidence Based Care For All Patients - Ajmdaniel martinNo ratings yet
- Jamaoncol 2015 3336Document8 pagesJamaoncol 2015 3336malvindersahiNo ratings yet
- Evaluation - For LT - in - Adults - Hep26972 - 0Document22 pagesEvaluation - For LT - in - Adults - Hep26972 - 0edwardmenesesNo ratings yet
- Wood 2004Document10 pagesWood 2004Mariano DomanicoNo ratings yet
- Prognostic and Predictive Factors Revisited: BreastDocument7 pagesPrognostic and Predictive Factors Revisited: BreastAndersson SaenzNo ratings yet
- Assessment of Tumor Infiltrating Lymphocytes Using.12Document9 pagesAssessment of Tumor Infiltrating Lymphocytes Using.12Muhammad Rifki100% (1)
- Review LESDocument16 pagesReview LESyoNo ratings yet
- Ajt 16318Document43 pagesAjt 16318ricardo arreguiNo ratings yet
- Article AgainDocument12 pagesArticle AgainMaya Putri HaryantiNo ratings yet
- Challenges in Organ TransplantationDocument10 pagesChallenges in Organ TransplantationBrie100% (1)
- gfr514 PDFDocument7 pagesgfr514 PDFnita noviantariNo ratings yet
- Digital Commons@Becker Digital Commons@BeckerDocument15 pagesDigital Commons@Becker Digital Commons@Beckerre septian IlhamsyahNo ratings yet
- Evaluating Ebola Therapies The Case For RCTsDocument3 pagesEvaluating Ebola Therapies The Case For RCTsHana AntonioNo ratings yet
- A Gift of Life Deserves Compensation: How To Increase Living Kidney Donation With Realistic Incentives, Cato Policy Analysis No. 604Document24 pagesA Gift of Life Deserves Compensation: How To Increase Living Kidney Donation With Realistic Incentives, Cato Policy Analysis No. 604Cato Institute100% (1)
- WJG 19 1625Document7 pagesWJG 19 1625Daniel MagalhãesNo ratings yet
- WJN 4 148Document13 pagesWJN 4 148Rafela Agatha ChristyNo ratings yet
- A Radiologist's Guide To The 2021 WHO Central Nervous System Tumor ClassificationDocument15 pagesA Radiologist's Guide To The 2021 WHO Central Nervous System Tumor ClassificationMANGNo ratings yet
- Periodontal TreatmentDocument21 pagesPeriodontal TreatmentAdyas AdrianaNo ratings yet
- 24 Guias Jama para ScreeningDocument7 pages24 Guias Jama para ScreeningCristhian Alvarez Del ValleNo ratings yet
- Paradoja de La Obesidad en HemodiálisisDocument11 pagesParadoja de La Obesidad en Hemodiálisisa.glaves.bNo ratings yet
- Bloodadvances 2022007569Document20 pagesBloodadvances 2022007569Yilianeth Mena DazaNo ratings yet
- Understanding The Stem Cell Transplantation Process, A Guide for Patients, Caregivers, and Loved Ones, July 2016From EverandUnderstanding The Stem Cell Transplantation Process, A Guide for Patients, Caregivers, and Loved Ones, July 2016No ratings yet
- Unit I. Introduction To Microbiology - EditedDocument33 pagesUnit I. Introduction To Microbiology - EditedadlskjflkdfkljdsNo ratings yet
- (You're Somebody's Type, Have A Lionheart's Vibe!) : StudentsDocument3 pages(You're Somebody's Type, Have A Lionheart's Vibe!) : StudentsJems AquinoNo ratings yet
- Gangren Diabetikum-Baca BTKVDocument21 pagesGangren Diabetikum-Baca BTKVridza_lubisNo ratings yet
- EPA Air Quality Index School Activity ChartDocument2 pagesEPA Air Quality Index School Activity ChartCourier JournalNo ratings yet
- Mathematical and Sensitivity Analysis On The Dynamics of Cholera Epidemic Model With VaccinationDocument11 pagesMathematical and Sensitivity Analysis On The Dynamics of Cholera Epidemic Model With VaccinationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- PP Insect Bite 2007Document16 pagesPP Insect Bite 2007Ali RumiNo ratings yet
- Final GIT Case PresentationDocument53 pagesFinal GIT Case PresentationRovan100% (1)
- Phytotherapy RSDocument34 pagesPhytotherapy RSyousernameNo ratings yet
- Simulasi TOEFL Buku EdukasiDocument28 pagesSimulasi TOEFL Buku EdukasiMuhammad Sudrajad100% (1)
- Sheehan Syndrome Lancet Eponym 2003Document3 pagesSheehan Syndrome Lancet Eponym 2003Alejandro GuillenNo ratings yet
- SLE234 Lab Report 1 - 2018Document3 pagesSLE234 Lab Report 1 - 2018Wafaa AdamNo ratings yet
- Rehan AfsarDocument55 pagesRehan AfsarEngr Syed Numan ShahNo ratings yet
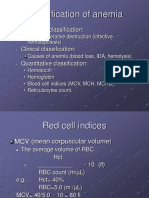
- Classification of AnemiaDocument8 pagesClassification of AnemiaHelao SilasNo ratings yet
- Food Safety Case - The Fat Duck Norovirus Outbreak, UK - 2009Document16 pagesFood Safety Case - The Fat Duck Norovirus Outbreak, UK - 2009OPGJrNo ratings yet
- Soal BedahDocument47 pagesSoal BedahDwi SulistyowatiNo ratings yet
- Get The Facts About Tuberculosis DiseaseDocument16 pagesGet The Facts About Tuberculosis Diseasedjprh tbdotsNo ratings yet
- 108 PDFDocument7 pages108 PDFpuspa sariNo ratings yet
- Communicable DiseasesDocument22 pagesCommunicable DiseaseskaramnNo ratings yet
- Reviewer in MicrobiologyDocument5 pagesReviewer in MicrobiologyLuzNo ratings yet
- Acute Tubular NecrosisDocument2 pagesAcute Tubular NecrosisGlogogeanu Cristina AndreeaNo ratings yet
- Septic Arthritis of The Wrist: Review ArticleDocument7 pagesSeptic Arthritis of The Wrist: Review ArticleDwiNo ratings yet
- San Luis, Trio - ActivityDocument4 pagesSan Luis, Trio - ActivityTrio San Luis100% (1)
- Kamal 2009Document14 pagesKamal 2009seruniallisaaslimNo ratings yet
- The Edge 9 June 2021Document26 pagesThe Edge 9 June 2021Amir HasridzNo ratings yet
- UNSMA2012ING999 54bd421b PDFDocument10 pagesUNSMA2012ING999 54bd421b PDFAgusSupriyonoNo ratings yet
- African Swine Fever: Now in WidespreadDocument2 pagesAfrican Swine Fever: Now in WidespreadMariaGlenda Dellosa Guevara-YusonNo ratings yet
- Research PaperDocument5 pagesResearch PaperAnnie OmlangNo ratings yet
- Assignment On Epidemiology (Relation Between Incidence and Prevalence)Document6 pagesAssignment On Epidemiology (Relation Between Incidence and Prevalence)Suraj_Subedi100% (1)