Professional Documents
Culture Documents
JMarMedSoc19287-6429589 175135
JMarMedSoc19287-6429589 175135
Uploaded by
Johan GautamaCopyright:
Available Formats
You might also like
- Module 2 Lesson 3 MISSIONARY RESPONSEDocument1 pageModule 2 Lesson 3 MISSIONARY RESPONSEHarriz Diether DomingoNo ratings yet
- Kirschen2000 - The Royal London Space Planning - Part 1Document8 pagesKirschen2000 - The Royal London Space Planning - Part 1drgeorgejose7818100% (2)
- 1.irosun OgbeDocument10 pages1.irosun OgbeOmo Awo Ifasina Aworeni91% (11)
- Effective Classroom ManagementDocument24 pagesEffective Classroom ManagementAmbrosious100% (1)
- Second-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceDocument10 pagesSecond-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceSitaNo ratings yet
- Levamisole Therapy in Children With Frequently Relapsing and Steroid-Dependent Nephrotic Syndrome - A Single-Center ExperienceDocument5 pagesLevamisole Therapy in Children With Frequently Relapsing and Steroid-Dependent Nephrotic Syndrome - A Single-Center ExperienceGading AuroraNo ratings yet
- Efficacy of Higher-Dose Levamisole in Maintaining Remission in Steroid-Dependant Nephrotic SyndromeDocument6 pagesEfficacy of Higher-Dose Levamisole in Maintaining Remission in Steroid-Dependant Nephrotic Syndromechandra maslikhaNo ratings yet
- Effectiveness and Adverse Drug Reactions of Levetiracetam and Midazolam in Refractory Neonatal Seizure: A Cross Sectional Comparative StudyDocument6 pagesEffectiveness and Adverse Drug Reactions of Levetiracetam and Midazolam in Refractory Neonatal Seizure: A Cross Sectional Comparative StudySultan Rahmat SeptianNo ratings yet
- Nuevos Antiepilépticos 2013Document8 pagesNuevos Antiepilépticos 2013Andres RodriguezNo ratings yet
- AhmadDocument6 pagesAhmadtengku maulanaNo ratings yet
- JurnalDocument8 pagesJurnalIndahNo ratings yet
- COPOUSEUPDocument8 pagesCOPOUSEUPamazedNo ratings yet
- Safety and Effectiveness of Lurasidone in Adolescents With Schizophrenia: Results of A 2-Year, Open-Label Extension StudyDocument11 pagesSafety and Effectiveness of Lurasidone in Adolescents With Schizophrenia: Results of A 2-Year, Open-Label Extension StudyNaiana PaulaNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916Sriram NagarajanNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916srirampharmNo ratings yet
- Childhood Nephrotic Syndrome: Steroid Sensitive, Steroid Resistant and BeyondDocument7 pagesChildhood Nephrotic Syndrome: Steroid Sensitive, Steroid Resistant and BeyondDorin Cristian AntalNo ratings yet
- Jurnal Baru 2Document6 pagesJurnal Baru 2FIRDA RIDHAYANINo ratings yet
- Comparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile Seizures PDFDocument5 pagesComparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile Seizures PDFCharina Geofhany DeboraNo ratings yet
- WJM 7 25Document9 pagesWJM 7 25Ainna SavitaNo ratings yet
- A Single-Centre Retrospective Study of The Safety and Ef Ficacy of Mycophenolate Mofetil in Children and Adolescents With Nephrotic SyndromeDocument6 pagesA Single-Centre Retrospective Study of The Safety and Ef Ficacy of Mycophenolate Mofetil in Children and Adolescents With Nephrotic SyndromeBakul TapeNo ratings yet
- Efficacy of Rituximab Therapy in Children With Nephrotic Syndrome: A 10-Year Experience From An Iranian Pediatric HospitalDocument9 pagesEfficacy of Rituximab Therapy in Children With Nephrotic Syndrome: A 10-Year Experience From An Iranian Pediatric HospitalAris BayuNo ratings yet
- The Effects of Dexamethasone On Sleep in Young Children With Acute Lymphoblastic LeukemiaDocument7 pagesThe Effects of Dexamethasone On Sleep in Young Children With Acute Lymphoblastic LeukemiaAndrye FernandesNo ratings yet
- Desvenlafaxine Versus Placebo in The TreatmentDocument12 pagesDesvenlafaxine Versus Placebo in The TreatmentNatalia OlmosNo ratings yet
- Incidence and Predictors of Adverse Drug Events Among People Receiving Drug Resistant Tuberculosis Treatment in Uganda 8-Year Retrospective Cohort STDocument12 pagesIncidence and Predictors of Adverse Drug Events Among People Receiving Drug Resistant Tuberculosis Treatment in Uganda 8-Year Retrospective Cohort STEghar EverydayishellNo ratings yet
- MagnascoDocument8 pagesMagnascoMeliana SulistioNo ratings yet
- Final NS Guidelines August 26 2019-1Document17 pagesFinal NS Guidelines August 26 2019-1Nido MalghaniNo ratings yet
- Adverse Drug Reaction Profile of Oseltamivir in Children: Research PaperDocument4 pagesAdverse Drug Reaction Profile of Oseltamivir in Children: Research PaperRega PermanaNo ratings yet
- 15-Polyphenol Nano Cancer ReviewDocument14 pages15-Polyphenol Nano Cancer Reviewmohamed lamrana jallohNo ratings yet
- 10126-Article Text-75914-1-10-20181208Document5 pages10126-Article Text-75914-1-10-20181208Odessa EnriquezNo ratings yet
- Lacosamide 1Document6 pagesLacosamide 1ezio93No ratings yet
- Seizure: U Nsal Yılmaz, Tuba Sevim Yılmaz, Gu Ls en Dizdarer, Gu LC in Akıncı, Orkide Gu Zel, Hasan Tekgu LDocument8 pagesSeizure: U Nsal Yılmaz, Tuba Sevim Yılmaz, Gu Ls en Dizdarer, Gu LC in Akıncı, Orkide Gu Zel, Hasan Tekgu LDHIVYANo ratings yet
- Ixazomib, Lenalidomide, and Dexamethasone PDFDocument14 pagesIxazomib, Lenalidomide, and Dexamethasone PDFJLNo ratings yet
- Therapeutic Use of Medicinal Cannabis in Dif Ficult To Manage EpilepsyDocument3 pagesTherapeutic Use of Medicinal Cannabis in Dif Ficult To Manage EpilepsyEnrique Molina LeonNo ratings yet
- Utilization of The Naranjo Scale To Evaluate Adverse Drug Reactions at A Free-Standing Children's HospitalDocument10 pagesUtilization of The Naranjo Scale To Evaluate Adverse Drug Reactions at A Free-Standing Children's HospitalSheerazNo ratings yet
- Risperidone Use in Autism SpectrumDocument5 pagesRisperidone Use in Autism SpectrumAdina CipariuNo ratings yet
- Uongffd TtyddfyDocument7 pagesUongffd TtyddfyVsbshNo ratings yet
- C PDFDocument11 pagesC PDFNadiea FetrisiaNo ratings yet
- Onasemnogene Abeparvovec For SMADocument2 pagesOnasemnogene Abeparvovec For SMAsurbhib268No ratings yet
- Biomedicines 11 03039Document14 pagesBiomedicines 11 03039Hans Kristian LorenzoNo ratings yet
- Prolonged Sedation And/or Analgesia and 5-Year Neurodevelopment Outcome in Very Preterm InfantsDocument6 pagesProlonged Sedation And/or Analgesia and 5-Year Neurodevelopment Outcome in Very Preterm InfantsmustafasacarNo ratings yet
- HamdDocument12 pagesHamdAldiola PerdanaNo ratings yet
- Use of A LowDocument8 pagesUse of A Lowirma suwandi sadikinNo ratings yet
- Dress Syndrome A Review and UpdateDocument5 pagesDress Syndrome A Review and UpdateCarlos Alberto Torres LópezNo ratings yet
- 1 MultimethodassessmentDocument8 pages1 MultimethodassessmentRoberto Alexis Molina CampuzanoNo ratings yet
- Comparison Predni and Dexa in Treatment of CroupDocument6 pagesComparison Predni and Dexa in Treatment of CroupBangkit Brillian FauziNo ratings yet
- Multiple SclerosisDocument15 pagesMultiple SclerosisThong MinyewNo ratings yet
- Treatment Outcomes of Oral Propranolol in The TreaDocument7 pagesTreatment Outcomes of Oral Propranolol in The TreabokobokobokanNo ratings yet
- Effect of Play Based... 2017Document5 pagesEffect of Play Based... 2017gemita aldeaNo ratings yet
- Dress Syndrome: A Review and Update: March 2016Document5 pagesDress Syndrome: A Review and Update: March 2016Carlos LuqueNo ratings yet
- Jurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresDocument15 pagesJurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresAnida HasnaNo ratings yet
- Nebulised Steroid in The Treatment of Croup: A Systematic Review of Randomised Controlled TrialsDocument7 pagesNebulised Steroid in The Treatment of Croup: A Systematic Review of Randomised Controlled TrialsSatriyo BagasNo ratings yet
- A Randomized Controlled Trial of Intranasal-Midazolam Versus Intravenous-Diazepam For Acute Childhood SeizuresDocument5 pagesA Randomized Controlled Trial of Intranasal-Midazolam Versus Intravenous-Diazepam For Acute Childhood SeizuresAdriel Chandra AngNo ratings yet
- 8 Sivakumar Et AlDocument7 pages8 Sivakumar Et Alkhalid alharbiNo ratings yet
- Nej Mo A 1109997Document10 pagesNej Mo A 1109997juan hurtadoNo ratings yet
- Comparative Study of The Efficacy and Safety of Topical Antifungal Agents Clotrimazole Versus Sertaconazole in The Treatment of Tinea Corporis/crurisDocument5 pagesComparative Study of The Efficacy and Safety of Topical Antifungal Agents Clotrimazole Versus Sertaconazole in The Treatment of Tinea Corporis/crurisRasyid Ali NatioNo ratings yet
- Kortikosteroid Nephrotic SyndromeDocument7 pagesKortikosteroid Nephrotic SyndromeDevi Albaiti JannatiNo ratings yet
- Pediatric Neurology: Hye-Ryun Yeh MD, Min-Jee Kim MD, Tae-Sung Ko MD, PHD, Mi-Sun Yum MD, PHD, Su-Jeong You MD, PHDDocument6 pagesPediatric Neurology: Hye-Ryun Yeh MD, Min-Jee Kim MD, Tae-Sung Ko MD, PHD, Mi-Sun Yum MD, PHD, Su-Jeong You MD, PHDAdrian KhomanNo ratings yet
- Rituximab Tullus Kjeil 2021Document9 pagesRituximab Tullus Kjeil 2021Carmen MunteanNo ratings yet
- Ref 11Document5 pagesRef 11Tiago BaraNo ratings yet
- Kulit3 PDFDocument5 pagesKulit3 PDFAhmad LabibNo ratings yet
- OtorhinolaryngologyDocument7 pagesOtorhinolaryngologyDeniNo ratings yet
- BMC NephrologyDocument10 pagesBMC Nephrologyselandia nisrinaNo ratings yet
- The Essential Guide to Prescription Drugs, Update on RemdesivirFrom EverandThe Essential Guide to Prescription Drugs, Update on RemdesivirNo ratings yet
- Buku Saku IdaiDocument1 pageBuku Saku IdaiJohan GautamaNo ratings yet
- Jurnal HemaDocument38 pagesJurnal HemaJohan GautamaNo ratings yet
- Pic Asi SeduniaDocument3 pagesPic Asi SeduniaJohan GautamaNo ratings yet
- Sepsis in Child With Burn Trauma: Death Case ReportDocument22 pagesSepsis in Child With Burn Trauma: Death Case ReportJohan GautamaNo ratings yet
- Cerebral Palsy NMPRA Conference SubmissionDocument61 pagesCerebral Palsy NMPRA Conference SubmissionJohan GautamaNo ratings yet
- Psychology and The Challenges of Life 13th Edition Nevid Solutions ManualDocument73 pagesPsychology and The Challenges of Life 13th Edition Nevid Solutions Manualbrianwoodsnjyoxepibt100% (14)
- Een Liefdesbrief Aan Amsterdam (By Ryan Bartek)Document5 pagesEen Liefdesbrief Aan Amsterdam (By Ryan Bartek)Ryan Bartek100% (1)
- Notified Vide SRO No. 575 Dated 22 May 2019Document3 pagesNotified Vide SRO No. 575 Dated 22 May 2019Hussain RahibNo ratings yet
- EverFlo Broch PDFDocument6 pagesEverFlo Broch PDFAdnan HuskicNo ratings yet
- Atlan A300 A300xl Pi 9107089 en MasterDocument12 pagesAtlan A300 A300xl Pi 9107089 en MasterHanh NguyenNo ratings yet
- KRAUSE 2016 Standard Catalog O1901-2000 20th Century 43rd Ed 381Document1 pageKRAUSE 2016 Standard Catalog O1901-2000 20th Century 43rd Ed 381Millona usdNo ratings yet
- KGianan-Stem12-Physics2 (Chapters 1-3)Document9 pagesKGianan-Stem12-Physics2 (Chapters 1-3)Kyle GiananNo ratings yet
- Gaius SMW Incest Sister BrotherDocument5 pagesGaius SMW Incest Sister BrotherShyam BhatNo ratings yet
- Cat Dissection ProjectDocument12 pagesCat Dissection Projectapi-309363754No ratings yet
- MSP TT MSP Al Leaflet en w4156 1Document8 pagesMSP TT MSP Al Leaflet en w4156 1serban_elNo ratings yet
- Aplus Coating Report FormatDocument1 pageAplus Coating Report FormatNnamdi AmadiNo ratings yet
- Quality Management Principles For Excellence: by - Sacchidanand Gogawale, Zen International SystemsDocument5 pagesQuality Management Principles For Excellence: by - Sacchidanand Gogawale, Zen International SystemsSanjeevani GogawaleNo ratings yet
- GMCO FOR INDUSTRIAL SERVICES - Welding Procedure SpecificationsDocument2 pagesGMCO FOR INDUSTRIAL SERVICES - Welding Procedure SpecificationsMohamedNo ratings yet
- CV Sayeed TeachingDocument8 pagesCV Sayeed TeachingGopal ReddyNo ratings yet
- Psychological TheoriesDocument19 pagesPsychological TheoriesYapieeNo ratings yet
- Asl Curriculum Writing 2021-2022Document20 pagesAsl Curriculum Writing 2021-2022api-589645770No ratings yet
- MFG Fiberglass Column Forms Product SheetDocument3 pagesMFG Fiberglass Column Forms Product SheetAboalmaail AlaminNo ratings yet
- Q.1 Write Short Answers of The Following Questions: Ghazali Guess Chemistry 1 10thDocument9 pagesQ.1 Write Short Answers of The Following Questions: Ghazali Guess Chemistry 1 10thAwais AliNo ratings yet
- Out 10Document12 pagesOut 10restu anindityaNo ratings yet
- A Mnemonic For The Treatment of HyperkalemiaDocument3 pagesA Mnemonic For The Treatment of Hyperkalemiakhangsiean89No ratings yet
- Zamil Product Brochure PDFDocument30 pagesZamil Product Brochure PDFZameer KhanNo ratings yet
- EJMCM - Volume 7 - Issue 11 - Pages 9184-9190Document7 pagesEJMCM - Volume 7 - Issue 11 - Pages 9184-9190Akshay BeradNo ratings yet
- Technical Data BCC 1250P-50 BCC 1400S-50: 50 Hz Cos Φ = 0.8 3-PhaseDocument3 pagesTechnical Data BCC 1250P-50 BCC 1400S-50: 50 Hz Cos Φ = 0.8 3-PhaseHectrateNo ratings yet
- Unsafe Act Danger of Horseplay at WorkDocument1 pageUnsafe Act Danger of Horseplay at WorkSn AhsanNo ratings yet
- 08 Proceduri de UrgentaDocument9 pages08 Proceduri de UrgentaSorescu Radu VasileNo ratings yet
- PU LPH 80540 80553 Esite GBDocument7 pagesPU LPH 80540 80553 Esite GBAl-Alamiya TradeNo ratings yet
JMarMedSoc19287-6429589 175135
JMarMedSoc19287-6429589 175135
Uploaded by
Johan GautamaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JMarMedSoc19287-6429589 175135
JMarMedSoc19287-6429589 175135
Uploaded by
Johan GautamaCopyright:
Available Formats
[Downloaded free from http://www.marinemedicalsociety.in on Wednesday, March 21, 2018, IP: 110.136.238.
52]
Original Article
Use of Levamisole in Children with Nephrotic Syndrome:
A Retrospective Study to Examine its Adverse Effects in
Children with Nephrotic Syndrome
Lt Col Suprita Kalra1,2, Maj Gen Madhuri Kanitkar VSM2, Kara Tiewsoh3
1
Department of Pediatrics, Command Hospital, 2Dean and Deputy Commandant, AFMC, Pune, Maharashtra, 3Department of Pediatrics, PGIMER, Chandigarh, India
Abstract
Introduction: Levamisole, a synthetic imidazothiazole derivative has been used as a steroid sparing agent in children with Frequently Relapsing
Nephrotic Syndrome (FRNS) and Steroid Dependent Idiopathic Nephrotic Syndrome (SDNS). Levamisole has been essentially considered
a safe drug with minimal toxicity. We conducted this study to re-examine the safety of Levamisole in children with nephrotic syndrome and
to describe the clinical profile of these children. Materials and Methods: Records of children with idiopathic nephrotic syndrome between
June 2014 and December 2016 were reviewed. We identified frequently relapsing or steroid dependent children between 1-18 years of age
who had received Levamisole for at least six months or in whom Levamisole was started but had to be withdrawn due to some adverse events
in the first 6 months. Results: 21 children were started on Levamisole in the study period. 13 (61.90%) were FRNS and remaining had a
steroid dependent course. Levamisole had to be withdrawn in one child at 1 month 13 days after initiation when the child developed severe
headache. Levamisole also had to be discontinued in a 9 years old girl at 13 months after initiation of therapy due to polyarticular arthralgia
involving both the small and large joints. Conclusions: The use of Levamisole warrants caution in children with Nephrotic Syndrome and its
efficacy needs to be balanced against its potential side effects.
Keywords: Levamisole, Nephrotic Syndrome, Steroid dependence
Introduction of Levamisole and to describe the clinical profile of these
children.
Levamisole, a synthetic imidazothiazole derivative, has been
used as a steroid‑sparing agent in children with Frequently
Relapsing Nephrotic Syndrome (FRNS) and Steroid Dependent Materials and Methods
Idiopathic Nephrotic Syndrome (SDNS). Studies have shown We conducted a retrospective study on all children with
that it reduces the frequency of relapses and cumulative nephrotic syndrome attending the Pediatric Nephrology Out
corticosteroid dose in children with FRNS and SDNS, thereby Patient Department (OPD) who had received Levamisole as
minimizing steroid toxicity in such children.[1‑3] a steroid‑sparing agent for at least 6 months. The study was
approved by the institutional ethics committee.
Levamisole has been essentially considered a safe drug
with minimal toxicity as compared to other steroid‑sparing We reviewed the records of children with Idiopathic Nephrotic
agents including alkylating agents and calcineurin inhibitors. Syndrome on follow‑up at Pediatric Nephrology OPD at our
The adverse effects of Levamisole are reported rarely and
have been found to be completely reversible after stopping Address for correspondence: Lt Col Suprita Kalra,
levamisole.[4] Department of Pediatrics, Command Hospital, AFMC, Pune,
Maharashtra, India.
We conducted this study to re‑examine the safety of E‑mail: kalrasuprita@gmail.com
levamisole in children with Nephrotic Syndrome in the light
of some of our patients facing adverse effects with the use
This is an open access article distributed under the terms of the Creative Commons
Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak,
Access this article online and build upon the work non‑commercially, as long as the author is credited and the new
creations are licensed under the identical terms.
Quick Response Code:
Website: For reprints contact: reprints@medknow.com
www.marinemedicalsociety.in
How to cite this article: Kalra S, Kanitkar M, Tiewsoh K. Use of levamisole
DOI: in children with nephrotic syndrome: A retrospective study to examine
10.4103/jmms.jmms_41_17 its adverse effects in children with nephrotic syndrome. J Mar Med Soc
2017;19:87-90.
© 2018 Journal of Marine Medical Society | Published by Wolters Kluwer - Medknow 87
[Downloaded free from http://www.marinemedicalsociety.in on Wednesday, March 21, 2018, IP: 110.136.238.52]
Kalra, et al.: Adverse effects of Levamisole in children with nephrotic syndrome
center between June 2014 and December 2016. We included
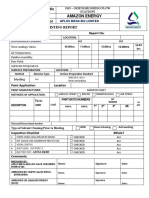
Table 1: Baseline characteristics of the children on
all children with FRNS or SDNS between 1 and 18 years of
levamisole therapy
age who had received Levamisole for at least 6 months or in
whom Levamisole was started but had to be withdrawn due Baseline characteristics n
to some adverse events in the first 6 months. The children Age in months* 42 months
who were noncompliant were excluded. The records of these Males, n (%) 11 (52.38)
children were then analyzed retrospectively to determine the FRNS, n (%) 10 (47.61)
adverse effects associated with the use of Levamisole. SDNS Age at onset of nephrotic syndrome in months* 23 (34-19)
was defined as two consecutive relapses while on alternate‑day Number of relapses in 6 months prior to levamisole 1.76 (0.55)
therapy**
steroids or within 14 days of their discontinuation. FRNS was
Duration of levamisole therapy in months* 18 (24-12.75)
defined as two or more relapses in 6 months or more than three
Age at initiation of levamisole therapy in months 42 (48-34)
relapses in any 12 months. Levamisole had been started in Number of relapses in 6 months after starting 0.67 (0.73)
children with FRNS or SDNS with features of steroid toxicity levamisole therapy**
as evidenced by short stature (defined by height <3 SD for age), Children on previous therapy with 3
cushingoid habitus, presence of cataract or raised intraocular cyclophosphamide (n)
pressure, or impaired glucose tolerance or if they had one or Children on previous therapy with mycophenolate 2
more relapses at a steroid dose of >0.5 mg/kg/day. All children mofetil
*Values in median (IQR), **Values in mean (SD). SD: Standard
received Levamisole at a dose of 2 mg/kg every alternate day.
deviation, IQR: Interquartile range, FRNS: Frequently relapsing nephrotic
All children were monitored every month for response to syndrome
therapy and examined for side effects. The number of relapses
in the previous 6 months before initiation of Levamisole was consecutive days with only partial relief with oral paracetamol.
recorded and compared to the number of relapses in the first The patient, a 5‑year‑old male, was in relapse at that time with
6 months on Levamisole as all children were followed up for urine protein of 4 + on dipstick examination. His blood pressure
a minimum of 6 months after starting levamisole. Complete was 90/66 mmHg (<90th centile for age and gender), there was
blood counts including total and differential blood cell counts, no papilledema or other signs of raised intracranial pressure on
liver function tests, serum urea, and creatinine were done every fundus examination. There was no focal neurological deficit
3 months. Steroids were tapered by 0.5 mg/kg every 2 weeks on examination. Magnetic resonance (MR) imaging brain and
if the child continued to be in remission. Two or more relapses MR venogram were done which were normal. The child had no
or when the dose of alternate‑day steroid was >0.5 mg/kg/day history of migraine and no history of similar headache in any
in 6 months after starting levamisole was taken as failure of relapse prior to starting Levamisole. The child was managed
Levamisole. The results were analyzed using Microsoft Excel. as per standard guidelines for relapse and later continued on
long‑term alternate‑day steroids. He had no recurrence of
Results headache on follow‑up in the subsequent 12 months.
Twenty‑one children were started on Levamisole in the study Levamisole also had to be discontinued in a 9‑year‑old girl at
period. Thirteen (61.90%) were FRNS and remaining had a 13 months after initiation therapy due to polyarticular arthralgia
SDNS. The baseline characteristics at the start of levamisole involving both the small and large joints. She had significant
therapy are shown in Table 1. The duration of levamisole pain in both the ankle joints, right knee joint, and small joints
therapy ranged from 1 month, 13 days to 26 months with of both the hands, interfering with her activities of daily living.
a median duration 18 months. Two children were excluded A history of morning stiffness was also present. There was
due to noncompliance, i.e., they stopped therapy after being no history of fever or symptoms of upper respiratory tract
on Levamisole for <6 months. These children had 37 relapses infection preceding the onset of joint pain. On examination,
in the 6 months prior to initiation of Levamisole therapy the child had no effusion or restriction of movement in any
(mean number of relapses: 1.76/child). Six children had one joint. Investigations showed raised C‑reactive protein and
relapse in the 6 months prior to initiation of Levamisole erythrocyte sedimentation rate. She was started on naproxen
therapy but were given Levamisole due to steroid threshold for the joint pains, but reported only minor relief. The arthralgia
being of >0.5 mg/kg/day. Fourteen relapses (mean number resolved 14 days after cessation of levamisole therapy and
of relapses: 0.67/child) were seen in the same children in the she had no recurrence in subsequent 12 months of follow‑up.
first 6 months of Levamisole therapy (P < 0.05). Three of the
21 children had two relapses in the 6 months’ period after The details of clinical features and investigations of the
they were started on Levamisole and were still on alternate children who faced adverse effects after starting levamisole
day steroids >0.5 mg/kg/day and were placed on alternate are mentioned in Table 2.
steroid‑sparing agents.
Levamisole had to be withdrawn in one child at 1 month, 13 days Discussion
after initiation when the child developed severe headache Various immunosuppressive agents have been used in
which was bifrontal, throbbing in nature, and lasted >4 h on 2 the management of children with FRNS and SDNS to
88 Journal of Marine Medical Society ¦ Volume 19 ¦ Issue 2 ¦ July-December 2017
[Downloaded free from http://www.marinemedicalsociety.in on Wednesday, March 21, 2018, IP: 110.136.238.52]
Kalra, et al.: Adverse effects of Levamisole in children with nephrotic syndrome
manifestation in the form of headache relatively early after
Table 2: Profile of children who faced adverse effects
the initiation of therapy (at 1 month, 13 days) while the
after starting levamisole
other child developed arthralgia at 13 months after she was
Patient 1 Patient 2 put on Levamisole therapy. The duration of therapy to onset
Age in completed years 5 9 of adverse effects has not been shown to be consistent and
Gender Male Female children may have the same any time during treatment with
Predominant symptom Headache Arthralgia Levamisole. Several cases of severe agranulocytosis have
necessitating withdrawal
been described in cocaine users inadvertently using cocaine
of levamisole
Investigations
contaminated with Levamisole. Cutaneous manifestations
Total leukocyte count in 11,600/cumm 12,000/cumm
consisting of large, painful hemorrhagic bullae and/or
cumm with neutrophils neutrophils 65% neutrophils 67% necrosis, most commonly involving the face, hyponatremia,
CRP Negative Positive seizures, and various other serious side effects, have been
(>6 mg/dL) described in this subset of patients. Gas chromatography
ESR 5 mm fall in 1st h 20 mm fall in 1st h or mass spectrometry has been used to test patients’ urine
Total bilirubin (mg/dL)/ 0.6/26/16 0.5/24/20 for the presence of Levamisole to confirm levamisole as the
AST/ALT (IU/mL)
causative agent.[6,11] This was, however, not required in our
Urea/creatinine (mg/dL) 24/0.4 17/0.3
children as exposure was definite, but to pinpoint Levamisole
Investigations specific to MRI brain and C3: Normal
presenting symptoms MR venography:
as the cause of adverse effect required exclusion of other
ANA by
Normal IF: Negative possible etiologies.
RA factor: The incidence of adverse events was not reported to be higher
Negative
with daily dosing of Levamisole as compared to the standard
CRP: C‑reactive protein, ESR: Erythrocyte sedimentation rate, AST:
Aspartate aminotransferase, ALT: Alanine aminotransferase, MRI: practice of giving it on alternate days.[3]
Magnetic resonance imaging, ANA: Antinuclear antibody, RF: Rheumatic
factor, IF: immuneflorescence
The strength of our study was that it focused on the adverse
events associated with Levamisole, The obvious limitation of
our study was that it was a retrospective analysis of data in a
minimize the toxicity of corticosteroids. Levamisole is a
single center.
well‑known anthelmintic agent with immunomodulatory
action. It also acts as an immune enhancer by increasing The adverse effects of Levamisole brought out in children with
macrophage chemotaxis and T‑cell function. It has been nephrotic syndrome in our study were found to be reversible
used in childhood idiopathic nephrotic syndrome since with drug withdrawal. However, their relatively high incidence
1980.[1] The effectiveness of levamisole in reducing the and the potential risk of serious side effects should be kept in
frequency of relapses in children with FRNS and SDNS mind while prescribing Levamisole which was traditionally
is well documented,[2,3] and it was seen in our study also. considered safe as compared to other immunosuppressive
It was withdrawn from use as an anthelmintic agent due agents in children with nephrotic syndrome.
to the risk of agranulocytosis and is not available in the This study also emphasizes the need for a large multicentric
US and Canada.[4,5] Apart from agranulocytosis, the other analysis of data related to the adverse events of all drugs used
prominent side effects include retiform purpura and seizures. as steroid‑sparing agents in children with nephrotic syndrome
The cutaneous lesions may represent a true vasculitis with to help weigh the benefits against the possible side effects.
positive staining for IgM, IgA, IgG, and C3, and vascular
staining for fibrin or a pseudovasculitis with negative
staining on immunofluorescence. The nervous system
Conclusions
manifestations have been attributed to accentuated nicotinic Although the number of relapses in children with FRNS and
acetylcholinergic release. Arthralgias and arthritis, especially SDNS is significantly reduced with the use of Levamisole, we
of the large joints, have also been commonly described.[6] In need to be cautious against its potential side effects.
children with nephrotic syndrome, studies have described Financial support and sponsorship
the incidence of side effects to vary from almost none[7,8] to Nil.
nearly 15%, but the adverse effects have been reported to
resolve completely after stopping therapy.[9] Rarely, serious Conflicts of interest
side effects such as disseminated autoimmune disease with There are no conflicts of interest.
high titers of IgM anticardiolipin and p‑Antineutrophil
cytoplasmic antibody antibodies have been described.[10] References
In our study also, we found the incidence of adverse effects 1. Tanphaichitr P, Tanphaichitr D, Sureeratanan J, Chatasingh S. Treatment
of nephrotic syndrome with levamisole. J Pediatr 1980;96:490‑3.
to be 9.52% (2/21), and as described in previous studies,
2. Bagga A, Sharma A, Srivastava RN. Levamisole therapy in
the adverse effects resolved completely on withdrawal corticosteroid‑dependent nephrotic syndrome. Pediatr Nephrol
of levamisole. In our series, one child had neurological 1997;11:415‑7.
Journal of Marine Medical Society ¦ Volume 19 ¦ Issue 2 ¦ July-December 2017 89
[Downloaded free from http://www.marinemedicalsociety.in on Wednesday, March 21, 2018, IP: 110.136.238.52]
Kalra, et al.: Adverse effects of Levamisole in children with nephrotic syndrome
3. Ekambaram S, Mahalingam V, Nageswaran P, Udani A, with levamisole in frequently relapsing, steroid‑dependent nephrotic
Geminiganesan S, Priyadarshini S, et al. Efficacy of levamisole in syndrome. Pediatr Nephrol 2006;21:201‑5.
children with frequently relapsing and steroid‑dependent nephrotic 8. Basu B, Babu BG, Mahapatra TK. Long‑term efficacy and safety of
syndrome. Indian Pediatr 2014;51:371‑3. common steroid‑sparing agents in idiopathic nephrotic children. Clin
4. Centers for Disease Control and Prevention (CDC). Agranulocytosis Exp Nephrol 2017;21:143‑51.
associated with cocaine use ‑ four states, March 2008‑November 2009. 9. Sümegi V, Haszon I, Iványi B, Bereczki C, Papp F, Túri S, et al.
MMWR Morb Mortal Wkly Rep 2009;58:1381‑5. Long‑term effects of levamisole treatment in childhood nephrotic
5. Knowles L, Buxton JA, Skuridina N, Achebe I, Legatt D, Fan S, et al. syndrome. Pediatr Nephrol 2004;19:1354‑60.
Levamisole tainted cocaine causing severe neutropenia in Alberta and 10. Barbano G, Ginevri F, Ghiggeri GM, Gusmano R. Disseminated
British Columbia. Harm Reduct J 2009;6:30. autoimmune disease during levamisole treatment of nephrotic syndrome.
6. Lee KC, Culpepper K, Kessler M. Levamisole‑induced thrombosis: Pediatr Nephrol 1999;13:602‑3.
Literature review and pertinent laboratory findings. J Am Acad Dermatol 11. McGrath MM, Isakova T, Rennke HG, Mottola AM, Laliberte KA,
2011;65:e128‑9. Niles JL, et al. Contaminated cocaine and antineutrophil cytoplasmic
7. Al‑Saran K, Mirza K, Al‑Ghanam G, Abdelkarim M. Experience antibody‑associated disease. Clin J Am Soc Nephrol 2011;6:2799‑805.
90 Journal of Marine Medical Society ¦ Volume 19 ¦ Issue 2 ¦ July-December 2017
You might also like
- Module 2 Lesson 3 MISSIONARY RESPONSEDocument1 pageModule 2 Lesson 3 MISSIONARY RESPONSEHarriz Diether DomingoNo ratings yet
- Kirschen2000 - The Royal London Space Planning - Part 1Document8 pagesKirschen2000 - The Royal London Space Planning - Part 1drgeorgejose7818100% (2)
- 1.irosun OgbeDocument10 pages1.irosun OgbeOmo Awo Ifasina Aworeni91% (11)
- Effective Classroom ManagementDocument24 pagesEffective Classroom ManagementAmbrosious100% (1)
- Second-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceDocument10 pagesSecond-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceSitaNo ratings yet
- Levamisole Therapy in Children With Frequently Relapsing and Steroid-Dependent Nephrotic Syndrome - A Single-Center ExperienceDocument5 pagesLevamisole Therapy in Children With Frequently Relapsing and Steroid-Dependent Nephrotic Syndrome - A Single-Center ExperienceGading AuroraNo ratings yet
- Efficacy of Higher-Dose Levamisole in Maintaining Remission in Steroid-Dependant Nephrotic SyndromeDocument6 pagesEfficacy of Higher-Dose Levamisole in Maintaining Remission in Steroid-Dependant Nephrotic Syndromechandra maslikhaNo ratings yet
- Effectiveness and Adverse Drug Reactions of Levetiracetam and Midazolam in Refractory Neonatal Seizure: A Cross Sectional Comparative StudyDocument6 pagesEffectiveness and Adverse Drug Reactions of Levetiracetam and Midazolam in Refractory Neonatal Seizure: A Cross Sectional Comparative StudySultan Rahmat SeptianNo ratings yet
- Nuevos Antiepilépticos 2013Document8 pagesNuevos Antiepilépticos 2013Andres RodriguezNo ratings yet
- AhmadDocument6 pagesAhmadtengku maulanaNo ratings yet
- JurnalDocument8 pagesJurnalIndahNo ratings yet
- COPOUSEUPDocument8 pagesCOPOUSEUPamazedNo ratings yet
- Safety and Effectiveness of Lurasidone in Adolescents With Schizophrenia: Results of A 2-Year, Open-Label Extension StudyDocument11 pagesSafety and Effectiveness of Lurasidone in Adolescents With Schizophrenia: Results of A 2-Year, Open-Label Extension StudyNaiana PaulaNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916Sriram NagarajanNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916srirampharmNo ratings yet
- Childhood Nephrotic Syndrome: Steroid Sensitive, Steroid Resistant and BeyondDocument7 pagesChildhood Nephrotic Syndrome: Steroid Sensitive, Steroid Resistant and BeyondDorin Cristian AntalNo ratings yet
- Jurnal Baru 2Document6 pagesJurnal Baru 2FIRDA RIDHAYANINo ratings yet
- Comparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile Seizures PDFDocument5 pagesComparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile Seizures PDFCharina Geofhany DeboraNo ratings yet
- WJM 7 25Document9 pagesWJM 7 25Ainna SavitaNo ratings yet
- A Single-Centre Retrospective Study of The Safety and Ef Ficacy of Mycophenolate Mofetil in Children and Adolescents With Nephrotic SyndromeDocument6 pagesA Single-Centre Retrospective Study of The Safety and Ef Ficacy of Mycophenolate Mofetil in Children and Adolescents With Nephrotic SyndromeBakul TapeNo ratings yet
- Efficacy of Rituximab Therapy in Children With Nephrotic Syndrome: A 10-Year Experience From An Iranian Pediatric HospitalDocument9 pagesEfficacy of Rituximab Therapy in Children With Nephrotic Syndrome: A 10-Year Experience From An Iranian Pediatric HospitalAris BayuNo ratings yet
- The Effects of Dexamethasone On Sleep in Young Children With Acute Lymphoblastic LeukemiaDocument7 pagesThe Effects of Dexamethasone On Sleep in Young Children With Acute Lymphoblastic LeukemiaAndrye FernandesNo ratings yet
- Desvenlafaxine Versus Placebo in The TreatmentDocument12 pagesDesvenlafaxine Versus Placebo in The TreatmentNatalia OlmosNo ratings yet
- Incidence and Predictors of Adverse Drug Events Among People Receiving Drug Resistant Tuberculosis Treatment in Uganda 8-Year Retrospective Cohort STDocument12 pagesIncidence and Predictors of Adverse Drug Events Among People Receiving Drug Resistant Tuberculosis Treatment in Uganda 8-Year Retrospective Cohort STEghar EverydayishellNo ratings yet
- MagnascoDocument8 pagesMagnascoMeliana SulistioNo ratings yet
- Final NS Guidelines August 26 2019-1Document17 pagesFinal NS Guidelines August 26 2019-1Nido MalghaniNo ratings yet
- Adverse Drug Reaction Profile of Oseltamivir in Children: Research PaperDocument4 pagesAdverse Drug Reaction Profile of Oseltamivir in Children: Research PaperRega PermanaNo ratings yet
- 15-Polyphenol Nano Cancer ReviewDocument14 pages15-Polyphenol Nano Cancer Reviewmohamed lamrana jallohNo ratings yet
- 10126-Article Text-75914-1-10-20181208Document5 pages10126-Article Text-75914-1-10-20181208Odessa EnriquezNo ratings yet
- Lacosamide 1Document6 pagesLacosamide 1ezio93No ratings yet
- Seizure: U Nsal Yılmaz, Tuba Sevim Yılmaz, Gu Ls en Dizdarer, Gu LC in Akıncı, Orkide Gu Zel, Hasan Tekgu LDocument8 pagesSeizure: U Nsal Yılmaz, Tuba Sevim Yılmaz, Gu Ls en Dizdarer, Gu LC in Akıncı, Orkide Gu Zel, Hasan Tekgu LDHIVYANo ratings yet
- Ixazomib, Lenalidomide, and Dexamethasone PDFDocument14 pagesIxazomib, Lenalidomide, and Dexamethasone PDFJLNo ratings yet
- Therapeutic Use of Medicinal Cannabis in Dif Ficult To Manage EpilepsyDocument3 pagesTherapeutic Use of Medicinal Cannabis in Dif Ficult To Manage EpilepsyEnrique Molina LeonNo ratings yet
- Utilization of The Naranjo Scale To Evaluate Adverse Drug Reactions at A Free-Standing Children's HospitalDocument10 pagesUtilization of The Naranjo Scale To Evaluate Adverse Drug Reactions at A Free-Standing Children's HospitalSheerazNo ratings yet
- Risperidone Use in Autism SpectrumDocument5 pagesRisperidone Use in Autism SpectrumAdina CipariuNo ratings yet
- Uongffd TtyddfyDocument7 pagesUongffd TtyddfyVsbshNo ratings yet
- C PDFDocument11 pagesC PDFNadiea FetrisiaNo ratings yet
- Onasemnogene Abeparvovec For SMADocument2 pagesOnasemnogene Abeparvovec For SMAsurbhib268No ratings yet
- Biomedicines 11 03039Document14 pagesBiomedicines 11 03039Hans Kristian LorenzoNo ratings yet
- Prolonged Sedation And/or Analgesia and 5-Year Neurodevelopment Outcome in Very Preterm InfantsDocument6 pagesProlonged Sedation And/or Analgesia and 5-Year Neurodevelopment Outcome in Very Preterm InfantsmustafasacarNo ratings yet
- HamdDocument12 pagesHamdAldiola PerdanaNo ratings yet
- Use of A LowDocument8 pagesUse of A Lowirma suwandi sadikinNo ratings yet
- Dress Syndrome A Review and UpdateDocument5 pagesDress Syndrome A Review and UpdateCarlos Alberto Torres LópezNo ratings yet
- 1 MultimethodassessmentDocument8 pages1 MultimethodassessmentRoberto Alexis Molina CampuzanoNo ratings yet
- Comparison Predni and Dexa in Treatment of CroupDocument6 pagesComparison Predni and Dexa in Treatment of CroupBangkit Brillian FauziNo ratings yet
- Multiple SclerosisDocument15 pagesMultiple SclerosisThong MinyewNo ratings yet
- Treatment Outcomes of Oral Propranolol in The TreaDocument7 pagesTreatment Outcomes of Oral Propranolol in The TreabokobokobokanNo ratings yet
- Effect of Play Based... 2017Document5 pagesEffect of Play Based... 2017gemita aldeaNo ratings yet
- Dress Syndrome: A Review and Update: March 2016Document5 pagesDress Syndrome: A Review and Update: March 2016Carlos LuqueNo ratings yet
- Jurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresDocument15 pagesJurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresAnida HasnaNo ratings yet
- Nebulised Steroid in The Treatment of Croup: A Systematic Review of Randomised Controlled TrialsDocument7 pagesNebulised Steroid in The Treatment of Croup: A Systematic Review of Randomised Controlled TrialsSatriyo BagasNo ratings yet
- A Randomized Controlled Trial of Intranasal-Midazolam Versus Intravenous-Diazepam For Acute Childhood SeizuresDocument5 pagesA Randomized Controlled Trial of Intranasal-Midazolam Versus Intravenous-Diazepam For Acute Childhood SeizuresAdriel Chandra AngNo ratings yet
- 8 Sivakumar Et AlDocument7 pages8 Sivakumar Et Alkhalid alharbiNo ratings yet
- Nej Mo A 1109997Document10 pagesNej Mo A 1109997juan hurtadoNo ratings yet
- Comparative Study of The Efficacy and Safety of Topical Antifungal Agents Clotrimazole Versus Sertaconazole in The Treatment of Tinea Corporis/crurisDocument5 pagesComparative Study of The Efficacy and Safety of Topical Antifungal Agents Clotrimazole Versus Sertaconazole in The Treatment of Tinea Corporis/crurisRasyid Ali NatioNo ratings yet
- Kortikosteroid Nephrotic SyndromeDocument7 pagesKortikosteroid Nephrotic SyndromeDevi Albaiti JannatiNo ratings yet
- Pediatric Neurology: Hye-Ryun Yeh MD, Min-Jee Kim MD, Tae-Sung Ko MD, PHD, Mi-Sun Yum MD, PHD, Su-Jeong You MD, PHDDocument6 pagesPediatric Neurology: Hye-Ryun Yeh MD, Min-Jee Kim MD, Tae-Sung Ko MD, PHD, Mi-Sun Yum MD, PHD, Su-Jeong You MD, PHDAdrian KhomanNo ratings yet
- Rituximab Tullus Kjeil 2021Document9 pagesRituximab Tullus Kjeil 2021Carmen MunteanNo ratings yet
- Ref 11Document5 pagesRef 11Tiago BaraNo ratings yet
- Kulit3 PDFDocument5 pagesKulit3 PDFAhmad LabibNo ratings yet
- OtorhinolaryngologyDocument7 pagesOtorhinolaryngologyDeniNo ratings yet
- BMC NephrologyDocument10 pagesBMC Nephrologyselandia nisrinaNo ratings yet
- The Essential Guide to Prescription Drugs, Update on RemdesivirFrom EverandThe Essential Guide to Prescription Drugs, Update on RemdesivirNo ratings yet
- Buku Saku IdaiDocument1 pageBuku Saku IdaiJohan GautamaNo ratings yet
- Jurnal HemaDocument38 pagesJurnal HemaJohan GautamaNo ratings yet
- Pic Asi SeduniaDocument3 pagesPic Asi SeduniaJohan GautamaNo ratings yet
- Sepsis in Child With Burn Trauma: Death Case ReportDocument22 pagesSepsis in Child With Burn Trauma: Death Case ReportJohan GautamaNo ratings yet
- Cerebral Palsy NMPRA Conference SubmissionDocument61 pagesCerebral Palsy NMPRA Conference SubmissionJohan GautamaNo ratings yet
- Psychology and The Challenges of Life 13th Edition Nevid Solutions ManualDocument73 pagesPsychology and The Challenges of Life 13th Edition Nevid Solutions Manualbrianwoodsnjyoxepibt100% (14)
- Een Liefdesbrief Aan Amsterdam (By Ryan Bartek)Document5 pagesEen Liefdesbrief Aan Amsterdam (By Ryan Bartek)Ryan Bartek100% (1)
- Notified Vide SRO No. 575 Dated 22 May 2019Document3 pagesNotified Vide SRO No. 575 Dated 22 May 2019Hussain RahibNo ratings yet
- EverFlo Broch PDFDocument6 pagesEverFlo Broch PDFAdnan HuskicNo ratings yet
- Atlan A300 A300xl Pi 9107089 en MasterDocument12 pagesAtlan A300 A300xl Pi 9107089 en MasterHanh NguyenNo ratings yet
- KRAUSE 2016 Standard Catalog O1901-2000 20th Century 43rd Ed 381Document1 pageKRAUSE 2016 Standard Catalog O1901-2000 20th Century 43rd Ed 381Millona usdNo ratings yet
- KGianan-Stem12-Physics2 (Chapters 1-3)Document9 pagesKGianan-Stem12-Physics2 (Chapters 1-3)Kyle GiananNo ratings yet
- Gaius SMW Incest Sister BrotherDocument5 pagesGaius SMW Incest Sister BrotherShyam BhatNo ratings yet
- Cat Dissection ProjectDocument12 pagesCat Dissection Projectapi-309363754No ratings yet
- MSP TT MSP Al Leaflet en w4156 1Document8 pagesMSP TT MSP Al Leaflet en w4156 1serban_elNo ratings yet
- Aplus Coating Report FormatDocument1 pageAplus Coating Report FormatNnamdi AmadiNo ratings yet
- Quality Management Principles For Excellence: by - Sacchidanand Gogawale, Zen International SystemsDocument5 pagesQuality Management Principles For Excellence: by - Sacchidanand Gogawale, Zen International SystemsSanjeevani GogawaleNo ratings yet
- GMCO FOR INDUSTRIAL SERVICES - Welding Procedure SpecificationsDocument2 pagesGMCO FOR INDUSTRIAL SERVICES - Welding Procedure SpecificationsMohamedNo ratings yet
- CV Sayeed TeachingDocument8 pagesCV Sayeed TeachingGopal ReddyNo ratings yet
- Psychological TheoriesDocument19 pagesPsychological TheoriesYapieeNo ratings yet
- Asl Curriculum Writing 2021-2022Document20 pagesAsl Curriculum Writing 2021-2022api-589645770No ratings yet
- MFG Fiberglass Column Forms Product SheetDocument3 pagesMFG Fiberglass Column Forms Product SheetAboalmaail AlaminNo ratings yet
- Q.1 Write Short Answers of The Following Questions: Ghazali Guess Chemistry 1 10thDocument9 pagesQ.1 Write Short Answers of The Following Questions: Ghazali Guess Chemistry 1 10thAwais AliNo ratings yet
- Out 10Document12 pagesOut 10restu anindityaNo ratings yet
- A Mnemonic For The Treatment of HyperkalemiaDocument3 pagesA Mnemonic For The Treatment of Hyperkalemiakhangsiean89No ratings yet
- Zamil Product Brochure PDFDocument30 pagesZamil Product Brochure PDFZameer KhanNo ratings yet
- EJMCM - Volume 7 - Issue 11 - Pages 9184-9190Document7 pagesEJMCM - Volume 7 - Issue 11 - Pages 9184-9190Akshay BeradNo ratings yet
- Technical Data BCC 1250P-50 BCC 1400S-50: 50 Hz Cos Φ = 0.8 3-PhaseDocument3 pagesTechnical Data BCC 1250P-50 BCC 1400S-50: 50 Hz Cos Φ = 0.8 3-PhaseHectrateNo ratings yet
- Unsafe Act Danger of Horseplay at WorkDocument1 pageUnsafe Act Danger of Horseplay at WorkSn AhsanNo ratings yet
- 08 Proceduri de UrgentaDocument9 pages08 Proceduri de UrgentaSorescu Radu VasileNo ratings yet
- PU LPH 80540 80553 Esite GBDocument7 pagesPU LPH 80540 80553 Esite GBAl-Alamiya TradeNo ratings yet