Professional Documents
Culture Documents
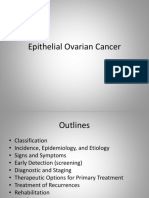
PDFsam ObGyn
PDFsam ObGyn
Uploaded by
Alessandro ZadraCopyright:
Available Formats
You might also like
- Reign Over Me ReflectionDocument2 pagesReign Over Me ReflectionBootstrapGamingNo ratings yet
- English Task Gynecology System: Case ReportDocument4 pagesEnglish Task Gynecology System: Case ReportCecepNo ratings yet
- Journal Reading Management of A Pelvic MassDocument40 pagesJournal Reading Management of A Pelvic MassCecilia SalimNo ratings yet
- O BGYNDocument84 pagesO BGYNselvie87100% (2)
- Current Diagnosis and Management of Ovarian Cysts: Review ArticlesDocument4 pagesCurrent Diagnosis and Management of Ovarian Cysts: Review ArticlesFelNo ratings yet
- Endometrial BiopsyDocument9 pagesEndometrial BiopsyAnna BartolomeNo ratings yet
- PancreatoblastomaDocument16 pagesPancreatoblastomaDr Farman AliNo ratings yet
- Malignant Ovarian TumourDocument46 pagesMalignant Ovarian Tumourahmed shorshNo ratings yet
- Ovarian Cancer SGTDocument25 pagesOvarian Cancer SGTAndre PutraNo ratings yet
- Abdominal (Retroperitoneal) Cystic Lympangioma.: KeywordsDocument3 pagesAbdominal (Retroperitoneal) Cystic Lympangioma.: KeywordsIordachescu AmaliaNo ratings yet
- Pre Mal Dis of CervixDocument44 pagesPre Mal Dis of CervixnoreenfatimamaanNo ratings yet
- Belle Cervical DiseaseDocument7 pagesBelle Cervical DiseaseRashed ShatnawiNo ratings yet
- Auto Article ProcessDocument6 pagesAuto Article ProcessJamshaid AhmedNo ratings yet
- Endometriosis and AdenomyosisDocument36 pagesEndometriosis and Adenomyosishacker ammerNo ratings yet
- Ca OvarioDocument13 pagesCa OvarioDaniel MálagaNo ratings yet
- 17-09-2019 Lower GI FINALDocument32 pages17-09-2019 Lower GI FINALNaima HabibNo ratings yet
- Mullerian Agenesis: An Unusual Presentation As Hematometra and Bilateral HematosalpinxDocument2 pagesMullerian Agenesis: An Unusual Presentation As Hematometra and Bilateral Hematosalpinxwanwan_adongNo ratings yet
- Frantz TumorDocument5 pagesFrantz TumorAndu1991No ratings yet
- B. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)Document14 pagesB. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)lizzy596No ratings yet
- MCQ Jeddah - Doc (FINAL) 2Document9 pagesMCQ Jeddah - Doc (FINAL) 2Indrajit Barua100% (1)
- Ovarian Masses: Surgery or Surveillance?Document9 pagesOvarian Masses: Surgery or Surveillance?MutianbllNo ratings yet
- ChanDocument2 pagesChankenny stefanusNo ratings yet
- A Case of Ovarian Fibroma Masquerading As A Uterine FibroidDocument5 pagesA Case of Ovarian Fibroma Masquerading As A Uterine FibroidAnonymous UHnQSkxLBDNo ratings yet
- Ovarian Cancer in PregnancyDocument36 pagesOvarian Cancer in PregnancyNicole BalagtasNo ratings yet
- Pico 1Document12 pagesPico 1annissaerceNo ratings yet
- Jurding BedahDocument18 pagesJurding BedahSharon Natalia RuntulaloNo ratings yet
- Adnexal Masses in Pediatric and Adolescent Females: A Review of The LiteratureDocument8 pagesAdnexal Masses in Pediatric and Adolescent Females: A Review of The LiteratureAlejandro GuzmanNo ratings yet
- Recurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Document2 pagesRecurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Motivational SpeechNo ratings yet
- gtg62 021211 OvarianmassesDocument14 pagesgtg62 021211 OvarianmassesMaryamNo ratings yet
- Cervical CancerDocument38 pagesCervical Cancerreema.saleh123No ratings yet
- Clinicopathological Profile of Ovarian Tumors in The Age Group 10-20 YearsDocument4 pagesClinicopathological Profile of Ovarian Tumors in The Age Group 10-20 YearsLauren RenNo ratings yet
- CRC and Other Colorectal Disease - PPT For Senior Medical StudentsDocument37 pagesCRC and Other Colorectal Disease - PPT For Senior Medical StudentsGiovanni HenryNo ratings yet
- 20.MBBS Pancreatic CancerDocument52 pages20.MBBS Pancreatic Cancermrajah95No ratings yet
- Surgical OncologyDocument10 pagesSurgical Oncologysofea zamriNo ratings yet
- Management of AISDocument10 pagesManagement of AISMaría Reynel TarazonaNo ratings yet
- Breast CancerDocument4 pagesBreast CancerMaikka IlaganNo ratings yet
- OvaryDocument4 pagesOvaryCarolina MartinezNo ratings yet
- Uterus NeoDocument11 pagesUterus NeoHester Marie SimpiaNo ratings yet
- Diagnostic Tools in ObgynDocument27 pagesDiagnostic Tools in ObgynHenok Y KebedeNo ratings yet
- A Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathDocument5 pagesA Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathLauren RenNo ratings yet
- (Gyne) Neoplastic Diseases of The Uterus (Dra. Ahyong-Reyes) ?Document6 pages(Gyne) Neoplastic Diseases of The Uterus (Dra. Ahyong-Reyes) ?RONALDO CUANo ratings yet
- (GYNE) Neoplastic Diseases of The Ovary-Dr. Dueñas (Parbs)Document10 pages(GYNE) Neoplastic Diseases of The Ovary-Dr. Dueñas (Parbs)adrian kristopher dela cruzNo ratings yet
- SESAP Abd HBPDocument90 pagesSESAP Abd HBPLamisNo ratings yet
- Impey Obs and Gynae Revision Notes PDFDocument9 pagesImpey Obs and Gynae Revision Notes PDFRoiseNo ratings yet
- Operative Treatment of Gynaecologic Diseases in Puberty: Seven Years of ExperienceDocument2 pagesOperative Treatment of Gynaecologic Diseases in Puberty: Seven Years of Experiencemajacokovikj.urologijaNo ratings yet
- Tambimuttu 2015Document2 pagesTambimuttu 2015cristian vivasNo ratings yet
- K GanDocument22 pagesK GancdatNo ratings yet
- 31422-Article Text-92425-1-10-20200923Document4 pages31422-Article Text-92425-1-10-20200923irvan bNo ratings yet
- FibroadenomaDocument5 pagesFibroadenomaAmalia FadhilaNo ratings yet
- Surgicopath July 2017Document105 pagesSurgicopath July 2017Rendy Adhitya PratamaNo ratings yet
- Laparoscopic Management of Giant Ovarian Cyst A Case ReportDocument3 pagesLaparoscopic Management of Giant Ovarian Cyst A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cancers of The Female Genital TractDocument31 pagesCancers of The Female Genital TractTresor MbuyiNo ratings yet
- Ovarian and Prostate CancerDocument51 pagesOvarian and Prostate CancerMa. Angelica Alyssa RachoNo ratings yet
- Clinical Case 54-Ovarian NeoplasmsDocument4 pagesClinical Case 54-Ovarian Neoplasmsselina kalenderNo ratings yet
- Cervical Dysgenesis With Transverse Vaginal Septum With Imperforate Hymen in An 11 Year Old Girl Presenting With Acute AbdomenDocument4 pagesCervical Dysgenesis With Transverse Vaginal Septum With Imperforate Hymen in An 11 Year Old Girl Presenting With Acute Abdomenshe-docNo ratings yet
- En Bloc Robot-Assisted Laparoscopic Partial Cystectomy, Urachal Resection, and Pelvic Lymphadenectomy For Urachal AdenocarcinomaDocument4 pagesEn Bloc Robot-Assisted Laparoscopic Partial Cystectomy, Urachal Resection, and Pelvic Lymphadenectomy For Urachal Adenocarcinomadr.tonichenNo ratings yet
- Potdar 2020Document8 pagesPotdar 2020Christian Leonardo Molina HinojosaNo ratings yet
- A Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesDocument2 pagesA Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesAlfa FebriandaNo ratings yet
- Management of Benign Breast Conditions: Part 2 - Breast Lumps and LesionsDocument3 pagesManagement of Benign Breast Conditions: Part 2 - Breast Lumps and Lesionspeter_mrNo ratings yet
- Periampullary CarcinomaDocument35 pagesPeriampullary Carcinomaminnalesri100% (2)
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentFrom EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentNo ratings yet
- Corn Agli A 2010Document2 pagesCorn Agli A 2010Alessandro ZadraNo ratings yet
- Managing Common Infections Summary TablesDocument8 pagesManaging Common Infections Summary TablesAlessandro ZadraNo ratings yet
- Practical Management of Anticoagulation in Patients With Atrial FibrillationDocument21 pagesPractical Management of Anticoagulation in Patients With Atrial FibrillationAlessandro ZadraNo ratings yet
- ArrhythmiasDocument1 pageArrhythmiasAlessandro ZadraNo ratings yet
- Treatment of Distal Iliotibial Band Syndrome in A Long Distance Runner With Gait Re Training Emphasizing Step Rate ManipulationDocument10 pagesTreatment of Distal Iliotibial Band Syndrome in A Long Distance Runner With Gait Re Training Emphasizing Step Rate ManipulationAlessandro ZadraNo ratings yet
- Who Recommends Assistance For People With Hiv To Notify Their PartnersDocument2 pagesWho Recommends Assistance For People With Hiv To Notify Their PartnerstashoneNo ratings yet
- Cholesterol Explained PDFDocument3 pagesCholesterol Explained PDFkapczukNo ratings yet
- The Interpersonal Approach and Group Theory Summary: ObjectivesDocument16 pagesThe Interpersonal Approach and Group Theory Summary: ObjectivesCami Matei CamiNo ratings yet
- Pricelist Alzetta AestheticDocument2 pagesPricelist Alzetta AestheticGisella Destiny Luh PrasastiNo ratings yet
- Rational Emotive Behaviour TherapyDocument30 pagesRational Emotive Behaviour TherapyJacqueline GonsalvesNo ratings yet
- Dimeglio Score Untuk ClubfootDocument4 pagesDimeglio Score Untuk ClubfootInezz LeonitaaNo ratings yet
- Nursing Care Plan: Assessment DataDocument2 pagesNursing Care Plan: Assessment DataDana CozorocNo ratings yet
- Nomophobia: No Mobile Phone Phobia: ArticleDocument5 pagesNomophobia: No Mobile Phone Phobia: ArticleAman ShabaNo ratings yet
- Effects of A Solution-Focused Mutual Aid Group For Hispanic Children of Incarcerated ParentsDocument12 pagesEffects of A Solution-Focused Mutual Aid Group For Hispanic Children of Incarcerated Parentssolutions4familyNo ratings yet
- Mental RetardationDocument19 pagesMental RetardationAsmarandi100% (1)
- Anxiety - Symptoms, Types, Causes, Prevention, and TreatmentDocument12 pagesAnxiety - Symptoms, Types, Causes, Prevention, and Treatmentzandro padillaNo ratings yet
- Early Mobilization in The Pediatric Intensive Care Unit A Systematic ReviewDocument6 pagesEarly Mobilization in The Pediatric Intensive Care Unit A Systematic ReviewJuly ZaballaNo ratings yet
- Letter To FreudDocument20 pagesLetter To FreudDaniel Lee Eisenberg JacobsNo ratings yet
- Biodose Models:Nsd, Cre, TDF, LQ& Their Limitations: Moderator: Mr. Ranjit Singh Presented By: Navneet KaurDocument54 pagesBiodose Models:Nsd, Cre, TDF, LQ& Their Limitations: Moderator: Mr. Ranjit Singh Presented By: Navneet KaurSAlonii ChawlaNo ratings yet
- End of Life EdDocument6 pagesEnd of Life EdZulkifli PomalangoNo ratings yet
- Antibiotic Resistant BacteriaDocument6 pagesAntibiotic Resistant BacteriaAmandaNo ratings yet
- Accelerated OrthodonticsDocument13 pagesAccelerated OrthodonticsJustin Kimberlake100% (1)
- A Comparison of Human Dental Pulp Response To CalcDocument5 pagesA Comparison of Human Dental Pulp Response To CalcrespikNo ratings yet
- Cancer of The BreastDocument19 pagesCancer of The BreastJoanna TaylanNo ratings yet
- Lyme, CF ProtocolDocument36 pagesLyme, CF ProtocolTheresa Dale100% (1)
- Clinical Experiences of Using A Cellulose Dressing On Burns and Donor Site WoundsDocument4 pagesClinical Experiences of Using A Cellulose Dressing On Burns and Donor Site WoundsabdmaliknasNo ratings yet
- Papini SIBIU 2018Document53 pagesPapini SIBIU 2018Alina Ioana PaduraruNo ratings yet
- Fracture Nursing Care PlansDocument14 pagesFracture Nursing Care PlansSheryl Ann Barit PedinesNo ratings yet
- Renal CalculiDocument16 pagesRenal CalculiMeenu NegiNo ratings yet
- Lecture - 2 - Psychopharmacology - History, Neurotransmitters Etc - May 2013Document24 pagesLecture - 2 - Psychopharmacology - History, Neurotransmitters Etc - May 2013Robert EdwardsNo ratings yet
- What Are Healing GardensDocument9 pagesWhat Are Healing GardensMuhammad Tahir PervaizNo ratings yet
- Solution-Focused Counseling: An Integrative Approach: by Jeffrey T. Guterman, PH.DDocument60 pagesSolution-Focused Counseling: An Integrative Approach: by Jeffrey T. Guterman, PH.DAriep IlhamNo ratings yet
- Guideline On Induction of Ovulation 2011Document20 pagesGuideline On Induction of Ovulation 2011Atik ShaikhNo ratings yet
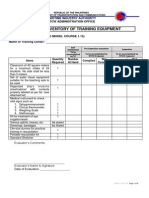
- Form 2B: Inventory of Training Equipment: Maritime Industry Authority STCW Administration OfficeDocument9 pagesForm 2B: Inventory of Training Equipment: Maritime Industry Authority STCW Administration OfficeDemp AlmiranezNo ratings yet
PDFsam ObGyn
PDFsam ObGyn
Uploaded by
Alessandro ZadraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PDFsam ObGyn
PDFsam ObGyn
Uploaded by
Alessandro ZadraCopyright:
Available Formats
USMLE Step 2 l Gynecology
PREPUBERTAL PELVIC MASS
An 8-year-old girl is evaluated in the emergency department for sudden onset
of severe lower abdominal pain. A general surgery consult was obtained, and
appendicitis is ruled out. Pelvic ultrasound reveals a 7-cm solid and irregular right
adnexal mass. Pelvic examination is consistent with a 7-cm right adnexal mass, and
there is lower abdominal tenderness but no rebound present.
Etiology. An adnexal mass in the prepubertal age group is abnormal. During the prepubertal
and the postmenopausal years, functional ovarian cysts are not possible because ovarian fol-
licles are not functioning. Therefore any ovarian enlargement is suspicious for neoplasm.
Differential Diagnosis. If sonography shows a complex adnexal mass in a girl or teenager, the
possibility of germ cell tumors of the ovary has to be considered. The following serum tumor
markers should be obtained: lactate dehydrogenase (LDH) for dysgerminoma, b-hCG for cho-
riocarcinoma, and a-fetoprotein for endodermal sinus tumor.
Presentation. Sudden onset of acute abdominal pain is a typical presentation of germ cell
tumors of the ovary. These tumors characteristically grow rapidly and give early symptomatol-
ogy as opposed to the epithelial cancers of the ovary that are diagnosed in advanced stages. Germ
cell tumors of the ovary are most common in young women and present in early stage disease.
Diagnosis. Surgical exploration. In a prepubertal patient who is symptomatic and has ultra-
sound evidence of an adnexal mass, a surgical evaluation is recommended.
• Simple mass. If the ultrasound shows the consistency of the mass to be simple (no
septations or solid components), this mass can be evaluated through a laparoscopic
approach.
• Complex mass. If the mass has septations or solid components, a laparoscopy or lapa-
rotomy should be performed, depending on the experience of the surgeon.
Table II-5-1. Prepubertal Pelvic Mass
Surgical diagnosis Simple cyst Laparoscopy
Complex mass Laparotomy
Management Benign Cystectomy
Annual followup
Malignant Unilateral S&O
Staging, chemotherapy
Prognosis 95% survival with chemotherapy
Definition of abbreviations: S&O, Salpingo-oophorectomy.
Management
• Benign histology. A cystectomy should be performed instead of a salpingo-oophorectomy.
Because of the patient’s age the surgical goal should be toward conservation of both
ovaries. If the frozen section pathology analysis is benign, no further surgery is needed.
Follow-up is on an annual basis.
190
S2 OB-GYN.indb 190 7/8/13 6:36 PM
Chapter 5 l Disorders of the Ovaries and Oviducts
• Germ cell tumor. A unilateral salpingo-oophorectomy and surgical staging (peritoneal
and diaphragmatic biopsies, peritoneal cytology, pelvic and para-aortic lymphadenec-
tomy, and omentectomy) should be done. All patients with germ cell tumors require
postoperative chemotherapy. The most active regimen used is vinblastine, bleomy-
cin, and cisplatin. Follow-up after conservative surgery is every 3 months with pelvic
examination and tumor marker measurements.
Prognosis. The current survival is >95% in patients with germ cell tumors managed with con-
servative management and chemotherapy. Before the chemotherapy age the majority of these
patients succumbed to their disease.
PREMENOPAUSAL PELVIC MASS
Complex Mass GYN Triad
Dysgerminoma
A 28-year-old woman is in the emergency department complaining of lower
abdominal discomfort the last 5 days. She has no history of steroid contraceptive • Solid pelvic mass in
reproductive years
use. A year ago, her pelvic exam and Pap smear were negative. Pelvic exam today
shows a 7-cm, mobile, painless right adnexal mass. An endovaginal sonogram in • b-hCG (–)
the emergency department confirms a 7-cm, mobile, irregular complex mass with • ↑ LDH level
prominent calcifications.
Definition. The most common complex adnexal mass in young women is a dermoid cyst
or benign cystic teratoma (discussed below). Other diagnoses include endometrioma, tubo-
ovarian abscess, and ovarian cancer.
Differential Diagnosis
• Pregnancy
• Functional cysts
Diagnosis.
• Qualitative b-human chorionic gonadotropin (b-hCG) test to rule out pregnancy.
• The appearance of a complex mass on ultrasound will rule out a functional cyst.
Management. Patients in the reproductive age group with a complex adnexal mass should be
treated surgically. The surgery can be done by a laparoscopy or a laparotomy according to the
experience of the surgeon.
• Cystectomy. At the time of surgery an ovarian cystectomy should be attempted to
preserve ovarian function in the reproductive age. Careful evaluation of the opposite
adnexa should be performed, as dermoid cysts can occur bilaterally in 10–15% of cases.
• Oophorectomy. If an ovarian cystectomy cannot be done because of the size of the
dermoid cyst, then an oophorectomy is performed, but conservative management
should always be attempted before an oophorectomy is done.
191
S2 OB-GYN.indb 191 7/8/13 6:36 PM
USMLE Step 2 l Gynecology
GYN Triad Benign cystic teratoma
Dermoid cysts are benign tumors. They can contain cellular tissue from all 3 germ layers. The
Benign Cystic Teratoma
most common histology seen is ectodermal skin appendages (hair, sebaceous glands), and
• Pelvic mass: reproductive therefore the name “dermoid.” Gastrointestinal histology can be identified, and carcinoid syn-
years drome has been described originating from a dermoid cyst. Thyroid tissue can also be identi-
• b-hCG (–) fied, and if it comprises more than 50% of the dermoid, then the condition of struma ovarii
is identified. Rarely, a malignancy can originate from a dermoid cyst, in which case the most
• S onogram: complex mass,
common histology would be squamous cell carcinoma, which can metastasize.
calcifications
PAINFUL ADNEXAL MASS
A 31-year-old woman is taken to the emergency department complaining of severe
sudden lower abdominal pain for approximately 3 h. She was at work when she
suddenly developed lower abdominal discomfort and pain, which got progressively
worse. On examination the abdomen is tender, although no rebound tenderness
is present, and there is a suggestion of an adnexal mass in the cul-de-sac area.
Ultrasound shows an 8-cm left adnexal mass with a suggestion of torsion of the ovary.
GYN Triad Diagnosis. Sudden onset of severe lower abdominal pain in the presence of an adnexal mass is
presumptive evidence of ovarian torsion.
Ovarian Torsion
• Abrupt unilateral pelvic pain Management. The management of the torsion should be to untwist the ovary and observe the
ovary for a few minutes in the operating room to assure revitalization. This can be performed
• b-hCG (–) with laparoscopy or laparotomy.
• Sonogram: >7 cm adnexal • Cystectomy. If revitalization occurs, an ovarian cystectomy can be performed with
mass preservation of the ovary.
• Oophorectomy. If the ovary is necrotic, a unilateral salpingo-oophorectomy is
performed.
Follow-Up. Patients should have routine examination 4 weeks after the operation and then
should be seen on a yearly basis. The pathology report should be checked carefully to make sure
that it is benign, and if this is the case, then they go to routine follow-up.
POSTMENOPAUSAL PELVIC MASS
A 70-year-old woman comes for annual examination. She complains of lower
abdominal discomfort; however, there is no weight loss or abdominal distention.
On pelvic examination a nontender, 6-cm, solid, irregular, fixed, left adnexal mass
is found. Her last examination was 1 year ago, which was normal.
Definition. A pelvic mass identified after menopause. Ovaries in the postmenopausal age group
should be atrophic; anytime they are enlarged, the suspicion of ovarian cancer arises.
192
S2 OB-GYN.indb 192 7/8/13 6:36 PM
Chapter 5 l Disorders of the Ovaries and Oviducts
Diagnostic Tests
• GI tract lesions. Abdominal pelvic CT scan or a pelvic ultrasound, and GI studies
(barium enema) to rule out any intestinal pathology such as diverticular disease
• Urinary tract lesions. IVP to identify any impingement of the urinary tract
Screening Test. There is no current screening test for ovarian cancer. Pelvic ultrasound is excel-
lent for finding pelvic masses, but is not specific for identifying which are benign and which
are malignant. Only 3% of patients undergoing laparotomy for sonographically detected pelvic
masses actually have ovarian cancer.
Epidemiology. Ovarian carcinoma is the second most common gynecologic malignancy, with
a mean age at diagnosis of 69 years. One percent of women die of ovarian cancer. It is the most
common gynecologic cancer leading to death.
Risk Factors. These include BRCA1 gene, positive family history, high number of lifetime ovu-
lations, infertility, and use of perineal talc powder.
Protective Factors. These are conditions that decrease the total number of lifetime ovulations: GYN Triad
oral contraceptive pills, chronic anovulation, breast-feeding, and short reproductive life.
Serous Carcinoma
Classification of Ovarian Cancer • Postmenopausal woman
• Epithelial tumors—80%. The most common type of histologic ovarian carcinoma
• Pelvic mass
is epithelial cancer, which predominantly occurs in postmenopausal women. These
include serous, mucinous, Brenner, endometrioid, and clear cell tumors. The most • ↑ CEA or CA-125 level
common malignant epithelial cell type is serous.
• Germ cell tumors—15%. Another histologic type of ovarian cancer is the germ cell GYN Triad
tumor, which predominantly occurs in teenagers. Examples are dysgerminoma, endo- Choriocarcinoma
dermal sinus tumors, teratomas, and choriocarcinoma. The most common malignant
germ cell type is dysgerminoma. It is uniquely x-ray sensitive. • Postmenopausal woman
• Stromal tumors—5%. The third type of ovarian tumor is the stromal tumor, which is • Pelvic mass
functionally active. These include granulosa-theca cell tumors, which secrete estrogen • ↑ hCG level
and can cause bleeding from endometrial hyperplasia and Sertoli-Leydig cell tumors,
which secrete testosterone and can produce masculinization syndromes. Patients with GYN Triad
stromal tumors usually present with early stage disease and are treated either with
removal of the involved adnexa (for patients who desire further fertility) or a TAH Sertoli-Leydig Tumor
and BSO (if their family has been completed). They metastasize infrequently, and then • Postmenopausal pelvic
they require chemotherapy (vincristine, actinomycin, and Cytoxan). mass
• Metastatic tumor. These are cancers from a primary site other than the ovary. The • Masculinization
most common sources are the endometrium, GI tract, and breast. Krukenberg tumors
are mucin-producing tumors from the stomach or breast metastatic to the ovary. • ↑ testosterone level
193
S2 OB-GYN.indb 193 7/8/13 6:36 PM
You might also like
- Reign Over Me ReflectionDocument2 pagesReign Over Me ReflectionBootstrapGamingNo ratings yet
- English Task Gynecology System: Case ReportDocument4 pagesEnglish Task Gynecology System: Case ReportCecepNo ratings yet
- Journal Reading Management of A Pelvic MassDocument40 pagesJournal Reading Management of A Pelvic MassCecilia SalimNo ratings yet
- O BGYNDocument84 pagesO BGYNselvie87100% (2)
- Current Diagnosis and Management of Ovarian Cysts: Review ArticlesDocument4 pagesCurrent Diagnosis and Management of Ovarian Cysts: Review ArticlesFelNo ratings yet
- Endometrial BiopsyDocument9 pagesEndometrial BiopsyAnna BartolomeNo ratings yet
- PancreatoblastomaDocument16 pagesPancreatoblastomaDr Farman AliNo ratings yet
- Malignant Ovarian TumourDocument46 pagesMalignant Ovarian Tumourahmed shorshNo ratings yet
- Ovarian Cancer SGTDocument25 pagesOvarian Cancer SGTAndre PutraNo ratings yet
- Abdominal (Retroperitoneal) Cystic Lympangioma.: KeywordsDocument3 pagesAbdominal (Retroperitoneal) Cystic Lympangioma.: KeywordsIordachescu AmaliaNo ratings yet
- Pre Mal Dis of CervixDocument44 pagesPre Mal Dis of CervixnoreenfatimamaanNo ratings yet
- Belle Cervical DiseaseDocument7 pagesBelle Cervical DiseaseRashed ShatnawiNo ratings yet
- Auto Article ProcessDocument6 pagesAuto Article ProcessJamshaid AhmedNo ratings yet
- Endometriosis and AdenomyosisDocument36 pagesEndometriosis and Adenomyosishacker ammerNo ratings yet
- Ca OvarioDocument13 pagesCa OvarioDaniel MálagaNo ratings yet
- 17-09-2019 Lower GI FINALDocument32 pages17-09-2019 Lower GI FINALNaima HabibNo ratings yet
- Mullerian Agenesis: An Unusual Presentation As Hematometra and Bilateral HematosalpinxDocument2 pagesMullerian Agenesis: An Unusual Presentation As Hematometra and Bilateral Hematosalpinxwanwan_adongNo ratings yet
- Frantz TumorDocument5 pagesFrantz TumorAndu1991No ratings yet
- B. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)Document14 pagesB. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)lizzy596No ratings yet
- MCQ Jeddah - Doc (FINAL) 2Document9 pagesMCQ Jeddah - Doc (FINAL) 2Indrajit Barua100% (1)
- Ovarian Masses: Surgery or Surveillance?Document9 pagesOvarian Masses: Surgery or Surveillance?MutianbllNo ratings yet
- ChanDocument2 pagesChankenny stefanusNo ratings yet
- A Case of Ovarian Fibroma Masquerading As A Uterine FibroidDocument5 pagesA Case of Ovarian Fibroma Masquerading As A Uterine FibroidAnonymous UHnQSkxLBDNo ratings yet
- Ovarian Cancer in PregnancyDocument36 pagesOvarian Cancer in PregnancyNicole BalagtasNo ratings yet
- Pico 1Document12 pagesPico 1annissaerceNo ratings yet
- Jurding BedahDocument18 pagesJurding BedahSharon Natalia RuntulaloNo ratings yet
- Adnexal Masses in Pediatric and Adolescent Females: A Review of The LiteratureDocument8 pagesAdnexal Masses in Pediatric and Adolescent Females: A Review of The LiteratureAlejandro GuzmanNo ratings yet
- Recurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Document2 pagesRecurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Motivational SpeechNo ratings yet
- gtg62 021211 OvarianmassesDocument14 pagesgtg62 021211 OvarianmassesMaryamNo ratings yet
- Cervical CancerDocument38 pagesCervical Cancerreema.saleh123No ratings yet
- Clinicopathological Profile of Ovarian Tumors in The Age Group 10-20 YearsDocument4 pagesClinicopathological Profile of Ovarian Tumors in The Age Group 10-20 YearsLauren RenNo ratings yet
- CRC and Other Colorectal Disease - PPT For Senior Medical StudentsDocument37 pagesCRC and Other Colorectal Disease - PPT For Senior Medical StudentsGiovanni HenryNo ratings yet
- 20.MBBS Pancreatic CancerDocument52 pages20.MBBS Pancreatic Cancermrajah95No ratings yet
- Surgical OncologyDocument10 pagesSurgical Oncologysofea zamriNo ratings yet
- Management of AISDocument10 pagesManagement of AISMaría Reynel TarazonaNo ratings yet
- Breast CancerDocument4 pagesBreast CancerMaikka IlaganNo ratings yet
- OvaryDocument4 pagesOvaryCarolina MartinezNo ratings yet
- Uterus NeoDocument11 pagesUterus NeoHester Marie SimpiaNo ratings yet
- Diagnostic Tools in ObgynDocument27 pagesDiagnostic Tools in ObgynHenok Y KebedeNo ratings yet
- A Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathDocument5 pagesA Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathLauren RenNo ratings yet
- (Gyne) Neoplastic Diseases of The Uterus (Dra. Ahyong-Reyes) ?Document6 pages(Gyne) Neoplastic Diseases of The Uterus (Dra. Ahyong-Reyes) ?RONALDO CUANo ratings yet
- (GYNE) Neoplastic Diseases of The Ovary-Dr. Dueñas (Parbs)Document10 pages(GYNE) Neoplastic Diseases of The Ovary-Dr. Dueñas (Parbs)adrian kristopher dela cruzNo ratings yet
- SESAP Abd HBPDocument90 pagesSESAP Abd HBPLamisNo ratings yet
- Impey Obs and Gynae Revision Notes PDFDocument9 pagesImpey Obs and Gynae Revision Notes PDFRoiseNo ratings yet
- Operative Treatment of Gynaecologic Diseases in Puberty: Seven Years of ExperienceDocument2 pagesOperative Treatment of Gynaecologic Diseases in Puberty: Seven Years of Experiencemajacokovikj.urologijaNo ratings yet
- Tambimuttu 2015Document2 pagesTambimuttu 2015cristian vivasNo ratings yet
- K GanDocument22 pagesK GancdatNo ratings yet
- 31422-Article Text-92425-1-10-20200923Document4 pages31422-Article Text-92425-1-10-20200923irvan bNo ratings yet
- FibroadenomaDocument5 pagesFibroadenomaAmalia FadhilaNo ratings yet
- Surgicopath July 2017Document105 pagesSurgicopath July 2017Rendy Adhitya PratamaNo ratings yet
- Laparoscopic Management of Giant Ovarian Cyst A Case ReportDocument3 pagesLaparoscopic Management of Giant Ovarian Cyst A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cancers of The Female Genital TractDocument31 pagesCancers of The Female Genital TractTresor MbuyiNo ratings yet
- Ovarian and Prostate CancerDocument51 pagesOvarian and Prostate CancerMa. Angelica Alyssa RachoNo ratings yet
- Clinical Case 54-Ovarian NeoplasmsDocument4 pagesClinical Case 54-Ovarian Neoplasmsselina kalenderNo ratings yet
- Cervical Dysgenesis With Transverse Vaginal Septum With Imperforate Hymen in An 11 Year Old Girl Presenting With Acute AbdomenDocument4 pagesCervical Dysgenesis With Transverse Vaginal Septum With Imperforate Hymen in An 11 Year Old Girl Presenting With Acute Abdomenshe-docNo ratings yet
- En Bloc Robot-Assisted Laparoscopic Partial Cystectomy, Urachal Resection, and Pelvic Lymphadenectomy For Urachal AdenocarcinomaDocument4 pagesEn Bloc Robot-Assisted Laparoscopic Partial Cystectomy, Urachal Resection, and Pelvic Lymphadenectomy For Urachal Adenocarcinomadr.tonichenNo ratings yet
- Potdar 2020Document8 pagesPotdar 2020Christian Leonardo Molina HinojosaNo ratings yet
- A Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesDocument2 pagesA Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesAlfa FebriandaNo ratings yet
- Management of Benign Breast Conditions: Part 2 - Breast Lumps and LesionsDocument3 pagesManagement of Benign Breast Conditions: Part 2 - Breast Lumps and Lesionspeter_mrNo ratings yet
- Periampullary CarcinomaDocument35 pagesPeriampullary Carcinomaminnalesri100% (2)
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentFrom EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentNo ratings yet
- Corn Agli A 2010Document2 pagesCorn Agli A 2010Alessandro ZadraNo ratings yet
- Managing Common Infections Summary TablesDocument8 pagesManaging Common Infections Summary TablesAlessandro ZadraNo ratings yet
- Practical Management of Anticoagulation in Patients With Atrial FibrillationDocument21 pagesPractical Management of Anticoagulation in Patients With Atrial FibrillationAlessandro ZadraNo ratings yet
- ArrhythmiasDocument1 pageArrhythmiasAlessandro ZadraNo ratings yet
- Treatment of Distal Iliotibial Band Syndrome in A Long Distance Runner With Gait Re Training Emphasizing Step Rate ManipulationDocument10 pagesTreatment of Distal Iliotibial Band Syndrome in A Long Distance Runner With Gait Re Training Emphasizing Step Rate ManipulationAlessandro ZadraNo ratings yet
- Who Recommends Assistance For People With Hiv To Notify Their PartnersDocument2 pagesWho Recommends Assistance For People With Hiv To Notify Their PartnerstashoneNo ratings yet
- Cholesterol Explained PDFDocument3 pagesCholesterol Explained PDFkapczukNo ratings yet
- The Interpersonal Approach and Group Theory Summary: ObjectivesDocument16 pagesThe Interpersonal Approach and Group Theory Summary: ObjectivesCami Matei CamiNo ratings yet
- Pricelist Alzetta AestheticDocument2 pagesPricelist Alzetta AestheticGisella Destiny Luh PrasastiNo ratings yet
- Rational Emotive Behaviour TherapyDocument30 pagesRational Emotive Behaviour TherapyJacqueline GonsalvesNo ratings yet
- Dimeglio Score Untuk ClubfootDocument4 pagesDimeglio Score Untuk ClubfootInezz LeonitaaNo ratings yet
- Nursing Care Plan: Assessment DataDocument2 pagesNursing Care Plan: Assessment DataDana CozorocNo ratings yet
- Nomophobia: No Mobile Phone Phobia: ArticleDocument5 pagesNomophobia: No Mobile Phone Phobia: ArticleAman ShabaNo ratings yet
- Effects of A Solution-Focused Mutual Aid Group For Hispanic Children of Incarcerated ParentsDocument12 pagesEffects of A Solution-Focused Mutual Aid Group For Hispanic Children of Incarcerated Parentssolutions4familyNo ratings yet
- Mental RetardationDocument19 pagesMental RetardationAsmarandi100% (1)
- Anxiety - Symptoms, Types, Causes, Prevention, and TreatmentDocument12 pagesAnxiety - Symptoms, Types, Causes, Prevention, and Treatmentzandro padillaNo ratings yet
- Early Mobilization in The Pediatric Intensive Care Unit A Systematic ReviewDocument6 pagesEarly Mobilization in The Pediatric Intensive Care Unit A Systematic ReviewJuly ZaballaNo ratings yet
- Letter To FreudDocument20 pagesLetter To FreudDaniel Lee Eisenberg JacobsNo ratings yet
- Biodose Models:Nsd, Cre, TDF, LQ& Their Limitations: Moderator: Mr. Ranjit Singh Presented By: Navneet KaurDocument54 pagesBiodose Models:Nsd, Cre, TDF, LQ& Their Limitations: Moderator: Mr. Ranjit Singh Presented By: Navneet KaurSAlonii ChawlaNo ratings yet
- End of Life EdDocument6 pagesEnd of Life EdZulkifli PomalangoNo ratings yet
- Antibiotic Resistant BacteriaDocument6 pagesAntibiotic Resistant BacteriaAmandaNo ratings yet
- Accelerated OrthodonticsDocument13 pagesAccelerated OrthodonticsJustin Kimberlake100% (1)
- A Comparison of Human Dental Pulp Response To CalcDocument5 pagesA Comparison of Human Dental Pulp Response To CalcrespikNo ratings yet
- Cancer of The BreastDocument19 pagesCancer of The BreastJoanna TaylanNo ratings yet
- Lyme, CF ProtocolDocument36 pagesLyme, CF ProtocolTheresa Dale100% (1)
- Clinical Experiences of Using A Cellulose Dressing On Burns and Donor Site WoundsDocument4 pagesClinical Experiences of Using A Cellulose Dressing On Burns and Donor Site WoundsabdmaliknasNo ratings yet
- Papini SIBIU 2018Document53 pagesPapini SIBIU 2018Alina Ioana PaduraruNo ratings yet
- Fracture Nursing Care PlansDocument14 pagesFracture Nursing Care PlansSheryl Ann Barit PedinesNo ratings yet
- Renal CalculiDocument16 pagesRenal CalculiMeenu NegiNo ratings yet
- Lecture - 2 - Psychopharmacology - History, Neurotransmitters Etc - May 2013Document24 pagesLecture - 2 - Psychopharmacology - History, Neurotransmitters Etc - May 2013Robert EdwardsNo ratings yet
- What Are Healing GardensDocument9 pagesWhat Are Healing GardensMuhammad Tahir PervaizNo ratings yet
- Solution-Focused Counseling: An Integrative Approach: by Jeffrey T. Guterman, PH.DDocument60 pagesSolution-Focused Counseling: An Integrative Approach: by Jeffrey T. Guterman, PH.DAriep IlhamNo ratings yet
- Guideline On Induction of Ovulation 2011Document20 pagesGuideline On Induction of Ovulation 2011Atik ShaikhNo ratings yet
- Form 2B: Inventory of Training Equipment: Maritime Industry Authority STCW Administration OfficeDocument9 pagesForm 2B: Inventory of Training Equipment: Maritime Industry Authority STCW Administration OfficeDemp AlmiranezNo ratings yet