Professional Documents
Culture Documents
Use of An Artificial Neural Network For The Diagnosis of Myocardial Infarction
Use of An Artificial Neural Network For The Diagnosis of Myocardial Infarction
Uploaded by
Dewi Cahya FitriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Use of An Artificial Neural Network For The Diagnosis of Myocardial Infarction
Use of An Artificial Neural Network For The Diagnosis of Myocardial Infarction
Uploaded by
Dewi Cahya FitriCopyright:
Available Formats
Use of an Artificial Neural Network for the Diagnosis of
Myocardial Infarction
William G. Baxt, MD
• Objective: To validate prospectively the use of an Jilectronic data processing technologies have been
artificial neural network to identify myocardial infarction used to aid in clinical diagnosis for more than 20 years
in patients presenting to an emergency department (1). The acceptance of such technologies has not oc-
with anterior chest pain. curred (2). The reasons for this are varied but can be
• Design: Prospective, blinded testing. traced to the fact that their use is time-consuming and
• Setting: Tertiary university teaching center. inconvenient and because most have not been able to
• Patients: A total of 331 consecutive adult patients perform consistently better than physicians (2, 3). Arti-
presenting with anterior chest pain. ficial neural network-based pattern recognition has been
• Measurements: Diagnostic sensitivity and speci- successfully used in several complex environments,
ficity with regard to the diagnosis of acute myocardial which suggests that this technology may, potentially, be
infarction. applied to the clinical setting (4-7). Unlike most other
• Main Results: An artificial neural network was forms of artificial intelligence, the artificial neural net-
trained on clinical pattern sets retrospectively derived work can improve performance by training. The net-
from the cases of 351 patients hospitalized with a high works can also define relationships among input data
likelihood of having myocardial infarction. It was pro- that are inapparent using other approaches, and they
spectively tested on 331 consecutive patients present- can use these relationships to improve accuracy. This
ing to an emergency department with anterior chest technology has been applied to the analysis of clinical
pain. The ability of the network to distinguish patients data (8-15); however, the network's diagnostic accuracy
with from those without acute myocardial infarction has not been substantially better than that of physicians
was compared with that of physicians caring for the (16-18).
same patients. The physicians had a diagnostic sensi- An artificial neural network has been trained to diag-
tivity of 77.7% (95% CI, 77.0% to 82.9%) and a diag- nose, with a high degree of accuracy, acute myocardial
nostic specificity of 84.7% (CI, 84.0% to 86.4%). The infarction in patients presenting to an emergency de-
artificial neural network had a sensitivity of 97.2% (CI, partment (19). Data sets that were retrospectively ob-
97.2% to 97.5%; P = 0.033) and a specificity of 96.2% tained from 356 patients suspected of having had a
(CI, 96.2% to 96.4%; P< 0.001). myocardial infarction were used to train and test the
• Conclusion: An artificial neural network trained to network. The network was trained on one half of the
identify myocardial infarction in adult patients present- patients and was tested on the remaining half to which
ing to an emergency department may be a valuable aid it had never been exposed. The process was reversed
to the clinical diagnosis of myocardial infarction; how- and the results pooled in order to test all patients. The
ever, this possibility must be confirmed through pro- network performed with a sensitivity of 92% and a
spective testing on a larger patient sample. specificity of 96% (19). These figures were substantially
better than those reported previously for either physi-
cians (sensitivity, 88%; specificity, 71%) or any comput-
er-based technology (sensitivity, 88%; specificity, 74%)
(20). The network had a sensitivity of 80% and a spec-
ificity of 96% when all patients with electrocardio-
graphic evidence of myocardial infarction were removed
from the study sets. This work has recently been inde-
pendently corroborated (21).
Because the initial study was retrospective, the net-
work's performance must be prospectively validated be-
fore this network can be considered a legitimate aid to
clinical diagnosis. We report the results of the first
phase of this validation, the prospective testing of the
network on a group of 331 adult patients presenting to
an emergency department with anterior chest pain.
Methods
Annals of Internal Medicine. 1991;115:843-848.
Description of Artificial Neural Network
From the University of California, San Diego Medical Center,
San Diego, California. For the current author address, see end An artificial neural network is a group of interconnected
of text. mathematic equations that accept input data and that calculate
©1991 American College of Physicians 843
Downloaded From: http://annals.org/ by a Stony Brook University User on 12/15/2016
an output based on this input. This structure is a predesigned
method for the application of nonlinear statistical techniques.
Network operation can be understood by referring to the
highly simplified artificial neural network depicted in Figure 1.
The input pattern in this instance consists of two variables, A
and B. Each of these variables is entered into the respective
input unit of the network. These values are multiplied by an
initially random number called a weight. The products of these
multiplications are summed and become the net input of the
hidden layer unit. This value is then entered in a logistic
function that calculates the activation of the hidden unit. The
activation of the hidden unit is multiplied by a third weight.
This product becomes the net input of the output unit. This
sum is then entered into the same logistic function that calcu-
lates the activation of the output unit or the ''network output."
The network is trained by modifying the value of the
weights. These values are modified through "back propaga-
tion," a process that uses the error in network output to
determine weight modification (5, 6). The error is defined as
the difference between the network output for a specific train-
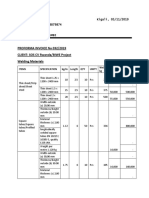
ing pattern and the expected output of that training pattern. Figure 2. Diagnostic network. 20x10x10x1 network with 20
During the training process, these weight values are deter- input units, 2 layers of 10 units, and 1 output unit.
mined so that the overall computation carried out by the net-
work is optimized to produce a minimal error. A properly
trained network is able to extract any functional or statistical adult patients presenting to an emergency department with
relationship between the input and output present in the train- anterior chest pain (Table 1). The network is trained so that
ing data. the output represents the presence or absence of acute myo-
Because of the large number of floating point calculations cardial infarction. Although network output is not a probabil-
made by the network, it must be run on a data processing ity, it can be viewed in a similar manner, and output values
platform. The network can be hard-wired into the platform and can be used as a measure of incident likelihood. To simplify
can reside as hardware or it can be written as a software this initial prospective study, a cut-off value was chosen to
application. The network used in this study is illustrated in discriminate between the presence and absence of myocardial
Figure 2. It consists of 20 input units, two layers of 10 internal infarction. In actual practice, the output could be viewed as
or hidden units, and an output unit. The numbers of input representing the likelihood of myocardial infarction.
units, hidden units, and layers of hidden units were chosen by
trial and error during the initial development of the network Training the Network
(19).
In applying the artificial neural network described here, the The network training process consists of the retrospective
inputs are selected from the presenting symptoms, the past selection of a large number of patients who have presented
history findings, and the physical and laboratory findings of with anterior chest pain and who are known to have had or to
have not had an acute myocardial infarction. These patients'
cases are used to derive a set of training patterns for the
network. Training consists of the repeated sequential presen-
tation of the training set to the network until the error in the
output stops decreasing. Training is optimized by concurrently
testing the network on a subset of patterns derived from the
training patterns to which the network has not been exposed.
When the error made on this set has stopped decreasing,
training has been optimized.
The mathematics of this process have been previously re-
ported (6) and are presented in the Appendix. The artificial
neural network simulator for this project was written specifi-
cally for this study in C and was run on an 80386 microcom-
puter using an 80387 math coprocessor running at 20 mHz. The
network was trained as reported previously, using 351 of the
original 356 patients from the original study as the training set
(19). The five patients whose cases were omitted all had ex-
tremely atypical presentations. These cases were never re-
solved by the network. Previous analysis revealed that, by
omitting these cases, a weight set that made the network more
accurate in identifying prospective patients was derived. These
patients' confusing cases were, therefore, removed from the
training set to optimize network training.
Figure 1. Simplified operation of artificial neural network with Ten thousand iterations were run. The training parameters of
two input units, one hidden unit, and one output unit (2x1x1). learning rate and momentum were set at 0.05 and 0.9, respec-
The input pattern consists of the two variables, A and B. Each tively (see Appendix for an explanation). The final trained
of these variables is entered into the respective input unit of weight set had an error rate of 0.00256 per pattern. Patients
the network. These values are multiplied by an initially random whose pattern, when entered into the network, yielded an
number called a weight [WT(1), WT(2)]. The products of these output of more than 0.55 were deemed to have had a myocar-
multiplications are summed and become the net input of the dial infarction, and patients whose pattern resulted in an out-
hidden layer unit. This value is placed in a logistic function put of 0.55 or more were deemed not to have had a myocardial
that calculates the net activation of the hidden unit. The net infarction. In this setting, the network output was between 0 to
activation of the hidden unit is multiplied by a third weight 0.1 and 0.9 to 1.0 97% of the time. The actual choice of cut-off
[WT(3)]. This product then becomes the net input of the output value—between 0.1 and 0.9—affects few cases. The value of
unit. This sum is entered into the same logistic function that 0.55 was chosen for this study because it segregated the pa-
calculates the net activation of the output unit (termed network tients best. When the trained network was tested on the train-
output). ing patterns, there were no diagnostic errors using the value of
844 1 December 1991 • Annals of Internal Medicine • Volume 115 • Number 11
Downloaded From: http://annals.org/ by a Stony Brook University User on 12/15/2016
0.55 to discriminate between the presence and absence of Table 2. Accuracyy of the Ph ysician and of th e Artificial
myocardial infarction. In the initial study (19), the network was Neural Network iin Diagnosinig Acute Myocarclial Infarc-
trained on half of the 351 patients and then was tested on the
second half to which it had not been exposed. This process tion
was then reversed so that the network could be tested on all
351 patients. In this instance, all 351 patients participating in Variable Data 95% CI P Value
the initial study were used as the training set (19). %
All patients 18 years of age or older presenting to an emer-
gency department with anterior chest pain were enlisted in the Sensitivity
study. The physician treating the patient was asked to com- Physicians
plete a questionnaire that documented the presence of the Correct, n 28
items listed in Table 1. In this way, all data used by the Incorrect, n 8
network were coded by the physicians caring for the patients, Percentage 77.7 77.0 to 82.9
and both the network and the physician used the same data as Network
the basis for diagnosis. To test the network in a setting as Correct, n 35
close as possible to the environment in which it would operate Incorrect, n 1
prospectively, it was tested only on the inputs provided by the Percentage 97.2 97.2 to 97.5 0.03
treating physicians. No attempt was made to change what, on Specificity
retrospective chart review, turned out to be inaccurate or Physicians
incorrect inputs made by these physicians. The physician was Correct, n 250
also asked to guess whether the patient had had a myocardial Incorrect, n 45
infarction. The physicians were medical residents in postgrad- Percentage 84.7 84.0 to 86.4
uate years 2 and 3 and emergency department attending faculty Network
physicians. Correct, n 284
Final patient diagnosis was established by the following: Incorrect, n 11
Admitted patients were followed through review of their inpa- Percentage 96.2 96.2 to 96.4 < 0.001
tient record after discharge. Patients who were referred to the
outpatient department were followed through review of their
outpatient records. Patients who were neither admitted nor
referred to the outpatient center were followed through tele- ues of less than 0.05 were considered statistically significant.
phone interview 3 weeks after their initial emergency depart- Power was calculated by use of standard power formulas.
ment visit. Patients who could not be followed were dropped
from the study. The follow-up data were entered into the data
base without reference to the presenting data so that this Results
process would be blinded to the initial data entry.
Myocardial infarction was defined in this study as fulfillment The cases of 355 patients were initially studied.
of one of the following criteria (20): characteristic evolution of Twenty-four nonadmitted patients could not be fol-
serum enzyme levels, including a creatine kinase MB fraction lowed. These 24 patients had noncardiac diagnoses, and
of at least 5% of the total creatine kinase or a lactate dehy- normal electrocardiograms were obtained for these pa-
drogenase isoenzyme 1 level that was higher than the isoen-
zyme 2 level (in the absence of hemolysis or renal infarction); tients in the emergency department. Of the study pa-
an electrocardiogram showing the development of new patho- tients, 192 were men (mean age, 51.6 years) and 139
logic Q waves (lasting at least 0.04 seconds) and at least a 25% were women (mean age, 52.4 years). Thirty-six patients
decrease in the amplitude of the following R wave, as com- had had a myocardial infarction, 63 patients had cre-
pared with that of the electrocardiogram obtained in the emer- scendo angina, 38 patients had angina, and the remain-
gency department; or a scintiscan showing the focal uptake of
tech-99m stannous pyrophosphate in the cardiac area if the ing 194 patients had noncardiac etiologies. No patient
serum enzyme level peaked before hospitalization. In addition, diagnosed with myocardial infarction did not fulfill the
all records were reviewed to determine whether the cases of all original study criteria.
patients diagnosed as having had a myocardial infarction met Network testing of all 331 patients yielded 0.03773
the study definition. Statistical analysis was carried out by the
calculation of confidence intervals (22) and by use of chi- error per patient. Table 2 depicts the diagnostic perfor-
square analysis of 2-by-2 contingency tables using the Yates mances of the physicians and of the artificial neural
correction and the McNemar symmetry chi-square test. P val- network. The physicians correctly diagnosed 28 patients
Table 1. Input Variables
History History Examination Electrocardiographic
Findings Findings Findings
Age*t Acute myocardial Jugular venous 2-mm ST-segment elevation*
infarction* distension*
Sex* Angina* Rales* 1-mm ST-segment elevation*
Left anterior location of pain* Diabetes* ST-segment depression*
Intensity of pain Hypertension* T-wave inversion*
Radiation of pain Significant ischemic change*
Nausea and vomiting*
Diaphoresis*
Syncope
Shortness of breath*
Palpitations*
Response to nitroglycerin*
* Variables actually used by the network.
t Analog coded.
1 December 1991 • Annals of Internal Medicine • Volume 115 • Number 11 845
Downloaded From: http://annals.org/ by a Stony Brook University User on 12/15/2016
with myocardial infarction for a sensitivity of 77.7% are linear statistical methodologies. The artificial neural
(95% CI, 77.0% to 82.9%) and correctly diagnosed 250 network is a method for the application of nonlinear
patients without myocardial infarction for a specificity statistics. Although it can only be postulated, the ability
of 84.7% (CI, 84.0% to 86.4%). The network incorrectly of the network to identify new relationships between
diagnosed 1 patient with myocardial infarction for a input clinical variables may emanate from its inherent
97.2% sensitivity (CI, 97.2% to 97.5%) and incorrectly nonlinear method of data analysis.
diagnosed 11 patients without myocardial infarction for The diagnostic accuracy afforded by the use of an
a specificity of 96.2% (CI, 96.2% to 96.4%). The differ- artificial neural network could significantly affect the
ence in the sensitivity had a chi-square Yates-corrected clinical diagnosis of myocardial infarction. The im-
P value of 0.033 and a McNemar symmetry chi-square provement in sensitivity could potentially lead to an
P value of 0.008. The difference in specificity had a improved ability to identify those patients with actual
Yates-corrected chi-square P value of less than 0.001 myocardial infarction. Missed diagnoses of myocardial
and a McNemar symmetry chi-square P value of less infarction have been reported to be the single largest
than 0.001. cause of the loss of medical malpractice settlements
The charts of all patients whom the network incor- made against emergency departments (24). Further, the
rectly diagnosed were analyzed. Eleven patients were high specificity that results from network use could lead
incorrectly diagnosed as having had a myocardial in- to significant cost savings by reducing the unnecessary
farction. Of these, 4 patients were recorded as having admission of patients to either the intensive care unit or
had new ischemic changes on their electrocardiograms: the hospital. One study estimated that a 3% improve-
1 with new 2 mm of ST-segment elevation, 2 with new ment in specificity could lead to an annual national cost
1 mm of ST-segment elevation, and 1 with new T-wave savings of $85 million (19). The improvement in speci-
inversion. When the electrocardiograms of these pa- ficity by at least 10%, as shown in this study, could
tients were reviewed by inpatient services, all four were yield a potential annual savings of over $0.28 billion.
thought not to have had new ischemic changes. The 1 Actual application of this technology would not be dif-
patient who was incorrectly diagnosed as not having ficult. Once the network is trained, it could be placed in
had a myocardial infarction had no significant clinical a hand-held calculator and could provide immediate
findings other than minimal left anterior chest pain. This outputs for inputted sets of clinical variables.
patient had no electrocardiographic evidence of acute
myocardial infarction, and this patient's final diagnosis The interpretation of these results is limited in several
was based on enzyme changes alone. ways: Not all patients were followed diagnostically in
the same manner. Neither serial cardiac enzyme level
measurements nor electrocardiograms were obtained for
Discussion patients not admitted to the hospital. Twenty-four pa-
The diagnostic accuracy of the artificial neural net- tients could not be followed and were dropped from the
work in predicting both the presence and the absence of study; however, all of these patients were thought to
acute myocardial infarction in a group of prospectively have chest pain of noncardiac etiology, and normal
collected patients to whom the network had never been electrocardiograms were obtained for these patients in
exposed was better than that of the physicians caring the emergency department. If these patients were in-
for these patients in the emergency department. Artifi- cluded in the study and were considered to have been
cial neural network technology was applied to clinical correctly diagnosed as not having had a myocardial
data in the hope that diagnostic accuracy could be im- infarction by the physicians, physician specificity would
proved by using information or relationships among improve to 85.89%, and physicians would still be sig-
clinical pattern sets that were inapparent using other nificantly less accurate than the network.
means. Although the evidence for this is indirect, the The network was tested against the physicians caring
better diagnostic accuracy of the network suggests that for the study patients, and its performance was not
it may identify such relationships in the clinical data compared with that of other previously developed elec-
sets that have heretofore not been elucidated. tronic aids to the diagnosis of myocardial infarction (20,
Another possible reason for the improved accuracy of 23). The sensitivity and specificity observed for physi-
the network is that this paradigm, in contrast to other cians in this study differed significantly from those pre-
computer-based approaches, can operate with inaccu- viously reported for a considerably larger number of
rate or missing data. Such networks are known to be physicians (20), the sensitivity reported here being
able to identify relationships even when some of the lower (77% compared with 88%) and the specificity
input data are incomplete or inaccurate (12). This fea- being higher (85% compared with 71%). The former
ture makes the network an excellent candidate to deal weighted the statistical analysis in favor of the rejection
with the inaccuracy and inconsistency associated with of the null hypotheses in terms of the reported differ-
patient histories and physical findings. Further, the net- ences in sensitivities. If physician sensitivity is 88%, as
work appears to be able to deal with the complexities of previously reported, then a minimum of 100 patients
singular disease states characterized by totally differing who have had an acute myocardial infarction or a total
clinical presentations. of 1100 patients must be enlisted to reach statistical
The artificial neural network may achieve higher ac- significance (Yates-corrected chi-square, P - 0.032). In
curacy than the other two widely used approaches to addition, the physician sensitivity and specificity in this
the diagnosis of myocardial infarction, regression anal- study was measured from the actual physician guess
ysis (23) and recursive partitioning (20), because these about the presence or absence of myocardial infarction,
846 1 December 1991 • Annals of Internal Medicine • Volume 115 • Number 11
Downloaded From: http://annals.org/ by a Stony Brook University User on 12/15/2016
whereas that with which it is compared was based on The activation of the second layer hidden units is calculated
triage decisions made by the treating physicians (20). by use of the first equation in a manner analogous to that used
to calculate the activation of the first layer hidden units. In the
Finally, only the diagnosis of myocardial infarction latter instance, the input signal now becomes the net activation
was studied, whereas the diagnosis of other important of each first layer hidden unit, which is multiplied by the
cardiac conditions, such as new-onset angina or cre- weights on the projections between each of the first and sec-
scendo angina, was not studied. This limitation simpli- ond layer hidden units. Unit activation is calculated by the use
of equation 2. Network output is also calculated in an analo-
fied the study and the interpretation of results. Clearly,
gous manner, with the second layer hidden units now provid-
if this technology proves to be as accurate as these ing the input signal, which is multiplied by the weights on the
initial data imply, the technology could be extended to ten projections to the output unit. Unit activation (network
other ischemic conditions. output) is again calculated by use of equation 2.
Until the network is tested on a large number of The difference between a training pattern output or target
value and the network output api, termed e, is calculated by
patients, the study can be seen only as a first step in the subtracting network output from the target value tpi. An e is
prospective validation of the use of the artificial neural calculated for each noninput unit of the network and used by
network as an aid to the clinical diagnosis of myocardial the back propagation algorithm to modify all weights of the
infarction. A multicenter study designed to compare network such that, when pattern p is again inputted, the dif-
prospectively the performance of the artificial neural ference between network output and the pattern target value
will diminish.
network with those of physicians and other technologies Weight is modified by the derivation of delta. The delta for
on a large number of patients is currently underway (20, the output unit is calculated by:
23). If this study is successful, the possibility that this
technology could be used prospectively as well as be 3. dp, = (tpi - api)fi(netpi)
extended to other clinical settings could be explored. where fi(netpi) is the derivative of the activation function with
Finally, potentially one of the most important aspects respect to a change in the net input to the unit.
of these findings may be that the network may be able The delta for the hidden units is calculated in terms of the
units to which they project and the weights on those projec-
to identify relationships between clinical patient varia- tions:
bles that have not been appreciated by clinicians in the
past. Strategies have already been developed to define n
these relationships (21, 25). Not only does this possibil- 4. SPi=fi(netpi) 2 SpkWki
ity have important implications about the limits of clin- k= Q
ical reasoning, but it also may suggest that such tech- Weights and biases are updated by the calculation of the
nologies as reported here may potentially be used in delta weight:
further elucidating disease processes in general. Such
conclusions await ultimate validation of these observa- 5. Awj = awj + ((1 - a)(e8jaj))
tions and the successful extension of these technologies where alpha is termed network momentum and epsilon is
to other disease states. termed the learning rate parameter. Weights are updated by
adding the delta weight to the old weight.
Acknowledgments: The author thanks Dr. David Zipser for technical Training of the network is followed by calculating the
help and Ms. Kathleen James for manuscript preparation. summed square of the error, represented by E, across the
entire pattern set:
Requests for Reprints: William G. Baxt, MD, Department of Emer-
gency Medicine, UCSD Medical Center, 225 Dickinson Street, #8676, 6. E = E E (tPi ~ Opi)2
San Diego, CA 92103-8676.
P i
Current Author Address: Dr. Baxt: Department of Emergency Medi- where the index p ranges over the set of input patterns P, i
cine, UCSD Medical Center, 225 Dickinson Street, #8676, San Diego,
CA 92103-8676. ranges over the set of output units, tpi is the target of pattern
p, Opi is the network output for pattern p. When the summed
square of the error has ceased diminishing or has reached 0,
Appendix the network has been trained. If no relationship between the
pattern sets and their target value exists, this value will not
The mathematical operation of the network can best be diminish.
appreciated by again referring to Figure 1. This aspect of
network application is independent of its specific use and can
be viewed as generic. The network functions by the application
of binary or analog coded data comprising the pattern set to References
the 20 input units (see Table 1). This signal is then multiplied 1. Reggia JA, Tuhrim S; eds. Computer-Assisted Medical Decision
by the initially random weights on the projections between Making. Computers and Medicine, v. 2. New York: Springer-Ver-
each input unit and the first layer hidden units: lag; 1985.
2. Szolovits P, Patil RS, Schwartz WB. Artificial intelligence in medical
n diagnosis. Ann Intern Med. 1988;108:80-7.
3. McDonald CJ. Protocol-based computer reminders, the quality of
1. netpi = ZJ wuapj + biasj care and the non-perfectibility of man. N Engl J Med. 1976;295:
j=o 1351-5.
4. Widrow G, Hoff ME. 1960 Adaptive Switching Circuits Institute of
where netpi equals the net input of the unit for pattern p, w is Radio Engineering Western Electronic Show and Convention. Con-
a random weight, a is the input value applied to the unit, j vention Record; part 4:96-104.
represents the input or presynaptic units, / represents the first 5. Rumelhart DE, Hinton GE, Williams RJ. Learning internal repre-
layer hidden unit or postsynaptic unit, and bias is a modifiable sentations by error propagation. In: Rumelhart DE, McClelland JL;
weight that is multiplied by an input that is always equal to 1. eds. Parallel Distributed Processing: Explorations in the Microstruc-
The net activation of the hidden unit is calculated by: ture of Cognition. Cambridge, Massachusetts: MIT Press; 1986:318-
64.
1 6. McClelland JL, Rumelhart DE. Training hidden units. In: McClel-
2 a [ =
land JL, Rumelhart DE; eds. Explorations in Parallel Distributed
' P J + e~netpi Processing. Cambridge, Massachusetts: MIT Press; 1988:121-60.
1 December 1991 • Annals of Internal Medicine • Volume 115 • Number 11 847
Downloaded From: http://annals.org/ by a Stony Brook University User on 12/15/2016
7. Weigend AS, Huberman BA, Rumelhart DE. Predicting the future: a diagnosis of dementia. Symposium on Computer Applications in
connectionist approach. Stanford PDP Research Group, April 1990. Medical Care 1988 Proceedings: 12th Annual Symposium, Washing-
8. Hudson DL, Cohen ME, Anderson MF. Determination of testing ton, DC. 1988;12:245-50.
efficacy in carcinoma of the lung using a neural network model. 17. Bounds DG, Lloyd PJ, Mathew BG. A comparison of neural net-
Symposium on Computer Applications in Medical Care 1988 Pro- work and other pattern recognition approaches to the diagnosis of
ceedings: 12th Annual Symposium, Washington, DC. 1988;12:251-5. low back disorders. Neural Networks. 1990;3:583-91.
9. Smith JW, Everhart JE, Dickson WC, Knowler WC, Johannes RS. 18. Yoon YO, Brobst RW, Bergstresser PR, Peterson LL. A desktop
Using the ADAP learning algorithm to forecast the onset of diabetes neural network for dermatology diagnosis. Journal of Neural Net-
mellitus. Symposium on Computer Applications in Medical Care work Computation. 1989;summer:43-52.
1988 Proceedings: 12th Annual Symposium, Washington, DC. 1988; 19. Baxt WG. Use of an artificial neural network for data analysis in
12:261-5. clinical decision-making: the diagnosis of acute coronary occlusion.
10. Saito K, Nakano R. Medical diagnostic expert system based on PDP Neural Computation. 1991;2:480-9.
model. Proceedings of the International Joint Conference on Neural 20. Goldman L, Cook EF, Brand DA, et al. A computer protocol to
Networks, San Diego. 1988;2:255-62.
predict myocardial infarction in emergency department patients with
11. Kaufman JJ, Chiabera A, Hatem M, et al. A neural network ap-
chest pain. N Engl J Med. 1988;318:797-803.
proach for bone fracture healing assessment. IEEE Engineering in
21. Harrison RF, Marshall SJ, Kennedy RL. The early diagnosis of
Medicine and Biology Magazine. 1990;9:23-30.
heart attacks: a neurocomputational approach. Proceedings of the
12. Hiraiwa A, Shimohara K, Tokunaga Y. EEG topography recognition
International Joint Conference on Neural Networks, Seattle. 1991;
by neural networks. IEEE Engineering in Medicine and Biology
Magazine. 1990;9:39-42. 1:1-5.
13. Cios KJ, Chen K, Langenderfer RA. Use of neural networks in 22. Bailey BJ. Large sample simultaneous confidence intervals for the
detecting cardiac diseases from echocardiographic images. IEEE multinomial probabilities based on transformations of the cell fre-
Engineering in Medicine and Biology Magazine. 1990;9:58-60. quencies. Technometrics. 1980;22:583-9.
14. Marconi L, Scalia F, Ridella S, Arrigo P, Mansi C, Mela GS. An 23. Posen MW, D'Agostino RB, Selker HP, Sytkowski PA, Hood WB Jr.
application of back propagation to medical diagnosis. Proceedings A predictive instrument to improve coronary-care-unit admission
of the International Joint Conference on Neural Networks, Wash- practices in acute ischemic heart disease. A prospective multicenter
ington, DC. 1989;2:577. clinical trial. New Engl J Med. 1984;310:1273-8.
15. Eberhart RC, Dobbins RW, Hutton LV. Neural network paradigm 24. Rusnak RA, Stair TO, Hansen K, Fastow JS. Litigation against the
comparisons for appendicitis diagnosis. Proceedings of the Fourth emergency physician: common features in cases of missed myocar-
Annual IEEE Symposium on Computer-Based Medical Systems. dial infarction. Ann Emerg Med. 1989;18:1029-34.
1991:298-304. 25. Gallant SI. Connectionist expert systems. Communications of the
16. Mulsant GH, Servan-Schreiber E. A connectionist approach to the ACM. 1988;31:152-61.
848 1 D e c e m b e r 1991 • Annals of Internal Medicine • Volume 115 • Number 11
Downloaded From: http://annals.org/ by a Stony Brook University User on 12/15/2016
You might also like
- Operating Instructions: V2500-A1/A5 SERIES Commercial Turbofan Engines On The Airbus A319/A320/A321 Ceo AIRPLANESDocument79 pagesOperating Instructions: V2500-A1/A5 SERIES Commercial Turbofan Engines On The Airbus A319/A320/A321 Ceo AIRPLANESBilal Abbasi100% (2)
- 1magnetic Forces On Wires: Equipment IncludedDocument12 pages1magnetic Forces On Wires: Equipment IncludedDewi Cahya FitriNo ratings yet
- Chemistry Investigatory Project On Bio-Diesel Made by Kamal/KishanDocument15 pagesChemistry Investigatory Project On Bio-Diesel Made by Kamal/KishanKishan Saluja76% (84)
- Use of Artificial Neural Network in Diagnostic PatDocument4 pagesUse of Artificial Neural Network in Diagnostic Patsellappan marappanNo ratings yet
- ScienceDocument1 pageScienceFionaNo ratings yet
- Artificial Neural Networks Based Heart Disease Predictive ApproachDocument4 pagesArtificial Neural Networks Based Heart Disease Predictive ApproachInternational Journal of Application or Innovation in Engineering & ManagementNo ratings yet
- Bmjopen 2018 022810Document15 pagesBmjopen 2018 022810syukronchalimNo ratings yet
- 2019 DsadaşsklDocument8 pages2019 DsadaşsklAhmet KaragozNo ratings yet
- Prediction of Heart Disease Using Neural Network With Back PropagationDocument4 pagesPrediction of Heart Disease Using Neural Network With Back PropagationIntegrated Intelligent ResearchNo ratings yet
- Automatic Seizure Detection Using Three-Dimensional CNN Based On Multi-Channel EEGDocument10 pagesAutomatic Seizure Detection Using Three-Dimensional CNN Based On Multi-Channel EEGDhanalekshmi YedurkarNo ratings yet
- Brain Tumor Classification Using Deep Learning AlgorithmsDocument12 pagesBrain Tumor Classification Using Deep Learning AlgorithmsIJRASETPublicationsNo ratings yet
- Stroke Prediction System Using ANN (Artificial Neural Network)Document3 pagesStroke Prediction System Using ANN (Artificial Neural Network)International Journal of Innovative Science and Research TechnologyNo ratings yet
- ABSTRACT TechnicalDocument2 pagesABSTRACT TechnicalSahil TiwariNo ratings yet
- BP 2Document6 pagesBP 2kandeharikabaiNo ratings yet
- Diagnosis of Pneumonia From Chest X-Ray Images Using Deep LearningDocument5 pagesDiagnosis of Pneumonia From Chest X-Ray Images Using Deep LearningShoumik MuhtasimNo ratings yet
- Transfer LearningDocument7 pagesTransfer LearningAdah EneNo ratings yet
- 2004-Neural Network Classification of Ped - Post FossaDocument10 pages2004-Neural Network Classification of Ped - Post FossaAhmet KaragozNo ratings yet
- Breast Cancer Diagnosis Using Artificial Intelligence Neural NetworksDocument13 pagesBreast Cancer Diagnosis Using Artificial Intelligence Neural NetworksAndy PutraNo ratings yet
- Document3 TexDocument4 pagesDocument3 TexNavin M ANo ratings yet
- Pneumonia Detection Using VGG19 (Group No. 10)Document20 pagesPneumonia Detection Using VGG19 (Group No. 10)Amrit Kumar100% (1)
- Rana 2018Document6 pagesRana 2018smritii bansalNo ratings yet
- Chronic Kidney Disease Prediciton Using Neural NetworksDocument5 pagesChronic Kidney Disease Prediciton Using Neural NetworksNirmal KumarNo ratings yet
- Urinary System Diseases Diagnosis Using Artificial Neural NetworksDocument5 pagesUrinary System Diseases Diagnosis Using Artificial Neural NetworksEsemuze LuckyNo ratings yet
- 2022-CMIG-End-systole and End-Diastole Detection in Short Axis Cine MRI Using A Fully CNN With Dilated ConvolutionsDocument8 pages2022-CMIG-End-systole and End-Diastole Detection in Short Axis Cine MRI Using A Fully CNN With Dilated ConvolutionsZhenyu BuNo ratings yet
- Icec 2020Document5 pagesIcec 2020Nur SakinahNo ratings yet
- Comparison of Different Types of Artificial Neural Networks For Diagnosing Thyroid DiseaseDocument11 pagesComparison of Different Types of Artificial Neural Networks For Diagnosing Thyroid DiseaseSabrina JonesNo ratings yet
- Implementation of An Incremental Deep Learning Model For Survival Prediction of Cardiovascular PatientsDocument9 pagesImplementation of An Incremental Deep Learning Model For Survival Prediction of Cardiovascular PatientsIAES IJAINo ratings yet
- Febrianto 2020 IOP Conf. Ser. Mater. Sci. Eng. 771 012031Document7 pagesFebrianto 2020 IOP Conf. Ser. Mater. Sci. Eng. 771 012031Asma ChikhaouiNo ratings yet
- Pediatric Seizure Forecasting Using Nonlinear Features and Gaussian Mixture Hidden Markov Models On Scalp EEG SignalsDocument6 pagesPediatric Seizure Forecasting Using Nonlinear Features and Gaussian Mixture Hidden Markov Models On Scalp EEG SignalsTanvin AyatNo ratings yet
- 1 s2.0 S2666522022000065 MainDocument13 pages1 s2.0 S2666522022000065 Mainamrusankar4No ratings yet
- Fisrt ReviewDocument62 pagesFisrt ReviewramhudiyaNo ratings yet
- Transfer Learning For Ultrasound ImagesDocument10 pagesTransfer Learning For Ultrasound ImagesKoundinya DesirajuNo ratings yet
- Predicting Outcome For Hospitalized Cardiac Patients Using A Combined Neural Network and Rough Set ApproachDocument4 pagesPredicting Outcome For Hospitalized Cardiac Patients Using A Combined Neural Network and Rough Set ApproachBryancito Chumbes LizarragaNo ratings yet
- Ann Clin Transl Neurol - 2017 - Stinear - PREP2 A Biomarker Based Algorithm For Predicting Upper Limb Function AfterDocument10 pagesAnn Clin Transl Neurol - 2017 - Stinear - PREP2 A Biomarker Based Algorithm For Predicting Upper Limb Function Afterginelly quinteroNo ratings yet
- Abe 2022 Oi 220481 1654263485.26457Document11 pagesAbe 2022 Oi 220481 1654263485.26457b4b758h7jhNo ratings yet
- Nuclear PP Diagnosis FaultDocument9 pagesNuclear PP Diagnosis FaultsuderNo ratings yet
- 19999-Article Text (Manuscript) in DOC or DOCX Format-84173-3!10!20230630Document15 pages19999-Article Text (Manuscript) in DOC or DOCX Format-84173-3!10!20230630Khusnun FirdhaNo ratings yet
- Segmentation of Vestibular Schwannoma From MRI, An Open Annotated Dataset and Baseline AlgorithmDocument6 pagesSegmentation of Vestibular Schwannoma From MRI, An Open Annotated Dataset and Baseline AlgorithmIndra PrimaNo ratings yet
- Analysis of Head CT Scans Flagged by Deep Learning Software For Acute Intracranial HemorrhageDocument6 pagesAnalysis of Head CT Scans Flagged by Deep Learning Software For Acute Intracranial HemorrhageAshish MehtaNo ratings yet
- Campen EllaDocument21 pagesCampen EllaWhy BotherNo ratings yet
- Sompawong 2019Document5 pagesSompawong 2019Mahmudur Rahman27No ratings yet
- Expert Systems With Applications: Xiaolong Zhai, Zhanhong Zhou, Chung TinDocument10 pagesExpert Systems With Applications: Xiaolong Zhai, Zhanhong Zhou, Chung Tinpuneet5246No ratings yet
- A Machine Learning System For Automated Whole-Brain Seizure DetectionDocument20 pagesA Machine Learning System For Automated Whole-Brain Seizure DetectionNEHA BHATINo ratings yet
- 10 1016@j Compbiomed 2019 04 017Document11 pages10 1016@j Compbiomed 2019 04 017tomniucNo ratings yet
- Application of Multi Layer Artificial Neural Network in The Diagnosis System: A Systematic ReviewDocument5 pagesApplication of Multi Layer Artificial Neural Network in The Diagnosis System: A Systematic ReviewIAES IJAINo ratings yet
- 1-S2.0-Neural Network Lisboa2002Document29 pages1-S2.0-Neural Network Lisboa2002Vildson BorbaNo ratings yet
- Transfer Learning For ECG ClassificationDocument12 pagesTransfer Learning For ECG ClassificationAbduljabbar Salem Ba-MahelNo ratings yet
- A Pneumonia Detection Method Based On ImprovedDocument6 pagesA Pneumonia Detection Method Based On ImprovedAmílcar CáceresNo ratings yet
- Risk Management of Investment Projects Based On Artificial Neural NetworkDocument13 pagesRisk Management of Investment Projects Based On Artificial Neural NetworkAakash DebnathNo ratings yet
- Wu 2017Document4 pagesWu 2017Vikas KumarNo ratings yet
- CNN-Based Image Analysis For Malaria Diagnosis: Abstract - Malaria Is A Major Global Health Threat. TheDocument4 pagesCNN-Based Image Analysis For Malaria Diagnosis: Abstract - Malaria Is A Major Global Health Threat. TheMiftahul RakaNo ratings yet
- Deep Learning For Automatically Visual Evoked Potential Classification During Surgical Decompression of Sellar Region TumorDocument7 pagesDeep Learning For Automatically Visual Evoked Potential Classification During Surgical Decompression of Sellar Region TumoradityaNo ratings yet
- Article 1Document4 pagesArticle 1Tashu SardaNo ratings yet
- BackprpDocument6 pagesBackprpAnay ChowdharyNo ratings yet
- Chest X-Ray Analysis Using Deep Learning AlgorithmDocument7 pagesChest X-Ray Analysis Using Deep Learning AlgorithmIJRASETPublicationsNo ratings yet
- Application of Neural Networks in Medical Image Processing: Zhenghao Shi, and Lifeng HeDocument4 pagesApplication of Neural Networks in Medical Image Processing: Zhenghao Shi, and Lifeng HeDanielle PerryNo ratings yet
- Automatic Prediction of Diabetic Retinopathy and Glaucoma Through Retinal Image Analysis and Data Mining Techniques PDFDocument4 pagesAutomatic Prediction of Diabetic Retinopathy and Glaucoma Through Retinal Image Analysis and Data Mining Techniques PDFMohammad RofiiNo ratings yet
- AB Report Group 2Document14 pagesAB Report Group 2Abyan HarahapNo ratings yet
- Project PresentationDocument3 pagesProject PresentationGourab PalNo ratings yet
- Artificial Intelligence 1Document8 pagesArtificial Intelligence 1Andy BaiNo ratings yet
- Teja - Technical Seminar PresentationDocument28 pagesTeja - Technical Seminar PresentationArjun P LinekajeNo ratings yet
- Predicting Heart Disease Using Neural NetworksDocument7 pagesPredicting Heart Disease Using Neural NetworksNitya BoyinaNo ratings yet
- Interfacing Bioelectronics and Biomedical SensingFrom EverandInterfacing Bioelectronics and Biomedical SensingHung CaoNo ratings yet
- Myocardial InfarctionDocument6 pagesMyocardial InfarctionDewi Cahya FitriNo ratings yet
- Detection of Myocardial Infarction in 12 Lead ECG Using Support Vector Machine PDFDocument10 pagesDetection of Myocardial Infarction in 12 Lead ECG Using Support Vector Machine PDFDewi Cahya FitriNo ratings yet
- Comparison Between Type-2 and Type-1 Myocardial Infarction: Clinical Features, Treatment Strategies and OutcomesDocument8 pagesComparison Between Type-2 and Type-1 Myocardial Infarction: Clinical Features, Treatment Strategies and OutcomesDewi Cahya FitriNo ratings yet
- BME 301: Biomedical Sensors: Lecture Note 3: Bioelectric Potentials and Biopotential ElectrodesDocument67 pagesBME 301: Biomedical Sensors: Lecture Note 3: Bioelectric Potentials and Biopotential ElectrodesDewi Cahya FitriNo ratings yet
- 3 6Document3 pages3 6Dewi Cahya FitriNo ratings yet
- Discovery Learning Dilaksanakan Dengan Langkah-Langkah: (A)Document6 pagesDiscovery Learning Dilaksanakan Dengan Langkah-Langkah: (A)Dewi Cahya FitriNo ratings yet
- Lecture 14 - Housing For All Mission (PMAY) & Technology Sub-MissionDocument15 pagesLecture 14 - Housing For All Mission (PMAY) & Technology Sub-MissionRadhika KhandelwalNo ratings yet
- C++ Exercises IIDocument4 pagesC++ Exercises IIZaid Al-Ali50% (2)
- Food Composition TableDocument3 pagesFood Composition Tablehafeesadetunji01No ratings yet
- A Comparative Study On Selected Fitness Components of 13-19 Years Female Basketball and Volleyball PlayersDocument11 pagesA Comparative Study On Selected Fitness Components of 13-19 Years Female Basketball and Volleyball PlayersAnonymous CwJeBCAXpNo ratings yet
- Process Oriented Measurements and Improvements - An Analysis of The OFCE-process at Tetra Pak BU DBFDocument5 pagesProcess Oriented Measurements and Improvements - An Analysis of The OFCE-process at Tetra Pak BU DBFĐạt Nguyễn ThànhNo ratings yet
- LLaVA MEDDocument17 pagesLLaVA MED권오민 / 학생 / 전기·정보공학부No ratings yet
- Full Download Retailing Management Levy 9th Edition Solutions Manual PDF Full ChapterDocument36 pagesFull Download Retailing Management Levy 9th Edition Solutions Manual PDF Full Chapterbeastlyfulberj6gkg100% (20)
- System Manuals: EBTS and Integrated Site ControllerDocument3 pagesSystem Manuals: EBTS and Integrated Site ControllerIsac LimaNo ratings yet
- Alywn Cosgrove Real World Fat Loss PDFDocument75 pagesAlywn Cosgrove Real World Fat Loss PDFJM Gym Manticao100% (1)
- Deliverable 5 - Trend Analysis & PresentationDocument6 pagesDeliverable 5 - Trend Analysis & PresentationRamizNo ratings yet
- Show All Work For Credit. Leave All Answers As Simplified FractionsDocument10 pagesShow All Work For Credit. Leave All Answers As Simplified FractionsAliRazaNo ratings yet
- Proposal Nanotechnology in GeotechnicsDocument4 pagesProposal Nanotechnology in GeotechnicsMOHAMED DiriyeNo ratings yet
- KBN Proforma BIWE Welding and Plumbing Materials.Document23 pagesKBN Proforma BIWE Welding and Plumbing Materials.Gilbert KamanziNo ratings yet
- Second Year Mba Syllabus (Only Electives) Third Semester Functional Area: MarketingDocument21 pagesSecond Year Mba Syllabus (Only Electives) Third Semester Functional Area: MarketingSatya ReddyNo ratings yet
- World Islamic Banking Competitiveness Report 2013 - 2014Document84 pagesWorld Islamic Banking Competitiveness Report 2013 - 2014Lena HafizNo ratings yet
- 3D PythagorasDocument4 pages3D Pythagorasraghed alkelaniNo ratings yet
- Location Decisions: Revision AnswersDocument4 pagesLocation Decisions: Revision AnswersZakir HalilovNo ratings yet
- DLL MAPEH7 - 3rd QuarterDocument69 pagesDLL MAPEH7 - 3rd QuarterArah May RobosaNo ratings yet
- Lesson1: Cell, The Basic Unit of LifeDocument4 pagesLesson1: Cell, The Basic Unit of Lifedream kingNo ratings yet
- 07-09-14 EditionDocument28 pages07-09-14 EditionSan Mateo Daily JournalNo ratings yet
- Dumps: Pdfdumps Can Solve All Your It Exam Problems and Broaden Your KnowledgeDocument10 pagesDumps: Pdfdumps Can Solve All Your It Exam Problems and Broaden Your KnowledgeyeddekfiihNo ratings yet
- Astm A307Document6 pagesAstm A307thakrarhits100% (3)
- Trust Bank Account InstructionsDocument5 pagesTrust Bank Account InstructionsGregNo ratings yet
- Tekla StructuresDocument2 pagesTekla StructurescallofdutyondutyNo ratings yet
- CSMI v. TrinityDocument22 pagesCSMI v. TrinityCTV OttawaNo ratings yet
- Adv. Simi Pillay-Van Graan CVDocument14 pagesAdv. Simi Pillay-Van Graan CVDana JonesNo ratings yet
- OCH NH CH CH NH CH CH CH Si OCH OCHDocument2 pagesOCH NH CH CH NH CH CH CH Si OCH OCHPermesh GoelNo ratings yet
- Trading PlanDocument12 pagesTrading Planpeterhash5No ratings yet