Professional Documents
Culture Documents
s9 Basic Life Support
s9 Basic Life Support
Uploaded by
putuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
s9 Basic Life Support
s9 Basic Life Support
Uploaded by
putuCopyright:
Available Formats
Basic Life Support
Standard 9: Recognising and Responding to
Clinical Deterioration in Acute Health Care
Basic Life Support 0
The Victorian Department of Health is making this document freely available on the internet for health
services to use and adapt to meet the National Safety and Quality Health Service Standards of the
Australian Commission on Safety and Quality in Health Care. Each health service is responsible for all
decisions on how to use this document at its health service and for any changes to the document. Health
services need to review this document with respect to the local regulatory framework, processes and
training requirements.
The author disclaims any warranties, whether expressed or implied, including any warranty as to the
quality, accuracy, or suitability of this information for any particular purpose. The author and reviewers
Basic Life Support 1
cannot be held responsible for the continued currency of the information, for any errors or omissions, and
for any consequences arising there from.
Published by Sector Performance, Quality and Rural Health, Victorian Government, Department of Health
June 2014
Acknowledgements
The Department of Health Victoria acknowledges the contribution of medical and health specialists,
Victorian health services, and members of the National Safety and Quality Health Service Standards:
Educational Resources Project project team, Steering Group and Advisory Committee.
The Educational Resources Project Steering Group members comprised:
Associate Professor Leanne Boyd, Steering Group Chair; Director of Education, Cabrini Education
and Research Precinct, Cabrini Health
Ms Madeleine Cosgrave, Project Manager
Ms Susan Biggar, Senior Manager, Consumer Partnerships, Health Issues Centre
Mr. David Brown, Consumer representative
Dr Jason Goh, Medical Administration Registrar - Cabrini Health
Mr Matthew Johnson, Simulation Manager, Cabrini Education and Research Precinct, Cabrini
Health
Ms Tanya Warren, Educator, Cabrini Education and Research Precinct, Cabrini Health
Ms Marg Way, Director, Clinical Governance, Alfred Health
Mr Ben Witham, Senior Policy Officer, Quality and Safety, Department of Health Victoria
The Educational Resources Project Advisory Committee members comprised:
Associate Professor Leanne Boyd, Advisory Committee Chair; Director of Education, Cabrini
Education and Research Precinct, Cabrini Health
Ms Madeleine Cosgrave, Project Manager
Ms Margaret Banks, Senior Program Director, Australian Commission on Safety and Quality in
Health Care
Ms Marrianne Beaty, Oral Health National Standards Advisor, Dental Health Services Victoria)
Ms Susan Biggar, Senior Manager, Consumer Partnerships, Health Issues Centre
Basic Life Support 2
Contents
Mr David Brown, Consumer representative
Dr Jason Goh, Medical Administration Registrar, Cabrini Health
Ms Catherine Harmer, Manager, Consumer Partnerships & Quality Standards, Department of
Health, Victoria
Ms Cindy Hawkins, Director, Monash Innovation and Quality, Monash Health
Ms Karen James, Quality and Safety Manager, Hepburn Health Service
Mr Matthew Johnson, Simulation Manager, Cabrini Health
Ms Annette Penney, Director ,Quality and Risk, Goulburn Valley Health
Ms Gayle Stone, Project Officer, Quality Programs , Commission for Hospital Improvement,
Department of Health Victoria
Ms Deb Sudano, Senior Policy Officer, Quality and Safety, Department of Health Victoria
Ms Tanya Warren, Educator, Cabrini Health
Ms Marg Way, Director, Clinical Governance, Alfred Health
Mr Ben Witham, Senior Policy Officer, Quality and Safety, Department of Health Victoria
Basic Life Support 3
Introduction 3
Learning outcomes 3
National Standards 3
Aim of Standard 9 3
Policies and procedures 3
Background 4
DRS ABCD 4
Automated external defibrillators 7
Basic Life Support 3
BLS in obstetric patients 8
Paediatric BLS 8
Foreign body airway obstruction (FBAO) 9
Your role in basic life support 10
Caring for the patient and carer 11
Caring for staf 11
Education and further resources 11
Reporting adverse events 11
Summary 12
Test Yourself 13
Answers15
References 16
Basic Life Support 4
Basic Life Support
Introduction National Standards
This module relates to The National Safety and The Australian Commission on Safety and Quality
Quality Health Service (NSQHS) Standard 9: in Health Care (ACSQHC) developed the 10 NSQHS
Recognising and Responding to Clinical Standards to reduce the risk of patient harm and
Deterioration in Acute Health Care. improve the quality of health service provision in
Australia. The Standards focus on governance,
consumer involvement and clinically related areas
and provide a nationally consistent statement of
the level of care consumers should be able to
expect from health services.
Aim of Standard 9
The intention of Standard 9: Recognising and
Responding to Clinical Deterioration in Acute
Health Care is to ensure that patient deterioration
is recognised promptly, and that appropriate action
is taken. The Standard builds on The National
Learning outcomes Consensus Statement: Essential elements for
On completion of this module, clinicians will be Recognising and Responding to Clinical
able to: Deterioration (ACSQHC, 2010).
Standard 9 also relates to Standard 1: Governance
1. Identify the indications for basic life support
for Safety and Quality in Health Service
(BLS).
Organisations and Standard 2: Partnering with
2. Describe the appropriate actions for DRS Consumers. The principles in these Standards are
ABCD. fundamental to all Standards and provide a
framework for their implementation.
3. Discuss the considerations needed when
performing basic life support on infants, ACSQHC, 2012
children and pregnant women. Criteria to achieve Standard 9:
4. Describe the management of a foreign body Establishing recognition and response systems
airway obstruction (FBAO).
Organisation wide systems consistent with the National
Consensus Statement are used to support and promote
recognition of, and response to, patients whose condition
deteriorates in an acute health care facility.
Basic Life Support 5
Recognising clinical deterioration and escalating care escalating care.
Patients whose condition is deteriorating are recognised and Table 1: Criteria to meet Standard 9 (ACSQHC, 2012)
appropriate action is taken to escalate care.
Policies and procedures
There are numerous policies, procedures and
resources within health care services to assist you
in basic life support. It is important to access, read
and adhere to systems, policies and procedures
within your organisation.
Background
Responding to clinical deterioration Basic life support (BLS) is the preservation or
restoration of life by the establishment and
maintenance of airway, breathing and circulation
and related emergency care.
This may include the use of an automatic external
defibrillator (AED).
Efective BLS:
Appropriate and timely care is provided to patients whose may increase the likelihood of successful
condition is deteriorating. defibrillation
helps maintain myocardial and cerebral
oxygenation until:
o reversible causes can be diagnosed
and treated
Communicating with patients and families o advanced life support clinicians
and equipment are available
Cardiopulmonary resuscitation (CPR) is the
combination of chest compressions and airway
ventilation to maintain efective basic life support.
Patients, families and carers are informed of recognition and
response systems and can contribute to the process of
Basic Life Support 6
All clinicians, including agency, casual and locum A: AIRWAY
staf, are expected to be trained and proficient in
Inspection
basic life support.
Australian Resuscitation Council (ARC), 2010 The patient’s airway should be inspected for
patency. Any foreign material causing obstruction
should be removed using suction.
DRS ABCD
If suction is unavailable, the clinician may use two
The acronym DRS ABCD is used to remind clinicians
fingers to sweep the patient’s mouth to remove
of the necessary steps to implement basic life
foreign materials which may be blocking the
support.
patient’s airway. Care should be taken when
performing a finger sweep to avoid patient and
D: DANGER clinician harm.
It is important for clinicians to check the
Correctly fitted dentures can maintain the
surrounding area for potential dangers to both the
structure of a patient’s face. This assists in
patient and clinicians.
establishing an adequate seal with a mask during
All clinicians must ensure that appropriate personal resuscitation. Loose dentures should be removed
protective equipment (PPE) such as gloves and as they may prevent an adequate seal and cause
eyewear is in place before commencing basic life airway obstruction.
support.
Maintaining airway patency
R: RESPONSE
The head tilt is used in conjunction with the chin
The clinician must assess the patient’s lift to open the patient’s airway.
responsiveness by using verbal and tactile stimuli.
This should be done by touching the patient and The head tilt involves placing one hand on the
asking for a response. This is referred to as “touch patient’s forehead or the top of their head. The
and talk” and can be done by giving a simple chin lift involves the clinician gently raising, and
command such as “open your eyes or squeeze my supporting, the patient’s chin. This opens the
hand”. patient’s mouth and pulls the tongue and soft
tissues away from the back of the throat.
S: SEND FOR HELP The chin lift is shown in the following picture:
The clinician needs to activate their local
emergency response system to access
help. The clinician should then continue
with assessment and management of
the patient.
Basic Life Support 7
The jaw thrust is shown in the following pictures:
Figure 1: Chin lift (ARC, 2010).
If cervical or thoracic trauma is noted, this
manoeuvre can cause further damage. In this
situation, a jaw thrust should be used to open a
patient’s airway and minimise movement of the
cervical spine.
The clinician must place two fingers behind each
side of the patient’s jaw under the ears and push
the jaw forward to open the airway. The clinician’s
thumbs can then be used to pull the chin down and
open the patient’s mouth.
ARC, 2010
Figure 2: Jaw thrust (European Resuscitation Council, 2010).
B: BREATHING
Once a patent airway is established the clinician
needs to assess whether or not the patient is
breathing. The clinician should:
Basic Life Support 8
LOOK and FEEL for the rise and fall of the
upper abdomen or lower chest
LISTEN and FEEL for the escape of air from
the nose or mouth
The following table outlines the necessary actions
once the patient’s level of consciousness is
determined.
Unresponsive and Unresponsive and not
breathing normally breathing normally
Position the patient on Continue the ABCD
their side in the steps
recovery position
Figure 3: Compression technique (ARC, 2010)
Continue to assess for
improvement or Incorrect technique when performing chest
deterioration compressions may cause regurgitation or damage
to internal organs.
C: COMPRESSIONS
Cardiac compressions are required to maintain Interruptions to chest compressions should be
perfusion to vital organs. The goal is to provide minimised at all times. Compressions should only
compressions that are: be paused to provide breaths, defibrillate or
perform procedures such as endotracheal
efective intubation.
continuous The depth of each chest compression should be
uninterrupted approximately one third of the depth of the chest.
To perform efective compressions, clinicians must The rate of compressions should be approximately
place the heel of one hand on the lower half of the 100 compressions per minute (two per second).
sternum with the other hand on top. This is shown
The ratio of chest compressions to breaths is thirty
in the following picture:
compressions to two breaths (30:2).
This means that after every thirty compressions the
clinician should pause and deliver two breaths.
Compressions are more likely to be efective by:
• placing the patient on a firm flat surface
Basic Life Support 9
• allowing complete recoil of the chest D: DEFIBRILLATION
following each compression Defibrillation is the application of an electrical
• changing the clinician performing chest shock to the heart, aiming to disrupt abnormal
compressions every 2 minutes to lessen electrical activity and restore a normal rhythm.
fatigue There are diferent types of defibrillators. Clinicians
• continuing compressions while the should familiarise themselves with the
defibrillator is being attached and charging defibrillation equipment in their organisation.
• minimising interruptions ARC, 2010
ARC, 2010
To ensure efective breaths are delivered clinicians Automated external defibrillators
should:
There is a strong correlation between early
LOOK for the rise and fall of the upper defibrillation and improved patient survival.
abdomen or lower chest
The use of an automatic external defibrillator (AED)
LISTEN and FEEL for the escape of air from is now considered part of basic life support. These
the nose or mouth machines can correctly identify rhythms which
require defibrillation and prompt the user to safely
Manual resuscitators administer defibrillation.
The use of manual resuscitators is recommended in AEDs must only be used for patients who are
the health care setting. Clinicians should familiarise unresponsive and not breathing normally. CPR
themselves with the manual resuscitation should be continued until the AED is turned on and
equipment in their organisation. the pads are attached.
When using a manual resuscitator it is important The clinician should then follow the AED prompts.
that the mask is applied correctly to create an
airtight seal. This can be done by holding the mask All clinicians must follow organisational policies
firmly against the patient’s face whilst maintaining and procedures in relation to the use of AEDs.
an open airway (head tilt, chin lift).
PAD PLACEMENT
The rise and fall of a patient’s chest during
ventilations will indicate an efective seal. Pads should be placed on the patient’s exposed
chest in an anterior – lateral position. Pad to skin
ARC, 2010
contact is important for efective defibrillation.
Clinicians should ensure:
• the skin is clean and dry.
Basic Life Support 10
• the pad placement areas are shaved if AED SAFETY
required Prior to defibrillation, clinicians must check the
• the pad is pressed down firmly surrounding area to ensure the safety of the
patient and all staf.
Pads should not be placed over ECG electrodes,
ECG leads, medication patches, implanted devices While the AED is being used, it is important that
(such as a pacemakers or AICDs) or a central line the patient and all staf do not come into contact
insertion site. with hazards such as water, metal fixtures, oxygen
and flammable substances.
The clinician pressing the shock button needs to
request all present to “stand clear” and ensure
compliance.
ARC 2010
Figure 4: Pad placement (ARC, 2010)
The operator should then: Failure to defibrillate
• connect the pads to the AED cable If the defibrillator fails to deliver a shock:
• turn the AED on and follow the prompts • recommence CPR
It is important to minimise delays in initiating
• check pad placement and skin contact
shock delivery.
• ensure a secure connection between the pads
CPR should be immediately resumed following the
and the AED device
delivery of the shock for a further two minute cycle
before initiating further defibrillation.
Basic Life Support 11
• consider changing the pads • with a pillow or towel under the right
ARC, 2010 buttock to tilt her pelvis to the left by 30°
This can relieve pressure on the inferior vena cava,
BLS in obstetric patients resulting in improved venous return.
ARC, 2011
The principles of basic life support apply for
pregnant women. There are physiological changes
during pregnancy which require consideration.
Emergency caesarean
PHYSIOLOGICAL CHANGES DURING PREGNANCY Efective resuscitation of the pregnant woman is
The physiological changes which occur in the best way to optimise survival for both her and
pregnancy include: the foetus.
• increased circulating blood volume and An emergency caesarean may be considered if
cardiac output initial resuscitation eforts are inefective.
increased oxygen consumption to meet the ARC, 2011
needs of both mother and the foetus
reduced lung volumes due to pressure Paediatric BLS
from the enlarged uterus and abdominal The principles of basic life support apply for infants
organs and children. There are physiological diferences
between adults and children which require
CONSIDERATIONS consideration during resuscitation.
These and other physical changes increase the risk
of hypoxia, aspiration and hypotension. PAEDIATRIC CLASSIFICATIONS
From 20 weeks gestation, the pregnant woman’s Newborn First few hours of life
uterus can cause compression on the major
abdominal veins when she is lying on her back. Neonate First 28 days of life
This compression reduces venous return, cardiac
Infant Less than one year of age
output and blood pressure.
During BLS, the pregnant woman should be Younger Child 1 - 8 years of age inclusive
positioned:
Older Child 9 - 14 years of age inclusive
• on her back
• keeping her shoulders flat
Basic Life Support 12
PHYSIOLOGICAL DIFFERENCES AND Compressions
CONSIDERATIONS The compression point for all age groups is the
Airway lower half of the sternum or centre of the chest.
The same rate and depth of compressions used in
The upper airway in infants is easily obstructed adult basic life support apply for infants and
because of narrow airway passages. The tissues of children. The ratio for paediatric patients is fifteen
the trachea and neck are softer and more pliable compressions to 2 breaths (15:2).
and can therefore be harmed by excessive head
tilt. Infants
Infants should be kept in a neutral position during Compression for infants may be performed using
BLS, with the lower jaw supported at the chin. either of the following techniques.
There should be no pressure on the neck. Very • two finger technique, which is performed by
slight head tilt can be used if the neutral position placing two fingers on the compression point
does not open the airway. This is referred to as the
‘sniffing position’. • encircling technique, which is performed by
encircling the infant with thumbs in the
Children and infants have a softer palate than centre of the chest
adults. They are also more likely to bite.
Children
Therefore, whilst the finger sweep is efective for
removing foreign materials causing airway A one or two hand technique can be used for
obstruction, care should be taken. Low pressure performing chest compressions in children.
suction can be used to remove foreign materials
causing airway obstruction. It is important to Defibrillation
ensure that the nostrils are clear.
Breathing
It is important to select an appropriately sized
mask when using a manual resuscitator. The
correctly sized facemask should extend from the
bridge of the nose to halfway between the lower
lip and the point of the chin.
The mask should be held firmly on the infant or
child’s face with the thumb and index finger. The
degree of head tilt should be consistent with the
age and size of the child.
Basic Life Support 13
An AED on adult settings should not routinely be sharp back blows to attempt to dislodge the
used for children under 8 years of age or less than foreign object.
25kg in weight.
Back blows should be performed using the heel of
An AED with paediatric capability and pads should one hand, in the middle of the back between the
be used. It is important to ensure that the pads are shoulder blades.
not in contact with each other.
The clinician should check after each blow to see if
If a paediatric AED is unavailable, the adult the airway obstruction has been relieved. The aim
defibrillator may be used on the manual setting. is to relieve the obstruction with the least number
of back blows.
Foreign body airway obstruction If the back blows are unsuccessful, the clinician
(FBAO) should then perform up to 5 chest thrusts.
A foreign body airway obstruction (FBAO) is a life- To perform chest thrusts, identify the same
threatening emergency. The simplest way to assess compression point as for chest compressions.
severity of a FBAO is to assess for an efective Chest thrusts are similar to compressions but are
cough. sharper and delivered at a slower rate.
The clinician should send for emergency medical The clinician should check between each chest
assistance if they are unable to relieve the thrust to see if the airway obstruction has been
obstruction or if the patient becomes unconscious. relieved.
If the obstruction is still not relieved the clinician
EFFECTIVE COUGH (MILD AIRWAY OBSTRUCTION) should continue to alternate 5 back blows with 5
If the patient has an efective cough, they should chest thrusts, whilst waiting for emergency
be encouraged to keep coughing to expel the assistance.
foreign body.
If the obstruction is not relieved seek urgent
medical assistance.
INEFFECTIVE COUGH (SEVERE AIRWAY
OBSTRUCTION)
Conscious patients
If the patient does not have an efective cough but
is still conscious, the clinician should perform five
Basic Life Support 14
Adults and children should be treated in a sitting or family and carers and for other patient’s in the
standing position. Infants should be positioned on area.
the clinician’s lap with their head lower than their
body. They should be placed face down for back Respecting patient’s choices
blows and face up for chest thrusts.
It is important to be aware of, and respect,
patient’s choices regarding resuscitation such as
Unconscious patients treatment limiting and not for resuscitation orders.
Basic life support should be commenced on
unconscious patients. Communication and teamwork
If there is visible foreign material obstructing the There is potential for resuscitation attempts to be
patient’s airway suction, or a finger sweep, can be disorganised and chaotic. All clinicians should be
used to clear the airway. mindful of their communication and teamwork.
ARC, 2010
Efective communication is important to ensure
that critical information is shared during
Your role in basic life support resuscitation, as errors can occur as a result of poor
or inefective communication.
All staf have a responsibility to provide timely and
efective basic life support. A capable clinician should be nominated to lead
the resuscitation and ensure that all staf are aware
Clinicians who are familiar with the patient have an of their delegated roles. For example, the person
important role in informing the emergency team who retrieves the resuscitation trolley may be
about: responsible for applying the pads and using the
• the patient’s medical history AED.
• presenting problems
• precipitating factors that led to the cardiac
arrest
The emergency team may require assistance with:
• chest compressions
• scribing and documentation
• obtaining required equipment and drugs
It is also important that clinicians consider
providing emotional support for the patient’s
Basic Life Support 15
It is important to notify the treating doctor as soon having these conversations that clinicians
as possible, if they are not in attendance. understand and take into account the patient’s
desire for information.
Documentation
In all circumstances, families and carers must be
Complete and accurate documentation should informed as soon as possible of what has
occur throughout resuscitation by a designated happened and the outcome.
clinician.
Other patients who may have witnessed or were
aware of the resuscitation should be ofered
support.
Restocking
Clinicians should be aware of the process to
Caring for staf
restock equipment, drugs and the resuscitation Staf should be provided with the opportunity to
trolley. debrief following any resuscitation, whether
successful or not.
Caring for the patient and carer Resuscitation can be extremely challenging and
CPR should be continued until: confronting for all staf, particularly if the outcome
is poor.
• the patient responds or begins to breathe
normally It is important that anyone involved should be
ofered the chance to debrief. During this debrief
• a doctor directs that CPR be ceased session, staf should be given opportunity to
• it is impossible for clinicians to continue discuss their thoughts and feelings about the
due to exhaustion event.
ARC, 2010
After the return of spontaneous circulation, it is
essential to continue maintenance of airway,
breathing and circulation until the patient is stable.
A full explanation should be given to the patient if
and when they are able. This conversation should
occur between the patient and a clinician who has
an understanding of what has occurred.
Conversations with patients and carers should be
tailored to meet their needs. It is important when
Basic Life Support 16
Summary
Debriefing is not about blaming individuals but policy, protocol and equipment improvements and
about discussing the situation and exploring what, education and training activities.
if anything could be done better next. ACSQHC, 2012
It is important for all staf to support each other
and be sensitive to colleagues who may not be Basic life support is an important aspect of
coping well. Standard 9 in the National Safety and Quality
Resuscitation events can be used as a learning tool. Health Service Standards.
All staf should be informed about any learning
outcomes, including what worked well and any The key messages are:
opportunities for improvement. 1. Basic life support (BLS) is the preservation
or restoration of life by the establishment
Education and further resources and maintenance of airway, breathing and
circulation and related emergency care.
The Australia Resuscitation Council website
provides further information and guidelines 2. Cardiopulmonary resuscitation (CPR) is the
regarding basic life support. combination of chest compressions and
airway ventilation to maintain efective
These can be accessed at: basic life support.
www.resus.org.au 3. All clinicians, including agency, casual and
locum staf, are expected to be trained and
Reporting adverse events proficient in basic life support.
All adverse events relating to poor or absent basic 4. The acronym DRS ABCD is used to remind
life support should be reported to the clinicians of the necessary steps to
nurse/midwife in charge, the attending medical implement basic life support.
officer (if necessary) and be documented in the
clinical record.
They should also be reported in your organisation’s
risk or incident management system.
Patients and carers should be fully informed of any
adverse events and the organisation’s open
disclosure processes implemented.
Information trends can then be used to inform
quality improvement activities such as system,
Basic Life Support 17
D: Danger - It is important for clinicians 6. A foreign body airway obstruction (FBAO)
to check the surrounding area for is a life-threatening emergency.
potential dangers to both the patient and
clinicians. 7. It is important to be aware of, and respect,
patient’s choices regarding resuscitation
R: Response - The clinician must assess such as treatment limiting and not for
the patient’s responsiveness by using resuscitation orders.
verbal and tactile stimuli.
8. A full explanation should be given to the
S: Send for help – Clinicians must patient if and when they are able. Carers
activate their local emergency response must be informed as soon as possible of
system to access help. what has happened and the outcome.
A: Airway - the patient’s airway should
9. All adverse events relating to poor or
be inspected for patency. Any foreign
absent basic life support should be
material causing obstruction should be
reported in your organisation’s risk or
removed using suction.
incident management system.
B: Breathing - the clinician needs to
assess whether or not the patient is 10. Staf should be provided with the
breathing. opportunity to debrief following any
resuscitation, whether successful or not.
C: Compressions - cardiac compressions
are required to maintain perfusion to
vital organs. The goal is to provide
compressions that are efective,
continuous and uninterrupted.
D: Defibrillation - Defibrillation is the
application of an electrical shock to the
heart, aiming to disrupt abnormal
electrical activity and restore a normal
rhythm.
5. There are physiological changes which
require consideration when applying the
principles of basic life support for pregnant
women, infants and children.
Basic Life Support 18
Test Yourself
For each of the following multiple-choice questions select the most appropriate answer.
1. Basic life support is started when the patient is:
a) silent and cyanosed
b) unresponsive and not breathing normally
c) unresponsive but breathing normally
d) responsive but not breathing normally
2. The initial step when approaching a collapsed patient is to:
a) turn the patient on their side
b) call out their name
c) start chest compressions
d) check for danger
3. After an unconscious adult’s airway is cleared and opened, the clinician should next check for
breathing. If the patient is breathing abnormally or breaths are absent, the rescuer should:
a) give 5 initial breaths allowing about 1 second per breath
b) give 1 initial breath allowing about 1 second per breath
c) start chest compressions at 100 compressions per minute
d) give 2 initial breaths allowing about 1 second per breath
Basic Life Support 19
4. The compression to ventilation ratio for adults is:
a) 30:2 b) 3:1
c) 15:2 d) 25:1
5. The first step in airway is to:
a) perform the head tilt/chin lift
b) open the mouth and turn the head slightly downwards, to allow for drainage by gravity
c) inspect the patient’s airway for any foreign material and remove if confident
d) deliver 2 rescue breaths
6. The compression ventilation ratio for paediatric patients in all hospital areas is:
a) 30:2 b) 15:1
d) 15:2 d) 3:1
7. In all age groups, the site and depth of compressions is best described as:
a) site: the upper chest & depth: 1/3 of the chest
b) site: the centre of the chest & depth: 1/3 of chest
Basic Life Support 20
c) site: abdominal region & depth: 5 cms in depth
d) site: whatever you can reach & depth: whatever you can reach
8. When performing chest compressions on a 6 month old, the compression technique used is
a) the heel of one hand
b) 2 thumbs
c) 2 fingers
d) B or C
5. When opening the airway, which age group is kept in the neutral position?
a) adults
b) children
c) infants
d) all of the above
10. Conversations explaining what has happened should be tailored to meet the needs of the patient or
carers. It is important when having these conversations that clinicians:
a) give a full and detailed explaination of the steps invovled
b) understand and take into account the patient or carer’s desire for information
Basic Life Support 21
c) give minimal information
d) wait to be asked for information
Basic Life Support 22
Answers
1. b) unresponsive and not breathing normally
2. d) check for danger
3. b) start chest compressions at 100 compressions per minute
4. a) 30:2
5. c) inspect the patient’s airway for any foreign material and remove if confident
6. d) 15:2
7. b) Site: the centre of the chest & depth: 1/3 of chest
8. d) B or C
9. c) infants
10. b) understand and take into account the patient or carer’s desire for information
Basic Life Support 23
References
Australian Resuscitation Council (2010) Guideline 2: Managing an Emergency. Available at
www.resus.org.au
Australian Resuscitation Council (2010) Guideline 3: Recognition and First Aid Management of the
Unconscious Victim. Available at www.resus.org.au
Australian Resuscitation Council (2010) Guideline 4: Airway. Available at www.resus.org.au
Australian Resuscitation Council (2010) Guideline 5: Breathing. Available at www.resus.org.au
Australian Resuscitation Council (2010) Guideline 6: Compressions. Available at www.resus.org.au
Australian Resuscitation Council (2010) Guideline 7: External Automated Defibrillation in Basic Life Support.
Available at www.resus.org.au
Australian Resuscitation Council (2010) Guideline 8: Cardiopulmonary resuscitation. Available at
www.resus.org.au
Australian Resuscitation Council (2010) Section 10: Education and Implementation. Available at
www.resus.org.au
Australian Resuscitation Council (2010) Guideline 11.7: Post-Resuscitation Therapy in Adult Advanced Life
Support. Available at www.resus.org.au
Australian Resuscitation Council (2010) Guideline 11.10: Resuscitation in Special Circumstances. Available
at www.resus.org.au
Australian Resuscitation Council (2010) Section 12: Paediatric Advanced Life Support. Available at
www.resus.org.au
Australian Resuscitation Council (2010) Section 13: Neonatal Guidelines. Available at www.resus.org.au
Basic Life Support 24
Basic Life Support 25
Basic Life Support 26
You might also like
- Draft SOPs For Hospital - ManagementDocument362 pagesDraft SOPs For Hospital - ManagementAnonymous 9qKa3495% (20)
- CCPC 3rd Edition STANDARDS ONLY PDFDocument18 pagesCCPC 3rd Edition STANDARDS ONLY PDFsrngm100% (1)
- Postoperative Management in AdultsDocument58 pagesPostoperative Management in AdultsAjay KumarNo ratings yet
- 1melnyk Ebp Igniting A Spirit of InquiryDocument4 pages1melnyk Ebp Igniting A Spirit of Inquiryapi-272725467No ratings yet
- The Ultimate Guide To Anxiety DisordersDocument66 pagesThe Ultimate Guide To Anxiety Disordersnajaxx100% (2)
- Joint Mobilization Techniques For Sacroiliac Joint DysfunctionDocument17 pagesJoint Mobilization Techniques For Sacroiliac Joint Dysfunctiongaby_spy100% (3)
- s6 Clinical HandoverDocument26 pagess6 Clinical HandoverirenediahjNo ratings yet
- S3 Aseptic TechniqueDocument19 pagesS3 Aseptic TechniqueChristian Angelo LeonorNo ratings yet
- QA PAFP Journal July December 59-2-2021 Pages 115 126Document12 pagesQA PAFP Journal July December 59-2-2021 Pages 115 126Norjetalexis Maningo CabreraNo ratings yet
- NSQHS Standards Fact Sheet Standard 1Document2 pagesNSQHS Standards Fact Sheet Standard 1Annette LowryNo ratings yet
- National Model Clinical Governance FrameworkDocument44 pagesNational Model Clinical Governance Frameworkwenhal100% (1)
- NSQHS Standards Fact Sheet Standard 4Document2 pagesNSQHS Standards Fact Sheet Standard 4Annette LowryNo ratings yet
- Das (2018) Universal Delivery of HealthcareDocument5 pagesDas (2018) Universal Delivery of HealthcareWaqasRabbaniNo ratings yet
- NSQHS Standards Fact Sheet Standard 2Document2 pagesNSQHS Standards Fact Sheet Standard 2Annette LowryNo ratings yet
- Au Ca1 - DLP - 01 - Dexel Lorren R. Valdez - Pasay 2023 - 2024Document2 pagesAu Ca1 - DLP - 01 - Dexel Lorren R. Valdez - Pasay 2023 - 2024Dexel Lorren ValdezNo ratings yet
- Barwon Health HMO PositionDocument7 pagesBarwon Health HMO Positionz9skylaNo ratings yet
- JCIDocument54 pagesJCIanaskamel82No ratings yet
- IACSD 2020 GuidelinesDocument122 pagesIACSD 2020 GuidelinesRicardo Del NiroNo ratings yet
- NSQHS Standards Fact Sheet Standard 6Document2 pagesNSQHS Standards Fact Sheet Standard 6Annette LowryNo ratings yet
- Dental Accreditation StandardsDocument66 pagesDental Accreditation Standardsdhir.ankurNo ratings yet
- National Safety and Quality Health Service Standards Second EditionDocument86 pagesNational Safety and Quality Health Service Standards Second EditionMRS FKM UHNo ratings yet
- National Safety and Quality Health Service Nsqhs Standards Second Edition - Updated May 2021Document92 pagesNational Safety and Quality Health Service Nsqhs Standards Second Edition - Updated May 2021Junk YardNo ratings yet
- Home Health Care Medical Standards: An OverviewDocument108 pagesHome Health Care Medical Standards: An OverviewSouheil DamajNo ratings yet
- SOP-10-008 Suction July 20 2010 PDFDocument23 pagesSOP-10-008 Suction July 20 2010 PDFSalsabilla KimikoNo ratings yet
- AKIN OTIKO B O Quality Nursing Care in NigeriaThe Ideals Realities and ImplicationsDocument19 pagesAKIN OTIKO B O Quality Nursing Care in NigeriaThe Ideals Realities and ImplicationsUmar Farouq Mohammed GalibNo ratings yet
- A 2020 Vision of Patient CenteredDocument13 pagesA 2020 Vision of Patient CenteredElya Amaliia100% (1)
- NSQHS Preventing and Controlling InfectionDocument2 pagesNSQHS Preventing and Controlling InfectionChloé Jane HilarioNo ratings yet
- 2013 Quality Health RecordsDocument36 pages2013 Quality Health RecordsBanin AbadiNo ratings yet
- GSK Public Policy Brief - QualityDocument2 pagesGSK Public Policy Brief - QualityAnna HerreraNo ratings yet
- Field Guide To Antibiotic StewardshipDocument30 pagesField Guide To Antibiotic StewardshipHosam GomaaNo ratings yet
- Consumer Fact Sheet 1: Introduction To The National Safety and Quality Health Service (NSQHS) Standards (Second Edition)Document3 pagesConsumer Fact Sheet 1: Introduction To The National Safety and Quality Health Service (NSQHS) Standards (Second Edition)rakeshkaydalwarNo ratings yet
- Jurnal PPMDocument13 pagesJurnal PPMVeren Magdalena OehlersNo ratings yet
- Medication Safety AustraliaDocument4 pagesMedication Safety AustraliaHijab Syar'i TerbaruNo ratings yet
- Woolf. 1999. Potential Benefits, Limitations, and Harms of Clinical GuidelinesDocument4 pagesWoolf. 1999. Potential Benefits, Limitations, and Harms of Clinical Guidelinestonghieu96No ratings yet
- MKGM PENJAMIN MUTU RS TIPE A - KLMPK 1 - FixDocument23 pagesMKGM PENJAMIN MUTU RS TIPE A - KLMPK 1 - FixNabila Firly Assyafia NurfayzaNo ratings yet
- Standardization of HealthcareDocument6 pagesStandardization of Healthcareita.harsh2030No ratings yet
- Bfcr182 Safe SedationDocument34 pagesBfcr182 Safe SedationMirza BaigNo ratings yet
- Food Hygiene PolicyDocument42 pagesFood Hygiene PolicyNani Hardianti100% (2)
- 10 1002@aorn 12722Document10 pages10 1002@aorn 12722Francisco NenteNo ratings yet
- 1 Community Health NursingDocument10 pages1 Community Health NursingSamantha Bernardo UndaNo ratings yet
- Optometry Code of ConductDocument14 pagesOptometry Code of ConductHarpreetNo ratings yet
- Key Points For Considering Adoption of The Who Labour Care Guide: Policy BriefDocument12 pagesKey Points For Considering Adoption of The Who Labour Care Guide: Policy BriefYuli AstutiNo ratings yet
- HealthandWellBeingofMedicalStaffandPhysicians in TrainingPolicy8.11Document8 pagesHealthandWellBeingofMedicalStaffandPhysicians in TrainingPolicy8.11Dani GintingNo ratings yet
- Hypo FPX 4020 Assessment 3Document14 pagesHypo FPX 4020 Assessment 3Sheela malhiNo ratings yet
- National GuidelineDocument110 pagesNational Guidelineanitn2020No ratings yet
- BACPR Standards and Core Components 2023Document31 pagesBACPR Standards and Core Components 2023ganesh goreNo ratings yet
- HAAD-Policy Scope of Practice For Practical Nurse PDFDocument4 pagesHAAD-Policy Scope of Practice For Practical Nurse PDFmyangel_peach3305No ratings yet
- Health Expectations - 2014 - Greenfield - Analysing Big Picture Policy Reform Mechanisms The Australian Health ServiceDocument13 pagesHealth Expectations - 2014 - Greenfield - Analysing Big Picture Policy Reform Mechanisms The Australian Health ServiceHellen MunetsiNo ratings yet
- A. Who: 1. Millennium Development Goals (MDGS)Document8 pagesA. Who: 1. Millennium Development Goals (MDGS)AmethystNo ratings yet
- NSWH RequisitionPD REQ320807Document4 pagesNSWH RequisitionPD REQ320807dr.nirmanneopaneNo ratings yet
- BMC Pregnancy and Childbirth: Criteria For Clinical Audit of Women Friendly Care and Providers' Perception in MalawiDocument9 pagesBMC Pregnancy and Childbirth: Criteria For Clinical Audit of Women Friendly Care and Providers' Perception in MalawiAz-Zahraa NaasNo ratings yet
- NSWH RequisitionPD CAM16936Document8 pagesNSWH RequisitionPD CAM16936ddddNo ratings yet
- Diabetes GuidelinesDocument29 pagesDiabetes GuidelinesFabiola NogaNo ratings yet
- NSWH RequisitionPD CAM16936Document8 pagesNSWH RequisitionPD CAM16936dddd100% (1)
- Competency AppraisalDocument131 pagesCompetency AppraisalGregory Litang100% (1)
- CHAPTER 7 - Value of Medical Lab Science PersonnelDocument8 pagesCHAPTER 7 - Value of Medical Lab Science PersonnelHannahjoy anainNo ratings yet
- Registered Nurse-Leading Self-2022 PDFDocument6 pagesRegistered Nurse-Leading Self-2022 PDFRoshini JayasundaraNo ratings yet
- Position Description: Medical Education and Training/ Junior Medical Workforce ManagerDocument8 pagesPosition Description: Medical Education and Training/ Junior Medical Workforce ManagerkdwsiwkNo ratings yet
- NSQHS Standards Sept2011Document80 pagesNSQHS Standards Sept2011Poonam Anala YeldandiNo ratings yet
- Health Care Delivery System (Reviewer)Document7 pagesHealth Care Delivery System (Reviewer)James Lord GalangNo ratings yet
- 5th Edition Hospital STD April 2020Document153 pages5th Edition Hospital STD April 2020Archana GaonkarNo ratings yet
- Early Cancer Detection in Primary Care: Are You Aware of New Blood-Based Multi-Cancer Screening ToolsFrom EverandEarly Cancer Detection in Primary Care: Are You Aware of New Blood-Based Multi-Cancer Screening ToolsNo ratings yet
- A Clinician’s Guide to HCV Treatment in the Primary Care Setting: A Multimedia eHealth Source™ Educational InitiativeFrom EverandA Clinician’s Guide to HCV Treatment in the Primary Care Setting: A Multimedia eHealth Source™ Educational InitiativeNo ratings yet
- Jebsens Maritime V RapizDocument6 pagesJebsens Maritime V RapizJoannalyn Libo-onNo ratings yet
- Grad 1516 PDFDocument435 pagesGrad 1516 PDFnitinfutaneNo ratings yet
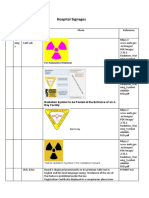
- SignagesDocument4 pagesSignagesRahul NegiNo ratings yet
- ImpressionDocument7 pagesImpressionAnnisa Nur AmalaNo ratings yet
- CHAP 2.docx Anesthesia Services CPT CODES 00000-09999 FOR National Correct Coding Initiative Policy Manual For Medicaid ServicesDocument14 pagesCHAP 2.docx Anesthesia Services CPT CODES 00000-09999 FOR National Correct Coding Initiative Policy Manual For Medicaid ServicesPravin Singh ChauhanNo ratings yet
- Medical Gases CalculationsDocument14 pagesMedical Gases CalculationsNghiaNo ratings yet
- ChokingDocument2 pagesChokingdrfidelenriqueNo ratings yet
- Case Analysis: American WellDocument2 pagesCase Analysis: American WellTatsat PandeyNo ratings yet
- UIC GowningDocument4 pagesUIC GowningBoy WithacoinNo ratings yet
- Students With Mental Health Problems - A Growing Problem.Document6 pagesStudents With Mental Health Problems - A Growing Problem.Lina SantosNo ratings yet
- Systemic Lupus Erythematosus (SLE)Document13 pagesSystemic Lupus Erythematosus (SLE)Kathrina IoannouNo ratings yet
- Asperger SyndromeDocument12 pagesAsperger Syndromeapi-301088340No ratings yet
- Ectopic PregnancyDocument52 pagesEctopic Pregnancybhakta100% (2)
- Anabolic PDFDocument21 pagesAnabolic PDFNe MiNo ratings yet
- Parkinson'S Diseases (PD) : by Dr. Rommanah Azmi PM 013/09Document17 pagesParkinson'S Diseases (PD) : by Dr. Rommanah Azmi PM 013/09Rommanah AzmiNo ratings yet
- Debeb, Simachew Gidey, Et Al. 2021Document13 pagesDebeb, Simachew Gidey, Et Al. 2021priya panaleNo ratings yet
- Anisometropia 4Document18 pagesAnisometropia 4Mamtha MMNo ratings yet
- Dimeglio 2012Document12 pagesDimeglio 2012Tantia Dewi HariantoNo ratings yet
- Outcomes of Crowding in Emergency Departments A SyDocument10 pagesOutcomes of Crowding in Emergency Departments A SyPatricio Marcos CasazzaNo ratings yet
- Patient Guide To Acl Injuries: What Is The Anterior Cruciate Ligament (ACL) ?Document8 pagesPatient Guide To Acl Injuries: What Is The Anterior Cruciate Ligament (ACL) ?Subbu MNo ratings yet
- Herbal CosmeticsDocument18 pagesHerbal Cosmeticstanushara0No ratings yet
- The Use of Pycnogenol in The Treatment of Melasma: Original ArticlesDocument5 pagesThe Use of Pycnogenol in The Treatment of Melasma: Original Articlesfreitasjonashenrique100% (1)
- SucroseDocument2 pagesSucroseMukesh StayzFlyNo ratings yet
- Flag Medicines - Inventory 04-Apr-2023Document30 pagesFlag Medicines - Inventory 04-Apr-2023Luis Alfredo Dominguez MoralesNo ratings yet
- AOS ERP Generic FlowchartDocument4 pagesAOS ERP Generic FlowchartRidha JuliyantiNo ratings yet
- Trauma Pedis S 92 Trauma Pelvis S 35Document2 pagesTrauma Pedis S 92 Trauma Pelvis S 351qwerty2asdfghNo ratings yet
- Sistema EcosterylDocument31 pagesSistema EcosterylAnonymous vC6IBqhtCuNo ratings yet