Professional Documents
Culture Documents
Emergency Department Procedural Sedation and Analgesia Physician Checklist
Emergency Department Procedural Sedation and Analgesia Physician Checklist
Uploaded by
calstudyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency Department Procedural Sedation and Analgesia Physician Checklist
Emergency Department Procedural Sedation and Analgesia Physician Checklist
Uploaded by
calstudyCopyright:
Available Formats
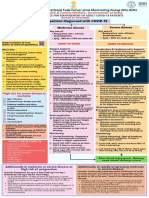
Emergency Department
Procedural Sedation and Analgesia [patient label]
Physician Checklist
Pre-Procedure Assessment
☐ Past medical history (note history of OSA) ________________________________________________________
☐ Prior problems with sedation/anesthesia __________________________________________________________
☐ Allergies to food or medications ________________________________________________________________
☐ Procedure _________________________________________________________________________________
☐ Dentures none / upper / lower [should remain in during PSA unless intubation required]
☐ Cardiorespiratory reserve no or mild impairment / moderate impairment / significant impairment
☐ Difficult airway features none / mild concern / significant concern
☐ Last oral intake (see fasting grid on reverse) _____________ ☐ Will delay procedure until _________
☐ Weight (kg) ________ ☐ Benefits of proceeding with PSA exceed risks
Difficult Airway Features
Difficult Laryngoscopy: Look externally, Evaluate 3-3-2 rule, Mallampati score, Obstruction, Neck Mobility
Difficult BVM Ventllation: Beard, Obese, No teeth, Elderly, Sleep Apnea / Snoring
Difficult LMA: Restricted mouth opening, Obstruction, Distorted airway, Stiff lungs or c-spine
Difficult Cricothyroidotomy: Surgery, Hematoma, Obesity, Radiation distortion or other deformity, Tumor*
☐ Is this patient a good candidate for ED procedural sedation and analgesia?
The less cardiorespiratory reserve, the more difficult airway features, and the less procedural urgency, the more likely the patient
should not receive PSA in the emergency department. If not a good candidate for ED-based PSA, other options include regional or local
anesthetic; PSA or GA in the operating room; or endotracheal intubation in the ED.
Pre-procedure Preparation Airway Equipment
☐ Analgesia - maximal patient comfort prior to PSA ☐ Ambu bag connected to oxygen
☐ Informed consent for PSA and procedure ☐ Laryngoscopy handles and blades
☐ Patient on monitor: telemetry, NIBP, SpO2, EtCO2 ☐ Suction, oral & nasal airways
☐ Oxygenate with NC O2 and high flow face mask O2 ☐ Endotracheal tubes & stylets
☐ Select and draw up PSA agent(s) ☐ LMA with lubricant and syringe
☐ Reversal agents and paralytic vials at bedside ☐ Colorimetric capnometer
☐ Prepare for endotracheal intubation ☐ Bougie & difficult airway equipment
Agent Dose* Contraindications Comments
Propofol 0.5-1 mg/kg IV, then 0.5 mg/ Egg or soy allergy Preferred for shorter procedures and where muscle
kg q1-2 min prn relaxation is of benefit; avoid if hypotension is a
concern
Ketamine 1-2 mg/kg IV over 30-60 sec Absolute: age < 3 months, schizophrenia Preferred for longer procedures; avoid if hypertension/
or 4-5 mg/kg IM, repeat half Relative: major posterior oropharynx procedures; history of tachycardia is a concern; have midazolam available to
dose prn airway instability, tracheal surgery, or tracheal stenosis; manage emergence distress; muscle tone is preserved
active pulmonary infection or disease; cardiovascular or increased; post-procedure emesis may be mitigated
disease; CNS masses, abnormalities, or hydrocephalus by prophylactic ondansetron
Etomidate 0.1-0.15 mg/kg IV, then 0.05 Intra-procedure myoclonus or hypertonicity, as well as
mg/kg q2-3 min prn post-procedure emesis, are common
Fentanyl 1-2 mcg/kg IV, then 1 mcg/ Comparatively delayed onset of action; do not re-dose
kg q3-5 min prn too quickly
Midazolam .05 mg/kg IV, then .05 mg/kg Pregnancy, allergy to benzyl alcohol Comparatively delayed onset of action; do not re-dose
q3-5 min prn too quickly
Pentobarbital 1 mg/kg IV, then 1 mg/kg Pregnancy, porphyria Use for painless procedures where analgesia is not
q3-5 min prn needed
Reversal Agent Dose Caution
Naloxone 0.01-0.1 mg/kg IV or IM (typical adult dose 0.4 mg), max 2 mg
Flumazenil 0.01 mg/kg IV (typical adult dose 0.2 mg ) over 20 seconds, max 1 mg Only use in benzodiazepine naïve patient
*All doses should be reduced in the elderly and in patients with marginal hemodynamics R. Strayer / P. Andrus emupdates.com 11.28.2013
Emergency Department PSA Checklist (page 2)
[patient label]
Detect hypoventilation early
Stop the drugs
Position the patient
Jaw thrust
Suction if needed
Laryngospasm notch pressure
PSA Intervention Sequence Nasal airways
• Proceed down intervention sequence as slowly as patient condition permits
Consider reversal agents
• Jaw thrust as illustrated above - thumbs on maxilla, four fingers posterior to ramus Bag mask or LMA ventilation
• Laryngospasm notch is behind the earlobe, between mastoid process and Oral airway, ventilation
condyle of mandible – bilateral, firm pressure medially and cephalad (up and in) Intubate
• If rescue ventilation is required, bag slowly and gently
• see emupdates.com/psa for details
Post-procedure Assessment
☐ Adverse events none / hypoxia (< 90%) / aspiration / hypotension / agitation / other: ____________________________________
☐ Interventions taken none / bag valve mask / LMA / ETT / reversal agent / hypotension Rx / admission for PSA / other: _____________
☐ Adequacy of PSA nondistressed / mild distress / severe distress
☐ Procedure successful / unsuccessful
☐ MD or RN at bedside until patient responds to voice
☐ Telemetry, EtCO2, SpO2 monitoring until patient responding to questions appropriately
☐ If reversal agent used, observation two hours after answering questions appropriately
☐ Mental status and ambulation at baseline at time of discharge/disposition
Fasting Grid
Standard risk patient** Higher-risk patient**
Oral intake in the Emergent Semi-urgent Non-urgent Oral intake in the Emergent Semi-urgent Non-urgent
Urgent Procedure Urgent Procedure
prior 3 hours Procedure procedure procedure prior 3 hours Procedure procedure procedure
All levels of All levels of
All levels of All levels of Nothing All levels of sedation All levels of sedation
Nothing All levels of sedation All levels of sedation sedation sedation
sedation sedation
Up to and including
Up to and including All levels of Up to and including Minimal sedation
All levels of Up to and including Clear liquids only extended moderate
Clear liquids only All levels of sedation extended moderate sedation brief deep sedation only
sedation
sedation brief deep sedation
sedation Up to and including
Up to and including dissociative
All levels of Minimal sedation Minimal sedation
dissociative Light snack sedation; non-
All levels of Up to and including Minimal sedation sedation only only
Light snack sedation; non- extended moderate
sedation brief deep sedation only sedation
extended moderate
sedation Up to and including
dissociative
Up to and including Heavier snack or All levels of Minimal sedation Minimal sedation
Heavier snack or All levels of Minimal sedation Minimal sedation sedation; non-
extended moderate meal sedation only only
meal sedation only only extended moderate
sedation sedation
Dissociative Brief: < 10 min
Intermediate or
Minimal sedation; brief or Extended moderate Brief deep
sedation only → intermediate-length → sedation → sedation → extended-length Intermediate: 10-20 min
deep sedation Extended: > 20 min
moderate sedation
Additional Comments
MD Name Sign Date/Time
*Walls RM and Murphy MF: Manual of Emergency Airway Management. Philadelphia, Lippincott, Williams and Wilkins, 3rd edition, 2008
**Green, Roback et al. Fasting and Emergency Department Procedural Sedation and Analgesia: A Consensus-Based Clinical Practice Advisory.
Ann Emerg Med. 2007;49:454-461. R. Strayer / P. Andrus emupdates.com 11.28.2013
You might also like
- PALS Provider Manual PDFDocument57 pagesPALS Provider Manual PDFtimie_reyes90% (21)
- Board Stiff ThreeDocument440 pagesBoard Stiff Threewin co100% (1)
- 1b. Ambulatory AnesthesiaDocument47 pages1b. Ambulatory AnesthesiaBakingpancakes100% (5)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (3)
- Seven Ps For RSI BOARDDocument2 pagesSeven Ps For RSI BOARDJames BrownNo ratings yet
- Rapid Sequence Intubation: Mask and MonitoringDocument6 pagesRapid Sequence Intubation: Mask and MonitoringHatim DziauddinNo ratings yet
- Propofol Drug StudyDocument3 pagesPropofol Drug StudyAngelica shane Navarro100% (2)
- Status Epilepticus Pediatric DR - RPDocument4 pagesStatus Epilepticus Pediatric DR - RPAdnin NugrohoNo ratings yet
- Anesthesia For Day Care SurgeryDocument60 pagesAnesthesia For Day Care Surgerymedico_bhalla93% (15)
- 9 Ketamine Drug StudyDocument7 pages9 Ketamine Drug Studyshadow gonzalezNo ratings yet
- Intubation ChecklistDocument2 pagesIntubation ChecklistDaniel CrookNo ratings yet
- Local Anesthesia and Concious SedationDocument43 pagesLocal Anesthesia and Concious Sedationpawi18No ratings yet
- EpinephrineDocument4 pagesEpinephrinegovind_soni_15No ratings yet
- CH 8Document12 pagesCH 8Олександр РабошукNo ratings yet
- Afebrile SeizuresDocument6 pagesAfebrile SeizuresKristoffer EscletoNo ratings yet
- Anaesthesia Drugs Used CommonlyDocument6 pagesAnaesthesia Drugs Used CommonlyAmar Mahesh KalluNo ratings yet
- Status EpilepticusDocument3 pagesStatus EpilepticusVandeosNo ratings yet
- Carboprost 1Document3 pagesCarboprost 1angerson5100% (1)
- Drug StudyDocument10 pagesDrug StudyBandana RajpootNo ratings yet
- Flip Chart-Converted 2Document10 pagesFlip Chart-Converted 2anisah mahmudah0% (1)
- Material, Vincent M. (Types of Anesthesia Used in Cesarean Section)Document22 pagesMaterial, Vincent M. (Types of Anesthesia Used in Cesarean Section)Vincent Maralit MaterialNo ratings yet
- Obat Ayu (Anestesi)Document11 pagesObat Ayu (Anestesi)Ayu PratiwiNo ratings yet
- Mosby - Mosby's Drug Reference For Health Professions, 4e-Mosby (2013) - DeletedDocument3 pagesMosby - Mosby's Drug Reference For Health Professions, 4e-Mosby (2013) - DeletedehsanNo ratings yet
- Anticoagulation Protocol For PostDocument8 pagesAnticoagulation Protocol For PostMohammed IbrahimNo ratings yet
- Status Epilepticus and ICPDocument9 pagesStatus Epilepticus and ICPjoomds51No ratings yet
- OVERVIEW Rapid Sequence Intubation (RSI) Is An Airway Management Technique That ProducesDocument7 pagesOVERVIEW Rapid Sequence Intubation (RSI) Is An Airway Management Technique That ProducesOkami PNo ratings yet
- Seizures and Status Epilepticus - Management Practice Guideline ©Document12 pagesSeizures and Status Epilepticus - Management Practice Guideline ©ANDREWNo ratings yet
- COVID19 Management Algorithm 22042021 v1Document1 pageCOVID19 Management Algorithm 22042021 v1shivani shindeNo ratings yet
- 8 Propofol Drug StudyDocument4 pages8 Propofol Drug Studyshadow gonzalez100% (1)
- Cu 7Document6 pagesCu 7VALERIANO TRISHANo ratings yet
- AtropinDocument9 pagesAtropinarfitaaaaNo ratings yet
- Neonatalseizureclinicalguideline PDFDocument15 pagesNeonatalseizureclinicalguideline PDFNURUL NADIA BINTI MOHD NAZIR / UPMNo ratings yet
- Drug Study GentamicinDocument3 pagesDrug Study GentamicinEARL GERALD RICAFRANCANo ratings yet
- Airway Management 19 IndDocument29 pagesAirway Management 19 IndChi MutiaNo ratings yet
- JAMBALOS JERALDEEN BSN 4 2 DRUG STUDY FormatDocument3 pagesJAMBALOS JERALDEEN BSN 4 2 DRUG STUDY FormatJeraldeen JambalosNo ratings yet
- Drugs Used in AneasthesiaDocument73 pagesDrugs Used in AneasthesiaCabdiladif Ahmed McrfNo ratings yet
- Atracurium BesylateDocument3 pagesAtracurium BesylateWidya WidyariniNo ratings yet
- Management of SeizureDocument3 pagesManagement of SeizureNaanthini Dilly KannanNo ratings yet
- Drug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrDocument7 pagesDrug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrMary EnsomoNo ratings yet
- ConnectorDocument4 pagesConnectoryetaung8No ratings yet
- Drug Study: Sympathomime Tic, Beta2-Selective Adrenergic Agonist, Bronchodilator, AntiasthmaticDocument3 pagesDrug Study: Sympathomime Tic, Beta2-Selective Adrenergic Agonist, Bronchodilator, AntiasthmaticJichutreasure100% (1)
- Anestesiologia VeterinariaDocument21 pagesAnestesiologia VeterinariaAngie G SuarezNo ratings yet
- 038 AnaphylaxisDocument5 pages038 AnaphylaxisabbuahmedibbuNo ratings yet
- 7698alorithm SeizureDocument3 pages7698alorithm Seizureboromeus abyasa daniswara100% (1)
- TivaDocument38 pagesTivasunny kumar100% (1)
- Esmeron 10 MG/ML Solution For Injection Rocuronium Bromide Prescribing InformationDocument3 pagesEsmeron 10 MG/ML Solution For Injection Rocuronium Bromide Prescribing InformationVeeta Ruchi LieNo ratings yet
- 1614978209sampleDocument9 pages1614978209sampleReddyNo ratings yet
- Drug-Assisted Intubation (Dai) : Expanded Scope Practice (NR)Document1 pageDrug-Assisted Intubation (Dai) : Expanded Scope Practice (NR)MEKSELINA KALENDERNo ratings yet
- Adult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAdult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of Indiapramodbankhele3845No ratings yet
- 5 Emergency Drugs (Zacarias)Document7 pages5 Emergency Drugs (Zacarias)Joheina Cyndril L. ZacariasNo ratings yet
- Guideline For Management of Generalised Convulsive Status Epilepticus in ChildrenDocument11 pagesGuideline For Management of Generalised Convulsive Status Epilepticus in ChildrenAnas Sheikh ibrahimNo ratings yet
- Drug 2Document4 pagesDrug 2Abie Jewel Joy RoqueNo ratings yet
- Anasthesia & AsthmaDocument30 pagesAnasthesia & AsthmafadhiliNo ratings yet
- Drug Study: PART 1: To Be Completed Prior To Clinical ExperienceDocument5 pagesDrug Study: PART 1: To Be Completed Prior To Clinical ExperienceFrozanSNo ratings yet
- Status Elipticus April 2018Document2 pagesStatus Elipticus April 2018walidNo ratings yet
- In Tub at IonDocument6 pagesIn Tub at IonWinnieChin LeeNo ratings yet
- CRASH CART Presentation PPTX 1 MELODocument33 pagesCRASH CART Presentation PPTX 1 MELOCamille GalasNo ratings yet
- Pre and Post OperationDocument5 pagesPre and Post Operationhacker ammerNo ratings yet
- MidazolamDocument2 pagesMidazolamiamlx2No ratings yet
- Anaesthetic Management of PheochromocytomaDocument22 pagesAnaesthetic Management of PheochromocytomaZoelNo ratings yet
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Combined Ventilator and Bicarbonate Strategy in The Management of Status AsthmaticusDocument4 pagesCombined Ventilator and Bicarbonate Strategy in The Management of Status AsthmaticusDaniel GilbertoNo ratings yet
- 10 1002@ptr 6698Document10 pages10 1002@ptr 6698Siti lestarinurhamidahNo ratings yet
- Sepsis - Eval and MGMTDocument62 pagesSepsis - Eval and MGMTDr Ankit SharmaNo ratings yet
- The Laryngeal Mask Airway: Technical Guidelines and Use in Special SituationsDocument10 pagesThe Laryngeal Mask Airway: Technical Guidelines and Use in Special Situationsjangkrik21No ratings yet
- Criticalcare Positionpaper 060114Document25 pagesCriticalcare Positionpaper 060114BillaMozaNo ratings yet
- 4 Weaning Ventilator-NIADocument31 pages4 Weaning Ventilator-NIAResyana Widyayani100% (1)
- Refractory Anaphylaxis Algorithm 2021Document1 pageRefractory Anaphylaxis Algorithm 2021ay254No ratings yet
- NCORT Book PDFDocument66 pagesNCORT Book PDFSintoun100% (2)
- HFO Training ManualDocument396 pagesHFO Training ManualMehek KhannaNo ratings yet
- QuestionsDocument4 pagesQuestionsKeerthi Chowdary AmaraneniNo ratings yet
- ETT SUCTION DEWASA ACI14 - Suction - 2-2 PDFDocument46 pagesETT SUCTION DEWASA ACI14 - Suction - 2-2 PDFAde Rahmah YuliaNo ratings yet
- European COnsensus SDRDocument19 pagesEuropean COnsensus SDRDiego DppNo ratings yet
- Atlas of Operative Maxillofacial Trauma Surgery Primary Repair of Facial Injuries (UnitedVRG)Document834 pagesAtlas of Operative Maxillofacial Trauma Surgery Primary Repair of Facial Injuries (UnitedVRG)Ahmad YNo ratings yet
- Advanced Airway: Lynn K. Wittwer, MD, MPD Clark County EMSDocument56 pagesAdvanced Airway: Lynn K. Wittwer, MD, MPD Clark County EMSiaaNo ratings yet
- Airway ExamDocument7 pagesAirway ExamCharmaine LingdasNo ratings yet
- Ear, Nose and Throat Emergencies: Learning ObjectivesDocument5 pagesEar, Nose and Throat Emergencies: Learning ObjectivesRidho RifhansyahNo ratings yet
- Paediatric Intensive Care Unit: Information For FamiliesDocument9 pagesPaediatric Intensive Care Unit: Information For FamiliesJaya PrabhaNo ratings yet
- 256 Care: Jurnal Ilmiah Ilmu Kesehatan Vol .8, No.2, 2020, Hal 256-272 Tersedia Online Di ISSN 2527-8487 (Online) ISSN 2089-4503 (Cetak)Document17 pages256 Care: Jurnal Ilmiah Ilmu Kesehatan Vol .8, No.2, 2020, Hal 256-272 Tersedia Online Di ISSN 2527-8487 (Online) ISSN 2089-4503 (Cetak)Hamam PrakosaNo ratings yet
- Dott 2nd Year Syllabus - TheoryDocument4 pagesDott 2nd Year Syllabus - TheoryRahul RoyNo ratings yet
- Applied Surgical Anatomy of The Larynx and TracheaDocument24 pagesApplied Surgical Anatomy of The Larynx and TracheaMihaNo ratings yet
- Journal Club: Surfactant Therapy in Premature InfantsDocument44 pagesJournal Club: Surfactant Therapy in Premature InfantsSubash PaudealNo ratings yet
- Saqib CIADocument4 pagesSaqib CIASaqib KhanNo ratings yet
- Airway Emergency ManagementDocument47 pagesAirway Emergency ManagementTerefe AlemayehuNo ratings yet
- Suctioning by PhysiotherapistDocument39 pagesSuctioning by PhysiotherapistRanjitha ArumugamNo ratings yet
- Penetrating Neck Injuries - Initial Evaluation and Management - UpToDateDocument20 pagesPenetrating Neck Injuries - Initial Evaluation and Management - UpToDateVerónica VidalNo ratings yet
- C Mac Video LaryngoscopesDocument20 pagesC Mac Video LaryngoscopesSayyid AbulkhairNo ratings yet
- CPRDocument19 pagesCPRNidhi KaushalNo ratings yet
- A Study To Assess The Knowledge and Practice of Endotracheal Suctioning Among Neuro NursesDocument55 pagesA Study To Assess The Knowledge and Practice of Endotracheal Suctioning Among Neuro NursesBilal A. AbdullahNo ratings yet