Professional Documents
Culture Documents
8
8
Uploaded by
atika sgrtCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8
8
Uploaded by
atika sgrtCopyright:
Available Formats
ARTICLE
Safety, Immunogenicity, and Immune Memory
of a Novel Meningococcal (Groups A, C, Y, and
W-135) Polysaccharide Diphtheria Toxoid Conjugate
Vaccine (MCV-4) in Healthy Adolescents
Harry Keyserling, MD; Thomas Papa, MD; Katalin Koranyi, MD; Robert Ryall, PhD; Ehab Bassily, MSc;
Michael J. Bybel, BS; Kevin Sullivan, PhD; Gregory Gilmet, MD; Al Reinhardt, PhD
Objective: A meningococcal (groups A, C, Y, and tial vaccination, geometric mean serum bactericidal
W-135) polysaccharide diphtheria toxoid conjugate antibody titers, and safety assessments.
vaccine (MCV-4; Menactra; Sanofi Pasteur Inc, Swift-
water, Pa) was developed to improve the profile of cur- Results: Both vaccines were well tolerated; most reac-
rently licensed products. The objective of this study tions were mild. More MCV-4 recipients reported solic-
was to compare the tolerability, immunogenicity, and ited local reactions (68.9%) than PSV-4 recipients (30.2%).
immune memory of MCV-4 with those of a quadriva- Both MCV-4 and PSV-4 were highly immunogenic; simi-
lent polysaccharide vaccine (PSV-4; Menomune A/C/Y/ lar proportions of participants had 4-fold or greater in-
W-135; Sanofi Pasteur Inc). creases in serum bactericidal antibody (range, 80.1%-
96.7%) to the 4 serogroups. Three-year follow-up showed
Design, Setting, Participants: A randomized, double- persistence of serum bactericidal antibody and booster
blind trial was performed at 11 clinical centers in the responses to MCV-4 consistent with immune memory
United States. The vaccine MCV-4 or PSV-4 was admin- in participants previously vaccinated with MCV-4, but
istered to 881 healthy 11- to 18-year-olds. Sera were col- not in those who had previously received PSV-4.
lected prevaccination and 28 days postvaccination. Three-
year follow-up and booster vaccination with MCV-4 were Conclusions: The vaccine MCV-4 was well tolerated and
performed in a participant subset from each group and highly immunogenic. Persistence of bactericidal activ-
a control group. ity with MCV-4, but not PSV-4, was evident 3 years af-
ter the initial immunization. Booster response was dem-
Main Outcome Measures: Proportion of partici- onstrated after a second vaccination with MCV-4.
pants with a 4-fold or greater increase in serum bacteri-
cidal antibody against each serogroup 28 days after ini- Arch Pediatr Adolesc Med. 2005;159:907-913
I
N S EPTEMBER 2004, THE V AC - ported mortality rates as high as 22.5%.1,4
cines and Related Biological Prod- Up to 83% of meningococcal disease re-
ucts Advisory Committee of the ported in adolescents would be poten-
US Food and Drug Administra- tially preventable with a vaccine directed
tion voted unanimously for reg- against serogroups A, C, Y, and W-135.4
istration of the first quadrivalent menin- In 2000, the US Advisory Committee
gococcal conjugate vaccine against on Immunization Practices recom-
serogroups A, C, Y, and W-135 (MCV-4; mended informing college freshmen about
Menactra; Sanofi Pasteur Inc, Swiftwater, meningococcal disease and the benefits of
Pa) intended for use in adolescents and vaccination. 5 The currently available
adults, which was licensed in January quadrivalent meningococcal polysaccha-
Author Affiliations: Emory 2005. In the United States, approxi- ride vaccine against groups A, C, Y, and
University, Atlanta, Ga mately 97% of invasive meningococcal dis- W-135 combined (PSV-4; Menomune A/C/
(Drs Keyserling and Sullivan); ease is sporadic, which underscores the Y/W-135; Sanofi Pasteur Inc) induces T-
Sanofi Pasteur Inc, Swiftwater, need for a vaccine prevention strategy.1-3 cell–independent immune responses that
Pa (Drs Papa and Ryall, Adolescents are a key target group for vac- diminish over time and is not recom-
Messrs Bassily and Bybel, and
cination against invasive meningococcal mended for routine immunization.2,5 In
Drs Gilmet and Reinhardt); and
Children’s Hospital, Columbus, disease because of a high incidence rate and contrast, T-cell–dependent antibody re-
Ohio (Dr Koranyi). risk of serious untoward outcomes. Me- sponses, such as those produced by mono-
Group Information: A list of ningococcal disease is the leading cause of valent meningococcal conjugate vac-
the members of the group meningitis and sepsis in adolescents and cines against serogroup C, are intended to
appears on page 913. young adults and is associated with re- persist over a longer period of time and
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
907
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
have been associated with the development of immune ing an overnight incubation at 37°C with 5% CO2, bacteria
memory, reductions in carriage rates, and herd immu- colonies in the wells were counted. The endpoint titer was de-
nity in the United Kingdom.2,6-8 The vaccine MCV-4 was termined as the reciprocal serum dilution yielding 50% or greater
developed in the hope that it would have similar effects killing of the bacteria as compared with the mean of the comple-
ment control wells. The lower limit of detection was a titer of
and broader protection against 4 major meningococcal
8. Samples with no detectable antibody were assigned a titer
disease-causing serogroups.9-13 This study was designed of 4 for the calculation of geometric mean titers (GMTs).
to assess the immunogenicity and safety profile of MCV-4
compared with PSV-4 after an initial vaccination and a
3-year follow-up assessment and vaccination with MCV-4. STATISTICAL METHODS
For the initial vaccination, the primary immunogenicity crite-
METHODS rion was the proportion of participants with a 4-fold or greater
rise in SBA titer for each serogroup 28 days postvaccination. We
STUDY DESIGN calculated GMTs, seroconversion rates, and the distribution and
cumulative frequency of SBA titers for each of the 4 serogroups
This randomized, blinded, multicenter trial was conducted at for both treatment groups at baseline and day 28. For GMTs, we
11 clinical sites in the United States in accordance with the prin- calculated 95% confidence intervals and P values using a t test;
ciples outlined in the Declaration of Helsinki. Local institu- we calculated 95% confidence intervals for seroconversion, de-
tional review boards approved the protocol and consent forms. fined as proportion of participants with titers of less than 8 at
Written informed consent was obtained from a parent or guard- day 0 who achieved a 4-fold or greater rise in SBA titers on day
ian and assent from each participant was obtained as required 28. For participants receiving a booster vaccination, 95% con-
by the institutional review board. fidence intervals were calculated for the GMTs on day 0 and 28
Eligible participants were healthy adolescents 11 to 18 years of the initial vaccination, before booster vaccination, and 8 and
of age. On the day of initial immunization, participants had no 28 days after booster vaccination. The sample size was chosen
recent history (within the preceding 72 hours) of acute illness based on the minimum number of participants needed to pro-
or antibiotic use, serious chronic illness, immunologic defi- vide 90% power to assess whether a similar proportion of the
ciency, prior diagnosis of meningococcal disease, or prior me- MCV-4 and PSV-4 had a 4-fold or greater rise in SBA titer. Par-
ningococcal vaccination. Three years after the initial vaccina- ticipants who provided sera between 28 and 56 days after the
tion, a convenience sample of participants from each vaccine initial vaccination were evaluated. Analyses were performed us-
group and a meningococcal vaccine–naive group received an ing SAS version 8.2 (SAS Institute, Cary, NC). We assessed safety
open-label dose of MCV-4. based on the proportion of participants who experienced a se-
All vaccines were provided by Sanofi Pasteur Inc. Each freeze- vere solicited reaction after initial vaccination and calculated 95%
dried dose of PSV-4 contained 50 µg of capsular polysaccha- confidence intervals. We calculated P values based on the Fisher
ride from each serogroup (A, C, Y, and W-135) with lactose exact text for individual solicited reactions to determine whether
stabilizer. Each dose was reconstituted with 0.5 mL of sterile, the observed proportion of participants with an individual re-
pyrogen-free distilled water. action was associated with vaccination.
Each dose of MCV-4 contained 4 µg of capsular polysac-
charide from each serogroup (A, C, Y, and W-135) covalently RESULTS
attached to a total of approximately 48 µg of diphtheria toxoid
protein. Each dose was formulated in 0.5 mL sterile, pyrogen-
free, phosphate-buffered physiological saline without preser- DEMOGRAPHICS
vative in a prefilled syringe.
Vaccines were administered in the deltoid region; MCV-4 For the initial vaccination, 881 participants (Table 1)
was administered intramuscularly and PSV-4 was adminis- were randomized to the MCV-4 (N = 440) and PSV-4
tered subcutaneously. A blinded, computer-generated random- (N=441) groups and underwent study procedures be-
ized allocation schedule with a block size of 2 was provided by tween September 2000 and October 2001. The 2 groups
the sponsor. To maintain blinding of study personnel, vacci- were similar in sex distribution, age, and racial compo-
nations and safety assessments were performed by different study sition. A total of 425 participants from the MCV-4 group
personnel. Booster vaccination was performed 3 years after ini- and 423 from the PSV-4 group were included in the im-
tial vaccination with open-label MCV-4.
Participants were monitored for 30 minutes postvaccina-
munogenicity analysis. Of the 33 total participants ex-
tion for immediate reactions. Solicited local and systemic re- cluded from the immunogenicity analysis, 23 (10 receiv-
actions were recorded on diary cards for 7 days following vac- ing MCV-4 and 13 receiving PSV-4) did not provide sera
cination. Any serious adverse events were to be reported within the prespecified visit windows, and 6 (2 receiv-
throughout the trial. Safety assessments were made 28 days and ing MCV-4 and 4 receiving PSV-4) had not met entry cri-
6 months after the initial vaccination and 28 days after the teria and were enrolled in error. The distribution of par-
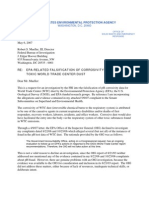
booster vaccination. Sera were obtained prior to and 28 days ticipants over the course of the trial is illustrated in
after each vaccination and also on day 8 after the booster vac- Figure 1.
cination. Assays were performed by Sanofi Pasteur Inc Global For the 3-year follow-up vaccination, 153 previously
Clinical Immunology Laboratory (Swiftwater, Pa) to deter- vaccinated and 88 control participants underwent study
mine functional serum bactericidal antibody (SBA) responses
for each serogroup.
procedures between February and April 2004 (Figure 1).
The SBA responses were determined using 2-fold serial di- There were no significant differences in demographic or
lutions of sera incubated in sterile 96-well microtiter plates with immunogenicity parameters between the cohort of par-
baby rabbit complement and serogroup-specific meningococ- ticipants who received a 3-year booster dose of MCV-4,
cal bacteria. An agar overlay medium was added to the serum/ control participants, or the overall study population for
complement/bacteria mixture and allowed to harden. Follow- the initial vaccination.
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
908
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
Table 1. Participant Demographics, Initial Vaccination* A Safety Population 881 Participants Enrolled
and Randomized
MCV-4 PSV-4
Characteristic (N = 440) (N = 441)
MCV-4 PSV-4
Age, mean (range), y 14.3 (11-18) 14.3 (11-17)
N (%) N (%)
Sex, No. (%)
Male 236 (53.6) 250 (56.7) Enrolled and Vaccinated 440 (100) 441 (100)
Female 204 (46.4) 191 (43.3)
Race, No. (%)
Provided Local and Systemic 440 (100) 441 (100)
White 421 (95.7) 418 (94.8)
Reaction Data (Days 0-7)
Black 14 (3.2) 15 (3.4)
Hispanic 1 (0.2) 2 (0.5)
Asian 1 (0.2) 1 (0.2) Lost to Follow-up 2 (0.5) 4 (0.9)
Other 3 (0.7) 5 (1.1) Voluntary Withdrawal 2 (0.5) 2 (0.5)
Abbreviations: MCV-4, quadrivalent meningococcal conjugate vaccine
against groups A, C, Y, and W-135; PSV-4, quadrivalent meningococcal Completed 6-Month Safety 436 (99.1) 435 (98.6)
polysaccharide vaccine against groups A, C, Y, and W-135. Follow-up
*No significant between-group differences were observed.
B Immunogenicity Population 881 Participants Enrolled
and Randomized
SAFETY AND REACTIONS
All enrollees provided a baseline blood sample, received MCV-4 PSV-4
N (%) N (%)
the study vaccine, and attended the 28-day follow-up visit
for safety assessment and second blood draw. Ten par- Enrolled and Vaccinated 440 (100) 441 (100)
ticipants did not provide safety data at the 6-month follow-
up: 4 were MCV-4 recipients (2 lost to follow-up and Did Not Meet an Entry Criterion 2 (0.5) 4 (0.9)
2 voluntarily withdrew) and 6 were in the PSV-4 group Visit Outside of Time Window 10 (2.3) 13 (2.9)
(4 lost to follow-up and 2 voluntarily withdrew). No par- Other Reason 3 (0.7) 1 (0.2)
ticipant dropped out or was withdrawn from the study
because of an adverse event. Per Protocol Immunogenicity 425 (96.6) 423 (95.9)
After the initial vaccination, 2 participants had a va- Data at Day 28
sovagal episode within 30 minutes of receiving MCV-4.
Vaccine-Naive
These events resolved spontaneously without medical in- Group Added
tervention. No other immediate reactions were re-
Convenience Sample for 76 77 88
ported after the initial vaccination. 3-Year Booster Vaccination
After the initial vaccination, local reaction data were
available for 438 participants in the MCV-4 group and
440 in the PSV-4 group. Local reactions were more com- Immunogenicity Data Reported 76 77 88
mon in MCV-4 recipients (Table 2). The majority of
these reactions were mild (73%) or moderate (26%) in Figure 1. Participant flow.
severity and of limited duration (median, 2 days). All lo-
cal reactions in the PSV-4 group were either mild (88%)
or moderate (12%). The most frequent local reaction in all reported solicited systemic reactions were mild to mod-
both groups was pain at the injection site, 302 (68.9%) erate in severity and resolved within 3 days of vaccina-
of 438 participants vs 133 (30.2%) of 441 participants tion. One case of high fever, defined as an oral tempera-
in the MCV-4 and PSV-4 groups, respectively. All local ture of 40°C or higher, occurred on day 7 after MCV-4
reactions resolved without sequelae. vaccination and lasted for 1 day. A similar percentage of
Systemic reaction data were available for 439 partici- participants in the MCV-4 group (17/439; 3.9%) and the
pants in the MCV-4 group and 441 participants in the PSV-4 group (18/441, 4.1%) had severe systemic reac-
PSV-4 group after the initial vaccination. The overall fre- tions.
quency of systemic reactions was similar in both groups.
More than half of the participants reported at least 1 so- SERIOUS ADVERSE EVENTS
licited systemic reaction, 251 (57.2%) of 439 partici-
pants in the MCV-4 group vs 229 (51.9%) of 441 par- Six participants, 5 in the MCV-4 group and 1 in the PSV-4
ticipants in the PSV-4 group (Table 3). Mild to moderate group, experienced 7 serious adverse events within 189
headache was the most common systemic reaction, re- days after the initial vaccination. Each of these events—
ported in 197 (44.9%) of 439 participants in the MCV-4 dehydration and pyelonephritis, bilateral testicular fixa-
group and 174 (39.5%) of 441 participants in the PSV-4 tion, acetaminophen overdose, facial baseball injury, torn
group. Fatigue, anorexia, and diarrhea were the next most meniscus, preexisting supraventricular tachycardia—
commonly reported solicited systemic reactions and oc- was considered unrelated to the vaccine by study inves-
curred with similar frequencies in both groups. Almost tigators.
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
909
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
Table 2. Solicited Local Reactions in the 2 Study Groups Table 3. Solicited Systemic Reactions in the 2 Study Groups
After Initial Vaccination* After Initial Vaccination*
MCV-4 PSV-4 MCV-4 PSV-4
(N = 438), (N = 441), (N = 439), (N = 441),
Reaction Severity No. (%) No. (%) Reaction Severity No. (%) No. (%)
Any reaction Mild 230 (52.5) 135 (30.6) Any reaction Mild 145 (33.0) 150 (34.0)
Moderate 82 (18.7) 18 (4.1) Moderate 89 (20.3) 61 (13.8)
Severe 5 (1.1) 0 Severe 17 (3.9) 18 (4.1)
Pain Mild 228 (52.1) 116 (26.3) Headache Mild 120 (27.3) 126 (28.6)
Moderate 73 (16.7) 17 (3.9) Moderate 70 (15.9) 40 (9.1)
Severe† 1 (0.2) 0 Severe† 7 (1.6) 8 (1.8)
Induration Mild 73 (16.7) 32 (7.3) Fatigue Mild 86 (19.6) 79 (17.9)
Moderate 13 (3.0) 2 (0.5) Moderate 33 (7.5) 22 (5.0)
Severe† 3 (0.7) 0 Severe† 5 (1.1) 3 (0.7)
Swelling Mild 49 (11.2) 21 (4.8) Diarrhea Mild 42 (9.6) 52 (11.8)
Moderate 11 (2.5) 3 (0.7) Moderate 6 (1.4) 9 (2.0)
Severe† 3 (0.7) 0 Severe† 0 1 (0.2)
Redness Mild 45 (10.3) 27 (6.1) Anorexia Mild 40 (9.1) 39 (8.8)
Moderate 7 (1.6) 1 (0.2) Moderate 10 (2.3) 12 (2.7)
Severe† 1 (0.2) 0 Severe† 4 (0.9) 3 (0.7)
Fever‡ Mild 12 (2.7) 10 (2.3)
Abbreviations: MCV-4, quadrivalent meningococcal conjugate vaccine Moderate 2 (0.5) 1 (0.2)
against groups A, C, Y, and W-135; PSV-4, quadrivalent meningococcal ⱖ40°C 1 (0.2) 0
polysaccharide vaccine against groups A, C, Y, and W-135. Vomiting Mild 7 (1.6) 2 (0.5)
*For all individual local reactions, a significantly greater percentage of Moderate 2 (0.5) 6 (1.4)
participants in the MCV-4 group had mild and moderate events compared Severe† 1 (0.2) 1 (0.2)
with the PSV-4 group (P⬍.001 for pain, induration, and swelling; P⬍.006
Rash Any 7 (1.6) 7 (1.6)
for redness).
†Severe pain is defined as disabling, unable to move arm; all other severe
reactions indicated were more than 2 inches in diameter. Abbreviations: MCV-4, quadrivalent meningococcal conjugate vaccine
against groups A, C, Y, and W-135; PSV-4, quadrivalent meningococcal
polysaccharide vaccine against groups A, C, Y, and W-135.
*The proportion of participants with moderate headache was significantly
higher in the MCV-4 group compared with the PSV-4 group (P = .02). No
At the 3-year follow-up, the safety profile, including other significant between-group differences were observed.
solicited reactions, was generally similar between †Severe symptoms were defined as follows: headache and fatigue,
participants in the MCV-4, PSV-4, and control groups. disabling requiring bed rest; anorexia, missing 3 or more meals; vomiting,
3 or more episodes; diarrhea, 5 or more episodes.
No serious adverse events or new or unexpected effects ‡Temperature measurement was not performed for 1 PSV-4 recipient,
were observed for any participant in any group. Among N = 440.
the cohort of 76 initial MCV-4 recipients revaccinated 3
years later, a second dose of MCV-4 was generally well
tolerated.
to 100% while those observed in the PSV-4 group were
IMMUNOGENICITY from 99.3% to 100% (data not shown).
In both groups of participants evaluated 3 years after
The SBA GMTs for each serogroup were similar be- the initial vaccination, bactericidal antibody levels re-
tween the MCV-4 and PSV-4 groups prior to the initial mained markedly higher than initial baseline values for
vaccination. Marked increases in SBA levels were ob- all 4 serogroups (Table 5). Overall, the percentage of
served 28 days after the initial vaccination for both study participants with SBA titers 128 or more ranged from 71%
groups (Table 4). The SBA response for serogroup A, to 95% for the MCV-4 group and from 57% to 83% for
assessed by GMTs, was significantly higher in the MCV-4 the PSV-4 group (data not shown). A booster dose of
group compared with the PSV-4 group. The GMTs for MCV-4 resulted in a rise in antibody response for all 4
the other serogroups were similar in the 2 vaccine groups. serogroups 8 days postvaccination. Participants who had
Overall, more than 90% of participants had titers of previously received PSV-4 also had high antibody re-
128 or more against all 4 serogroups after the initial vac- sponses 8 days postvaccination; however, the booster an-
cination (Table 4). The percentage of participants who tibody responses to the PSV-4 primed participants were
had a 4-fold or greater rise in SBA 28 days after the ini- not as high compared with the MCV-4 primed partici-
tial vaccination was highest for serogroups A and W-135 pants (Table 5). Both MCV-4 and PSV-4 groups had higher
for both vaccine groups. For all serogroups, the percent- bactericidal antibody levels compared with baseline for
age of participants with a 4-fold or greater rise was simi- all 4 serogroups at Day 28. Responses in the group of pre-
lar in the MCV-4 group compared with the PSV-4 group. viously meningococcal vaccine–naive participants were
Among participants with an SBA titer of less than 8 consistent with those observed after the initial vaccina-
before the initial vaccination, seroconversion, defined as tion with MCV-4, showing a marked rise in SBA levels.
a 4-fold or greater rise, occurred in the vast majority of These findings are further illustrated by the reverse cu-
participants 28 days after vaccination for all 4 sero- mulative distribution curves for bactericidal antibodies
groups. Values for the MCV-4 group ranged from 98.2% against the 4 serogroups on day 28 (Figure 2).
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
910
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
Table 4. Serum Bactericidal Antibody Activity: Initial Vaccination (per Protocol Population)
MCV-4 PSV-4 MCV-4 PSV-4
(N = 425) (N = 423) (N = 425) (N = 423)
Day 0 GMTs Day 28 GMTs Day 0 GMTs Day 28 GMTs Participants Participants
(95% (95% (95% (95% With ⱖ4-Fold Participants With ⱖ4-Fold Participants
Confidence Confidence Confidence Confidence Increase From With Titer Increase From With Titer
Serogroup Interval) Interval) Interval) Interval) Baseline, % ⱖ128, % Baseline, % ⱖ128, %
A 106 (87.6-129) 5483 (4920-6111) 88.7 (73.1-108) 3246 (2910-3620)* 92.7 99.8 92.4 100
C 33.7 (27.5-41.3) 1924 (1662-2228) 37.4 (30.4-46.0) 1639 (1406-1911) 91.7 98.9 88.7 98.5
Y 103 (87.8-121) 1322 (1162-1505) 112 (96.0-130) 1228 (1088-1386) 81.8 99.6 80.1 99.3
W-135 20.7 (17.7-24.2) 1407 (1232-1607) 23.9 (20.4-28.0) 1545 (1384-1725) 96.7 98.7 95.3 98.9
Abbreviations: GMTs, geometric mean titers; MCV-4, quadrivalent meningococcal conjugate vaccine against groups A, C, Y, and W-135; PSV-4, quadrivalent
meningococcal polysaccharide vaccine against groups A, C, Y, and W-135.
*P⬍.001 for MCV-4 vs PSV-4 at day 28.
Table 5. MCV-4 Booster 3 Years After Initial Vaccination: Convenience Sample From MCV-4 and PSV-4 Groups
With Vaccine-Naive Comparison
Geometric Mean Serum Bactericidal Antibody Titers (95% Confidence Intervals)
Day 0 Day 8 Day 28
MCV-4 PSV-4 Naive MCV-4 PSV-4 Naive MCV-4 PSV-4 Naive
Serogroup (n = 76) (n = 77) (n = 88) (n = 76) (n = 77) (n = 88) (n = 76) (n = 77) (n = 88)
A 1082 171 84 9393 4406 12 936 4326 3270 6399
(785-1491) (101-289) (48-146) (7613-11 590) (3286-5908) (10 007-16 722) (3475-5386) (2460-4348) (5069-8078)
C 211 109 43 18 113 1196 7453 8192 665 2955
(121-370) (59-203) (26-70) (14 296-22 949) (737-1939) (5340-10 402) (6317-10 624) (410-1078) (2045-4269)
Y 592 380 211 12 808 2896 7053 5846 2327 4366
(377-931) (251-577) (138-323) (9227-17 778) (2046-4100) (5072-9810) (4200-8137) (1690-3203) (3117-6114)
W-135 447 120 22 9566 1921 5657 4612 1577 2954
(305-654) (77-189) (15-32) (7244-12 633) (1450-2545) (4269-7498) (3523-6037) (1217-2044) (2314-3773)
Abbreviations: MCV-4, quadrivalent meningococcal conjugate vaccine against groups A, C, Y, and W-135; PSV-4, quadrivalent meningococcal polysaccharide
vaccine against groups A, C, Y, and W-135.
COMMENT centages of participants with systemic reactions were simi-
lar for both vaccines. A greater percentage of partici-
Adolescents and young adults in the United States repre- pants in the MCV-4 group reported immediate and local
sent a major target group for immunoprophylaxis against reactions, primarily pain, after initial vaccination com-
meningococcal disease.4,5 The reported incidence of in- pared with those in the PSV-4 group. These reactions were
vasive disease in this age group and the number of out- generally mild and resolved within 2 to 3 days. This find-
breaks have increased since 1991.3 The diagnosis of me- ing was not unexpected because PSV-4 has shown ex-
ningococcal disease presents challenges to the clinician cellent safety in clinical practice and the inclusion of a
because symptoms are similar to those of less serious ill- diphtheria toxoid carrier protein in MCV-4 had the po-
nesses, the symptoms have a sudden onset, and the dis- tential to cause more local reactions, similar to ob-
ease may rapidly progress to permanent disability or served reactions following tetanus-diphtheria vaccina-
death.3,13,14 Public concern is further heightened when cases tion. Further, the intramuscular route of MCV-4 injection
occur in school or college settings, resulting in mass im- might have caused increased reactogenicity relative to the
munization efforts as part of outbreak control.5 subcutaneous route used for PSV-4. Participants receiv-
The study described here was undertaken to evaluate ing a second dose of MCV-4 reported a similar level of
the immunogenicity and safety of a novel meningococcal local and systemic reactions compared with those who
(groups A, C, Y, and W-135) polysaccharide diphtheria tox- received a dose of MCV-4 3 years after an initial dose of
oid conjugate vaccine, MCV-4, vs those of PSV-4 in more PSV-4. Overall, safety findings among participants re-
than 800 participants. A 3-year follow-up was performed ceiving MCV-4 were consistent with those observed in
in a convenience sample of participants to evaluate the im- earlier trials in infants, toddlers, and adults.9-12
munogenicity of the vaccines within the time frame cur- Immunogenicity was evaluated using a standardized
rently recommended for revaccination with PSV-4.5 functional antibody assay, SBA with baby rabbit serum as
In this study, the safety profiles of the 2 vaccines were a complement source, as recommended by the World Health
comparable following the initial vaccination. The per- Organization (Geneva, Switzerland).15 The SBA re-
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
911
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
A Serogroup A B Serogroup C
100 100
90 90
Subjects Achieving Titer, %
80 80
70 70
60 60
50 50
40 40
30 30
20 20
10 10
0 0
8
16
32
64
24
48
96
92
36
16
32
64
24
48
96
92
36
12
25
51
38
76
53
12
25
51
38
76
53
10
20
40
81
55
10
20
40
81
55
16
32
65
16
32
65
>6
>6
C Serogroup Y D Serogroup W-135
100 100
90 90
Subjects Achieving Titer, %
80 80
70 70
60 60
50 50
40 40
30 30
20 20
10 10
0 0
8
16
32
64
24
48
96
92
36
16
32
64
24
48
96
92
36
12
25
51
38
76
53
12
25
51
38
76
53
10
20
40
81
55
10
20
40
81
55
16
32
65
16
32
65
>6
>6
SBA Antibody Titer SBA Antibody Titer
Figure 2. Reverse cumulative distribution curves for meningococcal (groups A, C, Y, W-135) polysaccharide diphtheria toxoid conjugate vaccine (MCV-4) booster
3 years after initial vaccination. Open circles indicate vaccine-naive subjects; triangles, quadrivalent polysaccharide vaccine (PSV-4) recipients; filled circles,
MCV-4 recipients; dotted lines, prebooster levels; solid lines, 28 days postvaccination; SBA, serum bactericidal antibody.
sponses elicited by the MCV-4 vaccine measured 28 days late that such a rise may be due to early onset of high-avidity
after the initial vaccination were comparable with or higher IgG antibodies. This is consistent with other studies that
than those observed after administration of the PSV-4 vac- have shown that booster responses are characterized by the
cine. Those participants with prevaccination SBA titers of presence of high-avidity IgG antibodies.
less than 8, a level considered at risk for serogroup C me- Immunogenicity findings in the current report are con-
ningococcal disease,16 exhibited comparable seroconver- sistent with those observed for the serogroup C menin-
sion rates to both vaccines, more than 98% for all 4 sero- gococcal conjugate vaccines, all of which induce robust
groups. Similarly, the proportion displaying a 4-fold increase immune responses in this age group.6 The efficacy of these
in SBA titers in the MCV-4 group was similar to that ob- vaccines against serogroup C meningococcal disease after
served with the licensed comparator vaccine, PSV-4, which 4 years was 96% in 15- to 17-year olds in the United King-
has proven efficacy and immunogenicity.5 dom and 96.8% in 2- to 20-year-olds in Quebec.19,20 The in-
Three years following primary vaccination, adolescents troduction of a universal vaccination program in the United
previously vaccinated with MCV-4 had higher SBA GMTs Kingdom resulted in a meningococcal serogroup C carriage
compared with those who had been vaccinated with PSV- reduction of 66% in 15- to 17-year-olds and herd immunity
4. A higher proportion of participants in the MCV-4 primed as evidenced by a 67% reduction of disease incidence among
group had SBA titers 128 or greater against serogroups A, unvaccinated infants, children, and adolescents.7,8,21 Further
C, Y, and W-135 compared with the PSV-4 primed group. experience is needed to determine whether the immunologi-
Rapid and robust booster SBA responses to a second dose cal properties observed with serogroup C meningococcal
of MCV-4 were observed in MCV-4 primed participants as conjugate vaccines will be observed with MCV-4 and the im-
illustrated by the reverse cumulative distribution curves. portant disease-causing serogroups A, Y, and W-135.
Responses to the MCV-4 booster dose among the PSV-4 In summary, results from this study of more than 800
primed group were less pronounced but nonetheless con- adolescents show that levels of protective serum bacte-
sistent with levels associated with protection against sero- ricidal antibodies to meningococcal serogroups A, C, Y,
group C meningococcal disease. The pattern of response and W-135 28 days after vaccination with MCV-4 were
observed in the PSV-4 primed group was similar to that ob- comparable with or higher than those observed after vac-
served with monovalent C conjugate vaccination of persons cination with PSV-4. Importantly, MCV-4 demon-
previously vaccinated with meningococcal polysaccharide strated the expected attributes of a conjugate vaccine, in-
vaccines.17 The finding that titers at day 8 were significantly cluding protective antibody persistence, priming and
higher than those seen at day 28 in all groups is unique com- booster responses, and a lack of hyporesponsiveness fol-
pared with other trials of conjugate vaccines.18 We specu- lowing repeat vaccination. Taken together, these find-
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
912
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
ings provide the scientific basis for the recent Advisory process and scientific presentation of the data and prepared
Committee on Immunization Practices working group drafts of the manuscript. Tom Le Duc, BS, oversaw the in-
recommendation for universal vaccination of 11- to 12- house conduct of the clinical trials at Sanofi Pasteur Inc.
year-olds, adolescents entering high school, and college
freshmen planning to live in dormitories with MCV-4
as a public health strategy to reduce the adolescent and REFERENCES
young adult meningococcal disease burden in the
United States.22 1. Rosenstein NE, Perkins BA, Stephens DS, et al. The changing epidemiology of
meningococcal disease in the United States, 1992-1996. J Infect Dis. 1999;
180:1894-1901.
Accepted for Publication: July 28, 2005. 2. Raghunathan PL, Bernhardt SA, Rosenstein NE. Opportunities for control of me-
ningococcal disease in the United States. Annu Rev Med. 2004;55:333-353.
Correspondence: Harry L. Keyserling, MD, Emory Uni- 3. Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococ-
versity School of Medicine, 2015 Uppergate Dr, NE, At- cal disease. N Engl J Med. 2001;344:1378-1388.
lanta, GA 30322 (hkeyser@emory.edu). 4. Harrison LH, Dwyer DM, Maples CT, et al. Risk of meningococcal infection in
college students. JAMA. 1999;281:1906-1910.
Meningococcal Vaccine Study Group Institutions and In- 5. Centers for Disease Control and Prevention. Prevention and control of menin-
vestigators: Center for Pediatric Research, Norfolk, Va, gococcal disease. MMWR Recomm Rep. 2000;49:1-10.
Douglas K. Mitchell, MD; Emory University School of Medi- 6. Borrow R, Goldblatt D, Andrews N, et al. Antibody persistence and immunologi-
cal memory at age 4 years after meningococcal group C conjugate vaccination
cine, Atlanta, Ga, Harry L. Keyserling, MD; Children’s Hos- in children in the United Kingdom. J Infect Dis. 2002;186:1353-1357.
pital, Columbus, Ohio, Katalin Koranyi, MD; Pennridge Pe- 7. Maiden MCJ, Stuart JM; United Kingdom Meningococcal Carriage Group. Re-
duced carriage of serogroup C meningococci in teenagers one year after the in-
diatric Associates, Sellersville, Pa, Erik F. Lamberth, MD; troduction of meningococcal C conjugate polysaccharide vaccine in the United
Holston Medical Group, Kingsport, Tenn, Joseph A. Ley, Kingdom. Lancet. 2002;359:1829-1830.
MD; Woburn Pediatric Associates, Woburn, Mass, Joseph 8. Ramsay ME, Andrews NJ, Trotter CL, Kaczmarski EB, Miller E. Herd immunity
from meningococcal serogroup C conjugate vaccination in England. BMJ. 2003;
P. Leader, MD; Wake Forest University School of Medi- 326:365-366.
cine, Winston-Salem, NC, Charles Woods, MD; Chil- 9. Campbell JD, Edelman R, King JC Jr, Papa T, Ryall R, Rennels MB. Safety, re-
dren’s Hospital Medical Center of Akron, Akron, Ohio, actogenicity, and immunogenicity of a tetravalent meningococcal polysaccharide-
diphtheria toxoid conjugate vaccine given to healthy adults. J Infect Dis. 2002;
Blaise Congeni, MD; Pediatrics and Adolescent Medicine 186:1848-1851.
PA, Marietta, Ga, Wilson P. Andrews, Jr, MD; North Shore 10. Rennels M, King J Jr, Ryall R, et al. Dosage escalation, safety and immunogenic-
ity study of four dosages of a tetravalent meningococcal polysaccharide diphtheria
University Hospital Division of General Pediatrics, Great toxoid conjugate vaccine in infants. Pediatr Infect Dis J. 2004;23:429-435.
Neck, NY, Stephen Barone, MD; Albany Medical Center, 11. Rennels M, King J Jr, Ryall R, et al. Dose escalation, safety and immunogenicity
Department of Pediatrics, Albany, NY, Martha Lepow, MD. study of a tetravalent meningococcal polysaccharide diphtheria conjugate vac-
cine in toddlers. Pediatr Infect Dis J. 2002;21:978-979.
Financial Disclosure: Dr Keyserling has received hono- 12. Pichichero M, Casey J, Blatter M, et al. A comparative trial of the safety and im-
raria from Sanofi Pasteur Inc, Swiftwater, Pa, as a speaker. munogenicity of quadrivalent (A, C, Y, W-135) meningococcal polysaccharide-
Funding/Support: This study was funded by a grant from diphtheria conjugate vaccine versus quadrivalent polysaccharide vaccine in 2-10
year-old children. Pediatr Infect Dis J. 2005;24:57-62.
Sanofi Pasteur Inc. Drs Papa and Ryall, Messrs Bassily and 13. Swartz MN. Bacterial meningitis—a view of the past 90 years. N Engl J Med.
Bybel, and Drs Gilmet and Reinhardt are employees of 2004;351:1826-1828.
14. van de Beek D, de Gans J, Spanjaard L, et al. Clinical features and prognostic
Sanofi Pasteur Inc. Dr Sullivan received grant support to factors in adults with bacterial meningitis. N Engl J Med. 2004;351:1849-1859.
conduct the statistical analysis. Drs Keyserling and 15. Jodar L, Cartwright K, Feavers IM. Standardisation and validation of serological
Koranyi received grant support to conduct the clinical assays for the evaluation of immune responses to Neisseria meningitidis sero-
group A and C vaccines. Biologicals. 2000;28:193-197.
trial. 16. Borrow R, Andrews N, Goldblatt D, et al. Serological basis for use of meningo-
Role of the Sponsor: Sanofi Pasteur Inc was actively in- coccal serogroup C conjugate vaccines in the United Kingdom. Infect Immun.
volved in the conception and design of the study, moni- 2001;69:1568-1573.
17. Southern J, Deane S, Ashton L, et al. Effects of prior polysaccharide vaccination
toring, evaluation and analysis of the data, manuscript on magnitude, duration, and quality of immune responses to and safety profile
writing, review, and authorization for manuscript sub- of a meningococcal serogroup C tetanus toxoid conjugate vaccination in adults.
Clin Diagn Lab Immunol. 2004;11:1100-1104.
mission. 18. Borrow R, Southern J, Andrews N, et al. Comparison of antibody kinetics fol-
Previous Presentations: Information about the initial lowing meningococcal serogroup C conjugate vaccine between healthy adults
immunization was presented in part at the 43rd Inter- previously vaccinated with meningococcal A:C polysaccharide vaccine and vaccine-
naive controls. Vaccine. 2001;19:3043-3050.
science Conference on Antimicrobial Agents and Che- 19. Trotter CL, Andrews NJ, Kaczmarski EB, Miller E, Ramsay ME. Effectiveness of
motherapy; September 17, 2003; Chicago, Ill; the 4th Pe- meningococcal serogroup C conjugate vaccine 4 years after introduction. Lancet.
diatric Infectious Disease Society Conference; October 2004;364:365-367.
20. De Wals P, Deceuninck G, Boulianne N, De Serres G. Effectiveness of a mass
12, 2003; Rancho Bernardo, Calif; and the 6th Canadian immunization campaign using serogroup C meningococcal conjugate vaccine.
Immunization Conference; December 6, 2004; Mon- JAMA. 2004;292:2491-2494.
21. Miller E, Salisbury D, Ramsey M. Planning, registration, and implementation of
treal, Quebec. A presentation of partial data from the an immunisation campaign against meningococcal serogroup C disease in the
3-year follow-up was made at the Pediatric Academic So- UK: a success story. Vaccine. 2001;20:S58-S67.
cieties Meeting; May 15, 2005; Washington, DC. 22. Bilukha OO, Rosenstein N; National Center for Infectious Diseases; Centers for
Disease Control and Prevention (CDC). Prevention and control of meningococ-
Acknowledgment:KeithVeitch,PhD,andLisaDeTora,PhD, cal disease: recommendations of the Advisory Committee on Immunization Prac-
of Sanofi Pasteur Inc provided guidance for the writing tices (ACIP). MMWR Recomm Rep. 2005;54:1-21.
(REPRINTED) ARCH PEDIATR ADOLESC MED/ VOL 159, OCT 2005 WWW.ARCHPEDIATRICS.COM
913
©2005 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/ on 09/09/2013
You might also like
- TCMDocument4 pagesTCMxuxumoNo ratings yet
- Chapter 19 Mental StatusDocument3 pagesChapter 19 Mental StatusAmber Nicole HubbardNo ratings yet
- Schiller JT - 09Document6 pagesSchiller JT - 09Bruno RalhaNo ratings yet
- 140794.3 20210324105625 CoveredDocument16 pages140794.3 20210324105625 CoveredBruno RamírezNo ratings yet
- 1 s2.0 S0264410X21009622 MainDocument7 pages1 s2.0 S0264410X21009622 Mainnqchi180418No ratings yet
- Vasquez, 2015Document13 pagesVasquez, 2015Jorge Hantar Touma LazoNo ratings yet
- Current Approach To HIV Vaccine (Melkamu and Begizaw)Document24 pagesCurrent Approach To HIV Vaccine (Melkamu and Begizaw)melkamuNo ratings yet
- Fase 3.1Document9 pagesFase 3.1Verliatesya TugasNo ratings yet
- Towards An Epitope-Based Human Vaccine For Influenza: Tamar Ben-Yedidia Ruth ArnonDocument7 pagesTowards An Epitope-Based Human Vaccine For Influenza: Tamar Ben-Yedidia Ruth ArnonPCRMANNo ratings yet
- Vaccine: D.N. Durrheim, W.A. Orenstein, W.W. SchluterDocument3 pagesVaccine: D.N. Durrheim, W.A. Orenstein, W.W. SchluterVanesa MaciasNo ratings yet
- Working Paper 3 h5n1Document7 pagesWorking Paper 3 h5n1vijayNo ratings yet
- Hoes 2022Document11 pagesHoes 2022contreraz7No ratings yet
- Seguridad Vacunal: Precauciones y Contraindicaciones de Las Vacunas. Reacciones Adversas. FarmacovigilanciaDocument25 pagesSeguridad Vacunal: Precauciones y Contraindicaciones de Las Vacunas. Reacciones Adversas. FarmacovigilanciaMaribel Catalan HabasNo ratings yet
- Reverse VaccinologyDocument6 pagesReverse Vaccinologywagester683No ratings yet
- Clinical Paper Vaxneuvance PNEU-DIRECTION (Interchangeability)Document9 pagesClinical Paper Vaxneuvance PNEU-DIRECTION (Interchangeability)Johannus Susanto WibisonoNo ratings yet
- Summaries of Evidence in Support of Proposed Recommendations FinalDocument25 pagesSummaries of Evidence in Support of Proposed Recommendations FinalodyNo ratings yet
- Mourtzoukou Et Al-2008-British Journal of SurgeryDocument8 pagesMourtzoukou Et Al-2008-British Journal of SurgeryTony AdeosunNo ratings yet
- Live Attenuated Human Rotavirus Vaccine, Rotarix™: David I. Bernstein, MD, MADocument7 pagesLive Attenuated Human Rotavirus Vaccine, Rotarix™: David I. Bernstein, MD, MACagar Irwin TaufanNo ratings yet
- A 9-Valent HPV Vaccine Against Infection and Intraepithelial Neoplasia in WomenDocument13 pagesA 9-Valent HPV Vaccine Against Infection and Intraepithelial Neoplasia in WomenleticiadelfinofotosNo ratings yet
- New Generation of Vaccines Prepared Using Genetically Modified MicroorganismsDocument7 pagesNew Generation of Vaccines Prepared Using Genetically Modified MicroorganismsSyed Waseem AbbasNo ratings yet
- Ham Mitt 2019Document11 pagesHam Mitt 2019heryanggunNo ratings yet
- Fast-Tracked Swine Flu Vaccine Under FireDocument4 pagesFast-Tracked Swine Flu Vaccine Under FireaparnasingNo ratings yet
- Efficacy and Safety of A RecombinantDocument13 pagesEfficacy and Safety of A RecombinantSofyanNo ratings yet
- Identification and Construction of A Multi Epitopes Vaccine Design Against Klebsiella Aerogenes: Molecular Modeling StudyDocument16 pagesIdentification and Construction of A Multi Epitopes Vaccine Design Against Klebsiella Aerogenes: Molecular Modeling StudySamer ShamshadNo ratings yet
- Jurnal 1Document9 pagesJurnal 1Riyan TrequartistaNo ratings yet
- Vaccines of The Future Nossal2011Document5 pagesVaccines of The Future Nossal2011Dr Varshil ShahNo ratings yet
- Human Papillomavirus Vaccine Effectiveness by Age at Vaccination A Systematic ReviewDocument20 pagesHuman Papillomavirus Vaccine Effectiveness by Age at Vaccination A Systematic ReviewdeasyarchikaalvaresNo ratings yet
- Human Papillomavirus Vaccine: History, Immunology, Current Status, and Future ProspectsDocument15 pagesHuman Papillomavirus Vaccine: History, Immunology, Current Status, and Future Prospectsnohora parradoNo ratings yet
- Viral GeneticDocument10 pagesViral Geneticfirdaus.kabiruNo ratings yet
- Vaccine-Induced Anti-Hbs Level in 5-6 Year-Old Malnourished ChildrenDocument6 pagesVaccine-Induced Anti-Hbs Level in 5-6 Year-Old Malnourished ChildrenDr.Tapash Chandra GopeNo ratings yet
- 1 s2.0 S0264410X21006113 MainDocument10 pages1 s2.0 S0264410X21006113 Mainflor rodriguezNo ratings yet
- 1 s2.0 S0264410X20315875 MainDocument8 pages1 s2.0 S0264410X20315875 MainLixia WeiNo ratings yet
- Vaccines For The 21st Century: ReviewDocument13 pagesVaccines For The 21st Century: ReviewMuhafizNo ratings yet
- Malaria ResearchDocument10 pagesMalaria ResearchYosfikriansyahYosfiqarNo ratings yet
- Nesseria Gonnorhea PaperDocument5 pagesNesseria Gonnorhea PaperHina BatoolNo ratings yet
- JSRP 13710Document45 pagesJSRP 13710Laida Neti MulyaniNo ratings yet
- Geier-Geier2017 - Article - QuadrivalentHumanPapillomaviru 2023-05-24 21 - 03 - 14Document9 pagesGeier-Geier2017 - Article - QuadrivalentHumanPapillomaviru 2023-05-24 21 - 03 - 14Stephany RodriguezNo ratings yet
- Correlates of Protection Against Symptomatic and Asymptomatic Sars-Cov-2 InfectionDocument31 pagesCorrelates of Protection Against Symptomatic and Asymptomatic Sars-Cov-2 InfectionAbasyakira RaihanNo ratings yet
- 1 s2.0 S222116911530366X MainDocument10 pages1 s2.0 S222116911530366X MainNatália FreitasNo ratings yet
- Nejmoa 1817307Document12 pagesNejmoa 1817307ANA CABARCASNo ratings yet
- Nej Mo A 1706804Document12 pagesNej Mo A 1706804rizki agusmaiNo ratings yet
- MR Gambia - 9 Months - PIIS2214109X16300754Document14 pagesMR Gambia - 9 Months - PIIS2214109X16300754RIRA MABRURATINo ratings yet
- Advances in The Development of Vaccines Against Neisseria MeningitidisDocument10 pagesAdvances in The Development of Vaccines Against Neisseria MeningitidisstephaniedianNo ratings yet
- Khvi 10 12 977719Document6 pagesKhvi 10 12 977719Deby A. IrwantoNo ratings yet
- Yunnan Key 2014Document9 pagesYunnan Key 2014crpen87No ratings yet
- Varicella Post-ProphylaxisDocument2 pagesVaricella Post-ProphylaxisAngelaTrinidadNo ratings yet
- Rot A VirusDocument12 pagesRot A Viruslolada123No ratings yet
- Is Hospital Mortality Higher at Weekends? If So, Why?: CommentDocument4 pagesIs Hospital Mortality Higher at Weekends? If So, Why?: CommentRatna KusumasariNo ratings yet
- Women Who Received Varicella Vaccine Versus Natural Infection Have Different Long-Term T Cell Immunity But Similar Antibody Levels 2020Document5 pagesWomen Who Received Varicella Vaccine Versus Natural Infection Have Different Long-Term T Cell Immunity But Similar Antibody Levels 2020Mohan PrasadNo ratings yet
- A Double-Blind, Randomized, Controlled, Multi-Center Safety and Immunogenicity Study of A Refrigerator-Stable Formulation of VarivaxDocument8 pagesA Double-Blind, Randomized, Controlled, Multi-Center Safety and Immunogenicity Study of A Refrigerator-Stable Formulation of VarivaxJose Eduardo Oliva MarinNo ratings yet
- Design of A Novel Multi-EpitopDocument19 pagesDesign of A Novel Multi-EpitopDesye MeleseNo ratings yet
- DNA Vaccines: Ready For Prime Time?: Michele A. Kutzler and David B. WeinerDocument13 pagesDNA Vaccines: Ready For Prime Time?: Michele A. Kutzler and David B. WeinerantNo ratings yet
- Fase 1.2Document11 pagesFase 1.2Verliatesya TugasNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofAlmuizzu NurjannahNo ratings yet
- Piis258953702200061x PDFDocument11 pagesPiis258953702200061x PDFRong LiuNo ratings yet
- Ku Rath 2008Document22 pagesKu Rath 2008OanaNo ratings yet
- SMall InhibitorsDocument17 pagesSMall Inhibitorslaserdog97No ratings yet
- CD4 PersenDocument13 pagesCD4 Persendon lodNo ratings yet
- Good Cop, Bad Cop? Interrogating The Immune Responses To Primate Lentiviral VaccinesDocument10 pagesGood Cop, Bad Cop? Interrogating The Immune Responses To Primate Lentiviral VaccinesMuhafizNo ratings yet
- Old and New Vaccine Approaches: Ruth Arnon, Tamar Ben-YedidiaDocument10 pagesOld and New Vaccine Approaches: Ruth Arnon, Tamar Ben-YedidiahansmeetNo ratings yet
- 1 s2.0 S0264410X18308156 MainDocument8 pages1 s2.0 S0264410X18308156 MainCarlos Eduardo SchnorrNo ratings yet
- Pediatric Immunology: A Case-Based Collection with MCQs, Volume 2From EverandPediatric Immunology: A Case-Based Collection with MCQs, Volume 2No ratings yet
- Total and Acute Uterine Inversion After Delivery A Case Report PDFDocument4 pagesTotal and Acute Uterine Inversion After Delivery A Case Report PDFatika sgrtNo ratings yet
- Metabolic Precursors of SurfactantDocument8 pagesMetabolic Precursors of Surfactantatika sgrtNo ratings yet
- Cervical Insufficiency A New Issue For Guidelines On Prevention of Perinatal Group B Streptococcal DiseaseDocument6 pagesCervical Insufficiency A New Issue For Guidelines On Prevention of Perinatal Group B Streptococcal Diseaseatika sgrtNo ratings yet
- PLACENTAL LESIONS ASSOCIATED WITH MATERNAL Underperfusion Are More Frequent in Early Onset Pre EclampsiaDocument22 pagesPLACENTAL LESIONS ASSOCIATED WITH MATERNAL Underperfusion Are More Frequent in Early Onset Pre Eclampsiaatika sgrtNo ratings yet
- Preeclampsia and The Risk of Bronchopulmonary Dysplasia in VLBW Infants A Population Based StudyDocument7 pagesPreeclampsia and The Risk of Bronchopulmonary Dysplasia in VLBW Infants A Population Based Studyatika sgrtNo ratings yet
- Clinical Risk Index For Babies (CRIB II)Document4 pagesClinical Risk Index For Babies (CRIB II)atika sgrtNo ratings yet
- Research Paper On Dengue Fever in PakistanDocument6 pagesResearch Paper On Dengue Fever in Pakistangvzz4v44100% (1)
- Indian Pharma Reference Guide 2006-07Document326 pagesIndian Pharma Reference Guide 2006-07kandasani100% (4)
- Healthcare District Sales Manager in Orlando FL Resume David TarkowskiDocument3 pagesHealthcare District Sales Manager in Orlando FL Resume David Tarkowskidtarkowski1952No ratings yet
- Jammu and Kashmir Delimitation: FactoidDocument4 pagesJammu and Kashmir Delimitation: Factoidsaumya bargotiNo ratings yet
- Grip StrengthDocument11 pagesGrip StrengthMiguel Angel HermosilloNo ratings yet
- Astrology, Medicine and HealthDocument56 pagesAstrology, Medicine and HealthSoror Onyx100% (1)
- Jenkins FBI 050607 WTC PH LIES 1stFBIcomplaintDocument138 pagesJenkins FBI 050607 WTC PH LIES 1stFBIcomplaintEnviroCatNo ratings yet
- Posture and Factor Affecting Posture in Physical TherapyDocument28 pagesPosture and Factor Affecting Posture in Physical TherapyAnand Vaghasiya100% (2)
- 850 SystemDocument20 pages850 SystemandikNo ratings yet
- Ama ListDocument12 pagesAma ListSANJAY SINGHNo ratings yet
- CADOCIANDocument4 pagesCADOCIANisolomonNo ratings yet
- Clinic SystemDocument21 pagesClinic Systemmarlon_tayagNo ratings yet
- What D'Ya Know?: Epstein Stress - Management Inventory For Individuals (Esmi - I) (Abridged)Document4 pagesWhat D'Ya Know?: Epstein Stress - Management Inventory For Individuals (Esmi - I) (Abridged)Sujit Kumar RautrayNo ratings yet
- OXY-Cardio Care ManagementDocument114 pagesOXY-Cardio Care Managementlalaine22daleNo ratings yet
- Whitepaper BRCGS9 EN 2022 08 8Document12 pagesWhitepaper BRCGS9 EN 2022 08 8Heleen StoffelsNo ratings yet
- Part 1:-Safety On Workplace: Q 1) What Are The Health Hazards Mentioned inDocument5 pagesPart 1:-Safety On Workplace: Q 1) What Are The Health Hazards Mentioned inSalman AlshammariNo ratings yet
- Tracing Family Traits Using A GenogramDocument3 pagesTracing Family Traits Using A GenogramArvin VelascoNo ratings yet
- Health 8 - 3Q - 3bDocument16 pagesHealth 8 - 3Q - 3bJohnfree VallinasNo ratings yet
- Macbeth Is A Cold-Blooded Killer. DiscussDocument2 pagesMacbeth Is A Cold-Blooded Killer. DiscussSam ShohetNo ratings yet
- Sof Lex DiamondDocument2 pagesSof Lex DiamondOral CareNo ratings yet
- English ProjectDocument17 pagesEnglish ProjectPreeti TiwariNo ratings yet
- CBC-Tailoring NC IIDocument66 pagesCBC-Tailoring NC IICharmaine Mae RetizaNo ratings yet
- Noise Monitoring Register Project SiteDocument2 pagesNoise Monitoring Register Project Siteshamroz khanNo ratings yet
- Blood Gas AnalyzerDocument13 pagesBlood Gas Analyzeranon_708486566No ratings yet
- Effectiveness of Hospital Clowns For Symptom Management in Paediatrics: Systematic Review of Randomised and Non-Randomised Controlled TrialsDocument13 pagesEffectiveness of Hospital Clowns For Symptom Management in Paediatrics: Systematic Review of Randomised and Non-Randomised Controlled TrialsMarcela HincapiéNo ratings yet
- Quiz Ortho 2Document4 pagesQuiz Ortho 2alwasity167No ratings yet
- Bone Tissue EngineeringDocument352 pagesBone Tissue EngineeringKeri Gobin SamarooNo ratings yet
- My Learning Experience at Lung Center of The: PhilippinesDocument3 pagesMy Learning Experience at Lung Center of The: PhilippinesMarie Aurora Gielbert MarianoNo ratings yet