Professional Documents
Culture Documents
10 1097@01 NPR 0000508174 26163 7f
10 1097@01 NPR 0000508174 26163 7f
Uploaded by
fkCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Step by Step Ultrasound in ObstetricsDocument177 pagesStep by Step Ultrasound in ObstetricsMildred M. Montero88% (8)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Expository Essay Sample PDFDocument2 pagesExpository Essay Sample PDFloradel abanillaNo ratings yet
- Surrogacy AssignmentDocument17 pagesSurrogacy AssignmentVishal PrakashNo ratings yet
- SupernaturalDocument147 pagesSupernaturalMark Balogh89% (9)
- Disputed MaternityDocument4 pagesDisputed Maternityapi-294992872No ratings yet
- CD006476 AbstractDocument4 pagesCD006476 AbstractfkNo ratings yet
- Management For Intussusception in Children (Review) : CochraneDocument4 pagesManagement For Intussusception in Children (Review) : CochranefkNo ratings yet
- Atls Cidera KepalaDocument25 pagesAtls Cidera KepalafkNo ratings yet
- CTTN ObgynDocument9 pagesCTTN ObgynfkNo ratings yet
- Retinal Injury Following Laser Pointer Exposure: Original ArticleDocument7 pagesRetinal Injury Following Laser Pointer Exposure: Original ArticlefkNo ratings yet
- UK Hospitals Assess Eye Damage After Solar Eclipse: AbergavennyDocument1 pageUK Hospitals Assess Eye Damage After Solar Eclipse: AbergavennyfkNo ratings yet
- Testosterone and Dominance in MenDocument45 pagesTestosterone and Dominance in MenGabriel BischinNo ratings yet
- Maternity Waiting HomesDocument2 pagesMaternity Waiting HomesRicky BustosNo ratings yet
- (Neurology-Laboratory and Clinical Research Developments) Calabro Rocco Salvatore-Male Sexual Dysfunctions in Neurological Diseases From Pathophysiology To Rehabilitation (Neurology-Laboratory and CLDocument196 pages(Neurology-Laboratory and Clinical Research Developments) Calabro Rocco Salvatore-Male Sexual Dysfunctions in Neurological Diseases From Pathophysiology To Rehabilitation (Neurology-Laboratory and CLcriki_blonduNo ratings yet
- The International Index of Erectile FunctionDocument1 pageThe International Index of Erectile FunctionnnisamaliaNo ratings yet
- Agro Technique of Selected Med PlantDocument131 pagesAgro Technique of Selected Med PlantsbsatyajitNo ratings yet
- DHFHKDDocument79 pagesDHFHKDYan AringNo ratings yet
- Sexual Fertility EssenceDocument17 pagesSexual Fertility EssenceNadezdaNo ratings yet
- UntitledDocument8 pagesUntitledPJ Manuel SuerteNo ratings yet
- Ellenbogen 2020Document17 pagesEllenbogen 2020MD LarasatiNo ratings yet
- Steroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanDocument23 pagesSteroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanMichaela Vania TanujayaNo ratings yet
- Bio Infertility Before Final PDFDocument31 pagesBio Infertility Before Final PDFmanojkumar200624No ratings yet
- Bleeding and Pain in Early Pregnancy - RCOG PDFDocument4 pagesBleeding and Pain in Early Pregnancy - RCOG PDFSyandri Agus RizkyNo ratings yet
- Region 7Document14 pagesRegion 7Estrella CaingalNo ratings yet
- FungiDocument10 pagesFungiRadhakrishnan SenthilkumarNo ratings yet
- OB-GYN - MCQ - 2012 - 5th-Year - Mu - TahDocument16 pagesOB-GYN - MCQ - 2012 - 5th-Year - Mu - TahHalah100% (2)
- Lesson Plan in Health 7 CSEDocument5 pagesLesson Plan in Health 7 CSEMiriam Ebora GatdulaNo ratings yet
- Structural Organisation in AnimalsDocument19 pagesStructural Organisation in AnimalsBiju Mylachal100% (1)
- Male and Female Reproductive SystemDocument4 pagesMale and Female Reproductive SystemcorpuzxyleneyaraNo ratings yet
- Commercial Surrogacy Project 5Document29 pagesCommercial Surrogacy Project 5farazNo ratings yet
- Honey Bee Pheromone I PNDocument8 pagesHoney Bee Pheromone I PNRizki ArismawatiNo ratings yet
- How Many Days Does A Butterfly Stay in Its CocoonDocument6 pagesHow Many Days Does A Butterfly Stay in Its CocoonMaricar RaciramNo ratings yet
- Birth Weight For Gestational Age (GA) : Male SingletonsDocument4 pagesBirth Weight For Gestational Age (GA) : Male Singletonsstrawberry pieNo ratings yet
- Revision Long Case Obs GynaeDocument10 pagesRevision Long Case Obs GynaeHo Yong WaiNo ratings yet
- Ncert Solutions For Class 8 March 31 Science Chapter 10 Reaching The Age of AdolescenceDocument6 pagesNcert Solutions For Class 8 March 31 Science Chapter 10 Reaching The Age of Adolescencekanchansharma7840No ratings yet
- Bleeding in Late PregnancyDocument39 pagesBleeding in Late PregnancyAhmed ElryahNo ratings yet
10 1097@01 NPR 0000508174 26163 7f
10 1097@01 NPR 0000508174 26163 7f
Uploaded by
fkOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1097@01 NPR 0000508174 26163 7f
10 1097@01 NPR 0000508174 26163 7f
Uploaded by
fkCopyright:
Available Formats
Primary care management
of women with persistent
vaginal discharge
Abstract: Vaginal discharge is a common complaint managed by NPs in ambulatory
settings. This article reviews noninfectious etiologies of vaginal discharge with diagnostic
criteria and recommended treatment to aid the NP in correctly managing these patients.
By Hilary S. Morgan, PhD, CNM
Ps see a variety of common primary care com- a withdrawal from intimate relationships.6-8 The NP must
N plaints. In women’s health, vaginal symptoms—
specifically vaginal discharge with or without
recognize other, noninfectious causes of vaginal discharge
and diagnose and treat the patient appropriately. If the NP
accompanying pruritus and odor—account for 10% of office cannot relieve the patient of her symptoms, a referral to a
visits.1 Most often, the patient is diagnosed with a vaginal gynecologic specialist is warranted.
infection, such as vulvovaginal candidiasis, bacterial vagino-
sis, or trichomoniasis. These infections account for over 75% ■ Normal vaginal flora
of vaginitis complaints, with vulvovaginal candidiasis and Women of reproductive age have vaginal flora that consists
bacterial vaginosis causing up to 90% of vaginal infections.2,3 predominately of lactobacillus, a Gram-positive rod that
Appropriate diagnosis and treatment result in symptom produces lactic acid from glucose and contributes to a nor-
relief for patients; however, up to 30% of women remain mal vaginal pH between 4.0 and 4.7.5,9 The acidity of the
without a diagnosis after workup and may receive an inap- vagina protects it from pathogens.10 After menarche, estro-
propriate treatment just to placate them.4 Not surprisingly, gen aids in the deposit of glycogen in the vaginal epithelial
these women continue to seek a diagnosis from different cells, which in turn converts the glycogen to glucose. The
providers or chose to self-medicate with over-the-counter lactobacillus then converts the glucose to lactic acid.9
(OTC) medications in an attempt to find a cure, increasing A thickening of the vaginal mucosa also occurs with
the cost to themselves and the healthcare system. The failure puberty due to the influence of estrogen.11 As women age,
to appropriately treat may also aggravate symptoms rather estrogen levels decline, resulting in a higher vaginal pH (over
than alleviate them.5 4.7). There is less glycogen in the epithelial cells and fewer
Additionally, the chronic nature of persistent vaginal lactobacilli present to convert the glucose to lactic acid,
discharge may impact a woman’s psychosocial health. resulting in less lactic acid production and a higher vaginal
Women may view vaginal complaints as a threat to their pH.5,11 Additionally, the loss of estrogen leads to vaginal
reproductive health, which may lead to poor self-image and atrophy and thinning.8
Keywords: atrophic vaginitis, bacterial vaginosis, desquamative inflammatory vaginitis, genitourinary syndrome of menopause, lichen planus,
lichen sclerosus, persistent vaginal discharge, trichomoniasis, vaginal discharge, vulvovaginal candidiasis
1 The Nurse Practitioner Copyright © 2016 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved.
Primary care management of women with persistent vaginal discharge
It is normal for women to have a physiologic vaginal is more likely indicative of reinfection, whereas a woman
discharge. The endocervix produces mucus, which combines with chronic symptoms not relieved with previous treatment
with epithelial sloughing, normal vaginal flora, and transudate should lead the NP to suspect inflammation unrelated to
to produce a vaginal discharge.2 This discharge is considered infectious process (see Evaluation of vaginal discharge by pH
part of a self-cleansing mechanism in a woman’s vagina and measurement).14 The timing of the symptoms in relation to
varies throughout the menstrual cycle due to effects of estro- the menstrual cycle may also yield clues, as a heavier dis-
gen and progesterone. The consistency of vaginal discharge charge is noted at ovulation.
is clear and stretchy during ovulation and thick, white, and Other symptoms, such as vulvovaginal burning and
tacky during the remainder of the cycle.5,12 The amount of pruritus, bleeding, dysuria, or dyspareunia may provide
vaginal discharge produced varies among women but averages information.5,15 The NP should ask if there are other associ-
approximately 1 mL to 4 mL fluid per 24 hours.2 ated symptoms, such as fever, nausea, vomiting, and pelvic
pain, which may indicate a more systemic issue. The sever-
■ Patient history ity of the complaints should be elicited as well as any aggra-
A detailed history is paramount if the NP is to succeed in vating or alleviating factors. Any history of sexually
correctly diagnosing women complaining of persistent transmitted infections and use of any type of contraceptives
vaginal discharge. Although the NP may consider a patient should also be obtained.
presenting with a complaint of vaginal discharge a problem- The woman’s sexual history must also be gathered,
focused visit, a thorough history (including medical and including if she is having sex with men, women, or both,
surgical history, reproductive and menstrual history, and and if they are stable or new partners. Women who have sex
nutritional history) may provide important information with women are at an increased risk of bacterial vagino-
aiding in diagnosis. The NP should keep in mind that sis.16,17 Although rare, allergy to semen has been noted, but
although some patients may be of reproductive age, there the symptoms are usually irritative rather than vaginal dis-
are medical conditions and treatments that inhibit normal charge.18 The NP should also inquire if the woman’s symp-
ovarian function, including surgical removal of the ovaries toms are noted by her partner as well.
and medications used to treat endometriosis, such as leup- It is also important to ask about any medications, both
rolide acetate.13 The NP needs to carefully avoid assumptions prescription and OTC. Recent intake of antibiotics may
based on a woman’s age. make a woman susceptible to vulvovaginal candidiasis, and
It is important to know if the woman’s symptoms are contraceptives containing estrogen may contribute to a
recent or chronic or if she has been treated successfully in heavier vaginal discharge.19 Antihistamines may cause vag-
the past and now the symptoms have recurred. Recurrence inal dryness.20 Women who use an intrauterine device for
contraception may also note a heavier discharge.21
Lastly, the woman’s hygienic practices must be evaluated.
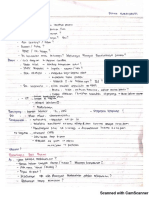
Evaluation of vaginal discharge by Vaginal tissue is very sensitive to chemicals and allergens,
pH measurement14 and the use of products such as perfumed soaps and douches,
scented panty liners, spermicides, latex condoms, and topi-
Process Vaginal pH <4.7 Vaginal pH ≥4.7
cal lotions may cause inflammation that contributes to
Infectious • Vulvovaginal • Bacterial
vaginal discharge.22 Shared use of sex toys between partners
candidiasis vaginosis
• Trichomoniasis • Trichomoniasis without adequate cleaning between use may also be a con-
(varies) (usually elevates tributing factor.17
pH but varies)*
Noninfectious • Normal flora • Genitourinary ■ Physical exam and diagnostic testing
• Physiologic syndrome of Although it is common to diagnose a patient with a vaginal
leukorrhea menopause
• Vulvar • Desquamative
infection based on history, a speculum exam should be done
dermatitis inflammatory in women with persistent vaginal discharge. A diagnosis
• Cytolytic vaginitis based solely on history is strongly discouraged. Normal
vaginosis • Lichen planus or vaginal discharge in women with functioning ovaries or who
lichen sclerosus
are receiving estrogen supplementation is white or clear and
*Trichomoniasis generally causes elevation of vaginal pH but due to limited odorless.2 The speculum exam allows the NP to see the color,
specificity of pH paper, this result may vary.
consistency, and amount of the vaginal discharge. A thorough
2 The Nurse Practitioner Copyright © 2016 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved.
Primary care management of women with persistent vaginal discharge
exam of the mons, vulva, perineum, vaginal canal, cervix, consider noninfectious causes of persistent vaginal dis-
and cervical os should be performed along with palpation charge. Again, pH findings may be helpful. An elevated pH
of the urethra and the Bartholin and Skene glands. may indicate genitourinary syndrome of menopause (the
Inspection for retained foreign bodies, the presence of more recent terminology for atrophic vaginitis and vulvo-
lesions, skin disorders, atrophy, and other signs of irritation vaginal atrophy), lichen planus, lichen sclerosus, or desqua-
should be done and managed by the NP. The NP should mative inflammatory vaginitis. A normal vaginal pH with
note any unusual or foul odors. A bimanual exam assessing negative diagnostic testing suggests physiologic leukorrhea
for cervical motion tenderness, uterine size, consistency and or vulvar dermatitis. A low vaginal pH may point toward
tenderness, adnexal tenderness, and the presence of any cytolytic vaginosis.2,5
masses should be performed. Physiologic leukorrhea. Many women, particularly those
of younger reproductive age, may not realize the cyclic
■ pH testing and microscopy variation in vaginal discharge. It is important to educate
The value of measuring the vaginal pH to help achieve diag- them that all women will have some vaginal discharge.
nosis cannot be overemphasized. Several commercial options Physiologic leukorrhea refers to the normal increased pro-
are available to the NP to obtain vaginal pH results. These duction of discharge that occurs during ovulation and preg-
products utilize nitrazine dye either on a swab or as paper nancy. Physiologic leukorrhea may also be influenced by
that changes color in contact with an elevated vaginal pH. diet, sexual activity, medications, hormonal contraception,
No change in color occurs if the vaginal pH is normal. If a and stress. A vaginal discharge that is mostly clear, odorless,
color change occurs, compare the pH paper to the color chart without accompanied erythema and significant irritative
supplied with the pH paper. These tests are easily performed symptoms, and has a pH under 4.7 is generally considered
and done at the point of care with the patient. The sensitiv- benign.2 Physiologic leukorrhea was diagnosed in 9% of
ity and specificity of the swab in diagnosing bacterial vagi- women in a prospective analysis of affected women.26
nosis and trichomoniasis based on elevated pH results is Cytolytic vaginosis. Also known as Döderlein’s cytolysis,
82.3% and 94.2%, respectively; the sensitivity and specificity cytolytic vaginosis is characterized by an overgrowth of
of the pH paper is 91.1% and 94.2%.23 An elevated vaginal lactobacillus.7 The overabundance of lactobacillus leads to
pH in a reproductive-age woman (pH over 4.7) is associated vaginal hyperacidity, which damages the vaginal epithelial
with bacterial vaginosis or trichomoniasis. Candida vulvo- cells and increases vaginal discharge. According to Cibley
vaginitis will typically have a vaginal pH between 4 and 4.5.5,24 and Cibley, diagnostic criteria include the absence of tricho-
The use of microscopy in diagnosing vaginal discharge monas, monilia and bacteria on microscopy, an increase of
consists primarily of saline and potassium hydroxide (KOH) lactobacilli, rare white blood cells, evidence of cytolysis, and
wet mounts, and identification of causative organism. the presence of vaginal discharge with pH between 3.5 and
Trichomonads and clue cells may be seen under the micro- 4.5.27 Cytolytic vaginosis occurs more commonly during the
scope using the saline mount, whereas hyphae and buds luteal phase of a women’s menstrual cycle.27
indicative of candidiasis are noted with KOH. The amine Cerikcioglu and Beksac tested 210 women with com-
test (whiff test) is also helpful in diagnosing bacterial vagi- plaints of vaginal discharge and other symptoms suggestive
nosis and involves mixing vaginal discharge with KOH and of vulvovaginal candidiasis and diagnosed 7.1% with cyto-
evaluating for the presence of a fishy odor.2 lytic vaginosis based on lab findings. Patients diagnosed
Amsel criteria for the diagnosis of bacterial vaginosis with cytolytic vaginosis were found to have abundant lac-
include a vaginal pH over 4.5, a positive whiff test, milky tobacilli, fragmented epithelial cells, and free nuclei due to
discharge, and the presence of clue cells on microscopy.25 cytolysis. Additionally, no fungal growth was identified
Many NPs prefer submitting specimens for vaginal or cervi- microscopically in these women.28 These findings were con-
cal cultures to a lab to aid in identifying pathology.2 Infection firmed in another study by Hu and colleagues, which com-
with Neisseria gonorrhoeae or Chlamydia trachomatis should pared the morphologic characteristics of vaginal discharge
be ruled out. of patients diagnosed with cytolytic vaginosis and vulvo-
vaginal candidiasis.29
■ Noninfectious conditions The treatment for cytolytic vaginosis involves restoring
Careful assessment and diagnostic testing will likely provide the vaginal pH to normal levels through the use of sodium
a diagnosis if the vaginal discharge is due to an infectious bicarbonate suppositories. Patients may prepare the appro-
cause. If testing does not provide a diagnosis, the NP should priate treatment by filling empty gelatin capsules with
3 The Nurse Practitioner Copyright © 2016 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved.
Primary care management of women with persistent vaginal discharge
baking soda and inserting the capsules in their vagina twice ing comes up negative, the NP should consider treating the
a week for 2 weeks.9 Gelatin capsules may be purchased woman with estrogen vaginal products. The results may take
inexpensively at local pharmacies. Patients should experi- a few months to demonstrate but most women will find
ence symptom relief within 2 to 3 weeks.9 their vaginal discharge lessens after use of vaginal estrogen
Retained foreign body. Women of all ages, particularly products.31 Low-dose vaginal estrogen can be highly effective
younger women of reproductive age, may inadvertently leave in treating genitourinary conditions related to estrogen
a tampon in their vagina for a prolonged period of time, deficiency (provided there are no contraindications to its
and this irritation may lead to a heavy discharge (usually use). Contraindications include history of breast, ovarian,
with odor). Surgical gauze has also been removed from or uterine cancer; undiagnosed vaginal bleeding; pregnancy
women returning for their postpartum or postgynecologic or lactation; thromboembolic disorders; or impaired liver
surgery exam. In both situations, removing the foreign body function.33
removes the irritant, and the resulting discharge resolves Estrogen deficiency may also occur in premenopausal
fairly quickly. Some NPs prefer to treat the patient with women, particularly during the postpartum period and while
vaginal antibiotic cream, although the evidence is not clear lactating. Additionally, contraceptives containing low or no
that this is necessary.30 estrogen amounts such as depot medroxyprogesterone acetate
Vulvar contact dermatitis. A study by Nyirjesy and col- may contribute to a lower vaginal estrogen level, production
leagues identified contact dermatitis as a leading cause of less lactic acid, and a higher vaginal pH.24,31,34,35 In this case,
(21%) of vaginal vulvar complaints.26 Contact dermatitis the NP may need to consider an alternative contraceptive
may be either due to irritants or allergens. Severe outbreaks option. Postpartum and lactating women should be educated
may be painful and associated with erosion and lesions, that their condition is self-limiting and once lactation is
whereas milder cases may present with erythema and irrita- discontinued, estrogen levels will return to normal.
tion. Chronic dermatitis may present as eczema with dry, Lichen planus and lichen sclerosus. These dermatologic
scaly patches and lichenification of tissue. The primary conditions are caused by chronic inflammation. Lichen
symptoms in both types of contact dermatitis include itch- planus is a cell-mediated immune response disease that usu-
ing, erythema, edema, and weeping from vulvar lesions may ally affects cutaneous areas, such as the vulva and vagina,
be present. The vaginal pH is typically under 4.7.22,31 and the oral and esophagus regions.36,37 It is considered an
Soaps, laundry detergent, sanitary products, toilet tissue, autoimmune disorder, although no defining antigen has been
and powders are all potential sources of irritation. Treatment identified. Lichen planus is characterized by either erosive
involves avoidance of known irritants, changing personal or papular lesions on the vulva; a friable vaginal epithelium
hygiene practices, and avoiding tight-fitting clothing. Med- may be noted as well as loss of vaginal architecture.
ication such as antihistamines and corticosteroids may be Pain is the most common complaint, but an irritating
necessary to relieve inflammation.31 NP management may vaginal discharge may also be noted. Microscopy will reveal
include identifying causative exposure and inflammation a marked increase in white blood cells, immature epithelial
treatment. Additionally, patient education on avoidance of cells (arising from erosive areas), an elevated vaginal pH,
identified irritating exposures is imperative to avoid reoc- and an absence of lactobacilli.36 Lichen planus is most com-
currence. Referral to a gynecologic specialist for biopsy and/ monly seen in women ages 50 to 60, and diagnosis is
or cultures may be necessary. achieved through biopsy. Treatment is difficult and usually
Estrogen deficiency. As women age, estrogen levels involves topical corticosteroids.37
decrease, and the vagina becomes atrophic. Estrogen is no Like lichen planus, lichen sclerosus is considered an
longer present at high enough levels to keep the vagina well autoimmune disorder without a specifically identified caus-
epithelialized and elastic. Over time, the vaginal tissue thins, ative antigen. Lichen sclerosus primarily affects the ano-
dries, and may become inflamed. With a decline in glycogen genital area, and although it shares characteristics with
levels, lactic acid production is diminished and the vaginal lichen planus, the two are different diseases. Genetic and
pH rises, usually over 5.32 environmental factors are hypothesized to contribute to the
The vaginal tissue is more easily traumatized and sus- development of lichen sclerosus; additionally, periods of low
ceptible to infection and inflammation. Even without a estrogen are also thought to play a role.38,39 Recent studies
source of infection, this inflammatory process results in an have suggested the use of oral contraceptives having anti-
increased discharge that often both the patient and NP believe androgenic properties that might trigger an early onset of
may be the result of a pathogen. However, if diagnostic test- lichen sclerosus in young women.38
4 The Nurse Practitioner Copyright © 2016 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved.
Primary care management of women with persistent vaginal discharge
Lichen sclerosus primarily affects women ages 50 to 70, cream, intravaginally for a period of 4 to 6 weeks until the
but children may be affected as well. Lichen sclerosus is signs and symptoms are in remission.42 If the NP suspects
characterized by intractable pruritus and burning that wors- desquamative inflammatory vaginitis, it maybe treated in
ens at night. The vulvar skin becomes thin (although some- the primary care setting, but if there is no relief of symptoms
times thickened) and is often accompanied by white plaques. after 2 months, referral to a gynecologic specialist is advised.
Progressive scratching and development of tissue adhesions
may lead to occlusion of the introitus. The vaginal tissue ■ Patient education
may lose its elasticity, resulting in tears and erosion and Patients must be instructed that often, a medical diagnosis
contributes to a vaginal discharge. Diagnosis is via exam, is achieved through an elimination process, and if the symp-
and biopsy and treatment, like lichen planus, also entail toms do not improve within a specified period of time, the
topical corticosteroids.38,39 patient needs to return to the same provider. Too often,
Early identification and diagnosis of lichen planus and patients who are not cured on initial visit feel they have not
lichen sclerosus are crucial to preserving vaginal structure been cared for appropriately and present to a different pro-
and integrity. Lichen planus and lichen sclerosus may be vider seeking answers, and the investigative process and
missed if a pelvic exam is not performed on a patient com- treatment begins again. Patients must be educated that
plaining of vaginal discharge. NPs who identify signs of follow-up care with the same provider is imperative to arrive
lichen planus and lichen sclerosus should not hesitate to at a correct diagnosis.
refer the patient to a gynecologic specialist for evaluation. Vaginal discharge in women may be due to a variety of
Granulation tissue. The presence of persistent granula- both infectious and noninfectious causes. Do not assume
tion tissue following gynecologic surgery has also been that the patient has the common infectious causes of
identified as a cause of vaginal discharge. A recent review vaginal discharge, such as vulvovaginal candidiasis, bacterial
found persistent granulation tissue occurred in 19% of vaginosis, or trichomoniasis. Treating a patient for a condi-
postoperative cases for vaginal prolapse repair.40 Although tion she does not have may exacerbate the symptoms and
more likely to cause vaginal spotting, discharge may also lead to frustration. The NP must take a careful history,
occur. The presence of blood in the vaginal vault may con- perform a thorough physical exam, and necessary diagnos-
tribute to a vaginal pH of 4.7 or higher. If the patient has tic testing before deciding on a course of action. Once
had gynecologic surgery within the past year, a careful vaginal infections have been ruled out, consider noninfec-
inspection of the vulva, perineum, vagina, cervix, and/or tious causes of vaginal discharge.
vaginal cuff is warranted. If the bleeding or discharge is
found to originate from granulation tissue, treatment with REFERENCES
application of silver nitrate may be beneficial, although in 1. Quan M. Vaginitis: diagnosis and management. Postgrad Med. 2010;122(6):
117-127.
some cases, repeat surgery intervention is required.41
2. Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA.
Desquamative inflammatory vaginitis. Although a rare 2004;291(11):1368-1379.
diagnosis, desquamative inflammatory vaginitis should be 3. Sobel JD, Hay P. Diagnostic techniques for bacterial vaginosis and vulvovagi-
considered as a possible cause of vaginal discharge, particu- nal candidiasis – requirement for a simple differential test. Expert Opin Med
Diagn. 2010;4(4):333-341.
larly in perimenopausal women. It is characterized by pro- 4. Nyirjesy P, Leigh RD, Mathew L, Lev-Sagie A, Culhane JF. Chronic vulvovagini-
fuse vaginal discharge accompanied by vaginal pain and tis in women older than 50 years: analysis of a prospective database. J Low
Genit Tract Dis. 2012;16(1):24-29.
inflammation. Vaginal exam reveals ecchymotic rash, ery-
5. Nyirjesy P. Management of persistent vaginitis. Obstet Gynecol. 2014;124(6):
thema, and erosion. Microscopy does not identify a causative 1135-1144.
agent; however, the vaginal pH is increased (over 4.7), and 6. Karasz A, Anderson M. The vaginitis monologues: women’s experiences of
vaginal flora is marked by an absence of lactobacilli. Unlike vaginal complaints in a primary care setting. Soc Sci Med. 2003;56(5):1013-
1021.
with vaginal atrophy, the vaginal structure with desquama- 7. Patel V, Pednekar S, Weiss H, et al. Why do women complain of vaginal
tive inflammatory vaginitis is maintained.41 discharge? A population survey of infectious and psychosocial risk factors in
a South Asian community. Int J Epidemiol. 2005;34(4):853-862.
However, vaginal atrophy and desquamative inflamma-
8. Bilardi JE, Walker S, Temple-Smith M, et al. The burden of bacterial vaginosis:
tory vaginitis are often confused. Treatment with estrogen women’s experience of the physical, emotional, sexual and social impact of
products does not alleviate symptoms with desquamative living with recurrent bacterial vaginosis. PLOS One. 2013;8(9):e74378.
inflammatory vaginitis.40 Instead, the treatment of desqua- 9. Suresh A, Rajesh A, Bhat RM, Rai Y. Cytolytic vaginosis: a review. Indian J Sex
Transm Dis. 2009;30(1):48-50.
mative inflammatory vaginitis involves use of a vaginal 10. Bowen-Simpkins P. Which patients with vaginal discharge should be
antibiotic cream, such as clindamycin and/or hydrocortisone referred? Practitioner. 2008;252(1704):18,21-22,24.
5 The Nurse Practitioner Copyright © 2016 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved.
Primary care management of women with persistent vaginal discharge
11. Parma M, Stella Vanni V, Bertini M, Candiani M. Probiotics in the 29. Hu Z, Zhou W, Mu L, Kuang L, Su M, Jiang Y. Identification of cytolytic
prevention of recurrences of bacterial vaginosis. Altern Ther Health Med. vaginosis versus vulvovaginal candidiasis. J Low Genit Tract Dis.
2014;20(suppl 1):52-57. 2015;19(2):152-155.
12. Larsen B, Monif GR. Understanding the bacterial flora of the female genital 30. Cernat G, Leung L. Odorous vaginal discharge: a case study for thorough
tract. Clin Infect Dis. 2001;32(4):e69-e77. investigation. Aust Fam Physician. 2011;40(8):611-613.
13. Rebar RW. Premature ovarian failure. Obstet Gynecol. 2009;113(6):1355-1363. 31. Schlosser BJ. Contact dermatitis of the vulva. Dermatol Clin. 2010;28(4):
14. Centers for Disease Control and Prevention. 2015 Sexually Transmitted Disease 697-706.
Treatment Guidelines. www.cdc.gov/std/tg2015/vaginal-discharge.htm. 32. Richardson MK. What can I do about chronic leukorrhea? Harv Womens
15. Fischer G, Bradford J. Persistent vaginitis. Br Med J. 2011;343:1169-1173. Health Watch. 2010. www.health.harvard.edu.
16. Evans AL, Scally AJ, Wellard SJ, Wilson JD. Prevalence of bacterial vaginosis 33. Reimer A, Johnson L. Atrophic vaginitis: signs, symptoms, and better
in lesbians and heterosexual women in a community setting. Sex Transm outcomes. Nurse Pract. 2011;36(1):22-28.
Infect. 2007;83(6):470-475. 34. Domoney C. Treatment of vaginal atrophy. Womens Health (Lond). 2014;
17. Marrazzo JM, Coffey P, Bingham A. Sexual practices, risk perception and 10(2):191-200.
knowledge of sexually transmitted disease risk among lesbian and bisexual 35. Spevack E. The long-term health implication of Depo-Provera. Integr Med.
women. Perspect Sex Reprod Health. 2005;37(1):6-12. 2013;12(1):27-34.
18. Carroll M, Horne G, Antrobus R, Fitzgerald C, Brison D, Helbert M. Testing 36. Mirowski GW, Goddard A. Treatment of vulvovaginal lichen planus.
for hypersensitivity to seminal fluid-free spermatozoa. Hum Fertil (Camb). Dermatol Clin. 2010;28(4):717-725.
2013;16(2):128-131.
37. Santegoets LA, Helmerhorst TJ, van der Meijden WI. A retrospective study
19. Berry M. Vaginal infections: an overview. Pharm Pract. 2005;21(9):S1-S8. of 95 women with a clinical diagnosis of genital lichen planus. J Low Genit
20. Bond S, Horton LS. Management of postmenopausal vaginal symptoms in Tract Dis. 2010;14(4):323-328.
women. J Gerontol Nurs. 2010;36(7):3-7. 38. Murphy R. Lichen sclerosus. Dermatol Clin. 2010;28(4):707-715.
21. Neale R, Knight I, Keane F. Do users of the intrauterine system (Mirena) 39. Wehbe-Alamah H, Kornblau BL, Haderer J, Erickson J. Silent no more! The
have different genital symptoms and vaginal flora than users of the lived experiences of women with lichen sclerosus. J Am Acad Nurse Pract.
intrauterine contraceptive device? Int J STD AIDS. 2009;20(6):423-424. 2012;24(8):499-505.
22. Connor CJ, Eppsteiner EE. Vulvar contact dermatitis. Proc Obstet Gynecol. 40. Mahal A, Zhang T, Zimmerman MB, Luck A, Bradley CS. Persistent
2014;4(2):1-14. postoperative granulation tissue following vaginal prolapse repair. Proc
23. Sobel JD, Nyirjesy P, Kessary H, Ferris DG. Use of the VS-sense swab in diag- Obstet Gynecol. 2013;3(3):12-13.
nosing vulvovaginitis. J Womens Health (Larchmt). 2009;18(9):1467-1470. 41. Steinberg BJ, Mapp T, Mama S, Echols KT. Surgical treatment of persistent
24. Mania-Pramanik J, Kerkar SC, Mehta PB, Potdar S, Salvi VS. Use of vaginal vaginal granulation tissue using CO(2) laser vaporization under
pH in diagnosis of infections and its association with reproductive colposcopic and laparoscopic guidance. JSLS. 2012;16(3):488-491.
manifestations. J Clin Lab Anal. 2008;22(5):375-379. 42. Sobel JD, Reichman O, Misra D, Yoo W. Prognosis and treatment of
25. Hainer BL, Gibson MV. Vaginitis. Am Fam Physician. 2011;83(7):807-815. desquamative inflammatory vaginitis. Obstet Gynecol. 2011;117(4):350.
26. Nyirjesy P, Peyton C, Weitz MV, Mathew L, Culhane JF. Causes of chronic
vaginitis: analysis of a prospective database of affected women. Obstet Hilary S. Morgan is an assistant professor at Jacksonville University,
Gynecol. 2006;108(5):1185-1191. Jacksonville, Fla.
27. Cibley LJ, Cibley LJ. Cytolytic vaginosis. Am J Obstet Gynecol. 1991;165(4 Pt The author has disclosed that she has no financial relationships related to this
2):1245. article.
28. Cerikcioglu N, Beksac MS. Cytolytic vaginosis: misdiagnosed as candidal
vaginitis. Infect Dis Obstet Gynecol. 2004;12(1):13. DOI-10.1097/01.NPR.0000508174.26163.7f
6 The Nurse Practitioner Copyright © 2016 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Step by Step Ultrasound in ObstetricsDocument177 pagesStep by Step Ultrasound in ObstetricsMildred M. Montero88% (8)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Expository Essay Sample PDFDocument2 pagesExpository Essay Sample PDFloradel abanillaNo ratings yet
- Surrogacy AssignmentDocument17 pagesSurrogacy AssignmentVishal PrakashNo ratings yet
- SupernaturalDocument147 pagesSupernaturalMark Balogh89% (9)
- Disputed MaternityDocument4 pagesDisputed Maternityapi-294992872No ratings yet
- CD006476 AbstractDocument4 pagesCD006476 AbstractfkNo ratings yet
- Management For Intussusception in Children (Review) : CochraneDocument4 pagesManagement For Intussusception in Children (Review) : CochranefkNo ratings yet
- Atls Cidera KepalaDocument25 pagesAtls Cidera KepalafkNo ratings yet
- CTTN ObgynDocument9 pagesCTTN ObgynfkNo ratings yet
- Retinal Injury Following Laser Pointer Exposure: Original ArticleDocument7 pagesRetinal Injury Following Laser Pointer Exposure: Original ArticlefkNo ratings yet
- UK Hospitals Assess Eye Damage After Solar Eclipse: AbergavennyDocument1 pageUK Hospitals Assess Eye Damage After Solar Eclipse: AbergavennyfkNo ratings yet
- Testosterone and Dominance in MenDocument45 pagesTestosterone and Dominance in MenGabriel BischinNo ratings yet
- Maternity Waiting HomesDocument2 pagesMaternity Waiting HomesRicky BustosNo ratings yet
- (Neurology-Laboratory and Clinical Research Developments) Calabro Rocco Salvatore-Male Sexual Dysfunctions in Neurological Diseases From Pathophysiology To Rehabilitation (Neurology-Laboratory and CLDocument196 pages(Neurology-Laboratory and Clinical Research Developments) Calabro Rocco Salvatore-Male Sexual Dysfunctions in Neurological Diseases From Pathophysiology To Rehabilitation (Neurology-Laboratory and CLcriki_blonduNo ratings yet
- The International Index of Erectile FunctionDocument1 pageThe International Index of Erectile FunctionnnisamaliaNo ratings yet
- Agro Technique of Selected Med PlantDocument131 pagesAgro Technique of Selected Med PlantsbsatyajitNo ratings yet
- DHFHKDDocument79 pagesDHFHKDYan AringNo ratings yet
- Sexual Fertility EssenceDocument17 pagesSexual Fertility EssenceNadezdaNo ratings yet
- UntitledDocument8 pagesUntitledPJ Manuel SuerteNo ratings yet
- Ellenbogen 2020Document17 pagesEllenbogen 2020MD LarasatiNo ratings yet
- Steroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanDocument23 pagesSteroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanMichaela Vania TanujayaNo ratings yet
- Bio Infertility Before Final PDFDocument31 pagesBio Infertility Before Final PDFmanojkumar200624No ratings yet
- Bleeding and Pain in Early Pregnancy - RCOG PDFDocument4 pagesBleeding and Pain in Early Pregnancy - RCOG PDFSyandri Agus RizkyNo ratings yet
- Region 7Document14 pagesRegion 7Estrella CaingalNo ratings yet
- FungiDocument10 pagesFungiRadhakrishnan SenthilkumarNo ratings yet
- OB-GYN - MCQ - 2012 - 5th-Year - Mu - TahDocument16 pagesOB-GYN - MCQ - 2012 - 5th-Year - Mu - TahHalah100% (2)
- Lesson Plan in Health 7 CSEDocument5 pagesLesson Plan in Health 7 CSEMiriam Ebora GatdulaNo ratings yet
- Structural Organisation in AnimalsDocument19 pagesStructural Organisation in AnimalsBiju Mylachal100% (1)
- Male and Female Reproductive SystemDocument4 pagesMale and Female Reproductive SystemcorpuzxyleneyaraNo ratings yet
- Commercial Surrogacy Project 5Document29 pagesCommercial Surrogacy Project 5farazNo ratings yet
- Honey Bee Pheromone I PNDocument8 pagesHoney Bee Pheromone I PNRizki ArismawatiNo ratings yet
- How Many Days Does A Butterfly Stay in Its CocoonDocument6 pagesHow Many Days Does A Butterfly Stay in Its CocoonMaricar RaciramNo ratings yet
- Birth Weight For Gestational Age (GA) : Male SingletonsDocument4 pagesBirth Weight For Gestational Age (GA) : Male Singletonsstrawberry pieNo ratings yet
- Revision Long Case Obs GynaeDocument10 pagesRevision Long Case Obs GynaeHo Yong WaiNo ratings yet
- Ncert Solutions For Class 8 March 31 Science Chapter 10 Reaching The Age of AdolescenceDocument6 pagesNcert Solutions For Class 8 March 31 Science Chapter 10 Reaching The Age of Adolescencekanchansharma7840No ratings yet
- Bleeding in Late PregnancyDocument39 pagesBleeding in Late PregnancyAhmed ElryahNo ratings yet