Professional Documents
Culture Documents
Westermann 2004 2 PDF
Westermann 2004 2 PDF
Uploaded by
fissionmailedCopyright:
Available Formats
You might also like
- Cardiology - Internal Medicine, Dr. A. Mowafy (2020-2021)Document202 pagesCardiology - Internal Medicine, Dr. A. Mowafy (2020-2021)NADER ELSAYED AHMED100% (1)
- Drip ChartDocument10 pagesDrip Chartmirzaocta100% (1)
- Pone 0032496 PDFDocument7 pagesPone 0032496 PDFGeaakmalokaNo ratings yet
- Antinuclear Antibodies by Indirect Immunofluorescence: Optimum Screening Dilution For Diagnosis of Systemic Lupus ErythematosusDocument5 pagesAntinuclear Antibodies by Indirect Immunofluorescence: Optimum Screening Dilution For Diagnosis of Systemic Lupus ErythematosusMargriet MayasinNo ratings yet
- S Venner Holm 1964Document17 pagesS Venner Holm 1964vsvsuresh2099No ratings yet
- The Accuracy of Serum Osmolarity Calculation in Small Children Ta Nost Izra Unavanja Serumskog Osmolariteta U Male DeceDocument11 pagesThe Accuracy of Serum Osmolarity Calculation in Small Children Ta Nost Izra Unavanja Serumskog Osmolariteta U Male DeceMilica AdzibabaNo ratings yet
- Description of Reference Ranges for Organic Acids in Urine مهمDocument11 pagesDescription of Reference Ranges for Organic Acids in Urine مهمfarkad rawiNo ratings yet
- AN 625 LC MS Steroids Plasma AN64333 ENDocument6 pagesAN 625 LC MS Steroids Plasma AN64333 ENVeronica Weber-DragonNo ratings yet
- Estron SulfatDocument7 pagesEstron SulfatMiswar KospalaNo ratings yet
- HPLC Method For Pharmacokinetics of Cis and Trans Isomer of Cefprozil Diastereomers in Human PlasmaDocument8 pagesHPLC Method For Pharmacokinetics of Cis and Trans Isomer of Cefprozil Diastereomers in Human PlasmaIOSR Journal of PharmacyNo ratings yet
- Epilepsia - 2009 - La Marca - A New Rapid Micromethod For The Assay of Phenobarbital From Dried Blood Spots by LC TandemDocument5 pagesEpilepsia - 2009 - La Marca - A New Rapid Micromethod For The Assay of Phenobarbital From Dried Blood Spots by LC TandemWaode RahmahNo ratings yet
- Blood Pressure, Heart Rate, and Urinary Catecholamines inDocument9 pagesBlood Pressure, Heart Rate, and Urinary Catecholamines inJoão Marcel CamargoNo ratings yet
- Physiologic and Pathologic Levels of Reactive Oxygen Species in Neat Semen of Infertile MenDocument6 pagesPhysiologic and Pathologic Levels of Reactive Oxygen Species in Neat Semen of Infertile MenMihajilo TosicNo ratings yet
- Pharmacokinetics and Concentration-Effect Relationship of Oral LSD in HumansDocument7 pagesPharmacokinetics and Concentration-Effect Relationship of Oral LSD in HumansasdadasdasNo ratings yet
- 1 s2.0 S0731708516312808 MainDocument7 pages1 s2.0 S0731708516312808 MainSergeat18BNo ratings yet
- Effect of Storage Time and Temperature On Some Serum Analytes8.21 PDFDocument4 pagesEffect of Storage Time and Temperature On Some Serum Analytes8.21 PDFyunitaNo ratings yet
- Assessmentof Fetal Lungmaturity:Lecithin/ Sphingomyelinratiovs. Cortisoland Foam-Test AssaysDocument4 pagesAssessmentof Fetal Lungmaturity:Lecithin/ Sphingomyelinratiovs. Cortisoland Foam-Test AssaysPatrick RamosNo ratings yet
- Arnhard 2012Document14 pagesArnhard 2012malwanafhc.adNo ratings yet
- 003-CC 1970 Cotlove-Biol & Analyt Components of Var 3 Physiol and MedicalDocument5 pages003-CC 1970 Cotlove-Biol & Analyt Components of Var 3 Physiol and MedicalFernando Cava ValencianoNo ratings yet
- Metabolic Fingerprinting of Royal Jelly: Characterization and Proof of AuthenticityDocument6 pagesMetabolic Fingerprinting of Royal Jelly: Characterization and Proof of AuthenticitycostytzuNo ratings yet
- Volume - 41 - 4 - 97 - 3 - MacacaDocument16 pagesVolume - 41 - 4 - 97 - 3 - MacacaAnindyaMustikaNo ratings yet
- Influence of Biological Variations and Sample Handling On Measured Microalbuminuria in Diabetic PatientsDocument7 pagesInfluence of Biological Variations and Sample Handling On Measured Microalbuminuria in Diabetic PatientsJ DNo ratings yet
- Biomedical Chromatography - 2011 - Mendes - Quantification of Cyproheptadine in Human Plasma by High Performance LiquidDocument8 pagesBiomedical Chromatography - 2011 - Mendes - Quantification of Cyproheptadine in Human Plasma by High Performance LiquidLuiz Fernando RibeiroNo ratings yet
- Package Insert 13695 - HCG D - en - 30405-01 PDFDocument10 pagesPackage Insert 13695 - HCG D - en - 30405-01 PDFadybaila4680No ratings yet
- Earwax As An Alternative Specimen For Forensic AnalysisDocument11 pagesEarwax As An Alternative Specimen For Forensic AnalysisNAYARA MOREIRA DAMASCENONo ratings yet
- Effects of Cypermethrin On Rainbow Trout (Oncorhynchus Mykiss)Document9 pagesEffects of Cypermethrin On Rainbow Trout (Oncorhynchus Mykiss)Daniel Morales CespedesNo ratings yet
- Variance of Melatonin and Cortisol Rhythm in Patients With Allergic RhinitisDocument4 pagesVariance of Melatonin and Cortisol Rhythm in Patients With Allergic RhinitisalfredoibcNo ratings yet
- Shin - Hypocholesterolemic Effect of Daily Fisetin Supplementation in High Fat Fed Sprague-Dawley Rats - 2013Document7 pagesShin - Hypocholesterolemic Effect of Daily Fisetin Supplementation in High Fat Fed Sprague-Dawley Rats - 2013thrNo ratings yet
- Reproductive Toxicology of Tartrazine (FD and C Yellow No. 5) in Swiss Albino MiceDocument6 pagesReproductive Toxicology of Tartrazine (FD and C Yellow No. 5) in Swiss Albino MiceMuchtar RezaNo ratings yet
- Androgenic Status of Lepromatous Leprosy Patients With GynecomastiaDocument6 pagesAndrogenic Status of Lepromatous Leprosy Patients With GynecomastianadyaNo ratings yet
- Estradiol and Progesterone Fecal Metabolites Analysis in Crab-Eating-FoxDocument5 pagesEstradiol and Progesterone Fecal Metabolites Analysis in Crab-Eating-FoxTiago AmaralNo ratings yet
- The Plasma Sugar, Free Fatty Acid, Cortisol, and Growth Hormone Response Insulin. I. in Control SubjectsDocument8 pagesThe Plasma Sugar, Free Fatty Acid, Cortisol, and Growth Hormone Response Insulin. I. in Control SubjectsYng TangNo ratings yet
- Journal of Pharmaceutical and Biomedical Analysis Volume 125 Issue 2016 (Doi 10.1016/j.jpba.2016.03.024) Abdallah, Inas A. Hammell, Dana C. Hassan, Hazem E. Stinchcom - Norelgestromin - Ethinyl eDocument9 pagesJournal of Pharmaceutical and Biomedical Analysis Volume 125 Issue 2016 (Doi 10.1016/j.jpba.2016.03.024) Abdallah, Inas A. Hammell, Dana C. Hassan, Hazem E. Stinchcom - Norelgestromin - Ethinyl eTri HandayaniNo ratings yet
- Preparation of Extracts and Analytical Chemistry: Supporting Information Extended Material and MethodsDocument10 pagesPreparation of Extracts and Analytical Chemistry: Supporting Information Extended Material and Methodsjuan arellano olivaresNo ratings yet
- Rodriguez G - Serum ACE Activity in Normal Children and in Those With SarcoidosisDocument5 pagesRodriguez G - Serum ACE Activity in Normal Children and in Those With SarcoidosisPhaimNo ratings yet
- 1 s2.0 S2095311916613862 MainDocument12 pages1 s2.0 S2095311916613862 MainGOKULA PRIYA R 19EC005No ratings yet
- NEJM appendixPDF2020Document7 pagesNEJM appendixPDF2020Marin AndreiNo ratings yet
- A Case of Severe Hypertriglyceridaemia and HypercholesterolaemiaDocument1 pageA Case of Severe Hypertriglyceridaemia and Hypercholesterolaemiathys2000No ratings yet
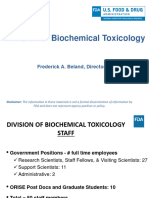
- 2018 SAB Presentation Division of Biochemical Toxicology Research Overview - 3Document21 pages2018 SAB Presentation Division of Biochemical Toxicology Research Overview - 3hellion00No ratings yet
- 30 - Evaluation of Prostate-Specific Antigen (PSA) Membrane Test Assays For The Forensic Identification of Seminal Fluid PDFDocument4 pages30 - Evaluation of Prostate-Specific Antigen (PSA) Membrane Test Assays For The Forensic Identification of Seminal Fluid PDFMN IrshadNo ratings yet
- Comparative Evaluation of Pyrogens Tests in Pharmaceutical ProductsDocument6 pagesComparative Evaluation of Pyrogens Tests in Pharmaceutical Productsnamchin parkNo ratings yet
- Tricyclic Antidepressant GC-MSDocument6 pagesTricyclic Antidepressant GC-MSrodrigoNo ratings yet
- Original Articles A Simple, Isocratic High-Performance Liquid Chromatography Assay For Linezolid in Human SerumDocument4 pagesOriginal Articles A Simple, Isocratic High-Performance Liquid Chromatography Assay For Linezolid in Human Serumharold.atmajaNo ratings yet
- Tlili2011 PDFDocument5 pagesTlili2011 PDFManju ManoharNo ratings yet
- Package Insert - 06038 - HCG - en - 30405 Europa PDFDocument7 pagesPackage Insert - 06038 - HCG - en - 30405 Europa PDFadybaila4680No ratings yet
- Mls 111b LAb MidDocument10 pagesMls 111b LAb MidJohanna MarieNo ratings yet
- Impact of Anticoagulants On Assessment of Zinc in Plasma: Croat. Chem. Acta 2018, 91 (3), 317-321Document5 pagesImpact of Anticoagulants On Assessment of Zinc in Plasma: Croat. Chem. Acta 2018, 91 (3), 317-321Andrea CardenaNo ratings yet
- ReproDocument3 pagesReproRiyaduNo ratings yet
- Detection and Quantification of Benzodiazepines An Z-DrugsDocument16 pagesDetection and Quantification of Benzodiazepines An Z-DrugsDFNo ratings yet
- Bioequivalence Study of Two Formulations of Bisoprolol Fumarate Tablets in Healthy SubjectsDocument7 pagesBioequivalence Study of Two Formulations of Bisoprolol Fumarate Tablets in Healthy SubjectsSan-Clin-Eq LaboratoryNo ratings yet
- Clinical & Diagnostic Tests For GpatDocument10 pagesClinical & Diagnostic Tests For GpatSHRIKANTNo ratings yet
- DEM-DEE007 Leptin ELISA 160503 MDocument26 pagesDEM-DEE007 Leptin ELISA 160503 MSusana Méndez GómezNo ratings yet
- Camparison Monovalente AntivenomsDocument1 pageCamparison Monovalente AntivenomsAndrea BaracaldoNo ratings yet
- Jurnal Amlodipin UdtDocument7 pagesJurnal Amlodipin UdtdidiisafitriNo ratings yet
- Comparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsDocument5 pagesComparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsgeoaislaNo ratings yet
- ALBUMIN BLOSR6x02 ENDocument2 pagesALBUMIN BLOSR6x02 ENMeethuanNo ratings yet
- Quantification of Pregabalin Using Hydrophilic Interaction HPLC-High-Resolution MS in Postmortem Human Samples: Eighteen Case ReportsDocument6 pagesQuantification of Pregabalin Using Hydrophilic Interaction HPLC-High-Resolution MS in Postmortem Human Samples: Eighteen Case ReportsLuisa Fernanda Velásquez QuijanoNo ratings yet
- Glucose (God Pap)Document2 pagesGlucose (God Pap)anggun990% (1)
- Journal Lesitin RasioDocument3 pagesJournal Lesitin RasioSUSANNo ratings yet
- 2Document8 pages2Chorrinha ChorraNo ratings yet
- ETAPDocument8 pagesETAParulprakashf.sdcNo ratings yet
- Clock Drawing Test PDFDocument6 pagesClock Drawing Test PDFfissionmailedNo ratings yet
- Toovey 2007Document22 pagesToovey 2007fissionmailedNo ratings yet
- NIH Public Access: The Teenage Brain: The Stress Response and The Adolescent BrainDocument11 pagesNIH Public Access: The Teenage Brain: The Stress Response and The Adolescent BrainfissionmailedNo ratings yet
- 1999 Anyas PDFDocument3 pages1999 Anyas PDFfissionmailedNo ratings yet
- Cystic Disease The Liver and Biliary: TractDocument7 pagesCystic Disease The Liver and Biliary: TractfissionmailedNo ratings yet
- LKPD - Recount Text 2Document2 pagesLKPD - Recount Text 2Sabian KalifiNo ratings yet
- Measles EpiDocument22 pagesMeasles Epiمحمد صالحNo ratings yet
- Complications of Diabetes MellitusDocument147 pagesComplications of Diabetes MellitusNisrina SariNo ratings yet
- CEA Pilgastrim Vs FilgastrimDocument13 pagesCEA Pilgastrim Vs FilgastrimMaya Aulia MulakhaillaNo ratings yet
- The Small Intestine Channel - Discernment, Sorting, Mental ClarityDocument5 pagesThe Small Intestine Channel - Discernment, Sorting, Mental Clarityلوليتا وردةNo ratings yet
- Clinical Practice Guidelines For Management of Bipolar DisorderDocument16 pagesClinical Practice Guidelines For Management of Bipolar DisorderKavita kumariNo ratings yet
- Oropharyngeal and Nasopharyngeal SuctioningDocument2 pagesOropharyngeal and Nasopharyngeal SuctioningAlana Caballero100% (1)
- Hepatitis C Education Class - 2009Document64 pagesHepatitis C Education Class - 2009BENNo ratings yet
- Lam. Pathway Gagal Jantung KongestiDocument2 pagesLam. Pathway Gagal Jantung KongestiMegawati Dwi PutriNo ratings yet
- Hubungan Kepadatan Hunian, Kelembaban Dan Status GiziDocument16 pagesHubungan Kepadatan Hunian, Kelembaban Dan Status GiziBenny SimanjuntakNo ratings yet
- Radio PsaDocument3 pagesRadio Psaapi-356356986No ratings yet
- Mechanical Ventilation in Pediatric PatientDocument11 pagesMechanical Ventilation in Pediatric PatientHandris YanitraNo ratings yet
- Vaccines 08 00321Document17 pagesVaccines 08 00321Kshitiz Raj ShresthaNo ratings yet
- Introduction and Around The World W Dr. Boyd": COVID-19 ResourcesDocument10 pagesIntroduction and Around The World W Dr. Boyd": COVID-19 ResourcesNabillahNo ratings yet
- OsteomyelitisDocument20 pagesOsteomyelitisYusri HarisNo ratings yet
- KoshtaDocument15 pagesKoshtaPanchakarma DepartmentNo ratings yet
- GONORRHOEADocument23 pagesGONORRHOEADwi Fikha AprilyantiNo ratings yet
- Effect of Single-Dose Antibiotic Prophylaxis Versus Conventional Antibiotic Therapy in Surgery A Randomized Controlled Trial in A Public Teaching HospitalDocument5 pagesEffect of Single-Dose Antibiotic Prophylaxis Versus Conventional Antibiotic Therapy in Surgery A Randomized Controlled Trial in A Public Teaching HospitalكنNo ratings yet
- War Card GameDocument2 pagesWar Card Gameapi-541744798No ratings yet
- Group 3 QUIZDocument4 pagesGroup 3 QUIZJessa Mae OhaoNo ratings yet
- Medication and Treatment Sheet: Mariano Marcos Memorial Hospital and Medical CenterDocument4 pagesMedication and Treatment Sheet: Mariano Marcos Memorial Hospital and Medical CenterWyn AgustinNo ratings yet
- Nueva Ecija University of Science And: A Case Analysis ofDocument68 pagesNueva Ecija University of Science And: A Case Analysis ofShane PangilinanNo ratings yet
- Episkleritis Dan SkleritisDocument41 pagesEpiskleritis Dan SkleritisSuryana AdityaNo ratings yet
- Normal Parturition and Management of Dystocia in Dogs and CatsDocument7 pagesNormal Parturition and Management of Dystocia in Dogs and Catsmcs.vet8473No ratings yet
- Liver Cirrhosis LectureDocument83 pagesLiver Cirrhosis LectureSheila Regina Tiza100% (1)
- Drug StudyDocument7 pagesDrug StudyAnn Therese C. GutierrezNo ratings yet
- Point of Care Ultrasound (Pocus) : Introduction: George A. FoxDocument76 pagesPoint of Care Ultrasound (Pocus) : Introduction: George A. FoxAna Belen Viteri LuzuriagaNo ratings yet
- List of Medical and Nursing Abbreviations, Acronyms, Terms 1 - NurseslabsDocument25 pagesList of Medical and Nursing Abbreviations, Acronyms, Terms 1 - NurseslabsbeingfiredNo ratings yet
Westermann 2004 2 PDF
Westermann 2004 2 PDF
Uploaded by
fissionmailedOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Westermann 2004 2 PDF
Westermann 2004 2 PDF
Uploaded by
fissionmailedCopyright:
Available Formats
Clin. Lab.
2004; 50; 11-24
©Copyright
ORIGINAL ARTICLE
Determination of Cortisol in Saliva and Serum by a
Luminescence-Enhanced Enzyme Immunoassay
JÜRGEN WESTERMANN, ANKE DEMIR, VICTOR HERBST
Immuno-Biological Laboratories GmbH, Hamburg,Germany
SUMMARY
A new luminescence-enhanced enzyme immunoassay (LEIA) has been developed and validated for the direct mea-
surement of cortisol in saliva and serum. It has been demonstrated that this LEIA has a very good analytical and
functional sensitivity. There was a good correlation to a commercial RIA. The assessment of diurnal cortisol pro-
files of healthy persons are discussed. Cortisol monitoring is indicated in diseases with abnormal glucocorticoid
production such as Cushing`s syndrome and Addison’s disease. Because of the diurnal fluctuation of cortisol levels
it is necessary to take several samples for an individual cortisol profile or during dynamic tests like the dexa-
methasone-suppression or ACTH stimulation. Salivary sample collection is an alternative method without the
stress of repeated venipuncture. The measurement of cortisol in saliva is advisable in patients with abnormal
cortisol-binding-globulin (CBG) levels such as pregnancy, hypothyroidism, nephrotic syndrome or marked adi-
positas and during the administration of certain drugs, especially oral contraceptives.
KEY WORDS released from the salivary glands (1). The normal sali-
vary cortisol concentration in the evening is about 1.5
Cortisol, saliva, luminescence, immunoassay, diurnal nmol/l (13). It is therefore necessary to develop an assay
profile, free hormones which enables observers to determine such small levels
of cortisol in saliva accurately. In using non-radioiso-
INTRODUCTION topic immunoasssays it is best to use a chemilumines
cent or a time resolved fluorescence labelled immuno-
Only the non protein bound fraction of the lipophilic assay because of the superior analytical sensitivity (14 -
steroid hormones passes quantitatively from the circula- 16).
tion into the saliva (1). This enables scientists to directly In saliva there is a diurnal fluctuation of the cortisol
assess the biologically active fraction of these hor- concentration in adult humans, reaching a peak around
mones. In addition, using saliva makes it possible to con- 30 to 60 minutes after awakening and falling to lower
veniently obtain several samples for assessing hormone levels in the afternoon which remains trough the next
profiles. As a result, using saliva as a sample signifi- morning (13, 17 - 20). The circadian pacemaker is re-
cantly extends the application of hormone testing in sponsible for this cortisol variation, which also influ-
such scientific fields as psychology, occupational medi- ences the diurnal melatonin profile, is located in the su-
cine, sport medicine and pediatrics. (2 - 12). prachiasmic nuclei of the hypothalamus (13, 21). New-
About 90 % of the cortisol in the circulation is bound to borns do not exhibit a diurnal cortisol profile. It devel-
the corticosteroid-binding globulin (CBG, transcortin), ops during the first 20 weeks after birth (22 – 25). Even
about 7 % is bound loosely to albumin, and only 1 – 3 % in adults large inter- individual differences in the di-
is unbound. Only cortisol from the two latter fractions is urnal cortisol pattern exists (26). It is advantageous to
take saliva samples in connection with the individual
Manuscript accepted May 8, 2003 waking time, rather than blood samples at fixed inter-
vals for the accurate assessment of daily variation.
Clin. Lab. 1+2/2004 11
JÜRGEN WESTERMANN et al.
MATERIALS AND METHODS were collected over a normal working day. Shift wor-
kers were not included in the study. The test persons
Chemicals were not on drugs which might have affected the corti-
All fine chemicals were purchased from Sigma-Aldrich sol level.
(Deisenkirchen, Germany) or Merck (Darmstadt, Ger-
many). Cortisol and compounds used for cross-reacti- Adult Females Adult Males Children
Elderly
subjects
vity studies were obtained from Steraloids, Inc. (New- Number 61 39 4 (3f,1m) 10 (4f,6m)
port, Rhode Island USA). Age
28.8 ± 11.1 32.6 ± 13.0 8.8 ± 5.1 67.5 ± 4.1
(mean ± SD)
Range
17 - 60 17 – 59 3 – 13 62 – 77
Reagents (min-max)
All reagents used in the LEIA kit were provided by the
manufacturer (IBL Hamburg GmbH; Hamburg, Ger-
many).
Microtiter Strips: ready for use; white microtiter plate Samples for saliva - serum correlation.
wells (Maxisorp, Nunc; Roskilde, Denmark) coated Paired saliva and serum samples were obtained from 84
with goat anti-rabbit IgG and anti-cortisol antibody clinically healthy volunteers within 10 minutes of each
(Scantibody Laboratory Inc., Santee, CA, USA and other.
Prof. Vescei Heidelberg, Germany), and blocked with
BSA (Sigma) and Karion (Merck).
Enzyme Conjugate: ready for use; Cortisol-3-carboxy- Samples for GC/MS correlation of serum samples
methyloxim was first coupled to horseradish peroxidase As reference method comparison, 20 quality assessment
with the mixed anhydride method and then dialyzed serum samples from the DGKC (Deutsche Gesellschaft
against phosphate-buffered saline. The peroxidase con- für klinische Chemie, Bonn, Germany) were used for
jugate was diluted in Stabilzyme® buffer (Sur Modics hormone measurement were used. These samples were
Inc., Eden Prairie, MN, USA). predetermined by the reference laboratory of the DGKC
Saliva Control 1 and 2: ready for use; Saliva was en- (Referenzinstitut für Bioanalytik, Bonn, Germany) us-
riched with different amounts of cortisol with 0.01 % ing a GC/MS reference method for determination of
thimerosal as a preservative. Cortisol.
Standard A - G: ready for use; contained cortisol in 0.1
mol/l phosphate buffer with 9 g/l NaCl, 0.1 %(w/v) Quality control samples
BSA and 0.01%(w/v) thimerosal. The standard concen- Control samples were prepared by adding different
trations are 0 nmol/l (Standard A, zero standard), 0.83 stock solutions with known cortisol concentrations to
nmol/l (Standard B), 1.7 nmol/l (Standard C), 5.5 nmol/l individual saliva and serum samples from normal
(Standard D), 17 nmol/l (Standard E), 41 nmol/l (Stan- volunteers. The controls were aliquoted and stored at -
dard F), 110 nmol/l (Standard G). 80 °C.
Wash Buffer: concentrate; phosphate buffer (0.1 mol/l,
pH 7.3) containing of 9g/l NaCl, 0.1 % (w/v) Tween 80
and 0.01%(w/v) thimerosal. This was diluted 1 to 10 LEIA kit
with distilled water prior to use. Handling of samples: Saliva samples were collected by
Substrate Reagents: Reagent 1 and reagent 2 were ob- either using Salivettes® (Sarstedt) without additives or
tained from Perbio Science, (Bonn, Germany). Reagent by transferring saliva with a straw into a glass or poly-
1 contained luminol and an enhancer. Reagent 2 con- propylene tube (IBL, Hamburg, Germany), after saliva
sisted of a peroxide solution with stabilizers. Reagents 1 flow has been stimulated by chewing on a piece of Para-
and 2 were mixed in equal amounts prior to use. filmTM (American National Can, Chicago, IL,USA).
Adhesive Foil: transparent plastic foils. Samples with a slightly reddish color, suspected of be-
All kit reagents were stable for at least 9 months when ing contaminated with blood, were discarded.
stored at 2 - 8 °C. The diluted wash buffer was stable It is highly recommended to freeze the samples once at
for up to 4 weeks at 2 - 8 °C and the mixed substrate –20°C prior to the test run in order to precipitate inter-
reagent is stable for 8 hours at room temperature. fering mucoproteins. After thawing and before assay,
the samples were centrifuged at 2000 - 3000 x g to re-
Samples for the diurnal profiles move solids. Repeated freeze-thaw cycles should be
Saliva was collected with Salivettes® (Sarstedt, Nüm- avoided. The saliva samples may be stored for up to 5
brecht, Germany) or with a straw into Polypropylene days at room temperature or up to 10 days at 2 - 8°C.
tubes (IBL, Hamburg, Germany) every 30 minutes for 4 For longer periods the saliva should be stored in ali-
hours after awakening. Then every hour for 15 hours a quots at –20°C.
sample was taken. The persons included in this study
were clinically healthy on a normal diet. The samples
12 Clin. Lab. 1+2/2004
DETERMINATION OF CORTISOL BY A LUMINESCENCE-ENHANCED ENZYME IMMUNOASSAY
Table 1: Specificity of the anti-cortisol antibody used in the described LEIA
Compound Cross-reactivity [%]
Cortisol, hydrocortisone (4-Pregnen-11β,17α,21-triol-3,20-dion) 100
Prednisolone (1,4-Pregnadien-11β,17α,21-triol-3,20-dion) 57
11-Deoxycortisol (4-Pregnen-17α,21-diol-3,20-dion 12
Corticosterone (4-Pregnen-11β,21-diol-3,20-dion) 2.5
Cortisone (4-Pregnen-17α,21-diol-3,11,20-trion) 2
Prednisone (1,4-Pregnadien-17α,21-diol-3,11,20-trion) 1
17α –Hydroxyprogesterone (4-Pregnen-17αol-3,20-dion) 0.5
Deoxycorticosterone (4-Pregnen-21-ol-3,20-dion) 0.3
6α-Methyl-17α-Hydroxyprogesterone (6α-Methyl-4-pregnen-17α-ol-3,20-dion) 0.1
Progesterone (4-Pregnen-3,20-dion) <0.05
Dexamethasone (9α-Fluor-16α-methyl-prednisolone) <0.05
17α–Hydroxypregnolene (5-Pregnen-3β,17α-diol-20-on) <0.01
Dehydroisoandrosterone (5-Androsten-3β-ol-17-on) <0.01
Androstenedione (4-Androstene-3,17-dion) <0.01
Oestriol (1,3,5(10)-Estratrien-3,16α,17β-triol) <0.01
6α-Methyl-17α-Hydroxyprogesteroneacetate (6α-Methyl-4-pregnen-3,17-acetate) <0.01
Pregnenolone (5-Pregnen-3β-ol-20-on) <0.01
Oestrone (1,3,5(10)-Estratrien-3-ol-17-on) <0.01
Testosterone (4-Androstene-17β-ol-3-on) <0.01
17α-Hydroxyprogesterone-17 sulphate (4-Pregnen-17α-ol-3,20-dion sulphate) <0.01
Androsterone sulphate (5α-Androstene-3α-ol-17-on sulphate) <0.01
Testosterone sulphate (4-Androstene-17β-ol-3-on sulphate) <0.01
Cholesteryl sulphate (5-Cholesten-3β-ol sulphate) <0.01
17β-Oestradiol-17 sulphate (1,3,5(10)-Estratrien-3,17β-diol 17-sulphate) <0.01
DHEA-S (5-Androstene-3β-ol-17-on sulphate) <0.01
All blood samples were obtained without an anticoagu- minescence units (RLU) are inversely proportional to
lant, stored at room temperature for 30 minutes until the cortisol concentration.
coagulation was complete, and then centrifuged for
10 min at 2000 x g. Serum was separated and stored at
-20 °C. LEIA test procedure: 20 µl of each standard, control,
and sample (saliva undiluted, serum diluted 1:50 in
Zero Standard) were pipetted in duplicate into the wells
LEIA test principle: The assay procedure of this corti- of the white microtiter strips and 100 µl of cortisol-
sol LEIA kit follows the basic principles of a competi- horseradish peroxidase conjugate added. After covering
tive immunoassay. The wells of a microtiter plate were with adhesive foil the plate was incubated for
first coated with goat anti-rabbit antibodies followed by 3 hours at room temperature (18 - 24°C). All wells
rabbit anti-cortisol antibodies. An unknown amount of were then washed four times with 250 µl wash buffer.
cortisol present in the sample and a fixed amount of per- Luminescence was read 10 minutes after addition of
oxidase-labelled cortisol compete for the binding sites 50 µl substrate solution. An MPL2 luminometer from
of the antigen-specific coated antibodies. After an incu- Berthold Detection Systems (Pforzheim,Germany) was
bation time the wells were washed to stop the competi- used for measurement. For calculation of the standard
tion reaction. The added luminescence substrate solu- curves with four-parameter logistics, the Microwin 2000
tion was converted to a light emitting component by the software was used (Mikrotek Laborsysteme GmbH,
bound peroxidase conjugate. The measured relative lu- Overath, Germany).
Clin. Lab. 1+2/2004 13
JÜRGEN WESTERMANN et al.
100
90
80
70
RLU/RLUmax [%]
60
50
40
30
20
10
0
0 1 10 100 1000
Cortisol [nmol/l]
Figure 1: Typical standard curve of the cortisol LEIA
Comparison methods Specificity of the antibodies
The radioimmunoassay from Diagnostic Systems Labo- The specificity of the anti-cortisol antibody used in our
ratories (DSL, Webster, Texas, USA) was used for LEIA was evaluated for cross-reactivity to various com-
comparison. The RIA was modified according to the pounds (Table 1) that may potentially interfere with the
method described by M. Gröschl et al (27). Regression assay.
analysis was performed according to Bablock et al. (28). A 57% cross-reactivity for prednisolone (difference
from cortisol is one double bond in position 1) was
seen. 11-deoxycortisol showed cross reactivity of 12%,
Shelf-life evaluation while all other compounds showed cross-reactivity less
Both accelerated and real-time stability testing of the than 2.5%.
reagents, standards and controls was performed to deter-
mine the expiration date (29).
LEIA standard curve and sensitivity
A typical standard curve is shown in Figure 1. A cali-
Statistical methods bration curve was established by using cortisol stan-
Statistical calculations were performed according to the dards from 0.83 to 110 nmol/l. The measuring range of
recommendations of Krouwer and Rabinowitz (30). The the LEIA covers the range of normal and elevated cor-
software used for calculation of statistical data was tisol concentrations in human saliva and in 1:50 diluted
Winstat (Kalmia Co. Inc.) and SigmaPlot 2001 (SPSS serum.
Inc.). The slope of the calibration curves was calculated The analytical sensitivity, calculated from the mean mi-
according to Rodbard (31). nus 3 standard deviations (SD) of 15 replicates of the
zero standard is 0.38 nmol/l. Functional sensitivity was
determined from the between-lot (n=6) assay variation
RESULTS coefficient of very low saliva samples. The lowest corti-
sol concentration which could be measured with a co-
The analytical performance of the newly developed efficient of variation below 20% is 0.52 nmol/l.
LEIA kit was determined by evaluating analytical speci-
ficity and sensitivity, precision, accuracy (recovery,
linearity) and comparison with other established im- Precision
munoassay kits. The intra-assay variation, the inter-assay variation and
the between-lot variation for saliva samples were deter-
14 Clin. Lab. 1+2/2004
DETERMINATION OF CORTISOL BY A LUMINESCENCE-ENHANCED ENZYME IMMUNOASSAY
Table 2: Precision of the cortisol LEIA for saliva samples
A. Determination of intra-assay variation of 6 different saliva samples
Saliva 1 Saliva 2 Saliva 3 Saliva 4 Saliva 5 Saliva 6
20 each in one run
[nmol/l] [nmol/l] [nmol/l] [nmol/l] [nmol/l] [nmol/l]
Mean value 2.65 4.33 5.96 10.82 24.01 71.46
SD 0.19 0.33 0.36 0.30 1.08 5.88
CV [%] 7.3 7.6 6.0 2.8 4.5 8.2
B. Determination of interassay variation of 6 different saliva samples
Duplicates in 20 runs Saliva 1 Saliva 2 Saliva 3 Saliva 4 Saliva 5 Saliva 6
[nmol/l] [nmol/l] [nmol/l] [nmol/l] [nmol/l] [nmol/l]
Mean value 2.07 3.67 5.71 9.52 18.82 66.54
SD 0.25 0.28 0.44 0.61 1.16 6.51
CV [%] 12.0 7.5 7.7 6.4 6.2 9.8
C. Determination of interlot variation of 6 different saliva samples
Saliva 1 Saliva 2 Saliva 3 Saliva 4 Saliva 5 Saliva 6
Duplicates in 7 different Kit Lots
[nmol/l] [nmol/l] [nmol/l] [nmol/l] [nmol/l] [nmol/l]
Mean value 1.96 3.48 5.93 9.69 19.13 64.34
SD 0.17 0.30 0.44 0.94 1.74 6.79
CV [%] 8.5 8.7 7.4 9.7 9.1 10.6
120
Cortisol Saliva IBL LEIA [nmol/l]
100
80
60
40
20
y = 1,38x - 0,88
2
R = 0,96
0
0 10 20 30 40 50 60 70 80
RIA [nmol/l]
Figure 2: Comparison of cortisol measured by immunoassays RIA (x) and IBL LEIA (y)
Clin. Lab. 1+2/2004 15
JÜRGEN WESTERMANN et al.
Table 3: Analytical recovery for saliva samples
Added Expected Found Recovery
Sample
[nmol/l] [nmol/l] [nmol/l] [%]
Saliva without added cortisol: 6.7
1.3 8.0 7.8 98
2.6 9.2 8.5 92
Saliva 1 5.2 11.9 11.0 92
10.4 17.0 16.9 99
20.7 27.4 26.6 97
41.4 48.1 50.8 106
Saliva without added cortisol: 10.7
1.3 12.0 11.2 93
2.6 13.3 11.8 89
Saliva 2 5.2 15.9 14.1 89
10.4 21.1 20.3 96
20.7 31.4 32.9 105
41.4 52.1 55.2 106
Saliva without added cortisol: 11.9
1.3 13.2 13.2 100
2.6 14.5 13.1 90
Saliva 3 5.2 17.1 15.7 92
10.4 22.3 21.8 98
20.7 32.7 35.3 108
41.4 53.4 60.8 114
25
20
Saliva [nmol/l]
15
10
0
0 200 400 600 800
Serum [nmol/l]
Figure 3: Cortisol values of simultaneously taken saliva and serum samples, measured with the cortisol LEIA.
16 Clin. Lab. 1+2/2004
DETERMINATION OF CORTISOL BY A LUMINESCENCE-ENHANCED ENZYME IMMUNOASSAY
Table 4: Serial dilution of saliva samples in the cortisol LEIA
Measured Expected Recovery
Saliva Dilution
conc.[nmol/L] conc.[nmol/L] [%]
neat 86.08 - 100
1:2 41.05 43.04 95
1:4 19.64 21.52 91
1
1:8 9.57 10.76 89
1:16 4.52 5.38 84
1:32 2.51 2.69 93
neat 63.18 - 100
1:2 36.23 31.59 115
1:4 16.75 15.80 106
2
1:8 7.50 7.90 95
1:16 3.75 3.95 95
1:32 1.99 1.97 101
neat 60.45 - 100
1:2 30.49 30.22 101
1:4 15.15 15.11 100
3
1:8 7.09 7.56 94
1:16 3.39 3.78 90
1:32 1.93 1.89 102
mined by repeated measurements of control samples. To demonstrate the assay accuracy by another method,
The results for the saliva samples are shown in Tables linearity studies were performed. Saliva samples with
2. A, B and C. For saliva (range 2 - 70 nmol/l) the mean high basal cortisol concentrations were serially diluted
intra-assay variation CV% was 6.13 %, the mean inter- with cortisol-free medium (standard A), and the cortisol
assay variation CV% was 8.13 % and the mean CV% concentration was assayed by the LEIA. The results are
for the between-lot variation of seven different lots was presented in Table 4. To cover the whole standard range
8.93 %. 5 dilutions were made of each sample. The ratio be-
For serum (range 50-2000 nmol/l), the mean intra-assay tween concentration and dilution of sera did not signifi-
variation CV% was 7.70 %, the mean inter-assay varia- cantly deviate from linearity across the concentration
tion CV% was 8.83 % and the mean CV% for the be- range studied (mean recovery 97%, range 84-115%).
tween-lot variation of four different lots was 8.14 %. In a dilution study of two serum samples we found a
mean recovery of 94% (range 83- 99%).
Accuracy
We estimated the analytical recovery of cortisol in the Method comparison
LEIA at six different concentrations added to three Sali- The LEIA was compared with a radioimmunoassay. 384
va samples (Table 3). Increasing amounts of cortisol saliva and 106 serum samples were assayed for cortisol
were added to saliva samples with various initial corti- concentrations, both by the comparison methods (x-
sol concentrations. Cortisol concentrations were mea- axis) and by the LEIA (y-axis). The results of linear re-
sured, and the percentage of recovery was calculated. gression analysis of saliva samples showed excellent
The mean recovery of cortisol from all three saliva sam- correlation, with a correlation coefficient r = 0.98. The
ples was 98% (range 89 - 114%). slope of the regression lines was 1.38 and the intercept
In a spike experiment with serum we found a mean re- was 0.88 nmol/l. Figure 2 demonstrates the results of
covery of 97% (range 90 -107%). the method comparison for saliva samples.
The method comparison data for serum samples are:
IBL LEIA = 0.94*RIA + 0.171 ; r = 0.95; n = 106
Clin. Lab. 1+2/2004 17
JÜRGEN WESTERMANN et al.
Table 5: Interferences of blood in saliva (bold samples show increased cortisol levels)
Final blood Measured conc. Recovery
Sample
concentration [%] v/v [nmol/l] [%]
0.000 23.73 100
0.060 24.56 103
0.125 23.45 99
0.250 22.62 95
1
0.500 26.49 112
0.625 45.52 192
1.250 68.98 291
2.500 114.50 483
0.000 61.25 100
0.060 69.53 114
0.125 77.53 127
0.250 62.63 102
2
0.500 61.80 101
0.625 87.46 143
1.250 113.39 185
2.500 126.09 206
40
35
30
Salivary Cortisol [nmol/l]
25
20
15
10
0
4 6 8 10 12 14 16 18
Time of day [h]
Figure 4: Typical diurnal profiles of persons waking up at different times
18 Clin. Lab. 1+2/2004
DETERMINATION OF CORTISOL BY A LUMINESCENCE-ENHANCED ENZYME IMMUNOASSAY
Table 6: Data of the diurnal profile study
Cortisol peak maximum Delay (decimal) Peak time (decimal) Wake up time (decimal) Age
[nmol/l] [h] [h] [h] [years]
Senior Citizens n=10
MEAN 11.56 1.13 7.98 6.72 67.5
MEDIAN 11.32 1.00 8.25 6.67 67.0
SD 4.08 0.62 0.87 0.67 4.14
MIN 5.08 0.00 6.00 5.50 62
MAX 19.46 2.00 9.00 7.83 77
Children n=4
MEAN 7.17 1.21 8.83 7.63 8.75
MEDIAN 7.38 1.13 8.88 7.50 9.50
SD 4.14 1.10 1.06 0.25 5.06
MIN 2.61 0.00 7.50 7.50 3
MAX 11.29 2.58 10.08 8.00 13
Females n=61
MEAN 28.1 0.83 7.81 6.98 28.8
MEDIAN 28.1 0.75 7.50 6.75 24.0
SD 13.3 0.55 1.60 1.60 11.1
MIN 6.8 0.00 4.50 4.00 17
MAX 78.4 2.50 12.75 12.25 61
Males n=39
MEAN 26.2 0.82 8.39 7.57 32.6
MEDIAN 24.3 0.50 8.00 7.00 27.5
SD 10.2 0.64 1.90 2.06 13.0
MIN 10.3 0.00 4.75 3.75 17
MAX 62.0 3.00 12.33 12.30 59
All n=110 (without children)
MEAN 27.6 0.85 8.06 7.17 33.8
MEDIAN 26.6 0.75 7.83 6.92 26.0
SD 12.1 0.59 1.71 1.74 15.8
MIN 6.8 0.00 4.50 3.75 17
MAX 78.5 3.00 12.75 12.30 77
Comparison of saliva and serum samples in the LEIA. Figure 7 shows excellent correlation to the
Figure 3 shows the correlation in simultaneously taken GC/MS reference method values and underlining the
saliva and serum samples from 84 healthy volunteers. sensitivity of the assay.
Both samples were measured with the LEIA. A non- The method comparison data for GC/MS predetermined
linear correlation between saliva and serum cortisol was serum samples are:
observed, with correlation coefficient r=0.951, because IBL LEIA=0.958*GC/MS+57.8; r = 0.987; n = 20
of the saturation of the binding proteins with high cor-
tisol levels in serum. The linear correlation coefficient
was r = 0.823. Stability of the kit
The stability of the developed cortisol LEIA kit was in-
vestigated by real-time stability studies. The kit was
Comparison to serum samples from the DGKC found to be stable for at least 9 months when stored at 2
For comparison the 20 serum samples from the DGKC to 8 °C (data not shown).
were diluted 1:100 in zero standard and then measured
Clin. Lab. 1+2/2004 19
JÜRGEN WESTERMANN et al.
100
80
Peak maximum [%]
60
40
20
0 2 4 6 8 10 12 14
Time after awakening [h]
Figure 5: Mean diurnal cortisol in saliva profile of 110 persons.
The black squares indicate the mean and the bars the ± 2SD range.
40
30
number
20
10
0
0,0 0,5 1,0 1,5 2,0 2,5 3,0
peak delay [hours]
Figure 6: Time intervals of maximum cortisol peak of 110 persons after waking up.
20 Clin. Lab. 1+2/2004
DETERMINATION OF CORTISOL BY A LUMINESCENCE-ENHANCED ENZYME IMMUNOASSAY
Table 7: Normal Ranges
Hours after awakening [hours] Salivary Cortisol Ranges [nmol/l]
decimal 5% Percentile Median 95% Percentile
0 - 1.5 5.1 18.9 40.2
1.5 - 3.0 3.6 11.8 28.4
3.0 - 6.0 2.1 6.7 15.7
6.0 - 9.0 1.8 5.5 12.1
9.0 - 15.0 0.9 3.3 9.2
1400
1200
IBL Cortisol LEIA [nmol/l]
1000
800
600
400
y = 0,958x + 57,798
200 R = 0,987; n=20
0
0 200 400 600 800 1000 1200 1400
GC/MS reference value [nmol/l]
Figure 7: LEIA comparison to GC/MS reference values of 20 serum samples
Interferences of blood in saliva Salivary cortisol determinations in healthy persons
Quality control samples with known concentrations of For estimating reference ranges, basal cortisol concen-
cortisol were enriched with amounts of blood (all results trations were determined in saliva samples from a total
given in nmol/l). Saliva samples with blood contamina- of 110 normal volunteers (see Material and Methods).
tion greater than 0.2% (V/V) are visually reddish in co- Figure 4 shows typical diurnal profiles of the cortisol
lor and therefore must be excluded. An increased level concentration in saliva. The wake-up time is indicated
of more than 10% was observed due to higher cortisol with an open circle. The overall results and those of the
concentrations in blood. The results are shown in different subgroups are shown in Table 6. We found no
Table 5. correlation between age and peak concentration (r=
0.234) or between peak time and peak concentration
Clin. Lab. 1+2/2004 21
JÜRGEN WESTERMANN et al.
(r=0.229). The maximum cortisol concentration in sali- The precision of the LEIA has demonstrated by
va was reached with a peak mean of 0.85h = 51 minutes the intra- (2.9-7.7%) and inter- (6.2-11.5%) assay coef-
after wake up (see Figure 6). The cortisol concentration ficients of variation. The assay can measure cortisol
maximum in saliva from normal volunteers covered a concentrations accurately in both serum and saliva
broad range of 10.5 – 52.7nmol/l (5-95% percentiles). samples. Our LEIA shows a good agreement between
The mean value for the whole group was 27.6nmol/l the expected and measured concentrations in recovery
(SD = 12.1 nmol/l). Figure 5 shows the diurnal profile tests and good linearity in dilution studies. The results
of all volunteers. To normalize the overall ranges, the are consistent with those obtained with other immuno-
percentage of the peak maximum for all profiles is assay kits (RIA). High aberration in regression slope to
plotted against time after awakening. The bars indicate the RIA (Figure 2, slope=1.38) is due to used diluted
two standard deviations of the mean (black squares). serum standards, while cited literature (27) used self
Table 7 shows normal values depending on awakening made saliva standards. Using the LEIA standards for the
time. RIA leads to a regression equation of:
LEIA=1.14*RIA-2.85, r = 0.974
The excellent correlation using GC/MS reference serum
DISCUSSION samples, measured in a 1:100 dilution demonstrates the
good calibration of the standards.
The aim of this study was the development of a non- In summary, the LEIA kit described here is useful for
radioactive, sensitive and reproducible immunoassay the routine determination of cortisol as well as for basic
which accurately measures cortisol in saliva. The devel- research, where a highly sensitive and reproducible as-
oped LEIA has an analytical sensitivity of 0.38 nmol/l say is required.
cortisol, which is sufficient to detect even decreased
salivary cortisol levels. It is important to mention the
functional sensitivity in order to estimate the reproduci-
bility of cortisol results in saliva samples. The func- References
tional sensitivity of the described LEIA is 0.52 nmol/l.
The assessment of salivary cortisol is a common method 1. Vining R F and McGinley RA. The measurement of hormones
in saliva: possibilities and pitfalls. J. Steroid Biochem. 27:81 -
in various scientific fields. It is well known that the sali- 94, 1987
vary cortisol level is not dependent on the saliva flow
rate (1, 12). Moreover, it has been proven that there is a 2. Baghai TC, Schüle C, Zwanzger P, Minov C, Holme C, Padberg
good correlation between the salivary and the non- F, Bidlingmaier M, Strasburger CJ and Rupprecht R. Evalua-
tion of a salivary based combined dexamethasone/CRH test in
protein bound plasma cortisol concentration (1). When patients with major depression. Psychoneuroendocrinology 27:
the protein bound plasma cortisol is compared to the 385 – 399, 2002
salivary cortisol level, it must be taken into account that
there is a nonlinear correlation because of the saturation 3. Klug I, Dressendörfer R, Strasburger C, Kühl GP, Reiter HL,
Reich A, Müller G, Meyer K, Kratzsch J and Kiess W. Cortisol
of the cortisol binding globulin at higher cortisol con- and 17-hydroxyprogesterone levels in saliva of healthy neo-
centrations. Therefore, we obtained a good correlation nates. Biol Neonate 78: 22 – 26, 2000
(r = 0.95; n = 84) with a hyperbolic regression function.
Even in recent literature a poor correlation has been 4. Passelergue P and Lac, G. Saliva cortisol, testosterone and T/C
ratio variations during a wrestling competition and during the
described due to the use of linear regression analysis post-competitive recovery period. Int J Sports Med 20: 109 –
(32, 33). 113, 1999
As requirement for further studies we established nor-
mal ranges for cortisol with the cortisol LEIA (Table 7). 5. Filaire E, Le Sanff C, Duché P and Lac G. The relationship be-
tween salivary adrenocortical hormones changes and personality
It is necessary to establish normal cortisol profiles be- in elite female athletes during handball and volleyball competi-
cause of the diurnal fluctuation of this hormone. As de- tion. Research Quarterly for Exercise and Sport 70 : 297 – 302,
scribed it is important to refer the cortisol values to the 1999
wake-up time of the individuals and not to the time of
6. Duclos M, Corcuff JB, Arsac L, Moreau-Gaudry F, Rashedi, M,
day. Even in newer studies this fact has not been taken Roger P, Tabarin A and Manier G. Corticotroph axis sensitivity
into account (22, 34 – 37). after exercise in endurance-trained athletes. Clinical Endocrino-
In accordance with the literature, the established day logy 48: 493 – 501, 1998
profiles in this study show a peak within 60 minutes
7. Filaire E, Duché P and Lac G. Effects of amount of training on
after awakening (13, 17 – 20). Compared to the plasma the saliva concentrations of cortisol, dehydroepiandrosterone
cortisol morning peak, the peak concentration in saliva and on the dehydroepiandrosterone :cortisol concentration ratio
is more significantly elevated and decreases more rapid- in women over 16 weeks of training. Eur. J. Appl. Physiol. 78 :
ly (39). 466 – 471, 1998
The developed assay is specific and does not cross-react 8. Hennig J, Kieferdorf P, Moritz C, Huwe S, and Netter P. Chang-
with analogues of cortisol except the drug prednisolone es in cortisol secretion during shiftwork: implications for toler-
and 11-desoxycortisol. ance to shiftwork? Ergonomics 41: 610 – 621, 1998
22 Clin. Lab. 1+2/2004
DETERMINATION OF CORTISOL BY A LUMINESCENCE-ENHANCED ENZYME IMMUNOASSAY
9. Rudolph DL and McAuley E. Cortisol and affective responses 25. Kiess W, Meidert A, Dressendörfer RA, Schriever K, Kessler U,
to exercise.Journal of Sports Sciences 16 : 121 – 128, 1998 König A, Schwarz HP, and Strasburger CJ. Salivary cortisol
levels throughout childhood and adolescence: relation with age,
10. Chatterton RT, Vogelsong, KM, Lu YC and Hudgens GA. Hor- pubertal stage and weight. Pediatr Res 40: 502 – 506, 1995
monal responses to psychological stress in men preparing for
skydiving. J Clin Endocrinol Metab 82: 2503 – 2509. 1997 26. Smyth JM, Ockenfels MC, Gorin AA, Catley D, Porter LS,
Kirschbaum C, Hellhammer DH and Stone AA. Individual
11. Lac G, Pantelidis D and Robert A. salivary cortisol response to a differences in the diurnal cycle of cortisol. Psychoneuroendo-
30 min submaximal test adjusted to a constant heart rate. J. crinology 22: 89 – 105, 1997
Sports Med Phys Fitness 37: 56 – 60. 1997
27. Gröschl M, Biskupek-Sigwart, Rauh M, Dörr HG. Measurement
12. Kirschbaum C and Hellhammer DH. Salivary cortisol in psy- of cortisol in saliva using a commercial radioimmunoassay de-
choneuroendocrine research: recent developments and applica- veloped for serum. J Lab Med 2000; 24 (6/7):314-318
tions. Psychoneuroendocrinology 19:313 – 333, 1994
28. Bablock W, Passing H, Bender R, Schneider B. A general pro-
13. Scheer FAJL and Buijs RM. Light affects morning salivary cedure for method transformation. Application of linear regres-
cortisol in humans. J Clin Endocrinol Metab 84: 3395 – 3398, sion procedures for method comparison studies in clinical chem-
1999 istry. J Clin Chem Clin Biochem 1988; 26:783-790.
14. Albrecht S, Zimmermann T, Brandl H, Saeger HD and Distler 29. Deshpande SS, ed. Enzyme immunoassays - from concept to
W. Chemiluminescence at the turn of the millenium – from an- product development. New York: Chapman & Hall, 1996.
nual fair curiosity to indispensable tool of laboratory diagnos-
tics. J Lab Med 21: 191 – 204, 1997 (German) 30. Krouwer JS, Rabinowitz R. How to improve estimates of impre-
cision. Clin Chem 1984; 30:290-292.
15. Dressendörfer RA, Kirschbaum C, Rohde W, Stahl F, and Stras-
burger CJ. Synthesis of cortisol biotin conjugate and evaluation 31. Rodbard D. Statistical quality control and routine data process-
as a tracer in an immunoassay for cortisol measurement. J Ste- ing for radioimmunoassays and immunometric assays. Clin
roid Biochem Mol Biol 7: 683 – 692, 1992 Chem 1974; 20:1255-60.
16. Bronstein I and Kricka LJ. Clinical applications of luminescent 32. Shimada M, Takahashi K, Ohkawa T, Segawa M and Higurashi
assays for enzymes and enzyme Labels. Journal of Clinical La- M. Determination of salivary cortisol by ELISA and its appli-
boratory Analysis 3: 316 – 322, 1989 cation to the assessment of the circadian rhythm in children.
Horm Res 44: 213 – 217, 1995
17. Wüst S, Wolf J, Hellhammer DH, Federenko I, Schommer N
and Kirschbaum C. The cortisol awakening response – normal 33. Calixto C, Martinez FE, Jorge SM, Moreira AC and Martinelli,
values and confounds. Noise & Health 7: 77 – 85, 2000 CE. Correlation between plasma and salivary cortisol levels in
preterm infants. J Pediatr 140: 116 – 118, 2002
18. Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federen-
ko I, Rohleder N, Schürmeyer TH and Kirschbaum C. The corti- 34. Lac G. Saliva assays in clinical and research biology. Pathol
sol response to awakening in relation to different challenge tests Biol 49: 660 – 667, 2001
and a 12-hour cortisol rhythm. Life Sciences 64: 1653 – 1660,
1999 35. Prudhomme White B, Gunnar MR, Larson MC, Donzella B and
Barr RG. Behavioral and physiological responsitivity, sleep, and
19. Pruessner JC, Hellhammer DH and Kirschbaum C. Burnout, patterns of daily cortisol production in infants with and without
Perceived stress, and cortisol responses to awakening. Psycho- colic. Child Development 71: 862 – 877, 2000
somatic Medicine 61: 197 – 204, 1999
36. Streptoe A, Cropley M, Griffith J, and Kirschbaum C. Job strain
20. Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum and anger expression predict early morning elevations in sali-
A, von Auer K, Jobst S, Kaspers F and Kirschbaum C. Free cor- vary cortisol Psychosomatic Medicine 62: 286 – 292, 2000
tisol levels after awakening: a reliable biological marker for the
assessment of adrenocortical activity. Life Sciences 61: 2539 – 37. Schommer NC, Kudielka BM, Hellhammer DH and Kirsch-
2549, 1997 baum C. No evidence for a close relationship between per-
sonality traits and circadian cortisol rhythm or a single cortisol
21. Vondrasova-Jelinkova D, Hajek I and Illnerova H. Adjustment stress response. Psychological Reports 84: 840 –842, 1999
of the human melatonin and cortisol rhythm to shortening of the
natural summer photoperiod. Brain Research 816: 249 – 253, 38. Wüst S, Federenko I, Hellhammer DH and Kirschbaum C.
1999 Genetic factors, perceived chronic stress, and the free cortisol
response to awakening. Psychoneuroendocrinology 25: 707 –
22. Antonini SRR, Jorge SM and Moreira AC. The emergence of 720, 2000
salivary cortisol circadian rhythm and its relationship to sleep
activity in preterm infants. Clinical Endocrinology 52: 423 – 39. Riad-Fahmy D, Read GF and Walker RF. Salivary steroid as-
426, 2000 says for assessing variation in endocrine activity. J Steroid Bio-
chem 19: 265 – 272, 1983
23. Bettendorf M, Albers N, Bauer J, Heinrich UE, Linderkamp O,
and Maser-Gluth C. Longitudinal evaluation of salivary cortisol 40. Meulenberg PMM and Hofman JA. The Effect of oral contra-
levels in full-term and preterm neonates. Horm Res 50:303 – ceptive use and pregnancy on the daily rhythm of cortisol and
308, 1998 cortisone. Clin Chim Acta 190: 211 – 222, 1990
24. Santiago LB, Jorge SM and Moreira AC. Longitudinal evalua- 41. Heuser I, Deuschle M, Weber A, Kniest A, Ziegler C, Weber B
tion of the development of salivary cortisol circadian rhythm in and Colla M. The role of mineralocorticoid receptors in the cir-
infancy. Clinical Endocrinology 44: 157 – 161, 1996 cadian activity of the human hypothalamus-pituitary-adrenal
system: effect of age. Neurobiology of Aging 21: 585 – 589,
2000
Clin. Lab. 1+2/2004 23
JÜRGEN WESTERMANN et al.
42. Hennig J, Firebe J, Ryl I, Krämer B, Böttcher J and Netter P. 52. Kirschbaum C, Prüssner JC, Stone AA, Federenko I, Gaab J,
Upright posture influences salivary cortisol. Psychoneuroendo- Lintz D, Schommer N and Hellhammer DH. Persistent high cor-
crinology 25: 69 – 83, 2000 tisol responses to repeated psychological stress in a subpopu-
lation of healthy men Psychosomatic Medicine 57: 468 – 474,
43. Rosmond R, Holm G, and Bjorntorp P. Food-induced cortisol 1995
secretion in relation to anthropometric, metabolic and haemo-
dynamic variables in men. Int. J. Obes. Relat. Metab. Disord. 24: 53. Kirschbaum C, Kudielka BM, Gaab J, Schommer NC and Hell-
416 – 422, 2000 hammer DH. Impact of gender, menstrual cycle phase, and oral
contraceptives on the activity of the hypothalamus-pituitary-
44. Follenius M, Brandenberger G and Hietter B. Diurnal cortisol adrenal axis. Psychosomytic Medicine 61: 154 – 162, 1999
peaks and their relationship to meals. J Clin Endocrinol Metab
55: 757 – 761, 1982 54. Kudielka BM, Hellhammer J, Hellhammer DH, Wolf OT, Pirke
KM, Varadi E, Pilz J and Kirschbaum C. Sex Differences in
45. Hucklebridge FH, Clow A, Abeyguneratne T, Huezo-Diaz P and endocrine and psychological responses to psychosocial stress in
Evans P. The awakening cortisol response and blood glu- healthy elderly subjects and the impact of a 2-week dehydroepi-
cose levels. Life Sciences 64: 931 – 937, 1999 androsterone Treatment. J Clin Endocrinol Metab 83: 1756 –
1761, 1998
46. Gonzales-Bono E, Rohleder, N, Hellhammer, DH, Salvador A
and Kirschbaum C. Glucose but not protein or fat load amplifies 55. Kudielka BM, Schmidt-Reinwald AK, Hellhammer DH and C
the cortisol response to psychosocial stress. Hormones and Be- Kirschbaum. Psychological and endocrine responses to psycho-
havior 41: 328 – 333, 2002 social stress and dexamethasone/corticotropin-releasing hor-
mone in healthy postmenopausal women and young controls:
47. Bergendahl M, Iranmanesh A, Evans WS and Veldhuis JD. the Impact of age and a two-week estradiol treatment. Neuro-
Short-term fasting selectively suppresses leptin puls mass and endocrinology 70: 422 – 430, 1999
24-h rhythmic leptin release in healthy midluteal phase women
without disturbing leptin pulse frequency or its entropy control
(pattern orderliness). J Clin Endocrinol Metab 85: 207 – 213,
2000
48. Kirschbaum C, Gonzalez-Bono E, Rohleder N, Gessner C, Pirke
KM, Salvador A and Hellhammer DH. Effects of fasting and
glucose load on free cortisol responses to stress and nicotine. J
Clin Endocrinol Metab 82: 1101 – 1105, 1997
49. Bandelow B, Wedekind D, Pauls J, Brooks A, Hajak G and
Rüther E. Salivary cortisol in panic attacks. Am J Psychiatry
157: 454 – 456, 2000
50. Smyth J, Ockenfels MC, Porter L, Kirschbaum C, Hellhammer Correspondence: Jürgen Westermann
DH and Stone AA. Stressors and mood measured on a momen- Immuno-Biological Laboratories GmbH
tary basis are associated with salivary cortisol secretion. Psy- Flughafenstraße 52a
choneuroendocrinology 23: 353 – 370, 1998
D-22335 Hamburg
51. Deinzer R, Kirschbaum C, Gresele C and Hellhammer DH. Germany
Adrenocortical responses to repeated parachute jumping and Phone +49 40 532891 36
subsequent j-CRH challenge in inexperienced healthy Subjects. Fax +49 40 532891 11
Physiol Behav 61: 507 – 511, 1997
e-mail: IBL@IBL-Hamburg.com
24 Clin. Lab. 1+2/2004
You might also like
- Cardiology - Internal Medicine, Dr. A. Mowafy (2020-2021)Document202 pagesCardiology - Internal Medicine, Dr. A. Mowafy (2020-2021)NADER ELSAYED AHMED100% (1)
- Drip ChartDocument10 pagesDrip Chartmirzaocta100% (1)
- Pone 0032496 PDFDocument7 pagesPone 0032496 PDFGeaakmalokaNo ratings yet
- Antinuclear Antibodies by Indirect Immunofluorescence: Optimum Screening Dilution For Diagnosis of Systemic Lupus ErythematosusDocument5 pagesAntinuclear Antibodies by Indirect Immunofluorescence: Optimum Screening Dilution For Diagnosis of Systemic Lupus ErythematosusMargriet MayasinNo ratings yet
- S Venner Holm 1964Document17 pagesS Venner Holm 1964vsvsuresh2099No ratings yet
- The Accuracy of Serum Osmolarity Calculation in Small Children Ta Nost Izra Unavanja Serumskog Osmolariteta U Male DeceDocument11 pagesThe Accuracy of Serum Osmolarity Calculation in Small Children Ta Nost Izra Unavanja Serumskog Osmolariteta U Male DeceMilica AdzibabaNo ratings yet
- Description of Reference Ranges for Organic Acids in Urine مهمDocument11 pagesDescription of Reference Ranges for Organic Acids in Urine مهمfarkad rawiNo ratings yet
- AN 625 LC MS Steroids Plasma AN64333 ENDocument6 pagesAN 625 LC MS Steroids Plasma AN64333 ENVeronica Weber-DragonNo ratings yet
- Estron SulfatDocument7 pagesEstron SulfatMiswar KospalaNo ratings yet
- HPLC Method For Pharmacokinetics of Cis and Trans Isomer of Cefprozil Diastereomers in Human PlasmaDocument8 pagesHPLC Method For Pharmacokinetics of Cis and Trans Isomer of Cefprozil Diastereomers in Human PlasmaIOSR Journal of PharmacyNo ratings yet
- Epilepsia - 2009 - La Marca - A New Rapid Micromethod For The Assay of Phenobarbital From Dried Blood Spots by LC TandemDocument5 pagesEpilepsia - 2009 - La Marca - A New Rapid Micromethod For The Assay of Phenobarbital From Dried Blood Spots by LC TandemWaode RahmahNo ratings yet
- Blood Pressure, Heart Rate, and Urinary Catecholamines inDocument9 pagesBlood Pressure, Heart Rate, and Urinary Catecholamines inJoão Marcel CamargoNo ratings yet
- Physiologic and Pathologic Levels of Reactive Oxygen Species in Neat Semen of Infertile MenDocument6 pagesPhysiologic and Pathologic Levels of Reactive Oxygen Species in Neat Semen of Infertile MenMihajilo TosicNo ratings yet
- Pharmacokinetics and Concentration-Effect Relationship of Oral LSD in HumansDocument7 pagesPharmacokinetics and Concentration-Effect Relationship of Oral LSD in HumansasdadasdasNo ratings yet
- 1 s2.0 S0731708516312808 MainDocument7 pages1 s2.0 S0731708516312808 MainSergeat18BNo ratings yet
- Effect of Storage Time and Temperature On Some Serum Analytes8.21 PDFDocument4 pagesEffect of Storage Time and Temperature On Some Serum Analytes8.21 PDFyunitaNo ratings yet
- Assessmentof Fetal Lungmaturity:Lecithin/ Sphingomyelinratiovs. Cortisoland Foam-Test AssaysDocument4 pagesAssessmentof Fetal Lungmaturity:Lecithin/ Sphingomyelinratiovs. Cortisoland Foam-Test AssaysPatrick RamosNo ratings yet
- Arnhard 2012Document14 pagesArnhard 2012malwanafhc.adNo ratings yet
- 003-CC 1970 Cotlove-Biol & Analyt Components of Var 3 Physiol and MedicalDocument5 pages003-CC 1970 Cotlove-Biol & Analyt Components of Var 3 Physiol and MedicalFernando Cava ValencianoNo ratings yet
- Metabolic Fingerprinting of Royal Jelly: Characterization and Proof of AuthenticityDocument6 pagesMetabolic Fingerprinting of Royal Jelly: Characterization and Proof of AuthenticitycostytzuNo ratings yet
- Volume - 41 - 4 - 97 - 3 - MacacaDocument16 pagesVolume - 41 - 4 - 97 - 3 - MacacaAnindyaMustikaNo ratings yet
- Influence of Biological Variations and Sample Handling On Measured Microalbuminuria in Diabetic PatientsDocument7 pagesInfluence of Biological Variations and Sample Handling On Measured Microalbuminuria in Diabetic PatientsJ DNo ratings yet
- Biomedical Chromatography - 2011 - Mendes - Quantification of Cyproheptadine in Human Plasma by High Performance LiquidDocument8 pagesBiomedical Chromatography - 2011 - Mendes - Quantification of Cyproheptadine in Human Plasma by High Performance LiquidLuiz Fernando RibeiroNo ratings yet
- Package Insert 13695 - HCG D - en - 30405-01 PDFDocument10 pagesPackage Insert 13695 - HCG D - en - 30405-01 PDFadybaila4680No ratings yet
- Earwax As An Alternative Specimen For Forensic AnalysisDocument11 pagesEarwax As An Alternative Specimen For Forensic AnalysisNAYARA MOREIRA DAMASCENONo ratings yet
- Effects of Cypermethrin On Rainbow Trout (Oncorhynchus Mykiss)Document9 pagesEffects of Cypermethrin On Rainbow Trout (Oncorhynchus Mykiss)Daniel Morales CespedesNo ratings yet
- Variance of Melatonin and Cortisol Rhythm in Patients With Allergic RhinitisDocument4 pagesVariance of Melatonin and Cortisol Rhythm in Patients With Allergic RhinitisalfredoibcNo ratings yet
- Shin - Hypocholesterolemic Effect of Daily Fisetin Supplementation in High Fat Fed Sprague-Dawley Rats - 2013Document7 pagesShin - Hypocholesterolemic Effect of Daily Fisetin Supplementation in High Fat Fed Sprague-Dawley Rats - 2013thrNo ratings yet
- Reproductive Toxicology of Tartrazine (FD and C Yellow No. 5) in Swiss Albino MiceDocument6 pagesReproductive Toxicology of Tartrazine (FD and C Yellow No. 5) in Swiss Albino MiceMuchtar RezaNo ratings yet
- Androgenic Status of Lepromatous Leprosy Patients With GynecomastiaDocument6 pagesAndrogenic Status of Lepromatous Leprosy Patients With GynecomastianadyaNo ratings yet
- Estradiol and Progesterone Fecal Metabolites Analysis in Crab-Eating-FoxDocument5 pagesEstradiol and Progesterone Fecal Metabolites Analysis in Crab-Eating-FoxTiago AmaralNo ratings yet
- The Plasma Sugar, Free Fatty Acid, Cortisol, and Growth Hormone Response Insulin. I. in Control SubjectsDocument8 pagesThe Plasma Sugar, Free Fatty Acid, Cortisol, and Growth Hormone Response Insulin. I. in Control SubjectsYng TangNo ratings yet
- Journal of Pharmaceutical and Biomedical Analysis Volume 125 Issue 2016 (Doi 10.1016/j.jpba.2016.03.024) Abdallah, Inas A. Hammell, Dana C. Hassan, Hazem E. Stinchcom - Norelgestromin - Ethinyl eDocument9 pagesJournal of Pharmaceutical and Biomedical Analysis Volume 125 Issue 2016 (Doi 10.1016/j.jpba.2016.03.024) Abdallah, Inas A. Hammell, Dana C. Hassan, Hazem E. Stinchcom - Norelgestromin - Ethinyl eTri HandayaniNo ratings yet
- Preparation of Extracts and Analytical Chemistry: Supporting Information Extended Material and MethodsDocument10 pagesPreparation of Extracts and Analytical Chemistry: Supporting Information Extended Material and Methodsjuan arellano olivaresNo ratings yet
- Rodriguez G - Serum ACE Activity in Normal Children and in Those With SarcoidosisDocument5 pagesRodriguez G - Serum ACE Activity in Normal Children and in Those With SarcoidosisPhaimNo ratings yet
- 1 s2.0 S2095311916613862 MainDocument12 pages1 s2.0 S2095311916613862 MainGOKULA PRIYA R 19EC005No ratings yet
- NEJM appendixPDF2020Document7 pagesNEJM appendixPDF2020Marin AndreiNo ratings yet
- A Case of Severe Hypertriglyceridaemia and HypercholesterolaemiaDocument1 pageA Case of Severe Hypertriglyceridaemia and Hypercholesterolaemiathys2000No ratings yet
- 2018 SAB Presentation Division of Biochemical Toxicology Research Overview - 3Document21 pages2018 SAB Presentation Division of Biochemical Toxicology Research Overview - 3hellion00No ratings yet
- 30 - Evaluation of Prostate-Specific Antigen (PSA) Membrane Test Assays For The Forensic Identification of Seminal Fluid PDFDocument4 pages30 - Evaluation of Prostate-Specific Antigen (PSA) Membrane Test Assays For The Forensic Identification of Seminal Fluid PDFMN IrshadNo ratings yet
- Comparative Evaluation of Pyrogens Tests in Pharmaceutical ProductsDocument6 pagesComparative Evaluation of Pyrogens Tests in Pharmaceutical Productsnamchin parkNo ratings yet
- Tricyclic Antidepressant GC-MSDocument6 pagesTricyclic Antidepressant GC-MSrodrigoNo ratings yet
- Original Articles A Simple, Isocratic High-Performance Liquid Chromatography Assay For Linezolid in Human SerumDocument4 pagesOriginal Articles A Simple, Isocratic High-Performance Liquid Chromatography Assay For Linezolid in Human Serumharold.atmajaNo ratings yet
- Tlili2011 PDFDocument5 pagesTlili2011 PDFManju ManoharNo ratings yet
- Package Insert - 06038 - HCG - en - 30405 Europa PDFDocument7 pagesPackage Insert - 06038 - HCG - en - 30405 Europa PDFadybaila4680No ratings yet
- Mls 111b LAb MidDocument10 pagesMls 111b LAb MidJohanna MarieNo ratings yet
- Impact of Anticoagulants On Assessment of Zinc in Plasma: Croat. Chem. Acta 2018, 91 (3), 317-321Document5 pagesImpact of Anticoagulants On Assessment of Zinc in Plasma: Croat. Chem. Acta 2018, 91 (3), 317-321Andrea CardenaNo ratings yet
- ReproDocument3 pagesReproRiyaduNo ratings yet
- Detection and Quantification of Benzodiazepines An Z-DrugsDocument16 pagesDetection and Quantification of Benzodiazepines An Z-DrugsDFNo ratings yet
- Bioequivalence Study of Two Formulations of Bisoprolol Fumarate Tablets in Healthy SubjectsDocument7 pagesBioequivalence Study of Two Formulations of Bisoprolol Fumarate Tablets in Healthy SubjectsSan-Clin-Eq LaboratoryNo ratings yet
- Clinical & Diagnostic Tests For GpatDocument10 pagesClinical & Diagnostic Tests For GpatSHRIKANTNo ratings yet
- DEM-DEE007 Leptin ELISA 160503 MDocument26 pagesDEM-DEE007 Leptin ELISA 160503 MSusana Méndez GómezNo ratings yet
- Camparison Monovalente AntivenomsDocument1 pageCamparison Monovalente AntivenomsAndrea BaracaldoNo ratings yet
- Jurnal Amlodipin UdtDocument7 pagesJurnal Amlodipin UdtdidiisafitriNo ratings yet
- Comparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsDocument5 pagesComparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsgeoaislaNo ratings yet
- ALBUMIN BLOSR6x02 ENDocument2 pagesALBUMIN BLOSR6x02 ENMeethuanNo ratings yet
- Quantification of Pregabalin Using Hydrophilic Interaction HPLC-High-Resolution MS in Postmortem Human Samples: Eighteen Case ReportsDocument6 pagesQuantification of Pregabalin Using Hydrophilic Interaction HPLC-High-Resolution MS in Postmortem Human Samples: Eighteen Case ReportsLuisa Fernanda Velásquez QuijanoNo ratings yet
- Glucose (God Pap)Document2 pagesGlucose (God Pap)anggun990% (1)
- Journal Lesitin RasioDocument3 pagesJournal Lesitin RasioSUSANNo ratings yet
- 2Document8 pages2Chorrinha ChorraNo ratings yet
- ETAPDocument8 pagesETAParulprakashf.sdcNo ratings yet
- Clock Drawing Test PDFDocument6 pagesClock Drawing Test PDFfissionmailedNo ratings yet
- Toovey 2007Document22 pagesToovey 2007fissionmailedNo ratings yet
- NIH Public Access: The Teenage Brain: The Stress Response and The Adolescent BrainDocument11 pagesNIH Public Access: The Teenage Brain: The Stress Response and The Adolescent BrainfissionmailedNo ratings yet
- 1999 Anyas PDFDocument3 pages1999 Anyas PDFfissionmailedNo ratings yet
- Cystic Disease The Liver and Biliary: TractDocument7 pagesCystic Disease The Liver and Biliary: TractfissionmailedNo ratings yet
- LKPD - Recount Text 2Document2 pagesLKPD - Recount Text 2Sabian KalifiNo ratings yet
- Measles EpiDocument22 pagesMeasles Epiمحمد صالحNo ratings yet
- Complications of Diabetes MellitusDocument147 pagesComplications of Diabetes MellitusNisrina SariNo ratings yet
- CEA Pilgastrim Vs FilgastrimDocument13 pagesCEA Pilgastrim Vs FilgastrimMaya Aulia MulakhaillaNo ratings yet
- The Small Intestine Channel - Discernment, Sorting, Mental ClarityDocument5 pagesThe Small Intestine Channel - Discernment, Sorting, Mental Clarityلوليتا وردةNo ratings yet
- Clinical Practice Guidelines For Management of Bipolar DisorderDocument16 pagesClinical Practice Guidelines For Management of Bipolar DisorderKavita kumariNo ratings yet
- Oropharyngeal and Nasopharyngeal SuctioningDocument2 pagesOropharyngeal and Nasopharyngeal SuctioningAlana Caballero100% (1)
- Hepatitis C Education Class - 2009Document64 pagesHepatitis C Education Class - 2009BENNo ratings yet
- Lam. Pathway Gagal Jantung KongestiDocument2 pagesLam. Pathway Gagal Jantung KongestiMegawati Dwi PutriNo ratings yet
- Hubungan Kepadatan Hunian, Kelembaban Dan Status GiziDocument16 pagesHubungan Kepadatan Hunian, Kelembaban Dan Status GiziBenny SimanjuntakNo ratings yet
- Radio PsaDocument3 pagesRadio Psaapi-356356986No ratings yet
- Mechanical Ventilation in Pediatric PatientDocument11 pagesMechanical Ventilation in Pediatric PatientHandris YanitraNo ratings yet
- Vaccines 08 00321Document17 pagesVaccines 08 00321Kshitiz Raj ShresthaNo ratings yet
- Introduction and Around The World W Dr. Boyd": COVID-19 ResourcesDocument10 pagesIntroduction and Around The World W Dr. Boyd": COVID-19 ResourcesNabillahNo ratings yet
- OsteomyelitisDocument20 pagesOsteomyelitisYusri HarisNo ratings yet
- KoshtaDocument15 pagesKoshtaPanchakarma DepartmentNo ratings yet
- GONORRHOEADocument23 pagesGONORRHOEADwi Fikha AprilyantiNo ratings yet
- Effect of Single-Dose Antibiotic Prophylaxis Versus Conventional Antibiotic Therapy in Surgery A Randomized Controlled Trial in A Public Teaching HospitalDocument5 pagesEffect of Single-Dose Antibiotic Prophylaxis Versus Conventional Antibiotic Therapy in Surgery A Randomized Controlled Trial in A Public Teaching HospitalكنNo ratings yet
- War Card GameDocument2 pagesWar Card Gameapi-541744798No ratings yet
- Group 3 QUIZDocument4 pagesGroup 3 QUIZJessa Mae OhaoNo ratings yet
- Medication and Treatment Sheet: Mariano Marcos Memorial Hospital and Medical CenterDocument4 pagesMedication and Treatment Sheet: Mariano Marcos Memorial Hospital and Medical CenterWyn AgustinNo ratings yet
- Nueva Ecija University of Science And: A Case Analysis ofDocument68 pagesNueva Ecija University of Science And: A Case Analysis ofShane PangilinanNo ratings yet
- Episkleritis Dan SkleritisDocument41 pagesEpiskleritis Dan SkleritisSuryana AdityaNo ratings yet
- Normal Parturition and Management of Dystocia in Dogs and CatsDocument7 pagesNormal Parturition and Management of Dystocia in Dogs and Catsmcs.vet8473No ratings yet
- Liver Cirrhosis LectureDocument83 pagesLiver Cirrhosis LectureSheila Regina Tiza100% (1)
- Drug StudyDocument7 pagesDrug StudyAnn Therese C. GutierrezNo ratings yet
- Point of Care Ultrasound (Pocus) : Introduction: George A. FoxDocument76 pagesPoint of Care Ultrasound (Pocus) : Introduction: George A. FoxAna Belen Viteri LuzuriagaNo ratings yet
- List of Medical and Nursing Abbreviations, Acronyms, Terms 1 - NurseslabsDocument25 pagesList of Medical and Nursing Abbreviations, Acronyms, Terms 1 - NurseslabsbeingfiredNo ratings yet