Professional Documents
Culture Documents
"A Fun Hazily Snail Barn-Aftermaster": Neisseria Gonorrhea and Chlamydia Trachomatis
"A Fun Hazily Snail Barn-Aftermaster": Neisseria Gonorrhea and Chlamydia Trachomatis
Uploaded by
Ike Rillera100%(1)100% found this document useful (1 vote)
58 views3 pagesThe document provides details on performing a pelvic examination, including:
1. Examining the external genitalia, vagina, and cervix using a speculum to inspect for abnormalities, discharge, or lesions.
2. Performing bimanual palpation to evaluate the size, shape, position, mobility and tenderness of the uterus, adnexa, and cul-de-sac.
3. Optionally conducting a rectovaginal or rectal examination to further assess the pelvic structures and check for masses, irregularities, or tenderness.
Original Description:
ofc gyne
Original Title
Office Gynecology
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document provides details on performing a pelvic examination, including:
1. Examining the external genitalia, vagina, and cervix using a speculum to inspect for abnormalities, discharge, or lesions.
2. Performing bimanual palpation to evaluate the size, shape, position, mobility and tenderness of the uterus, adnexa, and cul-de-sac.
3. Optionally conducting a rectovaginal or rectal examination to further assess the pelvic structures and check for masses, irregularities, or tenderness.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
100%(1)100% found this document useful (1 vote)
58 views3 pages"A Fun Hazily Snail Barn-Aftermaster": Neisseria Gonorrhea and Chlamydia Trachomatis
"A Fun Hazily Snail Barn-Aftermaster": Neisseria Gonorrhea and Chlamydia Trachomatis
Uploaded by
Ike RilleraThe document provides details on performing a pelvic examination, including:
1. Examining the external genitalia, vagina, and cervix using a speculum to inspect for abnormalities, discharge, or lesions.
2. Performing bimanual palpation to evaluate the size, shape, position, mobility and tenderness of the uterus, adnexa, and cul-de-sac.
3. Optionally conducting a rectovaginal or rectal examination to further assess the pelvic structures and check for masses, irregularities, or tenderness.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
Office Gynecology iii.
Mucosal characteristics-color, lesions, superficial
Gynecology vascularity, edema
iv. Structural abnormalities
Pap smear, gram stain, Normal Saline Solution (NSS) smear (for
HISTORY AND PHYSICAL EXAMINATION Dx of Trichomoniasis or bacterial vaginosis), KOH smear (for
fungal infection), Whiff test (differentiate presence of bacterial
After a dialogue has been established vaginosis from fungal infection, it’s positive for Trichomonas
Will rely on good doctor-patient relationship or interchange and bacterial vaginosis-how: put specimen on a slide then drop
Attention to details KOH, if it exudes amide like odor: (+) for Whifft test)
Risk factors identified Inspect cervix for unusual bleeding, inflammatory lesions,
History polyps and carcinoma
i. Chief complaint, present illness
ii. Complete medical and surgical history, reproductive
history (including menstrual history) Bimanual palpation:
iii. A thorough family and social history
Chief complaint and history of present illness The pelvic organs can be outlined by bimanual palpation.
i. Allow patient to talk about her chief complaint i. Introduce the well lubricate index and middle finger into
i.i Temporal relation to total duration of the illness the vagina at its posterior aspect near the
perineumadvance fingers until cervix is encountered
ii. Associated symptoms ii. Press the abdominal hand very gently downward, pushing
ii.i Put in chronological order, character of each symptom the pelvic structures toward the palpating vaginal fingers
Evaluate the body of uterus for:
ii.ii Pertinent negative and positive symptoms i. Position: anteverted (if uterus is directed anteriorly with
the fundus of the uterus pressing against the urinary
iii. Differential diagnosis bladder) or retroverted (uterus is directed posteriorly with
Thorough the fundus of the uterus towards the rectum)
i. Vital signs ii. Architecture, size, shape, symmetry, tumor
ii. Breast examination iii. Consistency
iii. Abdomen iv. Tenderness
Intra-abdominal mass v. Mobility
Organomegaly Evaluate the cervix for position, architecture, consistency and
Distention of bowels tenderness especially on the mobility of cervix, then explore
iv. Pelvic examination the anterior, posterior and lateral fornices
Place the “vaginal” fingers in the right lateral fornix and the
“abdominal“ hand on the right lower quadrant
Method of Female Pelvic Examination i. Outline the adnexa: palpate fallopian tube and ovary w/c
signifies enlarge ovary and fallopian tube
The patient is instructed to empty the bladder ii. A normal tube and ovary are not palpated
She is placed in dorsal lithotomy position: patient’s feet should iii. Adnexal mass is evaluated for its:
rest comfortably in the stirrups with the edge of the buttocks at o Location relative to the uterus and cervix
the lower end of the table o Architecture
The patient is draped properly o Consistency
External genitalia o Tenderness
i. Inspect mons pubis, labia majora, labia minora, perineal o Mobility
body and anal region for characteristics of the skin, hair Palpate the left adnexal region, repeating technique described
distribution, contour and swelling above
ii. Inspect the epidermal and mucosal characteristics and If a mass is fixed near the adnexal and mass is not movable, it is
anatomic configuration of: labia minora, clitoris, urethra more of a malignant process
orifice, vaginal outlet, hymen, perineal body, anus Follow the bimanual examination with a rectovaginal
iii. Disease of Skene’s gland (palpate anterior vaginal wall) abdominal examination: commonly done with post menopausal
and Bartholin’s gland (palpate posterior part of labia and pre menopausal women
majora) if disease is suspected i. Insert index finger into the vagina and middle finger into
Introitus: instruct the patient to bear down to rule out the rectum
i. Cystocele ii. Place other hand on infraumbilical region pushing the
ii. Rectocele structure
iii. Uterine prolapse iii. Assess the cul-de-sac
Vagina and Cervix In virginsrectal-abdominal technique: both fingers inserted in
i. Inspect using a speculum the rectum
ii. Proper insertion of speculum
o Instrument is warmed with tap water, not lubricated Rectal Examination
o Select proper size speculum
o Insert with blades in vertical position, closed and Inspect the perineal and anal area, the pilonidal
pressed against the perineum (sacrococcygeal) region and perineum for: a. color b.
o When fully inserted, rotate blades into horizontal lesions
position (can see cervix and lateral vaginal wall) Instruct the patient to “strain down”
o Open blades until cervix is exposed Palpate the pilonidal area, ischiorectal fossa, perineum
o Gently rotate speculum until all surfaces are and the perianal region before inserting the gloved finger
visualized into the anal canal
o Multigravida and used a smaller speculum-won’t see Palpate the anal canal and rectum with a well lubricated
the vagina gloved index finger
Inspect the vagina for the following Evaluate the anal canal for
i. Presence of blood o Sphincter tone
ii. Discharge-any purulence should be cultured to identify o Tenderness
Neisseria gonorrhea and Chlamydia trachomatis i. Tight sphincter
ii. Anal fissure
“a fun hazily snail barn-aftermaster” Page 1
iii. Painful hemorrhoids i. Young child:
o Tumor or irregularities especially at pectinate line ii. Toddler or infant: held in their mother’s arms. Mother
o Superior aspect (clothed) on examination table (feet in stirrup) with child
Evaluate the rectum on her lap. Others:
o Anterior wall o Knee-chest position
i. Cervix size, shape, symmetry, consistency, o Use of anesthesia
tenderness o Hysteroscope, cystoscope, etc.
ii. Uterine or adnexal masses
iii. Rectouterine fossa for tenderness or implants
o Right lateral wall, left lateral wall, posterior wall Examination of the Adolescent Patient
Examine the finger after its withdrawn:
o Gross blood, pus or other alterations in color or Earn patient’s trust, explain components of examination, use
consistency careful and gentle technique
o Smear stool to test for occult blood Indications for pelvic examination:
o She has had intercourse
o Positive pregnancy test
Abdominal examination o With abdominal pain
o Marked anemia
i. Supine position o Heavy bleeding
o Relaxed position Rectal examination is done if she is a virgin
o Pillow under the head Confidentiality is an important issue in adolescent health care
ii. Inspect for signs of intra-abdominal mass, organomegaly
or distention
iii. Initial palpation Follow up
o Liver
o Spleen Routine care patients with no disease
o Other abdominal contents, mass effect Further assessment, treatment plan for those with S/S
iv. All four quadrants Referral to other specialists if needed
v. Systemic approach- e.g. clockwise
vi. Percussion to measure the liver
vii. Auscultation-bowel sounds MINOR DIAGNOSTIC PROCEDURES
o Intestinal obstruction- “rushes” or “high-pitched”
sound 1. Papaniculao Smear (Pap smear)
o Ileus-less frequent but same pitch as normal For detection of carcinoma of the cervic and its precursors, as
bowel sound well as viral, bacterial, fungal or protozoal pathogens
Has reduced incidence of invasive cervical CA by 50%
Initial screening at age 18
Speculum Examination (Graves or Pederson) Annual screening for high risk patients
1-2 years screening for low risk patients
i. Smallest with adequate visualization Supplies
ii. Speculum warmed with warm water i. Cervical scraper: cotton pledgets, ayre’s spatula, cervical
iii. Cervix and vagina carefully inspected brush
iv. PAP smear ii. Glass slides
v. Biopsy of any lesions iii. Fixative: 95% alcohol, spray net
vi. Endometrial biopsy Instructions:
vii. Culture of purulent discharge i. No douche for 48 hrs before procedure
viii. A vaginal and cervical cytology done as screening tool for ii. No vaginal creams 1 wk before
cervical neoplasm iii. No coitus for 24 hrs in advance
After speculum is removed1st and 2nd fingers are inserted Technique:
gently into the vagina o Samples from both endocervix and exocervix
Carefully palpate: o Saline moistened cotton-tipped swab
i. Vagina i. No lubricant
ii. Fornices ii. Place the endocervical brush or cotton swab inside the
iii. Cervix endocervix and roll it firmly against canal
Opposite hand placed on patient’s abdomen (above symphysis iii. Remove the brush or swab and place sample on slide
pubis) iv. Place the spatula on cervix with longer protrusion in
Uterus assessed well cervical canal
Adnexa, gently palpated on both sides v. Rotate spatula clockwise 360o firmly on the cervix
On postmenopausal and premenopausal women in whom there enough to cover the entire transformation zone
is difficulty in ascertaining adnexal structure vi. Immediately fix the slide with either spray fixative or
Also to rule out possibility of concurrent rectal disease 95% ethanol fixative
Check on
i. Sphincter muscles
ii. Support of pelvis 4 sources of error:
iii. Masses and hemorrhoids i. Improper collection
iv. At completion of examination, patient should be informed ii. Poor transfer from collecting device to slide
about the findings. iii. Air drying
iv. Contamination with lubricant
Identification:
Examination of the Pediatric Patient i. Name, age, pregnancy status, LMP
ii. Pertinent history: hormonal therapy, radiation therapy,
Careful examination recent surgery, postpartum state, IUD
Familiarity with normal appearance of prepubertal
genitaliamildly erythematous
Positions:
“a fun hazily snail barn-aftermaster” Page 2
2. Colposcopy ii. Invasive cervical cancer have been ruled out
iii. Endocervical canal is uninvolved
Visualization of the vulva, vagina and cervix using a binocular iv. The lesion must be well encompassed by the freeze
microscope of low magnification (10-40x) and strong light v. There are no deep or excessive involvement of cervical
Uses: clefts
i. To supplement cytology vi. The patient is reliable for follow-up
ii. To direct biopsy Technique:
iii. Used before cones or hysterectomy for CIN III i. Choose an appropriate probe which will cover the entire
iv. Evaluation of lesions of the vagina and vulva lesion
v. Used in follow-up: cervical carcinoma, adenosis, CIN IIII ii. Freeze for 3 minutes, start timing when the edge of ice ball
Technique: has protruded 3-5 mm beyond the probe
i. With the patient in dorsal lithotomy position, an iii. Thaw for 3 minutes
unlubricated vaginal speculum is inserted iv. Refreeze for 3 minutes
ii. The cervix is exposed, taking care not to traumatize it
iii. The vagina and cervix are inspected with the surface
moistened with normal saline Other Diagnostic Procedures
iv. Acetic acid solution (3-5%) is applied to the cervix with
moistened cotton balls 1. Hysterosonosalpingogram
Abnormal colposcopic findings:
i. Acetowhite epithelium Part of evaluation of the patency of tubes in an infertile couple
ii. Punctation Similar to hysterosalpingogram
iii. Mosaic Done in the first half of the cycle after the menstrual flow and
iv. Leukoplakia before ovulation
v. Abnormal blood vessels Prophylactic antibiotics are given
Technique
i. Insert a vaginal speculum
3. Vulvar biopsy ii. With the cervical os visualized, insert a small foley catheter
aseptically into uterine cavity and inflate balloon with 3 cc
If a vulvar lesion has failed to respond to therapy of air or saline
Suspicion of malignant or premalignant condition iii. Do a baseline transvaginal US to visualize the uterus,
Careful inspection with colposcope endometrial stripe and adnexa
Infiltration with local anesthesia iv. Instill 10 cc of normal saline into catheter to visualize
Keyes punch biopsy with gentle rotation until full thickness of endometrial canal
skin has been reached v. Instill additional 10-20 cc of fluid until patency of both
Pressure over biopsy area to stop bleeding tubes is established. Fluid may be seen coursing through
the tubes, or fluid is seen in the cul-de-sac on both sides of
the uterus
4. Endometrial biopsy
For abnormal uterine bleeding 2. Urologic Evaluation
Easier, faster, more convenient, less costly
Can establish the diagnosis of a malignant or premalignant For women with urinary incontinence
lesion Differentiate if urinary symptoms are sensory or functional
Types of curette Sensory disorders are characterized by dysuria, frequency,
i. Randall-type suction of endoervical and endometrial canal urgency and sometimes incontinence. These are usually treated
ascertained by passing a blunt sound medically.
ii. Novak curette Functional disorders are mainly manifeste as difficulty in
Depth and direction of endocervical and endometrial canal voiding control.
ascertained by passing a blunt sound Technique of office cystometry
Curette the different quadrants of the endometrium from the i. Before examination, the patient is asked to void
fundus to the internal os ii. If the bladder remains palpable, it is catherized and
Indications: residual urine is measured
i. Abnormal Uterine Bleeding/postmenopausal bleeding iii. A 50 ml asepto syringe is attached to the catheter and held
ii. Endometrial dating just above the level of the pubis
iii. Follow up of previously diagnosed endometrial hyperplasia iv. 50 ml increments of saline is infused
iv. Evaluation of patient with 1 yr amenorrhea v. The bladder volume at the first urge to void is noted
v. Evaluation of infertility
vi. Pap smear with atypical cells favoring endometrial origin
Contraindications:
i. Pregnancy
ii. Acute pelvic inflammatory disease (PID)
iii. Clotting disorder (coagulopathy)
iv. Acute cervical and vaginal infection
v. Cervical cancer
vi. Morbid obesity
vii. Severe cervical stenosis
viii. Severe pelvic relaxation w/ uterine descensus
5. Cryosurgery
Use: ablation of benign and pre-malignant lesions of cervix,
vaginal and vulva
Criteria for patient selection:
i. The entire lesion must be visible
“a fun hazily snail barn-aftermaster” Page 3
You might also like
- Gynecology PDFDocument18 pagesGynecology PDFKatheryn100% (2)
- Suture Practice Kit Ebook PDFDocument18 pagesSuture Practice Kit Ebook PDFKarla Aguilar GuerreroNo ratings yet
- TeratologyDocument34 pagesTeratologyธิติวุฒิ แสงคล้อย100% (1)
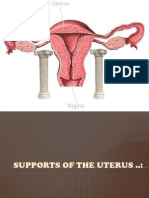
- Supports of The UterusDocument20 pagesSupports of The UterusAshwin Prem Solomon100% (1)
- Office Gynecology: Princess Cony CayabaDocument60 pagesOffice Gynecology: Princess Cony CayabaCarla Dela CruzNo ratings yet
- Pelvic Examiantion: BY: Charisse Ann G. GasatayaDocument27 pagesPelvic Examiantion: BY: Charisse Ann G. GasatayaCharisse Ann GasatayaNo ratings yet
- InfertilityDocument14 pagesInfertilityDrChauhanNo ratings yet
- Obstetrics PDFDocument14 pagesObstetrics PDFKatheryn100% (1)
- Physiology of LaborDocument49 pagesPhysiology of LaborGunung MahameruNo ratings yet
- 1-Obs&Gynae - Anatomy and Embryology of The Female Reproductive SystemDocument52 pages1-Obs&Gynae - Anatomy and Embryology of The Female Reproductive Systemfadiawwad100% (4)
- Physiological Changes of PregnancyDocument40 pagesPhysiological Changes of PregnancyAita AladianseNo ratings yet
- AmenorrheaDocument23 pagesAmenorrheaKarmmanya Razahani PurnamaNo ratings yet
- ObGyn Board Review PDFDocument85 pagesObGyn Board Review PDFCoolrobertizNo ratings yet
- Benign Gynecologic Lesions FinalDocument11 pagesBenign Gynecologic Lesions Final2012100% (4)
- 62 Lecture Menstrual Cycle Abnormalities, Infertility, MenopauseDocument69 pages62 Lecture Menstrual Cycle Abnormalities, Infertility, MenopauseTarek TarekNo ratings yet
- Blood Supply Pelvic OrgansDocument39 pagesBlood Supply Pelvic OrgansoliviaNo ratings yet
- Benign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDocument83 pagesBenign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDian Permata PutraNo ratings yet
- Benign Disease of The UterusDocument27 pagesBenign Disease of The UterusnyangaraNo ratings yet
- Early Pregnancy Complications: Ectopic Pregnancy Gestational Trophoblastic Disease Ji Aggasid, JanniecelDocument60 pagesEarly Pregnancy Complications: Ectopic Pregnancy Gestational Trophoblastic Disease Ji Aggasid, JanniecelmedicoNo ratings yet
- Total Abdominal Hysterectomy and Bilateral Salpingo-OophorectomyDocument12 pagesTotal Abdominal Hysterectomy and Bilateral Salpingo-OophorectomyBadri KobalavaNo ratings yet
- Diagnosis and Management of Pelvic Organ ProlapseDocument47 pagesDiagnosis and Management of Pelvic Organ ProlapseWindy Puspa Kusumah100% (1)
- MHN TerminologyDocument27 pagesMHN Terminologydonb27529No ratings yet
- Stroke & Hemiplegia LocalizationDocument54 pagesStroke & Hemiplegia LocalizationVasu PottabatthiniNo ratings yet
- OBGYN Clinical RotationDocument5 pagesOBGYN Clinical Rotationriczen mae vilaNo ratings yet
- Aquifer Case - Summary - FamilyMedicine17 - 55-YDocument9 pagesAquifer Case - Summary - FamilyMedicine17 - 55-YHyunsoo EllisNo ratings yet
- Management of Labor and DeliveryFrom EverandManagement of Labor and DeliveryGeorge A. MaconesNo ratings yet
- Prenatal Assessments by TrimesterDocument6 pagesPrenatal Assessments by TrimesterMauZungNo ratings yet
- Pediatric HistoryDocument96 pagesPediatric Historyapi-3712326100% (2)
- Neurofibromatosis in PregnancyDocument2 pagesNeurofibromatosis in PregnancyDwi Wahyu AprianiNo ratings yet
- Obs History Taking FormatDocument24 pagesObs History Taking FormatBibek PandeyNo ratings yet
- Understanding Basic Obstetrics and GynaecologyDocument60 pagesUnderstanding Basic Obstetrics and GynaecologyleaslimNo ratings yet
- Intraepithelial Neoplasia of The Lower Genital TractDocument54 pagesIntraepithelial Neoplasia of The Lower Genital TractDee Sarajan100% (1)
- Cesarean Section: Associate Professor Ph.D. E.A. EinyshDocument33 pagesCesarean Section: Associate Professor Ph.D. E.A. EinyshPrerit Aggarwal100% (1)
- Gynecology Abnormal Bleeding 2014aDocument8 pagesGynecology Abnormal Bleeding 2014aBhi-An BatobalonosNo ratings yet
- Obgyn Osce - Ob HistoryDocument3 pagesObgyn Osce - Ob HistoryErika Leah ManaloNo ratings yet
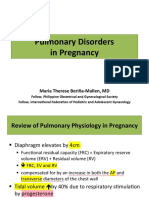
- Pulmonary Disorders in PregnancyDocument49 pagesPulmonary Disorders in PregnancyMara Medina - BorleoNo ratings yet
- Genital ProlapseDocument13 pagesGenital ProlapsesmbawasainiNo ratings yet
- Vaginal Bleeding in Pregnancy - 5-Minute Emergency ConsultDocument6 pagesVaginal Bleeding in Pregnancy - 5-Minute Emergency ConsultLaoMed plusNo ratings yet
- History TakingDocument26 pagesHistory TakingShauie CayabyabNo ratings yet
- (New) Early Pregnancy Complications RDocument51 pages(New) Early Pregnancy Complications RMesk Banat100% (2)
- Menopause NotesDocument5 pagesMenopause NotesJU WSD100% (1)
- Endometriosis GuidelineDocument44 pagesEndometriosis GuidelineHen DriNo ratings yet
- Reproductive Endocrinology FinalDocument98 pagesReproductive Endocrinology FinalChino Paolo SamsonNo ratings yet
- Examination of The Sensory SystemDocument17 pagesExamination of The Sensory SystemPaulo Henrique Neto Pais100% (1)
- Gynecology: 3.09 - AmenorrheaDocument13 pagesGynecology: 3.09 - AmenorrheaAnna Mae MarantanNo ratings yet
- Congenital Malformations of The Female Genital TractDocument7 pagesCongenital Malformations of The Female Genital TractDo le QuangNo ratings yet
- Leah M. Schenk, MD Infertility Reproductive EndocrinologyDocument2 pagesLeah M. Schenk, MD Infertility Reproductive EndocrinologyLeah M. Schenk MD100% (2)
- Management Normal Labor 2021 SBOGDocument118 pagesManagement Normal Labor 2021 SBOGAHMED .KNo ratings yet
- Amenorrhea - Algorithm & DifferentialsDocument9 pagesAmenorrhea - Algorithm & DifferentialsItharshan IndreswaranNo ratings yet
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementFrom EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementNo ratings yet
- Obgyn Osce - Breast ExaminationDocument2 pagesObgyn Osce - Breast ExaminationErika Leah ManaloNo ratings yet
- Nursing Abdominal AssessmentDocument5 pagesNursing Abdominal AssessmentPatricia G ChiuNo ratings yet
- Pelvic ExaminationDocument24 pagesPelvic ExaminationVictor SantawiNo ratings yet
- Skills Demo Guide For ClerksDocument11 pagesSkills Demo Guide For ClerksMariana B.No ratings yet
- Pelvic Examination: W - Newton LongDocument3 pagesPelvic Examination: W - Newton LongyuexinchongNo ratings yet
- Per Vaginal ExaminationDocument25 pagesPer Vaginal Examinationazulqaidah95No ratings yet
- 2021.2 - GYNE Written-AnswersDocument113 pages2021.2 - GYNE Written-AnswersLucas Victor AlmeidaNo ratings yet
- National College of Nursing: Procedure ONDocument6 pagesNational College of Nursing: Procedure ONSumit Yadav100% (1)
- Pulmonary DisorderDocument10 pagesPulmonary DisorderIke RilleraNo ratings yet
- Abnormal Labor, Dystocia IIDocument9 pagesAbnormal Labor, Dystocia IIIke RilleraNo ratings yet
- JaundiceDocument25 pagesJaundiceIke RilleraNo ratings yet
- Systemic Lupus ErythematosusDocument89 pagesSystemic Lupus ErythematosusIke RilleraNo ratings yet
- Phylum Aschelminthes - FormattedDocument30 pagesPhylum Aschelminthes - FormattedkingNo ratings yet
- ArrhythmiasDocument55 pagesArrhythmiasAzmi Ikhsan AzharyNo ratings yet
- Pediatrics Report Group 2 Feeding and NutritionDocument23 pagesPediatrics Report Group 2 Feeding and NutritionEd Daniel DavisNo ratings yet
- Management of Bleeding Disorders in Children - MannoDocument7 pagesManagement of Bleeding Disorders in Children - MannoRhiannon Bam OoiNo ratings yet
- Field Guide To Antibiotic StewardshipDocument30 pagesField Guide To Antibiotic StewardshipHosam GomaaNo ratings yet
- Avian EndosDocument15 pagesAvian EndosJosé Moreira Lima NetoNo ratings yet
- DocxDocument53 pagesDocxkuro hanabusaNo ratings yet
- Identification of Hemoglobin Varients Through HPLCDocument42 pagesIdentification of Hemoglobin Varients Through HPLCJohnNo ratings yet
- FNA CCX Ovojnice, CSF, KŽ Za Miru 2020 - gs15FDocument194 pagesFNA CCX Ovojnice, CSF, KŽ Za Miru 2020 - gs15FGoran SimicNo ratings yet
- Hand Hygiene Research PaperDocument3 pagesHand Hygiene Research PaperEd SllenNo ratings yet
- JoDD 17-1 26-37 Schroeder Et AlDocument12 pagesJoDD 17-1 26-37 Schroeder Et AlEspíritu Ciudadano100% (1)
- Mental Health Testu3Document5 pagesMental Health Testu3clarheenaNo ratings yet
- Folinic AcidDocument1 pageFolinic AcidMuhammad ArsalanNo ratings yet
- Lumbar Assessment Form FILLABLE Jun 2020Document2 pagesLumbar Assessment Form FILLABLE Jun 2020FejesNo ratings yet
- Test Drill OBDocument8 pagesTest Drill OBViviane Ńíáshéè Basod100% (1)
- Of Client Having A Nephrectomy: Nursing CareDocument1 pageOf Client Having A Nephrectomy: Nursing CareJayshree ParmarNo ratings yet
- Pneumonia: Meningococcal Pneumonia: A ReviewDocument13 pagesPneumonia: Meningococcal Pneumonia: A ReviewRizki Handayani SiregarNo ratings yet
- Graphic Organiser FactorDocument2 pagesGraphic Organiser FactorRogini SindhuNo ratings yet
- Practical Manual 171Document85 pagesPractical Manual 171Souvik Roy Chowdhury100% (1)
- Biodiversity and Ecosystem ServicesDocument30 pagesBiodiversity and Ecosystem ServicesNick NgNo ratings yet
- Icd 11 Introduction ClinicalDocument50 pagesIcd 11 Introduction ClinicalMuhammad Farooq Ul HassanNo ratings yet
- Vaginal Fungal InfectionsDocument15 pagesVaginal Fungal InfectionsBalsc Bals BalscNo ratings yet
- Toxicology Case Studies Carbon MonoxideDocument5 pagesToxicology Case Studies Carbon MonoxideMark Jayson T. AsinoNo ratings yet
- Biological Classification Class 11Document13 pagesBiological Classification Class 11abhhngouravNo ratings yet
- Diseases: Prevention of Progression in Myopia: A Systematic ReviewDocument25 pagesDiseases: Prevention of Progression in Myopia: A Systematic ReviewFauziah Dwi AprianiNo ratings yet
- Definitions and Reporting Framework For Tuberculosis - 2013 RevisionDocument47 pagesDefinitions and Reporting Framework For Tuberculosis - 2013 RevisionDavien UtoyoNo ratings yet
- Poster Session v3Document11 pagesPoster Session v3Fiola FinandakasihNo ratings yet
- Body World's 1 Running Head: BODY WORLDS EXHIBITDocument5 pagesBody World's 1 Running Head: BODY WORLDS EXHIBITiamruthannNo ratings yet
- Remedi KA6 Slides - Client PPT - Remedi IndiaDocument34 pagesRemedi KA6 Slides - Client PPT - Remedi IndiaSupport InvimedsNo ratings yet
- A Whole-Of-Nation Approach To COVID-19 Taiwan's National Epidemic Prevention TeamDocument16 pagesA Whole-Of-Nation Approach To COVID-19 Taiwan's National Epidemic Prevention Teamgrahma96No ratings yet