Professional Documents
Culture Documents
Amputation
Amputation
Uploaded by
Dhara NP0 ratings0% found this document useful (0 votes)
222 views141 pagesThe document discusses the history and reasons for amputation. It traces the term "amputation" back to Latin and describes its early uses. It then covers the various causes of amputation including trauma, diseases, infections, tumors, and circulatory disorders. The document also outlines the types of amputations, principles of closed vs open amputations, potential complications, and indications for amputation.
Original Description:
Amputation
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses the history and reasons for amputation. It traces the term "amputation" back to Latin and describes its early uses. It then covers the various causes of amputation including trauma, diseases, infections, tumors, and circulatory disorders. The document also outlines the types of amputations, principles of closed vs open amputations, potential complications, and indications for amputation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
222 views141 pagesAmputation
Amputation
Uploaded by
Dhara NPThe document discusses the history and reasons for amputation. It traces the term "amputation" back to Latin and describes its early uses. It then covers the various causes of amputation including trauma, diseases, infections, tumors, and circulatory disorders. The document also outlines the types of amputations, principles of closed vs open amputations, potential complications, and indications for amputation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 141
27-Jul-13 Dr.
PR Khuman,MPT(Ortho & Sport) 2
History
Amputatio – Latin noun from verb Amputare
Amputare– to cut off or cut away, derived from
Amb, about and
Putare, to prune or to lop
The verb “Amputare” was employed to cutting
off the hands of criminals.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 3
History cont…
Early 15th centurThe Cyrurgie of Guy de Chauliac
has a paragraph headed “The rewle in kyttyng of a
dede membre” (The rule in cutting off of a dead member)
Ambroise Pare,1564, Father of French surgery,
Improved ligation of larger vessels during surgery,
gangrene
Lowe, 1612, English, extirpation
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 4
History cont…
Woodall, 1617, Dismembering or Amputation
Woodall, 1639, Employed both amputation &
dismembering, the former as often.
Dionis, 1750, suggested employing the
Greek word Acrotiriasmos – cutting off the
extremities of the body.
17th century British authors Cooke &
Wiseman employed “Amputation”
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 5
Definition
Amputation is the removal of limb, part or
total from the body.
Disarticulation is removing the limb through
a joint.
Generally the amputation of Lower Limb are
more common than those of upper limb.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 6
Incidence
Age –
Common in 50 – 70 year
Gender –
Male – 75%
Female – 25%
Limbs –
Lower limbs 85%
Upper limbs – 15%
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 7
Indications of Amputation
Trauma – RTA, Gun shot
Malignant tumors
Nerve injuries & infection
Extreme heat & cold – burn, gangrene
Peripheral vascular insufficiency
Congenital absence of limbs or malformation
Severe infection
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 8
Causes of Amputation
Natural causes
Accidental causes
Ritual, Punitive & Legal Amputations
Cold steel & Gunshot causes
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 9
Natural causes of limb loss
Congenital absence
Arterial disease
Frostbite
Ergot and other toxins
Wound infections
Diabetes mellitus
Dietary deficiencies
Tumors
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 10
Accidents causes
Falls when running or from heights
Crushing by trees
Savaging by crocodiles and sharks
Effects of earthquakes, tsunamis and
Violent storms
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 11
Ritual, Punitive & Legal Amputations
Curing local pain
In removing deformity
Infection or gangrene
In saving lives
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 12
Cold steel & Gunshot causes
Iron & steel weapons evolved fingers & hands
Destructive gunshot wounding, associated with
mortal sepsis
Boiling oil
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 13
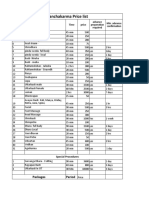
Relative % of causes of LL amputation
Developed world causes (%) Developing world causes (%)
PVD (approx. 25-50%
85-90 Trauma 55-95
diabetes mellitus)
Trauma 9 Disease 10-35
Tumour 4 Tumour 5
Congenital deficiency 3 Congenital deficiency 4
Infection 1 Infection 11-35
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 14
Relative % of causes of UL amputation
Developed world causes (%) Developing world causes (%)
Trauma 29 Trauma 86
Disease 30 Disease 6
Congenital deficiency 15 Congenital deficiency 6
Tumour 26 Tumour 1
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 15
Types of amputation
Closed Amputation
Open Amputation (Guillotine Operation)
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 16
Closed Amputation
It is done as an elective procedure.
After amputations, the soft tissues are
closed primarily over the bony stump.
E.g., above knee, below knee etc.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 17
Open Amputation (Guillotine Operation)
It is done as an emergency procedure.
E.g. life threatening infections
After amputations, the wound is left
open & not closed.
2 types depending upon the skin flaps:
Open amputation with inverted skin flap
Circular open amputation
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 18
Principles of Close Amputation
Tourniquets: desirable except in ischemic
limbs.
Level of amputation: it is very important to
fit the prosthesis.
Skin flaps: good skin coverage is important.
Skin should be mobile & sensitive.
Muscle: is divided at least 5cm distal to the
level of intended bone section & sutured.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 19
Principles of Close Amputation cont…
Methods of Muscle Suture
Myodesis – muscle is suture to bone
Myoplasty – muscle is sutured to opposite
muscle group under appropriate tension.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 20
Principles of Close Amputation cont…
Nerves: cut proximally & allowed to retract.
Large nerves are ligated before division.
Blood vessels: doubly ligated & cut. Then
the tourniquet is released & hemostasis is
completed.
Bone: section above level of muscle section.
Drains: removed after 48 – 72 hours.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 21
Principles of Close Amputation cont…
Compression dressing: Either elastic or a rigid
plaster dressing fitting immediately.
Absolute bed rest with limb elevation: This is
acceptable for the conventional prosthesis with
adequate vascularity.
Limb fitted: Conventional prosthesis is fitted a
minimum of 8 – 12 weeks after surgery. Rigid
dressing with temporary pylon prosthesis may
be elected as an alternative.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 22
Principle of open amputation
Indication:
Severe infection
Severe crush injuries
Types:
Open amputation with inverted skin flaps: it is a
common choice.
Circular open amputation: wound is kept open &
closed 2* by suture, skin graft or re-amputation.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 23
Principle of open amputation cont…
Rx following amputation:
Rigid dressing concept (Pylon): POP
cast is applied to the stump over
the dressing after surgery.
Soft dressing concept: The stump
is dressed with the sterile
dressing & elastocrepe bandage
applied over it.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 24
Complication of amputation
Haematomas Phantom sensation
Infections Hyperesthesia of
Necrosis stump
Contractures Stump edema
Neuromas Bone overgrowth
Stump pain Causalgia
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 25
Amputation - Complications
Phantom Limbs –
Some amputees experience the phenomenon of
Phantom Limbs; they feel body parts that are no
longer there.
Limbs can itch, ache, & feel as if they are moving.
Scientists believe it has to do with neural map
that sends information to the brain about limbs
regardless of their existence.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 26
Amputation – Complications cont…
In many cases, the
phantom limb aids in
adaptation to a
prosthesis, as it permits
the person to experience
proprioception of the
prosthetic limb.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 27
Amputation – Complications cont…
Painful adhesive scar formation
An adherent painful scar over the surgical
incision poses a problem in process of rehab.
It may obstacle in fitting prosthesis.
Early mobilization of the painful scar is
recommended with other therapeutic
modalities.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 28
Amputation – Complications cont…
New bone formation at the amputation sites
It has been reported that new bone formation 5
weeks after electrical burn.
The stump should be closely watch for any sing
& symptoms like – tenderness, warmth & swelling
(Helm & Walker, 1987)
Such symptoms delayed fitting final prosthesis.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 29
Amputation – Complications cont…
Flexion Deformity
Deformity complicates
the process of
prosthetic fitting &
ambulation.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 30
Amputation – Complications cont…
Hyperesthesia of the stump:
This is another annoying symptom that is
difficult to control.
Re-amputation results only in reproducing
the symptom at a higher level.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 31
Reasons for amputation
Circulatory disorders
Diabetic foot infection or gangrene (the
most common reason for non-traumatic
amputation)
Sepsis with peripheral necrosis
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 32
Reasons for amputation cont…
Neoplasm
Cancerous bone or soft tissue tumors
e.g. osteosarcoma, osteochondroma,
fibrosarcoma, epithelioid sarcoma, ewing's
sarcoma, synovial sarcoma, sacrococcygeal
teratoma
Melanoma
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 33
Reasons for amputation cont…
Trauma
Severe limb injuries in which the limb cannot be
spared or attempts to spare the limb have
failed
Traumatic amputation (Amputation occurs
usually at scene of accident, where the limb is
partially or wholly severed).
Amputation in utero (Amniotic band)
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 34
Reasons for amputation cont…
Infection
Bone infection (osteomyelitis)
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 35
Reasons for amputation cont…
As a punishment in Islam
According to Islamic Sharia Law, the
punishment for stealing is the amputation of
the hand & after repeated offense, the foot
(Quran 5:38)
This controversial practice is still in
practice today in countries like Iran, Saudi
Arabia & Northern Nigeria.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 36
Reasons for amputation cont…
Other
Sometimes professional athletes may choose to
have digit amputated to relieve chronic pain &
impaired performance.
Australian footballer Daniel Chick elected to
have his left ring finger amputated as chronic
pain & injury was limiting his performance.
Rugby player Jone Tawake also had a finger
removed.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 37
Amputation Level Nomenclature
Old Terminology Current Terminology
Partial hand Partial hand
Wrist disarticulation Wrist disarticulation
Below elbow Transradial
Elbow disarticulation Elbow disarticulation
Above elbow Transhumeral
Shoulder disarticulation Shoulder disarticulation
Forequarter Forequarter
Partial foot Partial foot
Syme’s Ankle disarticulation
Below knee Transtibial
Knee disarticulation Knee disarticulation
Above knee Transfemoral
Hip disarticulation Hip disarticualation
Hemipelvectomy Transpelvic
Levels of Amputation
Partial toe Excision of any part of one or more toes
Toe disarticulation Disarticulation at the MTP joint
Partial foot/ ray resection Resection of 3rd-5th metatarsal & digit
Transmetatarsal Amputation through the midsection of all metatarsals
Syme’s Ankle disarticulation with attachment of heel pad to distal of tibia
Long transtibial (Below knee) More than 50% tibial length
Short transtibial (Below Knee) Between 20% and 50% of tibial length
Knee disarticulation Through knee joint
Long transfemoral ( Above knee) More than 60% femoral length
Transfemoral (above knee) Between 35% and 60% femoral length
Short transfemoral (Above Knee) Less than 35% femoral length
Hip disarticulation Amputation through hip joint, pelvis intact
Hemipelvectomy Resection of lower half of the pelvis
Hemicorporectomy/ Translumbar Amputation both lower limb & pelvis below L4-L5 level
Level of Amputation (%)
Developing Developing
Level world world
Lower limb –
Trans-tibial (including foot) 29-62 49-71
Trans-femoral (including knee disarticulation) 33-49 26-40
Upper limb –
Trans-radial (including wrist disarticulation) 32-66 21-33
Trans-humeral (including elbow disarticulation) 14-26 25-36
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 40
Principle consideration to amputate
Preservation of life
Improvement of general health
Restoration of function
Reduction of pain
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 41
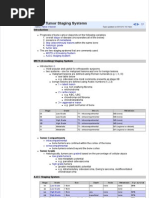
Clinical Team Members & Function (O'Sullivan, 1994)
Clinic chief; coordinates team decision making; supervises
Physician
client's general medical condition; prescribes appliances.
Evaluates & treats clients through pre & prosthetic phases;
Physical
makes recommendations for prosthetic components & whether
therapist
or not to fit client. May be clinic coordinator
Fabricates and modifies prosthesis; recommends prosthetic
Prosthetist
components; shares data on new prosthetic developments
Occupational Assesses & treats individuals with UL amputations; makes
therapist recommendations for components.
Financial counselor & coordinator; provides liaison with third-
Social worker party payers & community agencies; helps family cope with
social and financial problems.
Dietitian Consultant for diabetes or those needing diet guidance.
Vocational Assesses clients employment potential; coordinates and may
counselor fund education. training, and placemen
Rehabilitation of LL Amputation
Pre operative period
Post operative period
Pre-prosthetic stage
Prosthetic stage
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 43
Pre - Operative period
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 44
Pre Operative period
Assessment
Physical
Social
Psychological
Training
Re-assurance
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 45
Pre Operative Assessment
Assessment of –
The affected limb
The unaffected limb &
The patient as a whole is conducted thoroughly.
Assessment of physical, social &
psychological status of the patient should
be made.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 46
Physical Assessment
Muscle strength of UL, trunk & LL apart from
the affected limb before level of amputation.
Joint mobility, particularly proximal to the
amputation level.
Respiratory function
Balance reaction in sitting & standing
Functional ability
Vision & hearing status
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 47
Social assessment includes
Family & friends supports
Living accommodation –
Stairs, ramps, rails, width of door, wheelchair
accessibility
Proximity of shops
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 48
Psychological Assessment
Patients psychological approach to amputation.
Motivation to walk.
Other psychological problems.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 49
Pre Operative Training
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 50
Basic aims
To prevent post operative complication
To reduce the cost of rehabilitation
To reduce the period of rehabilitation
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 51
Training program includes
To prevention of thrombosis:
Maintaining circulation through movt of the
other good limb.
To prevent the chest complication:
Deep breathing, coughing & postural drainage
To relieve pressure:
Pressure mobility of all the joints
More emphasis is given to susceptible joints.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 52
Training program cont…
To improve mobility:
Mobility ex for trunk, pelvic or shoulder girdle
Mobility ex to compensate for the deficiencies
& restriction due to prosthesis.
Teach the technique to be adapted for mobility
& limb positioning in bed.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 53
Training program cont…
To educate the patient:
Educate the techniques of transfers, monitoring
wheelchair, single limb standing & balancing.
Explain important aspect of balance, equilibrium,
standing & walking techniques.
Educate to detect the possible complications
like – soft tissue tightness, pressure point,
expected degree of pain & phantom pain.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 54
Reassurance
Psychological reassurance play an important
roll in recovery
Reassurance with all possible encouragement
Practical demonstration by who has
undergone similar surgery.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 55
Post Operative Period
(pre prosthetic stage)
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 56
Aims of Rx
To prevent post operative complication
To prevent deformities
To control stump edema
To maintain strength of whole body & increase strength of
muscle controlling the stump
To maintain general mobility
To improve balance & transfer
To re-educate walking
To restore functional independence
To treat phantom pain
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 57
Prevention of post operative complication
Breathing ex to prevent respiratory
complications.
Brisk ankle & foot ex for unaffected leg to
prevent circulatory complications.
This exs are given form 1st day onward until
patient ambulate.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 58
Prevention of deformities
Positioning in bed:
Stump should be parallel to the unaffected leg
without resting on pillow.
Patient should lie as flat as possible & progress
to prone lying when drains are out.
Pt with cardiac & respiratory problems may
discomfort in prone lying, brought to supine.
Prolong sitting on soft mattress can predispose
to development of hip flexion deformity.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 59
Prevention of deformities cont…
Exercise to counteract the deformity:
Strong isometric quadriceps ex – BKA
Hip extensor & add isometric ex – high AKA
Hip extensor & abd isometric ex – low AKA
Progression is made to free active & resisted stump
ex.
Stump board – in BKA – stump should be rest on
board when sitting in wheelchair.
Prolong sitting with knee flex should be avoided.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 60
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 61
To control the stump edema
Control environment treatment (CET):
Here, the dressing free stump place over a clear
& sealed plastic sleeve which is attached to a
pressure cycle machine blowing sterile warmed
air over the wound.
The temp, pressure & humidity are set with
ideal environment for healing of stump.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 62
To control the stump edema cont…
Pressure environment treatment (PET):
This is simpler version of CET
Here, the air is not sterilized, no temp control &
limited pressure control.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 63
To control the stump edema cont…
Flowtron:
The stump is placed in an invaginated plastic bag.
The air pressure varies rhythmically,
compressing & relaxing the stump to reduce
edema.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 64
To control the stump edema cont…
Stump compression socks or bandaging:
Elastic stump compression socks ( Juzo
Socks) methods reduce edema &
conditioning the stump.
Bandaging is controversial method of
controlling stump edema particularly in
vascular patient.
Pressure should be firm, even & decreasing
pressure proximally.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 65
To control the stump edema cont…
Stump compression socks or bandaging:
Diagonal oblique & spiral turn should be used
rather than circular turns to prevent
tourniquet effect.
Bandage size:
Upper limb – 4”
Lower limb – 6”/8”
Above knee – 6”
Below knee – 4”
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 66
Stump compression socks or bandaging:
Above knee (AK) bandaging:
It should extend up to groin to prevent follicle
infection due to friction with socket of
prosthesis.
It should bandage with hip in extension &
adduction.
Below knee (BK) bandaging:
Stump should bandage with knee in slight flexion.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 67
Above knee
Below knee
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 68
Maintain body strength & strengthen
muscle controlling stump
Strengthening muscles are:
Shoulder – extensors, Adductors,
Elbow – extensors by working against weight or
springs attached to bed.
Examples are:
Grasp stretch lying (shoulder extension & adduction)
Grasp lying (elbow flexion)
Sitting push up
Strengthening of crutch muscle is very imp
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 69
Exercise for unaffected side
Lying:
Static quadriceps
Static gluteal
Straight leg raising (SLR)
Alternate hip & knee bending & stretching
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 70
Stump exercise
Begins when the drains are out
Gradually progressed from static to free
active then resisted ex (PRE)
In BKA progress to strengthening against
resistance.
In AKA prone lying leg lifting against
resistance
E.g. manual resistance, weighted pulley,
spring, theratube, theraband etc.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 71
Maintain good mobility
Exercise which moves the shoulder in all
direction will maintain shoulder mobility
Trunk movts in lying & sitting will improve
trunk mobility
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 72
Improve balance & transfers
Balance training
In sitting position by encouraging balance
reaction, tapping, perturbation & trunk
stabilization
Training of transfer techniques
Wheelchair to bed
Bed to wheelchair
Wheelchair to toilet etc
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 73
Walking Re-education
Partial weight bearing in parallel bar
using pneumatic post amputation
mobility aid (PPAM) 5 – 10 day post
operatively
Patient should wear normal dress & a
good walking shoe on unaffected side.
Initially preferred training in stable
surface & progress to unstable
surface. E.g. Walking in mud
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 74
Pneumatic Post Amputation Mobility Aid (Ppam)
It is a partial weight bearing early walking
aid that must only used under clinical
supervision in the therapy facility, not for
ward or home use.
It can use from 5 -7 day postoperatively
while the suture are still in the wound.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 75
Ppam Aid Advantages
Great psychological boost gained by walking soon
after amputation.
Reduction of oedema by pressure in bag.
Postural reaction are re-educated by encouraging
partial weight bearing.
Preparation of the residual limb for hard socket of
a prosthesis.
This may help in reducing phantom sensation.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 76
Ppam Aid Disadvantages
If a fixed flexion contracture is present, the
residual limb is more liable to break down.
If the amputee is very heavy or heavy footed gait,
excessive pistoning may occur & there will be
insufficient support.
Amputees used a stiff knee gait pattern, which is
unnatural for those with the trans-tibial level.
The inflation pressure may greater than the
arterial pressure in the residual limb.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 77
Walking without a prosthesis
Using firm compression socks or bandage the
gait training can be done in parallel bar
Progress to – a frame or crutch depending on
stability.
Crutch user found less adaptation time to use a
prosthesis
Normal alignment of pelvis & reciprocal movt of
stump should maintain.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 78
Principle of Bandaging of Stump
Pressure of bandage should be
Moderately firm
Evenly distributed
Decreasing proximally
Extra pressure over the corners – conical shape
Pattern of bandage:
Diagonal, oblique or spiral
Not circular
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 79
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 80
Main Aim at this Stage:
To understand the components of prosthesis
To independently fitting & removing of
prosthesis & checking its fit
To care of prosthesis
To independent mobility – with or without walker
To enable functional task with prosthesis
To enable occupational & leisure activities
To enable to cope with falls
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 81
Type of Prosthesis
Temporary prosthesis
It takes approx 2 week manufacture
Quick & easy to manufacture
Cheaper, lighter & relatively simple to apply
Allow time for stump shrinkage to take place
Final/ definitive prosthesis
It takes 2 – 3 month to manufacture
Measurement taken after shrinkage completed
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 82
Basic features of a Prosthesis
Sockets –
Provides weight bearing & receptive area of
stump
Interface between the patient and the
prosthesis
Suspension – holds the prosthesis to stump
Joints – amputated joints are replace with
artificial mechanical joints
Base – provides contact with the floor
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 83
Material used for prosthesis
Metal –
Steel & other alloys – for hip & knee mechanism
Duraluminium – for the socket & outer shell
Leather –
Soft leather for straps
Hardened leather for thigh corsets
Plastics –
Thermoplastic materials like polypropylene – for sockets
Plastic foam – to support distal tissue of stump
Wood –
Preferred as a socket material & prosthetic feet in topical climate
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 84
Factors To Be Consider Before
Prescribing Prosthesis
Age
General physique of the patient
Mental conditions
Length of the stump
Status of stump circulation
Level of amputation
Strength, ROM & mobility related body segment
Requirement of job & daily living
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 85
Prosthesis for Lower Limb Amputation
Depending on the level of amputation
Transmetatarsal
Below knee
Patella Tendon Bearing (PTB)
Above knee – Below knee (AKBK)
Mid thigh
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 86
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 87
Re-education with Prosthesis
After satisfactory fitting of prosthesis the
process of training & re-education begins.
It include the following:
Correct methods of applying & removing of
prosthesis
Early detection of any complication due to
prosthesis
Functions of various component of prosthesis
Limitation of activities with prosthetic limb
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 88
Restore functional independence
Taught to move up & down, side to side on
the bed by pressing on the sole of stump
Sitting up form lying by pushing down with
the arm – begin when the drip are removed
Good trunk rotation will make all reaching
function easier
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 89
Restore functional independence cont…
Functional training should start as soon as
patient is able
The exercise program should consist of
Resisted pulley work
Mat exercise
Slow reversal or repeated contraction
The patient must be encourage to be as
independent as possible
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 90
Treatment of Phantom Pain
Pharmacological Rx
Injection with steroid or local anesthetic has
reduced the pain temporarily
Intrathecal or epidural anesthetic with opioids
used successfully
Non invasive Rx
Such as – US, Icing, Icing, TENS or massage
have been used
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 91
Treatment of Phantom Pain cont…
Other methods –
Mild non narcotic analgesics,
Biofeedback,
Psychotherapy,
Nerve block & dorsal rhyzotomies have been used
with inconsistent result.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 92
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 93
COMMON ABNORMALITIES
INWALKING WITH A PROSTHESIS
The common problems encountered in
walking with a prosthesis can also be
divided into
Stance phase problem or
Swing phase problem.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 94
Stance Phase Problems with a BK
Prosthesis
Problems commonly encountered in the
stance phase of walking with a
prosthesis include
“Buckling” of the knee,
“Snapping back” of the knee,
“Foot slapping,” and
“Vaulting.”
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 95
Reasons for knee buckling
Weak quadriceps:
Can’t straighten the knee when heel strikes the
ground. This can be corrected by a muscle
strengthening program.
Pain from an ill-fitting socket:
Changing the socket might solve this problem.
A poorly-aligned prosthetic foot, or one with a
heel that is too hard: These also can be
corrected.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 96
Causes of snapping back
Weak thigh muscles or poor alignment of the
socket and the foot.
Fear of knee buckling is offset by keeping the
knee as straight as possible when heel strikes in
early stance phase.
One way of keeping it straight is to “snap” the
knee back.
Over time, this can cause pain & deformity in
knee.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 97
The knee may snap backwards because of a soft
heel or a foot that points downward more than it
should.
A good muscle strengthening program for the
thigh muscles is important to overcome this
problem.
Additionally, your prosthetist can check the
socket to ensure that there is a good fit and
alignment.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 98
Causes of slapping
A prosthetic foot that slaps the floor while
walking can be the result of a problem with
socket alignment or the foot.
E.g., there may be a slapping sound if the foot is
pointing up too much when the heel strikes the ground.
This can also potentially cause the knee to buckle.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 99
Vaulting
It is the term used when you
lift your body up onto the ball
of sound foot in order to
swing your prosthetic leg
forward.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 100
Reasons for vaulting
The prosthesis is too long, and as a result you
feel that you are going to trip over it as you walk.
It is compensate by raising entire body off the
ground with sound foot.
Other reasons include inadequate suspension of
the prosthesis or an ill-fitting socket.
These problems can be addressed by
correcting the length of the prosthesis.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 101
Swing Phase Problems with a BK
Prosthesis
The problems encountered during the swing
phase are related to inability to advance the leg.
This may be the result of –
The prosthesis being too long,
Being inadequately suspended, or
Having a contracture at knee, which limits the ability
to flex & extend the knee effectively.
Pain from a poorly fitting prosthesis or fear of
taking steps may affect swing phase.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 102
Swing Phase Problems with a BK
Prosthesis Cont…
These are all correctible.
The length of the prosthesis can be adjusted;
The suspension can be improved;
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 103
Gait Problems in AK Amputees
The most common problem encountered by the
AK amputee is flexion & extension of knee during
stance phase.
May feel that knee will buckle & cause to fall.
As a result, fearful of walking and take small,
cautious steps to compensate.
This problem can be corrected by changing the
alignment of the knee to make it more stable
during stance phase.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 104
Gait Problems in AK Amputee Cont…
Knee-buckling during stance phase that are not
related to the use of a prosthesis;
E.g., weak gluteal muscles on the prosthetic limb. This
can be remedied by strengthening program.
Prosthesis stick out away from the body during
stance phase as a result of a muscle imbalance
between adductor & abductor.
Strengthening of adductor muscle groups is
important.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 105
Gait Problems in AK Amputee Cont…
Too much bending of trunk during stance phase.
This can result from an ill-fitting socket, a
short prosthesis, or weak hip muscles.
Vaulting can be seen with an AK prosthesis
(same as BK prosthesis).
It can be caused by a prosthesis that is too
long or inadequately suspended.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 106
Gait Problems in AK Amputee Cont…
Circumduction is the term that is used to
describe a wide arc-like movement of the
prosthetic limb during swing phase.
Typically, it results from a prosthesis that is
too long.
The prosthesis may appear to be too long if the
suspension is inadequate or the prosthetic knee
does not bend.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 107
The Importance of the Hip Muscles
Weakness in key muscle groups around the hip
and contractures or tightness of the hip joint
can have a profound impact on ability to walk
with a prosthesis.
It can make walking awkward and force to use
more energy than it should.
It may become over cautious every time they
take a step.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 108
4 key muscle groups in the hip
Hip flexors are responsible for
advancing the leg forward during swing
phase.
It may find it difficult to advance the
limb during swing phase if they are weak.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 109
Hip extensors help pull the leg backward,
stabilizing it during the stance phase.
If they are weak, there may be a
buckling or unsteady sensation at heel
strike the ground during stance phase.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 110
Hip abductors pull the leg away from the
body.
They will walk with an excessive bending
of trunk if abductors are weak.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 111
Hip adductors pull the prosthetic leg
toward the body.
They will walk with the prosthetic limb
extended away from body if they are
weak.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 112
Criteria for gait training
Gait training should be perform in
front of full length mirror to observe
& correct any fault
Increase the walking time each day
Inspect the stump at the end of day
Young, fit amputees will required
1week training
Elderly, will required 2week or more
training.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 113
Training In Parallel Bar
Standing balance with equal weight on both legs.
Correct method of weight transfer on individual leg
Weight transfer on both legs alternatively.
PNF techniques of resistive gait, rhythmic
stabilization & approximation are emphasized.
Normal coordinated stepping with both hand
support.
Progress to single hand support.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 114
Training In Parallel Bar cont…
Raising to standing form sitting & back.
Side walk & turning
Reasonable gait progression is made by
walking with one stick in appropriate hand
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 115
Home visit
A home visit should be made prior to
discharge from the hospital
An assessment for floor coverings, stairs,
steps, door widths necessary for ramp,
additional rails, access to bathroom,
facilities in kitchen for cooking & washing
Proximity of shops
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 116
Final Rehabilitation
It involves the patients returning to a
normal active everyday life
Participation in sports such as squash, tennis,
golf etc.
Functional independent in case of elderly
Falling without injuries
Set a follow up
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 117
Safety falling techniques
Should be start on mat with precaution
Progression should be made by transferring
to various falling surface
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 118
HOW TO PREVENT FALLS
There is a risk of fall after limb amputation
E.g., It may happen in the middle of the night
when you get up to go to the bathroom because
you do not remember that you are missing a leg.
Although most of the time nothing serious will
happen, apart from you may break a bone, hit
your head, or cut yourself.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 119
HOW TO PREVENT FALLS Cont…
First, it is best to have a safe home that
minimizes risk of falling.
Second, must have a prosthesis that fits well
& is not at risk of breaking or malfunctioning.
Third, should know how to get up from the
floor if fall, and how to call for help if
cannot get up.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 120
Suggestions for modifying home to
prevent falls
General – Specific Rooms
Remove loose rugs Bathroom
Chairs should have arms Grab bars in the tub
Free of clutter A tub bench or seat
Adequate lighting A handheld showerhead
Adequate lighting
Non-skid mats
An elevated toilet seat
Bedroom
Flashlight in nightstand
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 121
WEIGHT ISSUES IN WALKING
WITH A PROSTHESIS
Weight gain can cause residual limb to
increase in size, making more difficult to
put on the prosthesis.
If the prosthesis is not on correctly –
It will make difficult to walk in smooth, energy-
efficient, and attractive manner.
It can also cause skin irritations and infections.
It can even cause fall also.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 122
WEIGHT ISSUES IN WALKING
WITH A PROSTHESIS Cont…
It is important to discuss any weight gain or
loss with prosthetist and physician.
Changes in prosthesis may be necessary if
unable to lose weight.
These changes may include the fabrication
of a new socket.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 123
Follow-Up Visits to Rehab Clinic
Tell your doctor if you are experiencing any
of the following:
Areas of redness, cuts or skin irritations on the
residual limb
Areas of pressure over bones on residual limb
Falls or near falls
Phantom pain
Low back pain
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 124
Follow-Up Visits to Rehab Clinic cont…
Sensations that the residual limb is moving
up and down within the socket (pistoning).
This is similar to walking with a pair of shoes
that are too big.
An ill-fitting prosthesis
Pain in the residual limb when putting on the
prosthesis or taking it off.
Pain in the opposite, remaining lower limb
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 125
Problems with respect to dressing, bathing,
transferring from bed to chair, or getting in and
out of a bathtub
Any problems with the skin on the opposite foot,
such as redness, cuts, and bruises. These are
typically on the ball of the foot, and may be
difficult to see.
Any recent weight loss or weight gain
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 126
Roll of rehab team in follow-up visits
Examine skin of residual limb for any
evidence of –
Blisters, infections, or abnormal areas of
pressures on bones
Also examine skin on opposite, remaining limb.
Check the ROM of the residual limb for the
presence of a contracture.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 127
Examine the strength of arms & legs, and
ability to get up from a seated position.
Examine gait with prosthesis for a short
distance to see if there are any alignment
or fit problems with the prosthesis.
After this short period of ambulation, skin
should be checked again for any areas of
abnormal pressure on the bones.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 128
References
Susan Sullivan, Physical Rehabilitation, 5th edition, 2007
Ann Thomson, Tidy Physiotherapy, 12th edition, 1995
Stuart Porter, Tidy Physiotherapy, 13th edition, 2003
Jayant Joshi, Essential of Orthopaedics & Applied
Physiotherapy, 2002
Bella J. May, Amputations And Prosthetics: A Case Study
Approach, 2nd edition, 2002
John Kirkup, A History of Limb Amputation,2007
Adrian Cristian, M.D., Lower Limb Amputation: A Guide to
Living a Quality Life, 2006
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 129
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 130
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 131
Gangrene
is necrosis & subsequent decay of body tissues
caused by infection or thrombosis or lack of blood
flow.
It is usually the result of critically insufficient
blood supply caused by injury and subsequent
contamination with bacteria.
This condition is most common in the extremities.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 132
The best of all Rx is revascularization (restoration)
of the affected organ, which can reverse some of
the effects of necrosis & allow healing.
Depending on the extent of tissue loss & location,
Rx other than revascularization runs the gamut to
auto-amputate (fall off), debridement and local
care, to amputation, the removal of infected
necrotic tissues.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 133
Gangrene - Types
Wet Gangrene – Gangrene caused by a serious
bacterial infection.
Dry Gangrene – Gangrene caused by lack of
circulation in an injured or diseased area.
Example
Diabetic foot in long-standing complicated diabetes. It is
caused by a combination of arterial ischemia, injury &
poor healing in diabetics. It often combines poor healing
with a superimposed infection.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 134
Gangrene - History
In the years before antibiotics, fly maggots
were used to Rx chronic wounds or ulcers to
prevent or stop necrotic spread.
Some species of maggots consume only dead
flesh, leaving nearby living tissue
unaffected.
Largely died out after the introduction of
antibiotics & enzyme Rx for wounds.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 135
Gangrene – History cont…
In recent years, maggot therapy has
regained some credibility and employed to
great effect in cases of chronic tissue
necrosis.
The most common surgical Rx for
irreversible gangrene is immediate
Amputation, as the infection grows 2-3cm/hr.
Gas gangrene
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 136
Gangrene - Pathophysiology
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 137
Gangrene - Wet gangrene
Wet gangrene is more familiar of two types,
at least in media portrayals.
An injury, such as a gunshot or laceration,
leads to a bacterial infection, which
produces pus.
If the pus does not drain well, the blood
supply to the area is blocked, and the
oxygen.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 138
Gangrene - Wet gangrene cont…
When O2 supply cut off, the tissue dies.
Rx of the underlying infection is necessary,
removal of the dead tissue.
Without Rx, the infection can spread
further & destroy large amount of tissue.
Eventually, sepsis & death can result.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 139
Gangrene - Dry gangrene
If the blood flow is interrupted for a
reason other than severe bacterial
infection, the result is a dry gangrene.
Persons with impaired peripheral blood
flow, such as diabetics, are at greater
risk for dry gangrene.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 140
Gangrene - Dry gangrene cont…
The early signs of dry gangrene are a
dull ache and sensation of coldness in the
area, along with pallor of the flesh. If
caught early, the process can sometimes
be reversed by vascular surgery.
However, if necrosis sets in, the
affected tissue must be removed just as
with wet gangrene.
27-Jul-13 Dr.PR Khuman,MPT(Ortho & Sport) 141
You might also like
- Recombiplastin 2G - 0020002950 (8 ML) : Al For Identification and Resolution of Out-Of-Control SituationsDocument5 pagesRecombiplastin 2G - 0020002950 (8 ML) : Al For Identification and Resolution of Out-Of-Control SituationsSteffyPérezPioNo ratings yet
- Cerebral Palsy Revalida FormatDocument10 pagesCerebral Palsy Revalida FormatChelsea CalanoNo ratings yet
- NPB 168 Practice Exam 1Document4 pagesNPB 168 Practice Exam 1Kim WongNo ratings yet
- (Chapter 73) Carpal Tunnel, Ulnar Tunnel, and Stenosing TenosynovitisDocument25 pages(Chapter 73) Carpal Tunnel, Ulnar Tunnel, and Stenosing TenosynovitisBlazxy EyreNo ratings yet
- PEOPLE Versus Teehankee Jr.Document37 pagesPEOPLE Versus Teehankee Jr.Ad Altiora TendoNo ratings yet
- Basic OrthopaedicsDocument38 pagesBasic OrthopaedicsKannamma DorairajNo ratings yet
- Molnar CPDocument4 pagesMolnar CPCatherine AgustinNo ratings yet
- AAOS2002 ShoulderDocument70 pagesAAOS2002 ShoulderHéctor Pando SánchezNo ratings yet
- Help Rockwoodfractureschildren PDFDocument1,242 pagesHelp Rockwoodfractureschildren PDFIulian FrunzăNo ratings yet
- Nerve InjuryDocument19 pagesNerve Injurybhavesh jain100% (2)
- Master Techniques OrthopedicsDocument378 pagesMaster Techniques OrthopedicsFabio Sales VieiraNo ratings yet
- Acetabular Fracture PostgraduateDocument47 pagesAcetabular Fracture Postgraduatekhalidelsir5100% (1)
- Carpal Tunnel SyndromeDocument22 pagesCarpal Tunnel SyndromeNUR ZAMZAM AZIZAHNo ratings yet
- Shoulder DislocationDocument29 pagesShoulder DislocationAndaleeb ZehraNo ratings yet
- Iof Compendium: of OsteoporosisDocument76 pagesIof Compendium: of OsteoporosisMia DangaNo ratings yet
- ArthroplastyDocument64 pagesArthroplastyAmit Kochhar75% (4)
- Open Tibial FracturesDocument36 pagesOpen Tibial FracturesMuhammed ElgasimNo ratings yet
- Orthopaedic SlidesDocument163 pagesOrthopaedic SlidesVivian ChepkemeiNo ratings yet
- Neurofibromatosis Etiology, Commonly Encountered Spinal Deformities and Surgical TreatmentDocument10 pagesNeurofibromatosis Etiology, Commonly Encountered Spinal Deformities and Surgical TreatmentChristoforos KampouridisNo ratings yet
- Club FootDocument19 pagesClub FootJonggi Mathias TambaNo ratings yet
- Antibiotic Classification & Mechanism - Basic Science - OrthobulletsDocument7 pagesAntibiotic Classification & Mechanism - Basic Science - OrthobulletsYuttapol PimpisonNo ratings yet
- Musculoskeletal Disease Associated With Diabetes MellitusDocument290 pagesMusculoskeletal Disease Associated With Diabetes Mellituscharanmann9165No ratings yet
- AAPMR - What Makes The Practice of Physiatry MultidisciplinaryDocument3 pagesAAPMR - What Makes The Practice of Physiatry MultidisciplinaryJared CoganNo ratings yet
- Tissue Repair: Kristine Krafts, M.D. - September 13, 2010Document59 pagesTissue Repair: Kristine Krafts, M.D. - September 13, 2010Antonino CassottaNo ratings yet
- Bone Forming TumorsDocument81 pagesBone Forming TumorsDoc NaumanNo ratings yet
- Patan Academy of Health Sciences School of Medicine Lagankhel, LalitpurDocument12 pagesPatan Academy of Health Sciences School of Medicine Lagankhel, LalitpurSARMITA SHRESTHANo ratings yet
- Concept of Gunshot Wound SpineDocument6 pagesConcept of Gunshot Wound SpineTina MultazamiNo ratings yet
- A Case Report On Potts Spine Spinal TubeDocument3 pagesA Case Report On Potts Spine Spinal TubeyaneemayNo ratings yet
- Tennis ElbowDocument13 pagesTennis ElbowPadma PadalNo ratings yet
- Orthopedic Exam Notes Apu PDFDocument6 pagesOrthopedic Exam Notes Apu PDFabiramirajalaksmiNo ratings yet
- Percutaneous Imaging-Guided Spinal Facet Joint InjectionsDocument6 pagesPercutaneous Imaging-Guided Spinal Facet Joint InjectionsAlvaro Perez HenriquezNo ratings yet
- AmputationDocument51 pagesAmputationStar CruiseNo ratings yet
- WHO Guidelines For OsteoporosisDocument206 pagesWHO Guidelines For Osteoporosisscribdandrealeoni100% (1)
- The Leg: - Orthopedic Anatomy - Clinical Anatomy - Radiologic AnatomyDocument50 pagesThe Leg: - Orthopedic Anatomy - Clinical Anatomy - Radiologic Anatomyspeedy.catNo ratings yet
- David Warwick (Editor), Ashley Blom (Editor), Michael Whitehouse (Editor) - Apley and Solomon - S Concise System of Orthopaedics and Trauma-CRC Press (2022)Document763 pagesDavid Warwick (Editor), Ashley Blom (Editor), Michael Whitehouse (Editor) - Apley and Solomon - S Concise System of Orthopaedics and Trauma-CRC Press (2022)filip100% (1)
- Filariasis: Ruzgal, Celeste Irah Saluta, Maria DivinaDocument10 pagesFilariasis: Ruzgal, Celeste Irah Saluta, Maria DivinaIrahRuzgalNo ratings yet
- Subacrominal Impingement JNR PT EditedDocument38 pagesSubacrominal Impingement JNR PT EditedAndrew Foster100% (1)
- Ankle Examination Orthopaedics McraeDocument6 pagesAnkle Examination Orthopaedics McraeHafizah HoshniNo ratings yet
- Bone Tumour Staging - PathologyDocument2 pagesBone Tumour Staging - Pathologyo7113No ratings yet
- Rhabdomyosarcoma - Pathology - OrthobulletsDocument3 pagesRhabdomyosarcoma - Pathology - OrthobulletsNanda PerdanaNo ratings yet
- Actures of The Midfoot and ForefootDocument37 pagesActures of The Midfoot and ForefootMrHadezz LamerNo ratings yet
- Shoulder PathologyDocument130 pagesShoulder PathologyNiko Pa100% (1)
- Principles of ImmobilizationDocument27 pagesPrinciples of ImmobilizationSivaneasan KandiahNo ratings yet
- Common Spinal Disorders Explained PDFDocument2 pagesCommon Spinal Disorders Explained PDFTamekaNo ratings yet
- A Core Syllabus in AnatomyDocument16 pagesA Core Syllabus in Anatomydod_nur100% (2)
- 2010 Orthopaedic JournalDocument80 pages2010 Orthopaedic JournalPooria1989No ratings yet
- The Talonavicular and Subtalar Joints The Calcaneopedal Unit ConceptDocument11 pagesThe Talonavicular and Subtalar Joints The Calcaneopedal Unit ConceptAnonymous kdBDppigENo ratings yet
- Ortho VIVA TopicsDocument22 pagesOrtho VIVA TopicsSiti RaudahNo ratings yet
- MPFL ReconstructionDocument16 pagesMPFL ReconstructiondrjorgewtorresNo ratings yet
- G04 Compartment SyndromeDocument31 pagesG04 Compartment Syndromesebastian1207No ratings yet
- The Effect of Therapeutic Ultrasound On Metallic Implants - A Study in RatsDocument5 pagesThe Effect of Therapeutic Ultrasound On Metallic Implants - A Study in RatsnatkwqNo ratings yet
- 24 Management of Facial FracturesDocument32 pages24 Management of Facial FracturesxienaistNo ratings yet
- Patellar InstabilityDocument16 pagesPatellar InstabilitydrjorgewtorresNo ratings yet
- Acute Distal Radioulnar Joint InstabilityDocument13 pagesAcute Distal Radioulnar Joint Instabilityyerson fernando tarazona tolozaNo ratings yet
- Workshop 1: Knots: Stage 1Document4 pagesWorkshop 1: Knots: Stage 1Noora jabeenNo ratings yet
- Rehabilitation of The Burn PatientDocument9 pagesRehabilitation of The Burn PatientErtania NirmalaNo ratings yet
- Review - Presby Residency ManualDocument400 pagesReview - Presby Residency ManualSneha SutharNo ratings yet
- Regenerative RehabilitationDocument9 pagesRegenerative RehabilitationAndreeaBubuNo ratings yet
- Current Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderFrom EverandCurrent Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderNo ratings yet
- AmputationsDocument141 pagesAmputationsdeepaseira2205100% (2)
- Shoulderimpingementsyndrome 130727141326 Phpapp02Document46 pagesShoulderimpingementsyndrome 130727141326 Phpapp02renaldi primaNo ratings yet
- Vitamin DDocument29 pagesVitamin DDhara NP100% (1)
- NucleotideDocument56 pagesNucleotideDhara NPNo ratings yet
- Nomophobia InterpretationDocument1 pageNomophobia InterpretationDhara NPNo ratings yet
- Service EvaluationDocument4 pagesService EvaluationDhara NPNo ratings yet
- Neer #Document3 pagesNeer #Dhara NPNo ratings yet
- DAPREDocument3 pagesDAPREDhara NPNo ratings yet
- Lipsey&Cullen - The Effectiveness of Correctional RehabilitationDocument44 pagesLipsey&Cullen - The Effectiveness of Correctional RehabilitationishantimalsinaNo ratings yet
- BTL-5000 Series: User'S ManualDocument65 pagesBTL-5000 Series: User'S ManualAlexaNo ratings yet
- Worrying About Worry: A Generalized Anxiety Disorder Case Study Khola TahirDocument12 pagesWorrying About Worry: A Generalized Anxiety Disorder Case Study Khola TahirMohammed GhozzNo ratings yet
- Cavanagh Biological Activities of Lavender Oil 2002 PDFDocument8 pagesCavanagh Biological Activities of Lavender Oil 2002 PDFIoana BrăteanuNo ratings yet
- Mechanisms of Change in PsychoDocument14 pagesMechanisms of Change in PsychoConstanza Toledo DonosoNo ratings yet
- SIY - My Take On PsychotherapyDocument2 pagesSIY - My Take On PsychotherapyChantelle SiyNo ratings yet
- Sensory DefensivenessDocument4 pagesSensory DefensivenessKarla CarazoNo ratings yet
- Case Study Cerebral PalsyDocument3 pagesCase Study Cerebral PalsyHabib Ullah KhanNo ratings yet
- Orthogeriatrics 2021Document355 pagesOrthogeriatrics 2021BlackthestralNo ratings yet
- BIOS LIFE - Utah Trial by Dr. Peter J.E. VerdegemDocument6 pagesBIOS LIFE - Utah Trial by Dr. Peter J.E. VerdegemHisWellnessNo ratings yet
- Development of Robots For Rehabilitation Therapy T PDFDocument13 pagesDevelopment of Robots For Rehabilitation Therapy T PDFManuel Fernando BallesterosNo ratings yet
- KidsElderly-FullContent Godesana Essential Oils-4112014Document58 pagesKidsElderly-FullContent Godesana Essential Oils-4112014kelleeNo ratings yet
- Notification Janakpuri Super Speciality Hospital Nursing Officer Other PostsDocument27 pagesNotification Janakpuri Super Speciality Hospital Nursing Officer Other PostsMonikaNo ratings yet
- PorphyriaDocument10 pagesPorphyriaDeepankar Srigyan0% (1)
- Dr. Marny Eulberg's BraceDocument2 pagesDr. Marny Eulberg's Braceapi-26005027No ratings yet
- Does Motivation Impact OCD Symptom Severity? An Exploration of Longitudinal EffectsDocument14 pagesDoes Motivation Impact OCD Symptom Severity? An Exploration of Longitudinal EffectsLaura HdaNo ratings yet
- Effect of Music Care On Depression and BehavioralDocument8 pagesEffect of Music Care On Depression and BehavioralSaul MorenoNo ratings yet
- Sitecore - Media Library - Files.3d Imaging - Shared.7701 3dbrochure UsDocument28 pagesSitecore - Media Library - Files.3d Imaging - Shared.7701 3dbrochure UsandiNo ratings yet
- PFT Interpretation AlgorithmDocument4 pagesPFT Interpretation AlgorithmJason Steel50% (2)
- Becadexamin PDFDocument14 pagesBecadexamin PDFakshay bhadauriaNo ratings yet
- Apical Extrusion of Debris and Irrigant Using HandDocument25 pagesApical Extrusion of Debris and Irrigant Using HandManva MonishNo ratings yet
- L Zeig FH4 UtilizationDocument7 pagesL Zeig FH4 Utilizationecenteno150% (2)
- Case Management For Addiction Professionals: Module 1-TrainingDocument27 pagesCase Management For Addiction Professionals: Module 1-TraininglissarlissaaNo ratings yet
- New Panchakarma Price ListDocument3 pagesNew Panchakarma Price ListDrSanjay Chhajed100% (1)
- My Resume Luis SanchezDocument2 pagesMy Resume Luis Sanchezapi-242986404No ratings yet
- Spa in Chembur - Google SearchDocument1 pageSpa in Chembur - Google Searchaniketsingh70211No ratings yet
- Breg, Inc. Store Catalog 1711052394Document5 pagesBreg, Inc. Store Catalog 1711052394Cecilia AguilaNo ratings yet
- CAncer Is Not A Disease-It's A Survival MechanismDocument5 pagesCAncer Is Not A Disease-It's A Survival Mechanismnichitacalin100% (2)