Professional Documents
Culture Documents
Atrial Fibrillation: Key Treatments
Atrial Fibrillation: Key Treatments
Uploaded by
choobi0 ratings0% found this document useful (0 votes)
14 views2 pagesThis document discusses treatments for various arrhythmias including atrial fibrillation, asystole, and ventricular fibrillation. Key treatments include antiarrhythmics, synchronized cardioversion, cardiopulmonary resuscitation (CPR), and advanced cardiac life support (ACLS) protocols. The document also summarizes cardiac tamponade, describing key signs and symptoms such as muffled heart sounds and narrow pulse pressure. Treatments for tamponade include pericardiocentesis or surgical drainage of fluid, with close monitoring for complications.
Original Description:
Arrhythmia
Original Title
Arrhythmia
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses treatments for various arrhythmias including atrial fibrillation, asystole, and ventricular fibrillation. Key treatments include antiarrhythmics, synchronized cardioversion, cardiopulmonary resuscitation (CPR), and advanced cardiac life support (ACLS) protocols. The document also summarizes cardiac tamponade, describing key signs and symptoms such as muffled heart sounds and narrow pulse pressure. Treatments for tamponade include pericardiocentesis or surgical drainage of fluid, with close monitoring for complications.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
14 views2 pagesAtrial Fibrillation: Key Treatments
Atrial Fibrillation: Key Treatments
Uploaded by
choobiThis document discusses treatments for various arrhythmias including atrial fibrillation, asystole, and ventricular fibrillation. Key treatments include antiarrhythmics, synchronized cardioversion, cardiopulmonary resuscitation (CPR), and advanced cardiac life support (ACLS) protocols. The document also summarizes cardiac tamponade, describing key signs and symptoms such as muffled heart sounds and narrow pulse pressure. Treatments for tamponade include pericardiocentesis or surgical drainage of fluid, with close monitoring for complications.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
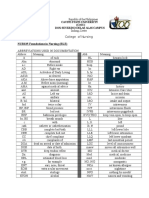
ARRHYTHMIAS (CONTINUED) • Pulsus paradoxus (an abnormal inspiratory drop in
Key treatments systemic
Atrial fibrillation blood pressure greater than 15 mm Hg)
• Antiarrhythmics (if client is stable): amiodarone • Restlessness
(Cordarone), • Upright, leaning forward posture
digoxin (Lanoxin), diltiazem (Cardizem), Key test results
procainamide, verapamil • Chest X-ray shows slightly widened mediastinum
(Calan) and cardiomegaly.
• Synchronized cardioversion (if client is unstable) • Echocardiography records pericardial effusion with
Asystole signs of
• Cardiopulmonary resuscitation (CPR) right ventricular and atrial compression.
• Advanced cardiac life support (ACLS) protocol for • ECG may reveal changes produced by acute
endotracheal pericarditis. This
intubation and possible transcutaneous pacing test rarely reveals tamponade but is useful to rule out
• Antiarrhythmics: atropine, epinephrine per ACLS other
protocol cardiac disorders.
Ventricular fibrillation Key treatments
• CPR • Surgery: pericardiocentesis (needle aspiration of the
• Defibrillation pericardial
• ACLS protocol for endotracheal intubation cavity) or surgical creation of an opening to drain fluid,
• Antiarrhythmics: amiodarone (Cordarone), thoracotomy
epinephrine, lidocaine • Adrenergic agent: epinephrine
(Xylocaine), magnesium sulfate, procainamide, • Inotropic agent: dopamine
vasopressin Key interventions
per ACLS protocol If the client needs pericardiocentesis
Ventricular tachycardia • Keep a pericardial aspiration needle attached to a
• CPR, if pulseless 50-ml
• Defibrillation syringe by a three-way stopcock, an ECG machine,
• Antiarrhythmics: amiodarone (Cordarone), and an
epinephrine, lidocaine emergency cart with a defibrillator at the bedside.
(Xylocaine), magnesium sulfate, procainamide Make sure the
• ACLS protocol for endotracheal intubation, if equipment is turned on and ready for immediate use.
pulseless • Position the client at a 45- to 60-degree angle.
Key interventions Connect the
• If the client’s pulse is abnormally rapid, slow, or precordial ECG lead to the hub of the aspiration
irregular, needle with an
watch for signs of hypoperfusion, such as alligator clamp and connecting wire. When the needle
hypotension and touches
altered mental status. the myocardium during fluid aspiration, an ST-
• When life-threatening arrhythmias develop, rapidly segment elevation
assess the or premature ventricular contractions appear.
level of consciousness, respirations, and pulse. • Monitor blood pressure and central venous pressure
• Initiate CPR, if indicated. (CVP)
• If trained, perform defibrillation early for ventricular during and after pericardiocentesis to monitor for
tachycardia complications
and ventricular fibrillation. such as hypotension, which may indicate cardiac
• Administer medications as needed, and prepare for chamber
medical puncture.
procedures (for example, cardioversion) if indicated. • Watch for complications of pericardiocentesis, such
• Provide adequate oxygen and reduce the heart’s as ventricular
workload, fibrillation, vasovagal response, or coronary artery or
while carefully maintaining metabolic, neurologic, cardiac chamber puncture.
respiratory, If the client needs a thoracotomy
and hemodynamic status. Follow ACLS protocol for • Explain the procedure to the client. Tell him what to
endotracheal expect
intubation. postoperatively (chest tubes and chest tube drainage
CARDIAC TAMPONADE system,
Key signs and symptoms administration of oxygen). Teach him how to turn,
• Muffled heart sounds on auscultation deep-breathe,
• Narrow pulse pressure and cough.
• Jugular vein distention • Maintain the chest tube drainage system and be
alert for complications,
such as hemorrhage and arrhythmias.
You might also like
- Test Bank For Understanding Abnormal Behavior 10th Edition SueDocument22 pagesTest Bank For Understanding Abnormal Behavior 10th Edition Sueandrewfranklin27051982otj100% (18)
- An Infectiouse Cure Help GuideDocument11 pagesAn Infectiouse Cure Help Guidemicrofreek100% (13)
- NEW BSN CURRICULUM - CMO 15 RevisedDocument2 pagesNEW BSN CURRICULUM - CMO 15 RevisedchoobiNo ratings yet
- Quiz On School Health NursingDocument7 pagesQuiz On School Health Nursingchoobi0% (2)
- Cardiac TamponadeDocument2 pagesCardiac TamponadechoobiNo ratings yet
- Hemodynamic Unstable Patient Following ArrhythmiaDocument30 pagesHemodynamic Unstable Patient Following Arrhythmialew chin hongNo ratings yet
- 10.15 Edrian Zulkarnain - ShockDocument42 pages10.15 Edrian Zulkarnain - ShockBintang UbamnataNo ratings yet
- Anestezia in Chirurgia CardiacaDocument179 pagesAnestezia in Chirurgia Cardiacamd.dascalescu2486No ratings yet
- Cardiovascular Disease: CPT Donald C Palma MCDocument46 pagesCardiovascular Disease: CPT Donald C Palma MCJorge RabajaNo ratings yet
- Tamponade KordisDocument20 pagesTamponade KordisMuhammad Aprianto RamadhanNo ratings yet
- Cardiac Tamponade (Suryani)Document72 pagesCardiac Tamponade (Suryani)Hamdani UsmanNo ratings yet
- LECTURE 8 - Early Detection and Management in Cardiac TamponadeDocument34 pagesLECTURE 8 - Early Detection and Management in Cardiac TamponadeWiwing SetionoNo ratings yet
- Richardson2014 PDFDocument2 pagesRichardson2014 PDFJanuar Alfred PoliNo ratings yet
- Theme 1 1Document97 pagesTheme 1 1lela ndociNo ratings yet
- Kardiogenik SyokDocument43 pagesKardiogenik SyokGalih Arief Harimurti WawolumajaNo ratings yet
- Pemicu 6 KGD DeniseDocument95 pagesPemicu 6 KGD DeniseVincent VandestyoNo ratings yet
- Angiography PDFDocument1 pageAngiography PDFanon_720827871No ratings yet
- Ptca PDFDocument1 pagePtca PDFOEDIEN-kmbNo ratings yet
- Angiography PDFDocument1 pageAngiography PDFanon_720827871No ratings yet
- Pericardial Effusion and Cardiac TamponadeDocument2 pagesPericardial Effusion and Cardiac TamponadeececasselNo ratings yet
- Aritmia Maligna - Abraham PDFDocument21 pagesAritmia Maligna - Abraham PDFDavid Ithu AgkhuNo ratings yet
- Multiprofessional Critical Care Review Course - 2005Document16 pagesMultiprofessional Critical Care Review Course - 2005asupicuNo ratings yet
- Chapter 5 Cardiovascular EmergenciesDocument6 pagesChapter 5 Cardiovascular Emergenciesعلاء البناءNo ratings yet
- 8 - DR. Khaled - Cardiac SurgeryDocument26 pages8 - DR. Khaled - Cardiac SurgeryMuhand.No ratings yet
- Structural Infectious and Inflammatory Cardiac Disorders and Medical ManagementDocument85 pagesStructural Infectious and Inflammatory Cardiac Disorders and Medical Managementmoncalshareen3No ratings yet
- Arrythmia ALLDocument103 pagesArrythmia ALLHeran MDNo ratings yet
- Thoracic Aortic AneurysmsDocument16 pagesThoracic Aortic AneurysmsdrchelluriNo ratings yet
- EmergencyDocument47 pagesEmergencymedstudy123No ratings yet
- MINI CP Angina PectorisDocument11 pagesMINI CP Angina Pectorisyasira100% (1)
- CH 46 Complications of AnaesthesiaDocument29 pagesCH 46 Complications of AnaesthesiaChristian LeepoNo ratings yet
- Cardiogenic ShockDocument49 pagesCardiogenic Shockmaibejose0% (1)
- Pericardium PDFDocument50 pagesPericardium PDFRawabi rawabi1997No ratings yet
- Patofisiologi Shock CardiogenicDocument44 pagesPatofisiologi Shock CardiogenicGalih Arief Harimurti Wawolumaja100% (1)
- Shock: & Metabolic Response To SurgeryDocument20 pagesShock: & Metabolic Response To SurgeryFemale calmNo ratings yet
- MVR CabgDocument57 pagesMVR CabgRoshani sharma100% (1)
- INTRA-AORTIC BALLOON PUMPING IN CARDIAC SURGERY (PDFDrive)Document55 pagesINTRA-AORTIC BALLOON PUMPING IN CARDIAC SURGERY (PDFDrive)shivalingam20No ratings yet
- Cardiac Catheterization and MonitoringDocument40 pagesCardiac Catheterization and MonitoringMarissa Asim100% (1)
- ECMO (Extracorporeal Membrane Oxygenation)Document22 pagesECMO (Extracorporeal Membrane Oxygenation)dhivya singhNo ratings yet
- Conduction Defects & ArrythmiasDocument73 pagesConduction Defects & Arrythmiasadamu mohammadNo ratings yet
- Valvular Heart Disease To TW FinalDocument13 pagesValvular Heart Disease To TW FinalMohammed ElSayedNo ratings yet
- Chapter - 036 Arrhythmias ClassDocument129 pagesChapter - 036 Arrhythmias ClassWisdomIsMiseryNo ratings yet
- ShockDocument24 pagesShockYaacub IbrahimNo ratings yet
- Valvular Heart DiseseDocument41 pagesValvular Heart DisesefadhiliNo ratings yet
- Physiomonitoring TransDocument4 pagesPhysiomonitoring TransAimie DagaleaNo ratings yet
- ARITMIADocument47 pagesARITMIASarah JR Nur AzizahNo ratings yet
- ACLS SubhankarDocument87 pagesACLS SubhankarMarc Andreo MalalaNo ratings yet
- Cardiac Arrythmias AbebawDocument50 pagesCardiac Arrythmias AbebawSufiyan AbduramanNo ratings yet
- ShockDocument19 pagesShockasmyr6975No ratings yet
- 12 Cardiac DisordersDocument27 pages12 Cardiac DisordersBheemasenachar PrasadNo ratings yet
- Screenshot 2565-05-03 at 10.34.19Document39 pagesScreenshot 2565-05-03 at 10.34.19Sugus PichayaNo ratings yet
- Atrial Fibrillation: Discussed by - DR Kunwar Sidharth SaurabhDocument45 pagesAtrial Fibrillation: Discussed by - DR Kunwar Sidharth SaurabhKunwar Sidharth SaurabhNo ratings yet
- Pericardialdiseases 190121084846Document65 pagesPericardialdiseases 190121084846Insta GrammerNo ratings yet
- Stable Ischemic HeartDocument217 pagesStable Ischemic HeartReda SoNo ratings yet
- 2 - PPT DR Erika Maharani SPJPDocument42 pages2 - PPT DR Erika Maharani SPJPAmry YusufNo ratings yet
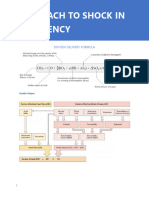
- Approach To Shock in Emergency - IGD RSFDocument15 pagesApproach To Shock in Emergency - IGD RSFMalikahNo ratings yet
- AntiarrhythmicsDocument7 pagesAntiarrhythmicszanderNo ratings yet
- LA Cardiac Arythmia - 0Document61 pagesLA Cardiac Arythmia - 0Karthik SNo ratings yet
- Cardiac TemponadeDocument18 pagesCardiac TemponadeDIVYA GANGWAR100% (1)
- CardioDocument67 pagesCardiovkhen88No ratings yet
- Pricardio Paracentesis/ Pericardiocentesis: Prepared By: Rashmita Byanju Shrestha Nursing Incharge Sicu and HduDocument17 pagesPricardio Paracentesis/ Pericardiocentesis: Prepared By: Rashmita Byanju Shrestha Nursing Incharge Sicu and HduArchana MaharjanNo ratings yet
- Myocardial Infarction: Maj Aswathy Ganesh I Year MSC (N) Con, AfmcDocument45 pagesMyocardial Infarction: Maj Aswathy Ganesh I Year MSC (N) Con, AfmcAswathy ganeshNo ratings yet
- CLASS 2 Low Cardiac Output Syndrome in Cardiac SurgeryDocument53 pagesCLASS 2 Low Cardiac Output Syndrome in Cardiac SurgeryjuanolivelloNo ratings yet
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- Advanced Concepts in Critical Care NursingDocument3 pagesAdvanced Concepts in Critical Care Nursingchoobi100% (1)
- Impact of Simulation-Based Teaching On Nursing Pharmacology Knowledge and Clinical CompetenceDocument2 pagesImpact of Simulation-Based Teaching On Nursing Pharmacology Knowledge and Clinical CompetencechoobiNo ratings yet
- Advanced Concepts in Critical Care NursingDocument3 pagesAdvanced Concepts in Critical Care Nursingchoobi100% (1)
- CIP Com Dev 2018Document4 pagesCIP Com Dev 2018choobiNo ratings yet
- ACCOMPLISHMENT REPORT On FAC. DEVDocument3 pagesACCOMPLISHMENT REPORT On FAC. DEVchoobiNo ratings yet
- Universal Prec QuestionsDocument8 pagesUniversal Prec QuestionschoobiNo ratings yet
- EVAL School Health NursingDocument4 pagesEVAL School Health NursingchoobiNo ratings yet
- Topics On Skills Lab Second SemDocument4 pagesTopics On Skills Lab Second SemchoobiNo ratings yet
- Assessment of Pulse SitesDocument2 pagesAssessment of Pulse SiteschoobiNo ratings yet
- Your Time Is LimitedDocument1 pageYour Time Is LimitedchoobiNo ratings yet
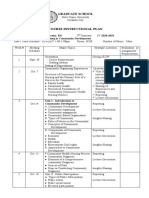
- Nres 1 Instructional PlanDocument10 pagesNres 1 Instructional PlanchoobiNo ratings yet
- level-of-disaster-preparedness-EDITED 1Document16 pageslevel-of-disaster-preparedness-EDITED 1choobiNo ratings yet
- Nurse RoleDocument1 pageNurse RolechoobiNo ratings yet
- Caselet School HealthDocument3 pagesCaselet School HealthchoobiNo ratings yet
- Eval Exam CHNDocument4 pagesEval Exam CHNchoobiNo ratings yet
- Abbreviations Used in DocumentationDocument6 pagesAbbreviations Used in DocumentationHydra Olivar - PantilganNo ratings yet
- Quatum DotsDocument9 pagesQuatum DotssherlyNo ratings yet
- Oncologic NursingDocument16 pagesOncologic NursingDharline Abbygale Garvida AgullanaNo ratings yet
- Classification of Dental CariesDocument79 pagesClassification of Dental Cariesmarukala100% (1)
- Appearance Anxiety Inventory (AAI)Document3 pagesAppearance Anxiety Inventory (AAI)Padmaja PradeepNo ratings yet
- Anticholinesterase AgentsDocument11 pagesAnticholinesterase AgentsEric AryantoNo ratings yet
- Draf BiDocument25 pagesDraf BiAhmad Aliuddin ShaharinNo ratings yet
- The Nursing Process in Psychiatric/Mental Health Nursing: PlanningDocument49 pagesThe Nursing Process in Psychiatric/Mental Health Nursing: PlanningJonalynCollodChewacheo50% (2)
- Cleansing and Moist Greg Goodman 2009Document1 pageCleansing and Moist Greg Goodman 2009Prajnamita Manindhya El FarahNo ratings yet
- Psychodynamic Treatment of Schizophrenia Is ThereDocument12 pagesPsychodynamic Treatment of Schizophrenia Is ThereMabel AppahNo ratings yet
- Emotional Behavior and Psychological Aspects ofDocument7 pagesEmotional Behavior and Psychological Aspects ofMar Jun Dalumbar AmpoNo ratings yet
- Cough N Cold Medicine List PDFDocument7 pagesCough N Cold Medicine List PDFDonna DominnoNo ratings yet
- Hyperbaric Oxygen Therapy Indications, Contraindictions and ComplicationsDocument5 pagesHyperbaric Oxygen Therapy Indications, Contraindictions and ComplicationsMark DingleNo ratings yet
- Introduction To Johari WindowDocument3 pagesIntroduction To Johari Windowsudhir letv100% (1)
- 2 - Harley Et Al 2008. Adaptation of Dialectical Behavior Therapy Skills Training Group For Treatment-Resistant DepressionDocument8 pages2 - Harley Et Al 2008. Adaptation of Dialectical Behavior Therapy Skills Training Group For Treatment-Resistant DepressionDaniele ModestoNo ratings yet
- Holistic Techs. LLC v. Lumina Group - ComplaintDocument63 pagesHolistic Techs. LLC v. Lumina Group - ComplaintSarah BursteinNo ratings yet
- UT Trauma HandbookDocument49 pagesUT Trauma Handbooksgod34No ratings yet
- Early DisturbsDocument3 pagesEarly DisturbsMaria GonzálezNo ratings yet
- A Review of Root Fractures Diagnosis Treatment andDocument10 pagesA Review of Root Fractures Diagnosis Treatment andAya Ibrahim YassinNo ratings yet
- Mudra - Supra PowersDocument3 pagesMudra - Supra PowersmakkuhotmailNo ratings yet
- Hospital Profile:: ApplicantDocument2 pagesHospital Profile:: Applicantdeepshikha singhNo ratings yet
- EbpDocument29 pagesEbpMad SlmNo ratings yet
- Co Misomal PresentationDocument46 pagesCo Misomal PresentationsalmanNo ratings yet
- 20hr Maternity Staff Course - Ses 5Document35 pages20hr Maternity Staff Course - Ses 5Norhanie Dida-agun AlimodenNo ratings yet
- Narcan InfographicDocument1 pageNarcan InfographicAnonymous C7bFTkrd5No ratings yet
- Memory and HypnosisDocument7 pagesMemory and HypnosisshadowraithsNo ratings yet
- Fournier S GangreneDocument8 pagesFournier S GangreneabhishekbmcNo ratings yet
- Dose Calculation: 1) Preparation of 1% V/V Tween 80 in Saline: (For 150 ML)Document3 pagesDose Calculation: 1) Preparation of 1% V/V Tween 80 in Saline: (For 150 ML)Apurba Sarker ApuNo ratings yet