Professional Documents
Culture Documents
Ophthalmology and Clinical Research: Clinmed
Ophthalmology and Clinical Research: Clinmed
Uploaded by
yohanes22Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ophthalmology and Clinical Research: Clinmed
Ophthalmology and Clinical Research: Clinmed
Uploaded by
yohanes22Copyright:
Available Formats
McElnea et al.
Int J Ophthalmol Clin Res 2015, 2:2
International Journal of ISSN: 2378-346X
Ophthalmology and Clinical Research
Case Report: Open Access
Corticosteroid in the Treatment of Neisseria gonorrhoeae Keratitis
Elizabeth McElnea1*, Sarah Moran2 and Gareth Higgins1
1
Department of Ophthalmology, University Hospital Waterford, Ireland
2
Department of Ophthalmology, Cork University Hospital, Ireland
*Corresponding author: Elizabeth McElnea, Department of Ophthalmology, University Hospital Waterford Ardkeen,
Co. Waterford, Ireland, Tel: 086 8528074, E-mail: mcelneaelizabeth@gmail.com
Abstract Comment
Aim: To describe the effective use of corticosteroid in the Ocular infection with Neisseria gonorrhoeae is relatively rare. We
management of keratitis caused by Neisseria gonorrhoeae. may be less suspicious of it as a result. Indeed, all four cases of corneal
perforation secondary to gonococcal infection described in one case
Methods: Retrospective review of the case of a nineteen year old series were originally misdiagnosed as epidemic keratoconjunctivitis
gentleman who presented with a purulent ocular discharge and in
[1].
whom peripheral corneal melt occurred.
Results: Neisseria gonorrhoeae was cultured from conjunctival Cases occur in sexually active individuals. Infection results from
swab. Systemic and topical antibiotics were given. The peripheral contact with infected urine and/or genital secretions. Such contact
corneal melt was unchanged until systemic corticosteroid was may be direct or by indirect ‘autoinoculation’ wherein infective
prescribed following which the corneal melt resolved promptly. genital secretions are transferred from their source to the eye’s surface
Conclusions: Neisseria gonorrhoeae keratitis may behave
by hand-eye contact.
like a peripheral ulcerative keratitis. In such cases topical and/ Genitourinary symptoms of gonococcal infection, if they occur
or systemic corticosteroid may be therapeutic despite their usual (up to 80% of males and 20% females affected in this regard are
contraindication in cases of acute infective keratitis.
asymptomatic) may precede ocular symptoms by one to several
Keywords weeks. Patients are howev er unlikely to make a connection between
their sexual behaviour, genital and ocular symptoms. Consequently,
Neisseria gonorrhoea, Keratitis, Corticosteroid, Peripheral
retrieval of the pertinent patient sexual and genitourinary system
ulcerative keratitis
history may be invaluable in suggesting a diagnosis of gonococcal
keratoconjunctivitis.
Description Neisseria gonorrhoeae causes a conjunctivitis which typically
The left eye of a nineteen year old gentleman became red and presents hyper-acutely with usually bilateral but occasionally, as
productive of a purulent discharge. A conjunctival swab was reserved.
Presumed to have bacterial conjunctivitis he was treated with topical
chloramphenicol and oral flucloxacillin 500mg both four times daily
for one week. Neisseria gonorrhoeae was however cultured. He was
referred to our service for further management.
His visual acuity at this time was 6/6 and 6/24 from his right and
left eyes respectively. The right eye looked normal. The conjunctiva
of the left eye was injected. It was however clear of discharge. A deep
gutter extended from the 10 o’clock to the 3 o’clock position in the
superior cornea. A smaller para-central area of corneal thinning
was also apparent (Figure 1). Treatment with topical exocin and
ceftazidime every hour and intravenous ceftriaxone 2g and oral
ciprofloxacin 750mg twice daily was commenced. The appearance
of this gentleman’s left eye remained unchanged however after five
days. Prednisolone 40 mg orally daily was commenced and reduced
Figure 1: A deep gutter extended from the 10 o’clock to the 3 o’clock
by 10mg daily every week thereafter. The peripheral corneal melt position in the superior portion of this gentleman’s cornea. A smaller para-
resolved within two weeks. central area of corneal thinning was also present.
Citation: McElnea E, Moran S, Higgins G (2015) Corticosteroid in the Treatment of
Neisseria gonorrhoeae Keratitis. Int J Ophthalmol Clin Res 2:020
ClinMed Received: March 07, 2015: Accepted: March 30, 2015: Published: April 02, 2015
Copyright: © 2015 McElnea E. This is an open-access article distributed under the terms of
International Library the Creative Commons Attribution License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original author and source are credited.
diffuse lamellar keratitis three years after laser in situ keratomileusis
has already been described [7].
Rapid progression of an ulcerative keratitis to corneal perforation
can reportedly occur within 24 h of infection with Neisseria
gonorrhoeae [8]. Further, the outcome of this infection depends
upon its severity when appropriate therapy is commenced [9].
‘Appropriate’ therapy in some cases may thus include topical and/or
systemic corticosteroid despite their usual contraindication in cases
of acute infective keratitis.
Conclusion
We hope this report will serve as a reminder of both the occurrence
and indeed the potential severity of gonococcal eye disease. A sexual
and genitourinary system history should be obtained from all
Figure 2: In this gentleman’s case the clinical appearance was very similar those with a purulent ocular discharge. Severe gonococcal keratitis
to an immune mediated peripheral corneal melt. Note the relative lack of may be unilateral. This may behave like a peripheral corneal melt.
stromal disease elsewhere in the cornea beyond the area of ulceration Consequently topical and/or systemic steroid may be therapeutic.
superiorly.
References
here, unilateral, extreme, conjunctival inflammation and an intensely 1. Kawashima M, Kawakita T, Den S, Tomita M, Shimazaki J (2009)
purulent ocular discharge. The presence of an intensely purulent Surgical management of corneal perforation secondary to gonococcal
keratoconjunctivitis. Eye (Lond) 23: 339-344.
ocular discharge in a sexually active individual should always raise
the suspicion of gonococcal eye infection. Tender eyelid oedema 2. Hegde V, Smith G, Choi J, Pagliarini S (2005) A case of gonococcal kerato-
can also occur. Ocular motility may be restricted. Indeed unilateral conjunctivitis mimicking orbital cellulitis. Acta Ophthalmol Scand 83: 511-512.
gonococcal conjunctivitis initially thought to be orbital cellulitis has 3. Wan WL, Farkas GC, May WN, Robin JB (1986) The clinical characteristics
been described [2]. and course of adult gonococcal conjunctivitis. Am J Ophthalmol 102: 575-
583.
Common corneal findings include a marginal corneal ulcer or 4. Centers for Disease Control and Prevention (CDC) (2012) Update to CDC’s
corneal melt, sub-epithelial and/or stromal infiltrates and a discrete Sexually transmitted diseases treatment guidelines, 2010: oral cephalosporins
oedema of the entire cornea [3]. The first of these may be most no longer a recommended treatment for gonococcal infections. MMWR Morb
common and is thought to be due to the formation of pus filled Mortal Wkly Rep 61: 590-594.
troughs beneath the eyelids. 5. Kenyon KR (1985) Inflammatory mechanisms in corneal ulceration. Trans Am
Ophthalmol Soc 83: 610-663.
Currently, the CDC recommends combination therapy with a
6. Ullman S, Roussel TJ, Culbertson WW, Forster RK, Alfonso E, et al. (1987)
single intramuscular dose of ceftriaxone 250mg plus either a single Neisseria gonorrhoeae keratoconjunctivitis. Ophthalmology 94: 525-531.
dose of azithromycin 1g orally or doxycycline 100mg orally twice daily
7. Symes RJ, Catt CJ, Males JJ (2007) Diffuse lamellar keratitis associated with
for 7 days for the treatment of uncomplicated urogenital, anorectal, gonococcal keratoconjunctivitis 3 years after laser in situ keratomileusis. J
and pharyngeal gonorrhea. In instances where ceftriaxone is not Cataract Refract Surg 33: 323-325.
available, cefixime 400mg orally, plus either azithromycin 1g orally or
8. Duke-Elder S (1965) Diseases of the outer eye. In: System of Ophthalmology
doxycycline 100mg orally twice daily for 7 days should be used. For Vol. 8. Part 1.St. Louis: CV Mosby Co, USA.
patients allergic to the cephalosporins, the CDC recommends use of a
9. Lee JS, Choi HY, Lee JE, Lee SH, Oum BS (2002) Gonococcal
single 2g dose of azithromycin orally. In both of these circumstances, keratoconjunctivitis in adults. Eye (Lond) 16: 646-649.
a test of cure for these patients should be carried out one week after
treatment [4].
In that particular case of gonococcal keratitis described here
the clinical appearance was very similar to an immune mediated
peripheral corneal melt. Indeed, we were particularly impressed by
the relative lack of stromal disease elsewhere in the cornea beyond the
area of ulceration (Figure 2).
The influence of inflammatory cells and their enzymatic products
in stromal destruction in auto-immune peripheral corneal melt
is already well established [5]. The polymorphonuclear (PMN)
cell is thought to be most important. Since the migration of PMN
cells is from the limbal vasculature into the corneal stroma most
immune mediated tissue damage is limbal. Neisseria gonorrhoea
was not cultured from the cornea of eyes with severe gonococcal
keratitis which were enucleated as might be expected were corneal
penetration secondary to active bacterial replication [6]. Similarly,
in our case, though an aggressive, extensive peripheral corneal
melt persisted following the administration of antibiotics, we were
unable to demonstrate the presence of organisms in specimens
taken at conjunctival swab and corneal scrape. The relative role of
the enzymatic products of the PMN cell in the pathogenesis of
gonococcal keratitis is unknown but given the appearance of the
cornea in the case we describe here we postulate that it is relatively
great. Indeed the peripheral corneal ulceration resolved only when
systemic corticosteroids were administered.
The successful use of topical corticosteroid in the treatment of
a case of Neisseria gonorrhoeae keratitis which was associated with
McElnea et al. Int J Ophthalmol Clin Res 2015, 2:2 ISSN: 2378-346X • Page 2 of 2 •
You might also like
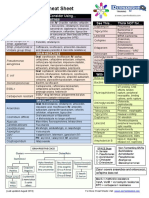
- Antibiotic Study Cheat Sheet August 2019Document1 pageAntibiotic Study Cheat Sheet August 2019Ryan TurnerNo ratings yet
- Cardio WorkbookDocument5 pagesCardio WorkbookZhy Caluza100% (1)
- 20 Powerful Health Benefits of Guyabano Leaves TeaDocument8 pages20 Powerful Health Benefits of Guyabano Leaves TeaJayson Jugan Mangubat100% (4)
- BNB ListDocument73 pagesBNB ListbenNo ratings yet
- Posted at The Institutional Resources For Unique Collection and Academic Archives at Tokyo Dental College, Available From Http://ir - Tdc.ac - JPDocument20 pagesPosted at The Institutional Resources For Unique Collection and Academic Archives at Tokyo Dental College, Available From Http://ir - Tdc.ac - JPwhiezardNo ratings yet
- Shukla2008 PDFDocument17 pagesShukla2008 PDFPpa Gpat AmitNo ratings yet
- Fig. 1 Fig. 2: E. Linton Et AlDocument2 pagesFig. 1 Fig. 2: E. Linton Et AlFitriAndiniNo ratings yet
- 005 PDFDocument7 pages005 PDFNely KartikaNo ratings yet
- Bab 1 KeratitisDocument12 pagesBab 1 Keratitisverlita utamiNo ratings yet
- Journal Reading - Update On The Management of Infectious KeratitisDocument23 pagesJournal Reading - Update On The Management of Infectious Keratitistasya noerchaerunisaNo ratings yet
- Microbial Keratitis in Corneal Grafts: Predisposing Factors and OutcomesDocument7 pagesMicrobial Keratitis in Corneal Grafts: Predisposing Factors and Outcomesmono1144No ratings yet
- American Journal of Ophthalmology Case Reports: Samantha Mcgirr, Dallin Andersen (MD), John Halgren (MD) TDocument2 pagesAmerican Journal of Ophthalmology Case Reports: Samantha Mcgirr, Dallin Andersen (MD), John Halgren (MD) TKhalfiaNo ratings yet
- Konjungtivitis GonoreDocument2 pagesKonjungtivitis Gonorefk unswagatiNo ratings yet
- The Pathogenesis and Prevention of Corneal Graft Melting After KeratoplastyDocument9 pagesThe Pathogenesis and Prevention of Corneal Graft Melting After KeratoplastywahyuNo ratings yet
- NiharikaKShetty 7557Document8 pagesNiharikaKShetty 7557Sriram ChandramohanNo ratings yet
- Cataract As A Complication of Severe Microbial KerDocument5 pagesCataract As A Complication of Severe Microbial KeryaddaNo ratings yet
- Contact Lens & Anterior EyeDocument4 pagesContact Lens & Anterior Eyedori45No ratings yet
- A Study On Clinico-Etiological Profile of Mycotic Keratitis in Tertiary Care Hospital at Government Medical College, Kota (Rajasthan)Document7 pagesA Study On Clinico-Etiological Profile of Mycotic Keratitis in Tertiary Care Hospital at Government Medical College, Kota (Rajasthan)IJAR JOURNALNo ratings yet
- Cronicon: Review Article Keratitis: An Inflammation of CorneaDocument7 pagesCronicon: Review Article Keratitis: An Inflammation of Corneaalter egoNo ratings yet
- Conjunctivitis As A Manifestation of Wegener 'S GranulomatosisDocument5 pagesConjunctivitis As A Manifestation of Wegener 'S GranulomatosisAsd DsaNo ratings yet
- Amniotic Membrane Transplantation Combined With Antiviral and Steroid Therapy For Herpes Necrotizing Stromal KeratitisDocument7 pagesAmniotic Membrane Transplantation Combined With Antiviral and Steroid Therapy For Herpes Necrotizing Stromal KeratitisnelyNo ratings yet
- JournalDocument16 pagesJournalNur intan cahyaniNo ratings yet
- PPK Perhati Vol1 Okt2015Document13 pagesPPK Perhati Vol1 Okt2015Nurul Annisa MuthaharaNo ratings yet
- Contact LensDocument6 pagesContact LensReno Prananditya AshafNo ratings yet
- Corneal Ulcer - StatPearls - NCBI BookshelfDocument5 pagesCorneal Ulcer - StatPearls - NCBI BookshelfAngel LimNo ratings yet
- Management of KeratitisDocument12 pagesManagement of KeratitisSeptian Harry WibowoNo ratings yet
- KeratitisDocument70 pagesKeratitisHoopmen Silaen100% (1)
- Conditions of The CorneaDocument38 pagesConditions of The Corneac/risaaq yuusuf ColoowNo ratings yet
- Viral Keratitis: Current ConceptsDocument8 pagesViral Keratitis: Current ConceptsDini MayrisdayaniNo ratings yet
- KeratitisDocument21 pagesKeratitistifano_arian9684No ratings yet
- Bacterial Keratitis: Signs and SymptomsDocument4 pagesBacterial Keratitis: Signs and Symptoms]]]100% (1)
- Successful Salvage Therapy of Fusarium Endophthalmitis Secondary To Keratitis: An Interventional Case SeriesDocument6 pagesSuccessful Salvage Therapy of Fusarium Endophthalmitis Secondary To Keratitis: An Interventional Case SeriesKreAch3RNo ratings yet
- JCDR 8 DD01Document4 pagesJCDR 8 DD01ojiNo ratings yet
- Case Report: An Unusual Unilateral Pterygium - A Secondary Pterygium Caused by Parasitosis in The Scleral FistulaDocument3 pagesCase Report: An Unusual Unilateral Pterygium - A Secondary Pterygium Caused by Parasitosis in The Scleral FistulaGrnitrv 22No ratings yet
- Gonococcal KCDocument10 pagesGonococcal KCfikerteadelleNo ratings yet
- 10.nicula Cristina Final PRDocument4 pages10.nicula Cristina Final PRayub01No ratings yet
- Kjo 19 233Document2 pagesKjo 19 233Rita HastaNo ratings yet
- HHS Public Access: Update On The Management of Infectious KeratitisDocument24 pagesHHS Public Access: Update On The Management of Infectious KeratitisBella Pratiwi AnzaniNo ratings yet
- Lit Review - Contact Lens Associated Pseudomonas KeratitisDocument8 pagesLit Review - Contact Lens Associated Pseudomonas KeratitisAlien4mearthNo ratings yet
- Fungal Keratitis in FarmerDocument4 pagesFungal Keratitis in FarmerChikita Rizqi HanifatiNo ratings yet
- Disease: Bacterial KeratitisDocument9 pagesDisease: Bacterial KeratitisDwi Ayu PrimadanaNo ratings yet
- Jceh 12 30 021Document3 pagesJceh 12 30 021Tatik HandayaniNo ratings yet
- Tugas BacaDocument20 pagesTugas BacaAyu WulansariNo ratings yet
- Jurnal MataaDocument35 pagesJurnal MataaWivan Havilian DjohanNo ratings yet
- Conjunctivitis Due To Neisseria Sicca: A Case Report: ReferencesDocument4 pagesConjunctivitis Due To Neisseria Sicca: A Case Report: ReferencesnidaNo ratings yet
- Queratitis BacterianaDocument5 pagesQueratitis BacterianaRichi CiriacoNo ratings yet
- Lacrimal Duct Occlusion Is Associated With Infectious KeratitisDocument6 pagesLacrimal Duct Occlusion Is Associated With Infectious KeratitisekaNo ratings yet
- KeratitisDocument32 pagesKeratitiscrushnaNo ratings yet
- Entropion 3 PDFDocument5 pagesEntropion 3 PDFdhitadwynNo ratings yet
- Acute Conjunctivitis (Pink Eye) - Overview, Clinical Evaluation, Bacterial ConjunctivitisDocument2 pagesAcute Conjunctivitis (Pink Eye) - Overview, Clinical Evaluation, Bacterial ConjunctivitisLutfi ari206No ratings yet
- M. Srinivasan - Keratitis-Intech (2012)Document70 pagesM. Srinivasan - Keratitis-Intech (2012)alex_andra_22No ratings yet
- Steroids in The Management of Infectious Keratitis.1Document7 pagesSteroids in The Management of Infectious Keratitis.1Ceendy AngelNo ratings yet
- 1 PBDocument11 pages1 PBMega RebbekaNo ratings yet
- Diagnosis and Management Protocol of Acute Corneal Ulcer: Vaishal P Kenia, Raj V Kenia, Onkar H PirdankarDocument10 pagesDiagnosis and Management Protocol of Acute Corneal Ulcer: Vaishal P Kenia, Raj V Kenia, Onkar H PirdankarEVINo ratings yet
- Scedosporium Apiospermium Keratitis: A Case: Case Report Open AccessDocument5 pagesScedosporium Apiospermium Keratitis: A Case: Case Report Open AccessqalbiNo ratings yet
- Corneal Atlas 2011Document20 pagesCorneal Atlas 2011Wentao Liu100% (5)
- Imprimir 2Document3 pagesImprimir 2Gino VitteriNo ratings yet
- Background: View Media GalleryDocument8 pagesBackground: View Media GalleryAza Patullah ZaiNo ratings yet
- NAME:-Puspendu Maity. ROLL: - 16101717014. Reg. No: - 171611210014. Subject: - Corneal Ulcer. Semester: - 7 SemesterDocument15 pagesNAME:-Puspendu Maity. ROLL: - 16101717014. Reg. No: - 171611210014. Subject: - Corneal Ulcer. Semester: - 7 SemesterKumar jit MaityNo ratings yet
- Steroid KeratitisDocument8 pagesSteroid KeratitisNanda Wiguna TyndiansyahNo ratings yet
- Interstitial Keratitis PDFDocument22 pagesInterstitial Keratitis PDFwilliam sitnerNo ratings yet
- Keratoconus An Updated Review PDFDocument26 pagesKeratoconus An Updated Review PDFMaria Jose SanjinesNo ratings yet
- MainDocument3 pagesMainomidazadmehr1375No ratings yet
- Complications in UveitisFrom EverandComplications in UveitisFrancesco PichiNo ratings yet
- Eosinophilic Laryngitis in Children With Aerodigestive DysfunctionDocument6 pagesEosinophilic Laryngitis in Children With Aerodigestive DysfunctionIntan Nur HijrinaNo ratings yet
- Ischemic Stroke Outcome - A Review of The Influence of Post-Stroke Complications Within The Different Scenarios of Stroke CareDocument13 pagesIschemic Stroke Outcome - A Review of The Influence of Post-Stroke Complications Within The Different Scenarios of Stroke CarewatiNo ratings yet
- Brochure PDFDocument16 pagesBrochure PDFFebinNo ratings yet
- ENT ExaminationDocument36 pagesENT ExaminationLiji GeorgeNo ratings yet
- Han Book of Signs in Clinical DermatologyDocument180 pagesHan Book of Signs in Clinical DermatologyLumière Cosmetología integralNo ratings yet
- The Spirurida WordDocument19 pagesThe Spirurida WordayaamrsharfNo ratings yet
- MED SURG Final CoachingDocument12 pagesMED SURG Final Coachingkim torino100% (1)
- DRUG STUDY OXYTOCIN, METHERGINE EtcDocument9 pagesDRUG STUDY OXYTOCIN, METHERGINE EtcPatricia Reese YutiamcoNo ratings yet
- Pathophysiology of Persistent Pulmonary Hypertension of The New BornsDocument3 pagesPathophysiology of Persistent Pulmonary Hypertension of The New Bornsnathaniel_ramos_3No ratings yet
- Supportive Care in Clinical ToxicologyDocument9 pagesSupportive Care in Clinical ToxicologyJAMAL WARIS0% (1)
- 11 Strategies To Overcome HashimotoDocument21 pages11 Strategies To Overcome Hashimotoalbinuta100% (1)
- PHP2018Document25 pagesPHP2018radu nicolaeNo ratings yet
- Post StrokeDocument23 pagesPost StrokeAthalia TalawayNo ratings yet
- Case-Scenario-Major Depressive Disorder-BuenconsejoDocument6 pagesCase-Scenario-Major Depressive Disorder-BuenconsejoCarna BuenconsejoNo ratings yet
- SilicosisDocument11 pagesSilicosisDurge Raj GhalanNo ratings yet
- Leukimia Dan ThalasemiaDocument39 pagesLeukimia Dan ThalasemialeilaNo ratings yet
- Good Morning.: @areebazainabDocument42 pagesGood Morning.: @areebazainabshabana waniNo ratings yet
- Biliary StrictureDocument27 pagesBiliary StrictureMohammad Nazar100% (2)
- DysphagiaDocument21 pagesDysphagiaRajendran Dinesh KumarNo ratings yet
- Melena, Diarrhea, NauseaDocument5 pagesMelena, Diarrhea, Nauseakelompok 6B IDIKNo ratings yet
- Case Study Introduction CKDDocument6 pagesCase Study Introduction CKDRhajibNo ratings yet
- Hipoglikemia Pada BayiDocument18 pagesHipoglikemia Pada BayiAngelika Gratia LiempepasNo ratings yet
- Music and Medicine The Affect of Music On The Human BeingDocument10 pagesMusic and Medicine The Affect of Music On The Human BeingTariq J FaridiNo ratings yet
- A & B Materia Medica by AlphabetDocument46 pagesA & B Materia Medica by AlphabetYASIR KHAN100% (2)
- Labor Stage II (Expulsion)Document15 pagesLabor Stage II (Expulsion)nursereview100% (7)
- Hematology Lecture - AnemiaDocument10 pagesHematology Lecture - AnemiaKimberly EspaldonNo ratings yet