Professional Documents
Culture Documents
Diabetes Care Nov 2003
Diabetes Care Nov 2003
Uploaded by
Priscilla ArtesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetes Care Nov 2003
Diabetes Care Nov 2003
Uploaded by
Priscilla ArtesCopyright:
Available Formats
Reviews/Commentaries/Position Statements
C O M M I T T E E R E P O R T
Follow-up Report on the Diagnosis of
Diabetes Mellitus
THE EXPERT COMMITTEE ON THE DIAGNOSIS predict diabetes, and questions have been
AND CLASSIFICATION OF DIABETES raised about the preference of the FPG test
MELLITUS* over the 2-h PG to diagnose diabetes (5–
7). Second, the IGT category has now
been associated with cardiovascular dis-
ease (CVD) risk factors (8 –10) and CVD
events (10,11), whereas IFG is much less
I
n 1997, an International Expert Com- odology resulting in varying nondiabetic
mittee was convened to reexamine the reference ranges among laboratories. strongly associated with CVD events and
classification and diagnostic criteria of 4) Although the OGTT (which con- CVD mortality (10,11). Third, the Na-
diabetes, which were based on the 1979 sists of an FPG and 2-h PG value) was tional Glycosylated Hemoglobin Stan-
publication of the National Diabetes Data recognized as a valid way to diagnose di- dardization Program (NGSP) has now
Group (1) and subsequent WHO study abetes, the use of the test for diagnostic ensured that most laboratories in the U.S.
group (2). As a result of its deliberations, purposes in clinical practice was discour- perform the assays using standardized
the Committee recommended several aged for several reasons (e.g., inconve- controls and report glycated hemoglobin
changes to the diagnostic criteria for dia- nience, less reproducibility, greater cost). results in a manner traceable to the assay
betes and for lesser degrees of impaired The diagnostic category of impaired glu- used in the Diabetes Control and Compli-
glucose regulation (IFG/IGT) (3). The fol- cose tolerance (IGT) was retained to de- cations Trial (DCCT) (12). These devel-
lowing were the major changes or issues scribe people whose FPG was ⬍126 opments have improved assay
addressed. mg/dl but whose 2-h PG after a 75-g oral performance and now allow caregivers
1) The use of a fasting plasma glucose glucose challenge was 140 –199 mg/dl. and patients to compare reported results
(FPG) test for the diagnosis of diabetes 5) The range of FPG levels between obtained among laboratories. Additional
was recommended, and the cut point sep- “normal” and that diagnostic for diabetes studies have suggested that the A1C may
arating diabetes from nondiabetes was was named “impaired fasting glucose” assist in diagnosing diabetes (13–17). Fi-
lowered from FPG ⱖ140 mg/dl (7.8 (IFG). IFG identified people whose FPG nally, data from major clinical trials that
mmol/l) to ⱖ126 mg/dl (7.0 mmol/l). (All ranged from 110 mg/dl (6.1 mmol/l) to tested whether the progression from IGT
glycemic values represent venous plas- 125 mg/dl (6.9 mmol/l). This construct to diabetes could be delayed or prevented
by a treatment intervention have pro-
ma.) This change was based on data that was established so that there would be a
duced concordant results: intensive life-
showed an increase in prevalence and in- fasting category analogous to IGT.
style modification (nutritional and
cidence of diabetic retinopathy beginning The WHO consultation (4) also
exercise interventions) (18,19), met-
at approximately a FPG of 126 mg/dl, as adopted most of the above conclusions.
formin (19,20), and acarbose (20,21)
well as on the desire to reduce the dis- The two significant differences were that, were effective to variable degrees. In ad-
crepancy that existed in the number of whenever feasible, individuals with IFG dition, a thiazolidinedione drug (troglita-
cases detected by the FPG cut point of should receive an OGTT to exclude the zone) reduced the incidence of diabetes in
ⱖ140 mg/dl and the 2-h value in the presence of diabetes, and the adoption of high-risk women with prior gestational
OGTT (2-h plasma glucose [2-h PG]) of different criteria for the diagnosis of ges- diabetes (22).
ⱖ200 mg/dl (11.1 mmol/l). tational diabetes. An inherent difficulty in the diagnosis
2) Normal FPG was defined as ⬍110 Since the 1997 Expert Committee re- of diabetes is the present lack of an iden-
mg/dl (6.1 mmol/l). port, many new data related to the diag- tified unique qualitative biological
3) The use of HbA1c (A1C) as a diag- nosis of diabetes have been published. marker that separates all people with dia-
nostic test for diabetes was not recom- First, many analyses of both old and new betes from all nondiabetic individuals.
mended. The primary reason for this epidemiological data have examined the The closest such characteristic for practi-
decision was a lack of standardized meth- equivalence of the FPG and the 2-h PG to cal purposes is diabetic retinopathy, but
this suffers from the obvious defect that in
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
most diabetic patients, retinopathy usu-
Address correspondence and reprint requests to Dr. Richard Kahn, 1701 North Beauregard St., Alexan- ally becomes evident years after the rec-
dria,VA 22311. E-mail: rkahn@diabetes.org. ognized onset of diabetes. The lack of a
A complete list of Expert Committee members can be found in the acknowledgments.
Abbreviations: 2-h PG, 2-h plasma glucose; CVD, cardiovascular disease; DCCT, Diabetes Control and suitable, unique marker of diabetes has
Complications Trial; DECODE, Diabetes Epidemiology: Collaborative analysis Of Diagnostic criteria in led to reliance on the metabolic abnor-
Europe; FPG, fasting plasma glucose; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; NGSP, mality historically associated with the dis-
National Glycosylated Hemoglobin Standardization Program; NHANES III, Third National Health and ease, i.e., hyperglycemia (as measured by
Examination Survey.
A table elsewhere in this issue shows conventional and Système International (SI) units and conversion
the FPG or 2-h PG) as the most useful
factors for many substances. diagnostic test. The selection of diagnos-
© 2003 by the American Diabetes Association. tic cut points for these tests rests on two
3160 DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003
Committee Report
observations: the bimodality of the distri- rent World Health Organization (WHO) who are more likely to have an elevated
bution of both glucose values in some criterion for diagnosing diabetes in epide- 2-h PG.
populations (23,24), albeit with overlap miological studies is an FPG ⱖ126 mg/dl The differences in the prevalence of
of normal and diabetic levels, and the (7.0 mmol/l) or a 2-h PG ⱖ200 mg/dl diabetes by one criterion versus the other
ability of FPG and 2-h PG to predict the (11.1 mmol/l) in the OGTT (4). Using the could be interpreted as indicating that
presence of diabetic retinopathy or the 2-h PG criterion, compared with the 1997 there might be two metabolically distinct
risk of developing it in the future (3). ADA criterion of FPG ⱖ126 mg/dl alone early forms of type 2 diabetes. However,
In light of the new information, a re- (5), the average difference in prevalence the data are too scant to subclassify type 2
constituted International Expert Com- of diabetes in 16 European populations diabetes formally into two distinct dis-
mittee met to evaluate these issues and from eight countries (totaling 26,190 eases, based on the use of FPG or 2-h PG.
make revisions to the previous criteria people) was ⫹0.5%, with a range of ⫺4 to It should be stressed that all these epide-
where appropriate. This report summa- ⫹13%. Based on the Third National miologic studies are based on a single glu-
rizes the deliberations. Health and Examination Survey cose measurement, while the full criteria
(NHANES III) data discussed in the 1997 for the diagnosis of diabetes require a con-
Question 1: Should the cut point of Report (3), the difference in prevalence firmatory test in asymptomatic subjects.
FPG >126 mg/dl (>7.0 mmol/l) or compared with the previous criterion of Differences in prevalence by the two dif-
the cut point for the 2-h PG of >200 FPG ⱖ140 mg/dl or 2-h PG ⱖ200 mg/dl ferent criteria could therefore also result
mg/dl (11.1 mmol/l) for the was ⫺2.0% (26). Thus, overall, no consis- from the large day-to-day variability in
diagnosis of diabetes, or both, be tent difference in the prevalence of diabetes the tests. In conclusion, we recommend
changed? across populations has been observed by that the cut points for the diagnosis of
The diagnostic levels of glucose, both FPG employing the 1997 FPG criterion. diabetes by FPG and 2-h PG should re-
and 2-h PG, are largely predicated on In the same studies, it was noted that main as in our 1997 report. (Table 1)
their association with the risk of having or although the FPG criterion of ⱖ126
developing retinopathy. Based on the data mg/dl and the 2-h PG criterion of ⱖ200 Question 2: Should the lower limit
reviewed in the 1997 report (3), the inci- mg/dl sometimes identify the same indi- for IFG be reduced from 110 mg/dl?
dence of retinopathy increases above an viduals, they often do not coincide. In the The category IFG was introduced to des-
FPG of ⱖ126 mg/dl, rather than above European DECODE study (5), of 1,517 ignate the zone between the upper limit of
140 mg/dl. Although one recent study people with diabetes by either criterion normal FPG and the lower limit of dia-
(49) suggests that an even lower FPG cut alone or by both criteria, only 28% met betic FPG, much as IGT designates the
point would be appropriate, in the ab- both criteria. A total of 40% met the fast- zone between the upper limit of normal
sence of supporting data from additional ing criterion only, and 31% met the 2-h 2-h PG and the lower limit of diabetic 2-h
populations, no new cut point can be rec- PG criterion only. Among those who met PG. The ideal method of selecting the
ommended. Similarly, there are no new the 2-h PG criterion, 51% did not meet lower limit of IFG would be the identifi-
cogent data favoring a change in the 2-h the fasting criterion, and 59% of those cation of a threshold of FPG at which the
PG cut point for the diagnosis of diabetes who met the fasting criterion did not meet risk of a clinical or metabolic outcome
per se. If all-cause mortality or CVD mor- the 2-h PG criterion. In the NHANES III rises sharply. Data from Mauritius (28)
tality were to be used as the criterion to study of previously undiagnosed diabetic indicate that such a threshold of FPG does
define a risk threshold, the Diabetes Epi- adults age 40 –74, 44% met both the 2-h not exist for cardiovascular risk factors,
demiology: Collaborative analysis Of Di- PG and FPG criteria, 14% met the FPG all-cause mortality, or future diabetes.
agnostic criteria in Europe (DECODE) criterion but not the 2-h PG criterion, and Also, the DECODE study recently re-
study reports that a 2-h PG of ⬃180 41% met the 2-h PG criterion alone (27). ported that there was no glycemic thresh-
mg/dl would provide a similar risk cutoff The discrepancy between the European old for either FPG or 2-h PG above which
as an FPG of 126 mg/dl (11). and U.S. distributions may be explained mortality increases sharply (11). Both
The 2-h criterion of 200 mg/dl iden- by the fact that the U.S. study population very low and high FPG were associated
tifies a larger fraction of the population as was more obese and, therefore, more with an increased risk of death, whereas
having diabetes than the previous fasting likely to have an elevated FPG and did not the 2-h PG was a continuous risk factor
criterion of 140 mg/dl. To eliminate, or at include elderly people (age ⱖ75 years) for mortality. On the other hand, data
least reduce this discrepancy, the Expert
Committee in 1997 recommended lower-
ing the fasting criterion to 126 mg/dl. Table 1—Diagnostic thresholds for diabetes and lesser degrees of impaired glucose regulation
It was believed at the time that this
change would justify de-emphasizing the Test
OGTT, since some of the individuals pre-
Category FPG 2-h PG
viously identifiable only by this test
would have fasting values between 126 Normal ⬍100 mg/dl (⬍5.6 mmol/l) ⬍140 mg/dl (⬍7.8 mmol/l)
and 139 mg/dl and would thus be identi- IFG 100–125 mg/dl (5.6–6.9 mmol/l) —
fied by the new fasting criterion. It was IGT — 140–199 mg/dl (7.8–11.0 mmol/l)
also believed at the time that these new Diabetes* ⱖ126 mg/dl (ⱖ7.0 mmol/l) ⱖ200 mg/dl (ⱖ11.1 mmol/l)
recommendations would have a minimal When both tests are performed, IFG or IGT should be diagnosed only if diabetes is not diagnosed by the other
impact on prevalence estimates. The cur- test. *A diagnosis of diabetes needs to be confirmed on a separate day.
DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003 3161
Committee Report
from the Pima Indians show that the risk line levels of FPG to predict diabetes, later In summary, the data we reviewed, on
of diabetes does increase markedly at FPG diagnosed by a FPG ⱖ126 mg/dl or 2-h balance, suggest that the cut point for IFG
concentrations above ⬃100 mg/dl (26). PG ⱖ200 mg/dl, have been recently ana- should be reduced from 110 mg/dl to 100
Thus, the selection of a lower limit of lyzed by the Expert Committee in four mg/dl, and that IFG should be redefined
IFG and 2-h PG is likely to be somewhat populations (data unpublished). The FPG as an FPG of 100 –125 mg/dl (5.6 – 6.9
arbitrary. The upper limit of normal in the value at the point on the receiver operator mmol/l). We also recommend that the cut
FPG (110 mg/dl) was taken from clinical characteristic curve closest to the ideal of point for IGT remain as a 2-h PG value
laboratory experience, although recently 100% sensitivity and 100% specificity between 140 –199 mg/dl (7.8 –11.0
a value of 106 mg/dl has been reported to over the glycemic range of 81–126 mg/dl mmol/l).
be the upper limit (95th percentile) of the (4.5–7.0 mmol/l) was 103 mg/dl (5.7
normal range established from measure- mmol/l) in a Dutch population, 97 mg/dl Question 3: Should the HbA1c (A1C)
ments made in a large population of ap- (5.4 mmol/l) in a Pima Indian population, level be included as a criterion for
parently healthy people (29,30). The 94 mg/dl (5.4 mmol/l) in a Mauritius pop- the diagnosis of diabetes?
rationale for establishing the intermediate ulation, and 94 mg/dl (5.2 mmol/l) in a Soon after the introduction of the glyco-
categories of impaired glucose regulation San Antonio population. These values hemoglobin assay as an index of glycemia,
was based on their ability to predict future suggest that 110 mg/dl was inappropri- its use for the diagnosis of diabetes was
diabetes. However, as pointed out in the ately high as a lower limit for IFG. Thus, considered. Measurement of glycohemo-
1997 report (3), the range of FPG values changing the IFG cut point to 100 mg/dl globin (A1C) for this purpose has numer-
that defines IFG (110 –125 mg/dl) in- (5.6 mmol/l) would optimize its sensitiv- ous advantages.
cludes a much lower proportion of the ity and specificity for predicting future di- 1) A1C measures average glycemic
population than is included in the IGT abetes. Of course, decreasing the lower levels in a time scale of weeks, whereas
category. This has been confirmed in limit of IFG will also have the virtue of plasma glucose varies greatly within any
eight population studies reviewed by Un- increasing the proportion of those with given day and from day to day. Thus, an
win et al. (31). Of those who had IFG IGT who can be identified by a FPG test. elevated A1C indicates a chronic state of
and/or IGT, 16% had both, 23% had IFG In addition, such a change will consider- hyperglycemia, while hyperglycemia as
alone, and 60% had IGT alone (31), with ably increase the absolute number of peo- measured by the FPG or 2-h PG may be
significant age and gender differences ple with IFG and, thereby, affect the transitory.
among the glucose intolerance categories. relative proportion of people with IFG or 2) The patient does not have to fast or
Although it may be desirable for IFG and IGT. otherwise prepare, and a blood sample
IGT to be equivalent (i.e., to represent While the choice of a lower cut point can be drawn any time of day.
similar proportions of the population or can be made on the basis of the epidemi- 3) In reference laboratories, the pre-
even better the same individuals), if the ologic predictive data as described above, cision of A1C measurement is similar to
two tests are measuring somewhat differ- other factors that should influence the the measurement of plasma glucose
ent metabolic states, then any discrepancy choice of the cut point are not currently (29,34).
is not necessarily a “flaw” in one of the known for IFG. For example, we do not 4) A test that can be used to diagnose
tests. yet know the total benefit or the total cost diabetes and evaluate the results of treat-
The predictive powers of IFG and IGT to an individual who is designated at risk ment is an attractive measurement, as
alone for development of diabetes over for diabetes by either test, by any crite- compared with our current situation,
several years are similar in some but not rion. The higher the ratio of benefit to which calls for using different tests to di-
all populations. The sensitivity of IFG as cost, the lower the optimal cut point that agnose the disease and then monitor
originally defined is less than that of IGT should be selected. Inasmuch as most treatment.
in most populations (31), but the speci- (⬃80%) of the participants in the Diabe- 5) There is a threshold level of A1C
ficity of IFG may be somewhat greater, as tes Prevention Program (19) with IGT associated with risk for retinopathy, as
was found in a population from Mauritius also had an FPG of 100 –125 mg/dl, an there is for FPG and 2-h PG (3). A graph
(28). IGT identifies a larger number of intensive lifestyle intervention may also showing the risk of diabetic microvascu-
individuals who will ultimately develop be beneficial in delaying or preventing di- lar complications based on A1C levels is
diabetes, largely because IGT is more abetes in individuals with IFG by the pro- superimposable on similar graphs, in
common than IFG in most populations. posed new definition. However, another which glycemia is expressed by the FPG
These differences between the predictive much less intensive lifestyle intervention or 2-h PG levels.
abilities of IFG and IGT were shown, at has not been shown to reduce the risk in 6) A recent meta-analysis showed that
least among Pima Indians, to be entirely a subjects selected by an FPG criterion when using a statistical cut point of 2 SDs
function of different cut points rather alone (33). At the same time, it must be above the nondiabetic mean A1C value to
than differences in FPG or 2-h PG as pre- acknowledged that a benefit similar to diagnose diabetes, as defined by the 2-h
dictive tests (26). When categorized in that shown in the DPP has not yet been PG, a variety of A1C assays had a mean
groups containing equal frequencies of proven by a clinical trial for people with sensitivity of 66% and a specificity of
the population, abnormalities of FPG or FPG of 100 –125 mg/dl who do not also 98%, which compares favorably to the
2-h PG had the same predictive values for have IGT. Finally, it should be noted that FPG (13).
subsequent diabetes (26). the lower cut point of 140 mg/dl that cur- On the other hand, measurement of
The receiver operator characteristic rently defines IGT was itself selected on A1C for the diagnosis of diabetes still has
(32) curve of the ability of various base- arbitrary criteria. disadvantages.
3162 DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003
Committee Report
1) A profusion of assay methods has using an OGTT. Thus, we now have sev- plasma glucose at a postchallenge stan-
led to different nondiabetic reference eral potential reasons to do a test of gly- dard time point at any time of day. The
ranges because different glycated hemo- cemia: to either diagnose diabetes or results of these studies led to the ascen-
globin fractions have been measured (30). impaired glucose regulation or to indicate dancy of the 2-h PG as the “gold standard
This problem has been reduced in the increased risk for CVD. The question aris- test.” However, if in the early studies only
U.S. because of the efforts of the NGSP. es: which test of hyperglycemia, the FPG fasting values had been reported, and the
Although the NGSP has succeeded in or 2-h PG, is most appropriate? FPG test was viewed as the “gold stan-
standardizing ⬃95% of the laboratories We think it helpful to frame the fol- dard,” then attention today would likely
in the U.S., with results certified as “trace- lowing discussion of diabetes tests on the be focused on the decreased sensitivity
able to the DCCT A1C assay,” (12) the basis of generic criteria that one might use and specificity of the 2-h PG to detect di-
level of precision and accuracy of the A1C for choosing any diagnostic tests. 1) Are abetes (i.e., some people meeting FPG cri-
test may still not be sufficient in all labo- the tests measuring an important feature teria for diabetes would be missed by the
ratories to allow the assay to be used to of the disease in question? 2) What are the 2-h PG alone, and some people nondia-
diagnose diabetes. Moreover, in many relative advantages and disadvantages of betic by FPG would be “falsely” diagnosed
countries, A1C assays are not widely the tests to detect the condition in ques- by the 2-h PG).
available and no A1C standardization tion? 3) What are the comparative fea- Neither the FPG nor 2-h PG cut point
program has even begun. Newer methods tures of the tests insofar as ease of use, denotes end-organ damage per se. Rather,
for measuring A1C by mass spectrometry, reproducibility of results, and cost to per- they indicate future risk for microvascular
although not practical for clinical use, form? 4) What are the adverse conse- and perhaps macrovascular complica-
have the potential to provide better stan- quences in terms of any “lost opportunity” tions (35– 42,49). Indeed, there is a su-
dardization across all A1C assays. if one test versus the other is used? perimposable, continuous relationship
2) A chemical preparation to create between the fasting and 2-h values and
uniform calibration standards has only re- How does the FPG or 2-h OGTT the risk of diabetic microvascular compli-
cently been established (30). This prepa- relate to the condition to be cations above a threshold for each (3,49).
ration however has not yet been widely detected? By lowering the cut point for IFG (as
adopted. The FPG and 2-h PG are both single recommended above), the IFG popula-
3) A1C values may be affected by point-in-time measures of glycemia. Both tion will now include a greater percentage
other conditions (e.g., hemoglobinopa- are associated with adverse outcomes that of individuals who also have IGT (⬃30%
thy, pregnancy, uremia, blood transfu- result from chronic hyperglycemia. Al- of those with IFG will have IGT). Of note,
sion, and hemolytic anemia), and though they are not entirely interchange- even with an IFG cut point of 100 mg/dl,
depending on the laboratory method able, since the FPG alone does not always there will be individuals who have IFG
used, this may confound the diagnosis of detect people with IGT and the 2-h PG but not IGT and vice versa. The clinical
diabetes. does not always detect people with IFG, significance of either discrepancy is not
On balance, therefore, it seems best to both tests are useful in terms of their abil- completely known, but each condition,
continue to use the A1C test as a monitor ity to detect hyperglycemia and the con- even in the absence of the other, is a risk
for the effectiveness of glycemic therapy sequences of disordered glucose factor for subsequent diabetes.
and as an indicator for when therapy metabolism. Most (25,42– 48), but not all (39,49 –
needs to be modified. In conclusion, the 52), longitudinal observational studies
Committee believes that it is still prema- What are their relative advantages have reported that an elevated 2-h PG
ture to add A1C to the group of tests used and disadvantages? value (but below that diagnostic of diabe-
for the definitive diagnosis of diabetes. A discussion of the sensitivity and speci- tes) is a better predictor of all-cause mor-
ficity of a test mandates comparison to tality or CVD morbidity/mortality than an
Question 4: What is the value of the some objective “gold standard.” In this re- elevated FPG value. From that finding, it
2-h PG in addition to the FPG? gard, the FPG test is compromised since it is inferred that the 2-h PG value is a better
In the 1997 report, we indicated that “al- is usually compared with the 2-h PG, test to employ for the diagnosis of diabe-
though the OGTT is an acceptable diag- which has de facto been considered the tes or impaired glucose regulation. All of
nostic test. . . it is not recommended for “gold standard.” By this standard, the FPG the studies, however, have one or more of
routine use” (3). This statement resulted has, of course, less sensitivity. The OGTT the following shortcomings that make it
in reports expressing concern that many was originally designed to detect an ab- difficult to conclude that the 2-h PG is the
individuals who would have been diag- normality in glucose metabolism in pa- better test.
nosed only by the 2-h PG would now be tients with normal FPG levels by First, in many reports, the ability of
missed. Other reports noted that the 2-h perturbing homeostasis with a glucose FPG and 2-h PG to predict CVD and total
PG is superior to the FPG because it challenge. The 2-h PG result from the mortality was evaluated using categorical
would detect individuals at increased risk OGTT subsequently became a convenient groupings, e.g., those with or without IFG
for CVD and that these individuals would way to detect glycemic abnormalities in were compared with those with IGT,
not be identified by the FPG (31). In ad- individuals, even when they were tested rather than studying the predictive power
dition, several major studies have now in a nonfasting state. Early studies took of each test over the entire range of its
documented the ability to prevent or de- advantage of the combination of the possible values. The categorical analyses
lay the onset of diabetes in individuals greater metabolic sensitivity of the OGTT affect the comparison between the tests
with IGT, only identifiable by definition with the conveniences of measuring because, for example, the “window” of
DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003 3163
Committee Report
plasma glucose (in mg/dl) is much larger a significant reduction in body weight, added information it may provide. How-
for IGT than it is for IFG. However, in blood pressure, and triglyceride levels, ever, questions still remain regarding the
some studies, the 2-h PG was better than the drug may be exerting a CVD benefit ultimate clinical impact or value of detect-
the FPG for predicting mortality across by a mechanism other than through its ing diabetes or IGT when the FPG is nor-
the range of plasma glucose values. glucose-lowering effect per se. In addi- mal. These uncertainties have led to
Second, in none of the studies was the tion, the secondary analysis may be con- opposing editorial positions (68,69) on
relationship between IFG and IGT and founded by some study design factors and which test to use. The evidence still pre-
the incident adverse outcome adjusted for limitations in the statistical analysis, as the cludes definitively declaring either test
incident diabetes that may have already authors acknowledged. Thus, although more advantageous than the other.
occurred first during the follow-up pe- there is growing evidence that glucose
riod. Thus, it is unclear to what extent the lowering in patients with impaired glu- What other features are related to
development of diabetes (or other CVD cose regulation may reduce CVD, a defin- either test?
risk factors that developed during follow- itive clinical study is needed before such a The measurement of FPG is less expensive
up, such as hypertension) influenced the treatment recommendation can be made. and less intrusive than the 2-h PG. Al-
end point adverse outcome. This short- In some patients, a 2-h PG value di- though both tests require overnight fast-
coming may be important, since in longi- agnostic of diabetes in an individual with ing for at least 8 h, the 2-h PG frequently
tudinal analyses (49,53), only individuals a normal FPG or IFG might trigger phar- results in an extended office visit for the
who progressed from NGT or IGT to dia- macologic glucose-lowering therapy. patient, potentially resulting in more lost
betes during follow up had increased all- However, in the vast majority of these pa- wages or an inability to engage in other
cause and CVD mortality compared with tients, the pretreatment A1C level will be desired activities. A minority of patients
those who did not progress to diabetes. ⬍6.5% (56), and the extent to which such cannot tolerate the glucose challenge
Therefore, IGT and IFG per se may not be patients would benefit from such drug drink, making the results of the test unin-
the causative factor for CVD, but rather therapy is not known. On the other hand, terpretable because the full glucose load
they are risk factors for developing diabe- a 2-h PG value diagnostic of diabetes was not ingested. On the other hand,
tes, which is then associated in some fash- mandates lower blood pressure and lipid some patients will not have actually
ion with the pathogenesis of CVD. goals compared with nondiabetic individ- fasted, potentially resulting in a falsely el-
Third, although these cohort studies uals (57), although no clinical trial has evated FPG, whereas the impact of non-
generally performed baseline adjustments focused specifically on the benefits of fasting on the 2-h PG value may be less.
for numerous well-known CVD risk fac- treating such patients to these targets. The FPG test is more reproducible
tors, none adjusted for all known CVD Among individuals with IFG, there will be than the 2-h PG. The day-to-day intra-
risk factors or for recently recognized some in whom the 2-h PG, if performed, individual coefficients of variation range
causal/associative factors such as plas- will identify diabetes. Thus, performing a from 6.4 to 11.4% for FPG and 14.3 to
minogen activator inhibitor 1 or C-reac- 2-h PG might be considered in subjects 16.7% for the 2-h PG (70 –73). In addi-
tive protein. This is an important with IFG, as recommended by the WHO tion, the overall test retest reproducibility
consideration because two recent studies consultation (4). using the OGTT is unsatisfactory (74).
found that the 2-h PG added relatively Much has been written on the patho- The San Antonio group (75) reported that
little (51) or nothing (52) for identifying genesis of diabetes (58 – 61), with consid- patients diagnosed with diabetes exclu-
CVD risk if other traditional risk factors erable data indicating that resistance to sively on the basis of the 2-h PG were five
were considered, although this has not insulin action in peripheral tissues is an times more likely to revert to nondiabetic
been a consistent finding (45). early feature, followed by or simultaneous status after 7– 8 years of follow-up than
Even if there is an independent rela- with progressive -cell dysfunction. Both those meeting the 126 mg/dl FPG diag-
tionship between IFG or IGT and all- ultimately contribute to the development nostic criteria. In the Paris Prospective
cause or CVD related outcomes, there is of diabetes. It has been suggested that in- Study (76), 72% of those in whom diabe-
incomplete evidence that a glycemic in- sulin resistance and/or compensatory hy- tes was diagnosed by the 2-h PG value
tervention benefits patients by preventing perinsulinemia convey an elevated risk of alone reverted to nondiabetic status after
CVD. In most of the diabetes prevention CVD (62,63). If this proves to be true, and 30 months of follow-up compared with
trials (18 –20), the participants were not an elevated 2-h PG is a marker for early- 42% of the patients diagnosed with dia-
followed long enough to determine stage insulin resistance, it might be useful betes by FPG. Thus, the FPG test is more
whether any clinical outcome was af- to identify individuals at particularly high reliable (at least for the diagnosis of dia-
fected. In the UKPDS (U.K. Prospective risk for CVD who might then benefit from betes) and less costly than the 2-h PG.
Diabetes Study) (54), the evidence was intervention. However, other parameters
inconclusive that lowering glucose per se related to the metabolic syndrome (64 – Is there a “lost opportunity” by
in people with diabetes will favorably im- 67) may be more relevant to CVD risk, doing one test versus the other?
pact macrovascular disease. Alternatively, and here too, we do not as yet have clin- Is there evidence that choosing the
a recent secondary analysis of the data ical trial evidence showing that lowering “wrong” test will have adverse conse-
from the STOP-IDDM trial indicated that insulin resistance per se in those with quences? If individuals who develop ab-
IGT subjects (most of whom also had IFG IGT, or even in those with diabetes, actu- normalities of one glucose test (FPG or
or diabetes by FPG criteria) had a signifi- ally reduces CVD events. 2-h PG) eventually develop an abnormal
cantly reduced risk of CVD (55). How- In summary, there are reasons why a value in the other, then the only disadvan-
ever, since acarbose is also associated with 2-h PG might be the preferred test for the tage of restricting testing to a single glu-
3164 DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003
Committee Report
cose test is delayed diagnosis for those in Conclusions K. Williamson (San Antonio) and Dr. R.L.
whom the “wrong” test was chosen. At Based on the data that have appeared in Hanson and S. Kobes (Phoenix) for perform-
present, there is no evidence that such the literature since the 1997 Expert Com- ing the receiver operating curve analysis.
delayed diagnosis is critical. Conversely, mittee report, we recommend that the cri- Members of the 2003 Expert Committee are
Saul Genuth, MD (Chair), K.G.M.M. Alberti,
it may be true that some or many individ- teria to diagnose diabetes should remain MD, FRCP, PhD, Peter Bennett, MB, FRCP,
uals with diabetes by 2-h PG or FPG will as previously defined. However, the lower John Buse, MD, PhD, Ralph DeFronzo, MD,
never develop diabetes as measured by cut point defining IFG should be reduced Richard Kahn, PhD, John Kitzmiller, MD, Wil-
the other test. In that case, the diagnosis of from ⱖ110 mg/dl to ⱖ100 mg/dl (ⱖ5.6 liam C. Knowler, MD, DrPH, Harold Lebovitz,
diabetes by either test might be worth- mmol/l). Thus, “normal” would now be MD, Ake Lernmark, MD, David Nathan, MD,
while. For either scenario, we have no defined as a FPG ⬍100 mg/dl. The re- Jerry Palmer, MD, Robert Rizza, MD, Christo-
data to inform our choice of test. The vised thresholds are shown in Table 1. In pher Saudek, MD, Jonathan Shaw, MD, Mi-
OGTT offers the obvious advantage that a addition, the Committee concludes that chael Steffes, MD, Michael Stern, MD, Jaakko
FPG and 2-h PG are both measured, the FPG and 2-h PG (but not the A1C test) Tuomilehto, MD, PhD, and Paul Zimmet, MD,
whereas when measuring FPG alone, no remain the tests of choice for the diagno- PhD.
information about the 2-h PG value is sis of both their respective impaired
known. As previously noted (11), all- states, as well as for the diagnosis of dia- References
cause mortality is increased in people betes. There are arguments in favor of ei- 1. National Diabetes Data Group: Classifica-
with normal FPG but who are diabetic ther test. The 2-h PG, because of the tion and diagnosis of diabetes mellitus
based on the 2-h PG; however, it is not currently defined cut points for diabetes, and other categories of glucose intoler-
known whether treating this state of is a more sensitive assay in most popula- ance. Diabetes 28:1039 –1057, 1979
asymptomatic diabetes will in fact reduce tions. But the FPG is more reproducible, 2. World Health Organization: Diabetes Mel-
mortality. less costly, and likely to be more conve- litus: Report of a WHO Study Group. Ge-
nient. neva, World Health Org., 1985 (Tech.
Is it possible to identify people likely Rep. Ser., no. 727)
There are obviously many aspects re-
3. The Expert Committee on the Diagnosis
to have IFG/IGT using other garding the specific measurements of gly- and Classification of Diabetes Mellitus:
characteristics? cemia that are still unclear. Further Report of the expert committee on the di-
Models to predict prevalent IGT, incident research is needed to improve our under- agnosis and classification of diabetes mel-
diabetes, or CVD without employing a standing and approach toward detecting litus. Diabetes Care 20:1183–1197, 1997
measure of glucose intolerance (52,77– IFG, IGT, or diabetes. For example, more 4. World Health Organization: Definition,
80) have been developed. Some of the work needs to be done to standardize the Diagnosis and Classification of Diabetes Mel-
models have excluded any measurement A1C assay worldwide, so that this mea- litus and its Complications: Report of a WHO
of glycemia (78 – 80), while others have sure could be routinely employed for di- Consultation. Part 1: Diagnosis and Classifi-
included FPG (52,77). Such models are agnosing diabetes. Second, we need to cation of Diabetes Mellitus. Geneva, World
invariably more effective in the popula- Health Org., 1999
better understand the pathophysiology 5. DECODE Study Group on Behalf of the
tion from which they were derived than in and risks associated with IFG and IGT. Do European Diabetes Epidemiology Study
independent confirmation datasets from they represent distinct metabolic abnor- Group: Will new diagnostic criteria for di-
other populations. In those few studies malities or to what extent are they part of abetes mellitus change phenotype of pa-
where the model was derived from one a continuum? What are the true adverse tients with diabetes? Reanalysis of
population and tested in another (78,79), outcomes associated with either? Will European epidemiological data. BMJ 317:
it did not perform sufficiently well to ob- measurement of factors other than plasma 371–375, 1998
viate the need for blood glucose testing. glucose identify populations that would 6. Larsson H, Berglund G, Lindgarde F,
Although these models hold promise, benefit from prevention strategies dem- Ahren B: Comparison of ADA and WHO
confirmatory independent testing across onstrated to be effective in clinical trials? criteria for diagnosis and glucose intoler-
various populations must be performed ance (Letter). Diabetologia 41:1124 –
Finally, to what extent can future CVD be 1125, 1998
in order to demonstrate sufficient utility ameliorated if the cut points for IFG, IGT, 7. Davies MJ, Raymond NT, Day JL, Hales
for their widespread use. or diabetes are changed and treatment of CN, Burden AC: Impaired glucose toler-
In summary, there is currently inade- glycemia is initiated earlier? The answers ance and the fasting hyperglycaemia have
quate clinical evidence that either test is to these and other questions will necessi- different characteristics. Diabet Med
superior. Given the methodological fea- tate regular surveillance and reconsidera- 17:433– 440, 2000
tures of the FPG test, it remains the test of tion of new data that may lead to 8. Rathmann W, Giani G, Mielck A: Cardio-
choice in clinical practice where cost, appropriate revisions to the diagnostic vascular risk factors in newly diagnosed
convenience, and reproducibility are im- and classification criteria for diabetes over abnormal glucose tolerance: comparison
portant considerations. For research of 1997 ADA and 1985 WHO criteria
time.
studies or in clinical situations in which it (Letter). Diabetologia 42:1268 –1269,
1999
is important, to the extent possible, to 9. Hanefield M, Temelkova-Kurktschiev T,
rule in or out every case of diabetes or Acknowledgments — The committee greatly Schaper F, Henkel E, Siegert G, Koehler
every case of IFG/IGT, the FPG and 2-h appreciates the Hoorn Study Research Group C: Impaired fasting glucose is not a risk
PG should be performed. It is important (Drs. L.M. Bouter, J.M. Dekker, R.J. Heine, G. factor for atherosclerosis. Diabet Med 16:
to keep in mind that confirmatory testing Nijpels, and C.D.A. Stehouwer) who provided 212–218, 1999
is recommended to diagnose diabetes. data from the Hoorn study. We also thank Dr. 10. The DECODE Study Group, the Euro-
DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003 3165
Committee Report
pean Diabetes Epidemiology Group: multicenter prospetive study. Clin J Endo- bet Med 19:708 –723, 2002
Glucose tolerance and cardiovascular crinol Metab 17:131–135, 2001 32. Bortheiry AL, Malerbi DA, Franco LJ: The
mortality: comparison of fasting and 21. Chiasson JL, Josse Rg, Gomis R, Hanefeld ROC curve in the evaluation of fasting
2-hour diagnostic criteria. Arch Intern M, Karasik A, Laakso M: Acarbose for pre- capillary blood glucose as a screening test
Med 161:397– 404, 2001 vention of type 2 diabetes mellitus: the for diabetes and IGT. Diabetes Care 17:
11. The DECODE Study Group, on behalf of STOP-NIDDM randomized trial. Lancet 1269 –1272, 2002
the European Diabetes Epidemiology 359:2072–2077, 2002 33. Dyson PA, Hammersley MS, Morris RJ,
Group: Is the current definition for diabe- 22. Buchanan TA, Xiang AH, Peters RK, Kjos Holman RR, Turner RC: The Fasting Hy-
tes relevant to mortality risk from all SL, Marroquin A, Goico J, Ochoa C, Tan perglycaemia Study. II. Randomized con-
causes and cardiovascuar and noncardio- S, Berkowitz K, Hodis HN, Azen SP: Pres- trolled trial of reinforced healthy-living
vascular diseases? Diabetes Care 26:688 – ervation of pancreatic -cell function and advice in subjects with increased but not
696, 2003 prevention of type 2 diabetes by pharma- diabetic fasting plasma glucose. Metabo-
12. Little RR: Glycated hemoglobin standard- cological treatment of insulin resistance in lism 46 (12 Suppl. 1):50 –55, 2002
ization: National Glycohemoglobin Stan- high-risk Hispanic women. Diabetes 51: 34. Sacks DB: College of American Pathologists
dardization Program (NGSP) Perspective 2796 –2803, 2002 Glycohemoglobic Survey 2002. Set GH2-A,
(Review). Clin Chem Lab Med. In Press 23. Rusforth NB, Bennett PH, Miller M: Fast- CAP2000
13. Peters AL, Davidson MB, Schriger DL, ing and two-hour post-blood glucose lev- 35. Coutinho M, Gerstein HC, Wang Y, Yusuf
Hasselblad V: A clinical approach for the els for the diagnosis of diabetes: the S: The relationship between glucose and
diagnosis of diabetes mellitus: an analysis relationship between glucose levels and incident cardiovascular events: a metar-
using glycosylated hemoglobin levels: complications of diagetes in the Pima In- egression analysis of published data from
Meta-analysis Research Group on the Di- dians. Diabetologia 16:373–379, 1970 20 studies of 95,783 individuals followed
agnosis of Diabetes Using Glycated He- 24. Zimmet P, Whitehouse S: Bimodality of for 12.4 years. Diabetes Care 22:233–240,
moglobin Levels. JAMA 276:1246 –1252, fasting and two-hour glucose tolerance 1997
1996 distributed in a Micronesian population. 36. Balkau B, Bertrais S, Ducimetiere P, Es-
14. Rohlfing CL, Little RR, Wiedmeyer H, En- Diabetes 27:793– 800, 1970 chwege E: Is there a glycemic threshold
gland JD, Madsen R, Harris MI, Flegal 25. Smith NL, Barzilay JI, Shaffer D, Savage for mortality risk? Diabetes Care 22:696 –
KM, Eberhardt MS, Goldstein DE: Use of PJ, Heckbert SR, Kuller LH, Kronmal RA, 699, 1997
GHb (HbA1c) in screening for undiag- Resnick HE, Psaty BM: Fasting and 37. Bjornholt JV, Erikssen G, Aaser E, Sand-
nosed diabetes in the U. S. population. 2-hour postchallenge serum glucose mea- vik L, Nitter-Hauge S, Jervell J, Erikssen J,
Diabetes Care 23:187–191, 2000 sures and risk of incident cardiovascular Thaulow E: Fasting blood glucose: an un-
15. Wang W, Lee ET, Fabsitz R, Welty TK, events in the elderly: the Cardiovascular derestimated risk factor for cardiovascu-
Howard BV: Using HbA1c to improve ef- Health Study. Arch Intern Med 162:209 – lar death: results from a 22-year follow-up
ficacy of the American diabetes associa- 216, 2002 of healthy nondiabetic men. Diabetes Care
tion fasting plasma glucose criterion in 26. Gabir MM, Hanson RL, Dabelea D, Im- 22:45– 49, 1999
screening for new type 2 diabetes in peratore G, Roumain J, Bennett PH, 38. Fuller JH, Shipley MJ, Rose G, Jarrett RJ,
American Indians. Diabetes Care 25: Knowler WC: The 1997 American Diabe- Keen H: Coronary-heart-disease risk and
1365–1370, 2002 tes Association and 1999 World Health impaired glucose tolerance: the Whitehall
16. Barr RG, Nathan DM, Meigs JB, Singer Organization criteria for hyperglycemia in study. Lancet 1:1373–1376, 1980
DE: Tests of glycemia for the diagnosis of the diagnosis and prediction of diabetes. 39. Saydah SH, Miret M, Sung J, Varas C,
type 2 diabetes mellitus. Ann Intern Med Diabetes Care 23:1108 –1112, 2000 Gause D, Brancati FL: Postchallenge hy-
137:263–272, 2002 27. Harris MI, Eastman RC, Cowie CC, Flegal perglycemia and mortality in a national
17. Ko G, Chan J, Yeung V, Chow C, Tsang L, KM, Eberhardt MS: Comparison of diabe- sample of U. S. adults. Diabetes Care 24:
Li J, So W, Wai H, Cockram C: Combined tes diagnostic categories in the U. S. pop- 1397–1402, 2001
use of a fasting plasma glucose concentra- ulation according to 1997 American 40. Eschwege E, Charles MA, Simon D, Thib-
tion and HbA1c or fructosamine predicts Diabetes Association and 1980 –1985 ult N, Balkau B: From policemen to poli-
the likelihood of having diabetes in high- World Health Organization diagnostic cies: what is the future for 2-h glucose?
risk subjects. Diabetes Care 21:1221– criteria. Diabetes Care 20:1859 –1862, The Kelly West Lecture, 2000. Diabetes
1225, 1998 1997 Care 24:1945–1950, 2001
18. Tuomilehto J, Lindström J, Eriksson JG, 28. Shaw JE, Zimmet PZ, Hodge AM, de 41. de Vegt F, Dekker JM, Stehouwer CD, Ni-
Valle TT, Hämäläinen H, Ilanne-Parikka Courten M, Dowse GK, Chitson P, Tuom- jpels G, Bouter LM, Heine RJ: Similar
P, Keinänen-Kiukaanniemi S, Laakso M, ilehto J, Alberti KGMM: Impaired fasting 9-year mortality risks and reproducibility
Louheranta A, Rastas M, Salminen V, glucose: how low should it go? Diabetes for the World Health Organization and
Uusitupa M: Prevention of type 2 diabetes Care 23:34 –39, 2000 American Diabetes Association glucose
mellitus by changes in lifestyle among 29. Burtis CA, Ashwood ER: Tietz Textbook of tolerance categories: the Hoorn Study. Di-
subjects with impaired glucose tolerance. Clinical Chemistry. 3rd ed. Philadelphia, abetes Care 23:40 – 44, 2000
N Engl J Med 344:1343–1350, 2001 W.B. Saunders, 1999, p. 782 42. de Vegt F, Dekker JM, Ruhe HG, Stehou-
19. Diabetes Prevention Program Research 30. Sacks DB, Bruns DE, Goldstein DE, Ma- wer CD, Nijpels G, Bouter LM, Heine RJ:
Group: Reduction in the incidence of type claren NK, McDonald JM, Parrott M: Hyperglycaemia is associated with all-
2 diabetes with lifestyle intervention or Guidelines and recommendations for lab- cause and cardiovascular mortality in the
metformin. N Engl J Med 346:393– 403, oratory analysis in the diagnosis and man- Hoorn population: the Hoorn Study. Dia-
2002 agement of diabetes mellitus. Clin Chem betologia 42:926 –931, 1999
20. Wenying Y, Lixiang L, Jimevu Q, Zhiqing 48:436 – 472, 2002 43. The DECODE Study Group, European
Y, Haicheng P, Guofeng H, et al: The pre- 31. Unwin N, Shaw J, Zimmet P, Alberti Diabetes Epidemiology Group: Diabetes
ventative effect of acarbose and met- KGMM: Impaired glucose tolerance and Epidemiology: Collaborative analysis Of
formin on the progression to diabetes impaired fasting glycaemia: the current Diagnostic criteria in Europe: glucose tol-
mellitus in the IGT population: a 3 year status on definition and intervention. Dia- erance and mortality: comparison of
3166 DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003
Committee Report
WHO and American Diabetes Association with conventional treatment and risk of Knowler WC: Components of the “meta-
diagnostic criteria. Lancet 354:617– 621, complications in patients with type 2 diabe- bolic syndrome” and incidence of type 2
1999 tes (UKPDS 33). Lancet 352:837– 853, diabetes. Diabetes 51:3120 –3127, 2002
44. Barzilay JI, Spiekerman CF, Wahl PW, 1998 68. Tuomilehto J: Point: a glucose tolerance
Kuller LH, Cushman M, Furberg CD, 55. Chiasson J-L, Josse RG, Gormis R, test is important for clinical practice. Di-
Dobs A, Polak JF, Savage PJ: Cardiovascu- Hanefeld M, Karasik A, Laakso M, the abetes Care 25:1880 –1882, 2002
lar disease in older adults with glucose STOP-NIDDM Trial Research Group: 69. Davidson MB: Counterpoint: the oral glu-
disorders: comparison of American Dia- Acarbose treatment and the risk of cardio- cose tolerance test is superfluous. Diabetes
betes Association criteria for diabetes mel- vascular disease and hypertension in pa- Care 25:1883–1885, 2002
litus with WHO criteria. Lancet 354:622– tients with impaired glucose tolerance: 70. Feskens EJ, Bowles CH, Kromhout D: In-
625, 1999 the STOP-NIDDM trial. JAMA 290:486 – tra- and interindividual variability of glu-
45. Barrett-Connor E, Ferrara A: Isolated post- 494, 2003 cose tolerance in an elderly population.
challenge hyperglycemia and the risk of fa- 56. Harris MI, Eastman RC: Early detection of J Clin Epidemiol 44:947–953, 1991
tal cardiovascular disease in older women undiagnosed diabetes mellitus: a US per- 71. McDonald GW, Fisker GF, Burnham C:
and men: the Rancho Bernardo Study. Dia- spective. Diabetes Metab Res Rev 16:230 – Resproducibility of the oral glucose toler-
betes Care 21:1236 –1239, 1998 236, 2000
ance test. Diabetes 14:473– 480, 1965
46. Rodriguez BL, Lau N, Burchfiel CM, Ab- 57. American Diabetes Association: Stan-
72. Olefsky JM, Reaven GM: Insulin and glu-
bott RD, Sharp DS, Yano K, Curb JD: Glu- dards of medical care for patients with di-
cose responses to identical oral glucose
cose intolerance and 23-year risk of abetes mellitus. Diabetes Care 26 (Suppl.
coronary heart disease and total mortality: 1):S33–S50, 2003 tolerance tests performed forty-eight
the Honolulu Heart Program. Diabetes 58. Bogardus C, Lillioja S, Howard BV, hours apart. Diabetes 23:449 – 453, 1974
Care 22:1262–1265, 1999 Reaven G, Mott D: Relationships between 73. Mooy JM, Grootenhuis PA, de Vries H,
47. Tominaga M, Eguchi H, Manaka H, Iga- insulin secretion, insulin action, and fast- Kostense PJ, Popp-Snijders C, Bouter LM,
rashi K, Kato T, Sekikawa A: Impaired ing plasma glucose concentration in Heine RJ: Intra-individual variation of
glucose tolerance is a risk factor for car- nondiabetic and noninsulin-dependent glucose, specific insulin and proinsulin
diovascular disease, but not impaired fast- diabetic subjects. J Clin Invest 74:1238 – concentrations measured by two oral glu-
ing glucose: the Funagata Diabetes Study. 1246, 1984 cose tolerance tests in a general Caucasian
Diabetes Care 22:920 –924, 1999 59. Ferrannini E, Bjorkman O, Reichard GA population: the Hoorn Study. Diabetolo-
48. Shaw JE, Hodge AM, de Courten M, Chit- Jr, Pilo A, Olsson M, Wahren J, DeFronzo gia 39:298 –305, 1996
son P, Zimmet PZ: Isolated post-challenge RA: The disposal of an oral glucose load in 74. Ko GT, Chan JC, Woo J, Lau E, Yeung VT,
hyperglycaemia confirmed as a risk factor healthy subjects: a quantitative study. Di- Chow CC, Cockram: The reproducibility
for mortality. Diabetologia 42:1050 – abetes 34:580 –588, 1985 and usefulness of the oral glucose toler-
1054, 1999 60. DeFronzo RA: Lilly Lecture 1987: the tri- ance test in screening for diabetes and
49. Gabir M, Hanson RL, Debelea D, Impera- umvirate: beta-cell, muscle, liver: a collu- other cardiovascular risk factors. Ann Clin
tore G, Rousmain J, Bennett PH, Knowler sion responsible for NIDDM. Diabetes 37: Biochem 35:62– 67, 1998
WC: Plasma glucose and prediction of mi- 667– 687, 1988 75. Burke JP, Haffner SM, Gaskill SP, Wil-
crovascular disease and mortality: evalu- 61. Weyer C, Bogardus C, Pratley RE: Meta- liams KL, Stern MP: Reversion from type 2
ation of 1997 American Diabetes bolic characteristics of individuals with diabetes to nondiabetic status: influence
Association and 1999 World Health Or- impaired fasting glucose and/or impaired of the 1997 American Diabetes Associa-
ganization criteria for diagnosis of diabe- glucose tolerance. Diabetes 48:2197– tion criteria. Diabetes Care 21:1266 –
tes. Diabetes Care 23:1113–1118, 2000 2203, 1999 1270, 1998
50. Balkau B, Forhan A, Eschwege E: Two 62. Reaven GM: Banting Lecture 1988: role of 76. Eschwege E, Charles MA, Simon D, Thib-
hour plasma glucose is not unequivocally insulin resistance in human disease. Dia- ult N, Balkau B: Reproducibility of the di-
predictive for early death in men with im- betes 37:1595–1607, 1988 agnosis of diabetes over a 30-month
paired fasting glucose: more results from 63. Haffner SM, Stern MP, Hazuda HP, Mitchell follow-up: the Paris Prospective Study.
the Paris Prospective Study. Diabetologia BD, Patterson JK: Cardiovascular risk fac- Diabetes Care 24:1941–1944, 2001
45:1224 –1230, 2002 tors in confirmed prediabetic individuals. 77. Stern MP, Williams K, Haffner SM: Iden-
51. Meigs JB, Nathan DM, D’Agostino RB Sr, Does the clock for coronary heart disease
tification of persons at high risk for type 2
Wilson PW: Fasting and postchallenge start ticking before the onset of clinical dia-
diabetes mellitus: do we need the oral glu-
glycemia and cardiovascular disease risk: betes? JAMA 263:2893–2898, 1990
cose tolerance test? Ann Intern Med 136:
the Framingham Offspring Study. Diabe- 64. Edwards KL, Austin MA, Newman B,
tes Care 25:1845–1850, 2002 Mayer E, Krauss RM, Selby JV: Multivari- 575–581, 2002
52. Stern MP, Fatehi P, Williams K, Haffner SM: ate analysis of the insulin resistance syn- 78. Ruige JB, de Neeling JN, Kostense PJ,
Predicting future cardiovascular disease: do drome in women. Arterioscler Thromb 14: Bouter LM, Heine RJ: Performance of an
we need the oral glucose tolerance test? Di- 1940 –1945, 1994 NIDDM screening questionnaire based on
abetes Care 25:1851–1856, 2002 65. Meigs JB, D’Agostino RB Sr, Wilson PW, symptoms and risk factors. Diabetes Care
53. Hunt KJ, Resendez RG, Williams K, Cupples LA, Nathan DM, Singer DE: Risk 20:491– 496, 1997
Haffner SM, Stern MP: Excess mortality variable clustering in the insulin resistance 79. Baan CA, Ruige JB, Stolk RP, Witteman
among individuals with impaired glucose syndrome: the Framingham Offspring JC, Dekker JM, Heine RJ, Feskens EJ: Per-
tolerance (IGT) is limited to those who Study. Diabetes 46:1594 –1600, 1997 formance of a predictive model to identify
develop diabetes: the San Antonio Heart 66. Gray RS, Fabsitz RR, Cowan LD, Lee ET, undiagnosed diabetes in a health care set-
Study (Abstract). Diabetes 51 (Suppl. 2): Howard BV, Savage PJ: Risk factor clus- ting. Diabetes Care 22:213–219, 1999
A229, 2002 tering in the insulin resistance syndrome: 80. Lindstrom J, Tuomilehto J: The diabetes
54. UK Prospective Diabetes Study (UKPDS) the Strong Heart Study. Am J Epidemiol risk score: a practical tool to predict type 2
Group: Intensive blood-glucose control 148:869 – 878, 1998 diabetes risk. Diabetes Care 26:725–731,
with sulphonylureas or insulin compared 67. Hanson RL, Imperatore G, Bennett PH, 2003
DIABETES CARE, VOLUME 26, NUMBER 11, NOVEMBER 2003 3167
You might also like
- 1.pharmacy Technician Study GuideDocument31 pages1.pharmacy Technician Study GuideAlan Hao93% (14)
- Pharmacology UNIT 1 - Lesson 1Document29 pagesPharmacology UNIT 1 - Lesson 1Bea Bianca CruzNo ratings yet
- Malnutrition Screening Tool (MST) : Obtain Consent To Complete This Screening by AskingDocument2 pagesMalnutrition Screening Tool (MST) : Obtain Consent To Complete This Screening by AskingAku dienaNo ratings yet
- Species Common/Other Name Pathogenesis Mot/Infective Stage Diagnostic Stage I. NematodesDocument2 pagesSpecies Common/Other Name Pathogenesis Mot/Infective Stage Diagnostic Stage I. NematodesautumntreesNo ratings yet
- Izotope Ozone 5 Help DocumentationDocument149 pagesIzotope Ozone 5 Help DocumentationJoao PessoaNo ratings yet
- Status Gizi BB U AsupanDocument5 pagesStatus Gizi BB U AsupanPavlovaNo ratings yet
- Fall 2013 PDFDocument10 pagesFall 2013 PDFlopezmegoNo ratings yet
- HP Latex 310 - 1 PDFDocument4 pagesHP Latex 310 - 1 PDFHuma NicolaeNo ratings yet
- For The Security of CitizensDocument33 pagesFor The Security of CitizensWissem DhaouadiNo ratings yet
- PC3 Drum MapDocument1 pagePC3 Drum MapTaichiaikidokaNo ratings yet
- Treadmill Repair Service PDFDocument2 pagesTreadmill Repair Service PDFSabeur ShabouNo ratings yet
- 9 SC - I-ZoologyDocument3 pages9 SC - I-ZoologyNikhil SinhaNo ratings yet
- Alter Ego + A1 - Livre de L'élève (218p) PDFDocument218 pagesAlter Ego + A1 - Livre de L'élève (218p) PDFAnderson PereiraNo ratings yet
- Oxygen Pro Mini - User Guide - V1.1Document54 pagesOxygen Pro Mini - User Guide - V1.1Joker KillNo ratings yet
- In Flames LyricsDocument4 pagesIn Flames LyricsniyammmNo ratings yet
- General Knowledge and Trivia Quiz Sheets For Teenagers With Answers (1) - February 2015Document2 pagesGeneral Knowledge and Trivia Quiz Sheets For Teenagers With Answers (1) - February 2015Annie MartinezNo ratings yet
- 8047 en 03Document84 pages8047 en 03José CarlosNo ratings yet
- 21-Day Abundance Challenge (Intro)Document1 page21-Day Abundance Challenge (Intro)FNHANo ratings yet
- CFD Analysis of Regenerator of Gifford Mcmahon Cryocooler at 2k TemperatureDocument6 pagesCFD Analysis of Regenerator of Gifford Mcmahon Cryocooler at 2k TemperatureIJIRSTNo ratings yet
- Zeiss Ikon Contaflex BookDocument24 pagesZeiss Ikon Contaflex BookAnonymous Pr8IgKeNo ratings yet
- List MAC AddressDocument2,172 pagesList MAC AddressidnetskyNo ratings yet
- AWS Certified SysOps Administrator - Associate (Retiring July 26th, 2021)Document2 pagesAWS Certified SysOps Administrator - Associate (Retiring July 26th, 2021)Franter OkNo ratings yet
- Basic Operation of Cryocoolers and Related Thermal MachinesDocument58 pagesBasic Operation of Cryocoolers and Related Thermal MachinesJoão PinaNo ratings yet
- EASN Ksma Upute HR 2008 PDFDocument64 pagesEASN Ksma Upute HR 2008 PDFregistracijusNo ratings yet
- 9914659r02 PDFDocument157 pages9914659r02 PDFCathy CadellNo ratings yet
- LinuxCBT Feat. OpenPGP Edition NotesDocument10 pagesLinuxCBT Feat. OpenPGP Edition NotesAnghel FlorinNo ratings yet
- Addictive Drums Keymap PDFDocument1 pageAddictive Drums Keymap PDFEma VidovikNo ratings yet
- Canon Ir C2570 C3100 C3170Document174 pagesCanon Ir C2570 C3100 C3170nieblaashxNo ratings yet
- DiabetesDocument8 pagesDiabetesDanielValenciaNo ratings yet
- The Revolution of The Antidiabetic Drugs in CardiologyEuropean Heart Journal SupplementDocument5 pagesThe Revolution of The Antidiabetic Drugs in CardiologyEuropean Heart Journal Supplementgabriela naranjoNo ratings yet
- Standar Medical TreatmentDocument17 pagesStandar Medical TreatmentIba SuprasabaNo ratings yet
- Ada 2 PDFDocument21 pagesAda 2 PDFdepy oktaNo ratings yet
- Sustaine 10Document10 pagesSustaine 10Ivan Dario Hernandez ErazoNo ratings yet
- GlucoseDocument5 pagesGlucosebagsouravNo ratings yet
- Adverse Effects and Safety of SGLT-2 Inhibitors: Diabetes & Metabolism December 2014Document8 pagesAdverse Effects and Safety of SGLT-2 Inhibitors: Diabetes & Metabolism December 2014Sahrul RiadiNo ratings yet
- Hba Measurement Improves The Detection of Type 2 Diabetes in High-Risk Individuals With Nondiagnostic Levels of Fasting Plasma GlucoseDocument7 pagesHba Measurement Improves The Detection of Type 2 Diabetes in High-Risk Individuals With Nondiagnostic Levels of Fasting Plasma GlucoseStone WangNo ratings yet
- VildagliptinDocument7 pagesVildagliptinwanburyNo ratings yet
- Comparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic PatientsDocument6 pagesComparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic Patientsthomas albertNo ratings yet
- Cardiovascular Outcomes StudiesDocument5 pagesCardiovascular Outcomes StudiesAnonymous LOeICSOqNo ratings yet
- Dia Care 2011 Bonora S184 90Document7 pagesDia Care 2011 Bonora S184 90castillojessNo ratings yet
- Diabetes Mellitus Postrasplante y Prediabetes en Receptores de Trasplante Renal 2021Document13 pagesDiabetes Mellitus Postrasplante y Prediabetes en Receptores de Trasplante Renal 2021Casti Garcia GomezNo ratings yet
- Clinical Study: The Effects of Glucose Fluctuation On The Severity of Coronary Artery Disease in Type 2 Diabetes MellitusDocument6 pagesClinical Study: The Effects of Glucose Fluctuation On The Severity of Coronary Artery Disease in Type 2 Diabetes MellitusEgi Dwi SatriaNo ratings yet
- Comparison of Hba1C and Ogtt For The Diagnosis of Type 2 Diabetes in Children at Risk of DiabetesDocument7 pagesComparison of Hba1C and Ogtt For The Diagnosis of Type 2 Diabetes in Children at Risk of DiabetesAnnisa FujiantiNo ratings yet
- Slide Deck RTD Pre Diabetes - FinalDocument39 pagesSlide Deck RTD Pre Diabetes - FinalVieca FauziahNo ratings yet
- SGLT2 Inhibitors: The Future For Treatment of Type 2 Diabetes Mellitus and Other Chronic DiseasesDocument6 pagesSGLT2 Inhibitors: The Future For Treatment of Type 2 Diabetes Mellitus and Other Chronic DiseasesLucian Siriteanu100% (1)
- E001279 FullDocument9 pagesE001279 FullgasiasiNo ratings yet
- Biomarkeri Diabet 2011 PDFDocument9 pagesBiomarkeri Diabet 2011 PDFKaycsa AdrianaNo ratings yet
- Management of The Patient With Heart Failure and Diabetes May Insulin Be A ProblemDocument16 pagesManagement of The Patient With Heart Failure and Diabetes May Insulin Be A ProblemGIBSON JOEL CUNYA YAHUANANo ratings yet
- Research ArticleDocument12 pagesResearch ArticleRodas GetachewNo ratings yet
- Diabetes Care Glucosa Promedio EstimadaDocument6 pagesDiabetes Care Glucosa Promedio EstimadaGemeneza GonzalesNo ratings yet
- Continuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic OutcomesDocument13 pagesContinuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic OutcomesguillermocochaNo ratings yet
- Prediabetes A High Risk State For Diabetes Development PDFDocument12 pagesPrediabetes A High Risk State For Diabetes Development PDFDario Neri CortezNo ratings yet
- Guideline ADA 2010Document51 pagesGuideline ADA 2010Rivano Frits Henry PandalekeNo ratings yet
- General Aspects of Diabetes Mellitus20160808 31394 U4lcrv With Cover Page v2Document13 pagesGeneral Aspects of Diabetes Mellitus20160808 31394 U4lcrv With Cover Page v2PanjiNo ratings yet
- CE F (AnG) PF1 (MJ AP) PFA (MJ AP) PB (MJ AP) PN (AP)Document5 pagesCE F (AnG) PF1 (MJ AP) PFA (MJ AP) PB (MJ AP) PN (AP)Nimesh ModiNo ratings yet
- Dapa CKDDocument11 pagesDapa CKDCarlos Andres Tejeda PerezNo ratings yet
- Insulin Treatment in Patients With Diabetes Mellitus and Heart Failure in The Era of New Antidiabetic MedicationsDocument13 pagesInsulin Treatment in Patients With Diabetes Mellitus and Heart Failure in The Era of New Antidiabetic MedicationsIsamar AgostoNo ratings yet
- ADO in BRCDocument10 pagesADO in BRCVlahtNo ratings yet
- J of Inher Metab Disea - 2018 - Hoogeveen - A Preliminary Study of Telemedicine For Patients With Hepatic Glycogen StorageDocument8 pagesJ of Inher Metab Disea - 2018 - Hoogeveen - A Preliminary Study of Telemedicine For Patients With Hepatic Glycogen StorageDemetrius LacetNo ratings yet
- International Federation Diabetes 1 Hora Hiperglicemia IntermediaDocument21 pagesInternational Federation Diabetes 1 Hora Hiperglicemia IntermediaMundo Mariano Venezuela.No ratings yet
- Pathophysiology of Prediabetes and Treatment Implications For The Prevention of Type 2 Diabetes MellitusDocument10 pagesPathophysiology of Prediabetes and Treatment Implications For The Prevention of Type 2 Diabetes MellitusSamir BenmouffokNo ratings yet
- New Combination Treatments in The Management of Diabetes: Focus On Sitagliptin - MetforminDocument10 pagesNew Combination Treatments in The Management of Diabetes: Focus On Sitagliptin - MetforminGd PadmawijayaNo ratings yet
- Euglycemic Diabetic Ketoacidosis: A Predictable, Detectable, and Preventable Safety Concern With SGLT2 InhibitorsDocument5 pagesEuglycemic Diabetic Ketoacidosis: A Predictable, Detectable, and Preventable Safety Concern With SGLT2 InhibitorsPierreNo ratings yet
- E002619 FullDocument9 pagesE002619 FullUsee TvNo ratings yet
- Rose Pinwheel Potholder: Home Printer-Friendly PDF Printer-Friendly PDFDocument3 pagesRose Pinwheel Potholder: Home Printer-Friendly PDF Printer-Friendly PDFPriscilla ArtesNo ratings yet
- Cesta de Revista em CoraçãoDocument4 pagesCesta de Revista em CoraçãoPriscilla ArtesNo ratings yet
- WEB L SNC BouquetBasketsDocument2 pagesWEB L SNC BouquetBasketsPriscilla ArtesNo ratings yet
- Coats & Clark - 016 - Rose Rhapsody (C)Document4 pagesCoats & Clark - 016 - Rose Rhapsody (C)Priscilla ArtesNo ratings yet
- Coats & Clark - 09 - Crinoline Lady in CrochetDocument15 pagesCoats & Clark - 09 - Crinoline Lady in CrochetPriscilla ArtesNo ratings yet
- "Home Style Life Style Your Style.": P.O. Box 40 Listowel ON N4W 3H3Document1 page"Home Style Life Style Your Style.": P.O. Box 40 Listowel ON N4W 3H3Priscilla ArtesNo ratings yet
- Pastel Jute Baskets PDFDocument2 pagesPastel Jute Baskets PDFPriscilla ArtesNo ratings yet
- What Is It?: National Customer Service WeekDocument1 pageWhat Is It?: National Customer Service WeekPriscilla ArtesNo ratings yet
- Project: A Mother's Blessing: American Patchwork & Quilting - Quilt Sampler - Quilts and MoreDocument5 pagesProject: A Mother's Blessing: American Patchwork & Quilting - Quilt Sampler - Quilts and MorePriscilla ArtesNo ratings yet
- 213s-24 Flower Pot CozyDocument6 pages213s-24 Flower Pot CozyPriscilla ArtesNo ratings yet
- Daftar Pustaka: Affect Disord. 2003 73 (1-2) :123-31Document2 pagesDaftar Pustaka: Affect Disord. 2003 73 (1-2) :123-31Jumria Tandi PanggaloNo ratings yet
- Hypertensive Urgency: University of Perpetual Help System DALTA - Las PiñasDocument8 pagesHypertensive Urgency: University of Perpetual Help System DALTA - Las PiñasJustin HericoNo ratings yet
- ADRnewReporting Form 1.4Document2 pagesADRnewReporting Form 1.4Sourabh kundara50% (2)
- Spectrum - Bone Densitometry WOrkshopDocument16 pagesSpectrum - Bone Densitometry WOrkshopanbufelix1939No ratings yet
- Tugas Individu B.inggris (Midwifery Care)Document11 pagesTugas Individu B.inggris (Midwifery Care)irmanurulNo ratings yet
- Laporan Home Visit (Revin)Document24 pagesLaporan Home Visit (Revin)marinNo ratings yet
- CATS Clinical Guidelines Upper Airway Obstruction (UAO) : 1 AssessmentDocument4 pagesCATS Clinical Guidelines Upper Airway Obstruction (UAO) : 1 AssessmentJohn DoeNo ratings yet
- Links To Books and Additional MaterialDocument2 pagesLinks To Books and Additional MaterialCarl FernandesNo ratings yet
- Jurnal Hospitalisasi Pada AnakDocument9 pagesJurnal Hospitalisasi Pada Anaktrio hidayatNo ratings yet
- Screenshot 2021-11-20 at 7.28.44 AMDocument134 pagesScreenshot 2021-11-20 at 7.28.44 AMhhashemNo ratings yet
- Restrictions in Use and Availability of PharmaceuticalsDocument328 pagesRestrictions in Use and Availability of PharmaceuticalsinfooncoNo ratings yet
- ObjectiveDocument2 pagesObjectiveMarvinNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument16 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaYadnya SaputraNo ratings yet
- Pregnancy and TBDocument24 pagesPregnancy and TBRoza MaulindraNo ratings yet
- Resume of Shirlene - R - SpatcherDocument1 pageResume of Shirlene - R - Spatcherapi-30461417No ratings yet
- New Jersey Health Department Report RE: Dr. John VecchioneDocument11 pagesNew Jersey Health Department Report RE: Dr. John VecchioneNews12NJWebNo ratings yet
- MBEB - Mindfulness-Based Emotional Balance Teacher Training IntensiveDocument10 pagesMBEB - Mindfulness-Based Emotional Balance Teacher Training IntensiveLina SantosNo ratings yet
- Loi - de Beer and THCDocument4 pagesLoi - de Beer and THCRyan TerblancheNo ratings yet
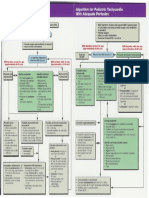
- Pediatric Tachycardia AlgorithmsDocument1 pagePediatric Tachycardia AlgorithmsGalih FatoniNo ratings yet
- Skull FractureDocument13 pagesSkull FractureEddie LimNo ratings yet
- Quiz Section: Level 1Document4 pagesQuiz Section: Level 1AinunZamiraNo ratings yet
- DR Prathap C ReddyDocument4 pagesDR Prathap C ReddyShakin ShaNo ratings yet
- Psych Unit I Part 1Document42 pagesPsych Unit I Part 1api-293070066No ratings yet
- Dowsing Resources & Techniques Joe Smith Diagnosing TechniqueDocument6 pagesDowsing Resources & Techniques Joe Smith Diagnosing TechniqueDina LazarosNo ratings yet
- Capítulo 10 SerdevDocument19 pagesCapítulo 10 SerdevErik BrooksNo ratings yet
- CSS Osteoarthritis GenuDocument33 pagesCSS Osteoarthritis Genufatimah putriNo ratings yet