Professional Documents
Culture Documents
Anaesthesiology, University of Regensburg, Regensburg, Germany
Anaesthesiology, University of Regensburg, Regensburg, Germany
Uploaded by
debby claudiCopyright:
Available Formats
You might also like
- Pharmacotherapeutics in ObstetricsDocument14 pagesPharmacotherapeutics in ObstetricsmercyNo ratings yet
- MBR 2019 - Anes ENT Ophtha HandoutsDocument17 pagesMBR 2019 - Anes ENT Ophtha HandoutsNica Lopez FernandezNo ratings yet
- Morkisch 2019Document15 pagesMorkisch 2019David Morote VillaNo ratings yet
- Baloxavir Marboxil - A Retrospective Study (Poster)Document2 pagesBaloxavir Marboxil - A Retrospective Study (Poster)Arun NachiappanNo ratings yet
- The Effect of Different Doses of Intrathecal Dexmedetomidine On Spinal Anesthesia A Meta AnalysisDocument8 pagesThe Effect of Different Doses of Intrathecal Dexmedetomidine On Spinal Anesthesia A Meta AnalysisAndhika DNo ratings yet
- Guerreiro (2013) Evidence-Based Rehabilitation After Acquired Brain InjuryDocument3 pagesGuerreiro (2013) Evidence-Based Rehabilitation After Acquired Brain Injuryhoranvera10No ratings yet
- Laser and TMJDocument5 pagesLaser and TMJMohamed FaizalNo ratings yet
- Long Term Outcome OCDDocument3 pagesLong Term Outcome OCDTSNo ratings yet
- Craniomandibular Index-ValidityDocument7 pagesCraniomandibular Index-ValidityVALESKA FARIÑA ESPINOSANo ratings yet
- Auricular Acupuncture at The Shenmen'' and Point Zero'' Points Induced Parasympathetic ActivationDocument5 pagesAuricular Acupuncture at The Shenmen'' and Point Zero'' Points Induced Parasympathetic Activationraspino1959No ratings yet
- Ji-Hua Xu 2018Document3 pagesJi-Hua Xu 2018Mary FallNo ratings yet
- Paresia Cevera Del Brazon Despues de Un Accidente Erebrovascular BOBATH PDFDocument12 pagesParesia Cevera Del Brazon Despues de Un Accidente Erebrovascular BOBATH PDFLuisa FernandaNo ratings yet
- Matsuoka2013 - Neural Correlates of The Components of The Clock Drawing TestDocument7 pagesMatsuoka2013 - Neural Correlates of The Components of The Clock Drawing TestErick SolisNo ratings yet
- A Comprehensive Approach of Manual Therapy and Exercise in LateralDocument1 pageA Comprehensive Approach of Manual Therapy and Exercise in Lateralapi-26919768No ratings yet
- Internal Dosimetry As A Tool For Radiation Protection of The Patient in Nuclear MedicineDocument11 pagesInternal Dosimetry As A Tool For Radiation Protection of The Patient in Nuclear MedicinesantoshaiimsNo ratings yet
- Practical Guidance in Echocardiographic Assessment of Global Longitudinal StrainDocument4 pagesPractical Guidance in Echocardiographic Assessment of Global Longitudinal StrainMathew McCarthyNo ratings yet
- Jurnal Saraf 1Document7 pagesJurnal Saraf 1Rifqi arinaNo ratings yet
- Additional Records IdentifiedDocument1 pageAdditional Records IdentifiedSebastian VanegasNo ratings yet
- Neuromudalação ECTDocument13 pagesNeuromudalação ECTCamila BeloNo ratings yet
- Original Article Effect of Acupuncture at Zulinqi gb41 On The Amplitude of Low Frequency Fluctuations in Migraine Without AuraDocument12 pagesOriginal Article Effect of Acupuncture at Zulinqi gb41 On The Amplitude of Low Frequency Fluctuations in Migraine Without AuraYoshua ViventiusNo ratings yet
- Analgesia and Sedation in Patients With ARDDocument15 pagesAnalgesia and Sedation in Patients With ARDsamuelNo ratings yet
- Parent ArticleDocument6 pagesParent ArticleUzra ShujaatNo ratings yet
- Christie 2019Document3 pagesChristie 2019yesakula30No ratings yet
- 1 s2.0 S1935861X19304280 MainDocument8 pages1 s2.0 S1935861X19304280 Mainjem bistreNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument50 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Journal 2Document5 pagesJournal 2nandhini raguNo ratings yet
- The WOMAC Score Can Be Reliably Used To Classify Patient Satisfaction After Total Knee ArthroplastyDocument9 pagesThe WOMAC Score Can Be Reliably Used To Classify Patient Satisfaction After Total Knee ArthroplastyIkmal ShahromNo ratings yet
- Effectiveness of Wii-Based Rehabilitation in Stroke: A Randomized Controlled StudyDocument7 pagesEffectiveness of Wii-Based Rehabilitation in Stroke: A Randomized Controlled StudyAfnes AstrianiNo ratings yet
- 999 EMSRFMEWSposterfinalDocument1 page999 EMSRFMEWSposterfinalzummyrightNo ratings yet
- JAC 11th Physics Syllabus 2023-24Document10 pagesJAC 11th Physics Syllabus 2023-24evil18ytNo ratings yet
- 10 3233@BMR-181135Document9 pages10 3233@BMR-181135Ayu SuprabawatiNo ratings yet
- Semiextended Intramedullary Nailing of The Tibia.6Document11 pagesSemiextended Intramedullary Nailing of The Tibia.6Guna NikhilNo ratings yet
- MJMR - Volume 31 - Issue 3 - Pages 236-239Document4 pagesMJMR - Volume 31 - Issue 3 - Pages 236-239Julio AltamiranoNo ratings yet
- PIIS1935861X21002229Document3 pagesPIIS1935861X21002229Liliane TelesNo ratings yet
- Anestesi Jurnal 3Document13 pagesAnestesi Jurnal 3dewi rahmanNo ratings yet
- Median Nerve Injury RT WDocument7 pagesMedian Nerve Injury RT WMirza IKFR9No ratings yet
- Prognostic Clinical and Radiological Parameters For Immediate Facial Nerve Function Following Vestibular Schwannomas SurgeryDocument7 pagesPrognostic Clinical and Radiological Parameters For Immediate Facial Nerve Function Following Vestibular Schwannomas SurgerySa'Deu FondjoNo ratings yet
- Cannabinoids in Multiple Sclerosis A Neurophysiological AnalysisDocument7 pagesCannabinoids in Multiple Sclerosis A Neurophysiological AnalysisAngel Fernando Santamaria MoralesNo ratings yet
- 09042020212858practical Statistical Methods 2019-20Document91 pages09042020212858practical Statistical Methods 2019-20Esrael KanbataNo ratings yet
- Uncertainty-Based Sampling Plans For Various Statistical DistributionsDocument14 pagesUncertainty-Based Sampling Plans For Various Statistical DistributionsScience DirectNo ratings yet
- SmallestdetectablechangeDocument4 pagesSmallestdetectablechangeBimo AnggoroNo ratings yet
- Lateral Epicondylitis: A Novel Non-Invasive Treatment ApproachDocument4 pagesLateral Epicondylitis: A Novel Non-Invasive Treatment ApproachAnonymous KpdjCwXG9TNo ratings yet
- Franca 2020 AtaxiaDocument6 pagesFranca 2020 AtaxiainervavsNo ratings yet
- Delatorrecanales 2019Document11 pagesDelatorrecanales 2019ELIAS DAVID NOBMAN ALVARADONo ratings yet
- Manejo de Dolor Facial Con RTMSDocument14 pagesManejo de Dolor Facial Con RTMSenviosmentalmedNo ratings yet
- The Use of Auricular Acupuncture To Reduce.24Document3 pagesThe Use of Auricular Acupuncture To Reduce.24Vi PhanNo ratings yet
- Bariatric Surgery and Brain HealthDocument20 pagesBariatric Surgery and Brain HealthAnna MudzNo ratings yet
- Reduction in Spasticity in Stroke Patient With Paraffin TherapyDocument10 pagesReduction in Spasticity in Stroke Patient With Paraffin TherapyayuNo ratings yet
- ActaNeuro AKNFacialDocument8 pagesActaNeuro AKNFacialTimothy CaldwellNo ratings yet
- Prognostic TestsDocument3 pagesPrognostic TestsHANS BENNo ratings yet
- 100205HM-SB CRA Poster Final 3Document1 page100205HM-SB CRA Poster Final 3Osama MariaNo ratings yet
- Ketamina y Dexmedetomidina en QuemadosDocument6 pagesKetamina y Dexmedetomidina en QuemadosVicky CascorNo ratings yet
- Internet-Supported Physical Exercise Training For Persons With Multiple Sclerosis-A Randomised, Controlled StudyDocument11 pagesInternet-Supported Physical Exercise Training For Persons With Multiple Sclerosis-A Randomised, Controlled StudyPoring CarnavasNo ratings yet
- HM 1Document6 pagesHM 1annisanadyapNo ratings yet
- Cai Et Al, 2021Document13 pagesCai Et Al, 2021Bruno KudekenNo ratings yet
- Assessing The Reliability and Responsiveness of 5 Shoulder QuestionnairesDocument8 pagesAssessing The Reliability and Responsiveness of 5 Shoulder QuestionnairesJanaiana UchoaNo ratings yet
- Analisis Jurnal PICO ENGLISHDocument2 pagesAnalisis Jurnal PICO ENGLISHSellyRestyPratamaNo ratings yet
- The Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryDocument4 pagesThe Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryInternational Organization of Scientific Research (IOSR)No ratings yet
- Of Of: Effect Proprioceptive Neuromuscular Facilitation On The Patients With Hemiplegia Long and Short DurationDocument8 pagesOf Of: Effect Proprioceptive Neuromuscular Facilitation On The Patients With Hemiplegia Long and Short DurationsridharNo ratings yet
- The Hemiplegic After Stroke: And: MeasurementDocument4 pagesThe Hemiplegic After Stroke: And: MeasurementAmi MarcuNo ratings yet
- IFCC 2007 Stornaiuolo Architect HBsAgDocument2 pagesIFCC 2007 Stornaiuolo Architect HBsAgFouad RahiouyNo ratings yet
- Neuroscientific based therapy of dysfunctional cognitive overgeneralizations caused by stimulus overload with an "emotionSync" methodFrom EverandNeuroscientific based therapy of dysfunctional cognitive overgeneralizations caused by stimulus overload with an "emotionSync" methodNo ratings yet
- The Pain, Agitation, and Delirium Practice Guidelines For Adult Critically Ill Patients: A Post-Publication PerspectiveDocument9 pagesThe Pain, Agitation, and Delirium Practice Guidelines For Adult Critically Ill Patients: A Post-Publication Perspectivedebby claudiNo ratings yet
- Raval PDFDocument5 pagesRaval PDFdebby claudiNo ratings yet
- Spinal Epidural Synovial Sarcoma A Case of Homogen PDFDocument5 pagesSpinal Epidural Synovial Sarcoma A Case of Homogen PDFdebby claudiNo ratings yet
- ArnoldDocument5 pagesArnolddebby claudiNo ratings yet
- Urn - Isbn - 978-952-61-1781-2Document92 pagesUrn - Isbn - 978-952-61-1781-2debby claudiNo ratings yet
- Demir 2015Document2 pagesDemir 2015debby claudiNo ratings yet
- NIH Public Access: Etiology and Treatment of Hypogonadism in AdolescentsDocument22 pagesNIH Public Access: Etiology and Treatment of Hypogonadism in Adolescentsdebby claudiNo ratings yet
- Management of Pain in The Intensive Care UnitDocument6 pagesManagement of Pain in The Intensive Care Unitdebby claudiNo ratings yet
- Best SoapDocument8 pagesBest Soapdebby claudiNo ratings yet
- Bestsoap PDFDocument1 pageBestsoap PDFdebby claudiNo ratings yet
- Common Sense Talk About Antibacterial ProductsDocument2 pagesCommon Sense Talk About Antibacterial Productsdebby claudiNo ratings yet
- 4.original SharifahDocument9 pages4.original Sharifahdebby claudiNo ratings yet
- NEL243403R03 Karasek Lewinski WRDocument6 pagesNEL243403R03 Karasek Lewinski WRdebby claudiNo ratings yet
- Musa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim NasseriDocument6 pagesMusa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim Nasseridebby claudiNo ratings yet
- Jovin2017 PDFDocument12 pagesJovin2017 PDFdebby claudiNo ratings yet
- Liquid Versus Gel Handrub Formulation: A Prospective Intervention StudyDocument8 pagesLiquid Versus Gel Handrub Formulation: A Prospective Intervention Studydebby claudiNo ratings yet
- 2014 Article 3830Document8 pages2014 Article 3830debby claudiNo ratings yet
- A 12-Week, Randomized, Controlled Trial With A 4-Week Randomized Withdrawal Period To Evaluate The Effi Cacy and Safety of Linaclotide in Irritable Bowel Syndrome With ConstipationDocument11 pagesA 12-Week, Randomized, Controlled Trial With A 4-Week Randomized Withdrawal Period To Evaluate The Effi Cacy and Safety of Linaclotide in Irritable Bowel Syndrome With Constipationdebby claudiNo ratings yet
- Coffee and Herbal Tea Consumption Is Associated With Lower Liver Stiffness in The General Population: The Rotterdam StudyDocument10 pagesCoffee and Herbal Tea Consumption Is Associated With Lower Liver Stiffness in The General Population: The Rotterdam Studydebby claudiNo ratings yet
- Ese 125 Dihydroxyvitamin D 3 Ante Rev.12.15 Low 1Document6 pagesEse 125 Dihydroxyvitamin D 3 Ante Rev.12.15 Low 1debby claudiNo ratings yet
- Vitamin D and Thyroid Diseases: Institute of Endocrinology, Prague, Czech RepublicDocument6 pagesVitamin D and Thyroid Diseases: Institute of Endocrinology, Prague, Czech Republicdebby claudiNo ratings yet
- 1 s2.0 S0002961011000638 Main PDFDocument7 pages1 s2.0 S0002961011000638 Main PDFdebby claudiNo ratings yet
- Nutrients: Vitamin D and Graves' Disease: A Meta-Analysis UpdateDocument15 pagesNutrients: Vitamin D and Graves' Disease: A Meta-Analysis Updatedebby claudiNo ratings yet
- Dolor PosduralDocument39 pagesDolor PosduralMarlen ValdesNo ratings yet
- Placenta PreviaDocument54 pagesPlacenta PreviabobtagubaNo ratings yet
- Regional Anesthesia For CsDocument29 pagesRegional Anesthesia For CsMohmed El KingNo ratings yet
- National List of Essential Medicines Nepal 2021Document72 pagesNational List of Essential Medicines Nepal 2021Sugandhi SahNo ratings yet
- Posicion de Vallejo en Acceso Neuroaxial DificilDocument7 pagesPosicion de Vallejo en Acceso Neuroaxial Dificiljuajimenez55No ratings yet
- Vaginal Hysterectomy CASE STUDYDocument18 pagesVaginal Hysterectomy CASE STUDYJeannie RobisNo ratings yet
- Persistent Paralysis After Spinal Paresthesia PDFDocument6 pagesPersistent Paralysis After Spinal Paresthesia PDFNadia Gina AnggrainiNo ratings yet
- Local AnaesthesiaDocument33 pagesLocal AnaesthesiatesfahuntekleNo ratings yet
- Transes - Perioperative NursingDocument10 pagesTranses - Perioperative NursingJAMES ANDRE RENDONNo ratings yet
- Medical ThesiasDocument360 pagesMedical ThesiasJessica CNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- National List of Essential Medicines: Medicines Route of Administration, Dosage Forms and Strengths Level of UseDocument51 pagesNational List of Essential Medicines: Medicines Route of Administration, Dosage Forms and Strengths Level of UseportosinNo ratings yet
- Test DoseDocument4 pagesTest DoseibunqumairaNo ratings yet
- Case - ViedyaDocument40 pagesCase - ViedyaRaka WibisonoNo ratings yet
- Final NLEM 2016 PDFDocument37 pagesFinal NLEM 2016 PDFBipashwi Nath UpretyNo ratings yet
- List of Dissertations (Subjectwise)Document458 pagesList of Dissertations (Subjectwise)Mayursinh SolankiNo ratings yet
- Anaesthesia - 2022 - Plaat - Prevention and Management of Intra Operative Pain During Caesarean Section Under NeuraxialDocument10 pagesAnaesthesia - 2022 - Plaat - Prevention and Management of Intra Operative Pain During Caesarean Section Under NeuraxialCedric VaillesNo ratings yet
- (OB) 2B - Obstetrical Anesthesia (By Dr. Bretta Lucion)Document3 pages(OB) 2B - Obstetrical Anesthesia (By Dr. Bretta Lucion)CleoGomezNo ratings yet
- Akukwata SeminarDocument22 pagesAkukwata SeminarjenniferNo ratings yet
- Local/Regional/Spinal Anaesthesia: DefinitionDocument4 pagesLocal/Regional/Spinal Anaesthesia: DefinitionThistell ThistleNo ratings yet
- Spinal & Epidural AnaesthesiaDocument31 pagesSpinal & Epidural AnaesthesiaKumar Gavali Suryanarayana0% (1)
- Anestesi EpiduralDocument2 pagesAnestesi EpiduralShazean ShahNo ratings yet
- AnaesthesiaDocument3 pagesAnaesthesiaJoan nakijjobaNo ratings yet
- PG Dissertation Topics-2020Document129 pagesPG Dissertation Topics-2020Jaggu MamidiNo ratings yet
- Perioperative Pre-Class Mini-Lecture - CH 17-19Document22 pagesPerioperative Pre-Class Mini-Lecture - CH 17-19Marcel YoungNo ratings yet
- Local and Regional AnesthesiaDocument78 pagesLocal and Regional AnesthesiaPatricia Feliani Sitohang100% (4)
- Spinal Anesthesia - Technique - UpToDateDocument37 pagesSpinal Anesthesia - Technique - UpToDateSamir Perez CasadiegoNo ratings yet
Anaesthesiology, University of Regensburg, Regensburg, Germany
Anaesthesiology, University of Regensburg, Regensburg, Germany
Uploaded by
debby claudiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anaesthesiology, University of Regensburg, Regensburg, Germany
Anaesthesiology, University of Regensburg, Regensburg, Germany
Uploaded by
debby claudiCopyright:
Available Formats
Local and regional anaesthesia 119
anesthetic had been completed, patients were placed in prone position quickly. mage scale time to achieve level I, duration of analgesia and adverse effects
The characteristics of sensory and motor block, haemodynamic data, advers (AE) was done.
effects, patient and surgeon satisfaction were recorded. The sample size was Results and Discussion: Patients data are shown in the table 1.
calculated to provide 80% power to detect a 25% reduction in the incidence of
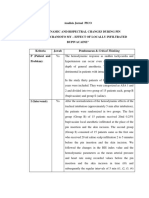
complete motor block in Group L compared with Group B. Descriptives were Table 1. Patients data by group (Median [25-75 percentages])
quoted as mean±SD, median (range), number (incidence) as appropriate. Sta- Group A Group B
tistical analyses were performed using Student’s t, Mann-Whitney U, Fischer’s (N=46) (N=14)
exact and Chi-Square tests.
VAS at positioning for spinal 3 [2-3] 0,5 [0-1]*
Results and Discussion: There were no significant differences between the Time to perform spinal anesthesia 3 [2-4] 3 [3-4]
two groups for patient demografic data, duration of operation, patient-surgeon Patient acceptance (yes/no) 35/11 14/0*
satisfaction, haemodynamic and side effects. The onset time, highest level, two Bupivacaine dose (mg) 17,5 [12,5-20] 17,5 [17,5-20]
segment regression, time to S2 regression of sensory block weren’t different in Onset of sensory block (min) 10 [9-10] 10 [9-10]
two groups (p=0.077, 0.057, 0.091 and 0.084 respectively). The incidence of Anesthesia level T4 – S5 T4 – S5
complete motor blok was 16% and 8% in Group B at the beginning and the Bromage scale time to achieve 12 [12-13] 12 [11-12,5]
end of the operation. There was not complete motor block in Group L (p=0.110 Duration of analgesia (min) 250 [240-260] 255 [240-260]
Downloaded from https://journals.lww.com/ejanaesthesiology by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3XLe684GKHSWSPs4K0vGEr9ueiboLKHEKN41Be1sFAYHofL76Si0a1g== on 10/07/2018
Number of patients with clinically significant adverse effects 5 2
and 0.490 respectively).
Conclusion(s): We concluded that both regimes are effective and safe in spinal *p<0,05.
anaesthesia for pilonidal cyst-sinus operations in prone position.
References: Both the groups showed rapid onset, excellent analgesia and good quality mo-
1 Løvstad RZ. Acta Anaesthesiol Scand 2000; 44: 48–52. tor block. There were no significant differences in clinical effects after performing
SA in StP and SpP and number of clinically significant AE. Group B showed a
significantly less incidence of pain during LP and this position was more ac-
8AP6-2 ceptable for patients in compared to group A. Using SpP for LP decreases risk
Urinary retention after spinal anaesthesia: Unilateral vs. removal of loose fragments in patients with unstable fractures. SpP can be also
bilateral spinal anaesthesia with 0.5% bupivacain. use to performing SA in patients with pelvis fractures wich can’t be placed in
A prospective randomized study sitting or lateral position.
Conclusion(s): Spinal anesthesia performed in supine position in selected pa-
R. Ehrenberg, P. Lemberger, C. Wiesenack
tients is more advantageous than performed in sitting position in patients with
Anaesthesiology, University of Regensburg, Regensburg, Germany unstable Femoral Fractures.
Background and Goal of Study: Urinary retention is one of the most com-
mon complications next to haemodynamic effects following spinal anaesthesia.
The aim of this prospective randomized study was to compare the time to first 8AP6-4
voiding and the incidence of urinary retention after two different techniques of
Does unilateral hypobaric spinal anaesthesia (U.h.S.A.)
spinal anaesthesia.
prevents from post-operative urinary retention in case of
Materials and Methods: 251 patients (ASA I-III) were randomly allocated in 2
using intrathecal morphine?
groups to receive either hyperbaric for unilateral (Group 1) or isobaric bupiva-
caine for bilateral (Group 2)spinal anaesthesia. Bladder volume was measured D. Asselineau
perioperative via ultrasound. Sensory and motor block was assessed by loss of Anaesthesiology, Clinique du Colombier, Limoges, France
cold sensation and modified Bromage scale. Time from spinal injection to first Background and Goal of Study: Post-Operative Urinary Retention incidence
voiding and necessity to catheterisation was recorded. is reported between 7% & 52%. With age, sex, post-operative morphine titra-
Results and Discussion: There were no differences between the two groups tion, large infusion volumes, & long-lasting surgery, Spinal Anaesthesia is a main
regarding demographic data. Postoperative measurements of bladder volume risk factor [2], with incidence around 25%, & more if intrathecal morphine is
were similar in both groups: Group 1: 282ml ±159; Group 2: 282ml±154). used. In such a case, we want to know if Unilateral hypobaric Spinal Anaesthesia
Unilateral block was recorded in 87% patients. Sensory level on the operated (U.h.S.A.) may lead to fewer Post-Operative Bladder Catheterization (P.O.B.C.).
side was Th 8 in both groups. Time of first voiding after injection required Materials and Methods: From Oct.06 to Oct.07, 120 patients with short
273±61minutes in group 1 and 329±73 minutes in group 2. All patients in (<90’) lower limb surgery, were randomized in 2 groups, after informed con-
group 1 were able to void spontaneously and 16 Patients (12%) need catheter- sent: Group 1: 60 patients had U.h.S.A.with hypobaric L-bupivacaine 2mg/ml.
ization in group 2. This study demonstrated no significant influence of risk fac- Group 2: 60 patients had U.h.S.A.with hypobaric L-bupivacaine 2mg/ml & in-
tors for urinary retention (e. g. age, sex, dosage of local anaesthetics). Solely trathecal morphine. We used a same protocol in both groups: 25G Whitacre
the technique of unilateral spinal aneasthesia reduced the incidence of urinary needle, no preloading infusion, ephedrine delivered if !SAP &/or !H.R. was
retention. >-20%. No postoperative morphine P.C.A. Items noticed were: Age, Sex, ASA
Conclusion(s): Our findings suggest that unilateral spinal anaesthesia reduces score, L-bupivacaine dose, ephedrine doses & peri-operative infusion volume
the incidence of disturbances of micturation and time of first voiding and. Firm required, spontaneous urination or bladder catheterization.
haemodynamic circumstances cause also significant earlier meet criteria for dis- Results and Discussion: Both groups had same characteristics for sex,
charge home compared to bilateral spinal anaesthesia. age, ASA score, L-bupivacaine dose, & surgery. No differences were found
in ephedrine consumption & in infusion volume required. Unilateral Spinal
Anaesthesia provides better early post-operative comfort & less haemodynamic
8AP6-3 changes than conventional spinal anaesthesia [1,3]. This is confirmed here, by
Performing a spinal anesthesia in the supine position in low doses of ephedrine and low volumes of peri-operative infusion required.
patients with unstable femoral fractures
I. Kuchyn, F. Glumcher Male Female Age L-bupivacaine Ephedrine Infusion vol. P.O.B.C.
Anesthesiology and Intensive Therapy, National Medical University, Kyiv,
Group 1 31 29 59,13 8,487mg 0,824mg 167,5ml 0
Ukraine Standard deviation 16,13 1,395 3,845 187,27
Background and Goal of Study: Surgical operation on account of femoral Group 2 28 32 62,55 8,762mg 3,35mg 268,33ml 8 (=13,33%)
fractures can be successfully done with using spinal anesthesia (SA) but un- Standard deviation 14,35 1,208 6,286 244,42
stable fractures makes difficult and dangerous moving the patients in sitting χ2 & t Student N.S. N.S. N.S. N.S. N.S. N.S. χ2 =8,57
(t=2,66) (t=2,54) p<0,01
or lateral position. Use the Orthopedic Navigation Table permits performing a
spinal SA in supine position (SpP). This study is designed to compare the clini-
cal effects of SA performed in SpP versus Sitting Position (StP). P.O.B.C. incidence is among lowest levels reported (no P.O.B.C.in the “mor-
Materials and Methods: 60 ASA physical status I-III patients, scheduled for phineless group”). But, as in conventional spinal anaesthesia, P.O.B.C. inci-
surgery account of femoral fractures were allocated into two equable groups. dence was significantly higher (p< 0,01) in the “morphineless group”, with inci-
SA in patients of group A (N=46) was performed in StP. SA in patients of group dence reaching 13% of patients.
B (N=14) was performed in SpP on the Orthopedic Navigation Table. All pa- Conclusion(s): U.h.S.A doesn’t protect from P.O.B.C.when intrathecal mor-
tients received 10-20 mg of 0.5% plain bupivacaine through a 23 gauge spinal phine is used.
needle at L3-L4 level. The VAS at positioning for lumbar puncture (LP), time to References:
perform SA and patient acceptance were observed. To investigate the clinical 1 Low-dose hyperbaric bupivacaine for unilateral spinal anaesthesia: Casati A, Can J
effects of SA the analysis of onset of sensory block, level of anesthesia, Bro- Anaesth 1998.
You might also like
- Pharmacotherapeutics in ObstetricsDocument14 pagesPharmacotherapeutics in ObstetricsmercyNo ratings yet
- MBR 2019 - Anes ENT Ophtha HandoutsDocument17 pagesMBR 2019 - Anes ENT Ophtha HandoutsNica Lopez FernandezNo ratings yet
- Morkisch 2019Document15 pagesMorkisch 2019David Morote VillaNo ratings yet
- Baloxavir Marboxil - A Retrospective Study (Poster)Document2 pagesBaloxavir Marboxil - A Retrospective Study (Poster)Arun NachiappanNo ratings yet
- The Effect of Different Doses of Intrathecal Dexmedetomidine On Spinal Anesthesia A Meta AnalysisDocument8 pagesThe Effect of Different Doses of Intrathecal Dexmedetomidine On Spinal Anesthesia A Meta AnalysisAndhika DNo ratings yet
- Guerreiro (2013) Evidence-Based Rehabilitation After Acquired Brain InjuryDocument3 pagesGuerreiro (2013) Evidence-Based Rehabilitation After Acquired Brain Injuryhoranvera10No ratings yet
- Laser and TMJDocument5 pagesLaser and TMJMohamed FaizalNo ratings yet
- Long Term Outcome OCDDocument3 pagesLong Term Outcome OCDTSNo ratings yet
- Craniomandibular Index-ValidityDocument7 pagesCraniomandibular Index-ValidityVALESKA FARIÑA ESPINOSANo ratings yet
- Auricular Acupuncture at The Shenmen'' and Point Zero'' Points Induced Parasympathetic ActivationDocument5 pagesAuricular Acupuncture at The Shenmen'' and Point Zero'' Points Induced Parasympathetic Activationraspino1959No ratings yet
- Ji-Hua Xu 2018Document3 pagesJi-Hua Xu 2018Mary FallNo ratings yet
- Paresia Cevera Del Brazon Despues de Un Accidente Erebrovascular BOBATH PDFDocument12 pagesParesia Cevera Del Brazon Despues de Un Accidente Erebrovascular BOBATH PDFLuisa FernandaNo ratings yet
- Matsuoka2013 - Neural Correlates of The Components of The Clock Drawing TestDocument7 pagesMatsuoka2013 - Neural Correlates of The Components of The Clock Drawing TestErick SolisNo ratings yet
- A Comprehensive Approach of Manual Therapy and Exercise in LateralDocument1 pageA Comprehensive Approach of Manual Therapy and Exercise in Lateralapi-26919768No ratings yet
- Internal Dosimetry As A Tool For Radiation Protection of The Patient in Nuclear MedicineDocument11 pagesInternal Dosimetry As A Tool For Radiation Protection of The Patient in Nuclear MedicinesantoshaiimsNo ratings yet
- Practical Guidance in Echocardiographic Assessment of Global Longitudinal StrainDocument4 pagesPractical Guidance in Echocardiographic Assessment of Global Longitudinal StrainMathew McCarthyNo ratings yet
- Jurnal Saraf 1Document7 pagesJurnal Saraf 1Rifqi arinaNo ratings yet
- Additional Records IdentifiedDocument1 pageAdditional Records IdentifiedSebastian VanegasNo ratings yet
- Neuromudalação ECTDocument13 pagesNeuromudalação ECTCamila BeloNo ratings yet
- Original Article Effect of Acupuncture at Zulinqi gb41 On The Amplitude of Low Frequency Fluctuations in Migraine Without AuraDocument12 pagesOriginal Article Effect of Acupuncture at Zulinqi gb41 On The Amplitude of Low Frequency Fluctuations in Migraine Without AuraYoshua ViventiusNo ratings yet
- Analgesia and Sedation in Patients With ARDDocument15 pagesAnalgesia and Sedation in Patients With ARDsamuelNo ratings yet
- Parent ArticleDocument6 pagesParent ArticleUzra ShujaatNo ratings yet
- Christie 2019Document3 pagesChristie 2019yesakula30No ratings yet
- 1 s2.0 S1935861X19304280 MainDocument8 pages1 s2.0 S1935861X19304280 Mainjem bistreNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument50 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Journal 2Document5 pagesJournal 2nandhini raguNo ratings yet
- The WOMAC Score Can Be Reliably Used To Classify Patient Satisfaction After Total Knee ArthroplastyDocument9 pagesThe WOMAC Score Can Be Reliably Used To Classify Patient Satisfaction After Total Knee ArthroplastyIkmal ShahromNo ratings yet
- Effectiveness of Wii-Based Rehabilitation in Stroke: A Randomized Controlled StudyDocument7 pagesEffectiveness of Wii-Based Rehabilitation in Stroke: A Randomized Controlled StudyAfnes AstrianiNo ratings yet
- 999 EMSRFMEWSposterfinalDocument1 page999 EMSRFMEWSposterfinalzummyrightNo ratings yet
- JAC 11th Physics Syllabus 2023-24Document10 pagesJAC 11th Physics Syllabus 2023-24evil18ytNo ratings yet
- 10 3233@BMR-181135Document9 pages10 3233@BMR-181135Ayu SuprabawatiNo ratings yet
- Semiextended Intramedullary Nailing of The Tibia.6Document11 pagesSemiextended Intramedullary Nailing of The Tibia.6Guna NikhilNo ratings yet
- MJMR - Volume 31 - Issue 3 - Pages 236-239Document4 pagesMJMR - Volume 31 - Issue 3 - Pages 236-239Julio AltamiranoNo ratings yet
- PIIS1935861X21002229Document3 pagesPIIS1935861X21002229Liliane TelesNo ratings yet
- Anestesi Jurnal 3Document13 pagesAnestesi Jurnal 3dewi rahmanNo ratings yet
- Median Nerve Injury RT WDocument7 pagesMedian Nerve Injury RT WMirza IKFR9No ratings yet
- Prognostic Clinical and Radiological Parameters For Immediate Facial Nerve Function Following Vestibular Schwannomas SurgeryDocument7 pagesPrognostic Clinical and Radiological Parameters For Immediate Facial Nerve Function Following Vestibular Schwannomas SurgerySa'Deu FondjoNo ratings yet
- Cannabinoids in Multiple Sclerosis A Neurophysiological AnalysisDocument7 pagesCannabinoids in Multiple Sclerosis A Neurophysiological AnalysisAngel Fernando Santamaria MoralesNo ratings yet
- 09042020212858practical Statistical Methods 2019-20Document91 pages09042020212858practical Statistical Methods 2019-20Esrael KanbataNo ratings yet
- Uncertainty-Based Sampling Plans For Various Statistical DistributionsDocument14 pagesUncertainty-Based Sampling Plans For Various Statistical DistributionsScience DirectNo ratings yet
- SmallestdetectablechangeDocument4 pagesSmallestdetectablechangeBimo AnggoroNo ratings yet
- Lateral Epicondylitis: A Novel Non-Invasive Treatment ApproachDocument4 pagesLateral Epicondylitis: A Novel Non-Invasive Treatment ApproachAnonymous KpdjCwXG9TNo ratings yet
- Franca 2020 AtaxiaDocument6 pagesFranca 2020 AtaxiainervavsNo ratings yet
- Delatorrecanales 2019Document11 pagesDelatorrecanales 2019ELIAS DAVID NOBMAN ALVARADONo ratings yet
- Manejo de Dolor Facial Con RTMSDocument14 pagesManejo de Dolor Facial Con RTMSenviosmentalmedNo ratings yet
- The Use of Auricular Acupuncture To Reduce.24Document3 pagesThe Use of Auricular Acupuncture To Reduce.24Vi PhanNo ratings yet
- Bariatric Surgery and Brain HealthDocument20 pagesBariatric Surgery and Brain HealthAnna MudzNo ratings yet
- Reduction in Spasticity in Stroke Patient With Paraffin TherapyDocument10 pagesReduction in Spasticity in Stroke Patient With Paraffin TherapyayuNo ratings yet
- ActaNeuro AKNFacialDocument8 pagesActaNeuro AKNFacialTimothy CaldwellNo ratings yet
- Prognostic TestsDocument3 pagesPrognostic TestsHANS BENNo ratings yet
- 100205HM-SB CRA Poster Final 3Document1 page100205HM-SB CRA Poster Final 3Osama MariaNo ratings yet
- Ketamina y Dexmedetomidina en QuemadosDocument6 pagesKetamina y Dexmedetomidina en QuemadosVicky CascorNo ratings yet
- Internet-Supported Physical Exercise Training For Persons With Multiple Sclerosis-A Randomised, Controlled StudyDocument11 pagesInternet-Supported Physical Exercise Training For Persons With Multiple Sclerosis-A Randomised, Controlled StudyPoring CarnavasNo ratings yet
- HM 1Document6 pagesHM 1annisanadyapNo ratings yet
- Cai Et Al, 2021Document13 pagesCai Et Al, 2021Bruno KudekenNo ratings yet
- Assessing The Reliability and Responsiveness of 5 Shoulder QuestionnairesDocument8 pagesAssessing The Reliability and Responsiveness of 5 Shoulder QuestionnairesJanaiana UchoaNo ratings yet
- Analisis Jurnal PICO ENGLISHDocument2 pagesAnalisis Jurnal PICO ENGLISHSellyRestyPratamaNo ratings yet
- The Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryDocument4 pagesThe Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryInternational Organization of Scientific Research (IOSR)No ratings yet
- Of Of: Effect Proprioceptive Neuromuscular Facilitation On The Patients With Hemiplegia Long and Short DurationDocument8 pagesOf Of: Effect Proprioceptive Neuromuscular Facilitation On The Patients With Hemiplegia Long and Short DurationsridharNo ratings yet
- The Hemiplegic After Stroke: And: MeasurementDocument4 pagesThe Hemiplegic After Stroke: And: MeasurementAmi MarcuNo ratings yet
- IFCC 2007 Stornaiuolo Architect HBsAgDocument2 pagesIFCC 2007 Stornaiuolo Architect HBsAgFouad RahiouyNo ratings yet
- Neuroscientific based therapy of dysfunctional cognitive overgeneralizations caused by stimulus overload with an "emotionSync" methodFrom EverandNeuroscientific based therapy of dysfunctional cognitive overgeneralizations caused by stimulus overload with an "emotionSync" methodNo ratings yet
- The Pain, Agitation, and Delirium Practice Guidelines For Adult Critically Ill Patients: A Post-Publication PerspectiveDocument9 pagesThe Pain, Agitation, and Delirium Practice Guidelines For Adult Critically Ill Patients: A Post-Publication Perspectivedebby claudiNo ratings yet
- Raval PDFDocument5 pagesRaval PDFdebby claudiNo ratings yet
- Spinal Epidural Synovial Sarcoma A Case of Homogen PDFDocument5 pagesSpinal Epidural Synovial Sarcoma A Case of Homogen PDFdebby claudiNo ratings yet
- ArnoldDocument5 pagesArnolddebby claudiNo ratings yet
- Urn - Isbn - 978-952-61-1781-2Document92 pagesUrn - Isbn - 978-952-61-1781-2debby claudiNo ratings yet
- Demir 2015Document2 pagesDemir 2015debby claudiNo ratings yet
- NIH Public Access: Etiology and Treatment of Hypogonadism in AdolescentsDocument22 pagesNIH Public Access: Etiology and Treatment of Hypogonadism in Adolescentsdebby claudiNo ratings yet
- Management of Pain in The Intensive Care UnitDocument6 pagesManagement of Pain in The Intensive Care Unitdebby claudiNo ratings yet
- Best SoapDocument8 pagesBest Soapdebby claudiNo ratings yet
- Bestsoap PDFDocument1 pageBestsoap PDFdebby claudiNo ratings yet
- Common Sense Talk About Antibacterial ProductsDocument2 pagesCommon Sense Talk About Antibacterial Productsdebby claudiNo ratings yet
- 4.original SharifahDocument9 pages4.original Sharifahdebby claudiNo ratings yet
- NEL243403R03 Karasek Lewinski WRDocument6 pagesNEL243403R03 Karasek Lewinski WRdebby claudiNo ratings yet
- Musa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim NasseriDocument6 pagesMusa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim Nasseridebby claudiNo ratings yet
- Jovin2017 PDFDocument12 pagesJovin2017 PDFdebby claudiNo ratings yet
- Liquid Versus Gel Handrub Formulation: A Prospective Intervention StudyDocument8 pagesLiquid Versus Gel Handrub Formulation: A Prospective Intervention Studydebby claudiNo ratings yet
- 2014 Article 3830Document8 pages2014 Article 3830debby claudiNo ratings yet
- A 12-Week, Randomized, Controlled Trial With A 4-Week Randomized Withdrawal Period To Evaluate The Effi Cacy and Safety of Linaclotide in Irritable Bowel Syndrome With ConstipationDocument11 pagesA 12-Week, Randomized, Controlled Trial With A 4-Week Randomized Withdrawal Period To Evaluate The Effi Cacy and Safety of Linaclotide in Irritable Bowel Syndrome With Constipationdebby claudiNo ratings yet
- Coffee and Herbal Tea Consumption Is Associated With Lower Liver Stiffness in The General Population: The Rotterdam StudyDocument10 pagesCoffee and Herbal Tea Consumption Is Associated With Lower Liver Stiffness in The General Population: The Rotterdam Studydebby claudiNo ratings yet
- Ese 125 Dihydroxyvitamin D 3 Ante Rev.12.15 Low 1Document6 pagesEse 125 Dihydroxyvitamin D 3 Ante Rev.12.15 Low 1debby claudiNo ratings yet
- Vitamin D and Thyroid Diseases: Institute of Endocrinology, Prague, Czech RepublicDocument6 pagesVitamin D and Thyroid Diseases: Institute of Endocrinology, Prague, Czech Republicdebby claudiNo ratings yet
- 1 s2.0 S0002961011000638 Main PDFDocument7 pages1 s2.0 S0002961011000638 Main PDFdebby claudiNo ratings yet
- Nutrients: Vitamin D and Graves' Disease: A Meta-Analysis UpdateDocument15 pagesNutrients: Vitamin D and Graves' Disease: A Meta-Analysis Updatedebby claudiNo ratings yet
- Dolor PosduralDocument39 pagesDolor PosduralMarlen ValdesNo ratings yet
- Placenta PreviaDocument54 pagesPlacenta PreviabobtagubaNo ratings yet
- Regional Anesthesia For CsDocument29 pagesRegional Anesthesia For CsMohmed El KingNo ratings yet
- National List of Essential Medicines Nepal 2021Document72 pagesNational List of Essential Medicines Nepal 2021Sugandhi SahNo ratings yet
- Posicion de Vallejo en Acceso Neuroaxial DificilDocument7 pagesPosicion de Vallejo en Acceso Neuroaxial Dificiljuajimenez55No ratings yet
- Vaginal Hysterectomy CASE STUDYDocument18 pagesVaginal Hysterectomy CASE STUDYJeannie RobisNo ratings yet
- Persistent Paralysis After Spinal Paresthesia PDFDocument6 pagesPersistent Paralysis After Spinal Paresthesia PDFNadia Gina AnggrainiNo ratings yet
- Local AnaesthesiaDocument33 pagesLocal AnaesthesiatesfahuntekleNo ratings yet
- Transes - Perioperative NursingDocument10 pagesTranses - Perioperative NursingJAMES ANDRE RENDONNo ratings yet
- Medical ThesiasDocument360 pagesMedical ThesiasJessica CNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- National List of Essential Medicines: Medicines Route of Administration, Dosage Forms and Strengths Level of UseDocument51 pagesNational List of Essential Medicines: Medicines Route of Administration, Dosage Forms and Strengths Level of UseportosinNo ratings yet
- Test DoseDocument4 pagesTest DoseibunqumairaNo ratings yet
- Case - ViedyaDocument40 pagesCase - ViedyaRaka WibisonoNo ratings yet
- Final NLEM 2016 PDFDocument37 pagesFinal NLEM 2016 PDFBipashwi Nath UpretyNo ratings yet
- List of Dissertations (Subjectwise)Document458 pagesList of Dissertations (Subjectwise)Mayursinh SolankiNo ratings yet
- Anaesthesia - 2022 - Plaat - Prevention and Management of Intra Operative Pain During Caesarean Section Under NeuraxialDocument10 pagesAnaesthesia - 2022 - Plaat - Prevention and Management of Intra Operative Pain During Caesarean Section Under NeuraxialCedric VaillesNo ratings yet
- (OB) 2B - Obstetrical Anesthesia (By Dr. Bretta Lucion)Document3 pages(OB) 2B - Obstetrical Anesthesia (By Dr. Bretta Lucion)CleoGomezNo ratings yet
- Akukwata SeminarDocument22 pagesAkukwata SeminarjenniferNo ratings yet
- Local/Regional/Spinal Anaesthesia: DefinitionDocument4 pagesLocal/Regional/Spinal Anaesthesia: DefinitionThistell ThistleNo ratings yet
- Spinal & Epidural AnaesthesiaDocument31 pagesSpinal & Epidural AnaesthesiaKumar Gavali Suryanarayana0% (1)
- Anestesi EpiduralDocument2 pagesAnestesi EpiduralShazean ShahNo ratings yet
- AnaesthesiaDocument3 pagesAnaesthesiaJoan nakijjobaNo ratings yet
- PG Dissertation Topics-2020Document129 pagesPG Dissertation Topics-2020Jaggu MamidiNo ratings yet
- Perioperative Pre-Class Mini-Lecture - CH 17-19Document22 pagesPerioperative Pre-Class Mini-Lecture - CH 17-19Marcel YoungNo ratings yet
- Local and Regional AnesthesiaDocument78 pagesLocal and Regional AnesthesiaPatricia Feliani Sitohang100% (4)
- Spinal Anesthesia - Technique - UpToDateDocument37 pagesSpinal Anesthesia - Technique - UpToDateSamir Perez CasadiegoNo ratings yet