Professional Documents
Culture Documents
Went LIVE 17 March 2014 One Woman Too Many Development Implementation
Went LIVE 17 March 2014 One Woman Too Many Development Implementation
Uploaded by
Daeng FarahnazOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Went LIVE 17 March 2014 One Woman Too Many Development Implementation
Went LIVE 17 March 2014 One Woman Too Many Development Implementation
Uploaded by
Daeng FarahnazCopyright:
Available Formats
MEWS - Maternity Early Warning Score
Conny Krebs, Clinical Midwife Educator - Ko Awatea, Auckland, New Zealand
Gail McIver, Midwife Manager - CM Health, Auckland, New Zealand
Kathy Ogilvy, Nurse/Midwife Educator - Ko Awatea, Auckland, New Zealand
One woman too many Development Implementation Went LIVE 17 March 2014
Introduction Research New Parameter
Affix patient’s identification label here
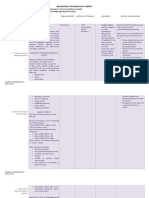
CM Health is introducing a systematic scoring chart for maternity Research indicates that warning signs precede virtually every critical A new parameter – blood loss – has been added to the MATERNITY EARLY WARNING SCORE
patients to Women’s Health Service. The MEWS (Maternity Early inpatient event. There are well-established early warning score (EWS) MEWS score. Blood loss is one of the most common causes *Standard vital signs: q4H, Respiratory rate, Saturation, Heart rate, BP, Blood Loss,Temp, Level of consciousness, Urine output and Pain
Warning Score) chart will assist staff to identify antenatal and postnatal charts in existence for use with general patients. A general EWS of preventable severe maternal morbidity, and is often Date
Time
MIDWIFERY AND NURSING ACTIONS
FOR PATIENTS WITH A MEWS SCORE
women at risk of deteriorating in condition and improve the response to physiologically unstable patient chart was introduced at CM Health in exacerbated by delayed or inappropriate treatment. It can be Pain at Rest 0-10
Pain On Movement 0-10
Score 0
the acutely deteriorating woman. 2007. (2) one of the critical indicators of deterioration, and the amount
>40 >40
30-39 30-39 Score 1
Respirations
25-29 25-29
of blood lost is frequently underestimated. 20 20 Score 2
However, EWS charts designed for general patients are unsuitable
Setting
15 15
10 10 Score 5+ 888
for use in obstetrics due to the physiological changes and modified
Modification for Birthing Units
<8 <8
98-100 98-100 ANY PATIENT VITAL SIGNS IN THE
Saturations
YELLOW SCORES 1
CM Health serves the Counties Manukau region in Auckland, New responses that occur during pregnancy. 94-98 94-98
for
91-93 91-93
Calculate the Total MEWS Score
Zealand. It has a birthing unit at Middlemore Hospital, one of the largest MEWS has also been introduced to the three primary birthing s
<90 <90
ter
1. Inform Midwife/Nurse in charge
O2 litres/min
2. Increase frequency of vital signs one hourly
tertiary hospitals in New Zealand, and primary birthing units at satellite Although the importance of early warning scores for obstetric units. As these units operate in the community setting, have
>140
e >140
ram th
or more frequently if required.
130 130
3. Treat Pain
patients is widely recognised, there are no national or international a
d P ldbir
120 120
sites in Botany Downs, Papakura and Pukekohe. All primary birthing no medical staff onsite and rely on the ambulance service for 110 110
e
ifi Chi
Heart Rate bpm
units offer pregnancy clinics, labour and birthing facilities and provide ‘gold standards’ obstetric warning scores currently in use. (3) transfer, the action plan has been modified to their needs. An
100
d
100
o ANY PATIENT VITAL SIGNS IN THE
90 90
postnatal care. easy peel-off sticker, with the action algorithm appropriate for
80
70 M 80
70
ORANGE SCORES 2 - 4
Multiprofessional Team 60 60
Calculate the Total MEWS Score
the birthing units, is applied and makes it instantly functional. 50
40
50
40
1. Inform Midwife/Nurse in charge
2. Repeat vital signs within 1/2 hour.
• The estimated Counties Manukau population for 2013 is 30 30
3. If MEWS score unchanged contact
Obstetric Registrar, notify PAR Team.
>200 >200
512,130, 11.5% of the total New Zealand population.
Trial 190 189-199
4. Continue 1/2 hourly vital signs until
180 180
Obstetric Registrar arrives.
170 170
5. If Obstetric Registrar not available
call Obstetric Consultant.
Systolic Blood Pressure mmHg
• Counties Manukau has high numbers of Maaori, Pacific and Midwives MEWS was trialled over 5 days for usability in Middlemore
160
150
160
150
Asian peoples and a relatively youthful population.
140
ctions
140
Hospital Delivery Suite and Maternity Ward, as well as 130 130 ANY PATIENT VITAL SIGNS IN THE
Acute Pain
120 A 120 PURPLE SCORES 5 OR MORE OR IF YOU ARE
Team Managers tested retrospectively on Serious and Sentinel Event cases. 110 110 CONCERNED ABOUT THE PATIENT CALL
• Counties Manukau has a high birth rate compared with many 100 100
All retrospectively reviewed cases would have triggered and 90 90 888
other areas – 7282 babies were delivered in 2013 at CM Health. 80 80
received early intervention if this chart had been available and 70 70 OBSTETRIC EMERGENCY TEAM or
r WOMENS HEALTH CARDIAC ARREST
oss
This contributes to relatively high demand on our maternity and
60 60
used. 50
ete 50 or STAT CAESAREAN SECTION
L
ram lood
Stay with the patient.
child health services.(1)
140 140
Diastolic Blood Pressure mmHg
a
130 130
Midwife & 120
w P lB 120 VARIATION TO BLOOD LOSS THRESHOLD
Audits a
Ne Tot
110 110
Nurse Nurses Measuring Blood Loss estimate.
Major Haemorrhage After Birth Have Tripled
100 100
Soaked Pad = 150mls
Educators
ing
90 90
MEWS
Soaked Blue inco sheet = 450mls
80
n n 80 Soaked Towel = 600mls
Currently we are in the process of evaluating the chart and Ru
70 70 1ml blood = 1 gm weight
60 60
Visua
Score 0 0-499mls OBSERVE
refining our measurable aim. 50 50
1500+
l Aid f 1500+
Blood Loss (ml)
Score 1 500-1000mls
Running Total
1000-1499
or Blo 1000-1499
751-999 751-999
odScore 2 1000-1500mls
Major Haemorrhage
Lo
Conclusion ss
500-750 500-750
Clinical Training 0-499 0-499 Score 5+ 1500mls+
& Education Obstetricians Est bld loss on arrival
PAD 150ml
> 1500 mls
>38.5 >38.5
148 Centre
PPH cannot be prevented. It is axiomatic that PPH occurs 38.1-38.4 38.1-38.4
Temperature
38 38
120
51
unpredictably and no patient is immune from it. 37
36
37
36
<35 <35
Patient at Risk Alert Alert
Anaesthetists
Urine Output Consciousness
Team What can be changed is how we react to and manage PPH. The Voice Voice
Level of
Pain Pain INCO SHEET 450ml
2010 2011 2012 introduction of a specific EWS for obstetrics combined with an Unresponsive
New Confusion
Unresponsive
New Confusion
evidence-based management model can potentially reduce the
Running Total
>30ml/hr >30ml/hr
Birth Rate 8171 8135 8103 16-29 ml/hr 16-29 ml/hr
practice variability and improve the quality of care. Glucose
<15 ml/hr <15 ml/hr
In 2010 the Women’s Health Quality Specialist Midwife brought Respiratory Rate
MEWS SCORE - Calculate total score. Add each vital sign to reach TOTAL MEWS SCORE
Respiratory Rate TOWEL 600ml
Over the last four years midwives in the delivery suite observed an
together a multiprofessional team with the idea to develop a modified Saturations
Sco re Saturations
s
Heart Rate Heart Rate
w
EWS for Maternity Services. l Me
Systolic BP Systolic BP
increase in major haemorrhages after birth, also known as postpartum Tota
Diastolic BP Diastolic BP
Blood Loss Blood Loss
haemorrhage(PPH), particularly major PPH over 1500mls. In too many
Temperature Temperature
Midwives, nurses, managers, members of the Patient At Risk team, Level of Consciousness
Urine Output
Conscious Level
Urine Output
cases, PPH was not managed in a timely manner to prevent women Clinical Training & Education Centre, Acute Pain team, obstetricians, TOTAL SCORE TOTAL SCORE
going down the continuum of deterioration, and patients became
Counties Manukau District Health Board Copyright © CMHealth 2014. All Rights Reserved. No part of this document may be reproduced without CMHealth’s express consent. Reorder No. OBST56 July 14
anaesthetists and midwife and nurse educators formed a group
unstable. and worked together over three years to develop and implement a
modified early warning score for women during childbirth.
Time to do something about it!
MEWS Team References
Gail McIver, Quality Specialist Midwife, Delivery Suite Manager / Lesley Ansell, Associate Clinical Charge Midwife / Karen Clarke, Nurse Educator / Kathy Ogilvy, Sponsorship and Funding: (1) CMDHB website; (2) Robb & Sebbon (2010) A multi-faceted approach to the physiologically unstable
Nurse / Midwife Educator / Clare Kirby, Clinical Midwife Educator / David Ansell, Obstetric SMO / Sarah Wadsworth, Obstetric SMO / Louise Sherman, Obstetric patient. Qual Saf Health Care; 2010; 19; e47; (3) Carle, C., Alexander, P., Columb, M. et al (2013) Design
Anaesthetist / Karla Masson, Acute Pain Nurse / Jenny Hunt, Acute Pain Nurse / Dwan Lee, Acute Pain Nurse / Susan Tareki, PAR Team / Tracey Cooper, CTEC / and internal validation of an obstetric early warning score: secondary analysis of the Intensive Care
Tanya Wilson, Associate Clinical Charge Midwife / Tish Taihia, Associate Clinical Charge Midwife / Conny Krebs, Clinical Midwife Educator National Audit and Research Centre Case Mix Programme database. Anaesthesia; 2013; 68; pp. 354-367
You might also like
- Free Medical Transcription Course PDFDocument28 pagesFree Medical Transcription Course PDFMichellePascualPullon90% (10)
- Regional Obstetric Early Warning Score ChartDocument2 pagesRegional Obstetric Early Warning Score ChartDaeng Farahnaz100% (2)
- CommunicationDocument4 pagesCommunicationapi-302578028No ratings yet
- 14 MEWS Maternity Early Warning ScoreDocument72 pages14 MEWS Maternity Early Warning ScoreDaeng FarahnazNo ratings yet
- M Solution, Pthis New Ppt-SimrsDocument34 pagesM Solution, Pthis New Ppt-SimrsSiskanarisaNo ratings yet
- BMT Flow Chart - 2018 PDFDocument1 pageBMT Flow Chart - 2018 PDFMisty Long NgenuyenNo ratings yet
- EDAN-F9 SeriesDocument2 pagesEDAN-F9 SeriesSheila BernalteNo ratings yet
- Cook 2014Document1 pageCook 2014Yolanda Dwi OktaviyaniNo ratings yet
- Hunt2018Global CareDocument9 pagesHunt2018Global CareDwi RahmawatiNo ratings yet
- Prevention and Management of Procedural Pain in The Neonate An U 2016Document13 pagesPrevention and Management of Procedural Pain in The Neonate An U 2016Indra WijayaNo ratings yet
- UNICEF Report of Rapid Essential Health Service AssessmentDocument8 pagesUNICEF Report of Rapid Essential Health Service AssessmentputrilgNo ratings yet
- Progesterone Vaginal SuppositoryDocument1 pageProgesterone Vaginal SuppositoryACOB, Jamil C.No ratings yet
- Treatment of Metabolic Syndrome in Children: Mini Review ArticleDocument11 pagesTreatment of Metabolic Syndrome in Children: Mini Review ArticleMadalina NastaseNo ratings yet
- First Trimester Screening For Preeclampsia An.6Document8 pagesFirst Trimester Screening For Preeclampsia An.6ronaNo ratings yet
- 2014 BJM MeowsDocument7 pages2014 BJM MeowshendraNo ratings yet
- A Modified Early Obstetric Warning System: ProfessionalDocument7 pagesA Modified Early Obstetric Warning System: ProfessionalitaindrianiNo ratings yet
- Relieving Anxiety in Patients Undergoing Cataract SurgeryDocument1 pageRelieving Anxiety in Patients Undergoing Cataract Surgeryapi-286232866No ratings yet
- The Tendency of Stunting Among Children Under Five in The North - 2023 - JornalDocument8 pagesThe Tendency of Stunting Among Children Under Five in The North - 2023 - JornalJuan ZilkyNo ratings yet
- 2018 ICU SRMO Critical CareDocument10 pages2018 ICU SRMO Critical CarespamvarunNo ratings yet
- Nutrition Workplan 2023 2025Document12 pagesNutrition Workplan 2023 2025Rico Jay GrasparilNo ratings yet
- Ida Jean Orlando-PellitierDocument2 pagesIda Jean Orlando-PellitierCrazy StrangerNo ratings yet
- Vii. (C) Gots-Ppa (Final)Document31 pagesVii. (C) Gots-Ppa (Final)Paulo AlunanNo ratings yet
- Quality of Evidence: Low Strength of RecommendationDocument10 pagesQuality of Evidence: Low Strength of Recommendationtri kurniawatiNo ratings yet
- IDoR2015 Paediatric-Imaging-Book FINAL PDFDocument129 pagesIDoR2015 Paediatric-Imaging-Book FINAL PDFMelii LujanNo ratings yet
- ARDS Nuevas TerapiasDocument3 pagesARDS Nuevas TerapiasEvelyn CóndorNo ratings yet
- Acog Committee Opinion: Medically Indicated Late-Preterm and Early-Term DeliveriesDocument5 pagesAcog Committee Opinion: Medically Indicated Late-Preterm and Early-Term DeliveriesBianca CaterinalisendraNo ratings yet
- Texas Health Steps Periodicity ScheduleDocument2 pagesTexas Health Steps Periodicity ScheduleLujain Al OmariNo ratings yet
- NCP Manela 305 DeficientKnowledgeDocument9 pagesNCP Manela 305 DeficientKnowledgeJimuel Brian ManelaNo ratings yet
- Deficient KnowledgeDocument3 pagesDeficient KnowledgeJoshuaCarmelo AquinoNo ratings yet
- The Effect of Physical Activity On Fertility: A Mini-ReviewDocument9 pagesThe Effect of Physical Activity On Fertility: A Mini-ReviewThiago SartiNo ratings yet
- NCP: Labor Stage 1 Latent PhaseDocument9 pagesNCP: Labor Stage 1 Latent PhaseJavieNo ratings yet
- Far Eastern University: Institute of NursingDocument2 pagesFar Eastern University: Institute of NursingSean Philippe CabralNo ratings yet
- Ncma217 Rle - Case StudyDocument15 pagesNcma217 Rle - Case Studyanjie kamidNo ratings yet
- Labor Stage I - Latent PhaseDocument9 pagesLabor Stage I - Latent Phasenursereview100% (3)
- Modified Early Obstetric Warning Score MEOWS MID33 AO13 v6.1Document7 pagesModified Early Obstetric Warning Score MEOWS MID33 AO13 v6.1deviNo ratings yet
- Gestational Hypertension and Preeclampsia ACOG.46Document24 pagesGestational Hypertension and Preeclampsia ACOG.46UWIMANA Jean ClaudeNo ratings yet
- Conception Pamphlet FINALDocument2 pagesConception Pamphlet FINALAvery ElleNo ratings yet
- Internasional 4Document10 pagesInternasional 4Aanii SNo ratings yet
- Acute and Critical Care Nursing: Unit Learning OutcomeDocument3 pagesAcute and Critical Care Nursing: Unit Learning OutcomeBunnie AlphaNo ratings yet
- Preeclampsia Pathophysiology and Implications For.9Document8 pagesPreeclampsia Pathophysiology and Implications For.9BiBiana PinToNo ratings yet
- Breaking Bad News: An Evidence-Based Review of Communication Models For Oncology NursesDocument8 pagesBreaking Bad News: An Evidence-Based Review of Communication Models For Oncology NursesDaniela Lepărdă100% (1)
- Pasien NyDocument6 pagesPasien NySuci MaghfirahNo ratings yet
- IJWH 352348 Determinants of Premature Rupture of Membrane Prom Among PDocument12 pagesIJWH 352348 Determinants of Premature Rupture of Membrane Prom Among PCitaNo ratings yet
- Maternity Early Obstetric Warning Scoring System UHL Obstetric GuidelineDocument12 pagesMaternity Early Obstetric Warning Scoring System UHL Obstetric GuidelinetjoemaNo ratings yet
- Using The ABCDE Approach For All Critically Unwell PatientsDocument6 pagesUsing The ABCDE Approach For All Critically Unwell PatientsYustitiNo ratings yet
- Pone 0217864Document15 pagesPone 0217864tioNo ratings yet
- PEWS BookDocument57 pagesPEWS Bookhendra firmansyahNo ratings yet
- Pediatric Dentistry: Fourth EditionDocument6 pagesPediatric Dentistry: Fourth EditionFadiaNo ratings yet
- Emergency and Disaster NursingDocument9 pagesEmergency and Disaster NursingDempsey AlmirañezNo ratings yet
- McAllister - David MSN FP6021 Assessment 1 Attempt 2Document6 pagesMcAllister - David MSN FP6021 Assessment 1 Attempt 2David McAllisterNo ratings yet
- IranianJNursingMidwiferyRes25123-1689391 044133.PDF AnxietyDocument8 pagesIranianJNursingMidwiferyRes25123-1689391 044133.PDF AnxietyZakkiyatus ZainiyahNo ratings yet
- Evidence-Based Outcomes CenterDocument19 pagesEvidence-Based Outcomes CenterSantosa TandiNo ratings yet
- Modified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2Document9 pagesModified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2indirinoor5No ratings yet
- NURS 4369 Preceptor Packet Core 2013Document11 pagesNURS 4369 Preceptor Packet Core 2013Aruna Chezhian100% (1)
- Nursing ProcessDocument5 pagesNursing Processchnllh19No ratings yet
- LAGAS - AssignmentDocument17 pagesLAGAS - AssignmentChristian LagasNo ratings yet
- Progression of First Stage LaourDocument14 pagesProgression of First Stage LaourAlmira Dyah PuspitariniNo ratings yet
- Escala Del Dolor PPPDocument16 pagesEscala Del Dolor PPPMariana SuarezNo ratings yet
- 13 PDFDocument9 pages13 PDFringgoNo ratings yet
- Pharmacy Daily 10th Nov 2023Document2 pagesPharmacy Daily 10th Nov 2023Marinero CzarNo ratings yet
- Developing A Teaching PlanDocument6 pagesDeveloping A Teaching PlanAntonette Africa MercadoNo ratings yet
- The COAT & Review Approach: How to recognise and manage unwell patientsFrom EverandThe COAT & Review Approach: How to recognise and manage unwell patientsRating: 5 out of 5 stars5/5 (1)
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- 2-Step Clinical Mastery: Elevate Your Practice as a Nurse Practitioner and NP StudentFrom Everand2-Step Clinical Mastery: Elevate Your Practice as a Nurse Practitioner and NP StudentNo ratings yet
- Electronic Fetal MonitoringFrom EverandElectronic Fetal MonitoringXiaohui GuoNo ratings yet
- The Digestive System Sistem PencernaanDocument55 pagesThe Digestive System Sistem PencernaanDaeng FarahnazNo ratings yet
- Bab 12 - Muscular SystemDocument73 pagesBab 12 - Muscular SystemDaeng FarahnazNo ratings yet
- Joints of The Skeletal System: Childbirth ContractionDocument54 pagesJoints of The Skeletal System: Childbirth ContractionDaeng FarahnazNo ratings yet
- Imews Escalation Guide PDFDocument2 pagesImews Escalation Guide PDFDaeng FarahnazNo ratings yet
- Went LIVE 17 March 2014 One Woman Too Many Development ImplementationDocument1 pageWent LIVE 17 March 2014 One Woman Too Many Development ImplementationDaeng FarahnazNo ratings yet
- Nepal PosterDocument1 pageNepal Posterapi-282838160No ratings yet
- Sir James Young Simpson CollectionDocument77 pagesSir James Young Simpson CollectionSuresh KumarNo ratings yet
- PrincetonDocument7 pagesPrincetonangel nahdeeNo ratings yet
- What Are Palliative Care and Hospice CareDocument13 pagesWhat Are Palliative Care and Hospice CareXo YemNo ratings yet
- Terminal Units ProvisionDocument5 pagesTerminal Units Provisionkhaledaj1977No ratings yet
- History of Nursing: Nursing in The Near EastDocument7 pagesHistory of Nursing: Nursing in The Near EastCatherine PradoNo ratings yet
- Ambulance Forms SampleDocument2 pagesAmbulance Forms SampleCOOP ER BuddiesNo ratings yet
- All India Hospital List 2Document113 pagesAll India Hospital List 2Arshad MohammedNo ratings yet
- 1782-Motion Re Info MGMT Services and Trust Ageement and Document Retention PlanDocument58 pages1782-Motion Re Info MGMT Services and Trust Ageement and Document Retention PlanConnaissableNo ratings yet
- Basic Statistics (3685) PPT - Lecture On 20-01-2019Document64 pagesBasic Statistics (3685) PPT - Lecture On 20-01-2019M Hammad ManzoorNo ratings yet
- American J Hematol - 2019 - BainDocument1 pageAmerican J Hematol - 2019 - Bainbassam alharaziNo ratings yet
- UNC ED Pediatric Asthma ProtocolDocument2 pagesUNC ED Pediatric Asthma ProtocolAhmed BekhetNo ratings yet
- Drs CVDocument2 pagesDrs CVNameNo ratings yet
- Resume - Narges Jalilian JamDocument2 pagesResume - Narges Jalilian Jammohammadrezahajian12191No ratings yet
- Placenta PreviaDocument2 pagesPlacenta PreviaIrish Joy S. DecrepitoNo ratings yet
- Test Practice 1Document5 pagesTest Practice 1syafwanNo ratings yet
- Clinical Objectives GuidelinesDocument11 pagesClinical Objectives GuidelinesprowritttersNo ratings yet
- Community Health NursingLectureDocument40 pagesCommunity Health NursingLectureMJCNo ratings yet
- Spacemed ArticleDocument4 pagesSpacemed ArticleBingDelaCruzNo ratings yet
- Cheruvim Ava V. Ortega, RN: Personal DataDocument6 pagesCheruvim Ava V. Ortega, RN: Personal DatarekcuftnucNo ratings yet
- Delivery Packages: Length of Stay Ward Semi-Private PrivateDocument1 pageDelivery Packages: Length of Stay Ward Semi-Private PrivateZohaib AhmedNo ratings yet
- Formulir Klaim Rawat InapDocument2 pagesFormulir Klaim Rawat InapGoris DonkeyNo ratings yet
- Why I Like The Hospital - PoemDocument2 pagesWhy I Like The Hospital - Poem6557.astroNo ratings yet
- English Language - Teacher's Guide (Year 2) PDFDocument140 pagesEnglish Language - Teacher's Guide (Year 2) PDFlaia martinNo ratings yet
- Communication Skills Course Role PlaysDocument6 pagesCommunication Skills Course Role PlaysnoldinaNo ratings yet
- Hospital Experiences Responding To The COVID-19 PandemicDocument41 pagesHospital Experiences Responding To The COVID-19 PandemicLaw&CrimeNo ratings yet