Professional Documents
Culture Documents
Anemia +bblr+prematur
Anemia +bblr+prematur
Uploaded by
Anonymous 0Mnt71Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anemia +bblr+prematur
Anemia +bblr+prematur
Uploaded by
Anonymous 0Mnt71Copyright:
Available Formats
http:// ijp.mums.ac.
ir
Systematic Review (Pages: 3323-3342)
Maternal Anemia and Pregnancy outcomes: a Systematic Review and
Meta-Analysis
Shoboo Rahmati1, Ali Delpisheh2, Naser Parizad3, *Kourosh Sayhmiri41
1
MSc Student of Epidemiology, Student Research Committee, Ilam University of Medical Sciences, Ilam, Iran.
2
Professor of Epidemiology, Public Health Faculty, Ilam University of Medical Sciences, Ilam, Iran.
3
Ph.D Candidate in Nursing, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz,
Iran. 4Associate Professor of Biostatistics, Psychosocial Injuries Research Center, Ilam University of Medical
Sciences, Ilam, Iran.
Abstract
Background
The aim of this study was to determine the relationship between maternal anemia during pregnancy
and pregnancy outcomes.
Materials and Methods
This systematic review was conducted in domestic (Sid, Iran.doc, Iran medex and Magiran) and
international (PubMed, Science Direct, Cochrane, Medline, Web of Science, Scopus, Springer,
Embase, Google scholar) databases from January 1, 1990 to April 10, 2016 with using standard key
words "Pregnancy", "Pregnant women", "Hemoglobin/ haemoglobin", "Anemia/ anaemia", and
"Pregnancy outcome". Relative risks (RR) and confidence intervals were extracted from each study.
Results
Overall 30 studies with a total sample size of 1,194,746 were entered into the final meta-analysis.
Maternal anemia in the first trimester showed a significant relationship with low birth weight (RR:
1.28, 95% CI, 1.10 - 1.50, P<0.01), pre-term birth (RR: 1.26, 95% CI, 1.11- 1.44, P<0.01) and small
for gestational age (RR: 1.12, 95% CI, 1.05 - 1.19, P<0.01`), that means maternal anemia in the first
trimester raises the risk of these outcomes.
Even though, maternal anemia in the second trimester has no significant relationship with low birth
weight (RR, 1.19, 95% CI, 0.65- 2.17, P>0.05) and pre-term birth (RR: 1.35, 95% CI, 0.54 - 3.24,
P>0.05). Similarly, maternal anemia in the third trimester has also, no significant relationship with
low birth weight (RR: 1.23, 95% CI, 0.97 - 1.55, P>0.05) and pre-term birth (RR: 1.55, 95% CI, 0.83
- 2.88, P>0.05).
Conclusion
Maternal anemia during pregnancy in the first trimester in particular can be considered as a
risk factor for pregnancy outcomes and must be treated as an advance.
Key Words: Anemia, Hemoglobin, Pregnancy, Meta-Analysis, Systematic review, Women.
*Please cite this article as: Rahmati Sh, Delpisheh A, Parizad N, Sayhmiri K. Maternal Anemia and Pregnancy
outcomes: a Systematic Review and Meta-Analysis. Int J Pediatr 2016; 4(8): 3323-42.
*
Corresponding Author:
Kourosh Sayehmiri, Associate Professor of Biostatistics, Psychosocial Injuries Research Center, Ilam University
of Medical Sciences, Ilam, Iran.
Email: sayehmiri@razi.tums.ac.ir
Received date: Jan 11, 2016; Accepted date: Mar 22, 2016
Int J Pediatr, Vol.4, N.8, Serial No.31, Aug 2016 3323
Anemia and Pregnancy outcomes: Meta-analysis
1-INTRODUCTION
Iron is one of the most essential preterm delivery, intrauterine growth
elements during pregnancy and iron restriction and increased blood pressure
deficiency anemia is the most common Intrauterine growth retardation (IUGR)
nutritional deficiency worldwide. So, (21); while others study not have been
maternal anemia is a common health achieved no association between
problem during pregnancy (1). Parasitic Hemoglobin concentration and adverse
diseases such as malaria, hookworm pregnancy outcomes(27). So far, various
infection, schistosomiasis, micronutrient studies which measured the link between
deficiencies including folic acid, vitamin hemoglobin concentrations with pregnancy
A, vitamin B12, genetic hemoglobin outcomes have been conducted in the
apathies such as thalassemia and world. Previous research has demonstrated
Helicobacter pylori has been shown in the a strong association between severe
etiology of anemia in pregnant women (2- anemia and maternal mortality (29); also,
4). The prevalence of anemia among other meta-analysis with the same title was
pregnant women is 52 percent in conducted in 2011. Since then, there have
developing countries and 22.5 percent in been many studies in this regard. To put all
developed countries (5).The high the findings together and provide a more
prevalence of the disease burden has been accurate picture of the problem,
reported in Asia (60%) and Africa (52%) performing another meta-analysis, seems
and 80 percent of anemic pregnant women to be necessary. The aim of this study was
live in South Asia (6-8). to evaluate the relationship between
maternal anemia in all trimesters
Prevalence is different during all trimesters
separately with pregnancy outcomes from
of pregnancy. According to meta-analysis
Jan 1990 to Apr 2016 and to investigate its
that had been conducted in Iran in 2015,
overall trend in the world by performing a
the prevalence of anemia was estimated to
systematic review and meta-analysis study.
19.6 percent in the first trimester, 10.1
percent in the second trimester and 16.1 2- MATERIALS AND METHODS
percent in the third trimester, respectively
2-1. Search strategy
(9). According to the US Center for
Disease Control (CDC), if hemoglobin This systematic review study was
levels in the first and the second trimester conducted from Jan 1990 to Apr 2016.
of pregnancy is less than 11 grams per Articles extracted by using related key
deciliter, and in the third trimester is less words in domestic (Sid, Iran.doc, Iran medex
than 10.5 grams per deciliter is considered and Magiran) and international (PubMed,
anemia (10, 11). Anemia during pregnancy Science Direct, Cochrane, Medline, Web of
is a risk factor for mother and the fetus. Science, Scopus, Springer, Embase, Google
Many studies have shown pregnancy scholar) databases. To maximize the
outcomes, including low birth weight, comprehensiveness of the search results,
neonatal deaths, perinatal deaths, Persian key words and all possible
premature birth, low gestational age, fetal combinations of words were searched in
death as a result of maternal anemia (12- domestic database. MESH key words
19). A U-shaped distribution has been including "Pregnancy", "Pregnant
shown between hemoglobin concentration women", "Hemoglobin/haemoglobin",
and pregnancy complications (20, 21). "Anemia/anaemia", "Hematologic",
This means that the increase of "Haematologic parameter", "Mortality",
hemoglobin (more than g / dL13 / 2) As "Preterm birth delivery", "Low birth
reductions, lead to complications such as weight" and "Small for gestational age",
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3324
Rahmati et al.
were searched in the international between maternal anemia and pregnancy
electronic database. Boolean searches outcomes were analyzed. Pregnancy
using "AND" or "OR" applied for outcomes including: low birth weight
searching combination words to get (LBW), pre-term birth (PTB), Small for
comprehensive results. The list of gestational age (SGA), stillbirth (SB),
evaluated article references was used to neonatal deaths (ND) and perinatal deaths
find more studies. The study was (PD). Only LBW, PTB and SGA were
performed based on the PRISMA check analyzed during analysis, because few
list for meta-analysis studies (38) studies were conducted to evaluate other
(Figure.1). outcomes. To assess the significance, the
relative risk with 95% confidence intervals
2-2. Inclusion and exclusion criteria
(CI) and P-value less than 0.05 was
Inclusion criteria in the present study, considered.
including:
2-4. Data Extraction
Studies in which the relationship
Data extraction was performed by two
between maternal anemia during
researchers independently and an
pregnancy and pregnancy outcomes
extraction form (the author's name, year of
was identified,
publication, country, Continent, the
Availability of full text articles,
number of participants, trimester and
The studies with population of
pregnancy outcome, relative risk and
infants and pregnancy outcomes,
confidence interval and P-value of
The studies science 1990 to next.
pregnancy outcomes) was used to
Exclusion criteria include studies: minimize bias and error in collecting data.
With non-random sample sizes, If some information in the articles, was not
clear and need to ask specific questions,
2-Unrelated to the topic,
needed questions were asked from the
with inadequate data,
author by e-mail. Each of the researchers
Unidentified the month of compared the extracted data and discussed
pregnancy,
together if they had any conflict about
With a different definition of extracted data. They discussed with a third
maternal anemia, researcher, until they came to an
Inaccessible to needed data, agreement by re-evaluating and comparing
7-the studies before 1990. the results.
To prevent the bias, search process, study 2-5. Outcomes of interests
selection, quality assessment and
extracting data conducted by two The outcomes of interests were LBW, PTB
researchers independently. and SGA. Low birth weight was defined as
a newborn with weight at birth of less than
2-3. Study Selection 2,500 grams. Pre-term birth was defined as
Firstly, the researchers obtained some a neonate born before 37 weeks of
articles from throughout the search. Every gestational age (the 259th day). Small for
study about hemoglobin concentration and gestational age was a newborn whose birth
pregnancy outcomes was selected. Then, weight was below the 10th percentile for
by reviewing abstract and full text, all the gestational age (47).
studies that had a real connection to the 2-6. Statistical Analysis
topic entered into the study. In this study,
all cohort, case-control and cross-sectional Extracted data in the present study,
studies that measured the relationship including the study code, type of the study,
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3325
Anemia and Pregnancy outcomes: Meta-analysis
the author’s name, year of publication, combine the study's results. In every study,
continent, the number of participants, Relative risks (RR) or Odds ratio (OR)
trimester, pregnancy outcomes, relative extracted the lower and higher limit. In
risk, confidence interval and P-value. A studies that this index was not extracted, it
hemoglobin classification was conducted was calculated through OR=ad/bc
as follows: <14, 11-13, 11> g/dl (10, 11). (Articles that had not the OR to use the
In this study, a mother with hemoglobin formula) and the logarithm of OR or RR
less than 11 has been considered as anemic was used to polarize the effect size. Error
and also, pregnancy outcomes were standard was calculated by SE= 1n (upper
analyzed based on their definition. The 95% CI / lower 95% CI) / (2× 1.96). If
effect of hemoglobin in pregnant women only upper and lower limit had been
in the first, the second and third trimester reported in studies, OR= ad/bc was used.
of pregnancy was investigated about all Meta-regression was used for evaluating
types of pregnancy outcomes using the the relation between year of study and
relative risk index and the heterogeneities effect size and evaluating the cause of
were assessed using I2 index statistic. I2 is heterogeneity of studies. Begg’s funnel
an index that shows heterogeneities among plot, was used to investigate publication
studies, I2 less than 25% show low bias and sensitivity analysis was
heterogeneities, %25 < I2 < 75% moderate performed to evaluate the effect of each
heterogeneity, and I2 > 75% high study on the overall results. STATA
heterogeneity. When Q statistics was software version 3.2 was used to analyze
significance we used random effect in this study and P<0.05 has been
models. For the heterogeneity of studies, considered significance level for all
the random effect model was used to analyzes.
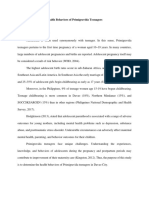
Fig.1: Entry procedures of studies to meta-analysis
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3326
Rahmati et al.
3- RESULTS There were 12 cohort studies that
Overall 30 studies with a total sample size evaluated maternal anemia in the first
of 1,194,746 were entered into the final meta- trimester and chronic low birth weight.
analysis. In the present meta-analysis about When these studies were combined using a
80 percent of the studies were cohort, 13.3 random effects model, it showed that there
percent cross-sectional and 6.6 percent is a significant relationship between
case-control. The mean age of the studies maternal anemia in the first trimester of
was under 30+ SD years old. Therefore, pregnancy and LBW (relative risk, 1.28
the age item was excluded during analysis [95% CI: 1.10 to 1.50]). Also, it showed
and the majority of studies had been that the Levy study (ref) had the highest
conducted in Asian countries. weight among these studies. As shown in
the following (Figure.2), Chi-square tests
3-1. The relationship between maternal show that the results of 12 cohort studies
anemia in the first trimester of were heterogeneous and significant (I2
pregnancy and low birth weight Index= 76%, P = 0.000). When there is
3-1-1. By type of study heterogeneity among results of studies that
means the results of studies are differents.
Study %
ID RR (95% CI) Weight
Zhou (1998) 2.96 (1.15, 7.62) 2.40
Hamalainen (2003) 3.14 (1.35, 7.29) 2.92
Xiong (2003) 0.75 (0.53, 1.07) 9.38
Levy (2005) 1.10 (1.05, 1.15) 17.29
Monawar (2006) 2.00 (1.18, 3.39) 5.90
Ren (2007) 1.16 (1.03, 1.30) 16.00
Kidanto (2009) 2.23 (1.44, 3.46) 7.41
Abeysena (2010) 0.56 (0.07, 4.61) 0.54
Kumar (2010) 1.02 (0.83, 1.25) 13.53
Mohamed (2012) 1.45 (1.14, 1.84) 12.57
Huang (2015) 0.61 (0.32, 1.16) 4.52
Chikjwa (2015) 2.00 (1.30, 3.09) 7.53
Overall (I-squared = 76.0%, p = 0.000) 1.28 (1.10, 1.50) 100.00
NOTE: Weights are from random effects analysis
.0681 1 14.7
Fig.2: The relationship between maternal anemia in the first trimester of pregnancy and low birth
weight by type of study
3-2. The relationship between maternal significant (relative risk, 1.24 [95% CI:
anemia in the first trimester of 1.07 to 1.45]). That means: study that was
pregnancy and low birth weight conducted in Asia have been significancy
relationship. So in developing countries
3-2-1. By continent
maternal anemia in the first trimester
This relationship has been evaluated by 11 increases the risk of low birth weight. Chi-
studies in Asia and one in Europe. By square tests show that heterogeneity was
combining Asian studies using a random 75.1 percent and it was significant
effects model, this relationship was (P=0.000)(Figure3).
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3327
Anemia and Pregnancy outcomes: Meta-analysis
Study %
ID RR (95% CI) Weight
Europe
Hamalainen (2003) 3.14 (1.35, 7.29) 2.92
Subtotal (I-squared = .%, p = .) 3.14 (1.35, 7.29) 2.92
.
Asia
Zhou (1998) 2.96 (1.15, 7.62) 2.40
Xiong (2003) 0.75 (0.53, 1.07) 9.38
Levy (2005) 1.10 (1.05, 1.15) 17.29
Monawar (2006) 2.00 (1.18, 3.39) 5.90
Ren (2007) 1.16 (1.03, 1.30) 16.00
Kidanto (2009) 2.23 (1.44, 3.46) 7.41
Abeysena (2010) 0.56 (0.07, 4.61) 0.54
Kumar (2010) 1.02 (0.83, 1.25) 13.53
Mohamed (2012) 1.45 (1.14, 1.84) 12.57
Huang (2015) 0.61 (0.32, 1.16) 4.52
Chikjwa (2015) 2.00 (1.30, 3.09) 7.53
Subtotal (I-squared = 75.1%, p = 0.000) 1.24 (1.07, 1.45) 97.08
.
Overall (I-squared = 76.0%, p = 0.000) 1.28 (1.10, 1.50) 100.00
NOTE: Weights are from random effects analysis
.0681 1 14.7
Fig.3: The relationship between maternal anemia in the first trimester of pregnancy and low birth
weight by continent
3-2-2. By sensitivity analysis study can change overall effect of meta-
Sensitivity analysis showed that the analysis significantly. In this study as
elimination of a study can change the shown in the following Figure.4,
results or not. It shows influence studies in eliminating a study had no effect on the
meta-analysis, sometimes, elimination a overall results.
Meta-analys is es tim ates , given nam ed s tudy is om itted
Lower CI Lim it Es tim ate Upper CI Lim it
Knotherland (1990)
Zhou (1998)
Ham alainen (2003)
Xiong (2003)
Chang (2003)
Hajian (2005)
Levy (2005)
Little (2005)
Monawar (2006)
Mam un (2006)
Lee (2006)
Ren (2007)
Zhang (2009)
Kidanto (2009)
Zhang (2009)
Abeys ena (2010)
Kum ar (2010)
Sekhavat (2011)
Elena (2011)
Kum ar (2012)
Salim i (2012)
Moham ed (2012)
Gus tava (2012)
Koura (2012)
Bakacak (2014)
Yildiz (2014)
Alizadeh (2014)
Huang (2015)
Chikjwa (2015)
0.05 0.09 0.25 0.41 0.54
Fig.4: The relationship between maternal anemia in the first trimester of pregnancy and low birth
weight by sensitivity analysis
3-3. Begg’s funnel plot for the first coefficient is 0.69 at Begg’s test and is not
trimester maternal anemia relationship significant statistically (P=0. 493). Egger's
with low birth weight test also, showed that there hasn’t been
publication bias (P = 0.152) (Figure.5).
Egger test has greater power to detect
publication bias. The Kendall correlation
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3328
Rahmati et al.
Note: default data input format (theta, se_theta) assumed.
Tests for Publication Bias
Begg's Test
adj. Kendall's Score (P-Q) = 10
Std. Dev. of Score = 14.58
Number of Studies = 12
z = 0.69
Pr > |z| = 0.493
z = 0.62 (continuity corrected)
Pr > |z| = 0.537 (continuity corrected)
Egger's test
Std_Eff Coef. Std. Err. t P>|t| [95% Conf. Interval]
slope .0713501 .0475634 1.50 0.164 -.0346279 .1773281
bias 1.081983 .6971966 1.55 0.152 -.4714681 2.635433
Fig.5: Begg’s funnel plot for the first trimester maternal anemia relationship with low birth weight
3-4. The relationship between maternal This relationship was investigated by a
anemia in the second trimester of study in Asia, Europe and U.S.A, but no
pregnancy with low birth weight significant relationship was found in any
3-4-1. By type of study of the continents.
Among all the studies, two cohort studies 3-4-3. By sensitivity analysis
and a case-control study were investigated Sensitivity analysis showed that the
in this relationship. There was no elimination of a study can change the
significant relationship in these studies. results or not. In this study as shown in the
When the results were combined together following (Figer.6), eliminating a study
by using a random effects model, no had no effect on the overall results and
significant relationship was found (relative anyway relationship between maternal
risk, 1.19 [95% CI: 0.65 to 2.17]). anemia and low birth weight is significant.
3-4-2. By continent
Meta-analys is es tim ates , given nam ed s tudy is om itted
Lower CI Lim it Es tim ate Upper CI Lim it
Abeys ena (2010)
Kum ar (2010)
Kidanto (2009)
Zhang (2009)
Zhang (2009)
Ren (2007)
Lee (2006)
Mam un (2006)
Monawar (2006)
Levy (2005)
Little (2005)
Chang (2003)
Ham alainen (2003)
Zhou (1998)
Knotherland (1990)
Xiong (2003)
Hajian (2005)
Kum ar (2012)
Gus tava (2012)
Salim i (2012)
Huang (2015)
Chikjwa (2015)
Alizadeh (2014)
Bakacak (2014)
Moham ed (2012)
Sekhavat (2011)
Yildiz (2014)
Elena (2011)
Koura (2012)
-0.95 -0.43 0.17 0.77 1.00
Fig.6: The relationship between maternal anemia in the second trimester of pregnancy and low birth
weight by sensitivity analysis
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3329
Anemia and Pregnancy outcomes: Meta-analysis
3-5. The relationship between maternal didn’t show significant relationship. A
anemia in the third trimester of random effects model was used to combine
pregnancy with low birth weight the studies and showed no significant
relationship between maternal anemia in
3-5-1. By type of the study
the third trimester and low birth weight
Among 8 studies that have been examined (relative risk, 1.23 [95% CI: 0.97 to 1.55]).
this relationship, 6 cohorts (relative risk, Chi-square tests showed that the results of
1.23 [95% CI: 0.94 to 1.60]), a case- 8 studies have been heterogeneous and
control (relative risk, 1.28 [95% CI: 0.63 significant (I-squared= 70.5%, P = 0.001)
to 2.61]), and a cross-sectional (relative (Figue.7).
risk, 1.65 [95% CI: 0.17 to 15.90]) studies
Study %
ID RR (95% CI) Weight
Cohort
Chang (2003) 0.70 (0.42, 1.16) 11.88
Knotherland (1990) 4.20 (1.92, 9.19) 6.76
Xiong (2003) 0.90 (0.70, 1.15) 20.03
Huang (2015) 2.07 (1.08, 3.97) 8.75
Sekhavat (2011) 1.40 (1.05, 1.87) 18.41
Yildiz (2014) 1.08 (1.05, 1.11) 25.38
Subtotal (I-squared = 78.6%, p = 0.000) 1.23 (0.94, 1.60) 91.21
.
Case-Control
Hamalainen (2003) 1.28 (0.63, 2.61) 7.74
Subtotal (I-squared = .%, p = .) 1.28 (0.63, 2.61) 7.74
.
Cross-Sectional
Hajian (2005) 1.65 (0.17, 15.90) 1.05
Subtotal (I-squared = .%, p = .) 1.65 (0.17, 15.90) 1.05
.
Overall (I-squared = 70.5%, p = 0.001) 1.23 (0.97, 1.55) 100.00
NOTE: Weights are from random effects analysis
.0629 1 15.9
Fig.7: The relationship between maternal anemia in the third trimester of pregnancy with low birth
weight by type of the study
3-5-2. By continent The effect of heterogeneity was significant
(P= 0.032, P = 0.003) (Figer.8).
In total, there were 4 studies in Asia
(relative risk, 1.28 [95% CI: 0.86 to 1.90]), 3-5-3. By sensitivity analysis
3 studies in Europe (relative risk, 1.67 Sensitivity analysis showed that the
[95% CI: 0.79 to 3.54]), and a study in the elimination of a study can change the
U.S.A (relative risk, 0.70 [95% CI: 0.42 to results or not. It shows influence studies
1.16]) that investigated this relationship in meta-analysis, sometimes elimination a
and were found no significant relationship study can change overall effect of meta-
between any of the Continents. Chi-square analysis significantly. In this study as
tests showed that there is heterogeneity shown in the following (Figure.9),
between studies conducted in Asia and eliminating a study had no effect on the
Europe (I-squared=70. 5%, P=0. 001). overall results.
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3330
Rahmati et al.
Study %
ID RR (95% CI) Weight
Asia
Xiong (2003) 0.90 (0.70, 1.15) 20.03
Hajian (2005) 1.65 (0.17, 15.90) 1.05
Huang (2015) 2.07 (1.08, 3.97) 8.75
Sekhavat (2011) 1.40 (1.05, 1.87) 18.41
Subtotal (I-squared = 65.9%, p = 0.032) 1.28 (0.86, 1.90) 48.24
.
Europe
Hamalainen (2003) 1.28 (0.63, 2.61) 7.74
Knotherland (1990) 4.20 (1.92, 9.19) 6.76
Yildiz (2014) 1.08 (1.05, 1.11) 25.38
Subtotal (I-squared = 83.0%, p = 0.003) 1.67 (0.79, 3.54) 39.88
.
USA
Chang (2003) 0.70 (0.42, 1.16) 11.88
Subtotal (I-squared = .%, p = .) 0.70 (0.42, 1.16) 11.88
.
Overall (I-squared = 70.5%, p = 0.001) 1.23 (0.97, 1.55) 100.00
NOTE: Weights are from random effects analysis
.0629 1 15.9
Fig.8: The relationship between maternal anemia in the third trimester of pregnancy with low birth
weight by continent
Meta-analys is es tim ates , given nam ed s tudy is om itted
Lower CI Lim it Es tim ate Upper CI Lim it
Abeys ena (2010)
Kum ar (2010)
Kidanto (2009)
Zhang (2009)
Zhang (2009)
Ren (2007)
Lee (2006)
Mam un (2006)
Monawar (2006)
Levy (2005)
Little (2005)
Chang (2003)
Ham alainen (2003)
Zhou (1998)
Knotherland (1990)
Xiong (2003)
Hajian (2005)
Kum ar (2012)
Gus tava (2012)
Salim i (2012)
Huang (2015)
Chikjwa (2015)
Alizadeh (2014)
Bakacak (2014)
Moham ed (2012)
Sekhavat (2011)
Yildiz (2014)
Elena (2011)
Koura (2012)
-0.09 -0.03 0.20 0.44 0.69
Fig.9: The relationship between maternal anemia in the third trimester of pregnancy and low birth
weight by sensitivity analysis
3-6. The relationship between maternal a significant relationship (relative risk,
anemia in the first trimester of 1.26 [95% CI: 1.11 to 1.44]). Chi-square
pregnancy with preterm birth tests showed that heterogeneity between
studies is 55 percent and this moderate
In total, 9 studies were evaluated in this
heterogeneity was significant
relationship, the studies were combined
(I-squared=55%, P=0.023) (Figure.10)
using a random effects model and showed
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3331
Anemia and Pregnancy outcomes: Meta-analysis
Study %
ID RR (95% CI) Weight
Zhou (1998) 2.07 (0.80, 5.33) 1.81
Hamalainen (2003) 1.80 (0.78, 4.18) 2.25
Xiong (2003) 1.01 (0.71, 1.44) 9.83
Levy (2005) 1.20 (1.15, 1.25) 32.42
Ren (2007) 1.11 (0.99, 1.25) 26.56
Kidanto (2009) 2.30 (1.48, 3.57) 6.99
Abeysena (2010) 0.64 (0.08, 5.27) 0.38
Mohamed (2012) 1.50 (1.18, 1.90) 16.02
Huang (2015) 0.89 (0.47, 1.69) 3.72
Overall (I-squared = 55.0%, p = 0.023) 1.26 (1.11, 1.44) 100.00
NOTE: Weights are from random effects analysis
.0778 1 12.9
Fig.10: The relationship between maternal anemia in the first trimester of pregnancy with preterm
birth
3-6-1. By type of the study Studies, were investigated in this
relationship, the studies were combined
Seven cohorts (relative risk, 1.20 [95% CI:
using a random effects model and showed
1.05 to 1.39]) and two case-control
a significant relationship (P=0.023)
(relative risk, 1.52 [95% CI: 1.21 to 1.91])
(Figure.11).
Study %
ID RR (95% CI) Weight
Cohort
Zhou (1998) 2.07 (0.80, 5.33) 1.81
Xiong (2003) 1.01 (0.71, 1.44) 9.83
Levy (2005) 1.20 (1.15, 1.25) 32.42
Ren (2007) 1.11 (0.99, 1.25) 26.56
Kidanto (2009) 2.30 (1.48, 3.57) 6.99
Abeysena (2010) 0.64 (0.08, 5.27) 0.38
Huang (2015) 0.89 (0.47, 1.69) 3.72
Subtotal (I-squared = 55.2%, p = 0.037) 1.20 (1.05, 1.39) 81.73
.
Case-Control
Hamalainen (2003) 1.80 (0.78, 4.18) 2.25
Mohamed (2012) 1.50 (1.18, 1.90) 16.02
Subtotal (I-squared = 0.0%, p = 0.683) 1.52 (1.21, 1.91) 18.27
.
Overall (I-squared = 55.0%, p = 0.023) 1.26 (1.11, 1.44) 100.00
NOTE: Weights are from random effects analysis
.0778 1 12.9
Fig.11: The relationship between maternal anemia in the first trimester of pregnancy with preterm
birth by type of the study
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3332
Rahmati et al.
3-6-2. By Continent percent and this heterogeneity was
significant (I-squared=55%, P=0. 018)
One study in Europe (relative risk, 1.80
(Figure.12).
[95% CI: 0.78 to 4.18]) and 8 studies in
Asia (relative risk, 1.25 [95% CI: 1.09 to 3-7. Begg’s funnel plot
1.43]), were conducted. The studies were This plot was used to check publication
combined using a random effects model bias and showed the effect of publication
and showed a significant relationship in bias was not significant with a P-value less
Asian countries. Chi-square tests showed than 0.05 (Figure.13).
that heterogeneity between studies is 58.6
Study %
ID RR (95% CI) Weight
Europe
Hamalainen (2003) 1.80 (0.78, 4.18) 2.25
Subtotal (I-squared = .%, p = .) 1.80 (0.78, 4.18) 2.25
.
Asia
Zhou (1998) 2.07 (0.80, 5.33) 1.81
Xiong (2003) 1.01 (0.71, 1.44) 9.83
Levy (2005) 1.20 (1.15, 1.25) 32.42
Ren (2007) 1.11 (0.99, 1.25) 26.56
Kidanto (2009) 2.30 (1.48, 3.57) 6.99
Abeysena (2010) 0.64 (0.08, 5.27) 0.38
Mohamed (2012) 1.50 (1.18, 1.90) 16.02
Huang (2015) 0.89 (0.47, 1.69) 3.72
Subtotal (I-squared = 58.6%, p = 0.018) 1.25 (1.09, 1.43) 97.75
.
Overall (I-squared = 55.0%, p = 0.023) 1.26 (1.11, 1.44) 100.00
NOTE: Weights are from random effects analysis
.0778 1 12.9
Fig.12: The relationship between maternal anemia in the first trimester of pregnancy with preterm
birth by Continent
Begg's funnel plot with pseudo 95% confidence limits
2
b
-2
0 .5 1
s.e. of: b
Fig13: Begg’s funnel plot of relationship between maternal anemia in the first trimester of pregnancy
with preterm birth
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3333
Anemia and Pregnancy outcomes: Meta-analysis
3-8. The relationship between maternal anemia in the first trimester increases the
anemia in the first trimester of risk of SGA (Figure.14).
pregnancy and SGA 3-8-2. By continent
3-8-1. By type of study In total, 4 studies in Asia, a study in
Among all the studies, 5 cohort studies and Europe and a study in the U.S.A were
a case-control study were investigated in investigated this relationship. By using a
this relationship. By using a random- random-effects model, the studies were
effects model cohort studies were combined together and this relationship
combined together and this relationship was significant (relative risk, 1.12 [95%
was significant (relative risk, 1.12 [95% CI: 1.05 to 1.19]) (Figure.15).
CI: 1.05 to 1.19]). That means maternal
Study %
ID RR (95% CI) W eight
Cohort
Abeysena (2010) 0.71 (0.08, 6.33) 0.08
Ren (2007) 1.11 (1.03, 1.19) 75.46
Zhou (1998) 0.99 (0.64, 1.54) 2.04
Gustava (2012) 1.11 (0.96, 1.28) 19.36
Chikjwa (2015) 1.60 (1.08, 2.38) 2.50
Subtotal (I-squared = 0.0%, p = 0.457) 1.12 (1.05, 1.19) 99.43
Case-Control
Hamalainen (2003) 0.94 (0.41, 2.16) 0.57
Subtotal (I-squared = .%, p = .) 0.94 (0.41, 2.16) 0.57
Overall (I-squared = 0.0%, p = 0.578) 1.12 (1.05, 1.19) 100.00
NOTE: W eights are from random effects analysis
.0797 1 12.5
Fig.14: The relationship between maternal anemia in the first trimester of pregnancy and SGA by type
of study
Study %
ID RR (95% CI) Weight
Asia
Abeysena (2010) 0.71 (0.08, 6.33) 0.08
Ren (2007) 1.11 (1.03, 1.19) 75.46
Zhou (1998) 0.99 (0.64, 1.54) 2.04
Chikjwa (2015) 1.60 (1.08, 2.38) 2.50
Subtotal (I-squared = 17.4%, p = 0.304) 1.15 (0.98, 1.34) 80.08
.
Europe
Hamalainen (2003) 0.94 (0.41, 2.16) 0.57
Subtotal (I-squared = .%, p = .) 0.94 (0.41, 2.16) 0.57
.
USA
Gustava (2012) 1.11 (0.96, 1.28) 19.36
Subtotal (I-squared = .%, p = .) 1.11 (0.96, 1.28) 19.36
.
Overall (I-squared = 0.0%, p = 0.578) 1.12 (1.05, 1.19) 100.00
NOTE: Weights are from random effects analysis
.0797 1 12.5
Fig.15: The relationship between maternal anemia in the first trimester of pregnancy and SGA by
Continent
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3334
Rahmati et al.
3-9. The relationship between maternal pregnancy and PTB (relative risk, 1.35
anemia in the second trimester of [95% CI: 0.54 to 3.34, P=0.86])
pregnancy and PTB (Figure.16).
3-9-1. By type of study 3-9-2. By continent
Among all the studies, 3 cohort studies Two studies in Asia (relative risk, 1.87
(relative risk, 1.50 [95% CI: 0.51 to 4.38]), [95% CI: 0.53 to 6.65]), a study in Europe
and a case-control study (relative risk, (relative risk, 0.97 [95% CI: 0.53 to 1.78])
0.97 [95% CI: 0.53 to 1.78]) showed and a study in U.S.A (relative risk, 0.85
significant relationship. Then, by using a [95% CI: 0.31 to 2.23]) had been
random-effects model studies were conducted and showed no significant
combined together and no significant relationship in any of the Continents
relationship was observed between (Figure.17).
maternal anemia in the second trimester of
Study %
ID RR (95% CI) Weight
Cohort
Zhang (2009) 3.50 (3.03, 4.04) 27.99
Chang (2003) 0.85 (0.31, 2.33) 20.92
Huang (2015) 0.96 (0.59, 1.57) 26.05
Subtotal (I-squared = 93.6%, p = 0.000) 1.50 (0.51, 4.38) 74.96
Case-Control
Hamalainen (2003) 0.97 (0.53, 1.78) 25.04
Subtotal (I-squared = .%, p = .) 0.97 (0.53, 1.78) 25.04
Overall (I-squared = 93.2%, p = 0.000) 1.35 (0.54, 3.34) 100.00
NOTE: Weights are from random effects analysis
.228 1 4.38
Fig.16: The relationship between maternal anemia in the second trimester of pregnancy and PTB by
type of study
Study %
ID RR (95% CI) W eight
Asia
Zhang (2009) 3.50 (3.03, 4.04) 27.99
Huang (2015) 0.96 (0.59, 1.57) 26.05
Subtotal (I-squared = 96.0%, p = 0.000) 1.87 (0.53, 6.65) 54.04
Europe
Hamalainen (2003) 0.97 (0.53, 1.78) 25.04
Subtotal (I-squared = .%, p = .) 0.97 (0.53, 1.78) 25.04
USA
Chang (2003) 0.85 (0.31, 2.33) 20.92
Subtotal (I-squared = .%, p = .) 0.85 (0.31, 2.33) 20.92
Overall (I-squared = 93.2%, p = 0.000) 1.35 (0.54, 3.34) 100.00
NOTE: W eights are from random effects analysis
.15 1 6.65
Fig.17: The relationship between maternal anemia in the second trimester of pregnancy and PTB by
Continent
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3335
Anemia and Pregnancy outcomes: Meta-analysis
3-9-3. By sensitivity analysis study has no effect to the results of other
studies (Figure.18).
It showed among the studies that were
measured in this relationship, removing a
Meta-analys is es tim ates , given nam ed s tudy is om itted
Lower CI Lim it Es tim ate Upper CI Lim it
Abeys ena (2010)
Kum ar (2010)
Kidanto (2009)
Zhang (2009)
Zhang (2009)
Ren (2007)
Lee (2006)
Mam un (2006)
Monawar (2006)
Levy (2005)
Little (2005)
Chang (2003)
Ham alainen (2003)
Zhou (1998)
Knotherland (1990)
Xiong (2003)
Hajian (2005)
Kum ar (2012)
Gus tava (2012)
Salim i (2012)
Huang (2015)
Chikjwa (2015)
Alizadeh (2014)
Bakacak (2014)
Moham ed (2012)
Sekhavat (2011)
Yildiz (2014)
Elena (2011)
Koura (2012)
-0.67
-0.61 0.30 1.20 1.49
Fig.18: The relationship between maternal anemia in the second trimester of pregnancy and PTB by
sensitivity analysis
3-10. The relationship between maternal risk, 2.37 [95% CI: 1.01 to 5.57]), were
anemia in the third trimester of investigated this relationship and a
pregnancy and PTB significant relationship was observed only
in cross-sectional study (P<0.05). Overall
3-10-1. By type of study
results showed no significant relationship
Five cohort studies (relative risk, 1.44 by using a random-effects model (relative
[95% CI: 0.66 to 3.16]), a case-control risk, 1.55 [95% CI: 0.83 to 2.88])
study (relative risk, 1.53 [95% CI: 0.88 to (Figure.19).
2.65]) and a cross-sectional study (relative
Study %
ID RR (95% CI) Weight
Cohort
Zhang (2009) 2.90 (2.57, 3.27) 16.05
Chang (2003) 0.73 (0.46, 1.15) 14.86
Knotherland (1990) 2.40 (1.01, 5.68) 12.32
Xiong (2003) 0.72 (0.56, 0.92) 15.74
Huang (2015) 1.84 (1.06, 3.19) 14.33
Subtotal (I-squared = 96.7%, p = 0.000) 1.44 (0.66, 3.16) 73.29
.
Case-Control
Hamalainen (2003) 1.53 (0.88, 2.65) 14.33
Subtotal (I-squared = .%, p = .) 1.53 (0.88, 2.65) 14.33
.
Cross-Sectional
Hajian (2005) 2.37 (1.01, 5.57) 12.37
Subtotal (I-squared = .%, p = .) 2.37 (1.01, 5.57) 12.37
.
Overall (I-squared = 95.1%, p = 0.000) 1.55 (0.83, 2.88) 100.00
NOTE: Weights are from random effects analysis
.176 1 5.68
Fig.19: The relationship between maternal anemia in the third trimester of pregnancy and PTB by
type of study
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3336
Rahmati et al.
3-10-2. By Continent 3-10-3. By year of publication
Four studies in Asia (relative risk, 1.77 The size of the circle shows the sample
[95% CI: 0.71 to 4.11]), two studies in size. Whatever sample size is large, the
Europe (relative risk, 1.74 [95% CI: 1.10 size of the circle is bigger and the
to 2.77]), and a study in U.S.A (relative regression equation was estimated as: y = -
risk, 0.73 [95% CI: 0.46 to 1.15]) had 18.61 + 0.0094x. Since, P=0.81 was
investigated this relationship and was estimated for the slope of the line. It was
found a significant relationship only in concluded that there was no significant
Europe (P<0.05). Overall results by using relationship between article's publication
random-effects model showed no year and effect size (Figure.21).
significant relationship (relative risk, 1.55
[95% CI: 0.88 to 2.88]) (Figure.20).
Study %
ID RR (95% CI) Weight
Asia
Zhang (2009) 2.90 (2.57, 3.27) 16.05
Xiong (2003) 0.72 (0.56, 0.92) 15.74
Hajian (2005) 2.37 (1.01, 5.57) 12.37
Huang (2015) 1.84 (1.06, 3.19) 14.33
Subtotal (I-squared = 97.0%, p = 0.000) 1.71 (0.71, 4.11) 58.48
.
Europe
Hamalainen (2003) 1.53 (0.88, 2.65) 14.33
Knotherland (1990) 2.40 (1.01, 5.68) 12.32
Subtotal (I-squared = 0.0%, p = 0.388) 1.74 (1.10, 2.77) 26.65
.
USA
Chang (2003) 0.73 (0.46, 1.15) 14.86
Subtotal (I-squared = .%, p = .) 0.73 (0.46, 1.15) 14.86
.
Overall (I-squared = 95.1%, p = 0.000) 1.55 (0.83, 2.88) 100.00
NOTE: Weights are from random effects analysis
.176 1 5.68
Fig.20: The relationship between maternal anemia in the third trimester of pregnancy and PTB by
Continent
3
2
lnrr1
1
0
-1
1990 1995 2000 2005 2010 2015
Date of Publication
Fig.21: The relationship between maternal anemia in the third trimester of pregnancy and PTB by
year of publication
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3337
Anemia and Pregnancy outcomes: Meta-analysis
3-10-4. By sensitivity analysis results or not. In this study as shown in the
following (Figer.22), eliminating a study
Sensitivity analysis showed that the
had no effect on the overall results.
elimination of a study can change the
Meta-analys is es tim ates , given nam ed s tudy is om itted
Lower CI Lim it Es tim ate Upper CI Lim it
Abeys ena (2010)
Kum ar (2010)
Kidanto (2009)
Zhang (2009)
Zhang (2009)
Ren (2007)
Lee (2006)
Mam un (2006)
Monawar (2006)
Levy (2005)
Little (2005)
Chang (2003)
Ham alainen (2003)
Zhou (1998)
Knotherland (1990)
Xiong (2003)
Hajian (2005)
Kum ar (2012)
Gus tava (2012)
Salim i (2012)
Huang (2015)
Chikjwa (2015)
Alizadeh (2014)
Bakacak (2014)
Moham ed (2012)
Sekhavat (2011)
Yildiz (2014)
Elena (2011)
Koura (2012)
-0.30 -0.19 0.44 1.06 1.23
Fig.22: The relationship between maternal anemia in the third trimester of pregnancy and PTB by
sensitivity analysis
4- DISCUSSION shown that significant relationships have
been observed more in studies with larger
The present study is a systematic
sample sizes, in pregnant women with
review and meta-analysis about
anemia in the first trimester. LBW and
hemoglobin concentration and pregnancy
PTB have been found in most of the
outcomes in the world that showed how
studies and significant relationship was
much effect maternal anemia has on
observed more in developing countries like
pregnancy outcomes. Nowadays, maternal
Asian countries. Similar Meta-analysis
anemia is considered as a public health
study had been conducted by Sukrat in
problem in the world, especially in
2013, showed that hemoglobin less than 11
developing countries. For example, the
g/dl in the first trimester is a risk factor for
prevalence of anemia among pregnant
LBW (relative risk, 1.14 [95% CI: 1.05 to
women is 52 percent in developing
1.24]), PTB (relative risk, 1.10 [95%
countries and 22.5 percent in developed
CI:1.02 to 1.19]) and SGA (relative risk,
countries (5). In this study the relationship
1.17 [95% CI: 1.03 to 1.33]) (53).
between hemoglobin concentrations and
pregnancy outcomes was investigated by This finding is consistent with the results
the type of study, year of publication, of this study. This study showed that
country, continent, sample size and by the maternal anemia in the third trimester has
trimesters of pregnancy. The result showed no significant relationship with the risk of
that maternal anemia in the first trimester LBW (relative risk, 1.23 [95% CI: 0.97 to
of pregnancy has a significant relationship 1.55]). Although, it can be said that
with LBW, PTB and SGA that means maternal anemia in the third trimester
maternal anemia in the first trimester could be a borderline risk for LBW but, it
increases the risk of these outcomes. Also, wasn't consistent with Sukrat study that
it was shown that maternal anemia in the showed maternal anemia in the third
second and the third trimester has no trimester increasing the risk of LBW
significant relationship with LBW and (relative risk, 1.30 [95% CI 1.08 to 1.58])
PTB. The analysis of sub-groups was (53).
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3338
Rahmati et al.
Another review study had been conducted Hereby deputy university of Ilam medical
by Ahankari about maternal hemoglobin science from professors who with their
and low birth weight in 2015. The finding guidance of helped us and all of
is consistent with our results (54). In a individuals who cooperated in the
subgroup analysis, the present study implementation of the plan our fullest
showed that this relationship is observed appreciation and give thanks.
more in developing countries that were
consistent with other study results (54-56). 8- REFERENCES
4-1. Limitations of the study 1. Kisioglu NN, Ozturk M, Cakmak ZA,
Ozguner F. Anemia prevalence and its
1. Inability of domestic and international affecting factors in pregnant women of Isparta
databases for searching the combined Province. Biomed Res 2004; 16(1):11-4.
keywords, combination keywords cannot
2. Kabiri AA, Sheioleslam H. Prevalence of
be used.
iron deficiency anemia in women who referred
2. Anemia is defined differently in various to Qazvin public health center. J Qazvin Univ
studies. Med Sci 1999; 3(1):62-6. (Persian).
3. The majority of studies have been
conducted in Asian countries. 3. Steketee RW, Nahlen BL, Parise ME,
Menendez C. The burden of malaria in
4. Some studies were excluded due to:
pregnancy in malaria-endemic areas. Am J
Poor quality such as studies with a Trop Med Hyg 2001; 64(1-2 Suppl):28-35.
small sample size; 4. Sayehmiri K, Darvishi K, Azami M.
Not identifying the months of Helicobacter pylori infection is associated with
pregnancy; anemia in pregnant women-a meta-analysis
Publication bias; study. Iran J Med Microbiol 2015; 9(1):1-5.
Inadequate data; 5. Morrone A, Nosotti L, Piombo L, Scardella
Failure to report particular P, Spada R, Pitidis A. Iron deficiency anaemia
outcome; prevalence in a population of immigrated
Definition of outcome was not women in Italy. European Journal of Public
clear; Health 2010; 22(2): 256–62.
Medical theses. 6. Bukar MM, Audu BM, Yahaya UR,
MelahGS.Anaemia in pregnancy at booking in
5- CONCLUSION Gombe, North-eastern Nigeria. J
The study showed that hemoglobin ObstetGynaecol 2008; 28(8): 775–78.
below11g/dl increases the risk of LBW, 7. Hyder SMZ, Persson LA, Chowdhury M,
PTB and SGA in the first trimester that Lo¨nnerdal B, Ekstrom EC. Anaemia and iron
this relationship observed more in deficiency during pregnancy in rural
developing countries. But, this relationship Bangladesh. Public Health Nutr 2004; 7(8):
(maternal anemia and pregnancy outcome) 1065–70.
in the second and third trimester of 8. World Health Organization. World Health
pregnancy was not significant. Report 1997. Conquering Suffering, Enriching
So, maternal anemia during pregnancy in Humanity. Geneva: World Health
the first trimester in particular, can be Organization, 1998.
considered as a risk factor for pregnancy 9. Sayehmiri K, Darvishi Z, Azami M, Qavam
outcomes and should be treated as S. The prevalence of anemia in the first
advance. quarter, the second and third pregnancy a
systematic review and meta-analysis. Iran J of
6- CONFLICT OF INTEREST: None. med Midwifery and Women Mashhad 2015;
7- ACKNOWLEDGMENT 168(18): 7-15.
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3339
Anemia and Pregnancy outcomes: Meta-analysis
10. Lowdermilk DL, Perry SE. Maternity & 21. Chang SC, O’Brien KO, Nathanson MS,
woman’s health care. 8th ed. St Louis: Mosby; Mancini J, Witter FR. Hemoglobin
2004. P.1219. concentrations influence birth outcomes in
pregnant African-American adolescents.
11. Cunningham FG, Leveno KJ, Bloom SL,
Journal of Nutrition 2003; 133(7): 2348–55.
Hauth JC, Gilstrap III L, Wenstrom KD.
Williams obstetrics. 22nd ed. Philadelphia: 22. Abeysena C, Jayawardana P, Seneviratne
McGraw-Hill; 2005:1143-67. A R. Maternal haemoglobin level at booking
visit and its effect on adverse pregnancy
12. Xiong X, Buekens P, Fraser WD, Guo Z.
outcome. Australian and New Zealand Journal
Anemia during pregnancy in a Chinese
of Obstetrics and Gynaecology 2010; 50(5):
population.Int J Gynaecol Obstet 2003; 83:
423–27.
159–64.
23. Kumar A, Chaudhary K, Prasad S.
13. Shobeiri F, Begum K, Nazari M. A
Maternal indicators and obstetric outcome in
prospective study of maternal hemoglobin
the north Indian population: a hospital- based
status of Indian women during pregnancy and
study. Journal of Postgraduate Medicine 2010;
pregnancy outcome.Nutr Res 2006; 26: 209–
56(3): 192–95.
13.
24. Kidanto H L, Mogren I, Lindmark G,
14. Marchant T, Schellenberg JA, Nathan R et
Massawe SN, Nystrom L. Risks for preterm
al. Anaemia in pregnancy and infant mortality
delivery and low birth weight are
in Tanzania. Trop Med Int Health 2004; 2:
independently increased by severity of
262–66
maternal anaemia. South African Medical
15- UNICEF. Malnutrition in South Asia: A Journal 2009; 99(2): 98–102.
Regional Profile. Kathmandu: UNICEF; 1997.
25. Zhang Q, Ananth CV, Li Z, Smulian JC.
16. Hamalainen H, Hakkarainen K, Heinonen Maternal anaemia and preterm birth: a
S. Anaemia in the first trimester bur not in the prospective cohort study. International Journal
second trimester is a risk factor for low birth of Epidemiology 2009; 38(5): 1380–89.
weight. Clin Nutr 2003; 22 (3): 271–75.
26. Zhang Q, Ananth CV, Rhoads GG, Li Z.
17. Mamun AA, Padmadas SS, Khatun M. The impact of maternal anemia on perinatal
Maternal health during pregnancy and mortality: a population-based, prospective
perinatal mortality in Bangladesh: evidence cohort study in China. Annals of
from a large-scale community-based clinical Epidemiology 2009; 19(11): 793–99.
trial. Paediatricand Perinatal Epidemiology
27. Ren A, Wang J, Ye RW, Li S, Liu J M, Li
2006; 20(6): 482–90.
Z. Low first trimester hemoglobin and low
18. Levy A, Fraser D, Katz M, Mazor M, birth weight, preterm birth and small for
Sheiner E. Maternal anemia during is an gestational age newborns. International
independent risk factor for low birthweight Journal of Gynecology and Obstetrics 2007;
and preterm delivery. Eur J 98(2): 124–28.
ObstetGynecolReprodBiol 2005; 122: 182–86.
28. Lee HS, Kim MS, Kim MH, Kim YJ, Kim
19. Scanlon K, Yip R, Schieve LA, Cogswell WY. Iron status and its association with
ME. High and lowhemoglobin levels during pregnancy outcome in Korean pregnant
pregnancy: differential risks for preterm birth women. European Journal of Clinical Nutrition
and small for gestational age. ObstetGynecol 2006; 60(9): 1130–35.
2000; 96: 741–47.
29. Brabin BJ, Hakimi M, Pelletier D. An
20. Scalon KS, Yip R, Schieve LA, Congwell analysis of anemia and pregnancy-related
SE. Hiegh and low hemoglobin levels during maternal mortality. Journal of Nutrition 2001;
pregnancy : different risk for preterm birth and 131(2): 604-614.
small for gestation age obstetcynecol 2000;
30. Monawar Hosain GM, Chatterjee N,
96(5): 741-48
Begum A, Saha SC. Factors associated with
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3340
Rahmati et al.
low birthweight in rural Bangladesh. Journal Gynecologica Scandinavica 1993; 72(4): 246–
of Tropical Pediatrics 2006; 52(2): 87–91. 51.
31. Levy A, Fraser D, Katz M, Mazor M, 40. Knottnerus JA, Delgado LR, Knipschild
Sheiner E. Maternal anemia during pregnancy PG, Essed G GM, Smits F. Haematologic
is an independent risk factor for low birth parameters and pregnancy outcome.
weight and preterm delivery. European Journal Aprospective cohort study in the third
of Obstetrics Gynecology and Reproductive trimester. Journalof Clinical Epidemiology
Biology 2005; 122(2): 182–86. 1990; 43(5): 461–66.
32. Ronnenberg AG, Wood RJ, Wang X. 41. Kumar KJ, Asha1 N, Srinivasa D, Sujatha2
Preconception hemoglobin and ferritin MS, Manjunath VG. Maternal Anemia in
concentrations are associated with pregnancy Various Trimesters and its Effect on Newborn
outcome in a prospective cohort of Chinese Weight and Maturity: An Observational Study.
women. Journal of Nutrition 2004; 134(10): International Journal of Preventive Medicine
2586–91. 2013; 4(2): 193-9.
33. Chang SC, O’Brien KO, Nathanson MS, 42. Gustavo F, Tapia V, Gasco M, Carlos EC.
Mancini J, Witter FR. Hemoglobin Maternal hemoglobin concentration and
concentrations influence birth outcomes in adverse pregnancy outcomes at low and
pregnant African-American adolescents. moderate altitudes in Peru. The Journal of
Journal of Nutrition 2003; 133(7): 2348–55. Maternal-Fetal and Neonatal Medicine 2012;
25(7): 1105–10.
34. Hamalainen H, Hakkarainen K, Heinonen
S. Anaemia in the first but not in the second or 43. Huang L, Purvarshi G, Wang S, Zhong L,
third trimester is a risk factor for low birth Tang H. The Influence of Iron-deficiency
weight. Clinical Nutrition 2003; 22(3): 271– Anemia during the Pregnancy on Preterm
75. Birth and Birth Weight in South China.
Journal of Food and Nutrition Research 2015:
35. Xiong X, Buekens P, Fraser W. D, Guo Z.
3(9): 570-74.
Anemia during pregnancy in a Chinese
population. International Journal of 44. Jwa SC, Fujiwara T, Yamanobe Y, Kozuka
Gynecology and Obstetrics 2003; 83(2): 159– K, Sago H. Changes in maternal hemoglobin
64. during pregnancy and birth outcomes. BMC
pregnancy and childbirth. 2015 Apr 2; 15(1):
36. Mart A, Pe˜na-Mart G, Mu˜noz S, Lanas F,
1-10.
Comunian G. Association between prematurity
and maternal anemia in Venezuelan pregnant 45. Alizadeh L, Raoofi A, Salehi L, Ramzi M.
women during third trimester at labor. Impact of Maternal Hemoglobin Concentration
Archivos Latinoamericanos de Nutricion 2001; on Fetal Outcomes in Adolescent Pregnant
51(1): 44– 8. Women. Iran Red Crescent Med J 2014; 16(8):
1-5.
37. Zhou LM, Yang WW, Hua JZ, Deng CQ,
Tao X, Stoltzfus RJ. Relation of hemoglobin 46. Bakacak M, Avci F, Ercan O, Köstü B,
measured at different times in pregnancy to Serin S, Kiran G, Bostanci MS, Bakacak Z.
preterm birth and low birth weight in The effect of maternal hemoglobin
Shanghai, China. The American Journal of concentration on fetal birth weight according
Epidemiology 1998; 148(10): 998–1006. to trimesters. The Journal of Maternal-Fetal &
Neonatal Medicine 2015; 28(17): 2106-10.
38. Moher D, Liberati A, Tetzlaff J, Altman
DG. Preferred reporting items for systematic 47. Mohamed MA, Ahmad T, Macri C, Aly
reviews and meta-analyses: the PRISMA H. Racial disparities in maternal hemoglobin
statement. J Clinical Epidemiology 2009; concentrations and pregnancy outcomes. J
62(10):1006-12. Perinat Med 2012:40: 141–49.
39. Rasmussen S, Oian P. First- and second- 48. Sekhavat L, Davar R, Hosseinidezoki S.
trimester hemoglobin levels. Relation to birth Relationship between maternal hemoglobin
weight and gestational age. Acta Obstetriciaet
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3341
Anemia and Pregnancy outcomes: Meta-analysis
concentration and neonatal birth weight. Okascharoen C, Attia J, et al. Hemoglobin
Hematology 2011; 16(6): 373-76. concentration and pregnancy outcomes: a
systematic review and meta-analysis. BioMed
49. Yildiz Y, Ozgu E, Unlu SB, Salman B,
research international 2013; 2013: 1-9.
YaparEyi EG. The relationship between third
trimester maternal hemoglobin and birth 54. Ahankari A, Leonardi-Bee J. Maternal
weight/length; results from the tertiary center hemoglobin and birth weight: systematic
in Turkey. J Matern F, et al. Neonatal Med review and meta-analysis. International
2014; 27(7): 729–32. Journal 2015; 4(4):435-45.
50. Chumak E L, Grjibovski A M. Association 55. Ellis M, ManandharN, Manandhar DS,
between different levels of hemoglobin in Costelloand AM. Risk factors for neonatal
pregnancy and pregnancy outcomes: a encephalopathy in Kathmandu, Nepal, a
registry-based study in Northwest Russia. developing country: unmatched case-control
International Journal of Circumpolar Health study. British Medical Journal 2000;
2011; 70(5): 457-59. 320(7244): 1229–36.
51. Koura G K, Ouedraogo S, Le Port A, 56. PetersH R, Vince J D, Friesen H. Low
Watier L, Cottrell G, Guerra J, et al. Anaemia birth weight at a Papua New Guinea Highlands
during pregnancy: impact on birth outcome Hospital. Journal of Tropical Pediatrics 2001;
and infant haemoglobin level during the first 47(1): 17–23.
18 months of life. Tropical Medicine and
International Health 2012; 17(3): 283-91. 57. Azami M, Darvishi Z, Sayehmiri K.
Systematic Review and Meta-Analysis of
52. Onadeko MO, Avokey F, Lawoyin TO. the Prevalence of Anemia among Pregnant
Observations of stillbirths, birth weight and Iranian Women (2005 - 2015). Shiraz E-
maternal haemoglobin in teenage pregnancy in
Medical Journal 2016; 17(4-5): e38462.
Ibadan, Nigeria. African Journal of Medicine
and Medical Sciences 1996; 25(1): 81–6. 58. Jehan I, McClure EM, Salat S. Stillbirths
in an urban community in Pakistan. The
53. Sukrat B, Wilasrusmee C,
American Journal of Obstetrics and
Siribumrungwong B, McEvoy M,
Gynecology2007;197(3):257–58.
Int J Pediatr, Vol.4, N.8, Serial No.32, Aug 2016 3342
You might also like
- Mathematics For Machine LearningDocument417 pagesMathematics For Machine LearningLê Mạnh94% (32)
- Anemia Dengan BBLRDocument10 pagesAnemia Dengan BBLRAnonymous 0Mnt71No ratings yet
- The Relationship Between Maternal Anemia During Pregnancy With Preterm Birth: A Systematic Review and Meta-AnalysisDocument12 pagesThe Relationship Between Maternal Anemia During Pregnancy With Preterm Birth: A Systematic Review and Meta-AnalysisYosi Puput MaharaniNo ratings yet
- Prevalence, Types and Determinants of Anemia Among Pregnant Women in Sudan: A Systematic Review and Meta-AnalysisDocument9 pagesPrevalence, Types and Determinants of Anemia Among Pregnant Women in Sudan: A Systematic Review and Meta-AnalysisAjay DNo ratings yet
- 9 JurnalDocument83 pages9 JurnalWanda AndiniNo ratings yet
- 155 ArticleText 415 1 10 20180808Document14 pages155 ArticleText 415 1 10 20180808Bunga JuwitaNo ratings yet
- Predictive Factors For Preeclampsia in Pregnant Women: A Unvariate and Multivariate Logistic Regression AnalysisDocument5 pagesPredictive Factors For Preeclampsia in Pregnant Women: A Unvariate and Multivariate Logistic Regression AnalysisTiti Afrida SariNo ratings yet
- Maternal Anemia and Risk of Adverse Birth and Health Outcomes in Low-And Middle-Income Countries: Systematic Review and Meta-AnalysisDocument10 pagesMaternal Anemia and Risk of Adverse Birth and Health Outcomes in Low-And Middle-Income Countries: Systematic Review and Meta-AnalysisCarlos GonzalesNo ratings yet
- HB Level (Workers and Non-Workers) Who Perform Antenatal Examination at Puskesmas. Final Assignment, Diploma 4 Program OccupationalDocument1 pageHB Level (Workers and Non-Workers) Who Perform Antenatal Examination at Puskesmas. Final Assignment, Diploma 4 Program OccupationalNindia SetyaningrumNo ratings yet
- A Study On Risk of Twin Pregnancy: Mahita Reddy A., Madhavi KSS., NiharicaDocument7 pagesA Study On Risk of Twin Pregnancy: Mahita Reddy A., Madhavi KSS., NiharicaElissa IsdasariNo ratings yet
- Pediatrics-2011-Hauck-Peds 2010-3000Document10 pagesPediatrics-2011-Hauck-Peds 2010-3000api-285797257No ratings yet
- Prevalence and Determinants of Anemia in Pregnancy, Sana'a, YemenDocument8 pagesPrevalence and Determinants of Anemia in Pregnancy, Sana'a, YemenIJPHSNo ratings yet
- Prasetya Lestari-R1111029Document8 pagesPrasetya Lestari-R1111029Theresia SulistyaningrumNo ratings yet
- Chapter 3Document32 pagesChapter 3Vaibhav JainNo ratings yet
- Review (Astuti, 2022)Document10 pagesReview (Astuti, 2022)melody tuneNo ratings yet
- Maternal Anemia and Low Birth Weight A Systematic Review and Meta-AnalysisDocument17 pagesMaternal Anemia and Low Birth Weight A Systematic Review and Meta-AnalysisAdib FraNo ratings yet
- 247-Article Text-1425-1-10-20200122Document11 pages247-Article Text-1425-1-10-20200122Gisela M SilvaNo ratings yet
- Running Head: Integrative Literature Review 1Document21 pagesRunning Head: Integrative Literature Review 1api-483044745No ratings yet
- JFRH 7 139 PDFDocument6 pagesJFRH 7 139 PDFClaudya TamaNo ratings yet
- Integrative Review of The LiteratureDocument17 pagesIntegrative Review of The Literatureapi-507789841No ratings yet
- Safety and Efficacy of Enoxaparin in Pregnancy: A Systematic Review and Meta-AnalysisDocument14 pagesSafety and Efficacy of Enoxaparin in Pregnancy: A Systematic Review and Meta-AnalysisChicinaș AlexandraNo ratings yet
- Pediatrics 2014Document14 pagesPediatrics 2014Randy PrayogoNo ratings yet
- The Safety of Proton Pump Inhibitors (Ppis) in Pregnancy: A Meta-AnalysisDocument5 pagesThe Safety of Proton Pump Inhibitors (Ppis) in Pregnancy: A Meta-AnalysisSilvia AryaniNo ratings yet
- Running Head: Integrative Literature Review 1Document18 pagesRunning Head: Integrative Literature Review 1api-433880230No ratings yet
- 33873-Article Text-121761-1-10-20170831Document6 pages33873-Article Text-121761-1-10-20170831AnggaNo ratings yet
- The Relationship Between Hemoglobin and Hematocrit in The First Trimester of Pregnancy and The Incidence of PreeclampsiaDocument3 pagesThe Relationship Between Hemoglobin and Hematocrit in The First Trimester of Pregnancy and The Incidence of PreeclampsiaBaru Chandrasekhar RaoNo ratings yet
- Knowledge, Attitude and Practice Related To Iron Deficiency Anemia Among Women of Child Bearing Age, Khartoum, SudanDocument7 pagesKnowledge, Attitude and Practice Related To Iron Deficiency Anemia Among Women of Child Bearing Age, Khartoum, SudanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 10 1111@jog 143436777777Document17 pages10 1111@jog 143436777777Epiphany SonderNo ratings yet
- Clinical Risk Factors For Pre-Eclampsia Determined in Early Pregnancy: Systematic Review and Meta-Analysis of Large Cohort StudiesDocument33 pagesClinical Risk Factors For Pre-Eclampsia Determined in Early Pregnancy: Systematic Review and Meta-Analysis of Large Cohort StudiesMirza JuandaNo ratings yet
- Jurnal Epilepsi 1Document20 pagesJurnal Epilepsi 1Titi SulistiowatiNo ratings yet
- The Correlation Between Hemoglobin Concentration During Pregnancy With The Maternal and Neonatal OutcomeDocument5 pagesThe Correlation Between Hemoglobin Concentration During Pregnancy With The Maternal and Neonatal OutcomeKhrisna AdjiNo ratings yet
- 80 (11) 871 1 PDFDocument5 pages80 (11) 871 1 PDFMahlina Nur LailiNo ratings yet
- Icosh Bahasa InggrisDocument13 pagesIcosh Bahasa InggrisUtari ErmawatiNo ratings yet
- Cesarean Section and The Risk of SDRDocument15 pagesCesarean Section and The Risk of SDRAnapaolaNo ratings yet
- Jurnal Intern 2Document7 pagesJurnal Intern 2Annisaa AndrianaNo ratings yet
- Anxiety During Pregnancy and Preeclampsia - A Case-Control StudyDocument9 pagesAnxiety During Pregnancy and Preeclampsia - A Case-Control StudyJOHN CAMILO GARCIA URIBENo ratings yet
- Literature Review Anaemia in PregnancyDocument7 pagesLiterature Review Anaemia in Pregnancyafmzmxkayjyoso100% (1)
- Literature Review On Anaemia in PregnancyDocument4 pagesLiterature Review On Anaemia in Pregnancyc5qp29ca100% (2)
- Effect of Low Birth Weight On Childhood Asthma: A Meta-AnalysisDocument8 pagesEffect of Low Birth Weight On Childhood Asthma: A Meta-Analysisnavali rahmaNo ratings yet
- Faktor-Faktor Yang Berhubungan Dengan Terjadinya PreeklampsiaDocument13 pagesFaktor-Faktor Yang Berhubungan Dengan Terjadinya PreeklampsiaSetiaty PandiaNo ratings yet
- The Incidence of Respiratory Distress Syndrome Among Preterm Infants Admitted To Neonatal Intensive Care Unit: A Retrospective StudyDocument6 pagesThe Incidence of Respiratory Distress Syndrome Among Preterm Infants Admitted To Neonatal Intensive Care Unit: A Retrospective StudyImin BuntaraNo ratings yet
- InformaciónDocument6 pagesInformaciónVIOLETA JACKELINE ARMAS CHAVEZNo ratings yet
- Screening and Treatment For Iron Deficiency Anemia in Women: Results of A Survey of Obstetrician-GynecologistsDocument7 pagesScreening and Treatment For Iron Deficiency Anemia in Women: Results of A Survey of Obstetrician-GynecologistsQonita RachmahNo ratings yet
- Pregnancy and Childbirth Outcomes Among Adolescent Mothers: A World Health Organization Multicountry StudyDocument9 pagesPregnancy and Childbirth Outcomes Among Adolescent Mothers: A World Health Organization Multicountry StudyMahyudin SimarokoNo ratings yet
- Running Head: LITERATURE REVIEW 1Document23 pagesRunning Head: LITERATURE REVIEW 1api-404271262No ratings yet
- Original ArticleDocument8 pagesOriginal ArticleFelicia DympnaNo ratings yet
- Perinatal Asphyxia and Its Associated Factors in Ethiopia: A Systematic Review and Meta-AnalysisDocument11 pagesPerinatal Asphyxia and Its Associated Factors in Ethiopia: A Systematic Review and Meta-AnalysisFatmaNo ratings yet
- 3.inka Puty Larasati-Arief Wibowo (Volume 1 Nomor 1)Document6 pages3.inka Puty Larasati-Arief Wibowo (Volume 1 Nomor 1)elda zulkarnainNo ratings yet
- Anemia 11Document16 pagesAnemia 11deni dianawatiNo ratings yet
- ANEMIA Edited 1Document11 pagesANEMIA Edited 1mnri46180No ratings yet
- Jurnal Risk FX SepsisDocument7 pagesJurnal Risk FX SepsiswilmaNo ratings yet
- Jurnal 2 AnemiaDocument3 pagesJurnal 2 AnemiaAyoek Iku WahyuniNo ratings yet
- Pregnancy Outcomes Following in Utero Exposure To Lamotrigine A Systematic Review and Meta AnalysisDocument12 pagesPregnancy Outcomes Following in Utero Exposure To Lamotrigine A Systematic Review and Meta AnalysisBagusHibridaNo ratings yet
- Integrative Review of The Literature Angela JacksonDocument18 pagesIntegrative Review of The Literature Angela Jacksonapi-606742390No ratings yet
- Health Behaviors of Primigravida TeenagersDocument6 pagesHealth Behaviors of Primigravida TeenagersAubrey UniqueNo ratings yet
- P H A R M A C e U T I C A L S C I e N C e SDocument7 pagesP H A R M A C e U T I C A L S C I e N C e SBaru Chandrasekhar RaoNo ratings yet
- Taiwanese Journal of Obstetrics & GynecologyDocument10 pagesTaiwanese Journal of Obstetrics & GynecologyAdriani HartantoNo ratings yet
- 1 PBDocument8 pages1 PBFitaNo ratings yet
- Faktor Pencegah AnemiaDocument7 pagesFaktor Pencegah AnemiamustikadewipaneNo ratings yet
- Prevalence and Determinants of Hypertensive Disorders of Pregnancy in Ethiopia: A Systematic Review and Meta-AnalysisDocument21 pagesPrevalence and Determinants of Hypertensive Disorders of Pregnancy in Ethiopia: A Systematic Review and Meta-AnalysisBADLISHAH BIN MURAD MoeNo ratings yet
- Contraception for the Medically Challenging PatientFrom EverandContraception for the Medically Challenging PatientRebecca H. AllenNo ratings yet
- Body Position and Obstructive Sleep Apnea in Children: Sleep-Related Breathing DisordersDocument6 pagesBody Position and Obstructive Sleep Apnea in Children: Sleep-Related Breathing DisordersAnonymous 0Mnt71No ratings yet
- Jurnal 3Document7 pagesJurnal 3Anonymous 0Mnt71No ratings yet
- 1 SM PDFDocument7 pages1 SM PDFAnonymous 0Mnt71No ratings yet
- Anemia Dengan BBLRDocument10 pagesAnemia Dengan BBLRAnonymous 0Mnt71No ratings yet
- Author, Tempat Tahun Judul Metode Hasil KomentarDocument1 pageAuthor, Tempat Tahun Judul Metode Hasil KomentarAnonymous 0Mnt71No ratings yet
- Tobacco Use: Lead AgencyDocument18 pagesTobacco Use: Lead AgencyAnonymous 0Mnt71No ratings yet
- Jurnal 5Document10 pagesJurnal 5Anonymous 0Mnt71No ratings yet
- Results of A Pilot Diabetes Prevention Intervention in East Harlem, New York City: Project HEEDDocument9 pagesResults of A Pilot Diabetes Prevention Intervention in East Harlem, New York City: Project HEEDAnonymous 0Mnt71No ratings yet
- Author, Tempat Tahun Judul Metode Hasil KomentarDocument1 pageAuthor, Tempat Tahun Judul Metode Hasil KomentarAnonymous 0Mnt71No ratings yet
- Jurnal 9Document10 pagesJurnal 9Anonymous 0Mnt71No ratings yet
- Jurnal 12Document22 pagesJurnal 12Anonymous 0Mnt71No ratings yet
- Jurnal 7Document9 pagesJurnal 7Anonymous 0Mnt71No ratings yet
- Jurnal 8Document10 pagesJurnal 8Anonymous 0Mnt71No ratings yet
- Acute Respiratory Distress Syndrome: Dewi Kartikawati NDocument29 pagesAcute Respiratory Distress Syndrome: Dewi Kartikawati NAnonymous 0Mnt71No ratings yet
- WHD InfographicDocument2 pagesWHD InfographicAnonymous 0Mnt71No ratings yet
- Module 11: Ipv4 Addressing: Introduction To Networks V7.0 (Itn)Document58 pagesModule 11: Ipv4 Addressing: Introduction To Networks V7.0 (Itn)Diana YacchiremaNo ratings yet
- 2013 Post Promo Exam TimetableDocument5 pages2013 Post Promo Exam Timetablemin95No ratings yet
- Coupled LinesDocument10 pagesCoupled LinesFatih TokgözNo ratings yet
- CS3691 Embedded and Iot Lab ManualDocument128 pagesCS3691 Embedded and Iot Lab Manualbalabasker50% (4)
- Control System ComponentsDocument29 pagesControl System Componentsshreemanti0% (1)
- User Instructions: Domestic Garage Door OperatorsDocument16 pagesUser Instructions: Domestic Garage Door OperatorsJack Smith100% (1)
- GN CFD I8 3015c 6000w Raycus Technical SolutionDocument23 pagesGN CFD I8 3015c 6000w Raycus Technical SolutionigorNo ratings yet
- Trigonometry Solid Mensuration SolutionDocument34 pagesTrigonometry Solid Mensuration SolutionVia AnapiNo ratings yet
- Recurrencua 2Document2 pagesRecurrencua 2CarlosNo ratings yet
- Abundance of Chemical Elements in The Continental Crust: A New TableDocument13 pagesAbundance of Chemical Elements in The Continental Crust: A New TableVictor Alejandro Faundez Olivos100% (1)
- Application ListDocument30 pagesApplication ListMario AlcazabaNo ratings yet
- Toc Recursive Function TheoryDocument83 pagesToc Recursive Function TheoryTaqi Shah100% (1)
- Lecture - 1Document46 pagesLecture - 1Melaku MehandisNo ratings yet
- Perfect Score SBP Fizik SPM 2011 QuestionDocument53 pagesPerfect Score SBP Fizik SPM 2011 QuestionSamion AwaldinNo ratings yet
- Mobile Wimax: Sector Antenna Installation ManualDocument17 pagesMobile Wimax: Sector Antenna Installation ManualjbonvierNo ratings yet
- 401b Intro To Atom Presentation NotesDocument16 pages401b Intro To Atom Presentation Notes28veralNo ratings yet
- Angular Measurement - Phan Van HanDocument24 pagesAngular Measurement - Phan Van Han손종인No ratings yet
- Matrices & Determinants - Practice Sheet - Varun JEE Advanced 2024Document5 pagesMatrices & Determinants - Practice Sheet - Varun JEE Advanced 2024shikharvashishtha1729No ratings yet
- 07 - SELinuxDocument46 pages07 - SELinuxridaNo ratings yet
- Chapter 2Document50 pagesChapter 2mopliqNo ratings yet
- A Load Cluster Management System Using SNMP and WebDocument31 pagesA Load Cluster Management System Using SNMP and WebgamezzzzNo ratings yet
- General AnesthesiaDocument2 pagesGeneral AnesthesiadhaineyNo ratings yet
- Configuring Tomcat To Work With IISDocument3 pagesConfiguring Tomcat To Work With IISWill Wolff-MyrenNo ratings yet
- With The Growth of Hard Rock CafeDocument1 pageWith The Growth of Hard Rock Cafekevin johnsNo ratings yet
- Topographic Map of MaypearlDocument1 pageTopographic Map of MaypearlHistoricalMapsNo ratings yet
- Hydril 533Document4 pagesHydril 533Fernando OlaveoNo ratings yet
- Bosch Motorsport Catalog 2012 PDFDocument377 pagesBosch Motorsport Catalog 2012 PDFКонстантин МакаровNo ratings yet
- Automatic Mains Failure Unit: DKG-545 User Manual V-11Document87 pagesAutomatic Mains Failure Unit: DKG-545 User Manual V-11VinhNo ratings yet
- AE1222 2021 GROUP E10E WingDesignReportDocument100 pagesAE1222 2021 GROUP E10E WingDesignReportBowmigowNo ratings yet