Professional Documents
Culture Documents
Liver Abscesses: Factors That Influence Outcome of Percutaneous Drainage
Liver Abscesses: Factors That Influence Outcome of Percutaneous Drainage
Uploaded by
Riqqah USCopyright:
Available Formats
You might also like
- Experiment 8: Fixed and Fluidized BedDocument6 pagesExperiment 8: Fixed and Fluidized BedTuğbaNo ratings yet
- S0090429521002594Document7 pagesS0090429521002594Mounia MarsouNo ratings yet
- The Outcome of Ultrasound Guided Percutaneous Drainage of Liver AbscessDocument6 pagesThe Outcome of Ultrasound Guided Percutaneous Drainage of Liver AbscessIJAR JOURNALNo ratings yet
- Dalton 2016Document4 pagesDalton 2016fjparadaNo ratings yet
- Bess Is Sow 2014Document2 pagesBess Is Sow 2014Alfredo ChoquetNo ratings yet
- Enfermedad Diverticular RevisionDocument7 pagesEnfermedad Diverticular RevisionCarolina Escobedo AcuñaNo ratings yet
- Editorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystDocument4 pagesEditorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystLogical MonsterNo ratings yet
- Cureus 0013 00000020528Document7 pagesCureus 0013 00000020528Cesar RcNo ratings yet
- 2015 Article 1418 PDFDocument5 pages2015 Article 1418 PDFJennifer JaneNo ratings yet
- Is It Necessary To Ligate Distal Common Bile Duct Stumps After Excising Choledochal Cysts?Document4 pagesIs It Necessary To Ligate Distal Common Bile Duct Stumps After Excising Choledochal Cysts?Rajarshi KumarNo ratings yet
- Curative Resection For Esophageal Adenocarcinoma: Analysis of 100 en Bloc EsophagectomiesDocument12 pagesCurative Resection For Esophageal Adenocarcinoma: Analysis of 100 en Bloc EsophagectomiesYacine Tarik AizelNo ratings yet
- A Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesDocument4 pagesA Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesSake Cinema21No ratings yet
- Role of Wound Drains VS Abdominal Binder and Percutaneous Aspiration After Open Repair of Ventral Hernia Using Polyprolene MeshDocument12 pagesRole of Wound Drains VS Abdominal Binder and Percutaneous Aspiration After Open Repair of Ventral Hernia Using Polyprolene MeshIJAR JOURNALNo ratings yet
- Advantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct StonesDocument5 pagesAdvantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct Stonesnaili nsnNo ratings yet
- Abses HatiDocument20 pagesAbses Hatisuherman paleleNo ratings yet
- Transcortical Approach Surgery Versus External Ventricular Drainage in Treating IVHDocument6 pagesTranscortical Approach Surgery Versus External Ventricular Drainage in Treating IVHResiden BedahNo ratings yet
- Management of Appendiceal Mass and Abscess. An 11-Year ExperienceDocument5 pagesManagement of Appendiceal Mass and Abscess. An 11-Year ExperienceimamattamamiNo ratings yet
- Classification of Hydatid Cysts According To Gharbi and The World... Download Scientific DiagramDocument1 pageClassification of Hydatid Cysts According To Gharbi and The World... Download Scientific DiagramMucNo ratings yet
- Treatment of Intra-Abdominal Hydatid Cyst Using Modified PAIR Technique: Single Center ExperiencesDocument5 pagesTreatment of Intra-Abdominal Hydatid Cyst Using Modified PAIR Technique: Single Center ExperiencesSandu AlexandraNo ratings yet
- Pancreatic ®stula After Pancreatic Head ResectionDocument7 pagesPancreatic ®stula After Pancreatic Head ResectionNicolas RuizNo ratings yet
- ANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Document13 pagesANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Ammar magdyNo ratings yet
- Klatskin Tumor 2Document8 pagesKlatskin Tumor 2Florian JeffNo ratings yet
- PTBDDocument8 pagesPTBDDaniSantikaNo ratings yet
- Percutaneous Treatment of Liver Hydatid Cysts in 190 Patients: A Retrospective StudyDocument9 pagesPercutaneous Treatment of Liver Hydatid Cysts in 190 Patients: A Retrospective StudySandu AlexandraNo ratings yet
- Renal and Perinephric Abscesses: Analysis of 65 Consecutive CasesDocument6 pagesRenal and Perinephric Abscesses: Analysis of 65 Consecutive CasesGio Eleceene LyneyNo ratings yet
- Liver Abscess: Catheter Drainage V/s Needle AspirationDocument6 pagesLiver Abscess: Catheter Drainage V/s Needle AspirationMishel Rodriguez GuzmanNo ratings yet
- Endoscopic Endonasal Approaches To The Craniovertebral Junction The Otolaryngologist's Perspective, Schwartz 2020Document6 pagesEndoscopic Endonasal Approaches To The Craniovertebral Junction The Otolaryngologist's Perspective, Schwartz 2020CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- Successful Percutaneous Treatment of Extrahepatic Cystic Echinococcosis Through PAIR and Single Puncture Catheter TechniquesDocument7 pagesSuccessful Percutaneous Treatment of Extrahepatic Cystic Echinococcosis Through PAIR and Single Puncture Catheter TechniquesSandu AlexandraNo ratings yet
- Outcome BcsDocument16 pagesOutcome BcsSowmya ANo ratings yet
- Abstracts / Pancreatology 19 (2019) S1 Es180 S30Document1 pageAbstracts / Pancreatology 19 (2019) S1 Es180 S30Hưng Nguyễn KiềuNo ratings yet
- Post Aua ReconstructivaDocument14 pagesPost Aua ReconstructivaIndhira Sierra SanchezNo ratings yet
- Valls 2020Document7 pagesValls 2020Nikos SerifisNo ratings yet
- Cambio de Laparoscopia A Cirugia AbiertaDocument7 pagesCambio de Laparoscopia A Cirugia AbiertaJosé David Cortez Centeno 20190155No ratings yet
- Endoscopic Interventional Management Using Adrenaline-Normal Saline Injection For Actively Bleeding Peptic Ulcers in South Kashmir, IndiaDocument6 pagesEndoscopic Interventional Management Using Adrenaline-Normal Saline Injection For Actively Bleeding Peptic Ulcers in South Kashmir, IndiaIJAR JOURNALNo ratings yet
- Deroofing of Auricular Pseudocyst: Our Experience: Abst TDocument3 pagesDeroofing of Auricular Pseudocyst: Our Experience: Abst Tsolikin ikinNo ratings yet
- 1 s2.0 S0002961017313703 MainDocument4 pages1 s2.0 S0002961017313703 MainFlorin AchimNo ratings yet
- Trans-Fistulary Endoscopic Drainage For Post-Bariatric Abdominal Collections Communicating With The Upper Gastrointestinal TractDocument8 pagesTrans-Fistulary Endoscopic Drainage For Post-Bariatric Abdominal Collections Communicating With The Upper Gastrointestinal TractAlexandra JichituNo ratings yet
- 10 1 1 525 6842Document6 pages10 1 1 525 6842sandyNo ratings yet
- Research Article: Characteristics of Patients With Colonic Polyps Requiring Segmental ResectionDocument7 pagesResearch Article: Characteristics of Patients With Colonic Polyps Requiring Segmental ResectionAkiko Syawalidhany TahirNo ratings yet
- Perforacion Esofagica Esofago Toracico Una Decada de Experiencia 2003Document4 pagesPerforacion Esofagica Esofago Toracico Una Decada de Experiencia 2003joseNo ratings yet
- Transluminal Endoscopic Necrosectomy After Acute Pancreatitis: A Multicentre Study With Long-Term Follow-Up (The GEPARD Study)Document8 pagesTransluminal Endoscopic Necrosectomy After Acute Pancreatitis: A Multicentre Study With Long-Term Follow-Up (The GEPARD Study)victorNo ratings yet
- International Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. ChitheerDocument7 pagesInternational Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. Chitheersamer falconNo ratings yet
- Short Term Outcome of "Double Crown" Tackers Mesh Fixation Vs Intra-Corporeal Suture Fixation in Laparoscopic Ventral Hernia Repair.Document4 pagesShort Term Outcome of "Double Crown" Tackers Mesh Fixation Vs Intra-Corporeal Suture Fixation in Laparoscopic Ventral Hernia Repair.BIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Cierre Primario ColédocoDocument6 pagesCierre Primario Colédocoava0311No ratings yet
- Salvage of Malfunction DPDocument5 pagesSalvage of Malfunction DPBandac AlexandraNo ratings yet
- Retos en Fistula Atmosfericas IncotrolablesDocument4 pagesRetos en Fistula Atmosfericas IncotrolablesZulema CangaNo ratings yet
- Gastric GIST Treatment by Laparoscopy Report of 49 Cases and Literature's ReviewDocument4 pagesGastric GIST Treatment by Laparoscopy Report of 49 Cases and Literature's ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Griffith 1996Document10 pagesGriffith 1996Sowmya ANo ratings yet
- Early fluid resuscitation ...Document5 pagesEarly fluid resuscitation ...meganhamm04No ratings yet
- Emailing Wjssr-V3-Id1256Document3 pagesEmailing Wjssr-V3-Id1256Charbel AounNo ratings yet
- Maheshwari 2000Document3 pagesMaheshwari 2000Phuoc LeNo ratings yet
- Aijcr 2009 02 005Document6 pagesAijcr 2009 02 005Apps OmNo ratings yet
- Prospective & Comparative Study of Various Techniques Used in The Management of Liver Abscess in The Bundelkhand AreaDocument10 pagesProspective & Comparative Study of Various Techniques Used in The Management of Liver Abscess in The Bundelkhand AreaIJAR JOURNALNo ratings yet
- Clinicalinvestigation Non-VascularinterventionsDocument7 pagesClinicalinvestigation Non-VascularinterventionsSandu AlexandraNo ratings yet
- Regeneración Periodontal de Defectos Infraóseos HumanosDocument7 pagesRegeneración Periodontal de Defectos Infraóseos HumanosAgustin BuryakNo ratings yet
- Cheema2003 Article TimingOfLaparoscopicCholecysteDocument4 pagesCheema2003 Article TimingOfLaparoscopicCholecysteBandac AlexandraNo ratings yet
- SurgeryDocument7 pagesSurgeryFrancisco GilNo ratings yet
- Yan 2015Document4 pagesYan 2015ELIECERNo ratings yet
- Effect of Pelvic-Floor Re-Education On Duration and Degree of Incontinence After Radical Prostatectomy: A Randomised Controlled TrialDocument5 pagesEffect of Pelvic-Floor Re-Education On Duration and Degree of Incontinence After Radical Prostatectomy: A Randomised Controlled Trialpalomachagas1986No ratings yet
- Article Hernie InterneDocument4 pagesArticle Hernie Interneabdourahmane ndongNo ratings yet
- Post-cholecystectomy Bile Duct InjuryFrom EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNo ratings yet
- MPD and MPK Series Midi Io Details 02Document3 pagesMPD and MPK Series Midi Io Details 02Jorge David Monroy PerezNo ratings yet
- Crabs Hell Ms DsDocument1 pageCrabs Hell Ms DsRega Wahyu AnggrainiNo ratings yet
- The Myth of PlutoDocument6 pagesThe Myth of PlutoZsuzsanna ZöldNo ratings yet
- SteelDocument61 pagesSteelSonNguyenNo ratings yet
- Confucianism: By: Alisha, Mandy, Michael, and PreshiaDocument15 pagesConfucianism: By: Alisha, Mandy, Michael, and PreshiaAvi Auerbach AvilaNo ratings yet
- Techniques For Collection, Isolation and Preservation of MicroorganismsDocument42 pagesTechniques For Collection, Isolation and Preservation of Microorganismsaziskf100% (2)
- Fish JordanDocument29 pagesFish JordanSarah SobhiNo ratings yet
- Voltage Stability Enhancement in Power System Using STATCOM Based On Specific Coefficient Algorithm (SCA)Document7 pagesVoltage Stability Enhancement in Power System Using STATCOM Based On Specific Coefficient Algorithm (SCA)ElafanNo ratings yet
- Chemistry Practical Procedure Systematic Analysis of Salt STD: Xi & XiiDocument9 pagesChemistry Practical Procedure Systematic Analysis of Salt STD: Xi & XiivarshiniNo ratings yet
- Quickstart Dx35 de en FR Es PT ZH Ja It Ru Im0044955Document2 pagesQuickstart Dx35 de en FR Es PT ZH Ja It Ru Im0044955ROSSNo ratings yet
- Brown Et Al. 2009 Tribolium A Model For Developmental and Pest BiologyDocument9 pagesBrown Et Al. 2009 Tribolium A Model For Developmental and Pest BiologyAneel Nizar AliNo ratings yet
- User S Manual Bedienungsanleitung: Version 1.0 October 1998Document32 pagesUser S Manual Bedienungsanleitung: Version 1.0 October 1998Ojit QuizonNo ratings yet
- BS 03900 0 2010Document26 pagesBS 03900 0 2010selvaNo ratings yet
- Free/Open Source Multibody and Aerodynamic Software For Aeroelastic Analysis of Wind TurbinesDocument14 pagesFree/Open Source Multibody and Aerodynamic Software For Aeroelastic Analysis of Wind TurbinesFrankNo ratings yet
- Tech Mahindra Antonyms and QuestionsDocument27 pagesTech Mahindra Antonyms and QuestionsNehaNo ratings yet
- 1st Year Chemistry Sc1 ChemistryDocument896 pages1st Year Chemistry Sc1 Chemistrybiranchi satapathyNo ratings yet
- Pharmaceutics 14 02240Document17 pagesPharmaceutics 14 02240oliverasrommelNo ratings yet
- Construction Method (PICC)Document2 pagesConstruction Method (PICC)rheymar diwaNo ratings yet
- RABE - Sexual Imagery On The Phantasmagorical Castles at KhajurahoDocument30 pagesRABE - Sexual Imagery On The Phantasmagorical Castles at KhajurahoMarco PassavantiNo ratings yet
- Chapter No.1 Meat CookeryDocument15 pagesChapter No.1 Meat CookeryKrishna Chaudhary0% (1)
- Dit 24Document1 pageDit 24Abvolt IndiaNo ratings yet
- Brenes 2006Document6 pagesBrenes 2006Alfonso CáceresNo ratings yet
- prEN 12390-11 - DRAFTDocument32 pagesprEN 12390-11 - DRAFTCarlos GilNo ratings yet
- CBT JournalDocument82 pagesCBT JournalPaige Bayly100% (1)
- Mobil PajeroDocument2 pagesMobil Pajeroesemelekete wele2No ratings yet
- 6 Biomechanical Basis of Extraction Space Closure - Pocket DentistryDocument5 pages6 Biomechanical Basis of Extraction Space Closure - Pocket DentistryParameswaran ManiNo ratings yet
- What Aspects of "Life" Are Covered by Vedic AstrologyDocument4 pagesWhat Aspects of "Life" Are Covered by Vedic AstrologyMariana SantosNo ratings yet
- Cold Agglutinin DiseaseDocument4 pagesCold Agglutinin Diseasenavneet21usNo ratings yet
- Child - Cerebral PalsyDocument3 pagesChild - Cerebral PalsyJamie Icabandi67% (3)
Liver Abscesses: Factors That Influence Outcome of Percutaneous Drainage
Liver Abscesses: Factors That Influence Outcome of Percutaneous Drainage
Uploaded by
Riqqah USOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Liver Abscesses: Factors That Influence Outcome of Percutaneous Drainage
Liver Abscesses: Factors That Influence Outcome of Percutaneous Drainage
Uploaded by
Riqqah USCopyright:
Available Formats
Va s c u l a r a n d I n t e r ve n t i o n a l R a d i o l o g y • O r i g i n a l R e s e a r c h
Haider et al.
Percutaneous Drainage of Liver Abscesses
Vascular and Interventional Radiology
Original Research
Liver Abscesses: Factors
That Influence Outcome of
Percutaneous Drainage
OBJECTIVE. The purpose of this study was to identify the details of percutaneous cath-
1
Steffen J. Haider
Massimo Tarulli2 eter drainage (PCD) of pyogenic liver abscesses, the etiologic factors, and the management
Nancy J. McNulty 3 techniques that contribute to successful treatment.
Eric K. Hoffer 3 MATERIALS AND METHODS. The records of 75 consecutively registered patients
who underwent PCD of 96 abscesses at a single institution between May 2009 and May 2014
Haider SJ, Tarulli M, McNulty NJ, Hoffer EK were retrospectively reviewed. Thirty-nine patients (52%) were oncology patients, and 36
(48%) had recently undergone abdominal surgery. Primary success was defined as abscess
American Journal of Roentgenology 2017.209:205-213.
healing with the primary PCD intervention and 30-day postdrainage survival. Salvage suc-
cess was defined as abscess healing with follow-up secondary PCD placement for symptom-
atic hepatic satellite collections or for clinical recurrence. Catheter adjustments were per-
formed during follow-up to optimize existing drains. Univariate, multivariate, and general
linear mixed model analyses were performed. The median follow-up time after catheter re-
moval was 6 months (range, 2–62 months).
RESULTS. Drains were primarily successful in 54 patients (72%), and 17 patients (23%)
needed salvage PCD; thus, overall success was achieved in 71 patients (95%). The other four
patients (5%) died of sepsis. The primary success rate was reduced in patients with unresect-
able malignancies (p = 0.01), multiple abscesses (p = 0.01), and output ≥ 15 mL/d at catheter
endpoint (n = 7, p = 0.001). Only unresectable malignancies had slightly lower overall success.
Large abscesses (> 150 cm3) required more catheter adjustments and longer drainage duration
to reach abscess cavity closure. Successfully drained abscesses reached cavity closure a mean
Keywords: abscess, liver abscess, malignancy,
percutaneous abscess drainage of 23 days (95% CI, 20–27 days) after treatment.
CONCLUSION. PCD was effective first-line treatment of complicated pyogenic liver
DOI:10.2214/AJR.16.17713 abscesses, which often require catheter adjustment and salvage drainage procedures to reli-
ably achieve success.
Based on a presentation at the Cardiovascular and
Interventional Radiological Society of Europe 2016
utcomes of therapy for pyogenic The reported failure rate of primary PCD
O
annual meeting, Barcelona, Spain.
liver abscess (PLA) have improved ranges widely, from 0% to 30% with an in-
Received November 29, 2016; accepted after revision
dramatically over the past 40 years fection-related mortality of 0–13.4% [7–16].
January 15, 2017.
owing to earlier imaging diagno- Several studies have shown that PCD is less
1
Department of Radiology, Columbia University Medical sis, more effective antibiotic coverage, and ad- effective than surgical drainage in the treat-
Center, New York, NY. vances in percutaneous drainage techniques. ment of large loculated abscesses, variably
2
By the 1980s, percutaneous catheter drainage defined as greater than 3–6 cm in diameter
Department of Medical Imaging, Faculty of Medicine,
University of Toronto, Toronto, ON, Canada.
(PCD) with antibiotic therapy was accepted [13, 14]. In other series, however, no differ-
therapy for simple hepatic abscesses [1, 2]. Ow- ence was found in drainage success rates of
3
Department of Radiology, Section of Interventional Radi- ing to advances in technique and management, large and small abscesses, regardless of loc-
ology, Dartmouth-Hitchcock Medical Center, 1 Medical PCD has supplanted surgical drainage as the ulation [3, 5, 9, 17–19]. Variation may be due
Center Dr., Lebanon, NH 03756. Address correspondence
first-line treatment of PLA. This development to differences in management given that fol-
to E. K. Hoffer (eric.k.hoffer@hitchcock.org).
has been accompanied by a reduction in the low-up practices are not standardized [20].
This article is available for credit. need for general anesthesia and the complica- Few studies have included detailed analy-
tions of an open abdominal procedure [3–5]. sis of percutaneous liver drain management,
AJR 2017; 209:205–213
Surgery remains first-line treatment of patients making extraction of best practices difficult
0361–803X/17/2091–205 who present with abscess rupture, peritonitis, [7, 20]. These include indications for addi-
or a concomitant surgical condition but is oth- tional drainage procedures and optimal du-
© American Roentgen Ray Society erwise reserved for failure of PCD [3–7]. ration of drainage. In this study, we inves-
AJR:209, July 2017 205
Haider et al.
tigated management details that contribute dalities included fluoroscopic contrast study of the Statistical Analysis
to optimal management of the percutaneous drain (drain study), CT, and ultrasound. Statistical analyses were performed with SPSS
PLA drainage catheter. Catheter adjustment was exchange or reposi- Statistics for Microsoft Windows software (ver-
tioning of an existing catheter under fluoroscopic sion 22.0, IBM). Significance was defined as p <
Materials and Methods guidance to optimize catheter drainage. Common 0.05. Data are expressed as mean and SD. Differ-
Patient Demographics and Study Design indications included accidental removal, retrac- ences in subgroup mean drainage duration were
This institutional review board–approved ret- tion, occlusion, and poor position of the catheter compared by nonparametric Mann-Whitney U test.
rospective review was conducted with a waiver of with respect to residual abscess collection. Subgroup association with failure of primary suc-
informed consent. Between May 2009 and May Salvage drainage was performed during fol- cess was analyzed at the univariate level with the
2014, 75 consecutively registered patients under- low-up if a patient had symptoms and imaging Fisher exact test, and relative risk was reported. A
went PCD of 96 PLAs at a single tertiary referral confirmed an undrained abscess. This could be multivariate logistic regression model was used to
academic medical center. The diagnosis of PLA an initially undrained satellite collection or a sec- test the independence of subgroups that had uni-
was confirmed by the finding of purulent aspirate ond abscess or recurrence that developed during variate association with primary success. Odds ra-
or positive microbiologic findings. Amebic, fun- follow-up. Salvage PCD was performed with the tios were generated from the logistic regression.
gal, and parasitic abscesses were excluded. Oth- same protocol as for primary PCD. The mean time to cavity closure was estimated
er than for the nonpyogenic abscesses, no patients Endpoint—A fluoroscopic drain study was with general linear mixed models [22] by regres-
who underwent percutaneous liver abscess treat- performed to ensure that the abscess cavity had sion of repeated measurements of abscess volume
ment were excluded. Table 1 shows the demo- healed when the patient had no symptoms and out- over the follow-up period. A random slope with
graphics of the patient cohort. Patient data were put was < 15 mL/d for 2 days. A residual cavity fixed intercept was assumed. We used a heteroge-
collected from the hospital electronic medical re- of < 3 cm and resistance to injection or leakage neous autoregressive structure to model covari-
cord (Epic, Epic Systems). The median length of of contrast material along the drain confirmed ab- ance [23]. We performed post hoc power analysis
follow-up after catheter removal was 6 months scess healing. However, the primary team occa- at α = 0.05. There was approximately 65% power
American Journal of Roentgenology 2017.209:205-213.
(range, 2–62 months). This study was performed sionally removed drains on the basis of clinical for detecting a 30% difference in primary success
in accordance with the Strengthening the Report- findings alone. rate in subgroups of 15–20 patients.
ing of Observational Studies in Epidemiology Abscess management after catheter removal—
guidelines [21]. CT or ultrasound studies were obtained for 62 pa- Results
tients (85%) a median of 37 days (range, 2–252 Demographics
Management Protocol days) after catheter removal. Routine follow-up The clinical and abscess characteristics of
Percutaneous catheter drain placement—Pa- imaging accounted for 55% of the studies; 45% of the 75 patients with 96 PLAs are reported in
tients received broad-spectrum antibiotic therapy, studies were prompted by symptoms. Clinical re- Tables 1 and 2. The most common under-
which the primary team refined according to bacte- currence was defined as worsening clinical symp- lying etiologic factors predisposing to PLA
rial culture results. PCD was performed with stan- toms and image confirmation of reaccumulation were assessed. Recent hepatic oncologic sur-
dard sterile technique after subcutaneous admin- of the originally drained collection. Salvage PCD gery (within 30 days of PCD) had been per-
istration of anesthesia and IV moderate sedation. was performed on clinically recurrent abscesses. formed on 25% of patients and recent nonhe-
The Seldinger technique was used to percutaneous- patic abdominal surgery on 23%; 19% had
ly introduce an 8- to 12-French catheter into the Definition of Outcomes unresectable hepatopancreatobiliary malig-
abscess cavity under CT or ultrasound guidance. Primary success was defined as abscess reso- nancies (Table 1). Hepatopancreatobiliary
Larger cavities and more viscous fluid prompted lution requiring only the primary PCD treatment malignancy was found in 52% of patients,
the use of the 12-French catheters. The abscess with 30-day survival after catheter removal. Pri- 87% had abscesses > 5 cm in diameter, 35%
cavity was fully aspirated. Immediate reimaging mary failure was failure to meet the criteria for had multiple abscesses, and 56% had locu-
was performed to identify persistent collections or primary success. Catheter adjustments to existing lated abscesses.
loculations. Drainage of smaller satellite collec- drains are reported as a part of primary success.
tions was performed at the discretion of the inter- Salvage success was defined as abscess healing Outcomes
ventionalist. Drainage catheters were sutured to the with 30-day posttreatment survival after salvage Patient outcomes are reported in Table 3.
skin and left to bulb suction drainage. The catheter PCD. Overall success was defined as either prima- Primary clinical success was achieved in 54
was flushed twice daily with 5–10 mL normal sa- ry or salvage success. patients (72%), and primary drainage failed
line solution, and output was recorded. in 21 patients (28%). Assisted salvage suc-
Follow-up management—The intervention- Imaging Analysis cess was achieved for 17 of the 18 patients
al radiology team assessed the patient clinical- Radiographic abscess characteristics were re- who underwent salvage PCD intervention.
ly every other day for the first week, then week- corded from primary radiographic reports by board- This resulted in overall success for 71 pa-
ly if the patient remained in the hospital. Patients certified diagnostic radiologists and then verified by tients (95%). The other four patients (5%)
with continued drainage after hospital discharge a board-certified interventional radiologist with 24 died of sepsis within 30 days of catheter re-
underwent follow-up in the interventional radiol- years of experience. Abscess volume was calcu- moval. Adjustment to an existing catheter
ogy clinic. Follow-up imaging was performed for lated with the ellipsoid formula at the greatest di- was required in 17 patients (23%) to optimize
pain, fever, or elevated WBC count after the 48- mension in each of the axial, sagittal, and coronal drainage. Three of the patients who died were
hour postprocedural period [3, 4, 19, 20]. Drain planes. If an ultrasound or drain study included only not surgical candidates because they had ad-
output that plateaued at ≥ 15 mL/d or increased two dimensions, the smaller of the two was used as vanced malignant hepatobiliary disease, in-
also prompted follow-up imaging. Imaging mo- a surrogate for the third dimension. cluding a case of multiorgan abscesses. The
206 AJR:209, July 2017
Percutaneous Drainage of Liver Abscesses
fourth death occurred during salvage drain- TABLE 1: Demographic Characteristics, Underlying Pathologic Condition,
age. The one major complication, cholecys- and Abscess Size
tocutaneous fistula, required surgical repair Variable Result
after successful healing of a pericholecystic
abscess. No patient needed surgical abscess Demographic characteristics
drainage. The mean duration of drainage was PCD-treated patients 75
28 (SD, 22) days (range, 3–115 days). PCD-treated abscesses 96
Salvage percutaneous catheter drain—Fig-
Age (y)
ure 1 shows salvage PCD of a symptomatic
satellite collections and catheter adjustment Mean 62
in a patient with multiple abscesses. Eighteen Range 15–90
of the 21 patients with primary failure un- SD 13
derwent salvage PCD. The 17 patients who
Sex
healed after salvage PCD included five with
follow-up drainage of symptomatic satellite Men 50 (67)
collections, eight with clinical recurrence, Women 25 (33)
and four with both drainage of satellite col- Malignancya 39 (52)
lections and recurrence. The initial salvage
Pancreatic or ampullary malignancy 15 (20)
PCD for symptomatic satellite abscesses was
performed a mean of 24 (SD, 12) days (range, Colorectal carcinoma with hepatic metastases 13 (17)
5–46 days) after the primary PCD procedure, Gallbladder cancer or cholangiocarcinoma 6 (7)
resulting in healing of 13 of the 17 salvage
American Journal of Roentgenology 2017.209:205-213.
Underlying pathologic condition predisposing to pyogenic liver abscess
successes. To achieve healing, four patients
Recent hepatic surgeryb 19 (25)
needed two or three salvage drainage proce-
dures 22–177 days after the initial PCD. Abscess of surgical bed after oncologic resection 18
Catheter adjustments—Between one and Abscess of radiofrequency ablation bed 1
five catheter adjustment procedures were Recent nonhepatic abdominal surgeryb 17 (23)
performed on 17 (23%) patients to optimize
Pancreatobiliary oncologic surgery 7
drainage during follow-up. This included 10
catheter exchanges, three caliber increases, Nononcologic abdominal surgery 10
two caliber decreases, and six catheter repo- Unresectable hepatopancreatobiliary malignancy 14 (19)
sitioning procedures. Catheter adjustments No malignancy or recent surgery 25 (33)
were performed in 10 of 28 patients (36%)
Abscess size
with abscess size ≥ 150 cm3 compared with
7 of 47 patients (15%) with smaller abscesses Volume (cm3)
(p = 0.05). Catheter adjustment was associ- Mean 153
ated with a longer mean drainage duration of Median 53
48 (SD, 31) days compared with 23 (SD, 15)
Range 3–1331
days for unrevised drains (p = 0.001).
SD 191
Associations With Primary Clinical Failure Median dimensions (cm)c
Univariate and multivariate relations are Length 4.7 (2.0)
reported in Tables 2 and 4. Three independent
Width 6.0 (2.6)
variables were associated with a significant-
ly lower rate of primary success in univar- Height 5.8 (2.5)
iate and multivariate analyses. These were Note—Unless otherwise indicated, values are number of patients with percentage in parentheses. PCD =
unresectable hepatopancreatobiliary malig- percutaneous catheter drainage.
aThe remaining five patients each had a different malignancy.
nancy as the predisposing pathologic condi- bAbscess risk factors refer to procedures within 30 days before abscess drainage.
tion (p = 0.01), presence of multiple abscess- cValues in parentheses are SD.
es (p = 0.01), and catheter removal despite
daily output ≥ 15 mL/d (p = 0.001). No other Unresectable hepatopancreatobiliary malig- symptomatic satellite collections, six to clinical
independent variable was associated with pri- nancy—Unresectable hepatopancreatobiliary recurrence, and one to both symptomatic satel-
mary success, including advanced age, diabe- malignancy was associated with a 57% (8/14) lite collections and clinical recurrence. Salvage
tes, postsurgical abscess, large abscess size, primary failure rate (Table 2). The risk of pri- PCD procedures resulted in overall success for
or loculations. The primary success rate was mary failure among patients with these malig- 11 patients (79%). Three septic deaths account-
lower among the 10 patients with biliary fis- nancies was 2.4 times as high as that among pa- ed for a lower overall success rate (p = 0.02).
tula in univariate analysis, but this did not tients with other causes of abscess (RR 95% CI, Multiple abscesses—Multiple abscesses
reach statistical significance (Tables 2 and 4). 1.4–5.2). Three primary failures were due to were associated with a 46% (12/26) prima-
AJR:209, July 2017 207
Haider et al.
ry failure rate (Table 2). The risk of prima- TABLE 2: Univariate Associations Between Demographic Characteristics,
ry failure among patients with multiple ab- Abscess Features, and Follow-Up Management and Primary Failure
scesses was 2.5 times as high as that among and Overall Success Rates
patients with a single abscess (RR 95% CI, No. With Relative Risk of Primary Failure No. With
1.2–5.2). Salvage PCD procedures resulted Total No. of Primary Overall
in overall success for 25 (96%) of these pa- Characteristic Patients Failures Risk 95% CI p Success
tients. One patient died of sepsis. Figure 1 Demographics
shows a patient with multiple abscesses re-
Age ≥ 55 y 57 (76) 17 (30) 1.3 0.5–3.5 0.76 53 (93)
quiring salvage PCD for abscess healing.
Primary failures included seven symptom- Diabetes mellitus 16 (21) 4 (25) 0.9 0.3–2.2 1 15 (94)
atic satellite collections, seven clinical re- Recent hepatic surgerya 19 (25) 5 (26) 0.9 0.4–2.2 1 19 (100)
currences, and cases of both symptomatic Recent nonhepatic 17 (23) 4 (24) 0.8 0.3–2.1 0.77 16 (94)
satellite collections and clinical recurrence. abdominal surgerya
There was an 86% (6/7) primary success rate Unresectable hepatopan- 14 (19) 8 (57) 2.7 1.4–5.2 0.02 11 (79)b
when initial drainage of all diagnosed col- creatobiliary malignancy
lections was performed, compared with 42%
No malignancy or recent 25 (33) 4 (16) 0.5 0.2–1.3 0.17 25 (100)
(8/19) when only the largest collection was surgery
initially drained (p = 0.08).
Abscess features
Removal of drain despite high output—There
was a 78% (7/9) primary failure rate among Multiple abscesses 26 (35) 12 (46) 2.5 1.2–5.2 0.01 25 (96)
patients who underwent catheter removal and Abscess volume > 150 cm3 28 (37) 7 (25) 0.8 0.4–1.8 0.79 27 (96)
had ongoing daily output ≥ 15 mL/d (range,
American Journal of Roentgenology 2017.209:205-213.
Fistula 10 (13) 5 (50) 2.0 1.0–4.3 0.13 9 (90)
20–90 mL/d) (Table 2). The risk of primary
Multiloculated abscess 42 (56) 11 (26) 0.9 0.4–1.8 0.80 40 (95)
failure among these patients was 4.1 times as
high as that among patients with lower end- Follow-up management
point drain output (RR 95% CI, 2.2–7.7). Catheter adjustments 17 (23) 4 (24) 0.8 0.3–2.1 0.77 16 (94)
Salvage PCD that was continued until drain Drainage duration ≥ 3 wk 41 (55) 11 (27) 0.9 0.4–1.9 1 38 (93)
output was minimal resulted in overall suc-
Drain output ≥ 15 mL/d at 9 (12) 7 (78) 4.1 2.2–7.7 0.001 9 (100)
cess for all nine of these patients (Table 2). catheter endpoint
Figure 2 shows primary failure after cathe-
Note—Except for relative risk, values are numbers of patients with percentages in parentheses.
ter removal despite ongoing high drain out- a Abscess risk factors refer to procedures within 30 days before abscess drainage.
put. The nine high-output catheter removals bp < 0.05 for lower rate of overall success.
were performed to ameliorate catheter-relat-
ed discomfort in patients who were in clin- TABLE 3: Cohort Outcomes
ically stable condition. The general surgery
service independently performed seven of Outcome No. of Patients
these removals. The seven primary failures Primary success 54 (72)
were solely due to abscess recurrence after
Primary failure 21 (28)
removal of the catheter.
Salvage success 17 (23)
Natural History of an Adequately Drained Drainage of symptomatic satellite collection 5
Hepatic Abscess Recurrence of original abscess 8
The rate of abscess cavity closure was es-
Satellite drainage and clinical recurrence 4
timated for successfully drained abscesses.
This idealized model excluded drains with Catheter adjustmentsa 17 (23)
high output at removal or recurrences, be- Overall success 71 (95)
cause these did not reflect optimal treatment. Death within 30 d 4 (5)
Successfully drained abscesses reached cav-
Note—Values in parentheses are percentages.
ity closure in a mean of 23 days (95% CI, a Adjustment to an existing catheter including caliber change or repositioning.
20–27 days). Cavity closure of large ab-
scesses (≥ 150 cm3) was reached a mean of difference in time to cavity closure based on another 23% needed a second drain. These
30 days (95% CI, 25–38), compared with 20 abscess loculation (p = 0.28) or multiplicity results compare favorably to published qual-
days (95% CI, 17–26 days) for abscesses < (p = 0.67). ity standards for percutaneous abscess drain-
150 cm3 (p = 0.01) (Fig. 3). This correlated age and reported success rates of 77–90% in
clinically to mean drainage duration of 35 Discussion similar PLA populations [7, 9, 10, 14, 17, 18].
(SD, 25) days for abscesses ≥ 150 cm3 com- Successful percutaneous drainage of Success rates reported for the percutane-
pared with 25 (SD, 20) days for smaller ab- PLAs was achieved in 95% of patients, al- ous drainage of complicated PLA (i.e., large,
scesses (p = 0.03). There was no significant though 23% needed catheter adjustments and loculated, multiple, or malignancy-associ-
208 AJR:209, July 2017
Percutaneous Drainage of Liver Abscesses
TABLE 4: Multivariate Associations Between Primary Failure Rate by ment alone. Although the patient population
Subgroup and Failure Rate in Univariate Analysis was heterogeneous in terms of underlying
Multivariate Regression of Primary Failure
pathologic condition, the demographics and
abscess complexity were similar to those in
Subgroup No. of Patients Odds Ratio 95% CI p comparable studies [3–6, 9, 11, 14, 15, 26].
Unresectable hepatopancreatobiliary 14 14.4 2.1–98 0.01 We report on primary success in each of the
malignancy etiologic groups. The cohort was fairly small,
Multiple abscesses 26 8.0 1.5–43 0.01 which may have underpowered detection of
small subgroup differences in primary fail-
Drain output ≥ 15 mL/d at catheter 9 42 4.4–393 0.001
endpoint ure rate. Patient care was multidisciplinary,
and this resulted in premature drain remov-
Fistula 10 4.3 0.2–4.3 0.16
al in some patients. Although this may have
No malignancy or recent surgery 25 0.7 0.1–5.7 0.73 compromised the primary PCD success rate,
it reflects the challenges of true clinical prac-
ated) range from 33% to 90% [7, 12–14, 16, results of similar advanced oncology sub- tice. The general linear model of abscess vol-
24–28]. This has led to controversy regard- groups, in which abscess survival ranged ume over time was limited by a lack of im-
ing the role of PCD versus surgical drainage, from 15% to 64% [12, 26]. aging at the time of drain removal in some
several nonrandomized comparisons favor- Patients with multiple abscesses also had patients. Furthermore, we assumed a linear
ing surgical drainage [13, 14, 24]. Some au- a lower primary PCD success rate owing to relation between abscess volume and time,
thors have argued that an open surgical ap- symptomatic satellite collections or primary and although some patients deviated from
proach allows the breakdown of loculations abscess recurrence. Salvage PCD for initial- this relation (i.e., times to 50% reduction
and that the placement of large (28-French) ly undrained satellite collections was com- may not be accurate), the time to cavity clo-
American Journal of Roentgenology 2017.209:205-213.
surgical catheters improves drainage of ne- monly required if all collections were not sure was well approximated.
crotic debris [24, 29]. In the current study, initially drained. Concordant to this logic, a
however, we found no evidence of a lower small subgroup of seven patients in whom Conclusion
success rate of PCD for loculated or large ab- all collections were initially drained did In the study cohort, PCD was effective
scesses. Catheter adjustments were more of- have a higher primary success rate. Persis- first-line treatment of complicated PLAs
ten required in patients with large abscesses, tence of satellite collections may have led to with overall success in 95% of patients. Sal-
but this did not compromise the success rate. reseeding of the nearly healed primary ab- vage drainage procedures were more often
This finding is concordant with the finding scess cavity in abscess recurrences [29]. Pa- required to achieve success in patients with
of Liu et al. [9] that PCD-treated single and tients with multiple abscesses may benefit unresectable hepatopancreatobiliary malig-
multiple abscesses had equivalent success from cross-sectional imaging before drain nancies and multiple abscesses. Recurrence
rates regardless of loculation. removal. Persistent satellite collections was associated with catheter removal when
In several reports, persistent symptoms af- could be drained to potentially avert clinical output was ≥ 15 mL/d. Patients with large
ter drain placement were considered failures abscess recurrence. abscesses needed more catheter adjustments
of PCD that could lead to surgical drainage Catheter removal despite high drain output and had longer drainage duration, but this
[12–14, 24, 25, 30]. Tan et al. [14] reported represented a correctable factor and empha- did not compromise the success rate. Percu-
that 40% of PCD failures were due to cath- sized the need for communication between taneous PLA drainage effectiveness is opti-
eter blockage or dislodgments in a cohort the interventional radiology and the prima- mized by diligent drain follow-up and inter-
comparable to that in our study. Hope and ry teams on the appropriate drain endpoint. vention and multidisciplinary coordination
colleagues [13] also found PCD inferior to Ahmed et al. [19] reported that an output end- regarding drainage endpoints.
surgical drainage for loculated abscesses > 3 point < 10 mL/d resulted in a 90% success rate
cm, at 33% (8/24) versus 100% (27/27). for large abscesses, which is concordant with Acknowledgment
Proactive drain management may differ- our experience. Although a drain may be un- We thank Todd A. MacKenzie of the Dart-
entiate the current results from reports of comfortable, and there is often a desire among mouth Clinical and Translational Science In-
high PCD failure rates [12–14, 25]. Our prac- patients and referring clinicians to remove the stitute (National Institutes of Health award
tice had a low threshold for performing a drain as soon as possible, we found no evi- UL1TR001086) for reviewing the statistical
contrast-enhanced drain study for drain dys- dence to support earlier removal of drains. methods in this study.
function with the intent of providing early Successful drainage of larger abscesses and
catheter adjustment or salvage drainage. This those that required catheter adjustments was References
may have prevented overall PCD failure that associated with longer drain dwell times. This 1. vanSonnenberg E, Mueller PR, Ferrucci JT Jr.
would require escalation of care to an open is further supported by the idealized mean Percutaneous drainage of 250 abdominal abscess-
surgical procedure. time to abscess healing of 3–4 weeks. es and fluid collections. Part 1. Results, failures,
Although patients with unresectable hepa- Selection bias was a potential limitation of and complications. Radiology 1984; 151:337–341
topancreatobiliary malignancies had a pri- this retrospective study because only patients 2. Gerzof SG, Johnson WC, Robbins AH, Nabseth DC.
mary success rate of only 43%, secondary referred for percutaneous drainage were in- Intrahepatic pyogenic abscesses: treatment by percu-
procedures improved the overall success rate cluded. There was no attempt to compare taneous drainage. Am J Surg 1985; 149:487–494
to 79%, which compared favorably with the PCD to surgical drainage or medical treat- 3. Ferraioli G, Garlaschelli A, Zanaboni D, et al.
AJR:209, July 2017 209
Haider et al.
Percutaneous and surgical treatment of pyo- comes and prognostic factors of cancer patients 21. von Elm E, Altman DG, Egger M, et al. The
genic liver abscesses: observation over a 21- with pyogenic liver abscess. J Gastrointest Surg Strengthening the Reporting of Observational
year period in 148 patients. Dig Liver Dis 2008; 2011; 15:2036–2043 Studies in Epidemiology (STROBE) statement:
40:690–696 13. Hope WW, Vrochides DV, Newcomb WL, Mayo- guidelines for reporting observational studies.
4. Seeto RK, Rockey DC. Pyogenic liver abscess: Smith WW, Iannitti DA. Optimal treatment of J Clin Epidemiol 2008; 61:344–349
changes in etiology, management, and outcome. hepatic abscess. Am Surg 2008; 74:178–182 22. Zeger SL, Liang KY, Albert PS. Models for longi-
Medicine (Baltimore) 1996; 75:99–113 14. Tan YM, Chung AY, Chow PK, et al. An appraisal tudinal data: a generalized estimating equation
5. Alvarez Pérez JA, González JJ, Baldonedo RF, et of surgical and percutaneous drainage for pyo- approach. Biometrics 1988; 44:1049–1060
al. Clinical course, treatment, and multivariate genic liver abscesses larger than 5 cm. Ann Surg 23. Littell RC, Pendergast J, Natarajan R. Modelling
analysis of risk factors for pyogenic liver abscess. 2005; 241:485–490 covariance structure in the analysis of repeated
Am J Surg 2001; 181:177–186 15. Pang TC, Fung T, Samra J, Hugh TJ, Smith RC. measures data. Stat Med 2000; 19:1793–1819
6. Stain SC, Yellin AE, Donovan AJ, Brien HW. Pyogenic liver abscess: an audit of 10 years’ expe- 24. Barakate MS, Stephen MS, Waugh RC, et al. Pyo-
Pyogenic liver abscess: modern treatment. Arch rience. World J Gastroenterol 2011; 17:1622–1630 genic liver abscess: a review of 10 years’ experi-
Surg 1991; 126:991–996 16. Lai KC, Cheng KS, Jeng LB, et al. Factors associ- ence in management. Aust N Z J Surg 1999;
7. Lo JZ, Leow JJ, Ng PL, et al. Predictors of therapy ated with treatment failure of percutaneous cath- 69:205–209
failure in a series of 741 adult pyogenic liver ab- eter drainage for pyogenic liver abscess in patients 25. Chen SC, Tsai SJ, Chen CH, et al. Predictors of
scesses. J Hepatobiliary Pancreat Sci 2015; with hepatobiliary-pancreatic cancer. Am J Surg mortality in patients with pyogenic liver abscess.
22:156–165 2013; 205:52–57 Neth J Med 2008; 66:196–203
8. Rahimian J, Wilson T, Oram V, Holzman RS. 17. Zerem E, Hadzic A. Sonographically guided per- 26. Mezhir JJ, Fong Y, Jacks LM, et al. Current man-
Pyogenic liver abscess: recent trends in etiology cutaneous catheter drainage versus needle aspira- agement of pyogenic liver abscess: surgery is now
and mortality. Clin Infect Dis 2004; 39:1654–1659 tion in the management of pyogenic liver abscess. second-line treatment. J Am Coll Surg 2010;
9. Liu CH, Gervais DA, Hahn PF, Arellano RS, Up- AJR 2007; 189:[web]W138–W142 210:975–983
American Journal of Roentgenology 2017.209:205-213.
pot RN, Mueller PR. Percutaneous hepatic abscess 18. Mangukiya DO, Darshan JR, Kanani VK, Gupta 27. McDonald MI, Corey GR, Gallis HA, Durack DT.
drainage: do multiple abscesses or multiloculated ST. A prospective series case study of pyogenic Single and multiple pyogenic liver abscesses: nat-
abscesses preclude drainage or affect outcome? J liver abscess: recent trends in etiology and man- ural history, diagnosis and treatment, with empha-
Vasc Interv Radiol 2009; 20:1059–1065 agement. Indian J Surg 2012; 74:385–390 sis on percutaneous drainage. Medicine (Balti-
10. Singh S, Chaudhary P, Saxena N, Khandelwal S, 19. Ahmed S, Chia CL, Junnarkar SP, Woon W, She- more) 1984; 63:291–302
Poddar DD, Biswal UC. Treatment of liver ab- lat VG. Percutaneous drainage for giant pyogenic 28. Pearce NW, Knight R, Irving H, et al. Non-opera-
scess: prospective randomized comparison of liver abscess: is it safe and sufficient? Am J Surg tive management of pyogenic liver abscess. HPB
catheter drainage and needle aspiration. Ann Gas- 2016; 211:95–101 (Oxford) 2003; 5:91–95
troenterol 2013; 26:332–339 20. Lewandowski RJ, Desai SB, Nemcek AA Jr. 29. Farges O, Leese T, Bismuth H. Pyogenic liver ab-
11. Alkofer B, Dufay C, Parienti JJ, Lepennec V, Treatment of effusions and abscesses. In: Mauro scess: an improvement in prognosis. Br J Surg
Dargere S, Chiche L. Are pyogenic liver abscesses MA, Murphy KP, Thomson KR, Venbrux AC, 1988; 75:862–865
still a surgical concern? A Western experience. Morgan RA, eds. Image-guided interventions, 30. Johnson RD, Mueller PR, Ferrucci JT Jr, et al. Per-
HPB Surg 2012;2012:316013 2nd ed. Philadelphia, PA: Saunders Elsevier cutaneous drainage of pyogenic liver abscesses.
12. Chen SC, Lee YT, Tsai SJ, et al. Clinical out- Health, 2014; 1137–1144 AJR 1985; 144:463–467
(Figures start on next page)
210 AJR:209, July 2017
Percutaneous Drainage of Liver Abscesses
A B
American Journal of Roentgenology 2017.209:205-213.
C D
Fig. 1—59-year-old previously healthy man with multiple abscesses who presented with 1 month of abdominal
pain, fever, and weight loss.
A, Contrast-enhanced CT image shows anterolateral (long white arrow), posterolateral (short white arrow), and
medial (black arrow) collections. Primary percutaneous catheter drainage of anterolateral and posterolateral
collections was performed with single catheter.
B, Contrast-enhanced CT image obtained 5 days after A because of persistent symptoms shows anterolateral
cavity improvement (long white arrow) but persistence of posterolateral (short white arrow) and medial (black
arrow) collections. Catheter was repositioned to better drain posterolateral collection, and multiple aspirations
of medial cavity were performed.
C, Follow-up fluoroscopic drain study image obtained because of persistent high output shows biliary fistula
without evidence of distal obstruction. Drainage was continued for 7 weeks until output was minimal and drain
study showed cavity closure. Oral antibiotics were continued for additional 2 months.
D, Follow-up CT image shows abscess resolution. There were no further complications.
AJR:209, July 2017 211
Haider et al.
A B
American Journal of Roentgenology 2017.209:205-213.
C D
Fig. 2—57-year-old man with fever and abdominal pain due large single abscess recurrence caused by
premature drain removal 3 weeks after partial hepatectomy for colorectal cancer metastatic to liver.
A, Contrast-enhanced CT image shows unilocular 9-cm abscess in hepatic resection bed. Primary
percutaneous catheter drainage (PCD) was performed. Catheter was removed after 22 days despite 20-mL/d
output.
B, Patient presented with right upper quadrant pain 1 month after A. CT image shows persistent abscess.
Salvage PCD was performed.
C, Output was minimal after 11 days of salvage PCD. Fluoroscopic drain study shows residual 2.5-cm3 cavity.
Catheter was removed.
D, CT image obtained 2 months after C shows abscess resolution. There were no further complications.
212 AJR:209, July 2017
Percutaneous Drainage of Liver Abscesses
110
Percentage of Original Abscess Volume
100 110
90 100
Percentage of Original Abscess
80 90
Volume With 95% CI
70 80
With 95% CI
70
60
60
50
50
40
40
30
30
20 20
10 10
0 0
0 7 14 21 28 35 0 7 14 21 28 35
Days Since Percutaneous Drain Placement Days Since Percutaneous Drain Placement
A B
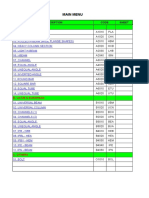
Fig. 3—Idealized model of time to abscess cavity healing. Models were composed of each appropriately managed collection that did not recur.
A, Graph shows successfully drained small abscesses (< 150 cm3) reached cavity healing by 2.5–3.5 weeks (n = 58 abscesses, which excludes high-output drain removal
and recurrence). Of note, 75% were still > 5 cm in long axis. General linear mixed model, p < 0.001 for trend with cavity closure in 20 days (95% CI, 17–26 days).
B, Graph shows successfully drained large abscesses (≥ 150 cm 3) reached cavity healing by 5–6 weeks (n = 22 abscesses, which excludes high-output drain removal and
American Journal of Roentgenology 2017.209:205-213.
recurrence). This time was significantly longer than for smaller abscesses (p = 0.012). General linear mixed model, p < 0.0001 for trend with cavity closure in 30 days (95%
CI, 25–38 days).
F O R YO U R I N F O R M AT I O N
This article is available for CME and Self-Assessment (SA-CME) credit that satisfies Part II requirements for
maintenance of certification (MOC). To access the examination for this article, follow the prompts associated with
the online version of the article.
AJR:209, July 2017 213
You might also like
- Experiment 8: Fixed and Fluidized BedDocument6 pagesExperiment 8: Fixed and Fluidized BedTuğbaNo ratings yet
- S0090429521002594Document7 pagesS0090429521002594Mounia MarsouNo ratings yet
- The Outcome of Ultrasound Guided Percutaneous Drainage of Liver AbscessDocument6 pagesThe Outcome of Ultrasound Guided Percutaneous Drainage of Liver AbscessIJAR JOURNALNo ratings yet
- Dalton 2016Document4 pagesDalton 2016fjparadaNo ratings yet
- Bess Is Sow 2014Document2 pagesBess Is Sow 2014Alfredo ChoquetNo ratings yet
- Enfermedad Diverticular RevisionDocument7 pagesEnfermedad Diverticular RevisionCarolina Escobedo AcuñaNo ratings yet
- Editorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystDocument4 pagesEditorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystLogical MonsterNo ratings yet
- Cureus 0013 00000020528Document7 pagesCureus 0013 00000020528Cesar RcNo ratings yet
- 2015 Article 1418 PDFDocument5 pages2015 Article 1418 PDFJennifer JaneNo ratings yet
- Is It Necessary To Ligate Distal Common Bile Duct Stumps After Excising Choledochal Cysts?Document4 pagesIs It Necessary To Ligate Distal Common Bile Duct Stumps After Excising Choledochal Cysts?Rajarshi KumarNo ratings yet
- Curative Resection For Esophageal Adenocarcinoma: Analysis of 100 en Bloc EsophagectomiesDocument12 pagesCurative Resection For Esophageal Adenocarcinoma: Analysis of 100 en Bloc EsophagectomiesYacine Tarik AizelNo ratings yet
- A Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesDocument4 pagesA Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesSake Cinema21No ratings yet
- Role of Wound Drains VS Abdominal Binder and Percutaneous Aspiration After Open Repair of Ventral Hernia Using Polyprolene MeshDocument12 pagesRole of Wound Drains VS Abdominal Binder and Percutaneous Aspiration After Open Repair of Ventral Hernia Using Polyprolene MeshIJAR JOURNALNo ratings yet
- Advantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct StonesDocument5 pagesAdvantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct Stonesnaili nsnNo ratings yet
- Abses HatiDocument20 pagesAbses Hatisuherman paleleNo ratings yet
- Transcortical Approach Surgery Versus External Ventricular Drainage in Treating IVHDocument6 pagesTranscortical Approach Surgery Versus External Ventricular Drainage in Treating IVHResiden BedahNo ratings yet
- Management of Appendiceal Mass and Abscess. An 11-Year ExperienceDocument5 pagesManagement of Appendiceal Mass and Abscess. An 11-Year ExperienceimamattamamiNo ratings yet
- Classification of Hydatid Cysts According To Gharbi and The World... Download Scientific DiagramDocument1 pageClassification of Hydatid Cysts According To Gharbi and The World... Download Scientific DiagramMucNo ratings yet
- Treatment of Intra-Abdominal Hydatid Cyst Using Modified PAIR Technique: Single Center ExperiencesDocument5 pagesTreatment of Intra-Abdominal Hydatid Cyst Using Modified PAIR Technique: Single Center ExperiencesSandu AlexandraNo ratings yet
- Pancreatic ®stula After Pancreatic Head ResectionDocument7 pagesPancreatic ®stula After Pancreatic Head ResectionNicolas RuizNo ratings yet
- ANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Document13 pagesANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Ammar magdyNo ratings yet
- Klatskin Tumor 2Document8 pagesKlatskin Tumor 2Florian JeffNo ratings yet
- PTBDDocument8 pagesPTBDDaniSantikaNo ratings yet
- Percutaneous Treatment of Liver Hydatid Cysts in 190 Patients: A Retrospective StudyDocument9 pagesPercutaneous Treatment of Liver Hydatid Cysts in 190 Patients: A Retrospective StudySandu AlexandraNo ratings yet
- Renal and Perinephric Abscesses: Analysis of 65 Consecutive CasesDocument6 pagesRenal and Perinephric Abscesses: Analysis of 65 Consecutive CasesGio Eleceene LyneyNo ratings yet
- Liver Abscess: Catheter Drainage V/s Needle AspirationDocument6 pagesLiver Abscess: Catheter Drainage V/s Needle AspirationMishel Rodriguez GuzmanNo ratings yet
- Endoscopic Endonasal Approaches To The Craniovertebral Junction The Otolaryngologist's Perspective, Schwartz 2020Document6 pagesEndoscopic Endonasal Approaches To The Craniovertebral Junction The Otolaryngologist's Perspective, Schwartz 2020CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- Successful Percutaneous Treatment of Extrahepatic Cystic Echinococcosis Through PAIR and Single Puncture Catheter TechniquesDocument7 pagesSuccessful Percutaneous Treatment of Extrahepatic Cystic Echinococcosis Through PAIR and Single Puncture Catheter TechniquesSandu AlexandraNo ratings yet
- Outcome BcsDocument16 pagesOutcome BcsSowmya ANo ratings yet
- Abstracts / Pancreatology 19 (2019) S1 Es180 S30Document1 pageAbstracts / Pancreatology 19 (2019) S1 Es180 S30Hưng Nguyễn KiềuNo ratings yet
- Post Aua ReconstructivaDocument14 pagesPost Aua ReconstructivaIndhira Sierra SanchezNo ratings yet
- Valls 2020Document7 pagesValls 2020Nikos SerifisNo ratings yet
- Cambio de Laparoscopia A Cirugia AbiertaDocument7 pagesCambio de Laparoscopia A Cirugia AbiertaJosé David Cortez Centeno 20190155No ratings yet
- Endoscopic Interventional Management Using Adrenaline-Normal Saline Injection For Actively Bleeding Peptic Ulcers in South Kashmir, IndiaDocument6 pagesEndoscopic Interventional Management Using Adrenaline-Normal Saline Injection For Actively Bleeding Peptic Ulcers in South Kashmir, IndiaIJAR JOURNALNo ratings yet
- Deroofing of Auricular Pseudocyst: Our Experience: Abst TDocument3 pagesDeroofing of Auricular Pseudocyst: Our Experience: Abst Tsolikin ikinNo ratings yet
- 1 s2.0 S0002961017313703 MainDocument4 pages1 s2.0 S0002961017313703 MainFlorin AchimNo ratings yet
- Trans-Fistulary Endoscopic Drainage For Post-Bariatric Abdominal Collections Communicating With The Upper Gastrointestinal TractDocument8 pagesTrans-Fistulary Endoscopic Drainage For Post-Bariatric Abdominal Collections Communicating With The Upper Gastrointestinal TractAlexandra JichituNo ratings yet
- 10 1 1 525 6842Document6 pages10 1 1 525 6842sandyNo ratings yet
- Research Article: Characteristics of Patients With Colonic Polyps Requiring Segmental ResectionDocument7 pagesResearch Article: Characteristics of Patients With Colonic Polyps Requiring Segmental ResectionAkiko Syawalidhany TahirNo ratings yet
- Perforacion Esofagica Esofago Toracico Una Decada de Experiencia 2003Document4 pagesPerforacion Esofagica Esofago Toracico Una Decada de Experiencia 2003joseNo ratings yet
- Transluminal Endoscopic Necrosectomy After Acute Pancreatitis: A Multicentre Study With Long-Term Follow-Up (The GEPARD Study)Document8 pagesTransluminal Endoscopic Necrosectomy After Acute Pancreatitis: A Multicentre Study With Long-Term Follow-Up (The GEPARD Study)victorNo ratings yet
- International Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. ChitheerDocument7 pagesInternational Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. Chitheersamer falconNo ratings yet
- Short Term Outcome of "Double Crown" Tackers Mesh Fixation Vs Intra-Corporeal Suture Fixation in Laparoscopic Ventral Hernia Repair.Document4 pagesShort Term Outcome of "Double Crown" Tackers Mesh Fixation Vs Intra-Corporeal Suture Fixation in Laparoscopic Ventral Hernia Repair.BIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Cierre Primario ColédocoDocument6 pagesCierre Primario Colédocoava0311No ratings yet
- Salvage of Malfunction DPDocument5 pagesSalvage of Malfunction DPBandac AlexandraNo ratings yet
- Retos en Fistula Atmosfericas IncotrolablesDocument4 pagesRetos en Fistula Atmosfericas IncotrolablesZulema CangaNo ratings yet
- Gastric GIST Treatment by Laparoscopy Report of 49 Cases and Literature's ReviewDocument4 pagesGastric GIST Treatment by Laparoscopy Report of 49 Cases and Literature's ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Griffith 1996Document10 pagesGriffith 1996Sowmya ANo ratings yet
- Early fluid resuscitation ...Document5 pagesEarly fluid resuscitation ...meganhamm04No ratings yet
- Emailing Wjssr-V3-Id1256Document3 pagesEmailing Wjssr-V3-Id1256Charbel AounNo ratings yet
- Maheshwari 2000Document3 pagesMaheshwari 2000Phuoc LeNo ratings yet
- Aijcr 2009 02 005Document6 pagesAijcr 2009 02 005Apps OmNo ratings yet
- Prospective & Comparative Study of Various Techniques Used in The Management of Liver Abscess in The Bundelkhand AreaDocument10 pagesProspective & Comparative Study of Various Techniques Used in The Management of Liver Abscess in The Bundelkhand AreaIJAR JOURNALNo ratings yet
- Clinicalinvestigation Non-VascularinterventionsDocument7 pagesClinicalinvestigation Non-VascularinterventionsSandu AlexandraNo ratings yet
- Regeneración Periodontal de Defectos Infraóseos HumanosDocument7 pagesRegeneración Periodontal de Defectos Infraóseos HumanosAgustin BuryakNo ratings yet
- Cheema2003 Article TimingOfLaparoscopicCholecysteDocument4 pagesCheema2003 Article TimingOfLaparoscopicCholecysteBandac AlexandraNo ratings yet
- SurgeryDocument7 pagesSurgeryFrancisco GilNo ratings yet
- Yan 2015Document4 pagesYan 2015ELIECERNo ratings yet
- Effect of Pelvic-Floor Re-Education On Duration and Degree of Incontinence After Radical Prostatectomy: A Randomised Controlled TrialDocument5 pagesEffect of Pelvic-Floor Re-Education On Duration and Degree of Incontinence After Radical Prostatectomy: A Randomised Controlled Trialpalomachagas1986No ratings yet
- Article Hernie InterneDocument4 pagesArticle Hernie Interneabdourahmane ndongNo ratings yet
- Post-cholecystectomy Bile Duct InjuryFrom EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNo ratings yet
- MPD and MPK Series Midi Io Details 02Document3 pagesMPD and MPK Series Midi Io Details 02Jorge David Monroy PerezNo ratings yet
- Crabs Hell Ms DsDocument1 pageCrabs Hell Ms DsRega Wahyu AnggrainiNo ratings yet
- The Myth of PlutoDocument6 pagesThe Myth of PlutoZsuzsanna ZöldNo ratings yet
- SteelDocument61 pagesSteelSonNguyenNo ratings yet
- Confucianism: By: Alisha, Mandy, Michael, and PreshiaDocument15 pagesConfucianism: By: Alisha, Mandy, Michael, and PreshiaAvi Auerbach AvilaNo ratings yet
- Techniques For Collection, Isolation and Preservation of MicroorganismsDocument42 pagesTechniques For Collection, Isolation and Preservation of Microorganismsaziskf100% (2)
- Fish JordanDocument29 pagesFish JordanSarah SobhiNo ratings yet
- Voltage Stability Enhancement in Power System Using STATCOM Based On Specific Coefficient Algorithm (SCA)Document7 pagesVoltage Stability Enhancement in Power System Using STATCOM Based On Specific Coefficient Algorithm (SCA)ElafanNo ratings yet
- Chemistry Practical Procedure Systematic Analysis of Salt STD: Xi & XiiDocument9 pagesChemistry Practical Procedure Systematic Analysis of Salt STD: Xi & XiivarshiniNo ratings yet
- Quickstart Dx35 de en FR Es PT ZH Ja It Ru Im0044955Document2 pagesQuickstart Dx35 de en FR Es PT ZH Ja It Ru Im0044955ROSSNo ratings yet
- Brown Et Al. 2009 Tribolium A Model For Developmental and Pest BiologyDocument9 pagesBrown Et Al. 2009 Tribolium A Model For Developmental and Pest BiologyAneel Nizar AliNo ratings yet
- User S Manual Bedienungsanleitung: Version 1.0 October 1998Document32 pagesUser S Manual Bedienungsanleitung: Version 1.0 October 1998Ojit QuizonNo ratings yet
- BS 03900 0 2010Document26 pagesBS 03900 0 2010selvaNo ratings yet
- Free/Open Source Multibody and Aerodynamic Software For Aeroelastic Analysis of Wind TurbinesDocument14 pagesFree/Open Source Multibody and Aerodynamic Software For Aeroelastic Analysis of Wind TurbinesFrankNo ratings yet
- Tech Mahindra Antonyms and QuestionsDocument27 pagesTech Mahindra Antonyms and QuestionsNehaNo ratings yet
- 1st Year Chemistry Sc1 ChemistryDocument896 pages1st Year Chemistry Sc1 Chemistrybiranchi satapathyNo ratings yet
- Pharmaceutics 14 02240Document17 pagesPharmaceutics 14 02240oliverasrommelNo ratings yet
- Construction Method (PICC)Document2 pagesConstruction Method (PICC)rheymar diwaNo ratings yet
- RABE - Sexual Imagery On The Phantasmagorical Castles at KhajurahoDocument30 pagesRABE - Sexual Imagery On The Phantasmagorical Castles at KhajurahoMarco PassavantiNo ratings yet
- Chapter No.1 Meat CookeryDocument15 pagesChapter No.1 Meat CookeryKrishna Chaudhary0% (1)
- Dit 24Document1 pageDit 24Abvolt IndiaNo ratings yet
- Brenes 2006Document6 pagesBrenes 2006Alfonso CáceresNo ratings yet
- prEN 12390-11 - DRAFTDocument32 pagesprEN 12390-11 - DRAFTCarlos GilNo ratings yet
- CBT JournalDocument82 pagesCBT JournalPaige Bayly100% (1)
- Mobil PajeroDocument2 pagesMobil Pajeroesemelekete wele2No ratings yet
- 6 Biomechanical Basis of Extraction Space Closure - Pocket DentistryDocument5 pages6 Biomechanical Basis of Extraction Space Closure - Pocket DentistryParameswaran ManiNo ratings yet
- What Aspects of "Life" Are Covered by Vedic AstrologyDocument4 pagesWhat Aspects of "Life" Are Covered by Vedic AstrologyMariana SantosNo ratings yet
- Cold Agglutinin DiseaseDocument4 pagesCold Agglutinin Diseasenavneet21usNo ratings yet
- Child - Cerebral PalsyDocument3 pagesChild - Cerebral PalsyJamie Icabandi67% (3)