Professional Documents
Culture Documents
Biennial Mammography and Disease-Stage Diagnoses: Pulmonology
Biennial Mammography and Disease-Stage Diagnoses: Pulmonology
Uploaded by
Kofi Frimpong-MansonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Biennial Mammography and Disease-Stage Diagnoses: Pulmonology
Biennial Mammography and Disease-Stage Diagnoses: Pulmonology
Uploaded by
Kofi Frimpong-MansonCopyright:
Available Formats
March 2013 ACPINTERNIST 11
PULMONOLOGY
Pulmonary continued from page 10
“Of all the patients that come here,
we make a diagnosis of PE in about 10% Modified Wells criteria Revised Geneva score
to 20% of patients,” Dr. Lim said.
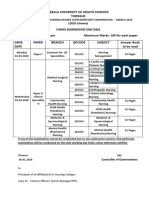
Criterion Score* Criterion Score*
However, given the deadly nature of
the condition, the old adage of “better safe Clinical signs or symptoms of DVT 3 Age older than 65 years 1
than sorry” still applies. Alternative diagnosis less likely Previous DVT or PE 3
“Keeping in mind that as a cause of sud- than PE 3
den death massive PE is second only to sud- Surgery (under general anesthetic) or
den cardiac death, it is certainly a risk cate- Heart rate 100 beats per minute 1.5 fracture (of the lower limbs) with the
past month 2
gory that should be not overlooked,” Dr. Immobilization (>3 days)
Harper said. or surgery in last 4 weeks 1.5 Active cancer 2
Physicians should keep particularly Previous history of DVT or PE 1.5 Unilateral lower-limb pain 3
close watch on patients older than 80 years
who have a significantly increased risk for Hemoptysis 1 Hemoptysis 2
PE, according to Dr. Harper. In addition, Active cancer within the last 6 months 1 Heart rate 75 to 94 beats per minute 3
physicians may want to give extra attention
to women who are pregnant; black patients, DVT = deep venous thrombosis; PE = pulmonary embolism. Heart rate 95 beats per minute or greater 5
Source: Lim W, Korenstein D. Physicians’ Information and
who tend to also have increased mortality Education Resource: Pulmonary embolism. Available to ACP Pain on lower-limb deep venous palpation
from PE; overweight patients; those who are members at http://pier.acponline.org/physicians/diseases/ and unilateral edema 4
otherwise healthy but have had a recent sur- d239/d239.html.
DVT= deep venous thrombosis; PE=pulmonary embolism. A score of 0-3 indicates low clinical
gery; or those who have recently traveled *Modified Wells criteria: <2 points = low risk for PE; 2-6 probability of PE, a score of 4-10 indicates intermediate probability, and a score of 11 or
for long periods involving immobility. points = moderate risk for PE; >6 points = high risk for PE. greater indicates high probability. Source: Le Gal G, Righini M, Roy PM, Sanchez O, Aujesky D,
Simplified Wells criteria: ≤4 points = PE unlikely; >4 points = Bounameaux H, et al. Prediction of pulmonary embolism in the emergency department: the
PE likely. revised Geneva score. Ann Intern Med. 2006;144:165-71. [PMID: 16461960]
Going with the gut
If a physician does not have D-dimer
testing or one of these clinical decision-
making tools available, it is still possible to ing an ongoing awareness of symptoms, using clinical judgment, a physician may there are specialized thrombosis clinics, it
ask questions that can uncover red flags. will help to ensure that patients who may still elect to do a CT scan.” is routine for primary care clinicians to refer
Questions outlined in the PIER module on have PE get the treatment that they need Ultimately, Dr. Hornbake said, physi- the patient to these clinics for diagnostic
pulmonary embolism include the following: quickly. However, clinicians shouldn’t rely cians should be informed by all the evi- testing.
■ Does the patient have a history of only on textbook definitions, according to dence accumulated in the last 15 years but Whether using clinical judgment or
cancer, recent trauma, surgery or a period Dr. Hornbake. should not underestimate the value of their the more proven pretest probability scores,
of immobilization? “For example, you may see a young own clinical judgment. Dr. Hornbake said that if PE is likely, treat-
■ Is the patient pregnant or taking a woman who is reporting symptoms and has “Admittedly, many physicians still use ment should begin promptly.
form of estrogen such as oral contraceptives just been put on oral contraceptives, and clinical judgment and probably incorporate “The decision of how and where to
or postmenopausal hormone therapy? also has a sister who had a fatal PE,” Dr. some of these pretest probability algorithms treat will vary based on the physician’s com-
■ Is there a history of venous throm- Hornbake said. “Using the Wells criteria, informally to decide whether PE is a likely fort level with treating PE,” Dr. Hornbake
boembolism in the family? she would be considered low risk, and she diagnosis or not,” Dr. Lim said. She added said. “You have to pick the fastest means of
Asking these questions, as well as hav- may also have a normal D-dimer level. But that in certain cities in Canada where getting the first dose into the patient.” A
IN THE NEWS
Biennial mammography and disease-stage diagnoses
Women age 66 to 89 years who under- Feb. 5 by the Journal of the National Cancer in this age group with no
go biennial screening mammography have Institute. comorbidity.
similar risk of advanced-stage disease and The proportion of women with adverse Researchers noted
lower cumulative risk of a false-positive tumor characteristics was similar among that there are 4.9 million
mammography study than those who are patients screened annually and biennially, U.S. women age 66 to 89
screened annually, regardless of comorbid- and there were no more adverse tumor char- years with comorbidities
ity, a study found. acteristics at diagnosis associated with less and 14.3 million women
Researchers sought to evaluate the frequent screening. Additionally, there was without comorbidities.
impact of biennial versus annual mammo- no association of tumor stage in patients They concluded, “If these
graphic screening in older women, and with comorbid illness versus those without women undergo annual
specifically whether the stage of disease comorbidities as assessed by the Charlson instead of biennial mam-
detected using this screening pattern would index, in contrast with previous studies. mography, this could
be affected by the presence of comorbid ill- Cumulative probability of a false-posi- result in approximately
ness in this population. tive result over 10 years of screening in one million additional
Data were prospectively collected on women at the lower age range of the study false-positive examina-
2,993 older women age 66 to 89 with inva- group (66 to 74 years) was higher among tions and 0.29 million
sive breast cancer or ductal carcinoma in those screened annually than among those additional false-positive
situ and 137,949 older women without screened biennially regardless of comorbid- biopsy recommenda-
breast cancer who underwent mammogra- ity: 48% (95% CI, 46.1% to 49.9%) of tions among women
phy from January 1999 to December 2006, women screened annually would have a with comorbidity plus 2.86 million addi- older women is unlikely to be performed,
and were then matched to Medicare claims. false-positive result compared with 29.0% tional false-positive examinations and 0.86 and therefore more high-quality observa-
The presence of comorbid illness in both (95% CI, 28.1% to 29.9%) of those screened million additional false-positive biopsy rec- tional studies that look at additional meas-
groups was quantified using the Charlson biennially. ommendations among women without ures of comorbidity and breast cancer mor-
index, a method that assigns a weighted Among women at the higher age range comorbidity. Thus, if older women undergo tality “may facilitate improved understand-
score to specific medical conditions and of the study group (75 to 89 years) with annual screening without consideration of ing of the benefits and harms of different
provides an indicator of disease burden; comorbidity, the rate of false-positives was the presence of comorbidity, it could result screening mammography frequencies
patients with a Charlson score of 0 in the 48.4% (95% CI, 46.1% to 50.8%) with annu- in substantial morbidity from screening among older women and, ultimately,
study were considered to have no comorbid al screening and 27.4% (95% CI, 26.5% to mammography.” inform clinical and policy decisions about
illness present. 28.4%) with biennial screening. Slightly The authors also noted that a random- the appropriate use of screening in this
Study results were published online lower estimates were obtained for women ized, controlled trial of mammography in growing population.” A
You might also like
- Pediatric Nursing Knowledge & Skills ChecklistDocument4 pagesPediatric Nursing Knowledge & Skills Checklistnorthweststaffing67% (3)
- American Board of Family Medicine: 2020 Questions & AnswersDocument112 pagesAmerican Board of Family Medicine: 2020 Questions & AnswersthanaaNo ratings yet
- Clinical Concept Map-7Document1 pageClinical Concept Map-7Brandi Offield100% (1)
- USMLE Step - 1 - Pathology - Vol.2 - Systematic Pathology - Chapters 10 - 28 - Kartik Carlo Rangaraj - 2013Document469 pagesUSMLE Step - 1 - Pathology - Vol.2 - Systematic Pathology - Chapters 10 - 28 - Kartik Carlo Rangaraj - 2013jisha mary sabuNo ratings yet
- Viral EncephalitisDocument36 pagesViral Encephalitishqayq100% (1)
- Pulmonary EmbolismDocument9 pagesPulmonary EmbolismGavin Texeirra100% (1)
- Discharge Counselling: by Margretta Odame Antwi Agcp, MPH, MPSGH, B. PharmDocument16 pagesDischarge Counselling: by Margretta Odame Antwi Agcp, MPH, MPSGH, B. PharmKofi Frimpong-Manson100% (4)
- Treating Vte Today: Practice Your Skills: Literature ReviewDocument14 pagesTreating Vte Today: Practice Your Skills: Literature ReviewOanaNo ratings yet
- Pulmonary Embolism: Clinical PracticeDocument13 pagesPulmonary Embolism: Clinical PracticeGustavo EduardoNo ratings yet
- Pulmonary EmbolismDocument13 pagesPulmonary EmbolismERISON REGONo ratings yet
- Afp 20200101 P 55Document3 pagesAfp 20200101 P 55adhiniNo ratings yet
- Clinical GuidelinesDocument8 pagesClinical Guidelinesong251183No ratings yet
- PE HeartofenglandDocument9 pagesPE HeartofenglandavfNo ratings yet
- Age-Adjusted D-Dimer Cutoff Levels To Rule Out Pulmonary Embolism The ADJUST-PE StudyDocument8 pagesAge-Adjusted D-Dimer Cutoff Levels To Rule Out Pulmonary Embolism The ADJUST-PE StudyRoxana Maria MunteanuNo ratings yet
- Peep1 s2.0 S0012369222002203 MainDocument10 pagesPeep1 s2.0 S0012369222002203 MainCarolina LassoNo ratings yet
- Tep Nejm 2022Document13 pagesTep Nejm 2022Jorge CastilloNo ratings yet
- 1 FullDocument4 pages1 FullphamdacNo ratings yet
- Diagnosisfor PEDocument28 pagesDiagnosisfor PEMohd Syaiful Mohd ArisNo ratings yet
- RecogniseCriticalIllness PDFDocument4 pagesRecogniseCriticalIllness PDFPutri Wulan SukmawatiNo ratings yet
- Pulmonary Embolism As Seen in The ED EditedDocument40 pagesPulmonary Embolism As Seen in The ED EditedSurgicalgownNo ratings yet
- Peripartum Cardiomyopathy: One Disease With Many FacesDocument3 pagesPeripartum Cardiomyopathy: One Disease With Many FacesVivi DeviyanaNo ratings yet
- Saddle Embolism in The Pulmonary Artery BifurcationDocument3 pagesSaddle Embolism in The Pulmonary Artery BifurcationAtiquzzaman RinkuNo ratings yet
- ASCP Corner Increased Risk of Cerebrovascular Adverse Events and Death in Elderly Demented PatienDocument1 pageASCP Corner Increased Risk of Cerebrovascular Adverse Events and Death in Elderly Demented PatienSantosh KumarNo ratings yet
- Botan's PE 2022Document69 pagesBotan's PE 2022Mimo HemadNo ratings yet
- Pulmonary Embolism 27 JanDocument8 pagesPulmonary Embolism 27 JanDeepak MulajkerNo ratings yet
- Tep 2023Document9 pagesTep 2023Sche Fra MediSiNo ratings yet
- Pulmonary Embolism (PE) - Acute Management - ABCDEDocument12 pagesPulmonary Embolism (PE) - Acute Management - ABCDESelamawit zerihunNo ratings yet
- Manejo de Trombosis PulmonarDocument8 pagesManejo de Trombosis PulmonarMartínz A. DiegoNo ratings yet
- Mitos y Realidades en TEP-1Document7 pagesMitos y Realidades en TEP-1Fernando atenciaNo ratings yet
- AdfgDocument9 pagesAdfgicha shafiraNo ratings yet
- Embolismo Pulmonar en Paciente OrtopedicoDocument10 pagesEmbolismo Pulmonar en Paciente OrtopedicoSOLEDAD GOMEZ FIGUEROANo ratings yet
- Clinical Reviews in Emergency MedicineDocument10 pagesClinical Reviews in Emergency MedicineJanetta RheaNo ratings yet
- Management of The Solitary Pulmonary NoduleDocument6 pagesManagement of The Solitary Pulmonary Nodulevictor ibarra romeroNo ratings yet
- Gomella 2009Document8 pagesGomella 2009Evelynππ θσυNo ratings yet
- Anticoagulante EP PDFDocument4 pagesAnticoagulante EP PDFMr. LNo ratings yet
- Brief Resolved Unexplained Event: Child Health UpdateDocument3 pagesBrief Resolved Unexplained Event: Child Health UpdateNATALIA LEMOS CALLENo ratings yet
- Diagnosis of Acute Pulmonary EmbolismDocument17 pagesDiagnosis of Acute Pulmonary Embolismpvs5155No ratings yet
- Acute PericarditisDocument7 pagesAcute PericarditisMirza AlfiansyahNo ratings yet
- Non G.I. Causes of Chronic Diarrhoea: OP KapoorDocument6 pagesNon G.I. Causes of Chronic Diarrhoea: OP KapoorchandanNo ratings yet
- Book-for - A دوسية من دكتور المقاصدDocument63 pagesBook-for - A دوسية من دكتور المقاصدAli Toma HmedatNo ratings yet
- Clinical ProjectDocument7 pagesClinical Projectapi-740498688No ratings yet
- AAOGUDocument6 pagesAAOGUGoran JosipovićNo ratings yet
- Diagnosis of Pulmonary Embolism During PregnancyDocument9 pagesDiagnosis of Pulmonary Embolism During PregnancyFátima AlmeidaNo ratings yet
- Troponin Assays: More Questions Than Answers?: Doi: 10.1111/j.1742-6723.2009.01225.xDocument2 pagesTroponin Assays: More Questions Than Answers?: Doi: 10.1111/j.1742-6723.2009.01225.xprashsubbuNo ratings yet
- Lung Ultrasound - Guided Emergency Department Management of Acute Heart Failure (BLUSHED-AHF)Document11 pagesLung Ultrasound - Guided Emergency Department Management of Acute Heart Failure (BLUSHED-AHF)Sara MendesNo ratings yet
- Is It Always Anterior Chest Pain Angina Pectoris?Document7 pagesIs It Always Anterior Chest Pain Angina Pectoris?Diana MinzatNo ratings yet
- Diagnosis and Exclusion of Pulmonary Embolism 2017Document14 pagesDiagnosis and Exclusion of Pulmonary Embolism 2017Julio César Ramos ZavalaNo ratings yet
- Validation of A Combined Comorbidity IndexDocument7 pagesValidation of A Combined Comorbidity IndexmarliivitorinoNo ratings yet
- Evaluation of The "Hemoptysis" Item in Clinical Decision Rules For The Diagnosis of Pulmonary Embolism in The Emergency DepartmentDocument8 pagesEvaluation of The "Hemoptysis" Item in Clinical Decision Rules For The Diagnosis of Pulmonary Embolism in The Emergency DepartmentNiatazya Mumtaz SagitaNo ratings yet
- Managing Pulmonary EmbolismDocument9 pagesManaging Pulmonary EmbolismBolívar IseaNo ratings yet
- Comparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismDocument8 pagesComparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismAlirio Rodrigo Bastidas GoyesNo ratings yet
- Deep Vein Thrombosis - Current Management Strategies: Heike Endig, Franziska Michalski and Jan Beyer-WestendorfDocument10 pagesDeep Vein Thrombosis - Current Management Strategies: Heike Endig, Franziska Michalski and Jan Beyer-WestendorfYantoNo ratings yet
- Solutions Beyond Drug Treatment: Your HealthDocument5 pagesSolutions Beyond Drug Treatment: Your HealthTimes MediaNo ratings yet
- Appendix StudyDocument5 pagesAppendix StudySunil RevankarNo ratings yet
- CEPI5100 M10 V2 HandoutDocument8 pagesCEPI5100 M10 V2 HandoutKarsana ParameswaranNo ratings yet
- M33 - Stase IPD - Hassan Assagaf Guidance For The Treatment of Deep Vein Thrombosis and Pulmonary EmbolismDocument16 pagesM33 - Stase IPD - Hassan Assagaf Guidance For The Treatment of Deep Vein Thrombosis and Pulmonary EmbolismHasan AssegafNo ratings yet
- Pediatric Hypertension Noon Conference 03.20.2019Document44 pagesPediatric Hypertension Noon Conference 03.20.2019Emily EresumaNo ratings yet
- Jaha 121 024425Document30 pagesJaha 121 024425Florencia TraficanteNo ratings yet
- Case #4 Asthma (BSN3F, Group3)Document19 pagesCase #4 Asthma (BSN3F, Group3)Eduard GarchitorenaNo ratings yet
- Acute DyspneaDocument37 pagesAcute Dyspneaisnaira imamNo ratings yet
- CaravagioDocument9 pagesCaravagiomohamed baba ahmedNo ratings yet
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Chronic Migraine Lab MethodDocument8 pagesChronic Migraine Lab MethodKofi Frimpong-MansonNo ratings yet
- All Bells in Paradise Rutter PDFDocument10 pagesAll Bells in Paradise Rutter PDFKofi Frimpong-MansonNo ratings yet
- 13 Priapism LRDocument11 pages13 Priapism LRKofi Frimpong-MansonNo ratings yet
- Envenomations: Wonder Abotsi, PHDDocument123 pagesEnvenomations: Wonder Abotsi, PHDKofi Frimpong-Manson100% (1)
- Thanks Be To GodDocument9 pagesThanks Be To GodKofi Frimpong-Manson100% (1)
- Protect Yourself From Mosquito BitesDocument1 pageProtect Yourself From Mosquito BitesKofi Frimpong-MansonNo ratings yet
- The History of BioethicsDocument2 pagesThe History of BioethicsKofi Frimpong-MansonNo ratings yet
- Antifungals AgentsDocument58 pagesAntifungals AgentsKofi Frimpong-MansonNo ratings yet
- A Report On Six Weeks Experiential Training at Kwadaso S.D.A. Hospital, KumasiDocument8 pagesA Report On Six Weeks Experiential Training at Kwadaso S.D.A. Hospital, KumasiKofi Frimpong-MansonNo ratings yet
- Presentation On Organic ChemistryDocument44 pagesPresentation On Organic ChemistryKofi Frimpong-MansonNo ratings yet
- Students Loan Application GuidelinesDocument8 pagesStudents Loan Application GuidelinesKofi Frimpong-MansonNo ratings yet
- RRLDocument3 pagesRRLKevin M. VillacorteNo ratings yet
- Knowledge Deficit Related To HypertensionDocument2 pagesKnowledge Deficit Related To HypertensionChenee Mabulay100% (1)
- 1st Internal Assessment Pharmacology 28.7.21 FinalDocument2 pages1st Internal Assessment Pharmacology 28.7.21 FinalSubhom MajumderNo ratings yet
- Autism Spectrum Disorder: Special Education and Language Therapy Cognitive Behavioral Therapy For Anxiety and AgitationDocument5 pagesAutism Spectrum Disorder: Special Education and Language Therapy Cognitive Behavioral Therapy For Anxiety and AgitationMuslim AqeelNo ratings yet
- COVID CONCEPTS - CBQ - Dr. GragedaDocument4 pagesCOVID CONCEPTS - CBQ - Dr. GragedaKonstantin KonstantiusNo ratings yet
- Hearing Aid InformationDocument22 pagesHearing Aid InformationDeepakRodeyNo ratings yet
- ITI Study Club-May EventDocument2 pagesITI Study Club-May EventS. BenzaquenNo ratings yet
- Diagnostic LaparosDocument11 pagesDiagnostic LaparosDr-Shadi MeteirNo ratings yet
- Nimotuzumab A Novel anti-EGFR Monoclonal PDFDocument8 pagesNimotuzumab A Novel anti-EGFR Monoclonal PDFAkbar SuuryoNo ratings yet
- ESAMCC7Document206 pagesESAMCC7jeremy_raineyNo ratings yet
- Don'T Exercise Cellercise!: by Rica E. VillalonDocument21 pagesDon'T Exercise Cellercise!: by Rica E. VillalonMónica SastoqueNo ratings yet
- Fajo 990Document238 pagesFajo 990Mohamed A SalehNo ratings yet
- Dried Ivy Leaf ExtractDocument3 pagesDried Ivy Leaf Extractfauzan26No ratings yet
- Albumin and Malnutrition AssessmentDocument22 pagesAlbumin and Malnutrition AssessmentLynette MiaqueNo ratings yet
- HemiparesisDocument35 pagesHemiparesisIsabela IacobNo ratings yet
- Coagulation of BloodDocument21 pagesCoagulation of BloodHery StiawanNo ratings yet
- Home Care For EpilepsyDocument16 pagesHome Care For Epilepsysanish4uNo ratings yet
- VHA NCPS Fall Prevention and ManagementDocument7 pagesVHA NCPS Fall Prevention and ManagementEvaNo ratings yet
- Isotonic Volume ImbalancesDocument12 pagesIsotonic Volume ImbalancesEnna PaulaNo ratings yet
- Thyroid DisorderDocument19 pagesThyroid DisorderBudi AthAnza SuhartonoNo ratings yet
- Kerala University of Health Sciences Thrissur: (2010 Scheme)Document1 pageKerala University of Health Sciences Thrissur: (2010 Scheme)subiNo ratings yet
- Premature LabourDocument3 pagesPremature LabourAnonymous Q236bSNo ratings yet
- Pediatric Nursing GastroDocument3 pagesPediatric Nursing GastronieacatleyaNo ratings yet
- The Beatles - The Noble PrizeDocument7 pagesThe Beatles - The Noble PrizeJuanitaNo ratings yet
- BLSPPT 180126100212 PDFDocument58 pagesBLSPPT 180126100212 PDFJerwynn Ilustre100% (1)
- Quantitative Flow Cytometry in The Clinical LaboratoryDocument20 pagesQuantitative Flow Cytometry in The Clinical Laboratorykmaher8256No ratings yet
- Assignment - Physiology Lab ReportDocument3 pagesAssignment - Physiology Lab ReportElizalde Husband100% (2)
- Manuver Head Tilt-Chin Lift-Jaw ThrustDocument6 pagesManuver Head Tilt-Chin Lift-Jaw ThrustKevin CindarjoNo ratings yet