Professional Documents
Culture Documents
ISK - Diagnosis Pada Bayi Dan Anak
ISK - Diagnosis Pada Bayi Dan Anak
Uploaded by
Qurratul AiniCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Project Report Heimalya HerbalDocument78 pagesProject Report Heimalya Herbalkeshu75% (4)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- BBM521/03 Research Methods Jan 2014: Tutor-Marked Assignment 2 (TMA 2 - 20%)Document3 pagesBBM521/03 Research Methods Jan 2014: Tutor-Marked Assignment 2 (TMA 2 - 20%)Shiyun SeNo ratings yet
- Exploration in The New Millenium: Coordinator: Bill Coker BHP Billiton World Exploration IncDocument6 pagesExploration in The New Millenium: Coordinator: Bill Coker BHP Billiton World Exploration Incalvaro MNo ratings yet
- Applied Statistics in Occupational PDFDocument199 pagesApplied Statistics in Occupational PDFFitri Jasmine AndrianiNo ratings yet
- Laboratory Quality Control Based Risk ManagementDocument12 pagesLaboratory Quality Control Based Risk ManagementPedro C. Jardon0% (1)
- Career Path PDFDocument2 pagesCareer Path PDFЕкатерина НестероваNo ratings yet
- Quality of Service Assessment On Some Major Mobile Network Operators in GhanaDocument7 pagesQuality of Service Assessment On Some Major Mobile Network Operators in GhanaJonah JayNo ratings yet
- Measure of Central TendancyDocument27 pagesMeasure of Central TendancySadia HakimNo ratings yet
- Audit Engagement Questionnaire: Review Questions For Audit EngagementsDocument25 pagesAudit Engagement Questionnaire: Review Questions For Audit EngagementsRSA ArcherNo ratings yet
- The Scientific AttitudeDocument2 pagesThe Scientific AttitudeDaniel FrazónNo ratings yet
- Syllabus TESP 302-4Document17 pagesSyllabus TESP 302-4Devin BlackwoodNo ratings yet
- 2013 Book Icord13Document1,404 pages2013 Book Icord13Rafael Mena FredesNo ratings yet
- Bilingual Mental Lexicon and Translation: A Psycholinguistic Study of Bengali-English Language PairsDocument18 pagesBilingual Mental Lexicon and Translation: A Psycholinguistic Study of Bengali-English Language PairsSouvik BaruaNo ratings yet
- BBDM2063 Cross-Cultural Studies Revised 20130904Document7 pagesBBDM2063 Cross-Cultural Studies Revised 20130904preetimutiarayNo ratings yet
- ds10 Bouncing Slime LabDocument7 pagesds10 Bouncing Slime Labapi-110789702No ratings yet
- IEEE Education Society Papers-05535216Document8 pagesIEEE Education Society Papers-05535216Anoop MathewNo ratings yet
- Module 5. T-Test One Sample TestDocument5 pagesModule 5. T-Test One Sample TestBelle AmeNo ratings yet
- TQM IMP Questions - MBA III Semester-OUDocument2 pagesTQM IMP Questions - MBA III Semester-OUsrinivas nallakuntaNo ratings yet
- Data Structures and Algorithms Design (Regular) DSE PDFDocument9 pagesData Structures and Algorithms Design (Regular) DSE PDFsrirams007No ratings yet
- Colleges of Education Evaluation Form: National Accreditation BoardDocument33 pagesColleges of Education Evaluation Form: National Accreditation Boardsarah AKPONo ratings yet
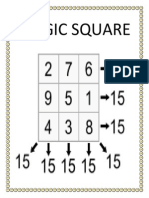
- Magic SquareDocument15 pagesMagic SquaresembeNo ratings yet
- Literature Review of Tuition Impact On Learning of StudentsDocument33 pagesLiterature Review of Tuition Impact On Learning of StudentsAsma Akram50% (4)
- MBA Assignment Topics 2011-12Document11 pagesMBA Assignment Topics 2011-12chitraNo ratings yet
- Review of Related Literature and Studies Related LiteratureDocument6 pagesReview of Related Literature and Studies Related LiteratureLeonard MedinaNo ratings yet
- Human Language As A Unique Human PossessionDocument2 pagesHuman Language As A Unique Human PossessionDahlia Galvan- MaglasangNo ratings yet
- RUL 670 - Research ProposalDocument28 pagesRUL 670 - Research Proposalxin suNo ratings yet
- CH 03Document11 pagesCH 03Atika AisyahNo ratings yet
- Chloe Wong ResumeDocument2 pagesChloe Wong ResumeChloe WongNo ratings yet
- Adb9 Bsbpmg517 Manage Project RiskDocument140 pagesAdb9 Bsbpmg517 Manage Project RiskLili Pabuena VillarrealNo ratings yet
- Sip Banana FinalDocument31 pagesSip Banana FinalAmran BhuiyanNo ratings yet
ISK - Diagnosis Pada Bayi Dan Anak
ISK - Diagnosis Pada Bayi Dan Anak
Uploaded by
Qurratul AiniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ISK - Diagnosis Pada Bayi Dan Anak
ISK - Diagnosis Pada Bayi Dan Anak
Uploaded by
Qurratul AiniCopyright:
Available Formats
ORIGINAL CONTRIBUTION
Recurrent Urinary Tract Infections in Children
Risk Factors and Association With Prophylactic Antimicrobials
Patrick H. Conway, MD, MSc Context The evidence regarding risk factors for recurrent urinary tract infection (UTI)
Avital Cnaan, PhD and the risks and benefits of antimicrobial prophylaxis in children is scant.
Theoklis Zaoutis, MD, MSCE Objectives To identify risk factors for recurrent UTI in a pediatric primary care co-
Brandon V. Henry, BS hort, to determine the association between antimicrobial prophylaxis and recurrent
UTI, and to identify the risk factors for resistance among recurrent UTIs.
Robert W. Grundmeier, MD
Design, Patients, and Setting From a network of 27 primary care pediatric prac-
Ron Keren, MD, MPH tices in urban, suburban, and semirural areas spanning 3 states, a cohort of children
aged 6 years or younger who were diagnosed with first UTI between July 1, 2001,
E
STIMATES OF CUMULATIVE INCI- and May 31, 2006, was assembled. Time-to-event analysis was used to determine risk
dence of urinary tract infec- factors for recurrent UTI and the association between antimicrobial prophylaxis and
tion (UTI) in children younger recurrent UTI, and a nested case-control study was performed among children with
than 6 years (3%-7% in girls, recurrent UTI to identify risk factors for resistant infections.
1%-2% in boys) suggest that 70 000 to Main Outcome Measures Time to recurrent UTI and antimicrobial resistance of
180 000 of the annual US birth cohort recurrent UTI pathogens.
will have experienced a UTI by age 6 Results Among 74 974 children in the network, 611 (0.007 per person-year) had a
years.1-3 Very few studies have evalu- first UTI and 83 (0.12 per person-year after first UTI) had a recurrent UTI. In multi-
ated the risk of recurrent UTI, and none variable Cox time-to-event models, factors associated with increased risk of recurrent
have studied children with UTI iden- UTI included white race (0.17 per person-year; hazard ratio [HR], 1.97; 95% confi-
tified and managed in a primary care dence interval [CI], 1.22-3.16), age 3 to 4 years (0.22 per person-year; HR, 2.75; 95%
setting. Most prior studies have esti- CI, 1.37-5.51), age 4 to 5 years (0.19 per person-year; HR, 2.47; 95% CI, 1.19-5.12),
mated 6- to 12-month UTI recurrence and grade 4 to 5 vesicoureteral reflux (0.60 per person-year; HR, 4.38; 95% CI, 1.26-
15.29). Sex and grade 1 to 3 vesicoureteral reflux were not associated with risk of
rates of 20% to 48%, but these esti-
recurrence. Antimicrobial prophylaxis was not associated with decreased risk of re-
mates may be exaggerated because they current UTI (HR, 1.01; 95% CI, 0.50-2.02), even after adjusting for propensity to re-
typically were derived from referral ceive prophylaxis, but was a risk factor for antibimicrobial resistance among children
populations with multiple previous with recurrent UTI (HR, 7.50; 95% CI, 1.60-35.17).
UTIs or from trials in which children Conclusion Among the children in this study, antimicrobial prophylaxis was not as-
were catheterized without symptoms, sociated with decreased risk of recurrent UTI, but was associated with increased risk
in which case positive culture results of resistant infections.
may represent asymptomatic bacteri- JAMA. 2007;298(2):179-186 www.jama.com
uria.1,4-9
The 1999 American Academy of Pe-
ing and treatment strategy is a theo- scarring.13-15 However, there is a pau-
diatrics practice guideline for manage-
retical model that links VUR to an in- city of evidence for this model,9 and re-
ment of children after first UTI recom-
creased risk of recurrent UTI and renal cent small clinical trials evaluating the
mends an imaging study to evaluate for
the presence and degree of vesicoure-
Author Affiliations: Robert Wood Johnson Founda- Informatics (Dr Grundmeier), Children’s Hospital of Phila-
teral reflux (VUR),10 a condition pre- tion Clinical Scholars Program (Dr Conway), Leonard delphia; and Center for Health Care Quality and Divi-
sent in approximately 30% to 40% of Davis Institute of Health Economics (Drs Conway, Zaou- sion of General Pediatrics, Cincinnati Children’s Hospi-
tis, and Keren), Center for Clinical Epidemiology and Bio- tal Medical Center, Cincinnati, Ohio (Dr Conway).
children with UTI.11 If the child has statistics (Drs Conway, Cnaan, Zaoutis, and Keren), and Corresponding Author: Patrick H. Conway, MD, MSc,
VUR, daily antimicrobial prophylaxis School of Medicine (Mr Henry), University of Pennsyl- Robert Wood Johnson Clinical Scholars Program, Uni-
vania, Philadelphia; Division of General Pediatrics (Drs versity of Pennsylvania, 423 Guardian Dr, Blockley Hall
is recommended to prevent recurrent Conway, Zaoutis, and Keren), Division of Biostatistics 1303A, Philadelphia, PA 19104 (pconway2@mail.med
UTIs.11,12 The basis for this VUR screen- and Epidemiology (Dr Cnaan), and Center for Biomedical .upenn.edu).
©2007 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2007—Vol 298, No. 2 179
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
tors for resistant organisms as the cause viewed the patients’ EHR and manu-
Figure. Primary Care Cohort
of the recurrent UTI. Power and ally entered urine antimicrobial
74 974 Children aged 6 years
sample-size calculations indicated that sensitivity and VCUG results into the
or younger with at least 77 patients with recurrent UTI were research database.
2 clinic visits
needed to have 90% power to detect a To minimize missing results from
775 With record of urinary
hazard ratio of 1.5, assuming a 15% re- outside the network, we also searched
tract infection currence rate, type I error of .05, and the electronic and paper charts for cor-
1-year follow-up. respondence from outside hospitals and
164 Excluded
91 Previous UTI
clinics and included any results ob-
55 Observation time <24 d Setting tained outside the network. All data ele-
17 Comorbid conditions
1 UTI diagnosed by Patients were drawn from a network ments were validated with the patient
bag specimen
of 27 primary care pediatric practices chart as the gold standard on a 5% ran-
611 With first UTI included
spanning 3 states (Delaware, New Jer- dom sample of patients, and all pre-
in analysis sey, and Pennsylvania) that share a sumed patients with higher acuity (⬎2
common electronic health record hospitalizations). Abstracted data
83 With recurrent UTI (EHR) managed by The Children’s agreed with the gold standard for all
Hospital of Philadelphia. The prac- data elements with greater than 95%
UTI indicates urinary tract infection.
tices are located in urban, suburban, sensitivity and specificity.
and semirural locations. The institu-
efficacy of prophylaxis have demon- tional review board of The Children’s Patients
strated no protective effect for prevent- Hospital of Philadelphia approved the The initial cohort (FIGURE) was de-
ing recurrent UTI and renal scar- study, waiving the need for patient fined as all children aged 6 years or
ring.5,16 Moreover, concerns have been consent. younger with at least 2 clinic visits be-
raised about the potential harm of an- tween July 1, 2001, and May 31, 2006
timicrobial prophylaxis because of its Data Sources (N=74 974). Two clinic visits were re-
potential to breed resistant organisms Data were extracted from the EHR used quired so that observation time could
that can cause recurrent UTIs.17 by the 27 primary care pediatric prac- be accrued. Microbiology records in the
Given the limited information tices in the research network. In addi- EHR for these children were queried for
regarding risk factors for recurrent tion to data entered at the point of care, presence of positive urine culture re-
UTI and the risks and benefits of anti- the EHR is automatically populated sults, defined as 50 000 colony-
microbial prophylaxis, we sought to with administrative and results data forming units/mL or greater of a single
(1) identify risk factors for recurrent from several other sources, including organism considered to be a urinary
UTI in a pediatric primary care the children’s hospital emergency de- tract pathogen, a criterion previously
cohort, (2) examine the association partment and main hospital as well as validated for catheterized specimens;
between prophylactic antimicrobials 2 laboratory vendors in the tri-state area 775 children who had experienced a
and recurrent UTI, and (3) determine (Quest Diagnostics [Lyndhurst, New first UTI were identified.18
the risk factors for resistance among Jersey] and LabCorp [Raritan, New The electronic and paper records (in-
recurrent UTIs. Jersey]). cluding correspondence from outside
Documents and results obtained hospitals and clinics, problem lists, visit
METHODS from hospitals and emergency depart- notes, and microbiology results) of all
Design ments outside the network also can be children with positive urine culture re-
We assembled a cohort of children aged scanned or manually entered into the sults were manually reviewed, and any
6 years or younger who were diag- EHR by practice staff. The EHR con- child with history of a previous UTI was
nosed with first UTI between July 1, tains demographic and clinic visit in- excluded (n = 91). To provide suffi-
2001, and May 31, 2006. Time-to- formation, laboratory data, radiology re- cient observation time to develop a re-
event analyses were used to determine sults, comorbid conditions coded using current UTI (at least 14 days after a typi-
risk factors for recurrent UTI and ef- the International Classification of Dis- cal 10-day treatment course), children
fectiveness of antimicrobial prophy- eases, Ninth Revision (ICD-9), and de- with fewer than 24 days of observa-
laxis. Time to event was defined as the tailed prescription data that were elec- tion time (n=55) were excluded. To as-
time from first UTI until recurrent UTI tronically extracted into the research semble a cohort representative of oth-
(event of interest) or until last clinic database. Antimicrobial sensitivity re- erwise well children in the community,
visit (observation censored without sults for urinary pathogens and re- we excluded 17 children with the fol-
event occurring). Among children with sults for voiding cystourethrogram lowing comorbid conditions defined a
recurrent UTI, a nested case-control (VCUG) could not be reliably ex- priori based on ICD-9 codes from the
study was performed to identify risk fac- tracted electronically; therefore, we re- EHR: malignancy (140-239.xx), diabe-
180 JAMA, July 11, 2007—Vol 298, No. 2 (Reprinted) ©2007 American Medical Association. All rights reserved.
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
tes (250.xx), human immunodefi- cluding fever, dysuria, and/or urinary tic and other antimicrobial exposure
ciency virus (042), other congenital im- frequency. In the nested study of chil- were considered time-varying vari-
munodeficiencies (279.xx), sickle cell dren with recurrent UTI, the outcome ables, coded as “0” on days without
disease (282.6), neurogenic bladder and was resistance among recurrent UTIs. prescribed antimicrobials and “1” on
paralytic syndromes (343-344.xx), hy- Resistance was defined as a pathogen days that antimicrobials were pre-
pertensive renal disease (403.xx), ne- resistant to any antimicrobial. scribed. This approach allowed accu-
phritis and renal failure (580-589.xx), rate modeling of the intermittent
renal calculi (592, 594), kidney disor- Exposures nature of the antimicrobial exposure
ders (593.xx, except hydroureter and Exposure variables were defined a priori and accounting for the effect of pro-
VUR), chronic cystitis (595.xx, ex- as age at first UTI, sex, race, VCUG re- phylaxis on a daily basis for each
cept 595.0, acute cystitis), bladder and sult, prophylactic antimicrobial expo- child. Multivariable Cox survival-time
urethra disorders (596, 598, and 599, sure on a daily basis, and other antimi- regression was then performed to
except 599.0 UTI), central nervous sys- crobial exposure on a daily basis. identify risk factors for recurrent UTI.
tem malformation (eg, myelomeningo- Antimicrobial prophylaxis prescrip- A stratified analysis (defined a priori)
cele; 655.0), and congenital anoma- tions were identified through a query was performed for antimicrobial pro-
lies of the urinary system (753.xx). We of electronic prescription records using phylaxis hazard ratio by sex, age, race,
also excluded 1 child with a urine cul- antimicrobial names, key terms such as and VUR status to evaluate for effect
ture collected from a bag specimen. prophylaxis, and duration of prescrip- modification. To control for potential
tion. Each identified prescription, confounding by indication that could
Outcomes blinded to the patient’s outcome, was occur if physicians prescribed prophy-
Because children entered the cohort at then manually reviewed to verify that laxis based on factors that increased the
different times and had different lengths it represented UTI antimicrobial pro- risk of recurrence, a propensity score
of follow-up, time to recurrent UTI was phylaxis. Any antimicrobial prescrip- also was developed for receipt of anti-
used as the primary outcome. The ob- tion not considered UTI prophylaxis microbial prophylaxis, based on sex,
servation-time end point was defined was categorized as “other antimicro- race, age at first UTI, and VCUG re-
conservatively as the last clinic visit as bial exposure.” VUR grade was based sult.20 The propensity score model pre-
opposed to the end of study, because on the maximum grade on either side dicted receipt of prophylactic antimi-
we did not want to assume that chil- of the urinary collecting system. Re- crobials with good accuracy (c statistic,
dren were still within the primary care sults of VCUG were categorized a priori 0.81). We reanalyzed the effect of pro-
network past their last documented as “not performed,” “normal,” “VUR phylaxis in analyses stratified by quin-
clinic visit. Recurrent UTI was de- grade 1-3,” and “VUR grade 4-5.”19 tile of propensity score and in multi-
fined by a second positive urine cul- Age was analyzed both ordinally by variable analyses controlling for
ture result 2 or more weeks after the ter- year and dichotomized as age younger propensity score as a continuous and
mination of therapy for the first UTI. than 2 years vs 2 to 6 years, based on categorical (quintiles) variable.
Of children with documented urine guidelines for imaging and prophy- For comparison of resistant vs non-
collection methods, only 1 had urine laxis specifically applying to children resistant recurrent UTIs, univariable
collected via bag specimen (ex- younger than 2 years.10,12 Race and eth- logistic regression was performed to
cluded); all but 2 younger than 2 years nicity were reported by parents in the measure the association between sex,
via catheterization; and all but 1 older EHR. Less than 3% of the patients were race, age at first UTI, VCUG result,
than 2 years via clean catch. Since col- Hispanic, so ethnicity was not evalu- prophylactic antimicrobial exposure,
lection included specimens collected via ated separately. Race was considered as and other antimicrobial exposure to
both catheterization and clean-catch, a white vs nonwhite, as there were less the outcome of resistance. Since this
sensitivity analysis also was per- than 3% Asian and no Native Ameri- was not a time-to-event analysis, the
formed in which results were recalcu- can patients. antimicrobial exposure variable was
lated using a cutoff of 100 000 colony- defined as ever prescribed vs never
forming units/mL or greater of a single Data Analysis prescribed. The predicted probability
organism. First, the incidence rates were calcu- of the recurrent UTI being antimicro-
A survey of network nurse manag- lated for first and recurrent UTI. bial resistant for each combination of
ers indicated that cultures were Single-variable time-to-event analysis exposures was calculated based on the
obtained only if UTI symptoms were was performed for each exposure vari- multivariable model (STATA predict
present; to validate this claim, we per- able to determine the hazard ratio command). All analyses were per-
formed a 20% random sample chart re- (HR) for the outcome of interest, time formed using STATA SE version 9.1
view of progress notes at UTI diagno- to recurrent UTI. Sex, race, age at first (StataCorp, College Station, Texas);
sis to evaluate for presence of symptoms UTI, and VCUG result were consid- P ⬍ .05 was considered statistically
documented consistent with UTI, in- ered fixed-time exposures. Prophylac- significant.
©2007 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2007—Vol 298, No. 2 181
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
RESULTS not have documented urine leukocyte
Table 1. First and Recurrent Urinary Tract
Infection (UTI) in The Children’s Hospital of Clinical Characteristics esterase and nitrite results. Of chil-
Pennsylvania Primary Care Cohort A total of 74 974 children aged 6 years dren with results, 473 (91%) of those
No. (%) or younger had at least 2 clinic visits with first UTI and 68 (95%) of those
between July 1, 2001, and May 31, with recurrent UTI had a positive uri-
First UTI Recurrent UTI
Characteristic (n = 611) (n = 83) 2006. Among these children, 666 had nalysis result, defined as presence of
Sex experienced a confirmed first UTI and leukocyte esterase or nitrites.18,21 In re-
Male a 68 (11.1) 8 (9.6) had no significant comorbid condi- view of progress notes for a 20% ran-
Female 543 (88.9) 75 (90.4) tions, resulting in a first-UTI inci- dom sample of first and recurrent UTI
Race
White 343 (56.1) 54 (65.1) dence rate in otherwise healthy chil- events, all children had symptoms con-
Nonwhite 268 (43.9) 29 (34.9) dren of 0.007 per person-year. Fifty- sistent with UTI including fever, dys-
Age, y five children had fewer than 24 days of uria, and/or urinary frequency at the
⬍2 236 (38.6) 26 (31.3) observation, leaving 611 children in the time of diagnosis. The mean observa-
2-6 375 (61.4) 57 (68.7) final analytic cohort. Eighty-three tion time for the cohort with first UTI
VCUG result (13.6%) of these children experienced was 408 days (median, 310 days; in-
Not performed 400 (65.5) 52 (62.7)
Normal 154 (25.2) 20 (24.1) a recurrent UTI, resulting in a recur- terquartile range, 150-584 days).
VUR grade 1-3 50 (8.2) 8 (9.6) rent UTI incidence rate of 0.12 per per- The majority of the 611 children with
VUR grade 4-5 7 (1.1) 3 (3.6) son-year (12% recurrence per year). first UTI were female (543 [88.9%]),
Any exposure to Fifty-one (61%) of these recurrent UTIs white (343 [56.1%]), and aged 2 to 6
antimicrobial were caused by a pathogen with anti- years (375 [61.4%]). Most did not have
prophylaxis
No 483 (79.1) 64 (77.1) microbial resistance. Pathogens in- a VCUG performed (400 [65.5%]) and
Yes 128 (20.9) 19 (22.9) cluded Escherichia coli (78%), other had not received antimicrobial prophy-
Abbreviations: VCUG, voiding cystourethrogram; VUR, vesi- gram-negative rods (16%), Enterococ- laxis (483 [79.1%]) (TABLE 1). Chil-
coureteral reflux.
a Among male children, there was no documented circum- cus (4%), and other organisms (2%). dren younger than 2 years were more
cision status for 32 (47%); of those with documented sta-
tus, 26 (38%) were uncircumcised, and 10 (15%) were
Fifteen percent of children in both the likely to have a VCUG performed (137
circumcised. first and the recurrent UTI groups did [58%]) compared with children older
than 2 years (75 [20%]). Prophylactic
antimicrobials prescribed included cot-
Table 2. Time-to-Event Analysis for Risk of Recurrent Urinary Tract Infection (UTI) a rimoxazole (61%), amoxicillin (29%),
HR (95% CI) nitrofurantoin (7%), and other antimi-
Characteristic Univariable Multivariable b crobials including first- through third-
Sex generation cephalosporins (3%). Of the
Male 1 [Reference] 1 [Reference] 68 male children, there was no docu-
Female 1.20 (0.58-2.50) 1.08 (0.51-2.30) mented circumcision status for 32
Race (47%). Twenty-six (38%) were uncir-
Nonwhite 1 [Reference] 1 [Reference]
White 1.99 (1.26-3.16) c 1.97 (1.22-3.16) c
cumcised and 10 (15%) were circum-
Age, y cised.
⬍1 1 [Reference] 1 [Reference]
1 to ⬍2 0.99 (0.43-2.27) 1.05 (0.20-3.37) Risk of Recurrent UTI
2 to ⬍3 1.22 (0.51-2.95) 1.26 (0.51-3.07) and Association With
3 to ⬍4 2.55 (1.33-4.81) c 2.75 (1.37-5.51) c Antimicrobial Prophylaxis
4 to ⬍5 2.17 (1.10-4.29) c 2.47 (1.19-5.12) c In both univariable and multivariable
5 to ⱕ6 1.36 (0.66-2.80) 1.62 (0.73-3.62)
Cox survival time regression (TABLE 2),
VCUG
Normal result 1 [Reference] 1 [Reference] the risk of recurrent UTI was in-
Not performed 1.00 (0.60-1.68) 0.70 (0.40-1.21) creased by white race (0.17 per person-
VUR grade 1-3 1.17 (0.52-2.66) 1.05 (0.43-2.57) year; multivariable HR, 1.97; 95% con-
VUR grade 4-5 4.59 (1.36-15.47) d 4.38 (1.26-15.29) d fidence interval [CI], 1.22-3.16), age 3
Antimicrobial prophylaxis e 1.05 (0.57-1.94) 1.01 (0.50-2.02) f to 4 years (0.22 per person-year; mul-
Abbreviations: CI, confidence interval; HR, hazard ratio; VCUG, voiding cystourethrogram; VUR, vesicoureteral reflux.
a Time-to-event analysis performed from date of first UTI until event, recurrent UTI, or last clinic visit within the network.
tivariable HR, 2.75; 95% CI, 1.37-
b Multivariable time-to-event analysis controlling for sex, race, age, VCUG result, and time-varying exposure to antimi- 5.51), age 4 to 5 years (0.19 per person-
crobial prophylaxis. year; multivariable HR, 2.47; 95% CI,
c P ⬍ .01.
d P ⬍ .05.
e Exposure to antimicrobial prophylaxis was modeled as a time-varying covariate on a daily basis to take into account
1.19-5.12), and grade 4 to 5 VUR (0.60
the intermittent nature of exposure and provide the most powerful estimate of its effect over time. per person-year; multivariable HR, 4.38;
f Adjusting antimicrobial prophylaxis by propensity score quintile, continuous propensity score, and propensity score in
addition to all covariates produced HRs of 1.03, 1.02, and 1.01, respectively.
95% CI, 1.26-15.29). When age was
considered as a dichotomous variable,
182 JAMA, July 11, 2007—Vol 298, No. 2 (Reprinted) ©2007 American Medical Association. All rights reserved.
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
2- to 6-year olds had significantly in-
Table 3. Risk of Antimicrobial Resistance Among Children With Recurrent Urinary Tract
creased risk of recurrent UTI (HR, 2.01; Infection (UTI)
95% CI, 1.20-3.37). Sex, grade 1 to 3 Resistant UTIs, Antimicrobial-Resistant
VUR, and other antimicrobial expo- Characteristic No. (%) Recurrent UTI, OR (95% CI) a
sure had no effect on risk of recurrent Total 51 (61.4)
UTI. Among male children in whom Sex
Male 7 (87.5) 1 [Reference]
circumcision status was known, 5 of 26
Female 44 (58.7) 0.20 (0.02-1.73)
(19%) uncircumcised vs 0 of 10 cir-
Race
cumcised children had a recurrent UTI Nonwhite 24 (82.8) 1 [Reference]
(P=.13). White 27 (50.0) 0.21 (0.07-0.63) b
Antimicrobial prophylaxis expo- Age, y
sure considered as a time-varying co- ⬍2 21 (80.8) 1 [Reference]
variate had no significant effect on the 2-6 30 (52.6) 0.26 (0.09-0.80) c
risk of recurrent UTI in multivariable VCUG
Normal result 14 (70.0) 1 [Reference]
analysis (HR, 1.01; 95% CI, 0.50-
Not performed 27 (51.9) 0.46 (0.15-1.39)
2.02). In stratified analyses for each of
VUR grade 1-3 7 (87.5) 3.00 (0.30-30.02)
the other covariates (sex, race, age, and
VUR grade 4-5 3 (100) NA d
VCUG result), antimicrobial prophy-
VUR grades 1-5 4.29 (0.44-41.37)
laxis had no significant effect in any of
Antimicrobial prophylaxis
the groups. Analyses stratified by pro- Not exposed 34 (53.1) 1 [Reference]
pensity score quintile also demon- Exposed 17 (89.5) 7.50 (1.60-35.17) b
strated no significant effect of antimi- Abbreviations: CI, confidence interval; NA, not available; OR, odds ratio; VCUG, voiding cystourethrogram; VUR, vesi-
crobial prophylaxis. Similarly, coureteral reflux.
a OR of resistant vs pan-sensitive organism as the cause of recurrent UTI.
antimicrobial prophylaxis did not de- b P ⬍ .01.
c P ⬍ .05.
crease the risk of recurrent UTI when d All (3/3) children with recurrent UTI and with grade 4-5 VUR had resistant infections, so OR is infinite and no CI was
controlling for the propensity quintile calculated.
(HR, 1.03; 95% CI, 0.51-2.08), propen-
sity score as a continuous variable (HR, ceipt propensity score (OR, 6.76; 95% ence of VUR, and exposure to antimi-
1.02; 95% CI, 0.51-2.05), or propen- CI, 1.26-30.57) and whether the first crobial prophylaxis. For example, a
sity score combined with all covari- UTI was resistant (OR, 8.66; 95% CI, nonwhite child younger than 2 years
ates (HR, 1.01; 95% CI, 0.51-2.02). 1.66-45.31). Any exposure to other who has VUR and is exposed to anti-
Analysis stratified by type of antimi- (nonprophylactic) antimicrobials and microbial prophylaxis has the highest
crobial prophylaxis demonstrated no as- exposure to other antimicrobials in the probability of resistance, 98.0%
sociation between type of prophylaxis 30 days prior to a recurrent UTI were (Table 4). In contrast, a white 2- to
and risk of recurrent UTI; however, a not significantly associated with resis- 6-year-old child who does not have
HR for nitrofurantoin prophylaxis could tant infections. Age at first UTI, VCUG VUR and is not exposed to prophy-
not be calculated because 0 of 9 chil- result, and exposure to antimicrobial laxis has only a 40.4% probability of a
dren receiving nitrofurantoin experi- prophylaxis were highly correlated resistant recurrent UTI. If this same
enced a recurrent UTI. (P ⬍ .001 for all) among the 83 chil- white, 2- to 6-year-old child without
dren with recurrent UTI, likely due to VUR is exposed to prophylaxis, our data
Risk of Resistance Among Children the American Academy of Pediatrics predict an increased absolute probabil-
With Recurrent UTI guideline recommending that a VCUG ity of resistance of more than 30% to
Among the 83 children with recurrent be performed in children younger than 73.3%, demonstrating that exposure to
UTI, white race (odds ratio [OR], 0.21; 2 years and prophylaxis given to those antimicrobial prophylaxis has a major
95% CI, 0.07-0.63) and age 2 to 6 years children with VUR.10 Since this colin- impact on risk of resistance in recur-
(OR, 0.26; 95% CI, 0.09-0.80) were as- earity prevents the ascertainment of the rent UTIs.
sociated with decreased risk of resis- effect of each individual exposure in a
tant infections. Conversely, exposure multivariable model and we wanted to COMMENT
to prophylactic antimicrobials signifi- provide clinicians with a risk profile To our knowledge, this study is the first
cantly increased the likelihood of re- based on exposures, we calculated the large primary care pediatric cohort
sistant infections (OR, 7.50; 95% CI, predicted probability of a recurrent UTI study to evaluate risk factors for recur-
1.60-35.17) (TABLE 3). This increased being antimicrobial resistant (TABLE 4) rent UTI and the association with an-
risk of resistance associated with anti- for each combination of exposures de- timicrobial prophylaxis. We found that
microbial prophylaxis persisted when rived from a multivariable regression antimicrobial prophylaxis was not as-
controlling for the antimicrobial re- model that included race, age, pres- sociated with lower risk of recurrent
©2007 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2007—Vol 298, No. 2 183
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
However, in analyses stratified by VUR
Table 4. Probability of Recurrent Urinary Tract Infection Being Antimicrobial Resistant Based
on Exposures grade, our study found that antimicro-
Exposure Type bial prophylaxis had no significant
effect on risk of recurrence for chil-
Nonwhite VUR Prophylactic Antimicrobial Probability of dren with either grade 1 to 3 or grade
Race Age ⬍2 y Present Exposure Resistance, % a
⫹ ⫹ ⫹ ⫹ 98.0
4 to 5 VUR, but no firm conclusions
⫹ − ⫹ ⫹ 97.2
could be made in the grade 4 to 5 VUR
⫹ ⫹ − ⫹ 94.2
group, which had only 7 children. Pre-
⫹ ⫹ ⫹ − 92.4 vious randomized trials also have dem-
− ⫹ ⫹ ⫹ 92.2 onstrated the lack of effectiveness of
⫹ − − ⫹ 92.0 prophylaxis to prevent recurrent UTI
⫹ − ⫹ − 89.6 and renal scarring in children with
− − ⫹ ⫹ 89.3 grade 1 to 3 VUR.5,16 Therefore, it is un-
⫹ ⫹ − − 79.9 clear how much of a role the presence
− ⫹ − ⫹ 79.5 of VUR, especially low-grade VUR,
− ⫹ ⫹ − 74.5 should play in making decisions about
⫹ − − − 73.8 starting prophylactic antimicrobials.
− − − ⫹ 73.3 Our study demonstrated that age may
− − ⫹ − 67.4 be an important consideration for risk
− ⫹ − − 48.9 of recurrent UTI and antimicrobial-
− − − − 40.4 resistant infections. Children aged 2 to
a Probability of causative organism for recurrent urinary tract infection being resistant to any antimicrobial based on 6 years, especially those aged 3 to 5
multivariable model including race, age, presence of vesicoureteral reflux (VUR), and antimicrobial prophylaxis
exposure. years, were at increased risk of recur-
rent UTI, possibly related to dysfunc-
tional elimination that previously has
UTI but was associated with increased timicrobial prophylaxis was associ- been identified as an underappreci-
risk of resistant infection. ated with significantly increased risk of ated risk factor.24-29 The observed in-
Also, to our knowledge, this is the resistant infections. The results did not creased risk of recurrent UTI in older
first study to estimate the incidence of change significantly when a more strin- children is contrary to previous con-
recurrent UTI after an initial UTI in a gent colony-count criterion (ⱖ100 000 cerns that younger children are at high-
large primary care pediatric cohort. The colony-forming units/mL) was used to est risk. Those concerns were based
incidence of first UTI, 0.007 per person- define a positive urine culture result. largely on the findings from a study of
year (4.2% cumulative incidence from Recent randomized trials of antimicro- Swedish children recruited from
ages 0-6 years), is similar to previous bial prophylaxis also have demon- Goteborg hospital in the 1960s.1,8 How-
population-based first-UTI cumula- strated no reduction in risk of UTI re- ever, that study included catheteriza-
tive incidence rate estimates of 2% to currence or renal scarring.5,16 Given tions performed at set follow-up times
8%.1,22 The rate of recurrent UTI (0.12 these previous findings and the unfa- irrespective of the presence of symp-
per person-year, or 12% per year) was vorable risk/benefit ratio demon- toms, which may have biased it to-
lower than recurrence rates previ- strated by the current study, we think ward detecting persistent asymptom-
ously reported from referral popula- it is prudent for clinicians to discuss the atic bacteriuria in younger infants,
tions or populations with cultures per- risks and unclear benefits of prophy- rather than recurrent UTI. Thus our
formed without symptoms (20%-48% laxis with families as they make family- study, which defined recurrent UTI
within 6-12 months).1,4-9 The estimate centered decisions about whether to based on physician diagnosis trig-
of recurrent UTI incidence was the same start prophylactic antimicrobials or to gered by symptoms, may better reflect
as that in a study that reported a 12% closely monitor a child without pre- the epidemiology of recurrent symp-
recurrence rate after diagnosis of first scribing antimicrobial prophylaxis af- tomatic UTI in a pediatric primary
UTI in an emergency department23 and ter a first UTI. care population. 1,8 Interestingly, a
probably better represents the inci- Currently, antimicrobial prophy- 2006 population-based study from the
dence of symptomatic recurrent UTI in laxis is recommended if a child has Netherlands found results similar to
a primary care setting. VUR.10,12 In analyses controlling for an- ours—in that study, the maximal inci-
No association was found between timicrobial exposure, our study found dence of UTI in both girls and boys was
antimicrobial prophylaxis and risk of no significantly increased risk of recur- in year 4 of life.30
recurrent UTI, either in multivariable rence for children with grade 1 to 3 Race also may play a role in risk of
Cox regression or in propensity score VUR and increased risk of recurrence recurrent UTIs and resistant infec-
analyses. In addition, exposure to an- in children with grade 4 to 5 VUR. tions. Nonwhites had a decreased risk
184 JAMA, July 11, 2007—Vol 298, No. 2 (Reprinted) ©2007 American Medical Association. All rights reserved.
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
of recurrent UTI yet an increased risk cause they may not have adhered to older children, and those with and with-
of resistant infections. All 9 recurrent their prescribed regimen. This could out VUR. It also will be important for
UTIs in nonwhites exposed to prophy- have biased the effect of prophylactic future studies to evaluate the poten-
lactic antimicrobials were caused by a antimicrobials toward the null. Sixth, tial risks of prophylaxis, such as resis-
resistant organism. We are not aware our measure of the effectiveness of an- tant infections.
of literature to explain the mechanism timicrobial prophylaxis could have been
for increased risk of resistance, but it affected by confounding by indica- CONCLUSIONS
raises questions about whether the ben- tion. We attempted to minimize this White race, age 3 to 5 years, and grade
efits of antimicrobial prophylaxis ex- confounding by controlling for plau- 4 to 5 VUR were associated with in-
ceed the risks in nonwhite children. sible observed factors that could influ- creased risk of recurrent UTI. Sex and
Clearly, more studies are needed to vali- ence the decision of a clinician to pre- grade 1 to 3 VUR were not associated
date these findings and to explore the scribe prophylaxis, such as sex, race, with risk of recurrence. Antimicrobial
genetic and environmental basis for this age, and VUR status, and by perform- prophylaxis was not associated with
observation. ing multiple propensity score analy- lower risk of recurrent UTI, but pro-
Our study has several limitations. ses.20,31 However, we must recognize phylaxis was associated with in-
First, as with all studies in which data that residual unobservable confound- creased risk of resistant infections.
are gathered via health care delivery net- ing could exist in the assessment of pro- Author Contributions: Dr Conway had full access to all
works, we could have missed results phylaxis efficacy. Finally, because less of the data in the study and takes responsibility for the
integrity of the data and the accuracy of the data analysis.
from outside the network. We at- than 5% of children underwent dimer- Study concept and design: Conway, Cnaan, Zaoutis,
tempted to minimize this loss through captosuccinic acid renal scintigraphy to Grundmeier, Keren.
Acquisition of data: Conway, Cnaan, Henry,
incorporation of results from outside assess for pyelonephritis and renal scar- Grundmeier, Keren.
hospitals and clinics. Second, if pat- ring, we could not comment on the Analysis and interpretation of data: Conway, Cnaan,
terns of care were different between effect of prophylaxis on these out- Zaoutis, Keren.
Drafting of the manuscript: Conway, Cnaan, Keren.
groups, then ascertainment bias could comes. Critical revision of the manuscript for important in-
have occurred. For example, if whites The major strength of this study is tellectual content: Conway, Cnaan, Zaoutis, Henry,
Grundmeier, Keren.
were more likely than nonwhites to seek that it is the first study of a large pedi- Statistical analysis: Conway, Cnaan, Henry, Keren.
or receive care or testing for urinary atric primary care cohort to simulta- Obtained funding: Conway, Zaoutis, Keren.
Administrative, technical, or material support: Henry,
symptoms, then that pattern of care neously examine the risks and ben- Grundmeier, Keren.
could explain the observed increased efits of antimicrobial prophylaxis for Study supervision: Cnaan, Keren.
Financial Disclosures: None reported.
risk of recurrent UTI in whites. How- children with first UTI. This study as- Funding/Support: Dr Conway was supported by a
ever, we found no evidence to support sessed more than 600 children after first training grant through the Robert Wood Johnson Clini-
this explanation—there was no signifi- UTI in a “natural experiment” setting cal Scholars Training Program. This project was sup-
ported through a pilot grant from a University of Penn-
cant difference between races in the for, on average, more than 1 year, which sylvania Center for Education and Research on
number of clinic visits per year overall is an adequate duration to assess the ef- Therapeutics (CERTS) grant. Dr Cnaan is supported
by National Institutes of Health (NIH) Clinical and
or after first UTI diagnosis. fectiveness of antimicrobial prophy- Translational Science Award U54 RR023567-01. Dr
Third, 65% of the children in our laxis in practice. Conducting the study Keren was supported by grant K23 HD043179 from
the National Institute of Child Health and Human De-
study did not have VCUGs per- in a primary care setting also freed it velopment, NIH.
formed; the majority of these children of the selection bias that has limited the Role of the Sponsors: None of the funding sources
were older than 2 years, for whom the generalizability of previous studies, had any role in the design and conduct of the study;
the collection, management, analysis, and interpre-
American Academy of Pediatrics guide- which typically were performed in re- tation of the data; or the preparation, review, or ap-
line is silent regarding recommenda- ferral populations. proval of the manuscript.
Additional Contributions: We thank the physicians
tions on screening for VCUG.10 But this Given the limitations of observa- and staff of the Practice-Based Research Network,
prevented us from fully exploring the tional studies, further investigation is especially Marguerite Swietlik, CRNP, and Louis Bell,
MD, who facilitated the performance of this study.
effect of VUR on recurrent UTI and the needed to better understand the risks We thank Chris Bell for research support and data
effectiveness of prophylactic antimi- and benefits of antimicrobial prophy- collection and Huaqing Zhao, MSc, The Children’s
Hospital of Pennsylvania Biostatistics and Data Man-
crobials by VUR grade. Fourth, the lack laxis. Specifically, a randomized trial in- agement Core, for statistical support. None of those
of circumcision documentation in 47% volving children in the community set- ackowledged received any compensation for their
of male children limited our ability to ting after first UTI comparing daily contributions.
accurately assess risk based on this im- prophylaxis vs close follow-up would
REFERENCES
portant factor. Fifth, we based expo- significantly improve understanding of
sure to antimicrobial prophylaxis on an- the efficacy of antimicrobial prophy- 1. Winberg J, Andersen HJ, Bergstrom T, Jacobsson
B, Larson H, Lincoln K. Epidemiology of symptomatic
timicrobial prescriptions and therefore laxis. Based on our findings, this type urinary tract infection in childhood. Acta Paediatr Scand
likely overestimated the degree of an- of study should be powered to exam- Suppl. 1974;(252):1-20.
2. Uhari M, Nuutinen M. Epidemiology of sympto-
timicrobial exposure in children both ine the efficacy of prophylaxis in pa- matic infections of the urinary tract in children. BMJ.
with and without recurrent UTI, be- tient subgroups including nonwhites, 1988;297(6646):450-452.
©2007 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2007—Vol 298, No. 2 185
Downloaded From: on 06/06/2018
RECURRENT URINARY TRACT INFECTIONS IN CHILDREN
3. Mahant S, Friedman J, MacArthur C. Renal ultra- port on the management of primary vesicoureteral re- old and previous urinary tract infection. Arch Dis Child.
sound findings and vesicoureteral reflux in children hos- flux in children. J Urol. 1997;157(5):1846-1851. 1991;66(2):232-234.
pitalised with urinary tract infection. Arch Dis Child. 13. Bisset GS III, Strife JL, Dunbar JS. Urography and 23. Panaretto K, Craig J, Knight J, Howman-Giles R,
2002;86(6):419-420. voiding cystourethrography: findings in girls with uri- Sureshkumar P, Roy L. Risk factors for recurrent uri-
4. Lohr JA, Nunley DH, Howards SS, Ford RF. Pre- nary tract infection. AJR Am J Roentgenol. 1987;148 nary tract infection in preschool children. J Paediatr
vention of recurrent urinary tract infections in girls. (3):479-482. Child Health. 1999;35(5):454-459.
Pediatrics. 1977;59(4):562-565. 14. Gleeson FV, Gordon I. Imaging in urinary tract 24. Mazzola BL, von Vigier RO, Marchand S, Tonz
5. Garin EH, Olavarria F, Garcia Nieto V, Valenciano infection. Arch Dis Child. 1991;66(11):1282-1283. M, Bianchetti MG. Behavioral and functional abnor-
B, Campos A, Young L. Clinical significance of pri- 15. McKerrow W, Davidson-Lamb N, Jones PF. Uri- malities linked with recurrent urinary tract infections
mary vesicoureteral reflux and urinary antibiotic pro- nary tract infection in children. Br Med J (Clin Res Ed). in girls. J Nephrol. 2003;16(1):133-138.
phylaxis after acute pyelonephritis: a multicenter, ran- 1984;289(6440):299-303. 25. Wan J, Kaplinsky R, Greenfield S. Toilet habits of
domized, controlled study. Pediatrics. 2006;117 16. Reddy P, Hughes PA, Dangman B, et al. Antimi- children evaluated for urinary tract infection. J Urol.
(3):626-632. crobial prophylaxis in children with vesico-ureteral re- 1995;154(2, pt 2):797-799.
6. Savage DC, Howie G, Adler K, Wilson MI. Con- flux: a randomised prospective study of continuous 26. Shaikh N, Hoberman A, Wise B, et al. Dysfunc-
trolled trial of therapy in covert bacteriuria of childhood. therapy vs intermittent therapy vs surveillance. tional elimination syndrome: is it related to urinary tract
Lancet. 1975;1(7903):358-361. Pediatrics. 1997;100(3):555-556. infection or vesicoureteral reflux diagnosed early in life?
7. Smellie JM, Katz G, Gruneberg RN. Controlled trial 17. Lutter SA, Currie ML, Mitz LB, Greenbaum LA. Pediatrics. 2003;112(5):1134-1137.
of prophylactic treatment in childhood urinary-tract Antibiotic resistance patterns in children hospitalized 27. Smellie JM, Gruneberg RN, Bantock HM, Pres-
infection. Lancet. 1978;2(8082):175-178. for urinary tract infections. Arch Pediatr Adolesc Med. cod N. Prophylactic co-trimoxazole and trimetho-
8. Winberg J, Bergstrom T, Jacobsson B. Morbidity, 2005;159(10):924-928. prim in the management of urinary tract infection in
age and sex distribution, recurrences and renal scar- 18. Hoberman A, Wald ER, Reynolds EA, Penchan- children. Pediatr Nephrol. 1988;2(1):12-17.
ring in symptomatic urinary tract infection in childhood. sky L, Charron M. Pyuria and bacteriuria in urine speci- 28. Hellerstein S, Nickell E. Prophylactic antibiotics in
Kidney Int Suppl. 1975;4:S101-S106. mens obtained by catheter from young children with children at risk for urinary tract infection. Pediatr
9. Williams GJ, Wei L, Lee A, Craig JC. Long-term an- fever. J Pediatr. 1994;124(4):513-519. Nephrol. 2002;17(7):506-510.
tibiotics for preventing recurrent urinary tract infec- 19. Lebowitz RL, Olbing H, Parkkulainen KV, Smellie 29. Snodgrass W. Relationship of voiding dysfunc-
tion in children. Cochrane Database Syst Rev. 2006;3: JM, Tamminen-Mobius TE; International Reflux Study tion to urinary tract infection and vesicoureteral re-
CD001534. in Children. International system of radiographic grad- flux in children. Urology. 1991;38(4):341-344.
10. American Academy of Pediatrics. Practice param- ing of vesicoureteric reflux. Pediatr Radiol. 1985;15 30. Kwok WY, de Kwaadsteniet MC, Harmsen M, van
eter: the diagnosis, treatment, and evaluation of the (2):105-109. Suijlekom-Smit LW, Schellevis FG, van der Wouden
initial urinary tract infection in febrile infants and young 20. Rosenbaum PR, Rubin DB. Reducing bias in JC. Incidence rates and management of urinary tract
children. Pediatrics. 1999;103(4, pt 1):843-852. observational studies using subclassification on the infections among children in Dutch general practice:
11. Downs SM; Urinary Tract Subcommittee of the propensity score. J Am Stat Assoc. 1984;79:516- results from a nation-wide registration study. BMC
American Academy of Pediatrics Committee on Qual- 524. Pediatr. 2006;6:10.
ity Improvement. Technical report: urinary tract in- 21. Gorelick MH, Shaw KN. Screening tests for uri- 31. Austin PC, Grootendorst P, Anderson GM. A com-
fections in febrile infants and young children. Pediatrics. nary tract infection in children: a meta-analysis. parison of the ability of different propensity score mod-
1999;103(4):e54. Pediatrics. 1999;104(5):e54. els to balance measured variables between treated and
12. Elder JS, Peters CA, Arant BS Jr, et al. Pediatric 22. Hellström A, Hanson E, Hansson S, Hjalmas K, Jo- untreated subjects: a Monte Carlo study. Stat Med.
Vesicoureteral Reflux Guidelines Panel summary re- dal U. Association between urinary symptoms at 7 years 2007;26(4):734-753.
Disease is very old and nothing about it has changed.
It is we who change as we learn to recognize what was
formerly imperceptible.
—Jean Martin Charcot (1825-1893)
186 JAMA, July 11, 2007—Vol 298, No. 2 (Reprinted) ©2007 American Medical Association. All rights reserved.
Downloaded From: on 06/06/2018
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Project Report Heimalya HerbalDocument78 pagesProject Report Heimalya Herbalkeshu75% (4)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- BBM521/03 Research Methods Jan 2014: Tutor-Marked Assignment 2 (TMA 2 - 20%)Document3 pagesBBM521/03 Research Methods Jan 2014: Tutor-Marked Assignment 2 (TMA 2 - 20%)Shiyun SeNo ratings yet
- Exploration in The New Millenium: Coordinator: Bill Coker BHP Billiton World Exploration IncDocument6 pagesExploration in The New Millenium: Coordinator: Bill Coker BHP Billiton World Exploration Incalvaro MNo ratings yet
- Applied Statistics in Occupational PDFDocument199 pagesApplied Statistics in Occupational PDFFitri Jasmine AndrianiNo ratings yet
- Laboratory Quality Control Based Risk ManagementDocument12 pagesLaboratory Quality Control Based Risk ManagementPedro C. Jardon0% (1)
- Career Path PDFDocument2 pagesCareer Path PDFЕкатерина НестероваNo ratings yet
- Quality of Service Assessment On Some Major Mobile Network Operators in GhanaDocument7 pagesQuality of Service Assessment On Some Major Mobile Network Operators in GhanaJonah JayNo ratings yet
- Measure of Central TendancyDocument27 pagesMeasure of Central TendancySadia HakimNo ratings yet
- Audit Engagement Questionnaire: Review Questions For Audit EngagementsDocument25 pagesAudit Engagement Questionnaire: Review Questions For Audit EngagementsRSA ArcherNo ratings yet
- The Scientific AttitudeDocument2 pagesThe Scientific AttitudeDaniel FrazónNo ratings yet
- Syllabus TESP 302-4Document17 pagesSyllabus TESP 302-4Devin BlackwoodNo ratings yet
- 2013 Book Icord13Document1,404 pages2013 Book Icord13Rafael Mena FredesNo ratings yet
- Bilingual Mental Lexicon and Translation: A Psycholinguistic Study of Bengali-English Language PairsDocument18 pagesBilingual Mental Lexicon and Translation: A Psycholinguistic Study of Bengali-English Language PairsSouvik BaruaNo ratings yet
- BBDM2063 Cross-Cultural Studies Revised 20130904Document7 pagesBBDM2063 Cross-Cultural Studies Revised 20130904preetimutiarayNo ratings yet
- ds10 Bouncing Slime LabDocument7 pagesds10 Bouncing Slime Labapi-110789702No ratings yet
- IEEE Education Society Papers-05535216Document8 pagesIEEE Education Society Papers-05535216Anoop MathewNo ratings yet
- Module 5. T-Test One Sample TestDocument5 pagesModule 5. T-Test One Sample TestBelle AmeNo ratings yet
- TQM IMP Questions - MBA III Semester-OUDocument2 pagesTQM IMP Questions - MBA III Semester-OUsrinivas nallakuntaNo ratings yet
- Data Structures and Algorithms Design (Regular) DSE PDFDocument9 pagesData Structures and Algorithms Design (Regular) DSE PDFsrirams007No ratings yet
- Colleges of Education Evaluation Form: National Accreditation BoardDocument33 pagesColleges of Education Evaluation Form: National Accreditation Boardsarah AKPONo ratings yet
- Magic SquareDocument15 pagesMagic SquaresembeNo ratings yet
- Literature Review of Tuition Impact On Learning of StudentsDocument33 pagesLiterature Review of Tuition Impact On Learning of StudentsAsma Akram50% (4)
- MBA Assignment Topics 2011-12Document11 pagesMBA Assignment Topics 2011-12chitraNo ratings yet
- Review of Related Literature and Studies Related LiteratureDocument6 pagesReview of Related Literature and Studies Related LiteratureLeonard MedinaNo ratings yet
- Human Language As A Unique Human PossessionDocument2 pagesHuman Language As A Unique Human PossessionDahlia Galvan- MaglasangNo ratings yet
- RUL 670 - Research ProposalDocument28 pagesRUL 670 - Research Proposalxin suNo ratings yet
- CH 03Document11 pagesCH 03Atika AisyahNo ratings yet
- Chloe Wong ResumeDocument2 pagesChloe Wong ResumeChloe WongNo ratings yet
- Adb9 Bsbpmg517 Manage Project RiskDocument140 pagesAdb9 Bsbpmg517 Manage Project RiskLili Pabuena VillarrealNo ratings yet
- Sip Banana FinalDocument31 pagesSip Banana FinalAmran BhuiyanNo ratings yet