Professional Documents
Culture Documents
Genetic Basis of Drug Metabolism: M K. M, M H. W, H L. M L
Genetic Basis of Drug Metabolism: M K. M, M H. W, H L. M L
Uploaded by
Jasmin AfifCopyright:
Available Formats
You might also like
- Tesda Written ExamDocument8 pagesTesda Written ExamAngel Cayanan95% (37)
- Do Not Crush MedsDocument3 pagesDo Not Crush Medsapi-249622140No ratings yet
- Commonly Prescribed Psychotropic MedicationsDocument2 pagesCommonly Prescribed Psychotropic Medicationsburlacuraduu100% (1)
- Usp 36 - NF 31 - ContenidoDocument2 pagesUsp 36 - NF 31 - ContenidoRodriguito Gabriel FloresNo ratings yet
- BHU Daily Stock PerformaDocument6 pagesBHU Daily Stock PerformabilalNo ratings yet
- Pharmaco GenomicsDocument6 pagesPharmaco GenomicsPrasanna BabuNo ratings yet
- Chapter 056Document42 pagesChapter 056Adistri KimNo ratings yet
- Pharmacogenetics and The Concept of Individualized Medicine: BS ShastryDocument6 pagesPharmacogenetics and The Concept of Individualized Medicine: BS Shastrykunalprabhu148No ratings yet
- DialoguesClinNeurosci 7 223Document8 pagesDialoguesClinNeurosci 7 223mantradaNo ratings yet
- Zhou2008 Vis DujDocument47 pagesZhou2008 Vis DujAnAn BanhGaoNo ratings yet
- PharmacogeneticsDocument30 pagesPharmacogeneticsShailendra Sk100% (3)
- Genetic Polymorphism in Drug MetabolismDocument55 pagesGenetic Polymorphism in Drug MetabolismMounika16 Pedamallu100% (2)
- Pharmacogenomics: Dr. Santoshkumar - Jeevangi Associate Professor Dept. of Pharmacology MR Medical College GulbargaDocument58 pagesPharmacogenomics: Dr. Santoshkumar - Jeevangi Associate Professor Dept. of Pharmacology MR Medical College GulbargaSantu PrashuNo ratings yet
- The Clinical Role of Genetic Polymorphisms in Drug-Metabolizing EnzymesDocument12 pagesThe Clinical Role of Genetic Polymorphisms in Drug-Metabolizing EnzymesMasDhedotNo ratings yet
- Dosage Form For Personalized Medicine: HistoryDocument11 pagesDosage Form For Personalized Medicine: HistoryNayeema KhowserNo ratings yet
- Genetic Factors in Drug MetabolismDocument9 pagesGenetic Factors in Drug MetabolismGloria Adetokunbo OjoNo ratings yet
- Pharmacogenetics and Pharmacogenomics in Moderate-to-Severe PsoriasisDocument14 pagesPharmacogenetics and Pharmacogenomics in Moderate-to-Severe PsoriasisDian Arief PutraNo ratings yet
- Lecture 8 - PharmacogeneticsDocument38 pagesLecture 8 - PharmacogeneticsNicko WijayaNo ratings yet
- Genetic Variation in Drug Disposition: Balmukunda Regmi and Laxman BharatiDocument11 pagesGenetic Variation in Drug Disposition: Balmukunda Regmi and Laxman BharatiAnsiSilambiNo ratings yet
- Pharmacogenomics PDFDocument12 pagesPharmacogenomics PDFsivaNo ratings yet
- Seminar in Pharmacology 2Document10 pagesSeminar in Pharmacology 2Jiggy JoeNo ratings yet
- Pharmacogenomics in Cardiovascular MedicineDocument11 pagesPharmacogenomics in Cardiovascular MedicineVeronica BalanNo ratings yet
- Kocal 2017Document24 pagesKocal 2017AnAn BanhGaoNo ratings yet
- Pharmacogenomics: New Challenges For Thai Anesthesiologists: J Med Assoc Thai 2017 100 (Suppl. 7) : S250-S258Document9 pagesPharmacogenomics: New Challenges For Thai Anesthesiologists: J Med Assoc Thai 2017 100 (Suppl. 7) : S250-S258Ronald André Buleje HinostrozaNo ratings yet
- PharmacogeneticsDocument80 pagesPharmacogeneticsThư SV. Nguyễn AnhNo ratings yet
- Pharmacogenetics: Dr. P.Naina Mohamed PHDDocument21 pagesPharmacogenetics: Dr. P.Naina Mohamed PHDJeevan Khanal100% (1)
- 1217-Article Text-5162-1-10-20220708Document6 pages1217-Article Text-5162-1-10-20220708srirampharmNo ratings yet
- Metabolic Drug Interactions With ImmunosuppressantsDocument32 pagesMetabolic Drug Interactions With Immunosuppressants陈梓强No ratings yet
- IA - Molecular Biology of Pharmacology 160908Document39 pagesIA - Molecular Biology of Pharmacology 160908Susi RutmalemNo ratings yet
- 5685 - UHN2012Pharmacogenomic PharmacogeneticDocument44 pages5685 - UHN2012Pharmacogenomic PharmacogeneticAdinda TobingNo ratings yet
- 2020 Article 80954Document9 pages2020 Article 80954Chintya Redina HapsariNo ratings yet
- Pharmagenomics: Pharmaceutical BiotechnologyDocument6 pagesPharmagenomics: Pharmaceutical Biotechnologykapy_123No ratings yet
- Pharmacogenetics of Drug-Gene Interactions: Muh. Akbar BaharDocument49 pagesPharmacogenetics of Drug-Gene Interactions: Muh. Akbar BaharHemi Amalia AmirullahNo ratings yet
- Pharmacogenetics of Drug-Metabolizing2005Document8 pagesPharmacogenetics of Drug-Metabolizing2005Hoàng Mỹ ChinhNo ratings yet
- Review Article: Volker M. Lauschke, Lili Milani, and Magnus Ingelman-SundbergDocument16 pagesReview Article: Volker M. Lauschke, Lili Milani, and Magnus Ingelman-SundbergLuis Angel Garcia RuizNo ratings yet
- Pharmacogenetics Polymorphism and Efficacy of DrugsDocument11 pagesPharmacogenetics Polymorphism and Efficacy of DrugsRohitNo ratings yet
- Pharmacogenetics 141110022651 Conversion Gate01Document45 pagesPharmacogenetics 141110022651 Conversion Gate01Jeevan Khanal0% (1)
- 1 Farmakogenomik 2023Document51 pages1 Farmakogenomik 2023yayu latifahNo ratings yet
- Pharmacogenetics of Cardiovascular Drug TherapyDocument11 pagesPharmacogenetics of Cardiovascular Drug Therapybalaji5563No ratings yet
- An Omics'' View of Drug DevelopmentDocument5 pagesAn Omics'' View of Drug DevelopmentOti DeeaNo ratings yet
- An Omics'' View of Drug Development: Research CommentaryDocument5 pagesAn Omics'' View of Drug Development: Research CommentaryVeronica BalanNo ratings yet
- 9 Personalized MedicineDocument34 pages9 Personalized Medicinehamza najmNo ratings yet
- Drug DispositionDocument22 pagesDrug DispositiongabriellaNo ratings yet
- Farm A Kogen EtikDocument60 pagesFarm A Kogen Etikrahmad wahyudiNo ratings yet
- BLOK 12 - IT 2 - Farmakogenetik 1 - MISDocument38 pagesBLOK 12 - IT 2 - Farmakogenetik 1 - MISMuhammad AdilNo ratings yet
- Genetic Polymorphisms of Cytochrome P450 Enzymes and The Effect On Interindividual, PharmacokinetDocument11 pagesGenetic Polymorphisms of Cytochrome P450 Enzymes and The Effect On Interindividual, PharmacokinetLuciana OliveiraNo ratings yet
- Pharmacology and Pharmacogenomics of Neurological Medications Used in Pregnancy 2013Document12 pagesPharmacology and Pharmacogenomics of Neurological Medications Used in Pregnancy 2013Ricardo Robles AlfaroNo ratings yet
- Assignment On Genetic PolymorphismDocument19 pagesAssignment On Genetic PolymorphismSayema KhanumNo ratings yet
- Pharmacogenetics 2022 23Document52 pagesPharmacogenetics 2022 23Erdem Altun100% (1)
- Karriker, 2007 - Genetic Predisposition To Adverse Drug Events in DogsDocument7 pagesKarriker, 2007 - Genetic Predisposition To Adverse Drug Events in DogsJoana CarreiraNo ratings yet
- Pharmaco GeneticsDocument52 pagesPharmaco GeneticsManikanta GupthaNo ratings yet
- Choi ClinPharmacolTher 2011 PDFDocument11 pagesChoi ClinPharmacolTher 2011 PDFhuouinkyoumaNo ratings yet
- PharmecogenomicsDocument21 pagesPharmecogenomicsRatan Ratan100% (1)
- Pharmacogenomics:: Increasing The Safety and Effectiveness of Drug TherapyDocument12 pagesPharmacogenomics:: Increasing The Safety and Effectiveness of Drug TherapyFlorentina GasttiNo ratings yet
- Research Pharmacogenomics PDFDocument10 pagesResearch Pharmacogenomics PDFmohammedNo ratings yet
- Pharmaco GenomicsDocument14 pagesPharmaco GenomicsMarfu'ah Mar'ahNo ratings yet
- A 30 Years Review On Pharmacokinetics ofDocument18 pagesA 30 Years Review On Pharmacokinetics ofAlexander CanoNo ratings yet
- Pharmacogenetics and Antipsychotic Treatment ResponseDocument15 pagesPharmacogenetics and Antipsychotic Treatment Responsebruna.c.moscatelNo ratings yet
- Future of Cancer Associated Transcription FactorDocument5 pagesFuture of Cancer Associated Transcription FactorIakovos GiacomoNo ratings yet
- Pharmacogenomics: Learning ObjectivesDocument16 pagesPharmacogenomics: Learning ObjectivesJamilNo ratings yet
- 2013 AapsjDocument8 pages2013 AapsjSCYoungNo ratings yet
- 215 FullDocument14 pages215 Fullnicacio18No ratings yet
- Personalized Medicine: The Promise of Pharmacogenomics Nancy ReinholdDocument9 pagesPersonalized Medicine: The Promise of Pharmacogenomics Nancy Reinholdnan-toddNo ratings yet
- Farmakogenetik AdoDocument31 pagesFarmakogenetik AdoEndang SusilowatiNo ratings yet
- Pharmacogenomics in Precision Medicine: From a Perspective of Ethnic DifferencesFrom EverandPharmacogenomics in Precision Medicine: From a Perspective of Ethnic DifferencesWeimin CaiNo ratings yet
- Daftar Obat High Alert Instalasi Farmasi Rsia Mutiara BundaDocument1 pageDaftar Obat High Alert Instalasi Farmasi Rsia Mutiara BundaAnonymous idPPyERfBnNo ratings yet
- Drug ListDocument104 pagesDrug Listخانه پزشکNo ratings yet
- Compulsive: Obsessive DisorderDocument16 pagesCompulsive: Obsessive DisorderGlyssa CabarrubiasNo ratings yet
- Piis0885392404002155 PDFDocument36 pagesPiis0885392404002155 PDFRohit ParasharNo ratings yet
- Zolpidem TartrateDocument2 pagesZolpidem Tartrateapi-3797941No ratings yet
- Codeine Phosphate (Drug Study)Document2 pagesCodeine Phosphate (Drug Study)Franz.thenurse6888100% (2)
- Borang JeanDocument102 pagesBorang JeanAsepDarussalamNo ratings yet
- Comprehensive Exam NCM 145Document17 pagesComprehensive Exam NCM 145Adrian Dela CruzNo ratings yet
- AnalgesicDocument42 pagesAnalgesicVinayak SinghNo ratings yet
- Admin Articles Formulation and Evaluation of Hydroxy Propyl Methyl Cellulose Transdermal Drug Delivery SystemsDocument4 pagesAdmin Articles Formulation and Evaluation of Hydroxy Propyl Methyl Cellulose Transdermal Drug Delivery SystemsKristine Dwi PuspitasariNo ratings yet
- Observation Reflection 1Document2 pagesObservation Reflection 1api-391659138No ratings yet
- Sitti Misfiyani Kusuma's VideoDocument18 pagesSitti Misfiyani Kusuma's VideoaniNo ratings yet
- Brompheniramine WikiDocument2 pagesBrompheniramine WikiMattNo ratings yet
- Walgreens LetterDocument5 pagesWalgreens LetterAnonymous P4XJDtdtq0No ratings yet
- Acalculous Cholecystitis CaseDocument35 pagesAcalculous Cholecystitis CaseSaada Enok MedtamakNo ratings yet
- PharmacologyDocument68 pagesPharmacologyvansal liu80% (5)
- Clinical ToxicologyDocument17 pagesClinical ToxicologyElfahra Casanza Amalda100% (1)
- Poster ThivyaDocument1 pagePoster ThivyaThivya ShankariNo ratings yet
- Patent UrachusDocument4 pagesPatent UrachusJustin Ahorro-DionisioNo ratings yet
- TinnitusDocument60 pagesTinnitusYowendruJunNo ratings yet
- Drug Admin and IV Rate Quiz - ANSWER KEYDocument3 pagesDrug Admin and IV Rate Quiz - ANSWER KEYJessica KruppNo ratings yet
- Extemporaneous Dispensing ProceduresDocument2 pagesExtemporaneous Dispensing ProceduresAsadZahidNo ratings yet
- CEKDocument4 pagesCEKTri SulistyoriniNo ratings yet
- PharmacologyDocument18 pagesPharmacologyMichael PiducaNo ratings yet
- Reviewing Depot Injection Efficacy in The Treatment of SchizophreniaDocument10 pagesReviewing Depot Injection Efficacy in The Treatment of SchizophreniaAnonymous raLgWVyqNo ratings yet
Genetic Basis of Drug Metabolism: M K. M, M H. W, H L. M L
Genetic Basis of Drug Metabolism: M K. M, M H. W, H L. M L
Uploaded by
Jasmin AfifOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Genetic Basis of Drug Metabolism: M K. M, M H. W, H L. M L
Genetic Basis of Drug Metabolism: M K. M, M H. W, H L. M L
Uploaded by
Jasmin AfifCopyright:
Available Formats
CL I N I C A L F R O N T I E R S Drug metabolism
CLINICAL FRONTIERS
Genetic basis of drug metabolism
MARGARET K. MA, MICHAEL H. WOO, AND HOWARD L. MCLEOD
T
he term “pharmacogenetics” was Abstract: The application of pharmacoge- studied. Individuals with aberrant genes for
first coined by Friedrich Vogel1 netics in identifying single nucleotide these enzymes may experience diminished
in 1959, who defined it as the polymorphisms (SNPs) in DNA sequences efficacy or increased toxicity in response to
“study of the role of genetics in drug that cause clinically significant alterations certain drugs because of the different levels
response.” It is one of the most rap- in drug-metabolizing enzyme activities is of activities associated with variant geno-
idly growing areas and is becoming discussed. types. The frequency of variant alleles for
Recent advances in pharmacogenomic drug-metabolizing enzymes often differs
increasingly important in clinical
research have begun to elucidate the among ethnic groups. Continued research
pharmacy. The pharmacogenetics of inherited nature of interindividual differ- in pharmacogenetics will further our under-
drug-metabolizing enzymes is a ences in drug-induced adverse reactions, standing in interindividual differences in
prominent focus of this field, because toxicity, and therapeutic responses. In one drug disposition. The application of this
genetic makeup is responsible for a particular area of study, variations in DNA knowledge will ultimately help individualize
significant portion of drug-induced sequences (i.e., genetic polymorphisms) drug dosing and drug therapy selection,
toxicity; many drugs are metabolized explain some of the variability in drug- predict toxicity or therapeutic failure, and
metabolizing enzyme activities which con- improve clinical outcomes.
by enzymes that are encoded by poly-
tribute to alterations in drug clearance and Pharmacogenetics has elucidated the
morphically expressed genes.2 Geno- impact patients’ response to drug therapy. genetic basis for interindividual variability
type analysis can be used to identify Historical and current examples of several in drug response and will continue to play a
DNA changes in specific metabolic extensively studied SNPs include the genes key role in defining strategies to optimize
pathways that produce aberrant phe- encoding for glucose-6-phosphate dehy- drug therapy.
notypes. Hence, patients can be clas- drogenase, N-acetyltransferase, and the su-
sified as extensive, intermediate, or perfamily of cytochrome P-450 (CYP) isoen- Index terms: Antiinflammatory agents; An-
zymes. Because CYP isoenzymes metabolize tituberculars; Hydralazine; Hypotensive
poor metabolizers according to their
a large number of structurally diverse drugs agents; Isoniazid; Metabolism; Pharmaco-
ability to metabolize certain drugs. and chemicals, most of the variant geno- genetics; Polymorphism; Race; Sulfona-
This classification can differentiate types of the CYP2D6, CYP2C9, CYP2C19, and mides; Toxicity
interpatient and intrapatient phar- CYP3A families have been identified and Am J Health-Syst Pharm. 2002; 59:2061-9
macokinetic and pharmacodynamic
variability3-5; however, not all genetic
polymorphisms of drug-metaboliz- of the drug, or if the number of ther- develop applications of pharmacoge-
ing enzymes are clinically relevant. apeutic alternatives is limited. With netic information for daily patient
The potential for a clinically signifi- increasing pharmacogenetic evi- care, many success stories illustrate
cant event is enhanced if the drug is dence, interindividual differences in how pharmacogenetics can be used
widely used and has a narrow thera- drug-related toxicity and therapeutic to guide therapy. Eventually, phar-
peutic range, if the enzyme pathway response are no longer idiosyncratic. macogenetic information may be-
plays a major role in the elimination Although much work is needed to come a routine tool for providing ra-
MARGARET K. MA, PHARM.D., is Research Associate of Medicine, Euclid Avenue, Campus Box 8069, St. Louis, MO 63110-1093
Washington University School of Medicine (WUSM), St. Louis, MO, (hmcleod@im.wustl.edu).
and Siteman Cancer Center (SCC), St. Louis. MICHAEL H. WOO, The work of Drs. Ma and McLeod was supported by grant
PHARM.D., BCPS, is Research Associate of Molecular Pharmacology, CA091842 from the Siteman Cancer Center and by grant GM63340-
St. Jude Children’s Research Hospital, Memphis, TN. HOWARD L. 01 from the National Institutes of Health.
MCLEOD, PHARM.D., is Associate Professor of Medicine, Molecular
Biology and Pharmacology, Genetics, WUSM, and SCC. Copyright © 2002, American Society of Health-System Pharma-
Address correspondence to Dr. McLeod at the Department of cists, Inc. All rights reserved. 1079-2082/02/1101-2061$06.00.
Medicine, Washington University School of Medicine, 660 South
Am J Health-Syst Pharm—Vol 59 Nov 1, 2002 2061
CL I N I C A L F R O N T I E R S Drug metabolism
tional individualized therapeutics she has two alleles for each gene, one variants and affecting more than 400
and patient care. on each chromosome. Different al- million people worldwide. However,
The pharmacogenetic differences leles produce variations in inherited the vast majority of affected individ-
in a number of phase-I enzymes, characteristics, such as eye color and uals are asymptomatic. Only 30 dif-
such as cytochrome P-450 (CYP) blood type. In an individual, one ferent functional mutations in the
isoenzymes, dehydrogenases, and es- form of the allele (the dominant one) gene have been reported, virtually all
terases, and phase-II (conjugating) may be expressed more than another of which are found in the region of
enzymes have been extensively stud- form (the recessive one). Two identi- the gene that codes for the protein.9,10
ied. This review introduces the con- cal alleles result in a homozygous All but one are point mutations, with
cept of pharmacogenetics in the con- dominant or homozygous recessive more than 50% being nucleotide con-
text of drug-metabolizing enzymes trait of that gene. A combination of versions from cytosine to guanine.11
and highlights the polymorphisms in two different alleles leads to a het- The consequence of these genetic
DNA sequences that lead to clinically erozygous trait. One or more genes polymorphisms is low G6PD activity,
significant alterations in drug- that code for a particular protein, resulting in reduced glutathione con-
metabolizing-enzyme activities. Many such as an enzyme or a receptor, may centrations in erythrocytes and subse-
of these genetic variants (i.e., geno- be expressed in different amounts in quently clinical manifestation of
types) were discovered after observing different tissues. In this review, all in- hemolytic anemia following the inges-
adverse reactions (i.e., phenotypes) af- dividual alleles (or genes) are refer- tion of certain drugs.12
ter administering common doses of enced by their gene name (e.g., The prevalence of G6PD deficiency
drugs to patients. We have focused on CYP2D6), followed by an asterisk and differs among ethnic groups. For in-
the most common single nucleotide an Arabic number (e.g., CYP2D6*1 stance, males of African and Mediter-
polymorphisms (SNPs), the inherit- designates the wild-type allele and ranean descent more frequently ex-
ed nature of their deficiency, their CYP2D6*3 is a mutant allele).6 press the trait. Two types of mutations
frequency, and the clinical impor- are commonly found in Africans,
tance of drug-metabolizing-enzyme Glucose-6-phosphate G6PD A and G6PD A(–). The former
variants. Most drug-metabolizing en- dehydrogenase protein produces normal red cell ac-
zymes discussed in this review (e.g., Phenotypes demonstrating varia- tivity, while the latter produces only
CYP isoenzymes, N-acetyltransferase) tions in people’s response to certain about 10% of the normal activity and
are located primarily in the liver and, drugs were first discovered in the is unstable in vivo. In patients with
to a lesser extent, in other organs, such early 1950s when antimalarial drugs G6PD A, an adenosine-to-guanine
as the small intestine. were found to cause hemolysis in pa- substitution at nucleotide 376
tients with glucose-6-phosphate de- (A376G) mutation causes an aspartic
Common terminology hydrogenase (G6PD) deficiency. acid residue to replace an asparagine
DNA consists of four bases: ade- G6PD, expressed in all of the body’s residue.13 There are three different
nine, guanine, thymine, and cy- tissues, controls the flow of carbon G6PD A(–) variants in one allele. The
tosine. Any combination of three nu- through the pentose phosphate A376G mutation occurs in all people,
cleic acids can form a codon, which is pathway, produces NADPH for re- but the enzyme deficiency is caused
transcribed into mRNA and translat- ductive biosynthesis, and maintains by a second amino acid substitution,
ed into a particular amino acid (e.g., oxidation-reduction in the cell to usually a G202A mutation, resulting
ACG encodes for threonine). The keep glutathione in a reduced state.7,8 in a valine-to-methionine substitu-
stop codon, TAG, terminates protein The absence of reduced glutathione tion at codon 68 (Val68Met). Other
synthesis. An incorrectly placed stop due to G6PD deficiency allows oxi- mutations are Val690Met and
codon in a gene, caused by mutation, dative drugs to oxidize sulfahydroxyl Val968Met. In Mediterranean peo-
prematurely truncates an amino acid groups of hemoglobin, leading to ples, the most common mutation is a
chain and may form a nonfunctional hemolysis. Currently, over two doz- C563T substitution resulting in an
protein. Many of the variations in the en drugs, including primaquine, sul- amino acid change (Ser188Phe).
human genome are single base fones, sulfonamides, nitrofurans, vi- Cases of drug-induced hemolytic
changes, termed SNPs. A mutation of tamin K analogues, cefotetan, and anemia have also been described in
one nucleotide of a codon may result chloramphenicol, are known to patients treated with cyclosporine,
in either a change in the coded amino cause hemolytic anemia in G6PD- tacrolimus, penicillin, and cefote-
acid (nonsynonymous SNP) or no deficient patients. G6PD deficiency is tan.14 The risk and severity of hemol-
change (silent polymorphism or syn- a sex-linked (chromosome X) reces- ysis are thought to be associated with
onymous SNP). Since each person sive trait and a widespread polymor- dose, duration of therapy, and other
has a pair of each chromosome, he or phism, with more than 400 known oxidant stresses, such as infection
2062 Am J Health-Syst Pharm—Vol 59 Nov 1, 2002
CL I N I C A L F R O N T I E R S Drug metabolism
and environmental factors. Be- suffered from peripheral nerve dam- notype as a result of a decrease in the
cause of these confounding factors, age, while fast acetylators were not amount of NAT2 protein. The pro-
genotyping patients for G6PD defi- affected.15 Slow acetylators are also at tein expressed from NAT2*5A, *5B,
ciency is not warranted, since the risk for sulfonamide-induced toxici- and *5C genes has lower activities
toxicity is rare and not typically ty and can suffer from idiopathic lu- than *6A and *7B, whereas *13 has
life-threatening and the genotype pus erythematosus while taking normal activity.27
does not adequately predict the de- procainamide.16-18 The slow acetyla- Currently, the importance of
velopment of hemolytic anemia. For tor phenotype is an autosomal reces- these variants in NAT2 is most stud-
example, some patients with these sive trait. Studies have shown large ied for their association with a mod-
mutations experience toxicity after variations of the slow acetylator phe- estly increased risk for cancers, possi-
drug administration, and others do notype among ethnic groups: 40– bly because of prolonged exposure of
not. In addition, the treatment for 70% of Caucasians and African- the body to chemicals, drugs, or me-
drug-induced oxidative hemolytic Americans, 10–20% of Japanese and tabolites compared with fast acetyla-
anemia is merely cessation of drug Canadian Eskimo, more than 80% of tors.28 A recent preliminary result
administration, with blood transfu- Egyptians, and certain Jewish popula- suggested that impaired isoniazid
sion and corticosteroid administra- tions are slow acetylators.19,20 In East metabolism is associated with point
tion warranted in severe cases. Asia, the further north the geographic mutations in NAT2 in a small Japa-
G6PD deficiency is an example of origin of the population, the lower the nese population.29 This exciting re-
how genotypic analysis was devel- frequency of the slow acetylator sult awaits large population studies
oped about half a century after the gene.21-23 The reason for this trend is to establish clearly the relationship
clinical observation was made, and unknown, but it has been speculated between the NAT2 genotype and iso-
further characterization of the genetic that differences in dietary habits or the niazid acetylation. It still takes some
mutation provided no added clinical chemical or physical environment time to establish the clinical utility of
advantages. Although genetic consti- may be contributing factors. NAT2 genotype analysis to indepen-
tution may be at the core of explaining Allelic variation at the NAT2 gene dently predict isoniazid acetylation.
drug toxicity and efficacy, genotyping locus accounts for the polymorphism However, genotype NAT2 mutations
may not always directly affect therapy seen with acetylation of substrate could be an addition to the tradition-
or predict patient outcomes. drugs. There are 27 NAT2 alleles that al therapeutic drug monitoring for
have been reported. NAT2 is an un- isoniazid in the near future.
N-Acetyltransferase usual gene because it consists of
The acetylation polymorphism il- open-reading frames (i.e., protein- Genetic polymorphisms in the
lustrates another genetic polymor- coding regions) with no introns. CYP isoenzymes
phism of a drug-metabolizing enzyme Most variant NAT2 alleles involve The CYP isoenzyme superfamily
studied in the early era of pharmaco- two or three point mutations. For ex- comprises over 50 heme-containing
genetics. N-acetyltransferase (gene, ample, the variant NAT2*5B differs proteins that catalyze the oxidative
NAT), a phase-II conjugating liver en- from the wild-type at three nucle- metabolism of many structurally di-
zyme, catalyzes the N-acetylation otide positions, 341, 481, and 803; verse drugs and chemicals. It is one
(usually deactivation) and O-acetyla- NAT2*6A has two changes at posi- of the most widely studied drug-
tion (usually activation) of arylamine tions 282 and 590; NAT*13 has one metabolizing-enzyme systems. Its
carcinogens and heterocyclic amines. point mutation at 282; and NAT2*7A name is derived from the characteris-
The slow acetylator phenotype often has two changes at positions 282 and tic maximum spectral absorbance at
experiences toxicity from drugs such 857.18 NAT2*5B and *6A account for 450 nm, when it is in its reduced
as isoniazid, sulfonamides, procaina- 72–75% of all the variant NAT2 al- state. CYP exists as multiple forms or
mide, and hydralazine, whereas the leles, which includes at least 94% of isoenzymes, with each having vari-
fast acetylator phenotype may not re- all variant alleles in Caucasians, Japa- able distribution in different tissues.
spond to isoniazid and hydralazine in nese, and Hispanics and 83% of the The basis for nomenclature is depen-
the management of tuberculosis and NAT2 alleles in African-Americans. dent on the similarity among the ge-
hypertension, respectively. During the NAT2*5B is the most common allele netic sequences that encode the
development of isoniazid, isoniazid in Caucasians (40–46%), but occurs isoenzymes. 30 When the DNA se-
plasma concentrations were observed at a very low frequency in Japanese quence of the gene for one CYP
in a distinct bimodal population after (0.5%).24-26 NAT*6A, *7B, and *13 isoenzyme is less than 40% similar to
a standard dose. Patients with the share a mutation at C282T. NAT*5A, that of another, the two isoenzymes
highest plasma isoniazid levels were *5B, *6A, *7A, *7B, and *13 are asso- belong to different CYP families.
generally slow acetylators and they ciated with the slow acetylator phe- Each enzyme family is represented by
Am J Health-Syst Pharm—Vol 59 Nov 1, 2002 2063
CL I N I C A L F R O N T I E R S Drug metabolism
an Arabic number (e.g., CYP1) and mal recessive trait.35,36 An ultrarapid lower occurrence of nonfunctional al-
further divided into subfamilies in metabolizer phenotype has also been leles (e.g., *3, *4, *5,*6), but a higher
which the isoenzymes’ correspond- identified and found to result from frequency of alleles associated with re-
ing DNA sequences are approxi- gene duplication (up to 13 copies of duced activity (e.g., *10, *17).42
mately 70% identical. For example, CYP2D6).37 Poor metabolizers are Genotyping CYP2D6 has been
CYP1A2 belongs to family 1 and sub- more likely to have adverse effects shown to successfully predict the clear-
family A; the last Arabic number in- from drugs that are substrates of the ance of fluoxetine, fluvoxamine, de-
dicates a particular gene encoding for isoenzyme and decreased efficacy sipramine, and mexiletine.43-46 In some
the isoenzyme within the A subfami- from drugs requiring CYP2D6- instances, the genotype for CYP2D6
ly. More detailed descriptions of the mediated activation (e.g., codeine is has been useful in predicting adverse
CYP nomenclature are found in the converted into morphine by effects associated with antidepressants
literature.31,32 CYP2D6), while extensive and ul- and neuroleptics. Arrhythmias, nau-
CYP2D6. CYP2D6 isoenzyme trarapid metabolizers may have thera- sea, and vomiting occurred selectively
metabolizes 25–30% of all clinically peutic failure with drugs activated by in poor metabolizers during treatment
used medications, including dex- CYP2D6 (e.g., standard antidepres- with mexiletine, propafenone, and
tromethorphan, β -blockers (e.g., sant doses). 38 Because CYP2D6 dexfenfluramine largely because of ele-
metoprolol), antiarrhythmics, anti- isoenzyme metabolizes such a large vated plasma drug concentrations.46-48
depressants (e.g., fluvoxamine, flu- number of drugs used in the clinical Currently, preliminary dosage recom-
oxetine, imipramine, nortriptyline), setting, pharmacists have an impor- mendations based on CYP2D6 geno-
antipsychotics (e.g., haloperidol, ris- tant role in drug monitoring, includ- types are available for antidepres-
peridone), morphine derivatives, ing identifying CYP2D6 substrates, sants.49 This gives us a glimpse of how
and many other drugs. Variability in monitoring for drug efficacy and pharmacogenetics can suggest dose
the interindividual responses to these toxicity, and understanding the phe- regimens for a small population of
agents is often caused by genetic notypic and genotypic tools available. patients. Prospective studies are war-
polymorphisms in CYP2D6, also The frequency of the phenotype of ranted to address whether genotype-
termed the debrisoquin/sparteine ge- poor metabolizers differs among eth- based dose recommendations have a
netic polymorphism in reference to nic groups. Less than 1% of Asians, positive outcome on therapy.
the drugs that are its substrates that 2–5% of African-Americans, and 6– CYP2C9. Impaired metabolism of
led to its discovery. 33 Unlike the 10% of Caucasians are poor metabo- drugs metabolized by the CYP2C9
CYP3A family, CYP2D6 is a nonin- lizers of CYP2D6.4 The most com- isoenzyme, such as phenytoin, S-
ducible enzyme; thus, its genotype mon variant alleles in Caucasians are warfarin, 50 tolbutamide, losartan,
offers a high predictability of CYP2D6*3, *4, *5, and *6, which ac- and nonsteroidal antiinflammatory
CYP2D6-mediated metabolism. count for about 98% of poor metab- drugs (NSAIDs) (e.g., ibuprofen, di-
CYP2D6, the gene encoding olizers.39 The CYP2D6*3A allele is a clofenac, piroxicam, tenoxicam,
CYP2D6 isoenzyme, has the most frameshift mutation caused by a sin- mefenamic acid) has been noted.51,52
variations of all genes for CYP isoen- gle adenine deletion in exon 5 that The CYP2C9 genotype was first
zymes, with more than 75 allelic vari- results in a premature stop codon. observed to be correlative with the
ants identified to date, resulting from CYP2D6*4A contains a G-to-A tran- pharmacokinetics of tolbutamide.
point mutations, single base-pair de- sition in the last nucleotide of intron Three allelic variants of the CYP2C9
letions or additions, gene rearrange- 3, producing a splicing defect and gene have been identified that are as-
ments, and deletion of the entire subsequent frameshift in the open- sociated with decreased enzyme ac-
gene. These mutations result in ei- reading frame and premature stop tivity. 52,53 The variant alleles
ther a reduction or complete loss of codon.40 The CYP2D6*5 variant is CYP2C9*2 (Arg144Cys) and *3
activity.34 Administering a CYP2D6 caused by a deletion of the entire (Ile359Leu) contain single nucle-
substrate as a probe drug (e.g., bu- CYP2D6 gene.41 Although poor me- otide polymorphisms that result in
furalol, dextromethorphan, debriso- tabolizers may be homozygous for single amino acid substitutions.
quin, sparteine) and measuring the one particular defective allele (e.g., CYP2C9*2 and *3 were associated
metabolite-to-parent drug ratio in the CYP2D6*4/*4), compound het- with a 5.5- and 27.0-fold decrease in
urine (metabolic ratio) differentiate erozygosity (e.g., CYP2D6*4/*6) is the intrinsic clearance of S-warfarin,
extensive metabolizers from poor me- common. Despite a lower frequen- respectively, compared with the
tabolizers. Genotype–phenotype stud- cy of poor metabolizers, Asian and wild-type allele.54,55 As such, clinical
ies have revealed that poor metaboliz- African-American populations tend consequences of the CYP2C9*3 allele
ers possess two nonfunctional alleles to have reduced CYP2D6 activity com- are likely to be more dramatic than
and that the phenotype is an autoso- pared with Caucasians because of a those of CYP2C9*2. Homozygous
2064 Am J Health-Syst Pharm—Vol 59 Nov 1, 2002
CL I N I C A L F R O N T I E R S Drug metabolism
CYP2C9*3 alleles were found in poor worth mentioning that a recent strates have been used in phenotyp-
metabolizers of phenytoin, glipizide, study has elucidated the role of ing studies. The poor metabolizer
tolbutamide, and losartan. Increased CYP2C9 genotype on the metabo- phenotype is a result of two non-
risks of bleeding were observed in lism of celecoxib, a cyclooxygenase- functional alleles and is inherited as
patients with mutant alleles (poor 2 inhibitor.59 The study found that an autosomal recessive trait. In con-
metabolizers), and subsequent dos- patients either heterozygous or ho- trast, the extensive metabolizer phe-
age adjustments were required.50,56,57 mozygous who have at least one notype consists of both heterozygous
Phenytoin is a substrate of both copy of the CYP2C9*2 (i.e., and homozygous dominant geno-
CYP2C9 and CYP2C19 isoenzymes, CYP2C9*1/*2 or CYP2C9*2/*2) or types, but they usually cannot be dis-
but CYP2C9 is responsible for its CYP2C9*3 (i.e., CYP2C9*1/*3 or tinguished by phenotyping methods.
metabolism to a greater extent; thus, CYP2C9*3/*3) allele would have an At least five mutant alleles have
mutant alleles encoding the CYP2CP increased celecoxib plasma area- been identified.62 The most common
gene have a greater effect on the clini- under-the-concentration–time curve variant alleles in poor metabolizers,
cal toxicity of phenytoin. The as a result of the reduced drug me- CYP2C19*2 and *3, arise from single
CYP2C9*3 mutant allele occurs in ap- tabolism. The clinical significance of base-pair substitutions in exons 4
proximately 6–9% of Caucasians and this observation remains unclear. (CYP2C19*3) and 5 (CYP2C19*2)
Asians.52 CYP2C9*2 occurs in approxi- CYP2C9 genotyping may affect that introduce premature stop
mately 8–20% of Caucasians and less the clinical use of warfarin because codons and truncated polypeptide
frequently in African-Americans and of the relatively high prevalence of chains with no functional activity.63
is virtually absent in Asians. Individ- poor metabolizers, severe outcomes CYP2C19*2 is identified with a 40
uals who require a low dose of war- as a consequence of drug overdose, base-pair deletion at the beginning of
farin to maintain optimum anticoagu- and frequency with which it is pre- the exon, which shifts the reading
lation have a slightly higher frequency scribed. CYP2C9 genotyping assays frame to create an aberrant splice site
of variant CYP2C9 alleles than those are available only for clinical re- and produces a premature stop
who require a higher dose.58 One study search, but commercial assays are be- codon about 20 amino acids down-
found that life-threatening bleeding ing developed.60 Genotype testing for stream.64 CYP2C19*3 is mainly found
was four times more likely in a group CYP2C9 will allow pharmacists to in the Japanese population. There are
of patients requiring a lower dose of develop dose recommendations to also ethnic differences in the frequency
warfarin. These patients also had more reduce the risk of adverse drug reac- of the poor metabolizer phenotype.
difficulty establishing therapeutic anti- tions in patients receiving warfarin About 3–5% of Caucasians and 12–
coagulation, which led to multiple vis- and screen for high-risk patients who 23% of most Asian populations are
its to the hospital and prolonged hos- are candidates for lower initial war- poor metabolizers.65,66
pital stays resulting from serious or farin doses.56 Although relatively few drugs are
life-threatening bleeding events, and CYP2C19. CYP2C19 isoenzyme metabolized by CYP2C19, pro-
additional required laboratory test- metabolizes several pharmacologi- nounced pharmacodynamic effects
ing.56 CYP2C9 genotyping may help cally important therapeutic agents. tend to be seen in Asians treated with
identify high-risk patients who are Extensive and poor metabolizers ex- omeprazole because of the higher
candidates for lower warfarin doses, ist for S-mephenytoin, omeprazole frequency of poor metabolizers.67
more frequent monitoring, or alterna- and other proton-pump inhibitors, Poor metabolizers of mephenytoin
tive drug treatments. diazepam, propranolol, imipramine, also have higher serum omeprazole–
In addition to the metabolism of and amitriptyline. The phenotype metabolite ratios than extensive me-
warfarin and phenytoin, polymor- was initially determined using me- tabolizers because of impaired ome-
phisms in CYP2C9 have the potential phenytoin as a probe drug because of prazole metabolism.68 Results of a
to affect the toxicity of several the significant correlation between study by Furuta et al.69 suggested that
NSAIDS. For example, homozygous formation of the 4-hydroxyme- the CYP2C19 genotype might influ-
CYP2C9*3 alleles may result in slow- phenytoin metabolite and the ence the cure rates for Helicobacter
er metabolism of these drugs. How- amount of CYP2C19 in human liver pylori infection in patients with pep-
ever, there have been no reports cor- microsomes. 61 Phenotyping of tic ulcers. The cure rate was 100% in
relating CYP2C9 genotype to the CYP2C19 with mephenytoin is limit- poor metabolizers, 60% in patients
pharmacokinetics of NSAIDs. Since ed because of concerns about the use with heterozygous genotypes, and
NSAIDs have relatively high thera- of the probe drug, low urinary me- 29% in patients with homozygous
peutic indices, these polymor- tabolite concentration, and stability wild-types. This may be explained by
phisms may have less of an impact of the metabolite in urine. More re- the higher accumulation of plasma
on clinical consequences. It is cently, omeprazole and other sub- omeprazole concentrations in poor
Am J Health-Syst Pharm—Vol 59 Nov 1, 2002 2065
CL I N I C A L F R O N T I E R S Drug metabolism
metabolizers, resulting in a greater been elusive until recently. Conse- contains a G30597A mutation in
degree of gastric acid suppression.67 quently, these variations play a sig- exon 7, causing the deletion of exon
Similar to omeprazole, the extent of nificant role in the variability of oral 7 and reducing CYP3A5 activity.
lansoprazole and pantoprazole me- bioavailability and metabolism of CYP3A5*1 is more frequently ex-
tabolism is highly dependent on CYP3A substrates, including HIV pressed in non-Caucasian popula-
CYP2C19 genotype. Thus, interindi- protease inhibitors, benzodiaz- tions (30% of Caucasians, Japanese,
vidual differences in plasma concen- epines, calcium channel blockers, and Mexicans; 40% of Chinese; and
trations of these proton-pump inhibi- hydroxymethylglutaryl coenzyme 60% of African-Americans, South-
tors may be prospectively predicted by A- reductase inhibitors, antineoplas- east Asians, Pacific Islanders, and
genetically determined CYP2C19 sta- tic drugs, nonsedating antihista- Southwestern American Indians);
tus. However, the contributions of mines, and immunosuppressants. thus, these populations may metabo-
CYP2C19 isoenzyme to the metabo- These variations can result in differ- lize CYP3A substrates more rapidly.86
lism of these proton-pump inhibitors ences in drug efficacy and toxicity CYP3A5 appears to be an important
are not evenly distributed; omeprazole among individuals. genetic contributor to interindividu-
is more extensively metabolized by CYP3A activities are the sum of al and interracial differences in
CYP2C19 than pantoprazole, lanso- the activities of at least three CYP3A CYP3A-dependent drug metabolism.
prazole, and rabeprazole.70 isoenzymes: CYP3A4, CYP3A5, and Patients expressing both wild-type
Diazepam is another example of a CYP3A7.77,78 Interindividual variabil- CYP3A4 and CYP3A5 genotypes ex-
CYP2C19 substrate affected by this ity due to CYP3A4 activity alone may tensively metabolize CYP3A sub-
polymorphism. The half-life of diaz- vary by up to 50-fold. Functional strates, which may lead to a lack of
epam in plasma is significantly pro- consequences of a polymorphism in therapeutic effect. Prediction of drug
longed in individuals who are ho- the CYP3A4 promoter region interactions involving the inhibition
mozygous for the mutant CYP2C19*2 (A290G) (i.e., CYP3A4*1B) have and induction of CYP3A will contin-
allele (80 hours) compared with het- been studied as a possible cause of ue to be a challenge and clinically im-
erozygotes (64 hours) and people with this variability,79-82 but the effects of portant because of the diverse role
homozygous wild-type CYP2C19 (20 this SNP have not been clearly de- CYP3A plays in the metabolism of
hours).71,72 Asian populations have fined. Ethnic variation has been sug- currently available and future drugs.
been reported to exhibit slower diaz- gested as a possible reason, which However, the variability observed in
epam metabolism than Caucasians, may explain the higher frequency of CYP3A activity may not be solely due
possibly due to a higher frequency of the homozygous mutation in Ghana- to polymorphisms in the genes for
CYP2C19*2 and CYP2C19*3 geno- ian (51%) than in Scottish Caucasian these isoenzymes. The recent discov-
types. Poor metabolizers of CYP2C19 (0%) and Saudi populations (1%).83 ery of the PXR gene, a regulator of CYP
may be at a higher risk for diazepam It is estimated that CYP3A5 isoen- gene expression, provides another
toxicity, and caution must be exercised zyme is only present in 10–30% of possible factor for the variability in
in dosing diazepam. liver samples tested. 84,85 Recently, drug metabolism and a molecular ba-
CYP3A subfamily. CYP3A isoen- CYP3A5 isoenzyme was found to ac- sis for drug interactions. Identifying
zymes are the predominant subfamily count for at least 50% of the total the regulatory mechanisms of enzyme
of CYP enzymes, making it one of the CYP3A content in people who carry induction and polymorphisms within
most important drug-metabolizing the wild-type CYP3A5*1 allele (96– these regulatory elements and high-
enzymes. The genes for CYP3A isoen- 98% of the combined population), throughput screening for future drugs
zymes are expressed primarily in the suggesting that CYP3A5 may play a may allow accurate prediction of
liver and small intestines.73,74 Hepatic significant role in the metabolism of CYP3A enzyme induction and drug–
CYP3A4 isoenzyme has been esti- CYP3A substrates.86 Only people with drug interactions.87-91 Specific guide-
mated to metabolize almost 50% of at least one wild-type CYP3A5*1 allele lines for the use of CYP3A pharmaco-
currently used drugs as well as en- express large amounts of CYP3A5 genetics to modulate drug therapy are
dogenous and exogenous corticos- isoenzyme, resulting in a 2.5-fold in- under development.
teroids. Intestinal CYP3A4 isoen- crease in clearance of the probe drug
zyme contributes significantly to the (midazolam). The most common Summary
first-pass metabolism of orally ad- cause of loss of the expression of the Major genetic polymorphisms
ministered drugs.75 There is large in- CYP3A5 gene in the liver is an SNP at that affect drug-metabolizing en-
terindividual variability in genetic nucleotide 22,893 in intron 3 zymes are summarized in Table 1.
expression for, CYP3A exceeding 30- (CYP3A5*3), which causes alterna- The technology to identify SNPs is
fold in some populations,76 but evi- tive splicing (exon 3B) and protein available, and databases that house
dence for polymorphic activity has truncation. The CYP3A5*6 allele these SNPs and gene sequence infor-
2066 Am J Health-Syst Pharm—Vol 59 Nov 1, 2002
CL I N I C A L F R O N T I E R S Drug metabolism
mation are rapidly growing and groups.92,93 Although a genetic basis Conclusion
readily accessible. In the past, phar- is preferable to less objective mea- Pharmacogenetics has elucidated
macogenetics has been used to ex- sures, such as skin color, currently the genetic basis for interindividual
plain clinically overt toxicity or the there is no algorithm that can pro- variability in drug response. Pharma-
lack of efficacy in a subset of patients. vide a comprehensive predictive sur- cogenetics will continue to play a key
As the field continues to develop, rogate for all drug-metabolizing- role in defining strategies to optimize
pharmacogenetics will play an im- enzyme SNPs. Pharmacogenetics has drug therapy.
portant role in prospectively predict- thus far provided a drug–gene rela-
ing a patient’s drug activation and tionship to drug response and has References
detoxification status, such that a contributed in learning how to ad- 1. Vogel F. [Modern problems in genetics.]
therapeutic intervention can be minister certain drugs more effec- Ergeb Inn Med Kinderheilkd. 1959; 12:52-
125. In German.
made prior to drug administration tively and safely. As functional con- 2. Phillips KA, Veenstra DL, Oren E et al.
without exposing the patient to drug sequences of polymorphisms within Potential role of pharmacogenomics in re-
toxicity or therapeutic failure. Fur- drug metabolizing enzymes become ducing adverse drug reactions: a systemat-
ic review. JAMA. 2001; 286:2270-9.
ther, recent evidence indicates that better understood and genotype 3. Evans DA, McLeod HL, Pritchard S et al.
genotyping tests can more accurately analysis becomes less costly, pharma- Interethnic variability in human drug re-
predict a person’s ability to metabo- cogenetics may lead to the individu- sponses. Drug Metab Dispos. 2001; 29: 606-
10.
lize certain drugs than an approach alization of medication dosing and 4. Kalow W, Otton SV, Kadar D et al. Ethnic
based solely on ethnic or geographic improved therapeutics.60 difference in drug metabolism: debriso-
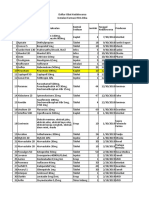
Table 1.
Genetic Polymorphisms Known To Influence Drug Response
Drugs with
Affected
Enzymea Variant Allele(s) Frequency of PMsb Metabolism Consequence(s) Recommendation
G6PD G6PD A, G6PD A(–) . . . Primaquine, sulfones, Hemolytic anemia Cessation of sulfa
sulfonamides, drugs
nitrofurans, vitamin
K analogues
NAT2 NAT*5B 40–70% of Caucasians Isoniazid, Increased relative risk . . .
and African- sulfonamides, of cancers and drug
Americans procainamide, toxicity
hydralazine
CYP2D6 CYP2D6*2A, 6–10% of Caucasians, β-receptor Lack of analgesic Dosage adjustment
CYP2D6*3, *4, *5, 2–5% of African- antagonists, effects from in PMs
*6, *10, *17 Americans, 1% of antiarrhythmics, codeine, standard
Asians antidepressants, antidepressant
antipsychotics, dosage ineffective
morphine
derivatives
CYP2C9 CYP2C9*2, CYP2C9*3 6–8% of Caucasians Warfarin, phenytoin, Increased bleeding Dosage adjustment
glipizide, episodes from needed for PMs to
tolbutamide, standard warfarin achieve optimal
losartan, NSAIDsc dose, low blood therapeutic
sugar levels in PMs benefit
CYP2C19 CYP2C19*2, 3–5% of Caucasians, S-mephenytoin, Increased omeprazole . . .
CYP2C19*3 12–23% of Asians omeprazole, AUCd and higher H.
diazepam, pylori eradication
propranolol, rate in PMs,
imipramine, prolonged half-life
amitriptyline of diazepam and
increased risk of
diazepam toxicity in
Asians
CYP3A4 CYP3A4*1B Under investigation Under investigation . . . . . .
CYP3A5 CYP3A5*1, CYP3A5*3, Under investigation Under investigation Increased CYP3A5*1 . . .
CYP3A5*6 activity, loss of
CYP3A5*3 activity,
lower CYP3A5*6
activity
a
G6PD = glucose-6-phosphate dehydrogenase, NAT = N-acetyltransferase, CYP = cytochrome P-450 isoenzyme system.
b
PMs = poor metabolizers.
c
NSAIDs = nonsteroidal antiinflammatory drugs.
d
AUC = area-under-the-concentration–time curve.
Am J Health-Syst Pharm—Vol 59 Nov 1, 2002 2067
CL I N I C A L F R O N T I E R S Drug metabolism
quine 4-hydroxylation in Caucasians and Kekkaku. 1967; 42:203-12. In Japanese. functional significance of individual muta-
Orientals. Can J Physiol Pharmacol. 1980; 22. Sunahara S, Motoyuki U, Ogawa M et al. tions by expression of chimeric genes. J
58:1142-4. Genetical and geographical studies on Biol Chem. 1990; 265:17209-14.
5. Wood AJ. Ethnic differences in drug dis- isoniazid inactivation. Science. 1961; 134: 37. Kroemer HK, Eichelbaum M. “It’s the
position and response. Ther Drug Monit. 1530-3. genes, stupid.” Molecular bases and clini-
1998; 20:525-6. 23. Karim AK, Elfellah MS, Evans DA et al. cal consequences of genetic cytochrome
6. Daly AK, Brockmoller J, Broly F et al. No- Human acetylator polymorphism: esti- P450 2D6 polymorphism. Life Sci. 1995;
menclature for human CYP2D6 alleles. mate of allele frequency in Libya and de- 56:2285-98.
Pharmacogenetics. 1996; 6:193-201. tails of global distribution. J Med Genet. 38. Bertilsson L, Dahl ML, Sjoqvist F et al. Mo-
7. Kletzien RF, Harris PK, Foellmi LA et al. 1981; 18:325-30. lecular basis for rational megaprescribing
Glucose-6-phosphate dehydrogenase: a 24. Cascorbi I, Drakoulis N, Brockmoller J et in ultrarapid hydroxylators of debriso-
“housekeeping” enzyme subject to tissue- al. Arylamine N-acetyltransferase (NAT2) quine. Lancet. 1993; 341:63. Letter.
specific regulation by hormones, nutri- mutations and their allelic linkage in unre- 39. Gaedigk A, Gotschall RR, Forbes NS et al.
ents, and oxidant stress. FASEB J. 1994; lated Caucasian individuals: correlation Optimization of cytochrome P4502D6
8:174-81. with phenotypic activity. Am J Hum Genet. (CYP2D6) phenotype assignment using a
8. Beutler E. G6PD deficiency. Blood. 1994; 1995; 57:581-92. genotyping algorithm based on allele fre-
84:3613-36. 25. Cascorbi I, Brockmoller J, Bauer S et al. quency data. Pharmacogenetics. 1999; 9:
9. Vulliamy TJ, D’Urso M, Battistuzzi G et al. NAT2*12A (803A–>G) codes for rapid 669-82.
Diverse point mutations in the human arylamine N-acetylation in humans. Phar- 40. Hanioka N, Kimura S, Meyer UA et al. The
glucose-6-phosphate dehydrogenase gene macogenetics. 1996; 6:257-9. human CYP2D locus associated with a
cause enzyme deficiency and mild or se- 26. Lin HJ, Han CY, Lin BK et al. Ethnic distri- common genetic defect in drug oxidation:
vere hemolytic anemia. Proc Natl Acad Sci. bution of slow acetylator mutations in the a G1934—a base change in intron 3 of a
1988; 85:5171-5. polymorphic N-acetyltransferase (NAT2) mutant CYP2D6 allele results in an aber-
10. Beutler E. The molecular biology of G6PD gene. Pharmacogenetics. 1994; 4:125-34. rant 3′ splice recognition site. Am J Hum
variants and other red cell enzyme defects. 27. Hein DW, Ferguson RJ, Doll MA et al. Genet. 1990; 47:994-1001.
Annu Rev Med. 1992; 43:47-59. Molecular genetics of human polymor- 41. Gaedigk A, Blum M, Gaedigk R et al. Dele-
11. Vulliamy T, Mason P, Luzzatto L et al. The phic N-acetyltransferase: enzymatic analy- tion of the entire cytochrome P450
molecular basis of glucose-6-phosphate sis of 15 recombinant wild-type, mutant, CYP2D6 gene as a cause of impaired drug
dehydrogenase deficiency. Trends Genet. and chimeric NAT2 allozymes. Hum Mol metabolism in poor metabolizers of the
1992; 8:138-43. Genet. 1994; 3:729-34. debrisoquine/sparteine polymorphism.
12. Carson PE, Ajmar F, Hashimoto F et 28. Grant DM, Goodfellow GH, Sugamori K Am J Hum Genet. 1991; 48:943-50.
al. Electrophoretic demonstration et al. Pharmacogenetics of the human ary- 42. Wang SL, Huang JD, Lai MD et al. Molec-
of stromal effects on haemolysate lamine N-acetyltransferases. Pharmacolo- ular basis of genetic variation in debriso-
glucose-6-phosphate dehydrogenase gy. 2000; 61:204-11. quin hydroxylation in Chinese subjects:
and 6-phosphogluconic dehydrogena- 29. Kita T, Tanigawara Y, Chikazawa S et al. polymorphism in RFLP and DNA se-
se. Nature. 1966; 210:813-5. N-acetyltransferase2 genotype correlated quence of CYP2D6. Clin Pharmacol Ther.
13. Hirono A, Beutler E. Molecular cloning with isoniazid acetylation in Japanese tu- 1993; 53:410-8.
and nucleotide sequence of cDNA for hu- berculous patients. Biol Pharm Bull. 2001; 43. Hamelin BA, Turgeon J, Vallee F et al.
man glucose-6-phosphate dehydrogenase 24:544-9. The disposition of fluoxetine but not ser-
variant A(–). Proc Natl Acad Sci. 1988; 85: 30. Nelson DR, Koymans L, Kamataki T et al. traline is altered in poor metabolizers of
3951-4. P450 superfamily: update on new se- debrisoquin. Clin Pharmacol Ther. 1996;
14. Stroncek D, Procter JL, Johnson J. Drug- quences, gene mapping, accession num- 60:512-21.
induced hemolysis: cefotetan-dependent bers and nomenclature. Pharmacogenetics. 44. Carrillo JA, Dahl ML, Svensson JO et al.
hemolytic anemia mimicking an acute in- 1996; 6:1-42. Disposition of fluvoxamine in humans is
travascular immune transfusion reaction. 31. Ingelman-Sundberg M, Oscarson M, Daly determined by the polymorphic CYP2D6
Am J Hematol. 2000; 64:67-70. AK et al. Human cytochrome P-450 (CYP) and also by the CYP1A2 activity. Clin
15. Evans DA, Manley KA, McKusch VA et al. genes: a web page for the nomenclature of Pharmacol Ther. 1996; 60:183-90.
Genetic control of isoniazid metabolism in alleles. Cancer Epidemiol Biomarkers Prev. 45. Spina E, Gitto C, Avenoso A et al. Rela-
man. Br Med J. 1960; 2:485-91. 2001; 10:1307-8. tionship between plasma desipramine
16. Evans DA. N-acetyltransferase. Pharmacol 32. Ingelman-Sundberg M, Daly AK, Oscar- levels, CYP2D6 phenotype and clinical
Ther. 1989; 42:157-234. son M et al. Human cytochrome P450 response to desipramine: a prospective
17. Wolkenstein P, Carriere V, Charue D et al. (CYP) genes: recommendations for the study. Eur J Clin Pharmacol. 1997; 51:
A slow acetylator genotype is a risk factor nomenclature of alleles. Pharmacogenetics. 395-8.
for sulphonamide-induced toxic epider- 2000; 10:91-3. 46. Lledo P, Abrams SM, Johnston A et al.
mal necrolysis and Stevens-Johnson syn- 33. Mahgoub A, Idle JR, Dring LG et al. Poly- Influence of debrisoquine hydroxylation
drome. Pharmacogenetics. 1995; 5:255-8. morphic hydroxylation of debrisoquine in phenotype on the pharmacokinetics of
18. Vatsis KP, Weber WW, Bell DA et al. No- man. Lancet. 1977; 2:584-6. mexiletine. Eur J Clin Pharmacol. 1993;
menclature for N-acetyltransferases. Phar- 34. Ingelman-Sundberg M, Evans WE. Un- 44:63-7.
macogenetics. 1995; 5:1-17. ravelling the functional genomics of the 47. Gross AS, Phillips AC, Rieutord A et al.
19. Knight RA, Selin MJ, Harris HW et al. Ge- human CYP2D6 gene locus. Pharmacoge- The influence of the sparteine/debriso-
netic factors influencing isoniazid blood netics. 2001; 11:553-4. quine genetic polymorphism on the dispo-
levels in humans. Trans Conf Chemother 35. Johansson I, Oscarson M, Yue QY et al. sition of dexfenfluramine. Br J Clin Phar-
Tuberc. 1959; 8:52-6. Genetic analysis of the Chinese cyto- macol. 1996; 41:311-7.
20. Evans DA. Survey of human acetylator chrome P4502D locus: characterization of 48. Botsch S, Heinkele G, Meese CO et al. Rap-
polymorphism in spontaneous disorders. J variant CYP2D6 genes present in subjects id determination of CYP2D6 phenotype
Med Genet. 1984; 21:243-53. with diminished capacity for debrisoquine during propafenone therapy by analysing
21. Nakagawa H, Sunahara S. [Studies on me- hydroxylation. Mol Pharmacol. 1994; 46: urinary excretion of propafenone glucu-
tabolism of isoniazid by a new chemical 452-9. ronides. Eur J Clin Pharmacol. 1994; 46:
determination of isoniazid (the 2nd re- 36. Kagimoto M, Heim M, Kagimoto K et al. 133-5.
port). Trimodal distribution of blood lev- Multiple mutations of the human cyto- 49. Kirchheiner J, Brosen K, Dahl ML et al.
els, inactivation in intestine and combina- chrome P450IID6 gene (CYP2D6) in poor CYP2D6 and CYP2C19 genotype-based
tion of isoniazid with serum protein.] metabolizers of debrisoquine. Study of the dose recommendations for antidepres-
2068 Am J Health-Syst Pharm—Vol 59 Nov 1, 2002
CL I N I C A L F R O N T I E R S Drug metabolism
sants: a first step towards subpopulation- phenytoin. J Pharmacol Exp Ther. 1998; 77. Schuetz JD, Beach DL, Guzelian PS et al.
specific dosages. Acta Psychiatr Scand. 286:1490-5. Selective expression of cytochrome P450
2001; 104:173-92. 63. Goldstein JA, de Morais SM. Biochemis- CYP3A mRNAs in embryonic and adult
50. Steward DJ, Haining RL, Henne KR et al. try and molecular biology of the human human liver. Pharmacogenetics. 1994; 4:
Genetic association between sensitivity to CYP2C subfamily. Pharmacogenetics. 11-20.
warfarin and expression of CYP2C9*3. 1994; 4:285-99. 78. Kolars JC, Lown KS, Schmiedlin-Ren P et
Pharmacogenetics. 1997; 7:361-7. 64. De Morais SM, Wilkinson GR, Blaisdell J al. CYP3A gene expression in human gut
51. Bhasker CR, Miners JO, Coulter S et al. et al. The major genetic defect responsible epithelium. Pharmacogenetics. 1994; 4:
Allelic and functional variability of cyto- for the polymorphism of S-mephenytoin 247-59.
chrome P4502C9. Pharmacogenetics. metabolism in humans. J Biol Chem. 79. Felix CA, Walker AH, Lange BJ et al.
1997; 7:51-8. 1994; 269:15419-22. Association of CYP3A4 genotype with
52. Sullivan-Klose TH, Ghanayem BI, Bell DA 65. Wilkinson GR, Guengerich FP, Branch treatment-related leukemia. Proc Natl
et al. The role of the CYP2C9-Leu359 allel- RA et al. Genetic polymorphism of S- Acad Sci. 1998; 95:13176-81.
ic variant in the tolbutamide polymor- mephenytoin hydroxylation. Pharmacol 80. Rebbeck TR, Jaffe JM, Walker AH et al.
phism. Pharmacogenetics. 1996; 6:341-9. Ther. 1989; 43:53-76. Modification of clinical presentation of
53. Stubbins MJ, Harries LW, Smith G et al. 66. Nakamura K, Goto F, Ray WA et al. In- prostate tumors by a novel genetic variant
Genetic analysis of the human cyto- terethnic differences in genetic polymor- in CYP3A4. J Natl Cancer Inst. 1998; 90:
chrome P450 CYP2C9 locus. Pharmaco- phism of debrisoquin and mephenytoin 1225-9.
genetics. 1996; 6:429-39. hydroxylation between Japanese and 81. Ball SE, Scatina J, Kao J et al. Population
54. Haining RL, Hunter AP, Veronese ME et Caucasian populations. Clin Pharmacol distribution and effects on drug metabo-
al. Allelic variants of human cytochrome Ther. 1985; 38:402-8. lism of a genetic variant in the 5′ promot-
P450 2C9: baculovirus-mediated expres- 67. Furuta T, Ohashi K, Kosuge K et al. er region of CYP3A4. Clin Pharmacol
sion, purification, structural character- CYP2C19 genotype status and effect of Ther. 1999; 66:288-94.
ization, substrate stereoselectivity, and omeprazole on intragastric pH in humans. 82. Paris PL, Kupelian PA, Hall JM et al. As-
prochiral selectivity of the wild-type and Clin Pharmacol Ther. 1999; 65:552-61. sociation between a CYP3A4 genetic
I359L mutant forms. Arch Biochem Bio- 68. Balian JD, Sukhova N, Harris JW et al. variant and clinical presentation in Afri-
phys. 1996; 333:447-58. The hydroxylation of omeprazole corre- can-American prostate cancer patients.
55. Rettie AE, Korzekwa KR, Kunze KL et al. lates with S-mephenytoin metabolism: a Cancer Epidemiol Biomarkers Prev. 1999;
Hydroxylation of warfarin by human population study. Clin Pharmacol Ther. 8:901-5.
cDNA-expressed cytochrome P-450: a 1995; 57:662-9. 83. Tayeb MT, Clark C, Ameyaw MM et al.
role for P-4502C9 in the etiology of (S)- 69. Furuta T, Ohashi K, Kamata T et al. Effect CYP3A4 promoter variant in Saudi, Gha-
warfarin-drug interactions. Chem Res of genetic differences in omeprazole me- naian and Scottish Caucasian popula-
Toxicol. 1992; 5:54-9. tabolism on cure rates for Helicobacter tions. Pharmacogenetics. 2000; 10:753-6.
56. Higashi MK, Veenstra DL, Kondo LM et pylori infection and peptic ulcer. Ann In- 84. Wrighton SA, Brian WR, Sari MA et al.
al. Association between CYP2C9 genetic tern Med. 1998; 129:1027-30. Studies on the expression and metabolic
variants and anticoagulation-related out- 70. Funck-Brentano C, Becquemont L, Lene- capabilities of human liver cytochrome
comes during warfarin therapy. JAMA. vu A et al. Inhibition by omeprazole of P450IIIA5 (HLp3). Mol Pharmacol. 1990;
2002; 287:1690-8. proguanil metabolism: mechanism of the 38:207-13.
57. Ninomiya H, Mamiya K, Matsuo S et al. interaction in vitro and prediction of in 85. Wrighton SA, Ring BJ, Watkins PB et al.
Genetic polymorphism of the CYP2C vivo results from the in vitro experi- Identification of a polymorphically ex-
subfamily and excessive serum phenytoin ments. J Pharmacol Exp Ther. 1997; 280: pressed member of the human cyto-
concentration with central nervous sys- 730-8. chrome P-450III family. Mol Pharmacol.
tem intoxication. Ther Drug Monit. 2000; 71. Wan J, Xia H, He N et al. The elimination 1989; 36:97-105.
22:230-2. of diazepam in Chinese subjects is depen- 86. Kuehl P, Zhang J, Lin Y et al. Sequence
diversity in CYP3A promoters and char-
58. Aithal GP, Day CP, Kesteven PJ et al. As- dent on the mephenytoin oxidation phe-
acterization of the genetic basis of poly-
sociation of polymorphisms in the cyto- notype. Br J Clin Pharmacol. 1996; 42:
morphic CYP3A5 expression. Nat Genet.
chrome P450 CYP2C9 with warfarin dose 471-4.
2001; 27:383-91.
requirement and risk of bleeding compli- 72. Qin XP, Xie HG, Wang W et al. Effect of
87. Dussault I, Lin M, Hollister K et al. Pep-
cations. Lancet. 1999; 353:717-9. the gene dosage of CgammaP2C19 on di- tide mimetic HIV protease inhibitors are
59. Tang C, Shou M, Rushmore TH et al. In- azepam metabolism in Chinese subjects. ligands for the orphan receptor SXR. J
vitro metabolism of celecoxib, a cycloox- Clin Pharmacol Ther. 1999; 66:642-6. Biol Chem. 2001; 276:33309-12.
ygenase-2 inhibitor, by allelic variant 73. Cholerton S, Daly AK, Idle JR et al. The 88. Synold TW, Dussault I, Forman BM. The
forms of human liver microsomal cyto- role of individual human cytochromes orphan nuclear receptor SXR coordinate-
chrome P450 2C9: correlation with P450 in drug metabolism and clinical re- ly regulates drug metabolism and efflux.
CYP2C9 genotype and in-vivo pharma- sponse. Trends Pharmacol Sci. 1992; 13: Nat Med. 2001; 7:584-90.
cokinetics. Pharmacogenetics. 2001; 11: 434-9. 89. Xie W, Barwick JL, Downes M et al. Hu-
223-35. 74. Shimada T, Yamazaki H, Mimura M et al. manized xenobiotic response in mice ex-
60. Evans WE, Relling MV. Pharmacoge- Interindividual variations in human liver pressing nuclear receptor SXR. Nature.
nomics: translating functional genomics cytochrome P-450 enzymes involved in 2000; 406:435-9.
into rational therapeutics. Science. 1999; the oxidation of drugs, carcinogens and 90. Forman BM. Polymorphisms in promis-
286:487-91. toxic chemicals: studies with liver mi- cuous PXR: an explanation for interindi-
61. Lasker JM, Wester MR, Aramsombatdee crosomes of 30 Japanese and 30 Cauca- vidual differences in drug clearance?
E et al. Characterization of CYP2C19 and sians. J Pharmacol Exp Ther. 1994; 270: Pharmacogenetics. 2001; 11:551-2.
CYP2C9 from human liver: respective 414-23. 91. Xie W, Barwick JL, Simon CM et al. Re-
roles in microsomal tolbutamide, S-me- 75. Paine MF, Shen DD, Kunze KL et al. First- ciprocal activation of xenobiotic response
phenytoin, and omeprazole hydroxyla- pass metabolism of midazolam by the hu- genes by nuclear receptors SXR/PXR and
tions. Arch Biochem Biophys. 1998; 353: man intestine. Clin Pharmacol Ther. 1996; CAR. Genes Dev. 2000; 14:3014-23.
16-28. 60:14-24. 92. McLeod HL. Pharmacogenetics: more
62. Ibeanu GC, Goldstein JA, Meyer U et al. 76. Watkins PB. Cyclosporine and liver than skin deep. Nat Genet. 2001; 29:247-8.
Identification of new human CYP2C19 transplantation: will the midazolam test 93. McLeod HL. Race and responsiveness to
alleles (CYP2C19*6 and CYP2C19*2B) in make blood level monitoring obsolete? drugs for heart failure. N Engl J Med.
a Caucasian poor metabolizer of me- Hepatology. 1995; 22:994-6. 2001; 345:766-7.
Am J Health-Syst Pharm—Vol 59 Nov 1, 2002 2069
You might also like
- Tesda Written ExamDocument8 pagesTesda Written ExamAngel Cayanan95% (37)
- Do Not Crush MedsDocument3 pagesDo Not Crush Medsapi-249622140No ratings yet
- Commonly Prescribed Psychotropic MedicationsDocument2 pagesCommonly Prescribed Psychotropic Medicationsburlacuraduu100% (1)
- Usp 36 - NF 31 - ContenidoDocument2 pagesUsp 36 - NF 31 - ContenidoRodriguito Gabriel FloresNo ratings yet
- BHU Daily Stock PerformaDocument6 pagesBHU Daily Stock PerformabilalNo ratings yet
- Pharmaco GenomicsDocument6 pagesPharmaco GenomicsPrasanna BabuNo ratings yet
- Chapter 056Document42 pagesChapter 056Adistri KimNo ratings yet
- Pharmacogenetics and The Concept of Individualized Medicine: BS ShastryDocument6 pagesPharmacogenetics and The Concept of Individualized Medicine: BS Shastrykunalprabhu148No ratings yet
- DialoguesClinNeurosci 7 223Document8 pagesDialoguesClinNeurosci 7 223mantradaNo ratings yet
- Zhou2008 Vis DujDocument47 pagesZhou2008 Vis DujAnAn BanhGaoNo ratings yet
- PharmacogeneticsDocument30 pagesPharmacogeneticsShailendra Sk100% (3)
- Genetic Polymorphism in Drug MetabolismDocument55 pagesGenetic Polymorphism in Drug MetabolismMounika16 Pedamallu100% (2)
- Pharmacogenomics: Dr. Santoshkumar - Jeevangi Associate Professor Dept. of Pharmacology MR Medical College GulbargaDocument58 pagesPharmacogenomics: Dr. Santoshkumar - Jeevangi Associate Professor Dept. of Pharmacology MR Medical College GulbargaSantu PrashuNo ratings yet
- The Clinical Role of Genetic Polymorphisms in Drug-Metabolizing EnzymesDocument12 pagesThe Clinical Role of Genetic Polymorphisms in Drug-Metabolizing EnzymesMasDhedotNo ratings yet
- Dosage Form For Personalized Medicine: HistoryDocument11 pagesDosage Form For Personalized Medicine: HistoryNayeema KhowserNo ratings yet
- Genetic Factors in Drug MetabolismDocument9 pagesGenetic Factors in Drug MetabolismGloria Adetokunbo OjoNo ratings yet
- Pharmacogenetics and Pharmacogenomics in Moderate-to-Severe PsoriasisDocument14 pagesPharmacogenetics and Pharmacogenomics in Moderate-to-Severe PsoriasisDian Arief PutraNo ratings yet
- Lecture 8 - PharmacogeneticsDocument38 pagesLecture 8 - PharmacogeneticsNicko WijayaNo ratings yet
- Genetic Variation in Drug Disposition: Balmukunda Regmi and Laxman BharatiDocument11 pagesGenetic Variation in Drug Disposition: Balmukunda Regmi and Laxman BharatiAnsiSilambiNo ratings yet
- Pharmacogenomics PDFDocument12 pagesPharmacogenomics PDFsivaNo ratings yet
- Seminar in Pharmacology 2Document10 pagesSeminar in Pharmacology 2Jiggy JoeNo ratings yet
- Pharmacogenomics in Cardiovascular MedicineDocument11 pagesPharmacogenomics in Cardiovascular MedicineVeronica BalanNo ratings yet
- Kocal 2017Document24 pagesKocal 2017AnAn BanhGaoNo ratings yet
- Pharmacogenomics: New Challenges For Thai Anesthesiologists: J Med Assoc Thai 2017 100 (Suppl. 7) : S250-S258Document9 pagesPharmacogenomics: New Challenges For Thai Anesthesiologists: J Med Assoc Thai 2017 100 (Suppl. 7) : S250-S258Ronald André Buleje HinostrozaNo ratings yet
- PharmacogeneticsDocument80 pagesPharmacogeneticsThư SV. Nguyễn AnhNo ratings yet
- Pharmacogenetics: Dr. P.Naina Mohamed PHDDocument21 pagesPharmacogenetics: Dr. P.Naina Mohamed PHDJeevan Khanal100% (1)
- 1217-Article Text-5162-1-10-20220708Document6 pages1217-Article Text-5162-1-10-20220708srirampharmNo ratings yet
- Metabolic Drug Interactions With ImmunosuppressantsDocument32 pagesMetabolic Drug Interactions With Immunosuppressants陈梓强No ratings yet
- IA - Molecular Biology of Pharmacology 160908Document39 pagesIA - Molecular Biology of Pharmacology 160908Susi RutmalemNo ratings yet
- 5685 - UHN2012Pharmacogenomic PharmacogeneticDocument44 pages5685 - UHN2012Pharmacogenomic PharmacogeneticAdinda TobingNo ratings yet
- 2020 Article 80954Document9 pages2020 Article 80954Chintya Redina HapsariNo ratings yet
- Pharmagenomics: Pharmaceutical BiotechnologyDocument6 pagesPharmagenomics: Pharmaceutical Biotechnologykapy_123No ratings yet
- Pharmacogenetics of Drug-Gene Interactions: Muh. Akbar BaharDocument49 pagesPharmacogenetics of Drug-Gene Interactions: Muh. Akbar BaharHemi Amalia AmirullahNo ratings yet
- Pharmacogenetics of Drug-Metabolizing2005Document8 pagesPharmacogenetics of Drug-Metabolizing2005Hoàng Mỹ ChinhNo ratings yet
- Review Article: Volker M. Lauschke, Lili Milani, and Magnus Ingelman-SundbergDocument16 pagesReview Article: Volker M. Lauschke, Lili Milani, and Magnus Ingelman-SundbergLuis Angel Garcia RuizNo ratings yet
- Pharmacogenetics Polymorphism and Efficacy of DrugsDocument11 pagesPharmacogenetics Polymorphism and Efficacy of DrugsRohitNo ratings yet
- Pharmacogenetics 141110022651 Conversion Gate01Document45 pagesPharmacogenetics 141110022651 Conversion Gate01Jeevan Khanal0% (1)
- 1 Farmakogenomik 2023Document51 pages1 Farmakogenomik 2023yayu latifahNo ratings yet
- Pharmacogenetics of Cardiovascular Drug TherapyDocument11 pagesPharmacogenetics of Cardiovascular Drug Therapybalaji5563No ratings yet
- An Omics'' View of Drug DevelopmentDocument5 pagesAn Omics'' View of Drug DevelopmentOti DeeaNo ratings yet
- An Omics'' View of Drug Development: Research CommentaryDocument5 pagesAn Omics'' View of Drug Development: Research CommentaryVeronica BalanNo ratings yet
- 9 Personalized MedicineDocument34 pages9 Personalized Medicinehamza najmNo ratings yet
- Drug DispositionDocument22 pagesDrug DispositiongabriellaNo ratings yet
- Farm A Kogen EtikDocument60 pagesFarm A Kogen Etikrahmad wahyudiNo ratings yet
- BLOK 12 - IT 2 - Farmakogenetik 1 - MISDocument38 pagesBLOK 12 - IT 2 - Farmakogenetik 1 - MISMuhammad AdilNo ratings yet
- Genetic Polymorphisms of Cytochrome P450 Enzymes and The Effect On Interindividual, PharmacokinetDocument11 pagesGenetic Polymorphisms of Cytochrome P450 Enzymes and The Effect On Interindividual, PharmacokinetLuciana OliveiraNo ratings yet
- Pharmacology and Pharmacogenomics of Neurological Medications Used in Pregnancy 2013Document12 pagesPharmacology and Pharmacogenomics of Neurological Medications Used in Pregnancy 2013Ricardo Robles AlfaroNo ratings yet
- Assignment On Genetic PolymorphismDocument19 pagesAssignment On Genetic PolymorphismSayema KhanumNo ratings yet
- Pharmacogenetics 2022 23Document52 pagesPharmacogenetics 2022 23Erdem Altun100% (1)
- Karriker, 2007 - Genetic Predisposition To Adverse Drug Events in DogsDocument7 pagesKarriker, 2007 - Genetic Predisposition To Adverse Drug Events in DogsJoana CarreiraNo ratings yet
- Pharmaco GeneticsDocument52 pagesPharmaco GeneticsManikanta GupthaNo ratings yet
- Choi ClinPharmacolTher 2011 PDFDocument11 pagesChoi ClinPharmacolTher 2011 PDFhuouinkyoumaNo ratings yet
- PharmecogenomicsDocument21 pagesPharmecogenomicsRatan Ratan100% (1)
- Pharmacogenomics:: Increasing The Safety and Effectiveness of Drug TherapyDocument12 pagesPharmacogenomics:: Increasing The Safety and Effectiveness of Drug TherapyFlorentina GasttiNo ratings yet
- Research Pharmacogenomics PDFDocument10 pagesResearch Pharmacogenomics PDFmohammedNo ratings yet
- Pharmaco GenomicsDocument14 pagesPharmaco GenomicsMarfu'ah Mar'ahNo ratings yet
- A 30 Years Review On Pharmacokinetics ofDocument18 pagesA 30 Years Review On Pharmacokinetics ofAlexander CanoNo ratings yet
- Pharmacogenetics and Antipsychotic Treatment ResponseDocument15 pagesPharmacogenetics and Antipsychotic Treatment Responsebruna.c.moscatelNo ratings yet
- Future of Cancer Associated Transcription FactorDocument5 pagesFuture of Cancer Associated Transcription FactorIakovos GiacomoNo ratings yet
- Pharmacogenomics: Learning ObjectivesDocument16 pagesPharmacogenomics: Learning ObjectivesJamilNo ratings yet
- 2013 AapsjDocument8 pages2013 AapsjSCYoungNo ratings yet
- 215 FullDocument14 pages215 Fullnicacio18No ratings yet
- Personalized Medicine: The Promise of Pharmacogenomics Nancy ReinholdDocument9 pagesPersonalized Medicine: The Promise of Pharmacogenomics Nancy Reinholdnan-toddNo ratings yet
- Farmakogenetik AdoDocument31 pagesFarmakogenetik AdoEndang SusilowatiNo ratings yet
- Pharmacogenomics in Precision Medicine: From a Perspective of Ethnic DifferencesFrom EverandPharmacogenomics in Precision Medicine: From a Perspective of Ethnic DifferencesWeimin CaiNo ratings yet
- Daftar Obat High Alert Instalasi Farmasi Rsia Mutiara BundaDocument1 pageDaftar Obat High Alert Instalasi Farmasi Rsia Mutiara BundaAnonymous idPPyERfBnNo ratings yet
- Drug ListDocument104 pagesDrug Listخانه پزشکNo ratings yet
- Compulsive: Obsessive DisorderDocument16 pagesCompulsive: Obsessive DisorderGlyssa CabarrubiasNo ratings yet
- Piis0885392404002155 PDFDocument36 pagesPiis0885392404002155 PDFRohit ParasharNo ratings yet
- Zolpidem TartrateDocument2 pagesZolpidem Tartrateapi-3797941No ratings yet
- Codeine Phosphate (Drug Study)Document2 pagesCodeine Phosphate (Drug Study)Franz.thenurse6888100% (2)
- Borang JeanDocument102 pagesBorang JeanAsepDarussalamNo ratings yet
- Comprehensive Exam NCM 145Document17 pagesComprehensive Exam NCM 145Adrian Dela CruzNo ratings yet
- AnalgesicDocument42 pagesAnalgesicVinayak SinghNo ratings yet
- Admin Articles Formulation and Evaluation of Hydroxy Propyl Methyl Cellulose Transdermal Drug Delivery SystemsDocument4 pagesAdmin Articles Formulation and Evaluation of Hydroxy Propyl Methyl Cellulose Transdermal Drug Delivery SystemsKristine Dwi PuspitasariNo ratings yet
- Observation Reflection 1Document2 pagesObservation Reflection 1api-391659138No ratings yet
- Sitti Misfiyani Kusuma's VideoDocument18 pagesSitti Misfiyani Kusuma's VideoaniNo ratings yet
- Brompheniramine WikiDocument2 pagesBrompheniramine WikiMattNo ratings yet
- Walgreens LetterDocument5 pagesWalgreens LetterAnonymous P4XJDtdtq0No ratings yet
- Acalculous Cholecystitis CaseDocument35 pagesAcalculous Cholecystitis CaseSaada Enok MedtamakNo ratings yet
- PharmacologyDocument68 pagesPharmacologyvansal liu80% (5)
- Clinical ToxicologyDocument17 pagesClinical ToxicologyElfahra Casanza Amalda100% (1)
- Poster ThivyaDocument1 pagePoster ThivyaThivya ShankariNo ratings yet
- Patent UrachusDocument4 pagesPatent UrachusJustin Ahorro-DionisioNo ratings yet
- TinnitusDocument60 pagesTinnitusYowendruJunNo ratings yet
- Drug Admin and IV Rate Quiz - ANSWER KEYDocument3 pagesDrug Admin and IV Rate Quiz - ANSWER KEYJessica KruppNo ratings yet
- Extemporaneous Dispensing ProceduresDocument2 pagesExtemporaneous Dispensing ProceduresAsadZahidNo ratings yet
- CEKDocument4 pagesCEKTri SulistyoriniNo ratings yet
- PharmacologyDocument18 pagesPharmacologyMichael PiducaNo ratings yet
- Reviewing Depot Injection Efficacy in The Treatment of SchizophreniaDocument10 pagesReviewing Depot Injection Efficacy in The Treatment of SchizophreniaAnonymous raLgWVyqNo ratings yet