Professional Documents
Culture Documents
Acute Diarrhea: Evidence-Based Management: Review Article
Acute Diarrhea: Evidence-Based Management: Review Article
Uploaded by
Iwan IrwanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Diarrhea: Evidence-Based Management: Review Article
Acute Diarrhea: Evidence-Based Management: Review Article
Uploaded by
Iwan IrwanCopyright:
Available Formats
+Model
ARTICLE IN PRESS
J Pediatr (Rio J). 2015;xxx(xx):xxx---xxx
1
www.jped.com.br
REVIEW ARTICLE
2 Acute diarrhea: evidence-based management夽
3 Q2 Kátia Galeão Brandt ∗ , Margarida Maria de Castro Antunes, Giselia Alves Pontes da Silva
4 Centro de Ciências da Saúde (CCS), Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil
5 Received 6 May 2015; accepted 15 June 2015
6
KEYWORDS Abstract
7
Acute diarrhea; Objectives: To describe the current recommendations on the best management of pediatric
8
Gastroenteritis; patients with acute diarrheal disease.
9
Children; Data source: PubMed, Scopus, Google Scholar.
10
Hydration; Data summary: There has been little progress in the use of oral rehydration salts (ORS) in
11
Child nutrition recent decades, despite being widely reported by international guidelines. Several studies have
12 been performed to improve the effectiveness of ORS. Intravenous hydration with isotonic saline
13 solution, quickly infused, should be given in cases of severe dehydration. Nutrition should be
14 ensured after the dehydration resolution, and is essential for intestinal and immune health.
15 Dietary restrictions are usually not beneficial and may be harmful. Symptomatic medications
16 have limited indication and antibiotics are indicated in specific cases, such as cholera and
17 moderate to severe shigellosis.
18 Conclusions: Hydration and nutrition are the interventions with the greatest impact on the
19 course of acute diarrhea.
20 © 2015 Sociedade Brasileira de Pediatria. Published by Elsevier Editora Ltda. All rights reserved.
21
22 PALAVRAS-CHAVE Diarreia aguda: manejo baseado em evidências
Diarreia aguda;
23
Gastroenterite; Resumo
24
Crianças; Objetivos: descrever as recomendações atuais sobre a melhor maneira de conduzir o paciente
25
Hidratação; pediátrico com doença diarreica aguda.
26
Nutrição infantil Fonte dos dados: PubMed, Scopus, Scholar Google.
27 Síntese dos dados: Houve pouco avanço na utilização dos sais de reidratação oral (SRO) nas
28 últimas décadas apesar de ser amplamente divulgado através de diretrizes internacionais.
29 Vários estudos vêm sendo realizados na tentativa de melhorar a eficácia do SRO. Hidratação
30 venosa com solução salina isotônica, infundida de forma rápida, deve ser indicada em casos
31 de desidratação grave. A nutrição deve ser assegurada logo após a resolução da desidratação,
夽 Please cite this article as: Brandt KG, de Castro Antunes MM, da Silva GAP. Acute diarrhea: evidence-based management. J Pediatr (Rio
J). 2015. http://dx.doi.org/10.1016/j.jped.2015.06.002
∗ Corresponding author.
E-mail: katiabrandt@uol.com.br (K.G. Brandt).
http://dx.doi.org/10.1016/j.jped.2015.06.002
0021-7557/© 2015 Sociedade Brasileira de Pediatria. Published by Elsevier Editora Ltda. All rights reserved.
JPED 295 1---8
+Model
ARTICLE IN PRESS
2 Brandt KG, et al.
32 sendo primordial para a saúde intestinal e imunológica. Restrições alimentares usualmente não
33 são benéficas e podem ser prejudiciais. As medicações sintomáticas têm indicação restrita e
34 antibióticos são indicados em casos específicos, cólera e shiguelose moderada a grave.
35 Conclusões: a hidratação e a nutrição continuam sendo as intervenções com melhor impacto
36 sobre o curso da diarreia aguda.
37 © 2015 Sociedade Brasileira de Pediatria. Publicado por Elsevier Editora Ltda. Todos os direitos
38 reservados.
39
40 Introduction researchers have observed physicians’ poor adherence to 87
the recommendations provided by international health orga- 88
41 Acute diarrheal disease (ADD) is a public health problem in nizations, as well as by medical societies, which periodically 89
42 many regions of the world, especially where poverty pre- publish guidelines on the subject.1,8---10 90
43 vails. A model that aims to explain the incidence or mortality Why --- in spite of broad scientific evidence --- do physicians 91
44 associated with the ADD involves a large number of variables choose to treat ADD based on obsolete conduct? This is the 92
45 (biological, environmental, socio-cultural) and is very com- reason for the performance of this review. Even at present, 93
46 plex. Conversely, a reductionist approach contributes little the inappropriate use of ORT/IRT can be observed, as well 94
47 to the understanding and solution of the problem.1,2 as dietary guidelines that are almost iatrogenic, and even 95
48 The scientific community, over the past four decades, the indication of medications without any scientific basis.4 96
49 established a consensus on the most effective measures Therefore, this review aimed to carry out a synthesis of 97
50 to reduce the incidence, morbidity, and mortality of ADD. the current knowledge on ADD management by focusing on 98
51 Some measures aimed at reducing the incidence of diar- ORT/IRT, diet during the acute diarrheal process, the judi- 99
52 rheal disease constitute interventions that are beyond the cious use of symptomatic medications, probiotics, zinc, and 100
53 medical approach of the problem and are based on envi- antibiotics. 101
54 ronmental condition improvement: water supply, adequate
55 treatment of human waste, education, and food safety.
56 Exclusive breastfeeding for at least 6 months and supple- ADD management 102
57 mented up to 2 years of age has a significant impact in
58 reducing the disease incidence and severity. In the field of There is no consensus on the concept of ADD, but some 103
59 biomedicine, the development of a vaccine against rotavirus basic aspects have been covered in several publications.8,9,11 104
60 and universal vaccine coverage are important contributions In this review, ADD is considered as a diarrheal episode 105
61 that have an impact on ADD incidence, by decreasing the that has the following characteristics: abrupt onset, pre- 106
62 severe forms and the number of hospitalizations, thus redu- sumably infectious etiology, potentially self-limited, with a 107
63 cing the risk of death.3,4 course of less than 14 days, increased volume and/or fre- 108
64 Regarding mortality, the therapeutic management with quency of stool, and fecal loss of nutrients (mainly water and 109
65 emphasis on oral rehydration therapy (ORT) and intravenous electrolytes). Its major complications can thus be inferred 110
66 rehydration therapy (IRT), recommended since the 1970s, (hydroelectrolytic disorders, nutritional deficits), providing 111
67 are milestones of twentieth-century medicine. In 1994, the basis for its management. 112
68 Ruxin5 wrote an article commemorating the 25th anniversary From a clinical point of view, ADD can be classified 113
69 of the ORT implementation and concluded (by observation, as: watery diarrhea syndrome (which constitutes the vast 114
70 and expressing some pessimism): ‘‘the formidable and per- majority of infectious diarrheal diseases), bloody diarrhea 115
71 sistent ignorance of the western medical establishment, syndrome, and persistent diarrhea (when the episode lasts 116
72 which continues over twenty-five years after the discovery more than 14 days). Regardless of the causative agent, in the 117
73 of ORT, is phenomenal.’’ majority of diarrheal episodes of infectious etiology, thera- 118
74 The 21st century has arrived, and despite several pub- peutic management is based on hydration maintenance and 119
75 lished articles showing the efficiency and effectiveness of nutritional status.1,4,9,12 120
76 ORT and IRT, it can be observed that ADD management is Regarding severity, ADD is classified as mild, moder- 121
77 still being performed in ignorance of scientific evidence.6,7 ate, or severe: mild when signs of dehydration are not 122
78 In a recent article, Walker and Walker2 presented a observed; moderate when there are mild or moderate signs 123
79 model, The Lives Saved Tool (LiST), and analyzed the impact of dehydration and rehydration can be performed orally; and 124
80 of using oral rehydration salts (ORS), zinc, and antibiotics severe when it results in more intense dehydration with or 125
81 for dysentery on ADD mortality reduction. Low-osmolality without electrolyte disturbances, and requires intravenous 126
82 ORS, the use of zinc in risk groups for persistent diarrhea, therapy.9,13 127
83 and use of antibiotics only in selected cases of dysentery all Most ADD cases show mild or moderate severity and are 128
84 demonstrated a positive impact on the assessed outcomes. not treated at health services, hence the importance of 129
85 The accumulated scientific knowledge on the best home treatment guidelines for diarrheal disease in order 130
86 management of patients with ADD is extensive; however, to prevent dehydration. Hospitals receive cases with more 131
JPED 295 1---8
+Model
ARTICLE IN PRESS
Q1 Acute diarrhea 3
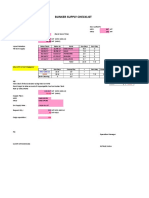
132 exuberant symptoms and dehydrated patients or those at Table 1 Clinical dehydration scale (adapted from Freed-
133 risk for dehydration; clinical pictures secondary to severe man et al.23 ).
134 vomiting or high-output diarrhea.9,13
135 From a physiopathological point of view, there are Characteristics 0 1 2
136 two basic mechanisms involved: osmotic and secretory. General Normal Thirsty, Drowsy,
137 Secondary to these mechanisms, alterations in intestinal appearance restless, or limp, cold,
138 motility can also occur. The osmotic mechanism is observed lethargic, sweaty;
139 when there is an increase in luminal osmolality, as it occurs but irritable comatose or
140 in diarrhea associated with rotavirus, in which damage when not
141 occurs in the proximal small bowel mucosa, with increasing touched
142 the undigested lactose in the intestinal lumen. The excess Eyes Normal Slightly Very sunken
143Q3 sugar, when fermented by bacteria that are part of the sunken
144 colonic microflora, originate short-chain fatty acids, acid Mucous Moist Sticky Dry
145 radicals that explain the distension and abdominal pain, and membranes
146 in some cases, perianal hyperemia. The diarrhea is watery (tongue)
147 and explosive. The secretory mechanism occurs when there Tears Present Decreased Absent tears
148 is a stimulation of secretion mediators by the exotoxins tears
149 produced by bacterial pathogens (Vibrio cholerae, entero-
150 toxigenic Escherichia coli) or by inflammation mediators, Note: Score = 0, no dehydration; score = 1---4, some dehydration;
151 such as in diarrhea associated with Shigella strains. From score = 5---8, moderate to severe dehydration.
152 the viewpoint of fecal losses, what essentially differentiates
153 the two mechanisms is the loss of sodium, which is higher
154 in the secretory form and may be greater than 70 mEq of diarrhea associated with vomiting has a higher risk of 191
155 sodium per liter of stool.14 dehydration.9 192
156 In more severe forms of ADD, in which high-output diar- The use of scoring systems to determine the hydration 193
157 rhea occurs, it is important to characterize the type of status and disease severity is considered useful in the mana- 194
158 mechanism involved so that the losses can be appropri- gement of children with diarrhea. The clinical dehydration 195
159 ately replaced. However, most ADD pictures in childhood, scale (CDS; Table 1), developed in 2008 for children aged 196
160 even those that lead to dehydration and require hospital 1---36 months with ADD treated in emergency rooms, has 197
161 treatment, show good response to standard management,13 been validated in several studies.15 The CDS considers four 198
162 which will be discussed elsewhere in this article. clinical items (overall appearance, eyes, mucosa, and tears) 199
163 The digestive-absorptive functions are maintained in to classify the child as ‘‘no dehydration,’’ ‘‘some dehy- 200
164 almost all children affected by ADD, and thus, if an adequate dration,’’ or ‘‘moderate/severe dehydration.’’ The disease 201
165 caloric intake is offered, there is minimum risk of malnour- severity score provides a more comprehensive measure of 202
166 ishment or aggravation of a pre-existing malnutrition status. ADD impact on the child’s health. The Vesikari severity score 203
167 There are few situations where diet restrictions or changes (Table 2) is a classic score that has been recently validated 204
168 are necessary. The nutritional approach will be reviewed in in a modified version; it has demonstrated good applicabil- 205
169 another item. ity in different services and populations.16 It does not assess 206
hydration status, but rather the impact of ADD in different 207
populations (mild, moderate, and severe) and the response 208
170 Hydration to interventions.17 209
Laboratory tests are not indicated in the routine assess- 210
171 Dehydration is the main complication of acute diarrhea, ment of children with ADD, but can help determine 211
172 and hydration status assessment should be one of the first dehydration severity, with low levels of serum bicarbonate 212
173 actions to be taken regarding the management of a child (<15 mEq/L) and increase in urea levels (>10 nmol/L) show- 213
174 with diarrhea. Acute weight loss during the diarrheal episode ing a good positive predictive value for moderate to severe 214
175 is considered the best parameter to assess dehydration. dehydration.18 215
176 According to the loss, dehydration is classified as mild (<5% In a dehydrated child, electrolyte treatment consists of 216
177 weight loss), moderate (5---10%), or severe (>10%); dehydra- rehydration and loss replacement. ORT should be prefer- 217
178 tion severity classification is essential for the treatment.9 ably used for rehydration, whereas IRT should be used only 218
179 Due to the difficulty in obtaining information on the previous in cases of ORT failure or severe dehydration. A systematic 219
180 weight (to estimate weight loss), this parameter has limited review that compared the use of ORT and IRT in children 220
181 practical usefulness, and other clinical variables should be with different degrees of dehydration concluded that there 221
182 used. was no difference regarding the risk of metabolic disorder, 222
183 Clinical evaluation is usually used to define the hydration mean duration of diarrheal episode, and need for fluids in 223
184 status; however, it may show interpersonal variations and, relation to the type of therapy used. The hospital length of 224
185 thus, validated clinical signs capable of being evaluated in stay was lower in the group using ORT. Regarding the unfa- 225
186 a simple and objective way should be used. The best signs vorable outcomes, there was more phlebitis in the group 226
187 related to moderate/severe dehydration are slowed capil- that received IRT, and higher incidence of paralytic ileus in 227
188 lary filling, decreased skin turgor, and changes in breathing the group that received ORT. The ORT failure rate was 1:25, 228
189 pattern. Clinical presentation of the disease can also alert i.e., for every 25 children that received ORT, one required 229
190 to the risk of dehydration, and a child with high-output IRT.19 230
JPED 295 1---8
+Model
ARTICLE IN PRESS
4 Brandt KG, et al.
Table 2 Vesicari modified severity score (adapted from Carmo et al.29 ).
Score 0 1 2 3
Diarrhea duration, hours 0 1---96 97---120 ≥121
Maximum number of stools in 24 h 0 1---3 4---5 ≥6
Vomiting duration, hours 0 1---24 25---48 ≥49
Maximum number of vomiting episodes in 24 h 0 1 2---4 ≥5
Maximum measured temperature (◦ C) <37 37.1---38.4 38.5---38.9 ≥39
Visit to a healthcare service --- --- Primary Hospital
healthcare service emergency
Treatment --- Venous rehydration Hospitalization ---
Note: mild, 0---8; moderate, 9---10; severe, ≥11.
231 Intravenous hydration has been used for more than a cen- progress regarding the use of ORS would be the fact that, ini- 277
232 tury, but the logistics required for its implementation and tially, there was a large investment in educational programs 278
233 the associated complications have shown that it is of little for the use of ORS, but with the emergence of several other 279
234 use when it is necessary to hydrate a large number of indi- educational efforts for ADD prevention and treatment (vac- 280
235 viduals during infectious diarrhea epidemics. Around 1970, cination, breastfeeding campaigns, nutrition, and hygiene), 281
236 ORS was developed in order to correct dehydration caused ORT has lost priority. The need to maintain educational cam- 282
237 by severe infectious diarrhea, particularly cholera-related paigns for priority use of ORS should be emphasized, so that 283
238 diarrhea. ORS was initially developed as an isotonic solution, new mothers can be educated about its use.4 284
239 i.e., osmolality of 311 mOsm/kg H2 O and sodium concentra- Other possible explanations for the inadequate use of ORS 285
240 tion of 90 mEq/L, thus becoming the standard solution of the include children’s refusal to drink it (possibly related to the 286
241 World Health Organization (WHO).20 flavor) and the fact that the oral solution does not reduce 287
242 In spite of the initial success, there was a change diarrheal losses. Considering this fact, a way to improve this 288
243 in the world scenario, characterized by a lower occur- scenario has been sought. Flavored ORS, present in some 289
244 rence of cholera-related diarrhea and higher incidence commercial products, increases its palatability, but it does 290
245 of viral diarrhea. In this context, there was a concern not appear to modify the consumed volume.24 The addition 291
246 regarding the sodium concentration of the standard WHO of zinc, prebiotics, amino acids, disaccharides, and glucose 292
247 solution, which would be very high in relation to losses polymers has resulted in only a modest improvement in ORS 293
248 in viral diarrhea cases. Approximately a decade ago, stud- effectiveness.9 294
249 ies confirmed the benefit of using hypotonic solutions with The addition of the substrate that leads to the produc- 295
250 osmolality of 245 mOsm/kg H2 O and sodium concentrations tion of short chain fatty acids (SCFAs) has aroused interest, 296
251 of 60---75 mEq/L in non-cholera-related diarrhea. It has been as SCFAs are readily absorbed by colonocytes and stimulate 297
252 shown that children who used hypotonic solutions had less the absorption of fluids and sodium. Studies have suggested 298
253 vomiting, lower fecal losses, shorter duration of disease, and a benefit of adding a resistant starch (substrate that leads 299
254 less need for intravenous hydration when compared with to the formation of SCFAs in the colon) to the ORS. In a sys- 300
255 those who used the solution previously recommended by tematic Cochrane review, the authors found that the use 301
256 the WHO. Hypotonic solutions also contain lower glucose of ORS added to a resistant starch was associated with a 302
257 concentrations, which ensure the adequate ratio for the reduced need for intravenous infusion and lower losses from 303
258 coupled transport of sodium ions and water by the intestinal diarrhea.25 Despite the possible benefits, some technical 304
259 mucosa.21 problems are yet to be solved, as an opaque solution is 305
260 To promote its acceptance, the oral hydration solution formed, which rapidly precipitates; the ideal suspension to 306
261 should be given in fractionated, small portions. How- solve this problem has not been identified yet. 307
262 ever, the high volume required for rehydration may not Although preferably ORT should be used, intravenous 308
263 be tolerated by the child, and solution intake refusal or hydration is necessary and crucial in severe dehydration 309
264 even vomiting may occur. A nasogastric tube (NGT) is cases. Possible controversies about what represents the best 310
265 indicated in such circumstances, as well as in situations procedure to implement intravenous hydration are related 311
266 where intravenous or intraosseous hydration is impossible, to the type of fluid, the volume, and rate of infusion. 312
267 with advantages such as: hyper-hydration prevention, non- Regarding the type of solution, there is evidence that the 313
268 invasiveness, rapid treatment onset, and lower cost. It has isotonic saline solution (0.9% saline) is preferable to the 314
269 been demonstrated that hydration via NGT is as effective as hypotonic solution (0.45% saline), preventing the occurrence 315
270 intravenous hydration in cases of moderate dehydration.22 of hyponatremia without causing hypernatremia.26 316
271 Nevertheless, healthcare workers are more familiar with the As for the infusion volume and velocity, studies compar- 317
272 use of intravenous hydration than with NGT hydration.23 ing the infusion of 20 mL/kg (fast) vs. 60 mL/kg (ultrafast) 318
273 The effectiveness of ORS in reducing morbidity and mor- of 0.9% saline solution, for one hour, in children with intra- 319
274 tality from acute diarrhea episodes is undeniable, but its venous hydration indication due to ORT failure, showed that 320
275 use does not meet the goals and has not made any progress children submitted to ultra-fast infusion had a higher fre- 321
276 in the last 30 years. A possible explanation for the lack of quency of hypernatremia and later hospital discharge than 322
JPED 295 1---8
+Model
ARTICLE IN PRESS
Acute diarrhea 5
323 those submitted to rapid infusion, with no difference in found an increased use of homemade ORS when compared 385
324 rehydration rate. Therefore, the current evidence does not to that observed in the 1996 PNDS (16% vs. 37%) and conse- 386
325 justify the use of ultra-fast rehydration.27 quent decrease in the use of ORS in the same period (44% 387
326 According to WHO recommendations, loss replacement vs. 19%).31 388
327 should be carried out, whenever possible, through the Consistent with this problem, Munos et al.,30 in the pre- 389
328 oral route, and it should be started during intravenous viously mentioned systematic review, found that advising on 390
329 rehydration.13 Intravenous hydration should be suspended as the use of both ORS and homemade solutions confuses the 391
330 soon as the child is hydrated and alert, ensuring the child’s population, decreasing the effectiveness of the strategy to 392
331 hydration through ORT. As a guideline, the WHO recommends combat mortality from diarrhea, and they recommend that 393
332 a volume of ¼ cup (50---100 mL) for children younger than priority should be given to ORS, by making it available to the 394
333 two years, ½ cup (100---200 mL) for children aged 2---10 years, entire population. 395
334 and free volume for those aged >10 years. The solution to Despite all considerations about rehydration, the goal to 396
335 be used for diarrheal loss replacement should be the hypo- be achieved is the initial prevention of dehydration. Thus, 397
336 tonic ORS, but if it cannot be used, the WHO advises using it is necessary, according to the strategy proposed by the 398
337 other salinized fluids, such as rice water, vegetable broth, WHO, to start ORT at home, at the start of the diarrheal 399
338 and homemade oral hydration solution. Breast milk can be picture, in order to replace the losses.13 The families should 400
339 used as replacement fluid in a nursing child. However, fluids be educated about the early onset of oral hydration and 401
340 such as energy drinks, soft drinks, and juices high in sorbitol evidence of its failure, such as vomiting and signs of dehy- 402
341 should not be used as replacement fluids due to low sodium dration. In a study that assessed the mother’s knowledge on 403
342 content and high osmolality. ADD management in the city of Recife, it was found that 404
343 The use of homemade ORS, a solution prepared by hand most mothers did not have adequate knowledge of the use- 405
344 at home by adding salt and sugar to water, is included fulness of ORS in preventing or treating dehydration. The 406
345 in the Child Health Handbook of the Brazilian Ministry of authors made the following considerations: ‘‘The results of 407
346 Health28 (Caderneta de Saúde da Criança do Ministério da this study show that, even with the improvement in mater- 408
347 Saúde do Brasil), which teaches how to prepare the solu- nal knowledge about ORT for more than a decade, a greater 409
348 tion by using the ‘‘pinch and scoop’’ method (a handful of effort is necessary by health professionals to create strate- 410
349 sugar and three pinches of salt in 200 mL of water). The ORS gies to transmit the information to the mothers in a more 411
350 can also be prepared by using a measuring spoon and a tea- efficient manner.’’32 412
351 spoon/tablespoon. The WHO, in its 2005 document on acute
352 diarrhea treatment, makes a brief comment on the possi-
353 bility of its use (by using a teaspoon/tablespoon), reporting Diet 413
354 that, while potentially effective, it is not recommended due
355 to its inadequate preparation and consumption. Although the maintenance of an adequate diet for the 414
356 A study carried out in Ouro Preto, Brazil, which assessed child’s age is a priority for intestinal mucosa regenera- 415
357 the concentration of sodium and glucose in ORS solutions tion, inadequate feeding practices are still observed in the 416
358 prepared by health workers in the region, found a high per- management of children with acute diarrhea. Enterocytes 417
359 centage (71.1---96.1%) of inadequate preparation, varying obtain their nutrients primarily from the intestinal lumen 418
360 according to the preparation method used (lower inade- content; thus fasting or dietary restrictions can slow down 419
361 quacy was observed with the pinch and scoop method). the renewal process of the cells damaged by infectious 420
362 When the health agents were asked about the ORS prepara- process.33 Intestinal malabsorption, of higher or lower sever- 421
363 tion method they taught to the families, about 30% reported ity, may occur in ADD depending on the damage caused by 422
364 they indicated the use of the measuring spoon, followed by the pathogen; however, good nutrition must be ensured and 423
365 the teaspoon/tablespoon (19%), and finally the pinch and dietary restrictions should not be implemented with the jus- 424
366 scoop method (6%). Conversely, only 17% of health work- tification of decreasing diarrheal losses. The usual diet must 425
367 ers reported the availability of the measuring spoon in the be maintained when the child is hydrated. In case of mild 426
368 Basic Health Units (Unidades Básicas de Saúde [UBS]) of the to moderate dehydration, food should be offered four to 427
369 region. In that study, the authors point to the fact that inade- five hours after the onset of rehydration.9 The maintenance 428
370 quate concentration of solutes and the balance between salt of breastfeeding during diarrheal episode, even in children 429
371 and glucose impairs the hydration potential of the home- with mild to moderate dehydration, is a consensus.34 430
372 made ORS, putting children at risk; the main message of the In a systematic review on dietary management of diar- 431
373 study was the lack of qualification of the health workers to rhea in low- and middle-income countries, a few points 432
374 teach the population with regard to homemade ORS.29 about the use of lactose in the diet were analyzed. The 433
375 In a systematic review on the effect of ORS on mortality normal amount of lactose can be maintained safely in most 434
376 from diarrhea, it was concluded that there is clear evidence children with diarrhea; however, the transient lactase defi- 435
377 that the WHO ORS is effective in reducing mortality; how- ciency and the consequent poor digestion of lactose can 436
378 ever, there is no evidence on the effectiveness of other worsen the diarrheal picture in a small group of children. 437
379 homemade solutions (including the homemade ORS) in com- Lactose restriction would be beneficial in selected cases, 438
380 bating child death from dehydration.30 Despite the lack of with reduced losses and shorter time of diarrheal episode 439
381 evidence and possible risks associated with ORS replacement after the restriction is observed. The children most likely 440
382 by the homemade ORS, the National Demographic Research to benefit from lactose restriction would be those who 441
383 on Women’s and Children’s Health (Pesquisa Nacional de develop severe dehydration and the malnourished. Lactose 442
384 Demografia e Saúde da Criança e da Mulher [PNDS]) of 2006 restriction by decreasing milk supply, associated with the 443
JPED 295 1---8
+Model
ARTICLE IN PRESS
6 Brandt KG, et al.
444 maintenance of the rest of the homemade diet, would be drugs (scopolamine) and antiphysetics agents (simethicone) 502
445 related to a better weight gain compared to the predomi- should not be indicated. 503
446 nant use of formulas without lactose.34
447 It is suggested that, for children not yet exposed to cow’s
448 milk-based formula, this first exposure should be avoided
Antiemetic drugs 504
449 during or shortly after the ADD episode, to avoid sensitiza-
450 tion to cow’s milk protein.35 However, there is no evidence Vomiting is frequent in ADD, and antiemetics are excessively 505
451 that switching to soy or hypoallergenic formula would be prescribed without considering the intensity of vomiting. In 506
452 beneficial for the child. most cases, the vomiting ceases when the child is hydrated, 507
453 In children that have started a solid food diet, it must as dehydration, even when subclinical, can cause vomiting. 508
454 have an adequate caloric content, as well as macro- and When vomiting is sporadic, there is no indication for 509
455 micronutrients. In hospitalized children with diarrhea, antiemetic use; when vomiting is intense, there is an 510
456 higher energy intake was associated with shorter duration increased risk of dehydration and hospitalization, and these 511
457 of the episode and, consequently, to a better outcome.36 drugs benefit the patients. It is important to remember 512
458 An adequate diet during the diarrheal picture can reduce that the risk of side effects increases when antiemetics 513
459 the occurrence of new episodes. Inadequate nutritional are used in dehydrated patients or those with electrolyte 514
460 approach during the diarrheal period can lead to mal- disturbances.39 515
461 nutrition, as well as installation of the vicious cycle of Among the most commonly used drugs are: H1- 516
462 malnutrition, reduced resistance to new enteropathogens, Histamine receptor blockers (promethazine, dimenhydri- 517
463 recurrence of diarrheal episodes, and more nate), dopamine receptor antagonists (metoclopramide), 518
464 malnutrition.37 and serotonin-5HT (ondansetron). 519
465 Regarding the use of handmade or processed food in the The literature does not have good scientific evidence that 520
466 diet during the diarrheal episode, no evidence was found supports the use of metoclopramide and dimenhydrinate in 521
467 on the superiority of industrial formulas compared to ade- ADD.39 Regarding ondansetron, several studies have shown 522
468 quate homemade diet. Juices with high fructose, sucrose, that it reduces the risk of dehydration and hospitalization in 523
469 and sorbitol contents should be avoided, because their high the subset of patients with a high frequency of vomiting.40 524
470 osmolality can exacerbate diarrheal losses.35
471 The child should be offered a usual diet, including foods Antidiarrheal drugs 525
472 with fiber and fat. Diet supplementation with vegetable oil
473 is a WHO recommendation to increase the caloric density The search for drugs that act by reducing the volume of 526
474 of foods, preventing malnutrition. Studies carried out in the stool and/or the time of diarrheal episode has been the 527
475 1990s suggested that fiber intake can decrease the time of subject of a constant search. Studies with adsorbents, alu- 528
476 liquid stools.38 minum silicate, and diosmectite are found in the literature, 529
477 Anorexia can affect children with acute diarrhea, a fact but without encouraging results. Loperamide, an antimotil- 530
478 commonly found in the acute phase of the disease, which ity drug, was banned from pediatric prescription since its 531
479 is more severe in the event of dehydration, acidosis, and toxic effects were identified as associated with the central 532
480 hypokalemia. The disorders must be corrected and food nervous system, in addition to the risk of causing paralytic 533
481 should be offered in small portions, often respecting the ileus.41 534
482 child’s wishes. The lack of appetite is transient and the Among the drugs classified as adsorbents, kaolin---pectin 535
483 appropriate food should be available to promote nutritional was used in the past, but its use was discontinued, as its 536
484 recovery at the earliest opportunity.38 effectiveness was not demonstrated. Its cosmetic effect 537
of making the stool semi-solid, without changing the fluid 538
485 Drug management of ADD volume, could give the impression of an improved clinical 539
picture and could reduce diarrheal surveillance in relation 540
to fluid supply. Another drug, diosmectite, a natural product 541
486 Symptomatic: pain and fever based on aluminum silicate and magnesium that is not com- 542
mercialized in Brazil, has been the object of studies, but its 543
487 Fever is absent in most cases of ADD. Dehydration may lead effectiveness has not been demonstrated.41 544
488 to an increase in body temperature in young children and The international guidelines are unanimous in stating 545
489 it can be an important symptom in ADD with blood in the that there is no indication for the use of these drugs in 546
490 stool. Fever should be treated when >39 ◦ C or when the tem- ADD.1,4,8,9 547
491 perature increase is associated with symptoms that cause
492 discomfort to the infant. The antipyretic drugs most fre-
493 quently used are acetaminophen and metamizole.1,4,8 Antisecretory drugs 548
494 Cramp-like abdominal pain is a common symptom of
495 osmotic diarrhea (excess of intestinal gas), and tenesmus In ADD pictures in which the secretory mechanism is involved 549
496 is observed when there is a significant inflammatory com- and diarrheal losses are important, the use of racecadotril 550
497 ponent, usually in ADD associated with Shigella. In the can benefit patients. By reducing fecal loss and disease 551
498 first case, a reduction in the diet supply of dairy prod- duration (it affects the secretory process by inhibiting the 552
499 ucts alleviates the symptoms; in the second case, the enkephalinase), it facilitates the hydration status mainte- 553
500 indication of drugs with analgesic effect --- acetaminophen nance and, therefore, reduces the chance of hospitalization. 554
501 and metamizole --- benefits the patient.1,4,8 Antispasmodic In these cases, ORT has been recommended as adjuvant 555
JPED 295 1---8
+Model
ARTICLE IN PRESS
Acute diarrhea 7
556 therapy; there is no evidence that its use reduces the need When the causative agent is a protozoan, the etiological 610
557 for IRT.42 treatment is rarely indicated, except in immunodepressed 611
patients.1,8,9 612
558 Zinc
Final considerations 613
559 In 2004, the WHO and UNICEF brought attention to the
560 impact of zinc in reducing the severity of the diarrheal In 2005, the World Health Organization revised13 the guide- 614
561 episode and the number of subsequent ADD episodes in chil- lines for ADD treatment, and defined the treatment goals: 615
562 dren younger than 5 years. The explanation for this effect prevent/treat dehydration, prevent nutritional aggrava- 616
563 would be the modulation of the immune system and also tion, and reduce the duration and severity of diarrheal 617
564 because it has an antisecretory property.43 episode. These goals can be achieved through the proper 618
565 Most studies were conducted in poor regions and use of ORT/IRT, maintenance of adequate food intake 619
566 recruited children at higher risk of developing more severe and, in some cases, judicious use of symptomatic med- 620
567 diarrheal episodes, including persistent diarrhea. At that ication (antipyretic, analgesic, and anti-emetic drugs), 621
568 moment, the recommendation was to use zinc associated zinc, antisecretory drugs, probiotics, and antibiotics. These 622
569 with ORT for all children younger than 5 years old. Later recommendations remain unaltered and almost all interna- 623
570 studies in developed regions, which recruited children at low tional guidelines published since then corroborate them. 624
571 risk for severe and/or persistent diarrhea, showed no addi- Despite the scientific evidence supporting this conduct, 625
572 tional benefit of the use of zinc. Currently, the indication why are children not being adequately treated in practice? 626
573 is restricted to children belonging to risk groups that origi- Why do pediatricians not adhere to the guidelines? 627
574 nate mainly from the poorest regions: malnourished children The explanation is not simple and involves several 628
575 younger than 5 years of age and those with history of previ- aspects: the fact that the families expect medical care to 629
576 ous episodes of ADD or hospitalization.44 offer an intervention that will result in a rapid disappear- 630
ance of symptoms; the belief that, for each disease, there 631
is a medication that will immediately terminate the patho- 632
577 Probiotics logical process; and the difficulty physicians have in building 633
a trusting relationship during consultations that often last 634
578Q4 Only some strains of probiotics have been studied in the ADD only a few minutes. 635
579 context. Such studies should be carefully analyzed regard- Nevertheless, researchers worldwide have been evaluat- 636
580 ing the evaluated outcomes and assessed strains, because ing intervention studies on ADD and assessing which conducts 637
581 there are different mechanisms of action; what is assessed in actually have a scientific basis. The consensus is that the 638
582 relation to a strain cannot simply be transferred to another. maintenance of hydration status and proper nutrition are 639
583 Lactobacillus GG and Saccharomyces boulardi are the most the recommended interventions for almost all children with 640
584 often scientifically tested. ADD. 641
585 The action of probiotics occurs mainly through antag-
586 onism, immunomodulation, or pathogen exclusion. The
587 antagonism and/or exclusion can have a short-term effect Conflicts of interest 642
588 on ADD.45
The authors declare no conflicts of interest. Q5
589 Most studies were carried out in developed countries. 643
590 They analyzed the following variables as outcome: duration
591 of diarrheal episode, reduction of fecal losses, and hospi- References 644
592 talization, and found a beneficial effect. It is necessary to
593 conduct studies to analyze the cost-benefit of using probi- 1. Farthing M, Salam MA, Lindberg G, et al. Acute diarrhea in 645
594 otics as an adjunct therapy to ORT/IRT in underdeveloped adults and children: a global perspective. J Clin Gastroenterol. 646
595 and developing countries.8,12 2013;47:12---20. 647
2. Walker CLF, Walker N. The Lives Saved Tool (LiST) as a model 648
for diarrhea mortality reduction. BMC Med. 2014;29:70. 649
596 Antibiotics 3. Assis AS, Valle DA, Antunes GR, et al. Rotavirus epidemiol- 650
ogy before and after vaccine introduction. J Pediatr (Rio J). 651
597 Antibiotics are not indicated in most ADD episodes, even 2013;89:470---6. 652
598 when the cause is bacterial. Almost all cases have a self- 4. The United Nations Children’s Fund (UNICEF)/World Health 653
599 limited and benign course, as long as the patient remains Organization (WHO). Diarrhea: why children are still dying and 654
600 hydrated. Even in the most severe diarrheal episodes, the what can be done. Geneva; 2009. 655
601 use of antimicrobials is a conduct of exception. 5. Ruxin JN. Magic bullet: the history of oral rehydration therapy. 656
Med Hist. 1994;38:363---97. 657
602 The main issue to be highlighted is that there is no effec-
6. Guandalini S. Acute diarrhea in children in Europe: do we know 658
603 tive antibiotic therapy for most agents associated with ADD. to treat it. J Pediatr Gastroenterol Nutr. 2008;46:S77---80. 659
604 Furthermore, the indiscriminate use may bring harm to the 7. Costa AD, Silva GA. Oral rehydration therapy in emergency 660
605 patient due to the devastating effect in the intestinal micro- departments. J Pediatr (Rio J). 2011;87:175---9. 661
606 biota, an important mechanism of protection. 8. NICE. Review of Clinical Guideline (CG84) --- Diarrhoea and 662
607 The WHO recommends the use of antimicrobial drugs in vomiting caused by gastroenteritis: diagnosis, assessment and 663
608 severe cases of ADD associated with Shigella (ciprofloxacin, management in children younger than 5 years. Available from: 664
609 ceftriaxone) and cholera (tetracycline, erythromycin). https://www.nice.org.uk/guidance/cg84 [cited 21.04.15]. 665
JPED 295 1---8
+Model
ARTICLE IN PRESS
8 Brandt KG, et al.
666 9. Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, rehydration of children with gastroenteritis: a prospective ran- 727
667 Szajewska H. European Society for Pediatric Gastroenterology, domised study. Arch Dis Child. 2006;91:226---32. 728
668 Hepatology, and Nutrition/European Society for Pediatric Infec- 27. Freedman SB, Parkin PC, Willan AR, Schuh S. Rapid versus 729
669 tious Diseases evidence-based guidelines for the management standard intravenous rehydration in paediatric gastroen- 730
670 of acute gastroenteritis in children in Europe: update 2014. J teritis: pragmatic blinded randomised clinical trial. BMJ. 731
671 Pediatr Gastroenterol Nutr. 2014;59:132---52. 2011;17:d6976. 732
672 10. Szajewska H, Hoekstra JH, Sandhu B. Management of acute 28. Caderneta de saúde da criança. Brasília: Ministério da Saúde; 733
673 gastroenteritis in Europe and the impact of the new recom- 2013. 734
674 mendations: a multicenter study. The Working Group on Acute 29. Carmo LF, Pereira LM, Silva CA, Cunha AC, Quintaes KD. 735
675 Diarrhoea of the European Society for Paediatric Gastroenterol- Concentração de sódio e glicose em soro de reidratação oral 736
676 ogy, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. preparado por agentes comunitários de saúde. Cien Saude 737
677 2000;30:522---7. Colet. 2012;17:445---52. 738
678 11. Pour TR, Koyfman A, Rumyar MS. Emergence centre manage- 30. Munos MK, Walker CL, Black RE. The effect of oral rehydration 739
679 ment of paediatric diarrhea: an overview. Afr J Emerg Med. solution and recommended home fluids on diarrhoea mortality. 740
680 2013;3:75---82. Int J Epidemiol. 2010;39:i75---87. 741
681 12. Piescik-Lech M, Shamir R, Guarino A, Szajewska H. Review 31. Ministério da Saúde Pesquisa nacional de demografia e saúde 742
682 article: the management of acute gastroenteritis in children. da criança e da mulher. Available from: http://bvsms.saude. 743
683 Aliment Pharmacol Ther. 2013;37:289---303. gov.br/bvs/pnds/saude nutricional.php [cited 30.05.15]. 744
684 13. World Health Organization. The treatment of diarrhea --- a man- 32. Vanderlei LC, Silva GA. Diarreia aguda: o conhecimento materno 745
685 ual for physicians and other senior health workers. 4th rev. sobre a doença reduz o número de hospitalizações nos menores 746
686 Geneva: WHO; 2005. de dois anos? Rev Assoc Med Bras. 2004;50:276---81. 747
687 14. Whyte LA, Jenkins HR. Pathophysiology of diarrhoea. PCH. 33. Sandhu BK. Rationale for early feeding in childhood gastroen- 748
688 2012;22:443---7. teritis. J Pediatr Gastroenterol Nutr. 2001;33:S13---6. 749
689 15. Goldman RD, Friedman JN, Parkin PC. Validation of the clini- 34. Gaffey MF, Wazny K, Bassani DG, Bhutta ZA. Dietary 750
690 cal dehydration scale for children with acute gastroenteritis. management of childhood diarrhea in low- and middle- 751
691 Pediatrics. 2008;122:545---9. income countries: a systematic review. Am J Public Health. 752
692 16. Schnadower D, Tarr PI, Gorelick MH, et al. Validation of 2013;13:S17. 753
693 the modified Vesikari score in children with gastroenteritis in 35. Koletzko S, Osterrieder S. Acute infectious diarrhea in children. 754
694 5 US emergency departments. J Pediatr Gastroenterol Nutr. Dtsch Arztebl Int. 2009;106:539---47. 755
695 2013;57:514---9. 36. Islam M, Roy SK, Begum M, Chisti MJ. Dietary intake and clinical 756
696 17. Freedman SB, Eltorky M, Gorelick M, Pediatric Emergency response of hospitalized patients with acute diarrhea. Food Nutr 757
697 Research Canada Gastroenteritis Study Group. Evaluation of Bull. 2008;29:25---31. 758
698 a gastroenteritis severity score for use in outpatient settings. 37. Guerrant RL, Oriá RB, Moore SR, Oriá MO, Lima AA. Malnutrition 759
699 Pediatrics. 2010;125:e1278---85. as an enteric infectious disease with long-term effects on child 760
700 18. Hayajneh WA, Jdaitawi H, Al Shurman A, Hayajneh YA. Com- development. Nutr Rev. 2008;66:487---505. 761
701 parison of clinical associations and laboratory abnormalities in 38. Sullivan PB. Nutritional management of acute diarrhea. Nutri- 762
702 children with moderate and severe dehydration. J Pediatr Gas- tion. 1998;14:758---62. 763
703 troenterol Nutr. 2010;50:290---4. 39. Carter B, Fedorowictz Z. Antiemetic treatment for acute gas- 764
704 19. Hartling L, Bellemare S, Wiebe N, Russell K, Klassen TP, Craig troenteritis in children: an updated Cochrane systematic review 765
705 W. Oral versus intravenous rehydration for treating dehydration with meta-analysis and mixed treatment comparison in a 766
706 due to gastroenteritis in children. Cochrane Database Syst Rev. Bayesian framework. BMJ Open. 2012;2:e000622. 767
707 2006;19:CD004390. 40. Freedman SB, Tung D, Cho d, Rumantir M, Chan KJ. Time-series 768
708 20. Binder HJ, Brown I, Ramakrishna BS, Young GP. Oral rehydration analysis of ondansetron use in pediatric gastroenteritis. J Pedi- 769
709 therapy in the second decade of the twenty-first century. Curr atr Gastroenterol Nutr. 2012;54:381---6. 770
710 Gastroenterol Rep. 2014;16:376. 41. Dupont C, Vernisse B. Anti-diarrheal effects of diosmectite in 771
711 21. Duggan C, Fontaine O, Pierce NF, et al. Scientific rationale for a the treatment of acute diarrhea in children: a review. Paediatr 772
712 change in the composition of oral rehydration solution. JAMA. Drugs. 2009;11:89---99. 773
713 2004;291:2628---31. 42. NICE. National Institute for Health and Care Excellence. 774
714 22. Rouhani S, Meloney L, Ahn R, Nelson BD, Burke TF. Alterna- ESNM12: Acute diarrhoea in children: racecadotril as an adjunct 775
715 tive rehydration methods: a systematic review and lessons for to oral rehydration. Last updated 12 March 2013. Available 776
716 resource-limited care. Pediatrics. 2011;127:e748---57. from: https://www.nice.org.uk [cited 21.04.15]. 777
717 23. Freedman SB, Keating LE, Rumatir M, Schuh S. Health care 43. WHO/UNICEF. Joint statement: clinical management of acute 778
718 provider and caregiver preferences regarding nasogastric and diarrhoea. New York: WHO/UNICEF; 2004. 779
719 intravenous rehydration. Pediatrics. 2012;130:e1504---11. 44. Lamberti LM, Walker CL, Jian W, Black RE. oral zinc 780
720 24. Goldman R. Palatability of oral rehydration solutions varies but supplementation for the treatment of acute diarrhea in 781
721 does not impact quantity consumed. J Pediatr. 2011;158:168---9. children: a systematic review and meta-analysis. Nutrients. 782
722 25. Gregorio GV, Gonzales ML, Dans LF, Martinez EG. Amylase- 2013;5:4715---40. 783
723 resistant starch as adjunct to oral rehydration therapy 45. Preids GA, Hill C, Guerrante RL, Ramakrishna BS, Tannock G, 784
724 in children with diarrhea. Cochrane Database Syst Rev. Versalovic J. Probiotics, enteric and diarrheal diseases, and 785
725 2009;15:CD006519. global health. Gastroenterology. 2011;140:8---14. 786
726 26. Neville KA, Verge CF, Rosenberg AR, O’Meara MW, Walker
JL. Isotonic is better than hypotonic saline for intravenous
JPED 295 1---8
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Booking Report 11-23-2021Document3 pagesBooking Report 11-23-2021WCTV Digital TeamNo ratings yet
- Commercial Paper: Presented by Dharani Dharan.m Vijaya Kumar S.BDocument16 pagesCommercial Paper: Presented by Dharani Dharan.m Vijaya Kumar S.Budaya37No ratings yet
- Vedic Astrology LagnaDocument24 pagesVedic Astrology LagnamarketsniperteluguNo ratings yet
- 100 S Oem S: 102R Low Flow PumpheadDocument2 pages100 S Oem S: 102R Low Flow PumpheadtechniqueNo ratings yet
- DB Pyranometer SMP10 en 20151208Document2 pagesDB Pyranometer SMP10 en 20151208matefucskoNo ratings yet
- Bahasa Inggris Verb PDFDocument16 pagesBahasa Inggris Verb PDFeka ginanjar saputraNo ratings yet
- Sentences, Fragments, & Run-OnsDocument6 pagesSentences, Fragments, & Run-Onslu liu100% (1)
- The Paper Makers of Snodland C 1740-1854Document28 pagesThe Paper Makers of Snodland C 1740-1854Andrew S. WardNo ratings yet
- Digipay GuruDocument13 pagesDigipay GuruPeterhill100% (1)
- Dyna SandDocument8 pagesDyna SandRuchi GuptaNo ratings yet
- 3GPP TS 22.278Document51 pages3GPP TS 22.278bhushan7408No ratings yet
- Procedure: Administering An Intradermal Injection For Skin TestDocument3 pagesProcedure: Administering An Intradermal Injection For Skin TestSofia AmistosoNo ratings yet
- Bou Stead 2012Document16 pagesBou Stead 2012huynhvanchauNo ratings yet
- Talent Acquisition 2008 - Survey and Analysis of The Changing Recruiting Landscape PDFDocument20 pagesTalent Acquisition 2008 - Survey and Analysis of The Changing Recruiting Landscape PDFVaishnavi SivaNo ratings yet
- Group 1 Dorb001 Bsce3aDocument16 pagesGroup 1 Dorb001 Bsce3aJan TheGamerNo ratings yet
- JLTR, 02Document8 pagesJLTR, 02Junalyn Villegas FerbesNo ratings yet
- Gerund NounDocument15 pagesGerund NounNanda PutriNo ratings yet
- Dwadasa Nama of KartaveeryaDocument4 pagesDwadasa Nama of KartaveeryaVijaya BhaskarNo ratings yet
- VedicReport6 10 20179 56 16PMDocument47 pagesVedicReport6 10 20179 56 16PManandpaithankar13No ratings yet
- Bunker & FW Supply ChecklistDocument3 pagesBunker & FW Supply ChecklistSampetua StmrgNo ratings yet
- Full Download Elementary Statistics A Step by Step Approach Bluman 9Th Edition Solutions Manual PDFDocument49 pagesFull Download Elementary Statistics A Step by Step Approach Bluman 9Th Edition Solutions Manual PDFsteven.engelke246100% (21)
- Creativity in Engineering Design ProcessDocument12 pagesCreativity in Engineering Design ProcessNurhuda HayatiNo ratings yet
- Commonly Asked Short QuestionsDocument4 pagesCommonly Asked Short QuestionsShubham JainNo ratings yet
- Hardness TestDocument8 pagesHardness TestlvasuthavanNo ratings yet
- Expt. 8 Salivary DigestionDocument25 pagesExpt. 8 Salivary DigestionLESLIE JANE BALUYOS JALANo ratings yet
- Randomized Controlled Trial On The Performance of Direct and in - 2021 - DentalDocument10 pagesRandomized Controlled Trial On The Performance of Direct and in - 2021 - Dentalnintendo anjayNo ratings yet
- Part-4-General English Set 3Document17 pagesPart-4-General English Set 3Yashwant SinghNo ratings yet
- Lesson Plans WK 26Document7 pagesLesson Plans WK 26api-280840865No ratings yet
- (20635303 - Journal of Behavioral Addictions) Fear of Missing Out (FoMO) and Internet Use - A Comprehensive Systematic Review and Meta-AnalysisDocument22 pages(20635303 - Journal of Behavioral Addictions) Fear of Missing Out (FoMO) and Internet Use - A Comprehensive Systematic Review and Meta-AnalysisNeeraj raiNo ratings yet
- Tổng Hợp Đề Thi Và Bài Mẫu IELTS Writing Năm 2021Document38 pagesTổng Hợp Đề Thi Và Bài Mẫu IELTS Writing Năm 2021Đoan Trang Trần NữNo ratings yet