Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
28 viewsCentral Nervous System: Zalak Patel, MBBS
Central Nervous System: Zalak Patel, MBBS
Uploaded by
Minaz PatelThis document summarizes key aspects of the central nervous system including cerebral blood flow, cerebral perfusion pressure, the effects of temperature, glucose, carbon dioxide, anesthetic agents, and neuromonitoring techniques like EEG. Specifically, it notes that cerebral blood flow is tightly regulated to maintain oxygen and glucose delivery to the brain and interruptions can cause rapid damage or death. Factors like carbon dioxide, temperature, glucose levels, and anesthetic agents can all impact cerebral blood flow and metabolism. EEG is commonly used for neuromonitoring to detect changes caused by these physiological variables.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Neurophysiology and AnaesthesiaDocument54 pagesNeurophysiology and AnaesthesiaBernard Panggabean100% (1)
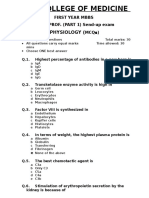
- 1st Year Sendup MCQsDocument8 pages1st Year Sendup MCQsTARIQNo ratings yet
- Physiology Lab Report 2 - Luis Anthony Jayanata - 1906421814Document18 pagesPhysiology Lab Report 2 - Luis Anthony Jayanata - 1906421814luis11256No ratings yet
- Anaesthesia For Liver TransplantationDocument54 pagesAnaesthesia For Liver TransplantationPeeyoosh RaiNo ratings yet
- Kenneth Lowther Resume 2015Document2 pagesKenneth Lowther Resume 2015api-286367605No ratings yet
- Physical Assessment and GordonsDocument14 pagesPhysical Assessment and GordonsRubelyn Joy LazarteNo ratings yet
- Effect of Anesthetic AgentsDocument26 pagesEffect of Anesthetic AgentsefrikoNo ratings yet
- Cerebral Blood Flow: ICP and The Monro-Kellie DoctrineDocument4 pagesCerebral Blood Flow: ICP and The Monro-Kellie DoctrineTonyNo ratings yet
- Intracranial Pressure: Dr. Akhmad Imron, Spbs Dept. of NeurosurgeryDocument26 pagesIntracranial Pressure: Dr. Akhmad Imron, Spbs Dept. of Neurosurgeryandisti2323No ratings yet
- Cerebral CirculationDocument16 pagesCerebral Circulationvarrakesh100% (1)
- NMB MyDocument91 pagesNMB MyGirish Bk B KNo ratings yet
- Sarcoplasmic Reticulum 3Document6 pagesSarcoplasmic Reticulum 3Syaidah umiNo ratings yet
- Spinal and Epidural Anesthesia: Jedarlyn G. Erardo, RPH, MDDocument101 pagesSpinal and Epidural Anesthesia: Jedarlyn G. Erardo, RPH, MDjedarlynNo ratings yet
- 24 Cerebral Blood FlowDocument31 pages24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Potassium ParticipantsDocument21 pagesPotassium ParticipantsSkylar IvyNo ratings yet
- Pathophysiology of ShockDocument56 pagesPathophysiology of ShockDr. Haricharan ANo ratings yet
- Coronary Artery DiseaseDocument33 pagesCoronary Artery DiseaseAlma Rifa'Ana LiskaNo ratings yet
- 8 Coronary CirculationDocument31 pages8 Coronary CirculationAhmed AliNo ratings yet
- Cerebral Protection & NeuroresuscitationDocument19 pagesCerebral Protection & NeuroresuscitationImad El SadekNo ratings yet
- Biomarkers For Myocardial Infarction, CVS BlockDocument13 pagesBiomarkers For Myocardial Infarction, CVS BlockGlucose DRglucoseNo ratings yet
- Evaluation and Management of Elevated Intracranial Pressure in AdultsDocument28 pagesEvaluation and Management of Elevated Intracranial Pressure in AdultssandykumalaNo ratings yet
- Diagnostic Cardiac EnzymesDocument27 pagesDiagnostic Cardiac Enzymesد.لطفي دحمانNo ratings yet
- Disorder of Potassium MetabolismDocument28 pagesDisorder of Potassium MetabolismSaif AliNo ratings yet
- Approach To The Patient in Shock: by James Holencik, DODocument52 pagesApproach To The Patient in Shock: by James Holencik, DOLydia MamurNo ratings yet
- Drugs Used For Treatment Stable Angina PectorisDocument29 pagesDrugs Used For Treatment Stable Angina PectorisAditya Andra PerdanaNo ratings yet
- Νευρολογία σύνολο απαντήσεωνDocument38 pagesΝευρολογία σύνολο απαντήσεωνCheng Kuao HengNo ratings yet
- Classification of Nerve FiberDocument21 pagesClassification of Nerve FiberNayab IftikharNo ratings yet
- Med SurDocument107 pagesMed Surapi-239934742No ratings yet
- Intravenous Fluid Therapy For 2nd Year ConceptDocument83 pagesIntravenous Fluid Therapy For 2nd Year ConceptMay Chelle ErazoNo ratings yet
- Anaesthetic Challenges and Management of Myelomeningocele RepairDocument6 pagesAnaesthetic Challenges and Management of Myelomeningocele RepairprastiaNo ratings yet
- Cardiac Action PotentialDocument41 pagesCardiac Action PotentialRadijska Postaja KoprivnicaNo ratings yet
- Hemostasis Physiology PDFDocument27 pagesHemostasis Physiology PDFIqmal CimolNo ratings yet
- Traumatic Brain InjuryDocument40 pagesTraumatic Brain InjuryRed DevilNo ratings yet
- Describe The Factors Affecting Cardiac OutputDocument6 pagesDescribe The Factors Affecting Cardiac OutputSis SukarnoNo ratings yet
- A Powerful Tool To Objectively Monitor Your Patients Ventilatory StatusDocument36 pagesA Powerful Tool To Objectively Monitor Your Patients Ventilatory StatusBeth Strom-Sturm100% (1)
- The Complications of DiabetesDocument1 pageThe Complications of DiabetesMiguel Cuevas DolotNo ratings yet
- Regulation of Circulation SystemDocument20 pagesRegulation of Circulation SystemwiwiNo ratings yet
- RhabdomyolysisDocument2 pagesRhabdomyolysisintrovoyz041No ratings yet
- Patient Controlled AnalgesiaDocument35 pagesPatient Controlled AnalgesiamochkurniawanNo ratings yet
- Muscle Relaxants and Neuromuscular Blocking AgentsDocument45 pagesMuscle Relaxants and Neuromuscular Blocking AgentsSomesh SharmaNo ratings yet
- Hyperosmolar Non Ketotic ComaDocument23 pagesHyperosmolar Non Ketotic Comaprakash gunaNo ratings yet
- Spinal & Epidural AnaesthesiaDocument10 pagesSpinal & Epidural AnaesthesiarafiaNo ratings yet
- The Physiology of A Frog Heart With The Effects of Temperature, Neurotransmitters, and Electrical IsolationDocument17 pagesThe Physiology of A Frog Heart With The Effects of Temperature, Neurotransmitters, and Electrical IsolationAbir Hasan ShuvoNo ratings yet
- TCD ProtokolDocument35 pagesTCD Protokolscepan100% (1)
- Physiology CH 15 - Vascular Distensibility and FunctionDocument31 pagesPhysiology CH 15 - Vascular Distensibility and FunctionDaniel AdamsNo ratings yet
- Anesthesia CHD Non Cardiac SurgeryDocument97 pagesAnesthesia CHD Non Cardiac SurgeryDon DavidNo ratings yet
- Blood Pressure and Heart PulseDocument7 pagesBlood Pressure and Heart PulseHuda Behrooz0% (1)
- Pre-Operative Assessment of Cardiac Patients in Non Cardiac SurgeryDocument36 pagesPre-Operative Assessment of Cardiac Patients in Non Cardiac SurgeryKush SurejaNo ratings yet
- Coronary Circulation: Dr. Syma RizwanDocument34 pagesCoronary Circulation: Dr. Syma RizwanAttiqaQureshiNo ratings yet
- Intracranial Pressure: Current Perspectives On Physiology and MonitoringDocument11 pagesIntracranial Pressure: Current Perspectives On Physiology and MonitoringWander ValentimNo ratings yet
- Sleep Apnoea - Prof - DR K.K.PDocument44 pagesSleep Apnoea - Prof - DR K.K.PjialeongNo ratings yet
- 5675932Document89 pages5675932JuhiJahan AmanullahNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- 10 Kidneys 2017 PDFDocument42 pages10 Kidneys 2017 PDFSajid AhmadNo ratings yet
- Circulatory ShockDocument16 pagesCirculatory ShockAndriNo ratings yet
- Arrhythmia 2Document31 pagesArrhythmia 2rittvedNo ratings yet
- Algorithms of Care (Myocardial Infarction)Document3 pagesAlgorithms of Care (Myocardial Infarction)Julius Delos SantosNo ratings yet
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationDocument28 pagesCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- R.N. Kapoor Memorial Homoeopathic Hospital & Medical College, INDOREDocument12 pagesR.N. Kapoor Memorial Homoeopathic Hospital & Medical College, INDOREvinay patidar100% (1)
- Pharmacology of Angina Pectoris: Prepared by Bashir Dhuh AliDocument11 pagesPharmacology of Angina Pectoris: Prepared by Bashir Dhuh AliZakarie Abdullahi HusseinNo ratings yet
- Point of View Heparin ResistanceDocument20 pagesPoint of View Heparin ResistanceSameer Goyal100% (1)
- Cerebral PhysiologyDocument27 pagesCerebral PhysiologyArmaanjeet SinghNo ratings yet
- IndianJAnaesth Adult 2017Document14 pagesIndianJAnaesth Adult 2017Minaz PatelNo ratings yet
- Airway Workshop FlyerDocument1 pageAirway Workshop FlyerMinaz PatelNo ratings yet
- Future of Pain & Palliative Medicine As A Career: 11 Master ClassDocument1 pageFuture of Pain & Palliative Medicine As A Career: 11 Master ClassMinaz PatelNo ratings yet
- Tracts of Spinal Cord: Dr. Fathima TasneemDocument31 pagesTracts of Spinal Cord: Dr. Fathima TasneemMinaz PatelNo ratings yet
- Fellowship of Neurocritical Care (FNCC) : Need For The CourseDocument12 pagesFellowship of Neurocritical Care (FNCC) : Need For The CourseMinaz PatelNo ratings yet
- QP Code:103101 Reg. No.: PG Degree Supplementary Examinations in Anaesthesiology (MD) October 2019lDocument1 pageQP Code:103101 Reg. No.: PG Degree Supplementary Examinations in Anaesthesiology (MD) October 2019lMinaz PatelNo ratings yet
- 159 Anaesthesia For Children With Obstructive Sleep ApnoeaDocument6 pages159 Anaesthesia For Children With Obstructive Sleep ApnoeaMinaz PatelNo ratings yet
- 311 1376 1 PB PDFDocument3 pages311 1376 1 PB PDFMinaz PatelNo ratings yet
- Solid Renal Mass: Hisham Alkhatib, M.DDocument49 pagesSolid Renal Mass: Hisham Alkhatib, M.DMinaz PatelNo ratings yet
- Sponsored Seat Matrix 5-6-20Document8 pagesSponsored Seat Matrix 5-6-20Minaz PatelNo ratings yet
- Takayasu'S Arteritis: Dr. AishwaryaDocument56 pagesTakayasu'S Arteritis: Dr. AishwaryaMinaz PatelNo ratings yet
- ASA Physical Status Classification System 2019 PDFDocument2 pagesASA Physical Status Classification System 2019 PDFMinaz PatelNo ratings yet
- 1324autonomicdysfunc 180617164555Document83 pages1324autonomicdysfunc 180617164555Minaz PatelNo ratings yet
- The Grey Matter: Something in The AirDocument28 pagesThe Grey Matter: Something in The AirMinaz PatelNo ratings yet
- University of Pune: Examination Circular No.115 of 2010Document3 pagesUniversity of Pune: Examination Circular No.115 of 2010Minaz PatelNo ratings yet
- 2.C StatisticsDocument5 pages2.C StatisticsMinaz PatelNo ratings yet
- University of Pune: Price: Rs. 30Document2 pagesUniversity of Pune: Price: Rs. 30Minaz PatelNo ratings yet
- Jama Abbasi 2020 MN 200023Document3 pagesJama Abbasi 2020 MN 200023Minaz PatelNo ratings yet
- Indian Medical Association: Dr. Avinash Bhondwe Dr. Pankaj Bandarkar President Hon. State SecretaryDocument1 pageIndian Medical Association: Dr. Avinash Bhondwe Dr. Pankaj Bandarkar President Hon. State SecretaryMinaz PatelNo ratings yet
- Shared RX Modules For FinalsDocument11 pagesShared RX Modules For FinalsOdyNo ratings yet
- Beauty Protocol With SCENAR DevicesDocument35 pagesBeauty Protocol With SCENAR Devicesstoic100% (2)
- Lowgimeals Food Index PDFDocument4 pagesLowgimeals Food Index PDFEmily JamesNo ratings yet
- Lidocaine and TetracaineDocument13 pagesLidocaine and TetracaineRamona MateiNo ratings yet
- Interview Method in AssessmentDocument13 pagesInterview Method in AssessmentAnanya100% (2)
- Business Model For A Water District Septage Management ProgramDocument61 pagesBusiness Model For A Water District Septage Management ProgramHammurabi Bugtai100% (1)
- Rekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFDocument12 pagesRekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFMedikaChanNo ratings yet
- Making CreamDocument9 pagesMaking CreamJai MurugeshNo ratings yet
- Policies and Procedure For Ensuring Quality of Sputum Microscopy ResultsDocument2 pagesPolicies and Procedure For Ensuring Quality of Sputum Microscopy ResultsReinald Raven GuerreroNo ratings yet
- Step 3 Surgery Uworld NotesDocument11 pagesStep 3 Surgery Uworld Notesaleks patralskaNo ratings yet
- Arie History of SurgeryDocument20 pagesArie History of SurgeryArie RezaNo ratings yet
- Lec 1-Week 1 - (Wastewater Collection System)Document32 pagesLec 1-Week 1 - (Wastewater Collection System)jahanzaibchNo ratings yet
- Chem Soft Copy FinalDocument17 pagesChem Soft Copy FinalArvin KumarNo ratings yet
- Interpositional Arthroplasty For Hallux Rigidus ADocument1 pageInterpositional Arthroplasty For Hallux Rigidus AGeorge FernandoNo ratings yet
- 20 Health Benefits of CoffeeDocument4 pages20 Health Benefits of CoffeeMunzir HassanNo ratings yet
- Nursing Care PlanDocument16 pagesNursing Care PlanJennifer Post100% (3)
- Karl Storz VAAFTDocument35 pagesKarl Storz VAAFTSalam KamilNo ratings yet
- Module 1: Perioperative Nursing/Preoperative Clinical Instructor: Rowena L. Madrid, R.N. 1.A Terminology Overview of The LessonDocument15 pagesModule 1: Perioperative Nursing/Preoperative Clinical Instructor: Rowena L. Madrid, R.N. 1.A Terminology Overview of The LessonCheryl Moana Marie Anova EnriquezNo ratings yet
- 09-Pediatrics in Review, September2009 PDFDocument71 pages09-Pediatrics in Review, September2009 PDFMobin Ur Rehman KhanNo ratings yet
- Case Study Sa Surgical WardDocument8 pagesCase Study Sa Surgical WardAiza ToledanaNo ratings yet
- Hypertensive Urgency EmergencyDocument5 pagesHypertensive Urgency Emergencydamondouglas100% (3)
- Syringe Pump TPPDocument28 pagesSyringe Pump TPPيحيى القهاليNo ratings yet
- AMCT 5203 Lesson 3 (21june2015)Document16 pagesAMCT 5203 Lesson 3 (21june2015)MAAbuBakarNo ratings yet
- Papp 2015 PFTDocument30 pagesPapp 2015 PFTWivina Bancoro100% (1)
- Cosmetic Surgery PpsDocument27 pagesCosmetic Surgery Ppsyamos2No ratings yet
- Differential Diagnosis of Tongue LesionsDocument12 pagesDifferential Diagnosis of Tongue LesionsKartikakhairaniNo ratings yet
- Ielts 1Document69 pagesIelts 1Ganga SharmaNo ratings yet
Central Nervous System: Zalak Patel, MBBS
Central Nervous System: Zalak Patel, MBBS
Uploaded by
Minaz Patel0 ratings0% found this document useful (0 votes)
28 views25 pagesThis document summarizes key aspects of the central nervous system including cerebral blood flow, cerebral perfusion pressure, the effects of temperature, glucose, carbon dioxide, anesthetic agents, and neuromonitoring techniques like EEG. Specifically, it notes that cerebral blood flow is tightly regulated to maintain oxygen and glucose delivery to the brain and interruptions can cause rapid damage or death. Factors like carbon dioxide, temperature, glucose levels, and anesthetic agents can all impact cerebral blood flow and metabolism. EEG is commonly used for neuromonitoring to detect changes caused by these physiological variables.
Original Description:
abc
Original Title
patel-cns
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes key aspects of the central nervous system including cerebral blood flow, cerebral perfusion pressure, the effects of temperature, glucose, carbon dioxide, anesthetic agents, and neuromonitoring techniques like EEG. Specifically, it notes that cerebral blood flow is tightly regulated to maintain oxygen and glucose delivery to the brain and interruptions can cause rapid damage or death. Factors like carbon dioxide, temperature, glucose levels, and anesthetic agents can all impact cerebral blood flow and metabolism. EEG is commonly used for neuromonitoring to detect changes caused by these physiological variables.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
28 views25 pagesCentral Nervous System: Zalak Patel, MBBS
Central Nervous System: Zalak Patel, MBBS
Uploaded by
Minaz PatelThis document summarizes key aspects of the central nervous system including cerebral blood flow, cerebral perfusion pressure, the effects of temperature, glucose, carbon dioxide, anesthetic agents, and neuromonitoring techniques like EEG. Specifically, it notes that cerebral blood flow is tightly regulated to maintain oxygen and glucose delivery to the brain and interruptions can cause rapid damage or death. Factors like carbon dioxide, temperature, glucose levels, and anesthetic agents can all impact cerebral blood flow and metabolism. EEG is commonly used for neuromonitoring to detect changes caused by these physiological variables.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 25
Central Nervous System
Zalak Patel, MBBS
Anesthesiology and Perioperative Medicine
Medical College of Georgia
Augusta University
2016
Cerebral Blood Flow
• Cerebral blood flow is 20% of the cardiac output and
averages 50 mL/100 g/min (gray matter 80%, white
matter 10-20%)
• Brain is normally responsible for 20% of total body O2
consumption CMRO2 = 3-3.5 m/100 g/min (50 mL/min)
in adults
• Interruption of CBF causes unconsciousness in 10 sec.
If blood flow is not restored within 3-8 min, irreversible
damage will occur
Cerebral Perfusion Pressure
• CPP = (MAP – RAP or ICP) = 100 mmHg
• Autoregulation serves to achieve constant CBF independent
of MAP over a range of 50-150 mmHg
• CBF < 20-25 mL/100 g/min (CPP <50 mmHg) –cerebral
impairment, as evidenced by slowing on EEG
• CBF 15-20 mL/100 g/min (25-40 mmHg) – flat (isoelectric)
EEG
• CBF <10 mL/100 g/min (sustained CPP <25 mmHg) –
irreversible brain damage
• Normal ICP = 8-12 mmHg; >30 mmHg will compromise CPP
• CSF production = 21 mL/hr (500 mL/day), yet total volume of
CSF = 150 mL
Effect of Temperature, Glucose
• Temperature increases CBF and CMR at 7%/°C
• At 20 °C, EEG becomes isoelectric, but further
decrease continues to reduce CMR throughout brain
• Acute sustained hypoglycemia is equally as
devastating as hypoxia
• Paradoxically, hyperglycemia can exacerbate global
hypoxic brain injury by accelerating cerebral acidosis
and cellular injury
Carbon Dioxide
• Most potent regulator of CBF
• Hyperventilation remains one of the fastest therapeutic
maneuvers to decrease cerebral blood volume (CBV)
• At PaCO2 of 25-65 mmHg, for each 1 mmHg increase
of CO2, there is an increase of 1-2 mL/100 g/min of
CBF (3% of baseline change)
Carbon Dioxide
• PaO2 less than 50 mmHg will increase the CBF
profoundly
• At PaO2 >300 mmHg, vasoconstriction occurs
• Optimal O2 delivery appears to occur at hematocrit of
30-34% range
• Anemia increases CBF via high CO, CPP, and low
viscosity, as well as induced cerebral vasodilation
Anesthetics and Cerebral Function
• Suppression of CMR (exceptions: ketamine and
nitrous oxide [N2O])
• Increasing plasma concentrations of Inhaled
anesthetics (sevoflurane, desflurane, isoflurane), IV
agents (barbiturates, propofol, etomidate) cause
progressive suppression of EEG activity and reduction
in CMR of O2 (CMRO2)
• Maximum reduction (50-60%) occurs with isoelectric
EEG. However EEG suppression produced by the
anesthetic is influenced by agent used
Anesthetics and Cerebral Function
• Barbiturates – at isoelectric EEG there is a uniform
depression in CBF and CMR throughout the brain
• With isoflurane, the relative reduction in CBF and CMR are
greater in the neocortex than in other portions of cerebrum
• All inhaled drugs including N2O have intrinsic cerebral
vasodilatory activity due to direct effect on vascular smooth
muscle
• Net effect on CBF is a balance between augmentation of
CBF due to vasodilatory effect and reduction in CBF due to
suppression of CMR
Effect of Inhaled Anesthetic Drugs
on CBF
• At 0.5 MAC, CMR suppression predominates and CBF
decreases compared to awake state
• At 1 MAC, CBF remains unchanged; suppression and
vasodilatory effects are balanced
• At >1 MAC, vasodilatory effect predominates and CBF
increases significantly even though CMR is suppressed
largely as well (uncoupling of flow and metabolism)
Inhalation Agents and CMR
• All of the volatile agents depress CMR to varying
degrees in a nonlinear fashion
• For most agents, after an isoelectric EEG, no further
decrease in CMR occurs
• Isoflurane abolishes EEG activity at clinically tolerated
doses (around 2 MAC); sevoflurane and desflurane are
similar to isoflurane
Inhalation Agents and CMR
• Critical CBF – blood flow at which EEG evidence of
cerebral ischemia develops – is significantly lower with
isoflurane than halothane (10 mL/100 g/min vs 18-20
mL/100 g/min)
Nitrous Oxide
• Increase in CBF, CMR (partly due to increased
sympathetic activity) and ICP
• N2O administered alone – substantial increase in CBF
and ICP can occur
• N2O + IV anesthetics – vasodilating effect is attenuated
or abolished
• N2O + volatile agents – moderate increase in CBF
• CO2 responsiveness is preserved during N2O
administration
Xenon
• Administration of 1 MAC of xenon – decrease in CBF
(15% reduction in cortex and 35% in cerebellum)
• Parallel reduction in CMR
• Cerebral autoregulation and CO2 reactivity are
preserved
• Xenon expands air-containing spaces, however,
magnitude of expansion is considerably less than with
N 2O
Intravenous Agents
• Barbiturate – decreases CMR and CBF until isoelectric
EEG appears (= maximum of 50-60% reduction in CMR at
this point) and additional doses of barbituate do not further
reduce CMR
• Propofol – similar to barbiturate; reduces CBF more than
reduction in CMRO2
• Etomidate – similar effect; CMR suppression in forebrain
• Methohexital – small doses may activate seizure; large
doses have anticonvulsant properties
• Benzodiazepine – reduces CMR and CBF (not as
pronounced as with barbiturate). Amount of reduction is
probably intermediate between narcotics and barbiturates
Intravenous Agents
• Flumazenil – reverses the CMR, CBF, and ICP lowering
effect of midazolam; use cautiously with high ICP
• Opioids – may cause minor reduction in or no effect on
CBF and CMR
• Morphine – may release significant amount of histamine –
can cause increase in CBV, CBF (depending on blood
pressure effect) because histamine is a cerebral
vasodilator
• Dexmedetomidine – appears to preserve flow-metabolism
coupling in healthy volunteers
Intravenous Agents
• Ketamine – increases CBF and CMR. However, other
anesthetic drugs (midazolam, propofol, isoflurane) appear
to blunt the increase in ICP or CBF associated with
ketamine
• Lidocaine – a bolus dose (1.5 mg/kg) helps to prevent and
treat increase in ICP with endotracheal suctioning
– Larger doses (>2 mg/kg) can cause seizures; therefore,
restrict dose
– Lidocaine produces dose-related reduction in CMRO2
Blood Brain Barrier
• Impedes flow of ions such as K, Ca, Mg, Na; polar
substances such as glucose, amino acids, mannitol;
and macromolecules like proteins
• Uses active or passive (facilitated diffusion-
concentration dependent) transport
• Lipid-soluble substances, i.e., CO2, O2, volatile
anesthetics and water pass rapidly
Pathway for CSF Circulation
Lateral ventricles
intraventricular foramen of Monro
Third ventricle
aqueduct of Sylvius
Fourth ventricle (foramen of Luschka)
and lateral aperture (foramen of Magendie)
Cerebral medullary cisterns (cisterna magna
Determinants of ICP
• CSF primarily formed by transport of Na, Cl, HCO3 +
osmotic movement of water
• Furosemide (inhibits Na/Cl transport), acetazolamide
(reduces HCO3 by inhibiting carbonic anhydrase)
reduce CSF formation
• CSF absorption – Arachnoid villi venous system
(one-way flow)
• Brain is enclosed in cranium, a bony structure which
has a fixed volume. Therefore, increase in volume of
any of its contents will increase ICP
Changes in PaCO2, CBF, and CSF pH with prolonged
hyperventilation
• Decreased PaCO2 and systemic alkalosis persist for the
duration of hyperventilation
• pH of the brain and CBF return to normal over 8-12 hr
• Vessel caliber returns to baseline
Neuromonitoring by EEG
Neuromonitoring by EEG
Neuromonitoring by EEG
Neuromonitoring by EEG
Other physiologic variables can alter SSEPs
• Hypothermia – increases latency
• Hypotension – MAP <40 decreases amplitude
• Hypoxia – decreases amplitude
• Hypocarbia – end-tidal CO2 <25 increases latency
• Isovolemic hemodilution – Hct <15% increases latency
When body temperature falls to <35 °C, there is progressive
slowly of EEG activity – complete electrical silence at 15-20°C
You might also like
- Neurophysiology and AnaesthesiaDocument54 pagesNeurophysiology and AnaesthesiaBernard Panggabean100% (1)
- 1st Year Sendup MCQsDocument8 pages1st Year Sendup MCQsTARIQNo ratings yet
- Physiology Lab Report 2 - Luis Anthony Jayanata - 1906421814Document18 pagesPhysiology Lab Report 2 - Luis Anthony Jayanata - 1906421814luis11256No ratings yet
- Anaesthesia For Liver TransplantationDocument54 pagesAnaesthesia For Liver TransplantationPeeyoosh RaiNo ratings yet
- Kenneth Lowther Resume 2015Document2 pagesKenneth Lowther Resume 2015api-286367605No ratings yet
- Physical Assessment and GordonsDocument14 pagesPhysical Assessment and GordonsRubelyn Joy LazarteNo ratings yet
- Effect of Anesthetic AgentsDocument26 pagesEffect of Anesthetic AgentsefrikoNo ratings yet
- Cerebral Blood Flow: ICP and The Monro-Kellie DoctrineDocument4 pagesCerebral Blood Flow: ICP and The Monro-Kellie DoctrineTonyNo ratings yet
- Intracranial Pressure: Dr. Akhmad Imron, Spbs Dept. of NeurosurgeryDocument26 pagesIntracranial Pressure: Dr. Akhmad Imron, Spbs Dept. of Neurosurgeryandisti2323No ratings yet
- Cerebral CirculationDocument16 pagesCerebral Circulationvarrakesh100% (1)
- NMB MyDocument91 pagesNMB MyGirish Bk B KNo ratings yet
- Sarcoplasmic Reticulum 3Document6 pagesSarcoplasmic Reticulum 3Syaidah umiNo ratings yet
- Spinal and Epidural Anesthesia: Jedarlyn G. Erardo, RPH, MDDocument101 pagesSpinal and Epidural Anesthesia: Jedarlyn G. Erardo, RPH, MDjedarlynNo ratings yet
- 24 Cerebral Blood FlowDocument31 pages24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Potassium ParticipantsDocument21 pagesPotassium ParticipantsSkylar IvyNo ratings yet
- Pathophysiology of ShockDocument56 pagesPathophysiology of ShockDr. Haricharan ANo ratings yet
- Coronary Artery DiseaseDocument33 pagesCoronary Artery DiseaseAlma Rifa'Ana LiskaNo ratings yet
- 8 Coronary CirculationDocument31 pages8 Coronary CirculationAhmed AliNo ratings yet
- Cerebral Protection & NeuroresuscitationDocument19 pagesCerebral Protection & NeuroresuscitationImad El SadekNo ratings yet
- Biomarkers For Myocardial Infarction, CVS BlockDocument13 pagesBiomarkers For Myocardial Infarction, CVS BlockGlucose DRglucoseNo ratings yet
- Evaluation and Management of Elevated Intracranial Pressure in AdultsDocument28 pagesEvaluation and Management of Elevated Intracranial Pressure in AdultssandykumalaNo ratings yet
- Diagnostic Cardiac EnzymesDocument27 pagesDiagnostic Cardiac Enzymesد.لطفي دحمانNo ratings yet
- Disorder of Potassium MetabolismDocument28 pagesDisorder of Potassium MetabolismSaif AliNo ratings yet
- Approach To The Patient in Shock: by James Holencik, DODocument52 pagesApproach To The Patient in Shock: by James Holencik, DOLydia MamurNo ratings yet
- Drugs Used For Treatment Stable Angina PectorisDocument29 pagesDrugs Used For Treatment Stable Angina PectorisAditya Andra PerdanaNo ratings yet
- Νευρολογία σύνολο απαντήσεωνDocument38 pagesΝευρολογία σύνολο απαντήσεωνCheng Kuao HengNo ratings yet
- Classification of Nerve FiberDocument21 pagesClassification of Nerve FiberNayab IftikharNo ratings yet
- Med SurDocument107 pagesMed Surapi-239934742No ratings yet
- Intravenous Fluid Therapy For 2nd Year ConceptDocument83 pagesIntravenous Fluid Therapy For 2nd Year ConceptMay Chelle ErazoNo ratings yet
- Anaesthetic Challenges and Management of Myelomeningocele RepairDocument6 pagesAnaesthetic Challenges and Management of Myelomeningocele RepairprastiaNo ratings yet
- Cardiac Action PotentialDocument41 pagesCardiac Action PotentialRadijska Postaja KoprivnicaNo ratings yet
- Hemostasis Physiology PDFDocument27 pagesHemostasis Physiology PDFIqmal CimolNo ratings yet
- Traumatic Brain InjuryDocument40 pagesTraumatic Brain InjuryRed DevilNo ratings yet
- Describe The Factors Affecting Cardiac OutputDocument6 pagesDescribe The Factors Affecting Cardiac OutputSis SukarnoNo ratings yet
- A Powerful Tool To Objectively Monitor Your Patients Ventilatory StatusDocument36 pagesA Powerful Tool To Objectively Monitor Your Patients Ventilatory StatusBeth Strom-Sturm100% (1)
- The Complications of DiabetesDocument1 pageThe Complications of DiabetesMiguel Cuevas DolotNo ratings yet
- Regulation of Circulation SystemDocument20 pagesRegulation of Circulation SystemwiwiNo ratings yet
- RhabdomyolysisDocument2 pagesRhabdomyolysisintrovoyz041No ratings yet
- Patient Controlled AnalgesiaDocument35 pagesPatient Controlled AnalgesiamochkurniawanNo ratings yet
- Muscle Relaxants and Neuromuscular Blocking AgentsDocument45 pagesMuscle Relaxants and Neuromuscular Blocking AgentsSomesh SharmaNo ratings yet
- Hyperosmolar Non Ketotic ComaDocument23 pagesHyperosmolar Non Ketotic Comaprakash gunaNo ratings yet
- Spinal & Epidural AnaesthesiaDocument10 pagesSpinal & Epidural AnaesthesiarafiaNo ratings yet
- The Physiology of A Frog Heart With The Effects of Temperature, Neurotransmitters, and Electrical IsolationDocument17 pagesThe Physiology of A Frog Heart With The Effects of Temperature, Neurotransmitters, and Electrical IsolationAbir Hasan ShuvoNo ratings yet
- TCD ProtokolDocument35 pagesTCD Protokolscepan100% (1)
- Physiology CH 15 - Vascular Distensibility and FunctionDocument31 pagesPhysiology CH 15 - Vascular Distensibility and FunctionDaniel AdamsNo ratings yet
- Anesthesia CHD Non Cardiac SurgeryDocument97 pagesAnesthesia CHD Non Cardiac SurgeryDon DavidNo ratings yet
- Blood Pressure and Heart PulseDocument7 pagesBlood Pressure and Heart PulseHuda Behrooz0% (1)
- Pre-Operative Assessment of Cardiac Patients in Non Cardiac SurgeryDocument36 pagesPre-Operative Assessment of Cardiac Patients in Non Cardiac SurgeryKush SurejaNo ratings yet
- Coronary Circulation: Dr. Syma RizwanDocument34 pagesCoronary Circulation: Dr. Syma RizwanAttiqaQureshiNo ratings yet
- Intracranial Pressure: Current Perspectives On Physiology and MonitoringDocument11 pagesIntracranial Pressure: Current Perspectives On Physiology and MonitoringWander ValentimNo ratings yet
- Sleep Apnoea - Prof - DR K.K.PDocument44 pagesSleep Apnoea - Prof - DR K.K.PjialeongNo ratings yet
- 5675932Document89 pages5675932JuhiJahan AmanullahNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- 10 Kidneys 2017 PDFDocument42 pages10 Kidneys 2017 PDFSajid AhmadNo ratings yet
- Circulatory ShockDocument16 pagesCirculatory ShockAndriNo ratings yet
- Arrhythmia 2Document31 pagesArrhythmia 2rittvedNo ratings yet
- Algorithms of Care (Myocardial Infarction)Document3 pagesAlgorithms of Care (Myocardial Infarction)Julius Delos SantosNo ratings yet
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationDocument28 pagesCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- R.N. Kapoor Memorial Homoeopathic Hospital & Medical College, INDOREDocument12 pagesR.N. Kapoor Memorial Homoeopathic Hospital & Medical College, INDOREvinay patidar100% (1)
- Pharmacology of Angina Pectoris: Prepared by Bashir Dhuh AliDocument11 pagesPharmacology of Angina Pectoris: Prepared by Bashir Dhuh AliZakarie Abdullahi HusseinNo ratings yet
- Point of View Heparin ResistanceDocument20 pagesPoint of View Heparin ResistanceSameer Goyal100% (1)
- Cerebral PhysiologyDocument27 pagesCerebral PhysiologyArmaanjeet SinghNo ratings yet
- IndianJAnaesth Adult 2017Document14 pagesIndianJAnaesth Adult 2017Minaz PatelNo ratings yet
- Airway Workshop FlyerDocument1 pageAirway Workshop FlyerMinaz PatelNo ratings yet
- Future of Pain & Palliative Medicine As A Career: 11 Master ClassDocument1 pageFuture of Pain & Palliative Medicine As A Career: 11 Master ClassMinaz PatelNo ratings yet
- Tracts of Spinal Cord: Dr. Fathima TasneemDocument31 pagesTracts of Spinal Cord: Dr. Fathima TasneemMinaz PatelNo ratings yet
- Fellowship of Neurocritical Care (FNCC) : Need For The CourseDocument12 pagesFellowship of Neurocritical Care (FNCC) : Need For The CourseMinaz PatelNo ratings yet
- QP Code:103101 Reg. No.: PG Degree Supplementary Examinations in Anaesthesiology (MD) October 2019lDocument1 pageQP Code:103101 Reg. No.: PG Degree Supplementary Examinations in Anaesthesiology (MD) October 2019lMinaz PatelNo ratings yet
- 159 Anaesthesia For Children With Obstructive Sleep ApnoeaDocument6 pages159 Anaesthesia For Children With Obstructive Sleep ApnoeaMinaz PatelNo ratings yet
- 311 1376 1 PB PDFDocument3 pages311 1376 1 PB PDFMinaz PatelNo ratings yet
- Solid Renal Mass: Hisham Alkhatib, M.DDocument49 pagesSolid Renal Mass: Hisham Alkhatib, M.DMinaz PatelNo ratings yet
- Sponsored Seat Matrix 5-6-20Document8 pagesSponsored Seat Matrix 5-6-20Minaz PatelNo ratings yet
- Takayasu'S Arteritis: Dr. AishwaryaDocument56 pagesTakayasu'S Arteritis: Dr. AishwaryaMinaz PatelNo ratings yet
- ASA Physical Status Classification System 2019 PDFDocument2 pagesASA Physical Status Classification System 2019 PDFMinaz PatelNo ratings yet
- 1324autonomicdysfunc 180617164555Document83 pages1324autonomicdysfunc 180617164555Minaz PatelNo ratings yet
- The Grey Matter: Something in The AirDocument28 pagesThe Grey Matter: Something in The AirMinaz PatelNo ratings yet
- University of Pune: Examination Circular No.115 of 2010Document3 pagesUniversity of Pune: Examination Circular No.115 of 2010Minaz PatelNo ratings yet
- 2.C StatisticsDocument5 pages2.C StatisticsMinaz PatelNo ratings yet
- University of Pune: Price: Rs. 30Document2 pagesUniversity of Pune: Price: Rs. 30Minaz PatelNo ratings yet
- Jama Abbasi 2020 MN 200023Document3 pagesJama Abbasi 2020 MN 200023Minaz PatelNo ratings yet
- Indian Medical Association: Dr. Avinash Bhondwe Dr. Pankaj Bandarkar President Hon. State SecretaryDocument1 pageIndian Medical Association: Dr. Avinash Bhondwe Dr. Pankaj Bandarkar President Hon. State SecretaryMinaz PatelNo ratings yet
- Shared RX Modules For FinalsDocument11 pagesShared RX Modules For FinalsOdyNo ratings yet
- Beauty Protocol With SCENAR DevicesDocument35 pagesBeauty Protocol With SCENAR Devicesstoic100% (2)
- Lowgimeals Food Index PDFDocument4 pagesLowgimeals Food Index PDFEmily JamesNo ratings yet
- Lidocaine and TetracaineDocument13 pagesLidocaine and TetracaineRamona MateiNo ratings yet
- Interview Method in AssessmentDocument13 pagesInterview Method in AssessmentAnanya100% (2)
- Business Model For A Water District Septage Management ProgramDocument61 pagesBusiness Model For A Water District Septage Management ProgramHammurabi Bugtai100% (1)
- Rekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFDocument12 pagesRekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFMedikaChanNo ratings yet
- Making CreamDocument9 pagesMaking CreamJai MurugeshNo ratings yet
- Policies and Procedure For Ensuring Quality of Sputum Microscopy ResultsDocument2 pagesPolicies and Procedure For Ensuring Quality of Sputum Microscopy ResultsReinald Raven GuerreroNo ratings yet
- Step 3 Surgery Uworld NotesDocument11 pagesStep 3 Surgery Uworld Notesaleks patralskaNo ratings yet
- Arie History of SurgeryDocument20 pagesArie History of SurgeryArie RezaNo ratings yet
- Lec 1-Week 1 - (Wastewater Collection System)Document32 pagesLec 1-Week 1 - (Wastewater Collection System)jahanzaibchNo ratings yet
- Chem Soft Copy FinalDocument17 pagesChem Soft Copy FinalArvin KumarNo ratings yet
- Interpositional Arthroplasty For Hallux Rigidus ADocument1 pageInterpositional Arthroplasty For Hallux Rigidus AGeorge FernandoNo ratings yet
- 20 Health Benefits of CoffeeDocument4 pages20 Health Benefits of CoffeeMunzir HassanNo ratings yet
- Nursing Care PlanDocument16 pagesNursing Care PlanJennifer Post100% (3)
- Karl Storz VAAFTDocument35 pagesKarl Storz VAAFTSalam KamilNo ratings yet
- Module 1: Perioperative Nursing/Preoperative Clinical Instructor: Rowena L. Madrid, R.N. 1.A Terminology Overview of The LessonDocument15 pagesModule 1: Perioperative Nursing/Preoperative Clinical Instructor: Rowena L. Madrid, R.N. 1.A Terminology Overview of The LessonCheryl Moana Marie Anova EnriquezNo ratings yet
- 09-Pediatrics in Review, September2009 PDFDocument71 pages09-Pediatrics in Review, September2009 PDFMobin Ur Rehman KhanNo ratings yet
- Case Study Sa Surgical WardDocument8 pagesCase Study Sa Surgical WardAiza ToledanaNo ratings yet
- Hypertensive Urgency EmergencyDocument5 pagesHypertensive Urgency Emergencydamondouglas100% (3)
- Syringe Pump TPPDocument28 pagesSyringe Pump TPPيحيى القهاليNo ratings yet
- AMCT 5203 Lesson 3 (21june2015)Document16 pagesAMCT 5203 Lesson 3 (21june2015)MAAbuBakarNo ratings yet
- Papp 2015 PFTDocument30 pagesPapp 2015 PFTWivina Bancoro100% (1)
- Cosmetic Surgery PpsDocument27 pagesCosmetic Surgery Ppsyamos2No ratings yet
- Differential Diagnosis of Tongue LesionsDocument12 pagesDifferential Diagnosis of Tongue LesionsKartikakhairaniNo ratings yet
- Ielts 1Document69 pagesIelts 1Ganga SharmaNo ratings yet