Professional Documents
Culture Documents
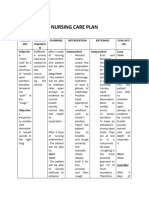
Date Assessment Cues Need Nursing Diagnosis Background Knowledge Objectives Nursing Actions Evaluation
Date Assessment Cues Need Nursing Diagnosis Background Knowledge Objectives Nursing Actions Evaluation
Uploaded by
Joyce Minerva Montero SamsonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Date Assessment Cues Need Nursing Diagnosis Background Knowledge Objectives Nursing Actions Evaluation
Date Assessment Cues Need Nursing Diagnosis Background Knowledge Objectives Nursing Actions Evaluation
Uploaded by
Joyce Minerva Montero SamsonCopyright:
Available Formats
DATE ASSESSMENT NEED NURSING BACKGROUND OBJECTIVES NURSING EVALUATION
CUES DIAGNOSIS KNOWLEDGE ACTIONS
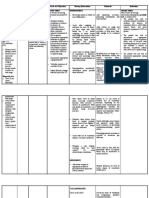
02-22-18
Subjective: Inability to Ineffective At the end of 2 - Independent: Goal met. Patient
“katung sa C provide a Breathing Pattern: days respiratory rate is
herbal ma’am? O home Inspiration and/or community 1. Assess and record 20 within normal
”, as verbalized G environment expiration that does exposure, the respiratory rate and range and was
by one of the N conducive to not provide community will depth. The average able to
purok residents I health adequate ventilation. be able to rate of respiration for demonstrated
during core T maintenance integrate with adults is 10 to 20 lung expansion
group. I or It is considered the community breaths per minute. and reported
V management the state in which the organizers in It is important to take feeling rested.
E and personal rate, depth, timing, starting a plan action when there is
development and rhythm, or on herbal an alteration in the
related to pattern of breathing preparation and pattern of breathing
inadequate is altered. When the gardening: to detect early signs
knowledge of breathing pattern is of respiratory
Objective: preventive ineffective, the body Specifically, the compromise.
measures or is most likely not purok residents
7 out of 48 immediate getting enough will: 2. Observe for
households N management oxygen to the cells. 1. Identify breathing patterns.
surveyed E due to lack of ways to how Unusual patterns
have herbal E herbal or Having a clear impart may imply and
garden D medicinal and effective airway something underlying disease
S garden is vital in patient in herbal or dysfunction.
care. Appropriate preparation
management for and 3. Auscultate
patients with gardening. breaths sounds at
oxygenation 2. Make a plan least every 2 hours.
difficulties are to This to detect
sustain or enhance 3. Participate decreased or
pulmonary in the adventitious breath
ventilation and designed/ sounds.
oxygenation, planned 4. Assess for use of
promote comfort and activities accessory muscle.
ease of breathing. 4. Work of breathing
2. Attend increases greatly as
(NANDA 14th Ed.) lung compliance
decreases.
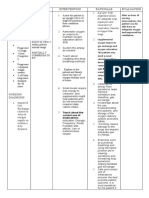
5. Utilize pulse
oximetry to check
oxygen saturation
and pulse rate.
6. Provide
respiratory
medications and
oxygen per doctor’s
orders. This will relax
airway smooth
muscles and cause
bronchodilation to
open air passages.
7. Avail a fan in the
room. Moving air can
decrease feelings of
air hunger.
8. Encourage
frequent rest periods
and teach patient to
pace activity. Extra
activity can worsen
shortness of breath.
You might also like
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee Baluyot100% (2)
- Nursing Care PlanDocument18 pagesNursing Care PlanLayo, Ivy L.No ratings yet
- Nursing Care Plan: Lipa City CollegesDocument13 pagesNursing Care Plan: Lipa City CollegesVincent Maralit MaterialNo ratings yet
- NCP MiniparDocument9 pagesNCP MiniparKyla Avila TorrevillasNo ratings yet
- Nursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceDocument6 pagesNursing Care Plan: Lorma Colleges Con Template Related Learning ExperiencePauline GarciaNo ratings yet
- Assesment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssesment Diagnosis Planning Intervention Rationale EvaluationTrisha Suazo100% (1)
- New Group A - NURSING CARE PLANDocument10 pagesNew Group A - NURSING CARE PLANVelmar De BelenNo ratings yet
- Group 1 Nursing Diagnosis FinalDocument59 pagesGroup 1 Nursing Diagnosis FinalChristian Angelo LeonorNo ratings yet
- Cap Nursing Care PlanDocument6 pagesCap Nursing Care PlanCharlene Grace ReginoNo ratings yet
- Cu 4Document3 pagesCu 4Paul SahagunNo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationElla EvangelistaNo ratings yet
- CuesDocument2 pagesCuesAndrea Love PalomoNo ratings yet
- NCP and Fdar Wk2 Sarscov-19Document4 pagesNCP and Fdar Wk2 Sarscov-19Jamaica Malicdem0% (1)
- Ineffective Breathing Pattern Related To HyperventilationDocument4 pagesIneffective Breathing Pattern Related To HyperventilationVanessa Charlotte LagunayNo ratings yet
- NCPDocument2 pagesNCPKrizia TepootNo ratings yet
- DULNUANDocument2 pagesDULNUANJB tindonganNo ratings yet
- NCPDocument3 pagesNCPDyanne BautistaNo ratings yet
- NCP1223Document3 pagesNCP1223Divine Mercy De JulianNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocument8 pagesNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNo ratings yet
- NCP For CAP TB.Document5 pagesNCP For CAP TB.Cherry Ann BalagotNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationTrisha SuazoNo ratings yet
- Intervensi Ispa Dan Oma FixDocument5 pagesIntervensi Ispa Dan Oma FixRizki ArifNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocument7 pagesNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNo ratings yet
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Nursing Intervention Rationale Evaluationjennelyn losantaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjectivecammel ramos100% (1)
- Myrna CruzDocument3 pagesMyrna CruzChris Opal NamocatcatNo ratings yet
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- PNNCPDocument2 pagesPNNCPJacky BrightNo ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- Nursing Care Plan: Ineffective Breathing Pattern Related ToDocument4 pagesNursing Care Plan: Ineffective Breathing Pattern Related ToFrudz OrjalezaNo ratings yet
- NCP IcuDocument2 pagesNCP Icujennelyn losantaNo ratings yet
- Nursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationCharlynne AraojoNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Goal Planning Interventions Rationale Evaluations Subjective Data: "I HaveDocument9 pagesNursing Care Plan: Assessment Diagnosis Goal Planning Interventions Rationale Evaluations Subjective Data: "I HaveRicha AcharyaNo ratings yet
- Nursing Care Plan: Assessm ENT Nursing Diagnos IS Planning Intervention Rationale Evaluati ON Subjectiv eDocument4 pagesNursing Care Plan: Assessm ENT Nursing Diagnos IS Planning Intervention Rationale Evaluati ON Subjectiv eJ. TSNo ratings yet
- NCP SciDocument3 pagesNCP SciJaylord VerazonNo ratings yet
- Name and Classification of DrugDocument7 pagesName and Classification of DrugMelrhean GraceNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanRachelleNo ratings yet
- Ineffective Breathing PatternDocument2 pagesIneffective Breathing PatternNicole Genevie MallariNo ratings yet
- Prematurity Assessment Nursing DX Scientific BG Goal/ Objective Nursing Intervention Rationale EvaluationDocument6 pagesPrematurity Assessment Nursing DX Scientific BG Goal/ Objective Nursing Intervention Rationale EvaluationJeanne Mari CostalesNo ratings yet
- APOLONIO, Reyjan L. (NCP 1)Document2 pagesAPOLONIO, Reyjan L. (NCP 1)REYJAN APOLONIONo ratings yet
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 pagesAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresNo ratings yet
- GRAND PAR FINAL NCP For PneumoniaDocument10 pagesGRAND PAR FINAL NCP For PneumoniaJustin AlejoNo ratings yet
- Careplan 1Document11 pagesCareplan 1ligaba1559No ratings yet
- NCPDocument3 pagesNCPErica Denice CastilloNo ratings yet
- CKD Case 2Document16 pagesCKD Case 2Arabylle Maranca AbuelNo ratings yet
- Student NurseDocument2 pagesStudent NurseTAYABAN, KENNETH JAKE, Q.No ratings yet
- Micro Lab#24Document2 pagesMicro Lab#24رجمه ديوانNo ratings yet
- Assessment Planning Intervention Rationale EvaluationDocument2 pagesAssessment Planning Intervention Rationale EvaluationIrish Jane GalloNo ratings yet
- Date/ Time/ Shift Cues Need Nursing Diagnosis With Rationale Objectives of Care Nursing Interventions With Rationale EvaluationDocument2 pagesDate/ Time/ Shift Cues Need Nursing Diagnosis With Rationale Objectives of Care Nursing Interventions With Rationale EvaluationPauleen Trisha SamparaniNo ratings yet
- Ineffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaDocument3 pagesIneffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaNiel MinatozakiNo ratings yet
- Group 2 SOAPIE Case FinalDocument4 pagesGroup 2 SOAPIE Case FinalJames De VeraNo ratings yet
- NCP (Baluyot Jason Lee) Group17Document3 pagesNCP (Baluyot Jason Lee) Group17Jasonlee BaluyotNo ratings yet
- Ncp3 CunananDocument2 pagesNcp3 CunananAbbyNo ratings yet
- Nursing Care Plan: Cystic FibrosisDocument4 pagesNursing Care Plan: Cystic FibrosisYael EzraNo ratings yet
- Romero, Deinielle Ingrid M. (Hiv)Document8 pagesRomero, Deinielle Ingrid M. (Hiv)Deinielle Magdangal RomeroNo ratings yet
- NCP in Caring For A Child With PneumoniaDocument2 pagesNCP in Caring For A Child With PneumoniaJermaen Lou U. GervacioNo ratings yet
- Assessment Nursing Diagnossis Scientific Basis Goal Nursing Intervention Rationale Evaluation IndependentDocument10 pagesAssessment Nursing Diagnossis Scientific Basis Goal Nursing Intervention Rationale Evaluation IndependentPamela laquindanumNo ratings yet
- NURSING CARE PLAN For TB 2003Document6 pagesNURSING CARE PLAN For TB 2003Princess Andrea Bulatao100% (1)
- Nursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPDocument2 pagesNursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPLP Benoza100% (2)
- The Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessFrom EverandThe Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessNo ratings yet
- Brain Tumor: Joyce Minerva S. TagnipesDocument46 pagesBrain Tumor: Joyce Minerva S. TagnipesJoyce Minerva Montero SamsonNo ratings yet
- Diabetic Ketoacidosis (DKA) : Clinical ManifestationsDocument3 pagesDiabetic Ketoacidosis (DKA) : Clinical ManifestationsJoyce Minerva Montero SamsonNo ratings yet
- British Isles RegionDocument79 pagesBritish Isles RegionJoyce Minerva Montero SamsonNo ratings yet
- British Isles Region: Joyce Minerva S. Tagnipes BSN3Document74 pagesBritish Isles Region: Joyce Minerva S. Tagnipes BSN3Joyce Minerva Montero SamsonNo ratings yet
- Pathophysiology DiagramDocument2 pagesPathophysiology DiagramJoyce Minerva Montero SamsonNo ratings yet
- Case Protocol SampleDocument1 pageCase Protocol SampleMarco Paulo Reyes NaoeNo ratings yet
- Anticougulation in PregnancyDocument21 pagesAnticougulation in PregnancyLubna AliNo ratings yet
- ITLSAdvancedPre TestDocument8 pagesITLSAdvancedPre TestMuhammad AsifNo ratings yet
- Oral White and Red LesionsDocument71 pagesOral White and Red LesionsHanin AbukhiaraNo ratings yet
- Vascular RehabilitationDocument10 pagesVascular RehabilitationSuman DeyNo ratings yet
- Introduction To AnesthesiologyDocument68 pagesIntroduction To AnesthesiologyOzza AlhudaNo ratings yet
- Medica Hospital PDFDocument131 pagesMedica Hospital PDFAdarsh ClinicNo ratings yet
- Final Hospital Quality IndicatorsDocument25 pagesFinal Hospital Quality Indicatorsnoor88100% (1)
- Summer 2013 BulletinDocument44 pagesSummer 2013 BulletinnosilaretselNo ratings yet
- Presentation1 Ankush (Autosaved)Document17 pagesPresentation1 Ankush (Autosaved)AnshulNo ratings yet
- ImmunizationDocument6 pagesImmunizationNIKAH PAULINE ALCANTARANo ratings yet
- Chapter33Walker2015 PDFDocument12 pagesChapter33Walker2015 PDFMai AngelNo ratings yet
- Edna K.huffman - Health Information Managemen 1994Document36 pagesEdna K.huffman - Health Information Managemen 1994gspot967% (6)
- Stok BHF 9 September HargaDocument22 pagesStok BHF 9 September Hargabayu ngrh512No ratings yet
- Laryngeal Cancer, Risk Factors, Symptoms and Treatment PDFDocument8 pagesLaryngeal Cancer, Risk Factors, Symptoms and Treatment PDFandre halimNo ratings yet
- Management of Acute Chemotherapy-Related Diarrhea - UpToDateDocument19 pagesManagement of Acute Chemotherapy-Related Diarrhea - UpToDateMarius PapuricaNo ratings yet
- Perioperative Medicine Managing Surgical Patients With Medical Problems by Chikwe, Joanna Walther, Axel Jones, PhilipDocument462 pagesPerioperative Medicine Managing Surgical Patients With Medical Problems by Chikwe, Joanna Walther, Axel Jones, PhilipIbrahim AlmohiniNo ratings yet
- Baba T.1984. Cell-Mediated Immune Protection in Chickens Against P MultocidaDocument6 pagesBaba T.1984. Cell-Mediated Immune Protection in Chickens Against P MultocidakrodriguezNo ratings yet
- AJGP 05 2021 Clinical Sweetman Step by Step Model Brief WEB 2Document7 pagesAJGP 05 2021 Clinical Sweetman Step by Step Model Brief WEB 2alex.ttkNo ratings yet
- Inn Effective TISSUE PERFUSION Related To Impaired O2 Ion AEB Dyspnea and Irregular Heart Rate and Rhythm.Document2 pagesInn Effective TISSUE PERFUSION Related To Impaired O2 Ion AEB Dyspnea and Irregular Heart Rate and Rhythm.Senyorita KHayeNo ratings yet
- Laboratory Critical Values List: Analytes Age Group Critical Low Critical High/ Toxic UnitsDocument2 pagesLaboratory Critical Values List: Analytes Age Group Critical Low Critical High/ Toxic Unitsmelita ratnaNo ratings yet
- Viral EncephalitisDocument101 pagesViral Encephalitisস্বপ্নকথাNo ratings yet
- Blocked Fallopian TubesDocument6 pagesBlocked Fallopian TubesJuliet Amondi100% (1)
- Attention Deficit Hyperactivity Disorder (Adhd)Document43 pagesAttention Deficit Hyperactivity Disorder (Adhd)Thevanath Gunasekaran100% (1)
- Pasquali - Treatment of NMSC PDFDocument109 pagesPasquali - Treatment of NMSC PDFIvanus NicoletaNo ratings yet
- Felton 2016 Journal of ProsthodonticsDocument16 pagesFelton 2016 Journal of Prosthodonticsbkprostho100% (1)
- Nursing BulletsDocument73 pagesNursing BulletsJanine Anjenette Sibayan100% (7)
- Chapter 33 - Assessment and Management of Patients With HematologicDocument8 pagesChapter 33 - Assessment and Management of Patients With HematologicMichael Boado100% (1)
- Obstetric Hemorrhage: by CC Nadine D. BacalangcoDocument87 pagesObstetric Hemorrhage: by CC Nadine D. BacalangcoNadine BacalangcoNo ratings yet
- MCQ CollectionDocument12 pagesMCQ CollectionTeslim RajiNo ratings yet