Professional Documents
Culture Documents
Atypical Hemolytic Uremic Syndrome During Pregnancy Short Review and Case Report With A Favorable Outcome PDF
Atypical Hemolytic Uremic Syndrome During Pregnancy Short Review and Case Report With A Favorable Outcome PDF
Uploaded by
Fortune JournalsCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Haitian Creole For HealthcareDocument15 pagesHaitian Creole For HealthcareAlton Johnson100% (1)
- A Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaDocument11 pagesA Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaFortune JournalsNo ratings yet
- Avsm 004Document7 pagesAvsm 004Fortune JournalsNo ratings yet
- Chemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFDocument17 pagesChemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFFortune JournalsNo ratings yet
- Cerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFDocument8 pagesCerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFFortune JournalsNo ratings yet
- Capsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFDocument18 pagesCapsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFFortune JournalsNo ratings yet
- Biomineralogy of Angiogenesis PDFDocument7 pagesBiomineralogy of Angiogenesis PDFFortune JournalsNo ratings yet
- Cancer Therapyinduced Cardiotoxicity Where Are We Now PDFDocument8 pagesCancer Therapyinduced Cardiotoxicity Where Are We Now PDFFortune JournalsNo ratings yet
- Biochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFDocument16 pagesBiochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFFortune JournalsNo ratings yet
- Final LSCS AuditDocument18 pagesFinal LSCS AuditMooham AяNo ratings yet
- Canine Vaginal CytlogyDocument89 pagesCanine Vaginal Cytlogyvetspain5448No ratings yet
- Hello EveryoneDocument2 pagesHello Everyonehely shahNo ratings yet
- Chatt 225230 P ManuDocument52 pagesChatt 225230 P ManuRICHIHOTS2100% (1)
- Final King Tut EssayDocument3 pagesFinal King Tut Essayapi-208349562No ratings yet
- Guidance Note On District-Level Gap Analysis of RMNCH+A ImplementationDocument49 pagesGuidance Note On District-Level Gap Analysis of RMNCH+A ImplementationJennifer Pearson-ParedesNo ratings yet
- Case Transient Tachypnea of The NewbornDocument52 pagesCase Transient Tachypnea of The NewbornYohana pestraNo ratings yet
- WHO EURO 2019 3497 43256 60624 EngDocument8 pagesWHO EURO 2019 3497 43256 60624 EngBasia JakubiakNo ratings yet
- Acu ProtocolsDocument3 pagesAcu ProtocolsDandhi Firmansyah100% (1)
- Book Guide For Clincal Rotations - Revised by ASODocument5 pagesBook Guide For Clincal Rotations - Revised by ASOOscar HotelNo ratings yet
- V6 - Health CS VC Collectors 22.08.2023Document92 pagesV6 - Health CS VC Collectors 22.08.2023MdnowfalNo ratings yet
- 3) Buku Log Clinical Practice Record PERIOPERATIVE CAREDocument41 pages3) Buku Log Clinical Practice Record PERIOPERATIVE CAREAslam AssandakaniNo ratings yet
- Cancer Hospital SanafontisDocument14 pagesCancer Hospital SanafontisZaid75% (4)
- Nursing Care Baby NewbornDocument41 pagesNursing Care Baby NewbornHengky Hanggara100% (1)
- Guidelines For Surfactant Administration (Surfactant Replacement Therapy) University of Iowa Stead Family Children's Hospital 2Document1 pageGuidelines For Surfactant Administration (Surfactant Replacement Therapy) University of Iowa Stead Family Children's Hospital 2Anonymous 18GsyXbNo ratings yet
- Quiz SampleDocument3 pagesQuiz Sampleyalahopa100% (1)
- Surat Buat VisaDocument12 pagesSurat Buat VisaNurul FitrianaNo ratings yet
- Need To Optimise Infant Feeding CounsellingDocument30 pagesNeed To Optimise Infant Feeding CounsellingfadnesNo ratings yet
- OSCE Mock ExamDocument52 pagesOSCE Mock Examanas100% (2)
- STORZ Powershaver SLDocument18 pagesSTORZ Powershaver SLregistro.infraNo ratings yet
- Brachytherapy Applicator GuideDocument64 pagesBrachytherapy Applicator GuideOky Nur SetyaniNo ratings yet
- Abnormalities of The Female Reproductive Tract Mullerian DefectsDocument1 pageAbnormalities of The Female Reproductive Tract Mullerian DefectsPreethi ShivanandNo ratings yet
- Kapur 2015Document4 pagesKapur 2015SuhartiniNo ratings yet
- Chronic Post-Surgical PainDocument3 pagesChronic Post-Surgical Painnabil mansourNo ratings yet
- Anesthesiology MCQ Sample Exam e PDFDocument5 pagesAnesthesiology MCQ Sample Exam e PDFOsob MohamudNo ratings yet
- Preg LeafletDocument2 pagesPreg LeafletGobind GarchaNo ratings yet
- List of Clinical Assignments: Requirement List First Year B.Sc. NursingDocument7 pagesList of Clinical Assignments: Requirement List First Year B.Sc. Nursingannu panchalNo ratings yet
- Principles of Occlusion in Complete DentureDocument72 pagesPrinciples of Occlusion in Complete DentureDaniel AtiehNo ratings yet
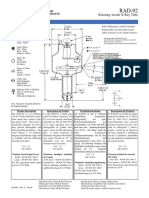
- RAD-92 PdsDocument12 pagesRAD-92 PdspietrokoNo ratings yet
Atypical Hemolytic Uremic Syndrome During Pregnancy Short Review and Case Report With A Favorable Outcome PDF
Atypical Hemolytic Uremic Syndrome During Pregnancy Short Review and Case Report With A Favorable Outcome PDF
Uploaded by
Fortune JournalsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Atypical Hemolytic Uremic Syndrome During Pregnancy Short Review and Case Report With A Favorable Outcome PDF
Atypical Hemolytic Uremic Syndrome During Pregnancy Short Review and Case Report With A Favorable Outcome PDF
Uploaded by
Fortune JournalsCopyright:
Available Formats
Obstet Gynecol Res 2018; 1 (2): 021-027 DOI: 10.
26502/ogr004
Case Report
Atypical Hemolytic Uremic Syndrome During Pregnancy:
Short Review and Case Report with a Favorable Outcome
N.A.Zharkin¹*, M.E.Statsenko¹, M.M.Stazharova², N.A.Burova¹, S.A.Prokhvatilov², N.E.Kushniruk²
1
Department of Obstetrics and Gynecology, Department of Internal Diseases of Pediatric Faculty of Volgograd State
Medical University, Volgograd, Russia.
2
Department of Nephrology, Department of Gynecology, VRCH No. 1, Volgograd Regional Clinical
Hospital Nо.1), Volgograd, Russia.
*Corresponding Author: N.A.Zharkin, Department of Obstetrics and Gynecology, Department of Internal
Diseases of Pediatric Faculty of Volgograd State Medical University, Volgograd, Russia; E-mail:
zharkin55@mail.ru
Received: 23 March 2018; Accepted: 09 April 2018; Published: 10 April 2018
Abstract
The atypical hemolytic uremic syndrome (aHUS) is the most complex disease in the diagnosis, treatment and
prognosis among the thrombotic microangiopathy. The article describes the clinical case of a 32-year-old woman
with an aHUS in 32 week of gestation. It is given the diagnosis and treatment of this case till clinical convalescence.
Observation within 1 year after the episode of the aHUS is showing up a chronic kidney failure, which will provide
renal replacement therapy in future.
Keywords: Atypical Hemolytic Uremic Syndrome; Acute Renal Failure; Complement Pathway; Chronic; Plasma
Exchange; Postpartum Period; Pregnancy; Chemotactic Factor Inactivator; Complement; Eculizumab; Renal
Dialysis; Thrombotic Microangiopathy.
1. Case
Thrombotic microangiopathy (TMA) is a group of diseases associated with hemolysis, hemorrhagic syndrome and
acute renal failure. During pregnancy, these diseases cause high maternal and perinatal morbidity and mortality due
to the difficulty of diagnosing and different approaches to treatment, depending on the TMA type.
Obstetrics and Gynecology Research - Vol. 1 No. 2 - Jun 2018. 21
Obstet Gynecol Res 2018; 1 (2): 021-027 DOI: 10.26502/ogr004
Recently, cases of TMA in pregnant women due to sometimes dramatic events have been reported more frequently,
that is why each case with a favorable outcome for the mother and her child can be an important matter for
discussion and enrichment of the general knowledge bank with data on this rare but life-threatening pathology.
There are several variants of TMA that complicate the course of pregnancy: pregnancy-associated hypertension,
preeclampsia (PE), DIC and HELLP syndrome, thrombotic thrombocytopenic purpura (TTP), catastrophic
antiphospholipid syndrome (CAS), sepsis and, as the main manifestation of TMA, - atypical hemolytic uremic
syndrome (aHUS) [1, 2]. Life-threatening complications of TMA include acute renal failure (ARF), brain injury
(coma), gastrointestinal tract injury (hemorrhage), and heart failure (acute heart failure). Predisposing factors of
TMA are preeclampsia, premature birth, caesarean section, infection, psycho-traumatic situations [3, 4].
Diagnosing and treatment of various variants of TMA in pregnant women involves considerable difficulties. That is
why, needless to say that colleagues wish to share their experience on each medical case with both favorable [4,5]
and unfavorable outcomes [6].
Among TMA, atypical hemolytic uremic syndrome (aHUS) is the most complicated disease in terms of diagnosing,
treatment and prognosis [7]. It is caused by genetic defects in regulatory proteins of the complement system. In this
regard, as opposed to preeclampsia and HELLP-syndrome, childbirth does not lead to the regression of symptoms;
on the contrary, the microangiopathic process worsens with rapid development of multiple organ failure.
Currently, there is no doubt that preeclampsia and HELLP-syndrome are connected with genetically determined
dysregulation of the alternative complement pathway (ACP), which may become excessive, uncontrolled during
pregnancy, which, probably, may contribute to the early-onset severe preeclampsia with subsequent transformation
to aHUS [8, 9].
The confounding factor is that these genetic disorders in the complement system manifest for the first time precisely
during pregnancy or childbirth, which causes the need to perform diagnosis and choose treatment policy within
a limited time period. Our medical case confirms this as well.
A 32-year-old patient with second pregnancy, first delivery. She had no diseases before pregnancy. In 2015, the first
pregnancy ended with an abortion at her will. The second pregnancy was uneventful until 33 weeks. Initial
laboratory blood and urine values were normal: hemoglobin 132 g/L, platelets 214x109. Common urine test has not
detected protein; urinary sediment was empty.
Ultrasound screening at 33 weeks revealed fetoplacental insufficiency and fetal intrauterine growth retardation
(IUGR), and therefore the patient was hospitalized for examination and treatment. Clinical and laboratory
examination revealed no abnormalities. In connection with IUGR and the perspective of preterm childbirth,
prevention of RDS (respiratory distress syndrome) of the fetus with corticosteroids was carried out.
Obstetrics and Gynecology Research - Vol. 1 No. 2 - Jun 2018. 22
Obstet Gynecol Res 2018; 1 (2): 021-027 DOI: 10.26502/ogr004
On 08/28/2016 at 11:10, a partial abruption of a normally situated placenta with external hemorrhage of
approximately 200 mL occurred. In this regard, the emergency caesarean section was performed. A girl was born
with mass of 1440 g, height of 40 cm, 4 and 6 scores by the Apgar scale. The total blood loss volume was 1250 mL:
before the surgery - 200 mL, the volume of the retroplacental hematoma - 400 mL, during the surgery - 650 mL. At
the end of the surgery, hemoglobin amounted to 78 g/L, platelets - 170x109.
Within the first 24 hours, the post-surgery period was complicated by the development of anuria, emergence and
rapid augmentation of azotemia (serum creatinine amounted to 188 - 203 µmol/L), which allowed to establish acute
renal failure. The patient was treated with infusions of crystalloids, fresh frozen plasma, and furosemide for diuresis
stimulation.
On the following day, 08/29/2016, negative dynamics was observed: pale skin and swelled face, lower limbs and the
anterior abdominal wall. Respiration rate - 24 breaths per minute. Vesicular breathing in the lungs, no crackles.
Heart sounds were rhythmic, muffled. Heart rate - 76 beats per minute, blood pressure - 130/90 mm Hg. The
progression of anemia was observed (Hg = 68 g/L), as well as a decrease in platelets up to 150 x 109 and a rise in
blood creatinine up to 342 μmol/L. Anuria persisted.
Laboratory tests showed rapidly increasing anemia (HB = 63-58 g/L) and thrombocytopenia up to 50 x 109, single
schizocytes. Blood chemistry: creatinine 404 - 611 μmol/L, AST - 205 U/L, ALT - 345 U/L, Potassium - 5.17
mmol/L, Sodium - 132 mmol/L, LDH - 2996 U/L, Coombs’ test negative.
Ultrasound of the abdominal cavity and kidneys: the liver and spleen are not changed, the urinary bladder is empty,
the size of the kidneys is not changed, the parenchyma with increased echogenicity, the corticomedullary
differentiation is pronounced; during CDI (Color Doppler Imaging), the vascularization is visible up to the level of
the arcuate vessels. Chest X-ray: lung pattern without focal and infiltrative shadows. There was a small amount of
fluid in the lower parts of the pleural cavities. Transfusion of washed red blood cells, antibacterial and detoxification
therapy were added to the treatment regimen.
Considering the rapidly increasing anemia in the absence of hemorrhage with signs of microangiopathic hemolysis
(high LDH values), thrombocytopenia, acute renal failure (anuria, rapid increase of creatinine), TMA was suspected,
namely, atypical hemolytic uremic syndrome.
To verify the diagnosis, a test for ADAMTS-13 was performed, the level of which amounted to 40% (reference
values 93 - 113%), which allowed to establish the final diagnosis of aHUS. Specialists from the Federal Center gave
consultation via videoconferencing.
On 08/31/2016, the treatment with fresh frozen plasma was started in plasma-exchange regimens in the volume of
30 mL/kg of body weight per day (in total - 4 procedures) under the cover of unfractionated heparin (UFH) in a dose
Obstetrics and Gynecology Research - Vol. 1 No. 2 - Jun 2018. 23
Obstet Gynecol Res 2018; 1 (2): 021-027 DOI: 10.26502/ogr004
of 70-80 mg/kg of weight. Renal replacement therapy was started in the form of prolonged veno-venous
hemodiafiltration sessions (PVVHDF). In total, 5 sessions were performed during the hospitalization.
Arterial hypertension appeared during the following days (blood pressure 150/90 - 170/100 mm Hg), for which
reason the therapy was supplemented with antihypertensive drugs. Echocardiography showed concentric remodeling
of the left ventricle myocardium, normal systolic and diastolic functions of the left ventricle, the ejection fraction
was 62%.
Despite the therapy, the signs of ongoing microangiopathic hemolysis were observed in the patient: persisting
anemia (HB=56 - 65 g/L), thrombocytopenia (plt=77 - 80x109), high LDH values (1269 - 714 U/L), lack of
resolution of acute renal failure, persisting azotemia (blood creatinine = 516 - 836 µmol/L). Skin hemorrhagic
syndrome appeared with a massive hemorrhagic rash on the body, upper and lower limbs. Swelling of the face and
the lower limbs increased. Weakening of breathing was observed in the lower sections of the lungs. There was
persistent hypertension in the range from 150/90 to 200/130 mm Hg.
On 09/02/16, on the 5th day of the patient’s stay in the hospital, after the second remote consultation with specialists
from Moscow, it was decided to cancel the plasma-exchange sessions and to start targeted therapy with Eculizumab
(Soliris), at a dose of 900 mg I.V. by drop infusion, once a week, a total of 4 infusions.
After 4 weeks, the patient’s condition improved: peripheral and cavitary swelling regressed, hemorrhagic syndrome
was neutralized, acute renal failure was resolved, diuresis recovered after the 2nd infusion of Eculizumab on the 17th
day of the anuretic period. Blood pressure decreased to 140/90 mm Hg.
Laboratory tests showed an improvement of anemia (HB = 109 g/L); the signs of microangiopathic hemolysis were
neutralized (platelets increased up to 180x109), LDH decreased to 341 U/L, the values of nitrogen metabolism
improved significantly, serum creatinine decreased to 219 μmol/L.
With repeated dynamic nephrosonographies after administration of Eculizumab, we observed a weakened blood
flow above the arcuate arches in the both kidneys. On echocardiography, the ejection fraction increased up to 70%.
Therapy with Eculizumab was cancelled. On 09/29/2016, the patient was discharged with recommendations to
continue nephrotoprotective therapy.
During a year after discharge, the patient was followed-up with monthly laboratory testing. The results are presented
in the chart. Nephrosonography performed in December 2017 showed signs of decreasing size of the kidneys and
signs of developing nephrosclerosis.
Obstetrics and Gynecology Research - Vol. 1 No. 2 - Jun 2018. 24
Obstet Gynecol Res 2018; 1 (2): 021-027 DOI: 10.26502/ogr004
2. Discussion
The present observation demonstrates the peculiarities of clinical manifestation and the course of “obstetric” aHUS
with onset in the postpartum period. The sum of various obstetric complications, namely, the combination of a
premature placental abruption with hemorrhage, caesarean section, postpartum inflammation caused by a large
wound surface in the uterus, led to systemic activation of the alternative complement pathway, which induced the
development of aHUS in the patient with a genetic predisposition.
A typical clinical and laboratory pattern of TMA involves primary renal damage in the onset of the disease,
development of microangiopathic hemolytic anemia and thrombocytopenia, decreased level of ADAMTS-13, which
indicates active formation of microthrombi [10]. Detection of these symptoms in progress allowed us to establish
aHUS in this patient.
Despite a moderate decrease in the severity of hemolysis, therapeutic plasma exchange started on the 3rd day of the
postpartum period had not led to the expected results. This fact required administration of targeted therapy with
complement-blocking drug Eculizumab. It is a glycosylated, humanized monoclonal antibody, a kappa-
immunoglobulin with high affinity for the complement component C5. Through binding to the latter, Eculizumab
prevents further activation of the complement by stopping its destroying activity. By the end of induction therapy
consisting of 4 infusions with a week’s interval, it was possible to stop the hematological signs of TMA.
Performed sessions of hemodiafiltration contributed to the resolution of acute renal failure. Although the renal
function had not fully recovered by the time of patient’s discharge, any further renal replacement therapy sessions
were not required.
Obstetrics and Gynecology Research - Vol. 1 No. 2 - Jun 2018. 25
Obstet Gynecol Res 2018; 1 (2): 021-027 DOI: 10.26502/ogr004
The follow-up showed that despite complete hematological remission of aHUS and nephroprotective therapy, the
patient still demonstrated signs of renal failure. A chronic renal disease has formed. Nephrosclerosis (renal scarring)
is developing, which determines an unfavorable outcome in terms of renal failure progression up to the terminal
stage and further transition of the patient to renal replacement therapy in the long term.
References
1. Elayoubi J, Donthireddy K, Nemakayala DR. Microangiopathies in pregnancy. BMJ Case Rep 2018.
2. Silver RM. Catastrophic antiphospholipid syndrome and pregnancy. Semin Perinatol 42 (2018): 23-32.
3. Fox L, Cohney SJ, Kausman JY, Shortt J, Hughes PD, et al. Consensus Opinion on Diagnosis and
Management of Thrombotic Microangiopathy in Australia and New Zealand. Nephrology (Carlton) 2018.
4. Valter Romão de Souza, Jr Ana Beatriz Cavalcante de Oliveira, Ana Maria Vanderlei, Amanda Queiroz da
Mota Silveira Aroucha, Bruna Pontes Duarte, et al. Inherited thrombotic thrombocytopenic purpura
mimicking immune thrombocytopenic purpura during pregnancy: a case report. J Med Case Report 2018.
5. Cravero R, Ardissino G, Colageo U, Staffa P, Bruschetta E, et al. Efficacy of eculizumab in a case of
pregnancy-associated aHUS. Ital Nefrol 33 (2016): 14.
6. Pronina I S. Trudniy diagnoz: aHUS, assotsiirovaniy c rodami. Bulletin of Medical Internet Conferences
2016.
7. Zephirova TP, Maltseva LI, Zamaleeva RS, Zhelezova ME. Syndrome of thrombotic microangiopathy in
life-threatening complications of pregnancy and labor in women. Prakticheskaya meditsina 7 (2017): 26-
30.
8. Skully M. Thrombotic Thrombocytopenic Purpura and Atypical Hemolytic Uremic Syndrome
Microangiopathy in Pregnancy. Semin Thromb Hemost 42 (2016):774-779.
9. Bruel A, Kavanagh D, Noris M, Delmas Y, Wong EKS, et al. Hemolytic Uremic Syndrome in Pregnancy
and Postpartum. Clin J Am Soc Nephrol 12 (2017):1237-1247.
10. Cines DB, Levine LD. Hematology Thrombocytopenia in pregnancy. Hematology Am Soc Hematol Educ
Program 2017 (2017): 144-151.
Citation: N.A.Zharkin, M.E.Statsenko, M.M.Stazharova, N.A.Burova, S.A.Prokhvatilov, N.E.Kushniruk. Atypical
Hemolytic Uremic Syndrome During Pregnancy: Short Review and Case Report with a Favorable Outcome. Obstetrics
and Gynecology Research 1 (2018): 021-027.
This article is an open access article distributed under the terms and conditions of the
Creative Commons Attribution (CC-BY) license 4.0
Obstetrics and Gynecology Research - Vol. 1 No. 2 - Jun 2018. 26
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Haitian Creole For HealthcareDocument15 pagesHaitian Creole For HealthcareAlton Johnson100% (1)
- A Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaDocument11 pagesA Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaFortune JournalsNo ratings yet
- Avsm 004Document7 pagesAvsm 004Fortune JournalsNo ratings yet
- Chemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFDocument17 pagesChemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFFortune JournalsNo ratings yet
- Cerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFDocument8 pagesCerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFFortune JournalsNo ratings yet
- Capsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFDocument18 pagesCapsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFFortune JournalsNo ratings yet
- Biomineralogy of Angiogenesis PDFDocument7 pagesBiomineralogy of Angiogenesis PDFFortune JournalsNo ratings yet
- Cancer Therapyinduced Cardiotoxicity Where Are We Now PDFDocument8 pagesCancer Therapyinduced Cardiotoxicity Where Are We Now PDFFortune JournalsNo ratings yet
- Biochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFDocument16 pagesBiochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFFortune JournalsNo ratings yet
- Final LSCS AuditDocument18 pagesFinal LSCS AuditMooham AяNo ratings yet
- Canine Vaginal CytlogyDocument89 pagesCanine Vaginal Cytlogyvetspain5448No ratings yet
- Hello EveryoneDocument2 pagesHello Everyonehely shahNo ratings yet
- Chatt 225230 P ManuDocument52 pagesChatt 225230 P ManuRICHIHOTS2100% (1)
- Final King Tut EssayDocument3 pagesFinal King Tut Essayapi-208349562No ratings yet
- Guidance Note On District-Level Gap Analysis of RMNCH+A ImplementationDocument49 pagesGuidance Note On District-Level Gap Analysis of RMNCH+A ImplementationJennifer Pearson-ParedesNo ratings yet
- Case Transient Tachypnea of The NewbornDocument52 pagesCase Transient Tachypnea of The NewbornYohana pestraNo ratings yet
- WHO EURO 2019 3497 43256 60624 EngDocument8 pagesWHO EURO 2019 3497 43256 60624 EngBasia JakubiakNo ratings yet
- Acu ProtocolsDocument3 pagesAcu ProtocolsDandhi Firmansyah100% (1)
- Book Guide For Clincal Rotations - Revised by ASODocument5 pagesBook Guide For Clincal Rotations - Revised by ASOOscar HotelNo ratings yet
- V6 - Health CS VC Collectors 22.08.2023Document92 pagesV6 - Health CS VC Collectors 22.08.2023MdnowfalNo ratings yet
- 3) Buku Log Clinical Practice Record PERIOPERATIVE CAREDocument41 pages3) Buku Log Clinical Practice Record PERIOPERATIVE CAREAslam AssandakaniNo ratings yet
- Cancer Hospital SanafontisDocument14 pagesCancer Hospital SanafontisZaid75% (4)
- Nursing Care Baby NewbornDocument41 pagesNursing Care Baby NewbornHengky Hanggara100% (1)
- Guidelines For Surfactant Administration (Surfactant Replacement Therapy) University of Iowa Stead Family Children's Hospital 2Document1 pageGuidelines For Surfactant Administration (Surfactant Replacement Therapy) University of Iowa Stead Family Children's Hospital 2Anonymous 18GsyXbNo ratings yet
- Quiz SampleDocument3 pagesQuiz Sampleyalahopa100% (1)
- Surat Buat VisaDocument12 pagesSurat Buat VisaNurul FitrianaNo ratings yet
- Need To Optimise Infant Feeding CounsellingDocument30 pagesNeed To Optimise Infant Feeding CounsellingfadnesNo ratings yet
- OSCE Mock ExamDocument52 pagesOSCE Mock Examanas100% (2)
- STORZ Powershaver SLDocument18 pagesSTORZ Powershaver SLregistro.infraNo ratings yet
- Brachytherapy Applicator GuideDocument64 pagesBrachytherapy Applicator GuideOky Nur SetyaniNo ratings yet
- Abnormalities of The Female Reproductive Tract Mullerian DefectsDocument1 pageAbnormalities of The Female Reproductive Tract Mullerian DefectsPreethi ShivanandNo ratings yet
- Kapur 2015Document4 pagesKapur 2015SuhartiniNo ratings yet
- Chronic Post-Surgical PainDocument3 pagesChronic Post-Surgical Painnabil mansourNo ratings yet
- Anesthesiology MCQ Sample Exam e PDFDocument5 pagesAnesthesiology MCQ Sample Exam e PDFOsob MohamudNo ratings yet
- Preg LeafletDocument2 pagesPreg LeafletGobind GarchaNo ratings yet
- List of Clinical Assignments: Requirement List First Year B.Sc. NursingDocument7 pagesList of Clinical Assignments: Requirement List First Year B.Sc. Nursingannu panchalNo ratings yet
- Principles of Occlusion in Complete DentureDocument72 pagesPrinciples of Occlusion in Complete DentureDaniel AtiehNo ratings yet
- RAD-92 PdsDocument12 pagesRAD-92 PdspietrokoNo ratings yet