Professional Documents
Culture Documents
Chronic Rinosinusitis With Nasal Polyposis and Smell Disorders One Emergent Association PDF
Chronic Rinosinusitis With Nasal Polyposis and Smell Disorders One Emergent Association PDF
Uploaded by
Fortune JournalsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chronic Rinosinusitis With Nasal Polyposis and Smell Disorders One Emergent Association PDF
Chronic Rinosinusitis With Nasal Polyposis and Smell Disorders One Emergent Association PDF
Uploaded by
Fortune JournalsCopyright:
Available Formats
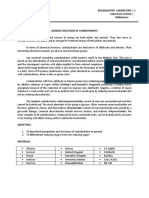
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.
10020011
Review Article
Chronic Rinosinusitis with Nasal Polyposis and Smell Disorders:
One Emergent Association
Melissa Castillo-Bustamante1*, Diego Bustamante-Mesa2, Wilson Bustamante-Hernandez3,
Stella Maris Cuevas4
1
Otolaryngologist, Hospital de Clinicas Jose de San Martin, Buenos Aires, Argentina
2
Otolaryngologist, Clinica Las Vegas, Medellin, Colombia
3
Otolaryngologist, Clinica ORLANT, Medellin, Colombia
4
Otolaryngologist, Hospital de Clinicas Jose de San Martin, Seccion Rinologia y Olfato, Buenos Aires, Argentina
*Corresponding Author: Melissa Castillo-Bustamante, Avenida Cordoba 2351, Primer Piso, Otolaryngology
Department, Buenos Aires, Argentina, Tel: +541132759594; E-mail: melissacastillobustamante@gmail.com
Received: 03 January 2019; Accepted: 16 January 2019; Published: 24 January 2019
Abstract
Nasal polyposis is one of the most frequent causes of nasal obstruction in Otorhinolaryngologic. This disorder is
associated to symptoms as nasal congestion, facial pain and olfactory disturbances. Although olfactory disorders are
indicated as one patient’s complaint, the study of smell disorders in patients with nasal polyposis has been
performed in other countries, in Latin America it is beginning. The aim of this work is to review the association
between smell disorders and nasal polyposis as the approach of these concomitant pathologies.
Keywords: Smell; Nasal polyps; Smell disorders
1. Introduction
Chronic rhinosinusitis is a disorder marked by inflammation of the nose and sinuses, whose diagnostic criteria
include facial pain, nasal obstruction and/or congestion, anterior or posterior discharge and olfactory alterations [1].
The olfactory alterations prevalence in patients with Chronic rhinosinusitis has been reported between 60 to 80%,
causing physical, and social alterations that affects the life quality of patients [1, 2]. As main causes of olfactory
dysfunction associated with chronic rhinosinusitis, there are two known mechanisms; one is the mechanical
obstruction of the olfactory cleft by nasal polyps which can cause disturbance on the airflow. The other is the
localized inflammation in the olfactory region that could cause functional disruption at the level of the olfactory
Journal of Surgery and Research 1
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
membrane [3]. However, these above are not the only ones etiologies associated, asthma, smoking and atopies are
related to olfactory dysfunction on patients with chronic rhinosinusitis and polyps [4, 5]. Despite the incidence of
olfactory dysfunctions in patients with chronic rhinosinusitis and nasal polyposis, there are few reviews of the
association of olfactory disturbances and chronic rhinosinusitis with nasal polyps [6, 7]. The aim of this article is to
review the definition and related concepts about the association between chronic rhinosinusitis with nasal polyposis
and olfactory alterations as their clinical approach in patients with these concomitant entities.
2. Epidemiology
Olfactory disturbances are conditions that emerge from multiple etiologies, being the most common: conditions in
the airway (39%), idiopathic causes (18%), trauma (17%), congenital abnormalities (3%) and other etiologies (3%)
[8]. Rhinosinusitis (21%) is the second leading cause of olfactory alterations, at least 200,000 visits per year in
North America are due to his cause and affects between 1-2% of the general population [9]. Around 10 million
people in the United States per year are diagnosed with olfactory disorders [10]; in Spain around 230,000 patients
consulted for anosmia and around 7.82 million people are diagnosed with different degrees of hyposmia [11]. In
Latin America, there is an underreport of olfactory alterations according to the literature review.
3. Chronic Rinosinusitis with Nasal Polyposis and Olfactory Disturbances
Nasal polyposis is defined as a chronic inflammatory process with edematous with hyperplasic nasal involvement, it
can be altered by comorbidities such as allergies, asthma or the combination of rhinitis and asthma, as well as
bacterial or fungal infections, drugs toxicity and injuries due to patient's occupational environment [12].The altered
perception of smell has been described as one of the most common symptoms in patients with nasal polyposis
affecting 65 to 80% of patients [13]. Within olfactory dysfunctions, variations in the odor’s perception are
considered, such as hyposmia, where there is a decrease in smell, anosmia described as the complete loss of the
odor. Other entities considered include distortion in olfactory perception such as dysgeusia and odor in the absence
of an external stimulus known as pantosmia [14]. Although the chronic rhinosinusitis with polyposis associated with
olfactory alterations’s pathogenesis stills under study, this may be due to a combination of factors such as
mechanical obstruction of the edematous mucosa and polyps as lesions in the olfactory neuroepithelium caused by
chronic inflammation. This is associated to transport disturbances of odorants to the sensory receptor cells, which is
defined as conductive loss. It has been found in patients with chronic rhinosinusitis with nasal polyposis, the nasal
obstruction is mainly generated by polypoid tissue at least in 78% [15]. An increase of inflammatory mediators
caused by the infiltration of cells of the immune system is also studied as an event associated with direct or indirect
effects on the structure and/or function of the neuroepithelium, which is defined as a neurosensory loss [16]. Authors
as Kern described in patients with chronic anosmia and rhinosinusitis significant levels of localized inflammation in
the olfactory neuroepithelium, this is related to damage onto bipolar neurons and alter neurogenesis [17]. Other
neurologic factors associated with olfactory compromise, are the inflammatory processes on the first and fifth
cranial nerve generated by the rhinosinusal process [18]. However, the neuroepithelial damage is not the only one
associated in the pathogenesis of the olfactory alteration; smoking, asthma, age, history of nasal endoscopic surgery
Journal of Surgery and Research 2
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
as well as allergic rhinitis are coadjuvants in the history of olfactory disruptions in patients with chronic
rhinosinusitis with olfactory alterations [19].
4. Evaluation of Patients with Chronic Rhinosinusitis and Nasal Polyposis and Smell Disorders
4.1 Clinical history
In the initial approach of patient with chronic rhinosinusitis with nasal polyposis and olfactory alterations, other
events related to age, occupation and medical status should be ruled out in order to direct the correct treatment and
follow-up. In young patients should be inquired for congenital anosmia and Kallmann syndrome, in patients between
sixty to seventy years old. Immunologic changes in smell should be taken in account, those are present without
medication intake [20]. Other causes as viral and bacterial infections, traumatic brain injuries, psychological states
should be asked. The smell loss is present at least in 10% of patients with traumatic injuries, on the frontal and/or
temporal lobes, affecting The olfactory tract and cleft [21]. Active smoking status, migraine as neurodegenerative
diseases as Alzheimer, Parkinson and multiple sclerosis are other disorders associated to smell disturbances. Other
less common causes are cocaine use, chemical exposition of butyl-acetate, formaldhehíde, thrichloroetilene,
benzene, selenide hydrogen and exposition to environmental agents as exposition to ashes, chalk, chromium, iron,
nickel, silicon dioxide [22] .Other factors as nutritional status as A and B vitamin and Iron or Zinc deficiency,
Chronic kidney failure, liver disease, cancer and human immunodeficiency syndrome should be inquired [22].
Psychiatric conditions as schizophrenia, depression, reference olfactory syndrome should be documented in the
clinical and physical exam [22]. Other conditions as meningiomas, frontal and temporal lobe tumors,aneuryms,
esthesioneuroblastoms and squamous cell cancer [22]. Drugs as antibiotics, antidepressives and anticonvulsants
should be ruled out in patients with nasal polyps and chronic rhinosinusitis with smell disorders [22]. In the initial
approach the type of olfaction loss needs to be documented if it was sudden, intermittent (due to inflammatory
process as allergies and infections), gradual (seen in patients with nasal polyps and chronic infections of respiratory
tract) and secondary as obstruction due to fracture and inflammation [22].
4.2 Physical exam
The rhinorrhea presence as intranasal lesions, polyps location (near the inferior turbinate or away classified for the
Lund Mackay Score) should be recorded, as well the careful evaluation of the function of the cranial nerves, mainly
with emphasis on the first and fifth cranial pairs [23]. The initial assessment of the patient with nasal polyposis and
olfactory alterations, involves from the anamnesis of the patient, complementary examinations assessed by fiber-
endoscopy and nasal endoscopy are especially useful in patients with nascent polyposis located in the middle meatus
[23]. However, findings in the ethmoid sinuses are not easily found with this method, being computed tomography a
complementary element in the study of patients with nasal polyposis and olfactory alterations. The analysis of the
olfactory region and the extrameatal area is also extended in tomographic assessment [23].
Journal of Surgery and Research 3
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
4.3 Imaging
In the study of patients with chronic rhinosinusitis with nasal polyposis and olfactory alterations, imaging studies
may be useful. However, all imaging techniques have limitations and studies with negative results may not rule out
structural injuries. Frontal radiographs have multiple limitations, because they do not offer enough detail about
structures such as the osteomeatal complex [23]. Computed tomography is one of the most effective techniques for
the study of olfactory alterations. Coronal sections are useful in the assessment of paranasal anatomy. 5 mm sections
are useful to identify bone structures in the ethmoid, cribriform plate and olfactory cleft, as well as in the temporal
bone and seventh cranial nerve [23]. Some classifications as Lund Mackay, is a validated staging system for chronic
rhinosinusitis with nasal polyposis. Each paranasal sinus is evaluated with a score between 0 and 2 (0=no
abnormality, 1=partial opacity, 2=total opacity) having a maximum score of 12 per side, being for both sides with a
total of 24. The obstruction of the complex Osteomeatal is rated as 0 (no obstruction) or 2 (obstructed). Although all
paranasal sinuses are qualified and staged, this scheme is an indicator of the inflammatory process in the nasal
cavities, which is a significant factor for olfactory dysfunction in sinonasal pathology [24]. Computed tomography is
less effective than nuclear magnetic resonance in the definition of soft tissue involvement. The use of intravenous
contrast is optimal for the identification of vascular lesions, tumors, abscesses and meningeal and parameningeal
processes that may occur concomitantly in patients with chronic rhinosinusitis with nasal polyposis [24].
4.4 Rhinodebitomanometry
Rhinodebitomanometry is a dynamic test which evaluates nasal function by calculating the airflow resistance
through the measurement of transnasal pressure and the air passage during respiration. Laminar and turbulent flows
are determined in accordance with nasal obstructive conditions such as the collapsibility of the nasal wall and
irregularities on its configuration. The final result indicates an objective obstruction of the airway found for
example, in patients with nasal polyposis where anatomical alterations at the nasal cavity are found. Other use
reported is the objective measurement of pre and postoperative airflow [25]. Acoustic rhinomanometry is based on
the analysis of the waves reflected from the nasal cavity, by sending pulses inside the nose, allowing recording and
analyzing the sound reflex. The main benefit of acoustic rhinomanometry is the ability to identify the narrowest part
of the nasal cavity, this usually corresponds to the area of the nasal valve or the head of the inferior turbinate. Its
main use is to provide reflection on the geometry and volume of the nasal cavities as well as their anatomical
assessment [25]. Although both studies have been used in the assessment of pre and postoperative nasal obstruction
in patients with sinus pathology, no studies have been reported at the time of the evaluation of the literature to
indicate its use in patients with olfactory disorders and chronic rhinosinusitis.
4.5 Tests for olfactory assessment
For the olfactory assessment, multiple tests have been described which are responsible for odorific discrimination in
addition to the assessment of first and fifth cranial nerve function, which are involved in olfactory phenomena. One
of the most widely used is the Odor Identification test, which evaluates the ability to identify 40 microencapsulated
odorants. These emerge by rubbing microencapsulated strips with a pen or pencil. The scores of the patients are then
Journal of Surgery and Research 4
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
compared according to established values for age and sex. It can be useful in the assessment of each nostril
separately. Unilateral olfactory deficits can suggest olfactory causes such as nasal obstruction due to septal
deviation, nasal polyps and others [26].
Other tests available for olfactory evaluation include the Pocket Smell Test that evaluates three encapsulated items
of forced choice, an olfactory briefcase for identification of odors and the kit of odors in squeezable bottles [27].
Currently, there are two references instruments known as the Pennsylvania Smell Identification Test (UPSIT) and
the Connecticut Chemosensory Clinical Research Center (CCCRC) developed in the United States. Together, they
have been used for olfactory evaluation studies in North America In Europe, smear tests as well as floppy tests are
the most commonly used, however, the identification of the nature of the odor is associated with aromatic family
items according to the region where they have been developed and validated [28].
As one of the olfactory assessment tools in Latin America, the BAST 24 (Barcelona Smell Test) has emerged as one
of the evaluation alternatives with validation in Spanish population. In this is registered the ability to perceive the
presence or absence of an odor, which is called detection and its ability to properly discern the presented odor,which
is called accuracy. The applied method consists of the forced response evaluating the first and fifth cranial nerve
components, verifying the olfaction and affection by the first cranial nerve and the affectation of the rhinosinusal
mucosa via the fifth cranial nerve [28]. Twenty-four chemical components (odorants) are included within the BAST
24, 20 scents evaluate the first cranial nerve which include odorants such as: banana, gasoline, lemon, rose, onion,
smoke, anise, coconut, vanilla, melon, tangerine, almond, pineapple, cheese, strawberry, mushrooms, eucalyptus,
cloves, turpentine and peach; as well as 4 scents for the evaluation of the fifth pair: formalin, vinegar, amonio and
mustard. Within the evaluation of some odors it can be determined that odorants such as lemon produce little
excitement or little trigeminal excitation, others like the eucalyptus produce a mixed but balanced stimulation and
that the mustard produces a strong trigeminal excitement [28].
5. Therapeutic Proposal and Post-Treatment
5.1 Nasal polyposis and postoperative olfactory alterations
The presence of nasal polyposis in patients with chronic rhinosinusitis with olfactory alterations can lead to initial
medical management and follow-up by otolaryngologists, requiring the use of local and systemic medical
treatments. In refractory processes, as well as permanent and persistent respiratory obstruction, the surgical option
emerges as an option [29]. The aim of endoscopic sinus surgery is to optimize rhinosinusal function and improve
access for topical medical therapy. However, olfactory outcomes after endoscopic nasal surgery can be variable and
their results are variable. Some previous studies indicate that these procedures improves olfactory dysfunction,
however, other recent prospective studies have added detail about the impact of endoscopic procedures on olfactory
dysfunction. In patients with anosmia who have nasal polyposis versus patients with hyposmia with same condition,
olfaction improvement has been reported for anosmic patients after endoscopic sinus surgery. The improvement for
this group of patients remained stable even one year after surgery [29].
Journal of Surgery and Research 5
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
The possible hypothesis associated with olfactory improvement in patients with anosmia was indicated as a
mechanical obstruction in the olfactory cleft which was sensitive to surgical removal. Compared with hyposmic
patients who have a multifactorial etiology of the olfactory tract associated with inflammation and neuroepithelial
damage, surgical removal was less amenable to surgical optimization [29]. Olfactory changes after surgery have
been reported in studies indicating at least 23% of patients who perceived change, 68% did not indicate
improvement and 9% of patients worsened after performing endoscopic nasal surgery. Regarding the clinical
evolution of patients with anosmia, an improvement of 75% has been reported in those who received endoscopic
surgery, although residual hyposmia was documented, probably due to a permanent lesion at the level of
neuroepithelium [30]. According to the reviewed evidence, it has been suggested that the improvement of olfactory
dysfunction related to chronic rhinosinusitis after endoscopic nasal surgery is variable and is a challenge to predict,
some factors studied such as the severity of olfactory loss, age less than 55 years, duration of olfactory loss less than
10 years, eosinophilia and the non-existence of endoscopic nasal surgery have been determinants in the evaluation of
olfactory improvement after endoscopic nasal procedures. Although there is contradictory evidence, it seems that in
anosmic patients with nasal polyposis they have a considerable olfactory improvement after rhinosinusal endoscopic
surgery [30, 31].
5.2 Medical treatment after endoscopic sinus surgery
The use of intranasal and systemic corticosteroids has been described within the schemes of use for pre and
postoperative treatment in patients with chronic rhinosinusitis with polyposis,some of them with olfactory
dysfunction associated. These are determinants in inflammatory decline and edema [32]. Oral corticosteroids have
shown subjective and objective improvement in the olfactory response in patients with chronic rhinosinusitis with
polyposis in periods of 8 to 12 weeks of medical treatment. It is plausible that the effect of oral corticosteroids may
decrease after the initial improvement in the first weeks. Evidence for objective improvement with steroids has been
indicated as a weak recommendation [32]. There is no evidence to support the use of antibacterials, antifungals, anti-
inflammatory injections or herbal medications in the improvement of olfactory results [32]. Since the medical
treatment after surgery is a short-term rehabilitation support, there are no studies with higher levels of evidence that
support olfactory improvement for longer periods, nor has the clinical characteristics of patients with chronic
rhinosinusitis been discriminated in other studies. operated by nasal polyposis with olfactory alterations and the
topical or oral treatment used [32]. Being an emergent association of care and follow-up by Otolaryngologists,
further studies are needed in Latin America for the characterization of patients with chronic rhinosinusitis with nasal
polyposis and olfactory disorders associated.
6. Conclusion
Nasal polyposis associated with chronic rhinosinusitis with olfactory alterations is a frequent pathology in the
otorhinolaryngology consult, whose study and follow-up must involve an adequate clinical and physical
examination to rule out other alterations associated with the chronic rhinosinusal process. Although in Latin
America there is no validated tool in the objective study of olfactory alterations, some tests such as olfactometry like
Journal of Surgery and Research 6
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
BAST 24 could be extrapolated and validated in the Hispanic population. There are still controversies in the
postoperative medical treatment of patients with chronic rhinosinusitis and nasal polyposis. Larger epidemiological
and olfactometric studies in the Latin population are required in the field of olfactory disorders.
References
1. Litvack JR, Mace JC, Smith TL. Olfactory function and disease severity in chronic rhinosinusitis. Am J
Rhinol Allergy 23 (2009): 139-144.
2. Soler ZM, Mace J, Smith TL. Symptom-based presentation of chronic rhinosinusitis and symptom specific
outcomes after endoscopic sinus surgery. Am J Rhinol 22 (2008): 297-301.
3. Banglawala SM, Oyer SL, Lohia S, et al. Olfactory outcomes in chronic rhinosinusitis with nasal polyposis
after medical treatments: A systematic review and meta-analysis. Int Forum Allergy Rhinol 4 (2014): 986-
994.
4. Jiang RS, Lu FJ, Liang KL, et al. Olfactory function in patients with chronic rhinosinusitis before and after
functional endoscopic sinus surgery. Am J Rhinol 22 (2008): 445-448.
5. Hugh SC, Siu J, Hummel T, et al. Olfactory testing in children using objective tools: comparison of Sniffin’
Sticks and University of Pennsylvania Smell Identification Test (UPSIT). J Otolaryngol Head Neck Surg 1
44 (2015): 10.
6. Croy I, Zehner C, Larsson M, et al. Test-retest reliability and validity of the Sniffin’ TOM odor memory
test. Chem Senses 40 (2015): 173-179.
7. Cardesin A, Alobid I, Benítez P, et al. Barcelona Smell Test-24 (BAST-24): Validation and smell
characteristics in the healthy Spanish population. Rhinology 44 (2006): 83-89.
8. Alobid I, De Haro J, Bernal-Sprekelsen MS, et al. Epidemiologic study of smell in the Catalan population.
Otolaryngology Head and Neck Surgery 135 (2006): 26.
9. Larsson M, Finkel D, Pedersen N. Odor identification:Influences of Age, Gender, Cognition, and
personality. J Gerontol 55 (2000): 304-310.
10. Hummel T, Welge-Luessen A. Assessment of olfactory function. Adv Otorhinolaryngol 63 (2006): 84-98.
11. De Haro J, Hernandez A, Benítez P, et al. Smell disorders as early diagnosis in the early stage of sinonasal
polyposis. Acta Otorrinolaringol Esp 61 (2010): 209-214.
12. Fokkens W, Lund V, Mullol J. Chronic rhinosinusitis with or without nasal polyps. Rhinology Supplement
1 (2007): 8-9.
13. Vento SI, Simola M, Ertama LO, et al. Sense of smell in long-standing nasal polyposis. Am J Rhinol 15
(2001): 159-163.
14. Rudmik L, Smith TL. Olfactory improvement after endoscopic sinus surgery. Curr Opin Otolaryngol Head
Neck Surg 20 (2012): 29-32.
15. Hornung DE. Nasal anatomy and the sense of smell. Eds.: Hummel T, Welge-Lussen A. Taste and smell:
an update. Basel, Karger Adv Otorhinolaringology (2006): 1-22.
Journal of Surgery and Research 7
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
16. Schiffman SS, Wedral E. Contribution of taste and smell losses to the wasting syndrome. Age Nutr 7
(1996): 106-120.
17. Hox V, Bobic S, Callebaux I, et al. Nasal obstruction and smell impairment in nasal polyp disease:
Correlation between objective and subjective parameters. Rhinology 48 (2010): 426-432.
18. Seiden AM, Duncan HJ. The diagnosis of a conductive olfactory loss. Laryngoscope 111 (2001): 9-14.
19. Litvack JR, Fong K, Mace J, et al. Predictors of olfactory dysfunction in patients with chronic
rhinosinusitis. Laryngoscope 118 (2008): 2225-2230.
20. Schiffman SS. Taste and smell in disease. N Engl J Med 308 (1983): 1275-1278.
21. Bachert C, Hormann K, Mosges R, et al. An update on the diagnosis and treatment of sinusitis and nasal
polyposis. Allergy 58 (2003): 176-191.
22. Bromley SM. Smell and taste disorders: A primary care approach. Am Fam Physician 61 (2000): 427-438.
23. Konstantinidis I, Triaridis S, Printza A, et al. Olfactory dysfunction in nasal polyposis: Correlation with
computed tomography findings. ORL J Otorhinolaryngol Relat Spec 69 (2007): 226-232.
24. Li C, Yousem DM, Doty RL, et al. Evaluation of olfactory deficits by medical imaging. Ed.: Doty RL.
Handbook of olfaction and gustation. New York, Dekker, (1995): 395-419.
25. Andre RF Vuyk HD, Ahmed A, Graamans K, et al. Correlation between subjective and objective
evaluation of the nasal airway. A systematic review of the highest level of evidence. Clin Otolaryngol 34
(2009): 518-525.
26. Snow JB. Clinical evaluation of disorders of the sense of smell. Eds.: Kurihara K, Suzuki N, Ogawa H.
Olfaction and taste XI: proceedings of the 11th International Symposium on Olfaction and Taste and of the
27th Japanese Symposium on Taste and Smell: joint meeting held at Kosei-nenkin Kaikan, Sapporo, Japan,
July 12-16, 1993. Tokyo: Springer-Verlag (1994): 605-608.
27. Solomon GS, Petrie WM, Hart JR, et al. Olfactory dysfunction discriminates Alzheimer's dementia from
major depression. J Neuropsychiatry Clin Neurosci 10 (1998): 64-67.
28. Cardesin A, Alobid I, Benitez P, et al. Barcelona Smell Test-24 (BAST-24): Validation and smell
characteristics in the healthy Spanish population. Rhinology 44 (2006): 83-89.
29. Perry BF, Kountakis SE. Subjective improvement of olfactory function after endoscopic sinus surgery for
chronic rhinosinusitis. Am J Otolaryngol 24 (2003): 366-369.
30. Min YG, Yun YS, Song BH, et al. Recovery of nasal physiology after functional endoscopic sinus surgery:
olfaction and mucociliary transport. ORL J Otorhinolaryngol Relat Spec 57 (1995): 264-268.
31. Wu D, Bleier BS, Wei Y. Temporary olfactory improvement in chronic rhinosinusitis with nasal polyps
after treatment. Eur Arch Otorhinolaryngol 275 (2018): 2193-2202.
32. Banglawala SM, Oyer SL, Shivangi L, et al. Olfactory outcomes in chronic rhinosinusitis with nasal
polyposis after medical treatments: A systematic review and meta-analysis. Int Forum Allergy Rhinol 4
(2014): 986-994.
Journal of Surgery and Research 8
J Surg Res 2019; 2 (1): 001-009 DOI: 10.26502/jsr.10020011
Citation: Melissa Castillo-Bustamante, Diego Bustamante-Mesa, Wilson Bustamante-Hernandez, Stella Maris
Cuevas. Chronic Rinosinusitis with Nasal Polyposis and Smell Disorders One Emergent Association. Journal of
Surgery and Research 2 (2019): 1-9.
This article is an open access article distributed under the terms and conditions of the
Creative Commons Attribution (CC-BY) license 4.0
Journal of Surgery and Research 9
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elce4012 4Document8 pagesElce4012 4ameerNo ratings yet
- JJAU BookletFinal 20150927 LQDocument5 pagesJJAU BookletFinal 20150927 LQYasuhito NumamuraNo ratings yet
- A Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaDocument11 pagesA Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaFortune JournalsNo ratings yet
- Avsm 004Document7 pagesAvsm 004Fortune JournalsNo ratings yet
- Chemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFDocument17 pagesChemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFFortune JournalsNo ratings yet
- Cerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFDocument8 pagesCerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFFortune JournalsNo ratings yet
- Capsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFDocument18 pagesCapsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFFortune JournalsNo ratings yet
- Biomineralogy of Angiogenesis PDFDocument7 pagesBiomineralogy of Angiogenesis PDFFortune JournalsNo ratings yet
- Cancer Therapyinduced Cardiotoxicity Where Are We Now PDFDocument8 pagesCancer Therapyinduced Cardiotoxicity Where Are We Now PDFFortune JournalsNo ratings yet
- Biochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFDocument16 pagesBiochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFFortune JournalsNo ratings yet
- Nischay Baghel Response CurveDocument21 pagesNischay Baghel Response CurveManish TandanNo ratings yet
- Cyber Terrorist ManualDocument35 pagesCyber Terrorist Manualdea187No ratings yet
- JR - English Practice - Qps.apDocument20 pagesJR - English Practice - Qps.apnsmviiif08chakravarthyygsNo ratings yet
- Seguridad en Nuestra Vidas SAFESTARTDocument19 pagesSeguridad en Nuestra Vidas SAFESTARTEfrain ZeballosNo ratings yet
- Bread and Pastry NC II CGDocument22 pagesBread and Pastry NC II CGrayna JUHAILINo ratings yet
- 1000 Puzzle Series Set - 1 To 25 Merged PDFDocument417 pages1000 Puzzle Series Set - 1 To 25 Merged PDFSangam ChauhanNo ratings yet
- Blue Chips Bags 4 Gold, 15 Silver, 1 Bronze Medals in ArcheryDocument1 pageBlue Chips Bags 4 Gold, 15 Silver, 1 Bronze Medals in ArcheryRodel Novesteras ClausNo ratings yet
- Solutions For Shrink Packaging FilmsDocument2 pagesSolutions For Shrink Packaging FilmsalfredoNo ratings yet
- ch1 - Part 2Document13 pagesch1 - Part 2Vivvian Grace M MolahidNo ratings yet
- The Spider and The Beehive Folk Fairy TalesDocument27 pagesThe Spider and The Beehive Folk Fairy TalesAleksandra VuNo ratings yet
- Enviando English For You NowDocument283 pagesEnviando English For You NowCarlos Vargas100% (1)
- Visit To PenthouseDocument12 pagesVisit To PenthouseTiu TonNo ratings yet
- Animal Nutrition 21-22Document12 pagesAnimal Nutrition 21-22lowkeydeadNo ratings yet
- ID Strategi Pengembangan Usahatani Ubi Kayu Manihot Utilissima Di Kecamatan MenggalDocument9 pagesID Strategi Pengembangan Usahatani Ubi Kayu Manihot Utilissima Di Kecamatan MenggalBukhori Thomas EdvanNo ratings yet
- Catalogue - Cambridge Exams Resources MaterialDocument162 pagesCatalogue - Cambridge Exams Resources MaterialBrinzea Laura100% (1)
- Carson Crash LawsuitDocument5 pagesCarson Crash LawsuitABC Action NewsNo ratings yet
- COA RulesDocument22 pagesCOA RulesNoraiza Mae Keith TalbinNo ratings yet
- Anurag Gautam (Policy)Document1 pageAnurag Gautam (Policy)Aravind AravindNo ratings yet
- CorrosionDocument20 pagesCorrosionDhruv SharmaNo ratings yet
- Sample School Report CardDocument12 pagesSample School Report CardMuradxan NovruzovNo ratings yet
- DTMF Controlled Robot Without MicrocontrollerDocument4 pagesDTMF Controlled Robot Without MicrocontrollershanofaNo ratings yet
- CH 7 Timers, Counters, T/C Applications 1Document67 pagesCH 7 Timers, Counters, T/C Applications 1tino pawNo ratings yet
- CSC321 Image ProcessingDocument5 pagesCSC321 Image ProcessingMag CreationNo ratings yet
- 10 CarbohydratesDocument6 pages10 CarbohydratesBryanNo ratings yet
- High Lateral Tension AbdominoplastyDocument14 pagesHigh Lateral Tension AbdominoplastyAhmad Arbi AninditoNo ratings yet
- A Comprehensive Review of The Present and Future Antibiotic Susceptibility Testing Ast SystemsDocument9 pagesA Comprehensive Review of The Present and Future Antibiotic Susceptibility Testing Ast SystemsrehanaNo ratings yet
- BackStop - Sma09047Document18 pagesBackStop - Sma09047Diego PalaciosNo ratings yet
- Chemistry Paper 1 - 2018-2003 - QP PDFDocument539 pagesChemistry Paper 1 - 2018-2003 - QP PDFal_helu26No ratings yet