Professional Documents
Culture Documents
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
Uploaded by
pricillyaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
Uploaded by
pricillyaCopyright:
Available Formats
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 12 Ver. I (December. 2016), PP 46-49
www.iosrjournals.org
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-
Diagnostic Dilemma
Dr. R. Rama Krishna Naik,M.S1,Dr.Sarada M.S2,Dr.V.Sureka3
1,2
Associate Professor Of General Surgery Department, Kurnool Medical College, Kurnool.
3
Postgraduate In General Surgery Department, Kurnool Medical College, Kurnool.
Abstract: Small bowel injuries are the third most common injuries in BAT, occur in less than 1% of the BAT
patients. [1,2]. Isolated jejunal perforation (IJP) in blunt abdominal trauma (BAT) is uncommon and most often
seen after motor vehicle accidents. There are higher chances of missing IJP in BAT, as majority of cases are
due to solid organ injury, which are managed conservatively, and thus there is delay in diagnosis of IJP,
leading to significant morbidity and mortality. Our study is a retrospective analysis of 20 patients, conducted at
government general hospital, Kurnool, for duration of one year, sharing our experience regarding management
of IJP in Blunt abdominal trauma patients. Exploratory laparotomy was performed and cases were managed
accordingly. The diagnosis of traumatic IJP is challenging. For most favourable results, strict monitoring, high
index of clinical suspicion and the help of available appropriate diagnostic tools like DPL/FAST are mandatory.
Keywords: Abdomen; blunt trauma; injuries; intestinal tract; jejunum
I. Introductione
Isolated jejunal perforation (IJP) in blunt abdominal trauma (BAT) is uncommon and most often seen
after motor vehicle accidents. Small bowel injuries are the third most common injuries in BAT, occur in less
than 1% of the BAT patients. [1,2]
Mechanisms of small bowel injuries with blunt trauma include shearing forces, compression forces and
bursting injury. Punctate or slit like perforations often occurring on the antimesenteric border are the
consequences of raised intraluminal pressure in a fluid or air filled loops of bowel referred as blow out
perforations.[3]
II. Aims and objectives
Incidence of IJP in BAT is infrequent; the objective of this work is to review our experience and
describe the clinical presentation of IJP.
III. Methods
20 patients diagnosed with IJP in BAT between August 2014 to June 2016 in the department of General
Surgery, GGH, Kurnool, were retrospectively reviewed in order to share our experience with IJP. Exploratory
laparotomy was performed and cases were managed accordingly.
Data obtained from 20 cases included demographics and clinical features, examined for significant
findings such as abdominal pain, vomiting, fever , and the relevant investigations were done.
IV. Results
Between July 2014 to July 2016, 20 patients (14 males, 6 females; average age – 35yrs range 25 to
45yrs) were diagnosed with IJP in BAT.
Mode of injury in 15 patients is road traffic accidents and in remaining 5 patients is assault. 7 patients
presented immediately (1-2hours), 5 patients presented after 6hrs, 5 patients presented after 12hrs and 3 patients
presented 24hrs after blunt abdominal trauma to our hospital.
Pain abdomen is the leading symptom in all 20 patients. Clinically Bruises noted in anterior abdominal
wall in 4 patients and abdominal tenderness was the commonest finding in all patients.
X-ray erect abdomen was done in all patients, pneumoperitoneum detected in 4 patients and the
remaining patients were started on conservative treatment and CECT abdomen was planned. Ultrasound
abdomen was done in all patients it is normal in 7 patients who presented immediately after BAT, in rest of the
patients free fluid noted in peritoneal cavity. CECT abdomen done in selected cases (16 cases); who were
planned for conservative management. In 13 cases pneumoperitoneum and free fluid noted; only free fluid noted
in 3 cases.Laparotomy was done in all cases. 2 cases required resection and anastomosis and remaining cases
primary closure of IJP done. Wound infection was noted in 7 patients, which was treated accordingly.
Postoperative stay period on an average was around 10 days.
DOI: 10.9790/0853-1512014649 www.iosrjournals.org 46 | Page
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
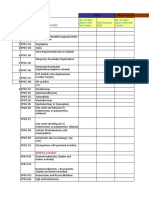
Clinical data of twenty patients with IJP in BAT
Timing
of
Mode Timing of X-ray USG
S. Age Symptom CECT diagnosis
Sex of presentati erect abdome Treatment
no (yr) s abdomen after
injury on (hrs) abdomen n
BAT
(hrs)
Pain Free Primary
1 25 F RTA 6 NAD Free fluid 16
abdomen fluid closure
Free Primary
2 28 F RTA Immed Pain NAD Free fluid 10
fluid closure
Resection
Pain +
Assaul Pneumoperi Free &
3 32 M 24 fever + Not done 26
t toneum fluid Anastomosi
distension
s
Free Pneumo & Primary
4 26 M RTA 6 Pain NAD 18
fluid free fluid closure
Primary
5 45 M RTA Immed Pain NAD NAD Free fluid 8
closure
Pain + Free Primary
6 40 M RTA 12 NAD Free fluid 18
fever fluid closure
Assaul Primary
7 29 M 6 Pain NAD NAD Free fluid 16
t closure
Primary
8 37 M RTA Immed Pain NAD NAD Free fluid 9
closure
Pain + Free Primary
9 34 F RTA 12 NAD Free fluid 20
fever fluid closure
Primary
10 36 M RTA Immed Pain NAD NAD Free fluid 10
closure
Pain Free Primary
12 45 M RTA 6 NAD Free fluid 17
abdomen fluid closure
Assaul Pain Pneumo & Primary
13 25 M Immed NAD NAD 10
t abdomen free fluid closure
Pain, Resection
vomiting, Pneumoperi Free &
14 27 F RTA 24 Not done 26
fever, toneum fluid Anastomosi
distension s
Primary
15 29 F RTA Immed Pain NAD NAD Free fluid 11
closure
Pneumo & Primary
16 33 M RTA 6 Pain NAD NAD 18
free fluid closure
Pain,
Assaul Free Pneumo & Primary
17 32 F 12 vomiting, NAD 19
t fluid free fluid closure
fever
Pain,
Pneumoperi Free Primary
18 34 M RTA 12 vomiting, Not done 18
toneum fluid closure
fever
Pain,
Assaul Pneumoperi Free Primary
19 28 F 24 vomiting, Not done 26
t toneum fluid closure
fever
Free Primary
20 30 M RTA Immed Pain NAD Free fluid 9
fluid closure
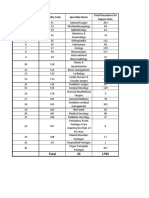
30
25
20
15 timing of
10 presentation
5
timing of diagnosis
0
category category category category
1 (1-2 2 (6hrs) 3 4
hrs) (12hrs) (24hrs)
DOI: 10.9790/0853-1512014649 www.iosrjournals.org 47 | Page
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
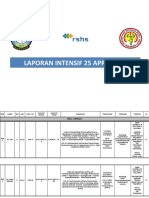
Intra operative images
V. Conclusion
The diagnosis of traumatic IJP is challenging, as the signs and symptoms of peritonitis appear in a later
time. Physical examination was found to be reliable only in 30% of BAT cases.[1]. The presence of
pneumoperitoneum in erect X-ray abdomen after traumatic small bowel injury is the exception rather than the
rule. CECT abdomen is the gold standard investigation for the assessment of BAT.
A high index of suspicion, repeated clinical examination and proper utilization of investigational tools
definitely helps in diagnosing these cases at an earlier period.
Although there is no consensus in the literature regarding the effects of delay in treatment of small
bowel injury in BAT, the widely accepted position is that the sooner treated, the lower the morbidity for the
patient.
VI. Discussion
Seventy-five percent of the blunt abdominal trauma cases are caused by motor vehicle accidents [4].
Although small bowel injuries have been reported to be the third most common injuries in blunt abdominal
trauma, they occur in less than 1% of the blunt trauma patients [5,6] . The mechanisms of small bowel injuries
with blunt trauma include shearing forces, compression between the abdominal wall and the vertebral column
DOI: 10.9790/0853-1512014649 www.iosrjournals.org 48 | Page
Isolated Jejunal Perforation Following Blunt Abdominal Trauma-Diagnostic Dilemma
and bursting injury due to a sudden increase in the intraluminal pressure. The isolated “blowout type” of rupture
of the jejunum following constriction by a dhoti or fall from the stairs is extremely uncommon. This leads to a
sudden increase in the intra-abdominal pressure, which in association with a full stomach, can lead to this kind
of perforation. A similar mechanism of small bowel injury was caused by physical assault [7] and knee kick [8]
during a game of foot ball.
Physical examination is not adequate on its own for the diagnosis of such cases, and it was found to be
reliable in only 30% of the blunt trauma cases [4]. Fakhry et al [9] observed that 67.7% out of 198 patients with
blunt small bowel injury, initially presented with signs or symptoms which were highly suggestive of
perforative peritonitis and 84.3% were taken to the operating room without delay. X ray of the erect abdomen,
USG, diagnostic peritoneal lavage and CT of the abdomen are most commonly used diagnostic aids other than
physical examination. According to Burney et al [10], peritoneal lavage has proven to be sensitive for the
demonstration of the haemoperitoneum, but it was found to be less reliable in the early diagnosis of intestinal
injuries. The gold standard for the assessment of blunt trauma diagnosis is C T scanning, with a sensitivity of
92% and a specificity of 94%. In recent times, laparoscopy has played an important role in the diagnosis as well
as in the treatment of blunt abdominal trauma. Diagnostic laparoscopy should be preferred instead of diagnostic
peritoneal lavage in relatively haemodynamically stable patients. Most of the patients will be having punctuate
or slit like perforations on the anti mesenteric border and so, ideally they require laparotomy and the primary
closure of the perforation, with peritoneal lavage. Now, with the advent of laparoscopy, it is possible to close the
perforation by using endosutures or staplers[11].
Small bowel perforation has low mortality and complication rates if it is treated before 24 hours after
the injury [7]. Delayed jejunal perforation is often associated with high mortality and morbidity. Since 1990, 9
cases of isolated jejunal perforations have been reported , but the nature of the injury which was seen in our
cases was different.
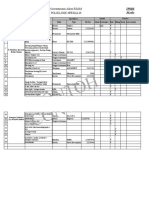
S.No Year Author No. of cases Nature of injury
1 1993 W K Chiang et al 1 Blunt injury
2 1994 J M Lindenmann et al 1 Blunt injury
3 2004 H Razali et al 1 Blunt injury
4 2006 I A Munshi et al 1 Blunt injury
5 2007 A K Coskun et al 1 Knee kick
6 2010 Kostantinidis C et al 1 Assault
7 2010 A Baccoli et al 3 Blunt injury
Clinical observation was not sufficient to justify the diagnosis and so the pre operative diagnosis of
isolated jejunal perforation was definitely challenging. A high index of suspicion, repeated clinical examinations
and the utilization of imaging modalities really helped us to diagnose these kinds of clinical entities.
References
[1]. Chiang WK. Isolated jejunal perforation from nonpenetrating abdominal trauma. Am J Emerg Med 1993;11:473-5.
[2]. Robbs JV ,Moore SW ,Pillay SP.Blunt abdominal trauma with jejunal injury: A review. J Trauma 1980;20:308-11.
[3]. Munshi IA, DiRocco JD,Khanchi G. Isolated jejunal perforation after blunt thoracoabdominal trauma. J Emerg Med 2006;30:393-5.
[4]. Griswold RA, Collier HS. Blunt abdominal trauma. Int Abstr Surg 1961;112:309-29.
[5]. Allen GS, Moore FA, Cox CS Jr, Wilson JT, Cohn JM, Duke JH. Hollow visceral injury and blunt trauma. J Trauma 1998;45:69-
78.
[6]. Neugebauer H, Wallenboeck E, Hungerford M. Seventy cases of injuries of the small intestine caused by blunt abdominal trauma: A
retrospective study from 1970 to 1994. J Trauma 1999;46:116-21.
[7]. Kostantinidis C, Pitsinis V, Fragulidis G. Isolated jejunal perforation following blunt abdominal trauma. Ulus Travma Acil Cerrahi
Derg 2010; 16:87-89.
[8]. Lindenmann JM, Schmid D, Akovbiantz A. Jejunal perforation following blunt abdominal trauma. Schweiz Rundsch Med Prax
1994; 83:857-60.
[9]. Fakhry SM , Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays [8 hours] produce morbidity and
mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J
Trauma. 2000; 48:408-15.
[10]. Burney RE, Mueller GL, Coon WW, Thomas EJ, Mackenzie JR. Diagnosis of isolated small bowel injury following blunt
abdominal trauma. Ann Emerg Med 1983; 12:71-74.
[11]. Townsend MS, Pelias ME. A technique for the rapid closure of traumatic small intestinal perforation without resection. Am J Surg
1992; 164:171-72.
DOI: 10.9790/0853-1512014649 www.iosrjournals.org 49 | Page
You might also like
- The Arthroscopy Book PDFDocument478 pagesThe Arthroscopy Book PDFSara Perez Pastrana100% (1)
- Naturalised Birds of The WorldDocument353 pagesNaturalised Birds of The Worldaromero888100% (5)
- Nursing Care Plan: Short Term: Difficulty in Swallowing Nursing Diagnosis Planning Implementation Rationale EvaluationDocument6 pagesNursing Care Plan: Short Term: Difficulty in Swallowing Nursing Diagnosis Planning Implementation Rationale EvaluationNico Angelo Hibaya TugononNo ratings yet
- 189 Gotera, Chloe Lynn - Week 8 Day 3Document5 pages189 Gotera, Chloe Lynn - Week 8 Day 3Chloe GoteraNo ratings yet
- OT List 25-10-2023Document4 pagesOT List 25-10-2023ArhanNo ratings yet
- IMA NHB Suggested Package Amount For Negotiation With Insurance CompaniesDocument5 pagesIMA NHB Suggested Package Amount For Negotiation With Insurance Companiesmonikparmar1No ratings yet
- 189 Gotera, Chloe Lynn - HPS DAY 2Document7 pages189 Gotera, Chloe Lynn - HPS DAY 2Chloe GoteraNo ratings yet
- Doctor's Order SampleDocument3 pagesDoctor's Order SampleXerxes DejitoNo ratings yet
- Parashospitaltriff PDFDocument96 pagesParashospitaltriff PDFBajane wala baba बजाने वाला बाबाNo ratings yet
- History FormDocument5 pagesHistory FormYazeed AsrawiNo ratings yet
- Utilization Form AND Proposed Rates FormDocument18 pagesUtilization Form AND Proposed Rates FormArunNo ratings yet
- 189 Gotera, Chloe Lynn Activity 2 Day 2 Sigmoid VolvulusDocument6 pages189 Gotera, Chloe Lynn Activity 2 Day 2 Sigmoid VolvulusChloe GoteraNo ratings yet
- Pediatric Cardiology: Original ArticlesDocument5 pagesPediatric Cardiology: Original ArticlesAdrian KhomanNo ratings yet
- Ayushman Bharat General Surgery List 4Document3 pagesAyushman Bharat General Surgery List 4Rahul SakalleNo ratings yet
- Pre Operative Planning MONDAY, December 31 2018: Resident On DutyDocument17 pagesPre Operative Planning MONDAY, December 31 2018: Resident On DutyRakhmad HidayatNo ratings yet
- Laporan Nccu 11012022 SMDocument24 pagesLaporan Nccu 11012022 SMbobirfansyahputraNo ratings yet
- CCU 2017 AntiplateletDocument22 pagesCCU 2017 AntiplateletDhinie NovianiNo ratings yet
- Peralatan Medis Periode Tahun 2015: NO Nama Alat Medis Unit Kerja JumlahDocument2 pagesPeralatan Medis Periode Tahun 2015: NO Nama Alat Medis Unit Kerja JumlahMyke RumapeaNo ratings yet
- Vaga Hospital - LUC005 - Care HelthDocument7 pagesVaga Hospital - LUC005 - Care HelthjaipalNo ratings yet
- Laparoscopic in TraumaDocument37 pagesLaparoscopic in TraumaronaldNo ratings yet
- Clinical History of Cardiopulmonary Resuscita: Update On Cardiopulmonary ResuscitationDocument13 pagesClinical History of Cardiopulmonary Resuscita: Update On Cardiopulmonary ResuscitationDennis Nabor Muñoz, RN,RMNo ratings yet
- CD ListDocument80 pagesCD ListOFC accountNo ratings yet
- 189 Gotera, Chloe Lynn M. Thyroid Cancer Day 2Document13 pages189 Gotera, Chloe Lynn M. Thyroid Cancer Day 2Chloe GoteraNo ratings yet
- All PackageRates (ABPMJAY) PDFDocument300 pagesAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- Friday 11-5-2019 Emfisema SubcutisDocument13 pagesFriday 11-5-2019 Emfisema SubcutisJefri SusantoNo ratings yet
- Laparoscopic Ureterolithotomy For Ureteral Calculi: European UrologyDocument5 pagesLaparoscopic Ureterolithotomy For Ureteral Calculi: European Urologysunshine bloomNo ratings yet
- April Mortality & Morbidity ReviewDocument31 pagesApril Mortality & Morbidity ReviewAsfaw NurhussenNo ratings yet
- Course in The Ward: Date and Time Focus Doctor's Order Nurses Note August 28, 2018 3:50PM Vital Signs: AdmissionDocument4 pagesCourse in The Ward: Date and Time Focus Doctor's Order Nurses Note August 28, 2018 3:50PM Vital Signs: AdmissionMartin T ManuelNo ratings yet
- Surgery 23 Surgery 1 Surgery - 44 2 Debridement-23 Appendectomy-22Document1 pageSurgery 23 Surgery 1 Surgery - 44 2 Debridement-23 Appendectomy-22Lodi PetmaluNo ratings yet
- Ny - Herlina/20 THN: No - Nama/Umursubyektifobyektifa S S E S M E N Tplanningk E T E R A N G A N 1 ADocument17 pagesNy - Herlina/20 THN: No - Nama/Umursubyektifobyektifa S S E S M E N Tplanningk E T E R A N G A N 1 ANafilah SyellaNo ratings yet
- Format Inventaris Alkes Lab RSAMDocument4 pagesFormat Inventaris Alkes Lab RSAMAbyan TaufikNo ratings yet
- 9 Extension: (7) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document8 pages9 Extension: (7) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnNo ratings yet
- Laporan Jaga Igd: Rsud Adhiyatma, MPH Coass Bedah UnimusDocument27 pagesLaporan Jaga Igd: Rsud Adhiyatma, MPH Coass Bedah UnimusDony Hamonangan SiregarNo ratings yet
- March 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADDocument3 pagesMarch 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADJhon PauloNo ratings yet
- (Trauma) 01 - 07 - 2023 - Ny. Furi - Vulnus Laceratum With Avultion Nail Digiti IV Manus DextraDocument14 pages(Trauma) 01 - 07 - 2023 - Ny. Furi - Vulnus Laceratum With Avultion Nail Digiti IV Manus DextraRasyidu MashuriNo ratings yet
- Yellow Team Census 4 - 16 - 22Document10 pagesYellow Team Census 4 - 16 - 22Ardy Antonio MDNo ratings yet
- Torsion Tunica Vaginalis FlapDocument7 pagesTorsion Tunica Vaginalis FlapSinbijeo GinNo ratings yet
- ICU Progress NoteDocument7 pagesICU Progress NoteDiana Hylton100% (1)
- Curriculum Vitae: Lulus Handayani, MDDocument31 pagesCurriculum Vitae: Lulus Handayani, MDpisangphoeNo ratings yet
- Monthly-Census-February-2022 SEMIFINALDocument13 pagesMonthly-Census-February-2022 SEMIFINALApmc SchwartzNo ratings yet
- Daily Preop Kamis DianDocument8 pagesDaily Preop Kamis DianpogimudaNo ratings yet
- Abdomen Blunt Trauma 2 - 3 - 2020Document6 pagesAbdomen Blunt Trauma 2 - 3 - 2020Iqra NazNo ratings yet
- Anatomy Radio: AbdomenDocument10 pagesAnatomy Radio: AbdomenMonique BorresNo ratings yet
- AECP - Chest PainDocument7 pagesAECP - Chest PainBenny TrisaktyariNo ratings yet
- Name: Mohammad Turhan Pathan Group:5 Gene of Interest: BMP1 in STADDocument9 pagesName: Mohammad Turhan Pathan Group:5 Gene of Interest: BMP1 in STADTurhan PathanNo ratings yet
- RSI ChecklistDocument2 pagesRSI ChecklistKyra PoggenpoelNo ratings yet
- A - Onkologi Obgin: 22 Januari 2024Document1 pageA - Onkologi Obgin: 22 Januari 2024Hartomo BenxNo ratings yet
- Course in The Wards FormatDocument2 pagesCourse in The Wards FormatJade MonrealNo ratings yet
- Laporan Intensif 25 April 2021Document21 pagesLaporan Intensif 25 April 2021bosnia agusNo ratings yet
- Mrs. I/ 38 Y.o/ w.8 Chief Complaint: History of Present IllnessDocument19 pagesMrs. I/ 38 Y.o/ w.8 Chief Complaint: History of Present IllnessIka AyuNo ratings yet
- Ayushman Bharat General Surgery List 1Document3 pagesAyushman Bharat General Surgery List 1Rahul SakalleNo ratings yet
- Rtog 0813 Marina CousinsDocument22 pagesRtog 0813 Marina Cousinsapi-426094285No ratings yet
- Clinical Profile of Patients Presented With Post Traumatic Vision Loss in A Tertiary Care CentreDocument4 pagesClinical Profile of Patients Presented With Post Traumatic Vision Loss in A Tertiary Care CentreIJAR JOURNALNo ratings yet
- Schneider1992 (Biopsia A Todos)Document5 pagesSchneider1992 (Biopsia A Todos)ouf81No ratings yet
- Thyroid StormDocument35 pagesThyroid StormZulfanaNo ratings yet
- 9 Extension: (8) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document7 pages9 Extension: (8) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnNo ratings yet
- Emergency Case TemplateDocument46 pagesEmergency Case TemplateJacky JunaediNo ratings yet
- Medicine FMGE Sprint by Dr. Santosh Patil (PW Med Ed)Document31 pagesMedicine FMGE Sprint by Dr. Santosh Patil (PW Med Ed)Stella ParkerNo ratings yet
- 5 6305127245975389215Document21 pages5 6305127245975389215dicky goradinataNo ratings yet
- Commonicd10procedurecodes State1911Document1 pageCommonicd10procedurecodes State1911Monika Putong PaatNo ratings yet
- 10 Respiratory System 2Document120 pages10 Respiratory System 2rosalyn gaboniNo ratings yet
- Percutaneous Treatment of Left Side Cardiac Valves: A Practical Guide for the Interventional CardiologistFrom EverandPercutaneous Treatment of Left Side Cardiac Valves: A Practical Guide for the Interventional CardiologistCorrado TamburinoNo ratings yet
- Atlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrom EverandAtlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrieder BerrNo ratings yet
- Bottari2020 PDFDocument5 pagesBottari2020 PDFpricillyaNo ratings yet
- Intestinal Perforation: BackgroundDocument5 pagesIntestinal Perforation: BackgroundpricillyaNo ratings yet
- Intestinal Perforation Clinical Presentation: HistoryDocument2 pagesIntestinal Perforation Clinical Presentation: HistorypricillyaNo ratings yet
- Single Jejunal Blowout Perforation Following Blunt Abdominal Trauma: Diagnostic DilemmaDocument3 pagesSingle Jejunal Blowout Perforation Following Blunt Abdominal Trauma: Diagnostic DilemmapricillyaNo ratings yet
- Short Case TraumaDocument19 pagesShort Case TraumapricillyaNo ratings yet
- Short Case (Trauma) : Ayu Dahniar K1A1 11002Document19 pagesShort Case (Trauma) : Ayu Dahniar K1A1 11002pricillyaNo ratings yet
- Delayed Presentation of Isolated Jejunal Perforation Following Accidental TraumaDocument2 pagesDelayed Presentation of Isolated Jejunal Perforation Following Accidental TraumapricillyaNo ratings yet
- LycopodiumDocument1 pageLycopodiumRoger Knight100% (11)
- Instructions For Use: DescriptionDocument32 pagesInstructions For Use: DescriptionHugo MoralesNo ratings yet
- Cattle Dehorning - Questions and AnswersDocument5 pagesCattle Dehorning - Questions and AnswersAfan Syafi'iNo ratings yet
- WBC CastsDocument41 pagesWBC CastspikachuNo ratings yet
- Nn. CranialesDocument3 pagesNn. CranialesFaisal Yusuf AzhariNo ratings yet
- The AASM Manual For The Scoring of Sleep and Associated EventsDocument136 pagesThe AASM Manual For The Scoring of Sleep and Associated EventsSerkan KüçüktürkNo ratings yet
- Coltene BrochureDocument4 pagesColtene BrochureHenryScheinDentalNo ratings yet
- PPHNDocument32 pagesPPHNAnonymous NeRC5JYiSNo ratings yet
- Emarking Notes On Biology SSC-II May Exam 2012Document5 pagesEmarking Notes On Biology SSC-II May Exam 2012AbdulSalam BhattiNo ratings yet
- Hematinics BPTDocument17 pagesHematinics BPTbpt2No ratings yet
- Transplantation PDFDocument18 pagesTransplantation PDFChandan Kumar100% (1)
- Eruptii CutanateDocument5 pagesEruptii CutanateIoanaNo ratings yet
- Sisters, Friends and Lovers CH 11Document5 pagesSisters, Friends and Lovers CH 11spectacularfuel82No ratings yet
- Mazuri 5E5L StudyDocument9 pagesMazuri 5E5L StudyLawrence TancincoNo ratings yet
- Urinalysis and Body Fluids 6th Edition by Susan King Strasinger - Test BankDocument45 pagesUrinalysis and Body Fluids 6th Edition by Susan King Strasinger - Test Bankroseyoung0No ratings yet
- Anatomy and Physiology of Respiratory SystemDocument6 pagesAnatomy and Physiology of Respiratory SystemMonica VelascoNo ratings yet
- Med Surg Questions Oct 25 Angela DeVarsoDocument38 pagesMed Surg Questions Oct 25 Angela DeVarsonochip10100% (1)
- Presentation Case Tuberculosis: Milda Dwi Risnandar 111170046Document26 pagesPresentation Case Tuberculosis: Milda Dwi Risnandar 111170046mildadwirisnandarNo ratings yet
- Our Lungs Are The Organs That Bring in Oxygen Into Our BodyDocument17 pagesOur Lungs Are The Organs That Bring in Oxygen Into Our BodySaidatul Atyah Mohd ApendaiNo ratings yet
- Trematodes TableDocument3 pagesTrematodes TableFarlogy88% (8)
- Renal Abscess, Xanthogranulomatous Pyelonephritis and Renal TuberculosisDocument41 pagesRenal Abscess, Xanthogranulomatous Pyelonephritis and Renal TuberculosisAnas Mk HindawiNo ratings yet
- Medical Parasitology in The Philippines (Belizario, de Leon) - Pages-307-340Document34 pagesMedical Parasitology in The Philippines (Belizario, de Leon) - Pages-307-340Mae Rose Charlene MendozaNo ratings yet
- Dr. Fairuz Quzwain, Sppa, M.Kes: Bagian Patologi Anatomi Program Studi Pendidikan Dokter Universitas JambiDocument119 pagesDr. Fairuz Quzwain, Sppa, M.Kes: Bagian Patologi Anatomi Program Studi Pendidikan Dokter Universitas JambiAlfian DaudNo ratings yet
- Kajal Vaghasia - Codominance and Incomplete Dominance WorksheetDocument6 pagesKajal Vaghasia - Codominance and Incomplete Dominance WorksheetKajal VaghasiaNo ratings yet
- Model Test 3 - Progress TestDocument1 pageModel Test 3 - Progress Testfarah zahraNo ratings yet
- Lecture 1, Introduction To EndocrinologyDocument86 pagesLecture 1, Introduction To EndocrinologyAlexandru Ionut Popistaș100% (1)
- GerdDocument34 pagesGerdmrbrutusNo ratings yet