Professional Documents
Culture Documents
Pal Ese 2011
Pal Ese 2011
Uploaded by
retta tataCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pal Ese 2011
Pal Ese 2011
Uploaded by
retta tataCopyright:
Available Formats
NAN200181.
qxd 9/6/11 2:49 AM Page 319
The Art and Science of Infusion Nursing
Alvisa Palese, MNS, RN Catia Cassin, MNS, RN
Andrea Cassone, MNS, RN Sandra Cialdella, MNS, RN
Annamaria Kulla, MNS, RN Giuseppe Floridia, MNS, RN
Sabrina Dorigo, RN Boris Nadlišek, MNS, RN
Jesse Magee, RN Annamaria Palcic, MNS, RN
Marco Artico, MNS, RN Giulia Valle, MNS, RN
Francesco Camero, MNS, RN Paola Sclauzero, MNS, RN
Factors Influencing Nurses’ Decision-Making
Process on Leaving in the Peripheral
Intravascular Catheter After 96 Hours
A Longitudinal Study
ABSTRACT at 96 hours after its positioning, in accordance with
The clinical and research debate on the peripheral the international guideline. Several factors were
intravascular (PIV) catheter length of stay in situ is taken into account in regard to replacement of the
ongoing. The principal aim of this study was to PIV catheters by nurses, ranging from analysis based
explore the factors behind a nurse’s decision to leave on their own clinical experience with PIV complica-
a PIV in place for more than 96 hours. The study tions and analysis of the patient’s clinical situation to
focused on 7 northern Italian hospitals in 2009. A the critical analysis of their own work situation. This
consequent sample of 269 PIV catheters was includ- clinical decision-making process is valuable: leaving
ed. Direct observation and interviews were adopted. the PIV in place for more than 96 hours is a complex
The time of the expected PIV replacement was fixed decision and not simply a guideline violation.
Author Affiliations: University of Udine (Mss Palese and Dorigo) and University of Udine and Trieste (Messrs Floridia, Cassone, Camero,
Nadlišek, and Artico, and Mss Cialdella, Valle, Kulla, Palcic, Sclauzero, and Cassin), Udine, Italy; and Wilmington University, Wilmington,
Delaware (Mr Magee).
Alvisa Palese is an Associate Professor in Nursing Science and a teacher in evidence-based nursing courses.
Andrea Cassone, Annamaria Kulla, Francesco Camero, Sandra Cialdella, Boris Nadlišek, and Giulia Valle are members of the nursing
team and members of the CIPE96’ Group Research team.
Sabrina Dorigo is a collaborator in research at Udine School of Nursing.
Jesse Magee is a research project assistant.
Marco Artico, Catia Cassin, Giuseppe Floridia, Annamaria Palcic, and Paola Sclauzero are members of the nursing team and members
of the CIPE96’ Group Research team.
Corresponding Author: Alvisa Palese, MNS, RN, School of Nursing, Udine University, Viale Ungheria 18, 33100 Udine, Italy
(alvisa.palese@uniud.it).
DOI: 10.1097/NAN.0b013e3182290a20
VOLUME 34 | NUMBER 5 | SEPTEMBER/OCTOBER 319
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 320
I
ntravenous therapy is frequently used in hospitalized PIV catheter within 72 to 96 hours of its positioning were
patients and the peripheral intravascular (PIV) available in the hospitals. These recommendations were
catheter is the device adopted by nurses to perform implemented during recent years with 1 or more strategies
intravenous administrations. Current guidelines rec- (eg, educational courses, sheets, brochures, and protocols)
ommend that the PIV catheter should be replaced after developed at the institutional level.
72 to 96 hours to prevent phlebitis.1 This recommendation
is ranked at level 1B (strongly recommended for implemen-
SAMPLE AND SAMPLING
tation and supported by some experimental, clinical, or epi-
demiologic studies) and is based on 1 study,2 according to
the references reported in the guideline. Notwithstanding the A consequent sample of 269 PIV catheters measuring less
contents of the guideline,1 the length of stay in situ is still than 3 inches positioned in peripheral veins was included.
debated. Recent literature3-8 and clinical practice data9 show Peripheral intravascular catheters were excluded if they
the tendency to maintain the catheter over the prescribed were in the following categories: (a) more than 3 inches
96 hours. This lack of guideline adherence seems to be sup- in length (eg, midline)10; (b) positioned in the feet; (c)
ported by several factors: (a) for nurses, it is difficult to placed in urgent or emergent conditions; (d) placed
explain to and argue with the patients about the need to during a night shift; (e) replacing previous PIV catheters;
replace a properly functioning PIV catheter4,9; (b) the (f ) used for administering lipids, chemotherapies, and
replacement may have a negative impact, such as discom- hyperosmolar solutions; (g) used in patients younger
fort and pain, on patients4; (c) the replacement might also than 18 years; or (h) if it was not possible to monitor
increase the risk of infection, because each time skin the catheter continuously until the 96th hour after posi-
integrity is breached, a potential portal for pathogens is tioning (eg, patient transferred to intensive care unit).
provided4; and (d) the recent systematic review made by
Webster and colleagues5 found no conclusive evidence in DATA COLLECTION PROCEDURES
the need for catheter replacement every 72 to 96 hours.
In their daily practice, nurses make the decision to
Direct observations of the nurse’s daily practice and an
leave the catheter in situ over the 96 hours or to replace
interview with the nurse responsible for each patient were
it. This decision is made on the basis of clinical infor-
adopted. The researchers (13 total) were appropriately
mation and circumstances as stated by Johansson and
educated with a 4-hour course focusing on the aim of the
colleagues,9 who have described under a qualitative
study and on the data collection procedures. Preliminarily,
study design combining observations and interviews,
a pilot phase observing 11 PIV catheters, not included in
the decision-making process adopted by 43 nurses in
this report, was done. Each researcher observed 10-28 PIV
their natural setting. Exploring the factors involved in
catheters and interviewed 10-28 nurses, in accordance
the decision-making process affecting the PIV catheter’s
with the number of PIV catheters observed.
length of stay in situ and capturing the variability and
richness of the nurses’ clinical decision making in prac-
tice was the general aim of this study. Observation
Each new intravenous catheter positioned was observed
AIMS 2 times per day, every 12 hours (8 times in total per
catheter) until the 96th hour after its positioning. For
Exploring the factors behind a nurse’s decision to leave a each PIV catheter, patients’ documentation was consult-
PIV catheter in place for more than 96 hours was the ed to collect data on the positioning day/hour and on
principal aim of the study. infusion(s) prescribed (eg, none, intermittent during the
first 96 hours). Direct observation was done at the bed-
side, collecting data on PIV laterality (right-/left-hand
STUDY DESIGN side), exposure (front or rear), vein site (eg, basilic,
cephalic), and catheter lumen size (mm) according to
Researchers adopted a prospective observation study design. International Organization for Standardization stan-
dards.11 When nursing records reported incomplete
data on the hour of positioning, researchers have
SETTING assumed 9:00 AM and 4:00 PM as a standard reference,
according to the ward’s routine, which scheduled new
The study took place in 2009, involving 7 hospitals (each PIV positioning at these times.
with at least 600 beds) located in northern Italy; for each
hospital, the available medical and surgical wards (N ⫽ 14), Interview
which had on average 30.3 beds (⫾10.1; range, 13-45),
were included in the study. Protocols based on the inter- The nurse responsible for the patient was interviewed 1
national guideline1 recommending the need to replace a time but with 2 different sets of questions according to the
320 Journal of Infusion Nursing
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 321
PIV length of stay in situ: (a) for the PIV catheters removed calculated. The 2 test, ANOVA test (or Student t test),
before the 96 hours, the nurse responsible was asked when and relative risk (RR) (95% confidence interval [CI]),
removal occurred, and for which reason(s); (b) for the PIV when appropriate, were calculated. The statistical signifi-
catheters present in situ at 96 hours, the nurse was asked cance level was positioned at P ⬎ .05.
the reason(s) why he or she decided to leave the catheter in Factors determining the PIV catheter removal before
place after the deadline recommended by the international the 96 hours were categorized according to the reasons
guideline,1 with the reasons ranked in priority (first, sec- reported by nurses (occlusion, phlebitis, extravasations,
ond, and third reasons). All the responses were collected by and infusion interruption); frequencies and percentages
researchers and reported exactly according to the nurse’s were then calculated.
answer. No modifications in the responses were made dur- For the PIV catheters remaining more than 96 hours,
ing the data collection process. the reasons reported by the nurses at the 96th hour were
organized on the basis of the modified categories that
emerged with Johansson and colleagues.9 For each catego-
QUANTITATIVE AND QUALITATIVE ry that emerged in the original qualitative study,9
DATA ANALYSIS researchers decided the significance to give in accordance
with the aim of this study. Then, sample answers obtained
Quantitative data were elaborated with SPSS version from the participants were appropriately included in the
18.00. For quantitative variables, average, median, stan- categories to explain each unequivocally (Table 1).9 To
dard deviations (⫾), frequencies, and proportions were avoid personal bias, this process was first conducted by
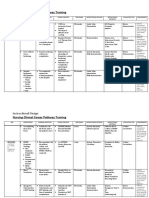
TABLE 1
Factors Determining the Decision to Leave the
Peripheral Intravascular Catheter in Place After
96 Hours: Categories Adopted and Definitions
Category Redefined by Researchers and Examples of
Main Categories9 Subcategories9 Answers Obtained at 96 Hours by Nurses’ Participanta
Individual patient situation The patient need for PIV catheter Patient does not need PIV catheter in the near future:“I left
it more than 96 hours because it would be removed soon
according to his/her clinical conditions.” (N111)
The PIV catheter’s applicability Patient does not have other veins available: “I preserved
the veins leaving the PIV in situ because if I remove it
I am not sure I would find another vein.” (N56)
Patient situation in relation to PIV catheter Patient is severely ill (morbidly), disoriented, afraid of
replacement limits injections, or does not want replacements: no
appropriate answers have emerged. (⫺)
Nurse’s work situation Time aspects PIV catheter replacement has low priority because of the
workloads: “I had to replace it today, but the workload
was high.” (N76)
Routines for planning and following up There is a lack of standardization in the PIV management:
PIV catheter “No appropriate answers have emerged.” (⫺)
Nurse’s attitudes toward PIV management The nurse is responsible for the patients: “I would give the
best individualized PIV care and for this reason, I have
decided to leave the catheter in situ.” (N5)
Experience of PIV management Experience of PIV complications Nurses have no experience of complications: “I have never
seen complications after 96 hours.” (N150)
Nurse’s capability There is a lack of capability within the nursing staff in the
insertion of the PIV: “Is better to leave the actual PIV
because we are without experts.” (N93)
Abbreviation: PIV, peripheral intravascular.
a
Number of interviews at the 96th hour (from 1 to 166).
VOLUME 34 | NUMBER 5 | SEPTEMBER/OCTOBER 2011 321
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 322
TABLE 2 TABLE 2 Continued
Characteristics of the Frequencies
Peripheral Intravascular Characteristics
Infusion prescribed
(N ⴝ 269) %
Catheter Observed No 13 4.8
Frequencies Continuously 29 10.8
Characteristics (N ⴝ 269) % Intermittently 46 17.1
Outside diameter of catheter tube10 Mixed (continuously and intermittent) 181 67.2
1.9, 2.0, 2.1, 2.2 0 … Abbreviation: PIV, peripheral intravascular.
a
Out of 103 removed before 96 hours.
1.6-1.8 4 1.5
1.2-1.3 108 40.2
1.0-1.1 117 43.5 3 researchers, who worked independently: each answer
collected was included in 1 or more categories according
0.8-0.9 38 14.1
to the framework established by Johansson and col-
Missing 2 0.7 leagues.9 Later, another researcher compared each catego-
Positioning day/hour reported in nursing records rization made by the previous researchers and prepared a
final file highlighting the discordances between the cate-
Yes 205 76.2
gories. These discrepancies were discussed and agreed on
No 64 23.7 by all the researchers, and all of the responses were then
PIV catheter permanence, h categorized in their final location appropriately.
Average ⫾ 80.2 ⫾ 23.7
ⱕ24 13 4.8 ETHICAL CONSIDERATIONS
25-48 29 10.8
The internal review boards of the hospitals involved
49-72 46 17.1
approved the project after having received information
73-95 15 506 on the aim, methodology, and confidentiality of the data
166 61.7 collected. Each nurse involved was informed about the
ⱖ96
a
study and gave her or his consent before the interview.
Removal day/hour reported in nursing records
Yes 32 31.1
RESULTS
No 71 68.9
Site laterality
Peripheral Intravascular Catheter
Right-hand side 94 34.9 Characteristics
Left-hand side 175 65.1 The PIV catheters included were observed in medical (175;
65.1%) and surgical wards (94; 34.9%). The catheters
Exposure
were in situ for an average of 80.2 hours (median 96 hours,
Front 113 42 ⫾23.7); 166 (61.7%) PIV catheters were left more than 96
Rear 156 58 hours, while 103 (38.3%) remained from 8 to 95 hours.
Catheters that remained less than 96 hours were removed
Site: vein
for occlusion (6; 5.8%), phlebitis (4; 3.9%), and extrava-
Hand veins 44 16.3 sations (2; 2.0%), and because patients needed no further
Cephalic 91 33.8 infusions (91; 88.3%). The main characteristics of the
catheters observed are recorded in Table 2.
Basilic 45 16.7
Median cubital 58 21.6 PIV Factors Associated With a Permanence
Ulnar 19 7.1 of 96 Hours or More
Brachial 12 4.5
Peripheral intravascular catheters positioned in
(continues) patients admitted in medical wards showed a higher
322 Journal of Infusion Nursing
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 323
length of stay in situ (average 87.8 hours, ⫾17.8) tioned in the forearm front (50/113). Also, those posi-
compared with those observed in surgical wards tioned in the forearm veins have a greater probability to
(average 66 hours, ⫾26.7). This difference is statisti- remain more than 96 hours than PIV catheters positioned
cally significant (P ⫽ .000). No difference emerged in in the veins of the hands (RR, 1.82; 95% CI, 1.35-2.45).
the average catheter’s permanence or lumen size (F ⫽
2.391, P ⫽ .06). Decision-Making Factors Pertaining to More
The probability of the PIV catheters’ remaining in place Than 96 Hours’ Catheter Permanence
after the 96 hours is no different in PIV catheters docu-
mented in the nursing records than in those that are not For the 166 PIV catheters that remained more than
(RR, 0.84; 95% CI, 0.69-1.02). There is no difference in 96 hours, nurses have reported 256 reasons, on average
the length of PIV permanence within catheters recorded 1.5 (median 1; ⫾0.7; minimum 0; maximum 3) per each
for day and hour of placement in the nursing records and PIV catheter left in situ. Out of 166 interviews made at
those not recorded (RR, 0.84; 95% CI, 0.69-1.02). the 96th hour, 68 (26.5%) nurses have reported 2 rea-
Peripheral intravascular catheters positioned in the left sons, and 21 (8.3%) have reported 3 reasons (Table 3).9
arm have more probability to be in place longer than 96 Nurses working in surgical wards have reported more
hours than those positioned in the right arm (RR, 7.57; reasons (average 1.8, ⫾ 0.7) than those working in med-
95% CI, 4.33-13.22). Catheters positioned in the forearm ical wards (1.5, ⫾ 0.6) (P = .00). Table 3 reports the fre-
rear (116/156) have more probability to be in place after quencies that emerged for each factor and the priority
96 hours (RR, 1.80; 95% CI, 1.38-2.3) than those posi- given by nurses.
TABLE 3
Factors Determining the Decision to Leave Peripheral
Intravascular Catheter In Situ at 96 Hours
Total no.
of Reasons
Definition (in Current Reported ⴝ Frequencies 1st no. ⴝ 2nd no. ⴝ 3rd no. ⴝ
Categories9 Subcategories9 Study) 256 (%) no. ⴝ 256 (%) 167 (%) 68 (%) 21 (%)
Individual The patient need of Patient does not need PIV 73 (28.6) 57 (22.2) 28 (16.7) 20 (29.4) 9 (42.8)
patient PIV catheter catheter in the near future.
situation
The PIV catheter’s Patient does not have other 16 (6.2) 9 (5.3) 4 (5.8) 3 (14.2)
applicability veins available.
Patient situation in … …
relation to PIV
replacement limits
Nurse’s work Time aspects PIV catheter replacement 49 (19.1) 43 (16.8) 35 (20.9) 8 (11.7)
situation has low priority because of
the workload.
Routines for planning … …
and following up
PIV catheter
Nurses’ attitudes The nurse is responsible 6 (2.3) 1 (0.5) 4 (5.8) 1 (4.7)
toward PIV for the patients.
management
Experience Experience of PIV— Nurses have no experience 134 (52.3) 81 (31.6) 53 (31.7) 26 (38.2) 2 (9.5)
of PIV man- complications of complications.
agement
The nurse’s capability There is a lack of capability 53 (20.7) 41 (24.5) 6(8.8) 6 (28.5)
in the insertion of the
PIV catheter within the
nursing staff.
Abbreviation: PIV, peripheral intravascular.
VOLUME 34 | NUMBER 5 | SEPTEMBER/OCTOBER 2011 323
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 324
DISCUSSION are lacking for both PIV catheter insertion and removal,
as documented by Ahlqvist and colleagues,12 but this is
not associated with the length of stay in situ. Moreover,
Limitations and Strengths creating a structured nursing record highlighting specif-
The study has several limitations. A limited number of ic items on PIV data per hour application, site, lumen,
PIV catheters were followed, and with the specific and other variables, might help nurses register these
inclusion criteria adopted, the external validity of the important data. Nurses’ PIV surveillance might be
results may be reduced, since the results are generalized affected by the lack of documentation, which also
only to PIV catheters positioned in patients admitted to threatens future comparative research.
medical and surgical wards, in nonurgent or emergent The main cause of a PIV catheter’s early removal is
conditions, and for nonirritable infusions. The high the interruption of the infusion, as recommended by the
number of the researchers involved (13) might have guideline,1 which suggests promptly removing any
also threatened the accuracy of the data collection intravascular catheter that is no longer essential (category
process, although, to reduce bias, specific education on IA).1 Under this point of view, the aptitudes of the nurses
data collection was provided. In accordance with the involved are adherent to the international guideline.
aim of the study, nurses interviewed by researchers Other causes of early removal are, in order of frequency,
were not assessed on their educational background, occlusion, phlebitis, and extravasations. The occurrence
competencies, and clinical experience. Also, few data of occlusions (defined as failure to infuse) must be
were collected on patients, which has limited the ability carefully compared with the results documented by
to consider the relevance of nurses’ competence as well Randolph and colleagues,13 because data on the patency
as the patient’s clinical condition and its effect on the strategy adopted (heparin vs physiologic solutions) were
nurses’ clinical judgment. not collected. Bregenzer,6 Fujita,8 and their colleagues
In addition, to account for the variability of the fac- have documented occlusion occurrence ranging from
tors influencing the decision-making process of the 6.0% to 6.9%, more than what was observed in our
nurses involved, the reasons determining the decision to study. The phlebitis ratio was similar to those docu-
leave the PIV catheter in situ for more than 96 hours mented on the third day by Homer and Holmes14 and
have been collected as the nurses reported verbatim. less than what Fujita and Namiki8 have documented
The subsequent categorization process, on the basis of (11.1%). Extravasations have been observed on only
the factors documented in the literature available, was 2 occasions, less than documented by Fujita and
done by triangulating the judgment of 3 researchers. Namiki.8
Moreover, the focus of the research was mainly on the Several decisions made by nurses at the time of the PIV
PIV catheters. The involvement of several hospitals catheter positioning influence its permanence. In fact, PIV
reflects the efforts to develop an extensive image of PIV catheters positioned in the left arm, in the rear surface,
management and daily variability among Italian institu- and in the arm veins (eg, in the basilic or cephalic) have
tions, a variation not previously documented. shown higher probability to remain after 96 hours. From
the results of this study, when nurses make an insertion
Factors Related to the PIV Length of site decision, they create the initial conditions for a more
Stay In Situ stable PIV site, which can be important for patients need-
ing it. Most patients, who are predominantly right-hand
Scheduled replacement of intravascular catheters has dominant,12 use the left arm less, reducing movements
been proposed as a standard method to prevent that might increase the risk of catheter traumas. Also, the
phlebitis and catheter-related infections.1 The incidence PIV catheters positioned on the rear surface of the fore-
of thrombophlebitis and bacterial colonization of arm have more probability to remain in situ over the 96th
catheters increases when catheters are left in place more hour; this can be explained with the usual bed position
than 72 hours; however, rates of phlebitis are not sub- adopted by most patients (arms alongside the body with
stantially different in peripheral catheters left in place palms resting on the sheets), which can be maintained
72 hours compared with 96 hours,2 which was assumed during infusions. The lumen of the cephalic and basilic
as the reference time for the study. veins compared with hand veins is important, and this
Several patients received PIV catheters during their can prevent local irritation documented by Maki15 and
hospitalization, and more than half (61.7%) remained Catney et al.16 The observed PIV catheters were never
in situ for more time than recommended by the litera- positioned in the wrists, which are considered a critical
ture. Peripheral intravascular catheters remained longer point, because it increases the risk of continuing move-
in patients admitted in medical wards compared with ment and creates dependency in the patient, who cannot
those in surgical wards, a fact that might be explained freely move the hand.
by the short length of stay and the different clinical con- After the site decision, which can influence the
ditions of the 2 groups of patients. The nursing records permanence of the PIV catheter, the next decision made
324 Journal of Infusion Nursing
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 325
by nurses17 is whether to leave the PIV in situ after composition of the staff, including experts and nonex-
96 hours. This clinical decision seems to be multidi- perts) because the lack of capability might have also
mensional. In fact, each nurse has reported more than negative effects on urgent or emergent cases.
1 factor involved in the decision-making process. The Two factors documented by Johansson and colleagues,9
factors that emerged were appropriately placed in the who conducted their study in Sweden, were not consis-
categories developed by Johansson and colleagues9: this tent with the results of this study (Table 3). The absence
methodological approach gives value to the results and of Johansson and his colleagues in the decision-making
hypothesis originated in qualitative studies, building on process might be related to the specific characteristics of
new results with a quantitative approach. With this the Italian nursing practice and may need to be studied
methodology, it is possible to develop progressively further in the future.
increased levels of evidence,18 strengthening their force. In this study, having excluded the PIV catheters posi-
Deciding not to adhere to the international guideline1 tioned during the night, it was not possible to describe
implies a sophisticated clinical judgment based on several the factors supporting the clinical decision-making
factors and not simply a violation19: in order of frequency, process developed by nurses during the night shift for
nurses have critically analyzed their personal experience catheters that had reached the 96th hour.
with PIV management (52.3%), then the individual
patient situation (28.6%), and the nurses’ work experience
(19.1%). Inside each category, as aggregated by Johansson CONCLUSIONS
and colleagues,9 some specific factors have emerged as
priorities. Implications for Practice
Complications in PIV management in the nurses’ pre- The clinical and research debate on PIV catheter length
vious personal experiences emerged as a priority: nurs- of placement is still ongoing. The nurses’ clinical deci-
es who did not have any experience with PIV complica- sion to leave the PIV catheter in place is multifactorial.
tions after 96 hours seem to be more comfortable leav- Because of the site decided by the nurses at the time of
ing the PIV catheter for a longer period. This is a risk the insertion, some PIV catheters have more probability
because it indicates an attitude in which only what has to stay in place for a longer time: this seems to be the
been experienced creates concerns. Nurses need to base prerequisite when nurses need a catheter available for
their judgments also on what could happen, or what is an extended period (eg, patient in unstable condition).
described as a risk in a particular situation, so that At the moment of the expected replacement, fixed at
unnecessary complications do not occur. It is important 96 hours after the positioning in accordance with the
to counteract this unnecessary risk during nurses’ bach- available guideline, several cognitive factors are taken
elor’s-level education and also through continuing edu- into account by nurses. These factors range from an
cation courses. This can be achieved simply through analysis based on their own clinical experience with PIV
presenting examples (such as photos or lectures given by complication and analysis of the patient’s clinical situa-
nurses with experience) to develop awareness of the sev- tion, to the critical analysis of their experience with
eral complications that can occur with peripheral inserting PIV catheters. This decision-making process is
catheterization. valuable: leaving the PIV catheter for more than 96 hours
The second priority that was given was regard for the is a complex decision-making process and not simply a
patient’s needs: the patient’s improved clinical condition guideline violation. Health care organizations might
and the patient’s no longer requiring the infusion change their policies regarding the need to replace
through the PIV catheter are the criteria that are consid- catheters by considering if it is clinically indicated. This
ered at the 96th hour in the decision to leave the PIV would have a significant effect on cost savings and would
catheter for a few additional hours instead of replacing also have a positive impact on patients, who would be
it. This decision should be considered appropriate: it spared the unnecessary pain of routine reinsertion in the
protects the patient from pain and discomfort, reduces absence of clinical indications.
the risk of introducing pathogens through the skin, and
also minimizes the consumption of valuable hospital Implications for Research
resources.
The third priority given was again the experience of Several questions might arise from the results of this
the nurses: this should be considered appropriate but study. Confronting the interreliability factors influencing
should be acted on cautiously. Nurses involved have nurses’ decision making regarding whether or not to
recognized their lack of experience in the reinsertion of leave the PIV catheter in situ and individuating discor-
PIV catheters. This may be improved with a combina- dances and agreements at different stages of a nurse’s
tion of courses providing instruction on insertion of PIV competence and expertise can provide valuable informa-
catheters and ad hoc strategies (such as an outreach tion on the process of PIV management. Also, developing
team, which is not available in Italy, and/or mixing the a multinational project to investigate differences within
VOLUME 34 | NUMBER 5 | SEPTEMBER/OCTOBER 2011 325
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
NAN200181.qxd 9/6/11 2:49 AM Page 326
nurses’ aptitudes in this critical decision, and the propor- 8. Fujita T, Namiki N. Replacement of peripheral intravenous
tion of PIV cases left in situ after 96 hours in daily prac- catheter. J Clin Nurs. 2008;17:2509-2510.
tice, might also contribute to PIV management practices 9. Johansson ME, Pilhammar E, Willman A. Nurses’ clinical reason-
ing concerning management of peripheral venous cannulae. J Clin
across the world. Finally, monitoring the negative out-
Nurs. 2009;18:3366-3375.
comes (eg, phlebitis) and their occurrence after 96 hours
10. Cheung E, Baerlocher MO, Asch M, Myers A. Venous access:
and involving nurses and patients at an international level a practical review for 2009. Can Fam Physician. 2009;55:
might help to provide a more in-depth understanding of 494-496.
when, and in which conditions, nurses can safely decide 11. International Organization for Standardization. International
to leave PIV catheters in situ after 96 hours. Standard ISO 10555-5. Sterile, Single Use, Intravascular Catheters.
Part 5: Over Needle Peripheral Catheters. Amendment 1 (1999).
REFERENCES Switzerland: Incorporating Technical Corrigendum; 2002:3.
12. Ahlqvist M, Berglund B, Wiren M, Klang B, Johansson E.
1. O’Grady NP, Alexander M, Dellinger EP, et al; and Healthcare Accuracy in documentation: a study of peripheral venous
Infection Control Practices Advisory Committee. Guidelines for catheter. J Clin Nurs. 2009;18:1945-1952.
the prevention of intravascular catheter-related infections. Infect 13. Randolph AG, Cook DJ, Gonzales CA, Andrew M. Benefit of
Control Hosp Epidemiol. 2002;23(12):759-769. heparin in peripheral venous and arterial catheters: systematic
2. Lai KK. Safety of prolonging peripheral cannula and I.V. tubing review and meta-analysis of randomized controlled trials. BMJ.
use from 72 to 96 hours. Am J Infect Control. 1998;26:66-70. 1998;316(7136):969-975.
3. Webster J, Clarke S, Paterson D, et al. Routine care of peripheral 14. Homer LD, Holmes KR. Risks associated with 72 and 96 hours
intravenous catheters versus clinically indicated replacement: peripheral intravenous catheter dwell times. J Intraven Nurs.
randomized controlled trial. BMJ. 2008;337(7662):157-160. 1998;21:301-305.
4. Webster J, Osborne S, Hall J, Rickard C. Clinically indicated 15. Maki DG. Reactions associated with catheters for intravenous
replacement versus routine replacement of peripheral venous access. Ann Intern Med. 1991;123:884-886.
catheter (protocol). The Cochrane Library. 2009;2. http://www98. 16. Catney MR, Hillis S, Wakenfield B, et al. Relationship between
griffith.edu.au/dspace/bitstream/10072/32191/1/62829_1.pdf peripheral intravenous catheter dwell time and the develop-
5. Webster J, Osborne S, Rickard C, Hall J. Clinically-indicated ment of phlebitis and infiltration. J Infus Nurs. 2001; 24(5):
replacement versus routine replacement of peripheral venous 332-341.
catheters. Cochrane Database Syst Rev. 2010;17(3):CD007798. 17. Higgs J, Jones M. Clinical Reasoning in the Health Professions.
6. Bregenzer T, Conen D, Sakmann P, Wildmer AF. Is routine Philadelphia, PA: Butterworth-Heinemann; 2006:107-116.
replacement of peripheral intravenous catheters necessary? Arch 18. Di Censo A, Gyuatt G, Ciliska D. Evidence-Based Nursing: A
Intern Med. 1998;158:151-156. Guide to Clinical Practice. St Louis, MO: Elsevier Mosby; 2005.
7. Barker P, Anderson ADG, MacFie J. Randomized clinical trial of 19. Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians fol-
elective re-siting of intravenous cannulae. Ann R Coll Surg Engl. low clinical practice guidelines? A framework for improvement.
2008;86:281-283. JAMA. 1999;282:1458-1465.
For more than 6 additional continuing education articles related
to infusion therapy, go to NursingCenter.com/CE.
326 Journal of Infusion Nursing
Copyright © 2011 Infusion Nurses Society. Unauthorized reproduction of this article is prohibited.
You might also like
- Critical Care Intravenous DrugsDocument1 pageCritical Care Intravenous DrugsMarynel Dixie Izon Brao91% (11)
- NCP GunshotDocument13 pagesNCP GunshotMichael John F. Natividad0% (1)
- Registered Medical Device - 08 - 03 - 20Document104 pagesRegistered Medical Device - 08 - 03 - 20Md. Shafi Newaz100% (1)
- Health Teaching DengueDocument3 pagesHealth Teaching DenguearjeighNo ratings yet
- Colloids and CrystalooidsDocument42 pagesColloids and Crystalooidsلؤي زعيترNo ratings yet
- 1 s2.0 S2452247318300384 Main PDFDocument4 pages1 s2.0 S2452247318300384 Main PDFDinny ApriliaNo ratings yet
- Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes WorldwideDocument7 pagesUse of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes WorldwidemochkurniawanNo ratings yet
- A Nurse-Driven Process For TimelyDocument7 pagesA Nurse-Driven Process For TimelyWardah Fauziah El SofwanNo ratings yet
- Large Scale Implementation of A Respiratory Therapist WESLEY ELYDocument8 pagesLarge Scale Implementation of A Respiratory Therapist WESLEY ELYKinesio FernandezNo ratings yet
- POCUSenColelitiasis 200618 162923Document5 pagesPOCUSenColelitiasis 200618 162923David Salomon Gomez AscencioNo ratings yet
- Article-Er (2024) - 2 - HernandezDocument3 pagesArticle-Er (2024) - 2 - HernandezloveviaNo ratings yet
- Journal For MEdical WardDocument8 pagesJournal For MEdical WardValcrist BalderNo ratings yet
- Evaluation of A Radial Artery Cannulation Training Program For Intensive Care Nurses: A Descriptive, Explorative StudyDocument9 pagesEvaluation of A Radial Artery Cannulation Training Program For Intensive Care Nurses: A Descriptive, Explorative StudyAngelina PondeteNo ratings yet
- AJA2019 Cspine ExtubationDocument7 pagesAJA2019 Cspine ExtubationSeveNNo ratings yet
- Farach 2014Document5 pagesFarach 2014mia widiastutiNo ratings yet
- Al-Natour - 2016 - Peritoneal DialysisDocument3 pagesAl-Natour - 2016 - Peritoneal Dialysisridha afzalNo ratings yet
- Goldman Et Al-2017-Neurourology and UrodynamicsDocument26 pagesGoldman Et Al-2017-Neurourology and UrodynamicsJorge Mario RinconNo ratings yet
- 11.1 AP Accuracy of Fine Needle Aspiration Cytology FNAC IDocument7 pages11.1 AP Accuracy of Fine Needle Aspiration Cytology FNAC IdrdivyeshgoswamiNo ratings yet
- Cryotherapy For Acute Ankle Sprains - A Randomised Controlled Study of Two Different Icing ProtocolsDocument7 pagesCryotherapy For Acute Ankle Sprains - A Randomised Controlled Study of Two Different Icing ProtocolsBlessing NyazikaNo ratings yet
- 440 Leadership Strategic AnalysisDocument7 pages440 Leadership Strategic Analysisapi-212894173No ratings yet
- Ventilation tubes - מאמר2Document5 pagesVentilation tubes - מאמר2Avishay ZoarNo ratings yet
- 12Hiệu quả mở kq sớm pt gộp 2015Document10 pages12Hiệu quả mở kq sớm pt gộp 2015Cường Nguyễn HùngNo ratings yet
- Hernia InguinalisDocument7 pagesHernia InguinalisabduNo ratings yet
- Artigo 2 CinhalDocument7 pagesArtigo 2 CinhalSara PereiraNo ratings yet
- Infusion Nursing Standards of PracticeDocument2 pagesInfusion Nursing Standards of Practiceajip ejepNo ratings yet
- Thyroid Disorders in North India and Their Reporting by Bethesda System  " 1 Year Retrospective StudyDocument5 pagesThyroid Disorders in North India and Their Reporting by Bethesda System  " 1 Year Retrospective StudyIJAR JOURNALNo ratings yet
- Intravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofDocument1 pageIntravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofoomculunNo ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Initial Experience With Same Day Discharge After Laparoscopic Appendectomy For Nonperforated AppendicitisDocument6 pagesInitial Experience With Same Day Discharge After Laparoscopic Appendectomy For Nonperforated AppendicitisrizkianiNo ratings yet
- Indications of Ventriculoperitoneal Shunt: A Prospective StudyDocument8 pagesIndications of Ventriculoperitoneal Shunt: A Prospective Studyvalencia suwardiNo ratings yet
- El Beheiry2019Document4 pagesEl Beheiry2019achmadaNo ratings yet
- Daud Jurnal PDFDocument9 pagesDaud Jurnal PDFAngga PratamaNo ratings yet
- Torsion BMC 02 July - 012901Document21 pagesTorsion BMC 02 July - 012901Olasinde AnthonyNo ratings yet
- International Journal of Nursing Studies: SciencedirectDocument4 pagesInternational Journal of Nursing Studies: Sciencedirectyoga madaniNo ratings yet
- Multiple Choice Questions in Medical Schools: Saudi Medical Journal December 2000Document10 pagesMultiple Choice Questions in Medical Schools: Saudi Medical Journal December 2000RAJESH SHARMANo ratings yet
- Jurnal Uro 2Document8 pagesJurnal Uro 2Lisa HikmawanNo ratings yet
- Point-Of-Care Gastric Ultrasound and Aspiration Risk Assessment - A Narrative Review PDFDocument12 pagesPoint-Of-Care Gastric Ultrasound and Aspiration Risk Assessment - A Narrative Review PDFJohana FuentesNo ratings yet
- 40 PDFDocument5 pages40 PDFIJAR JOURNALNo ratings yet
- Jurnal VaskularDocument5 pagesJurnal VaskulardrelvNo ratings yet
- Closure Vs Nonclosure of PeritoneumDocument6 pagesClosure Vs Nonclosure of PeritoneumFrancisco Xavier Beltrán Vallejo100% (1)
- 1 s2.0 S088394412300196X MainDocument14 pages1 s2.0 S088394412300196X MainCristina LopezNo ratings yet
- Fixation of The Short-Term Central Venous Catheter. A Comparison of Two TechniquesDocument11 pagesFixation of The Short-Term Central Venous Catheter. A Comparison of Two TechniquesJaime Augusto Quimbayo GuarnizoNo ratings yet
- Daily Interruption of Sedation in Patients Receiving Mechanical VentilationDocument10 pagesDaily Interruption of Sedation in Patients Receiving Mechanical VentilationJim LinNo ratings yet
- Guidelines For Laparoscopic Peritoneal Dialysis Access SurgeryDocument28 pagesGuidelines For Laparoscopic Peritoneal Dialysis Access SurgeryIgnatia Rosalia KiranaNo ratings yet
- Prevalence of Postoperative Bariatric Surgery Complications Specially GallstoneDocument7 pagesPrevalence of Postoperative Bariatric Surgery Complications Specially GallstoneIJAR JOURNALNo ratings yet
- Bladder ManagemenDocument5 pagesBladder ManagemenFayza RihastaraNo ratings yet
- C Nursing Diagnosis IJONKDocument8 pagesC Nursing Diagnosis IJONKkatonyalalainaNo ratings yet
- Clinico-Radiological Diagnosis OfappendicitisDocument14 pagesClinico-Radiological Diagnosis OfappendicitisIJAR JOURNALNo ratings yet
- Editorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystDocument4 pagesEditorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystLogical MonsterNo ratings yet
- The DENALI Trial: An Interim Analysis of A Prospective, Multicenter Study of The Denali Retrievable Inferior Vena Cava FilterDocument10 pagesThe DENALI Trial: An Interim Analysis of A Prospective, Multicenter Study of The Denali Retrievable Inferior Vena Cava FilterMostafaNo ratings yet
- 10 1111@ans 15125Document7 pages10 1111@ans 15125Sahily MoralesNo ratings yet
- Appendicular MasDocument6 pagesAppendicular MasSangeetha VijianNo ratings yet
- A Study On Effective Post-Operative Care in Emergency/elective LSCS PatientsDocument9 pagesA Study On Effective Post-Operative Care in Emergency/elective LSCS PatientsIJAR JOURNALNo ratings yet
- A Prospective, Multi Center Study Assessing Early Loading With Short Implants in Posterior Regions. A 3 Year Post Loading Follow Up StudyDocument9 pagesA Prospective, Multi Center Study Assessing Early Loading With Short Implants in Posterior Regions. A 3 Year Post Loading Follow Up StudyBagis Emre GulNo ratings yet
- Barriers To Effective PARU Handover: ACORN December 2010Document6 pagesBarriers To Effective PARU Handover: ACORN December 2010Pebri IrawanNo ratings yet
- Bloomberg 1989 (Advantages of Paramedian Approach)Document5 pagesBloomberg 1989 (Advantages of Paramedian Approach)Olivia LimNo ratings yet
- Turning Frequency in Adult Bedridden Patients To Prevent Hospital-Acquired Pressure Ulcer: A Scoping ReviewDocument12 pagesTurning Frequency in Adult Bedridden Patients To Prevent Hospital-Acquired Pressure Ulcer: A Scoping ReviewfajaqaNo ratings yet
- 10 1111@anae 15390Document11 pages10 1111@anae 15390ailed.36363638No ratings yet
- Total Pancreatectomy: Short-And Long-Term Outcomes at A High-Volume Pancreas CenterDocument10 pagesTotal Pancreatectomy: Short-And Long-Term Outcomes at A High-Volume Pancreas CenterJherinNo ratings yet
- Self Catheterization ToolDocument13 pagesSelf Catheterization ToolAmanuel GirmayeNo ratings yet
- Harris 2012Document5 pagesHarris 2012Nurul AidaNo ratings yet
- Bess Is Sow 2014Document2 pagesBess Is Sow 2014Alfredo ChoquetNo ratings yet
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDocument5 pagesA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinNo ratings yet
- Percutaneous NephrolithotomyFrom EverandPercutaneous NephrolithotomyGuohua ZengNo ratings yet
- CB English For Nursing (Int) GlossaryDocument12 pagesCB English For Nursing (Int) GlossaryMorne Du Plooy TeacherNo ratings yet
- Pediatric and Geriatric ProceduresDocument9 pagesPediatric and Geriatric ProceduresTeza RizkyNo ratings yet
- Isosorbide Dinitrate Kinetics and Dynamics After IDocument11 pagesIsosorbide Dinitrate Kinetics and Dynamics After IFicka HanafiNo ratings yet
- Safe Handling of Hazardous DrugsDocument35 pagesSafe Handling of Hazardous Drugsvasu.nadapanaNo ratings yet
- NP3 4Document65 pagesNP3 4Edward Nicko Garcia100% (1)
- Konversi Kode Prosedure INACBGs Ke Kode ICD 9-CMDocument349 pagesKonversi Kode Prosedure INACBGs Ke Kode ICD 9-CMTri Muhammad HaniNo ratings yet
- EMS Burn Reference CardDocument2 pagesEMS Burn Reference CardCassie CabreraNo ratings yet
- LASA AdministrationDocument3 pagesLASA AdministrationgursinNo ratings yet
- Instructional Plan Career PathDocument6 pagesInstructional Plan Career PathKarl RobleNo ratings yet
- IV Cannulation Study Questions 2015Document2 pagesIV Cannulation Study Questions 2015KNo ratings yet
- CancerDocument14 pagesCancerClara De Guzman83% (6)
- GN-13-R2 Guidance On The Risk Classification of General Medical Devices (18Jun-Pub)Document36 pagesGN-13-R2 Guidance On The Risk Classification of General Medical Devices (18Jun-Pub)Gina ArcNo ratings yet
- Funda Past Board 2 Brilliant ChoiceDocument5 pagesFunda Past Board 2 Brilliant Choicecoffee bean100% (2)
- Nurses NotesDocument3 pagesNurses Notesamita chakrabortyNo ratings yet
- Malnutrition: A Secular Challenge To Child Nutrition: Review ArticleDocument13 pagesMalnutrition: A Secular Challenge To Child Nutrition: Review ArticleAdi ParamarthaNo ratings yet
- A General Guide To Blood Transfusion: Information For Patients & FamiliesDocument2 pagesA General Guide To Blood Transfusion: Information For Patients & FamiliesVette Angelikka Dela CruzNo ratings yet
- Cancer and Oncology Nursing NCLEX Practice Quiz-1Document30 pagesCancer and Oncology Nursing NCLEX Practice Quiz-1Susie Salmon100% (2)
- Monitoring System On Intravenous Fluid (IVF)Document4 pagesMonitoring System On Intravenous Fluid (IVF)ab3720No ratings yet
- CBAHI and JCI FAQs 2023 1 ٢Document12 pagesCBAHI and JCI FAQs 2023 1 ٢Magdi SalemNo ratings yet
- Drug CalculationsDocument5 pagesDrug CalculationsVikram SamyNo ratings yet
- Ivt Form2Document2 pagesIvt Form2Ina Patricia ErjasNo ratings yet
- Guidance To The Internaitonal Medical Guide For Ships 3rd EdDocument14 pagesGuidance To The Internaitonal Medical Guide For Ships 3rd EdSaurabh YadavNo ratings yet
- CPR PPT FinalDocument119 pagesCPR PPT Finalcriselda.pabuaNo ratings yet
- 1515 InfInjHyd Gonzales PDFDocument41 pages1515 InfInjHyd Gonzales PDFtimvrghs123No ratings yet
- 12 To 24 HoursDocument45 pages12 To 24 HoursstellaNo ratings yet