Professional Documents
Culture Documents
Morgan Bahasa Inggris Mau Ditranslate
Morgan Bahasa Inggris Mau Ditranslate
Uploaded by
Muhammad Fahreza Wardhana0 ratings0% found this document useful (0 votes)
4 views4 pagesOriginal Title
morgan bahasa inggris mau ditranslate.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
4 views4 pagesMorgan Bahasa Inggris Mau Ditranslate
Morgan Bahasa Inggris Mau Ditranslate
Uploaded by
Muhammad Fahreza WardhanaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 4
Preoperative Laboratory Testing
Routine laboratory testing when patients are fi t and
asymptomatic is not recommended. Testing should
be guided by the history and physical examination.
“Routine” testing is expensive and rarely alters perioperative
management; moreover, abnormal values
oft en are overlooked or if recognized may result in
unnecessary delays. Nonetheless, despite the lack of
evidence of benefi t, many physicians order a hematocrit
or hemoglobin concentration, urinalysis,
serum electrolyte measurements, coagulation studies,
an electrocardiogram, and a chest radiograph for
all patients, perhaps in the misplaced hope of reducing
their exposure to litigation.
9 To be valuable, preoperative testing must discriminate:
there must be an increased perioperative
risk when the results are abnormal (and
unknown when the test is not performed), and there
must be a reduced risk when the abnormality is not
detected (or it has been corrected). Th is requires that
the test have a very low rate of false-positive and
10 false-negative results. Th e utility of a test
depends on its sensitivity and specifi city. Sensitive
tests have a low rate of false-negative results
and rarely fail to identify an abnormality when one
is present, whereas specifi c tests have a low rate of
false-positive results and rarely identify an abnormality
when one is not present . Th e prevalence of a
disease or of an abnormal test result varies with the
population tested. Testing is therefore most eff ective
when sensitive and specifi c tests are used in patients
in whom the abnormality will be detected frequently
enough to justify the expense and inconvenience of
the test procedure. Accordingly, laboratory testing
should be based on the presence or absence of underlying
diseases and drug therapy as detected by the
history and physical examination. Th e nature of the
proposed surgery or procedure should also be taken
into consideration. Th us, a baseline hemoglobin or
hematocrit measurement is desirable in any patient
about to undergo a procedure that may result in
extensive blood loss and require transfusion, particularly
when there is suffi cient time to correct anemia
preoperatively (eg, with iron supplements).
Testing fertile women for an undiagnosed early
pregnancy is controversial and should not be done
without the permission of the patient; pregnancy
testing involves detection of chorionic gonadotropin
in urine or serum. Routine testing for HIV antibody
is not indicated. Routine coagulation studies and urinalysis
are not cost-eff ective in asymptomatic healthy
patients; nevertheless, a preoperative urinalysis is
required by state law in at least one U.S. jurisdiction.
PREMEDICATION
A classic study showed that a preoperative visit from
an anesthesiologist resulted in a greater reduction in
patient anxiety than preoperative sedative drugs.
Yet, there was a time when virtually every patient
received premedication before arriving in the preoperative
area in anticipation of surgery. Despite the
evidence, the belief was that all patients benefi tted
from sedation and anticholinergics, and most
patients would benefi t from a preoperative opioid.
Aft er such premedication, some patients arrived
in a nearly anesthetized state. With the move to outpatient
surgery and “same-day” hospital admission,
the practice has shift ed. Today, preoperative
sedative-hypnotics or opioids are almost never
administered before patients arrive in the preoperative
holding area (other than for intubated patients
who have been previously sedated in the intensive
care unit). Children, especially those aged 2–10 years
who will experience separation anxiety on being
removed from their parent, may benefi t from premedication
administered in the preoperative holding
area. Th is topic is discussed in Chapter 42. Midazolam,
administered either intravenously or orally,
is a common method. Adults oft en receive intravenous
midazolam (2–5 mg) once an intravenous line
has been established, and if a painful procedure (eg,
regional block or a central venous line) will be performed
while the patient remains awake, small doses
of opioid (typically fentanyl) will oft en be given.
Patients who will undergo airway surgery or extensive
airway manipulations benefi t from preoperative
administration of an anticholinergic agent (glycopyrrolate
or atropine) to reduce airway secretions
before and during surgery. Th e fundamental
message here is that premedication should be
given purposefully, not as a mindless routine.
DOCUMENTATION
Physicians should fi rst and foremost provide highquality
and effi cient medical care. Secondly, they
must document the care that has been provided.
Adequate documentation provides guidance to
those who may encounter the patient in the future.
It permits others to assess the quality of the care
that was given and to provide risk adjustment of
outcomes. Adequate documentation is required for
a physician to submit a bill for his or her services.
Finally, adequate and well-organized documentation
(as opposed to inadequate and sloppy documentation)
supports a potential defense case should
a claim for medical malpractice be fi led.
Preoperative Assessment Note
Th e preoperative assessment note should appear in
the patient’s permanent medical record and should
describe pertinent fi ndings, including the medical
history, anesthetic history, current medications (and
whether they were taken on the day of surgery),
physical examination, ASA physical status class,
laboratory results, interpretation of imaging, electrocardiograms,
and recommendations of any consultants.
A comment is particularly important when the
consultant’s recommendation will not be followed.
As most North American hospitals are transitioning
to electronic medical records, the preanesthetic note
will oft en appear as a standardized form.
Th e preoperative note should briefl y describe
the anesthetic plan and include a statement regarding
informed consent from the patient (or guardian).
Th e plan should indicate whether regional or general
anesthesia (or sedation) will be used, and whether
invasive monitoring or other advanced techniques
will be employed. Documentation of the informed
consent discussion sometimes takes the form of a
narrative indicating that the plan, alternative plans,
and their advantages and disadvantages (including
their relative risks) were presented, understood, and
accepted by the patient. Alternatively, the patient may
be asked to sign a special anesthesia consent form
that contains the same information. A sample preanesthetic
report form is illustrated in Figure 18–1 .
In the United States, Th e Joint Commission
(TJC) requires an immediate preanesthetic reevaluation
to determine whether the patient’s status has
changed in the time since the preoperative evaluation
was performed. Even when the elapsed time
is less than a minute, the bureaucracy will not be
denied: the “box” must be checked to indicate that
there has been no interval change.
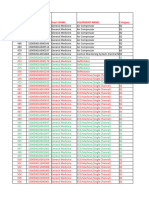
Intraoperative Anesthesia Record
Th e intraoperative anesthesia record ( Figure 18–2 )
serves many purposes. It functions as documentation
of intraoperative monitoring, a reference for
future anesthetics for that patient, and a source of
data for quality assurance. Th is record should be
terse, pertinent, and accurate. Increasingly, parts
of the anesthesia record are generated automatically
and recorded electronically. Such anesthesia
information management systems (commonly
abbreviated AIMS) have many theoretical and
practical advantages over the traditional paper
record but also introduce all the common pitfalls of
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Candida CytoplanDocument12 pagesCandida CytoplanIsh VadgamaNo ratings yet
- Chem 353 Pyruvate Dehydrogenase DeficiencyDocument24 pagesChem 353 Pyruvate Dehydrogenase Deficiencyapi-308400395No ratings yet
- Prof. DR Yeyen M (Ictrops)Document14 pagesProf. DR Yeyen M (Ictrops)Muhammad Fahreza WardhanaNo ratings yet
- Morning Report IGD: Kamis, 3 Mei - Jumat, 4 Mei 2018Document6 pagesMorning Report IGD: Kamis, 3 Mei - Jumat, 4 Mei 2018Muhammad Fahreza WardhanaNo ratings yet
- Morning Report 28 Maret 2018Document3 pagesMorning Report 28 Maret 2018Muhammad Fahreza WardhanaNo ratings yet
- My Family Structure: Hj. Noordnjenah (Grandmother) H.M. Djoenaid Suntung (Grandfather)Document1 pageMy Family Structure: Hj. Noordnjenah (Grandmother) H.M. Djoenaid Suntung (Grandfather)Muhammad Fahreza WardhanaNo ratings yet
- Name Product Link For Clients To UseDocument46 pagesName Product Link For Clients To UseGerry GimenaNo ratings yet
- JHS - Syllabus AFA-7 (Crop Prod) - 1920-EricoDocument2 pagesJHS - Syllabus AFA-7 (Crop Prod) - 1920-EricoEdwin SorianoNo ratings yet
- Subacromial Impingement Syndrome E Book 1Document28 pagesSubacromial Impingement Syndrome E Book 1niko.zaroNo ratings yet
- Mobility, Stability and MovementDocument62 pagesMobility, Stability and MovementYuldashNo ratings yet
- Lymphocytic LeukemiaDocument6 pagesLymphocytic Leukemiaル シリ100% (1)
- Restoration of Occlusal Plane and Esthetics in Severely Worn DentitionDocument4 pagesRestoration of Occlusal Plane and Esthetics in Severely Worn DentitionUJ CommunicationNo ratings yet
- Caries Diagnosis and TreatmentDocument18 pagesCaries Diagnosis and Treatmentrxmskdkd33No ratings yet
- Theme: Junk FoodDocument7 pagesTheme: Junk FoodsarjitgaurNo ratings yet
- Legal Medicine: The Branch of Medicine That Deals With TheDocument3 pagesLegal Medicine: The Branch of Medicine That Deals With TheEthel Joi Manalac MendozaNo ratings yet
- Approved InstDocument368 pagesApproved InstSatish VermaNo ratings yet
- Risk Assesment CSSDDocument9 pagesRisk Assesment CSSDTianti Puadi100% (1)
- Villones Table of ContentsDocument5 pagesVillones Table of ContentsBevsly VillonesNo ratings yet
- NeurosexologyDocument23 pagesNeurosexologydo2005No ratings yet
- Vegan CompaniesDocument32 pagesVegan CompaniesLaura MelendezNo ratings yet
- DMSCO Log Book Vol.50 1972Document57 pagesDMSCO Log Book Vol.50 1972Des Moines University Archives and Rare Book RoomNo ratings yet
- HAZOP Case Study ExampleDocument4 pagesHAZOP Case Study ExampleanushaNo ratings yet
- Equipment Details-1Document40 pagesEquipment Details-1ElanthirayanNo ratings yet
- Smart VillageDocument24 pagesSmart VillageDhruv100% (1)
- Personal Hygiene: Tve-ExploratoryDocument3 pagesPersonal Hygiene: Tve-ExploratoryPoseidon NipNo ratings yet
- Clinical Outcome PDF Update 2010Document62 pagesClinical Outcome PDF Update 2010Breno Mendes CardosoNo ratings yet
- Republic of The Philippines Regional Trial Court Branch 26Document5 pagesRepublic of The Philippines Regional Trial Court Branch 26JenMarlon Corpuz AquinoNo ratings yet
- 12th Zoolgy Guess Paper 2021 PDFDocument3 pages12th Zoolgy Guess Paper 2021 PDFMir FozAnNo ratings yet
- BETA VitaHop CaseSty R2Document1 pageBETA VitaHop CaseSty R2ALEJANDRO AstudilloNo ratings yet
- Barytes SDS 12 04INT19 03Document5 pagesBarytes SDS 12 04INT19 03Shola EshoNo ratings yet
- 2-Physiotherapy For FracturesDocument17 pages2-Physiotherapy For FracturesJuanitoCabatañaLimIIINo ratings yet
- MicroorganismsDocument17 pagesMicroorganismsLindzhy LimNo ratings yet
- Factors of Care During Pregnancy, ScreeningsDocument38 pagesFactors of Care During Pregnancy, ScreeningssabhyaNo ratings yet
- Passport Appointment ScheduleDocument3 pagesPassport Appointment ScheduleSonia ShinoharaNo ratings yet