Professional Documents
Culture Documents
Mines 1993
Mines 1993
Uploaded by
Mădălina StănășelOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mines 1993
Mines 1993
Uploaded by
Mădălina StănășelCopyright:
Available Formats
CASE REPORT
pneumothorax
thoracostomy
N e e d l e Thoracostomy Fails to Detect a Fatal
Tension Pneumothorax
From the EmergencyDepartment, Daniel Mines, MD Needle thoracostomy is an emergency procedure used to beth
Depaitment of Medicine, University Stephanie Abbuhl, MD, FACEP diagnose and initially treat a tension pneumothorax. We report a
of Pennsylvania, Philadelphia.
case of fatal tension pneumothorax in an intubated patient with
Receivedfor publication
September9, 1992. Acceptedfor chronic obstructive pulmonary disease that was missed by this
publication November 16, 1992. technique. A tension pneumothorax involving only the right
middle and lower lobes was found at autopsy.The autopsy also
suggested that needle thoracostomy was misleading because it
sampled air from a noncommunicating bulla in the right upper
lobe rather than from the pleural space. Tension physiology
can exist with only localized collapse of a lung, and diagnostic
needle thoracostomy can be falsely negative. When tension
pneumothorax is strongly suspected, if empiric thoracentesis
does not vent air under pressure, subsequenttube thoracostomy
is indicated.
[Mines D, Abbuhl S: Needle thoracostomy fails to detect a fatal
tension pneumothorax. Ann EmergMed May 1993;22:863-866.]
INTRODUCTION
Tension pneumothorax, which can be rapidly fatal, often
is diagnosed on clinical grounds because time may not
permit radiographic confirmation. Needle thoracostomy--
also known as thoracentesis and needle decompression of
the chest--can quickly diagnose and temporarily treat a
tension pneumothorax by venting intrapleural air under
pressure to the atmosphere. 1-3 Although it is used
commonly in this setting, this technique has limitations
that may not be widely recognized, as the following case
illustrates.
CASE REPORT
A 68-year-old man with a history of chronic obstructive
pulmonary disease and hypertension presented to the
emergency department because of difficulty breathing.
During the course of the daB the patient became short
of breath, and after the onset of left-sided chest pain that
radiated to his back, the dyspnea intensified. There was
MAY 1993 22:5 ANNALS OF EMERGENCY MEDICINE 863/ 133
TENSION PNEUMOTHORAX
Mines & Abbuhl
no recent change in sputum, fever, or chills, nor history of the patient went into ventricular fibrillation and could
coronary artery disease. Medications included an albuterol not be resuscitated.
inhaler, sustained-release theophylline, and prednisone. At autopsy, air under pressure escaped when the right
The patient was cyanotic, unresponsive, and in marked hemothorax was opened. The right middle and lower
respiratory distress. Blood pressure was 190/110 mm Hg lobes of the lung were collapsed completely, and the
in both arms; pulse, 140; rectal temperature, 37.4 C; and mediastinum was deviated leftward. There was no evidence
respirations, 40. The jugular veins were not distended. On of myocardial infarction, cardiac tamponade, thoracic
auscultation, breath sounds were markedly diminished aortic dissection, or pulmonary embolism. These findings
bilaterally, and there were scattered rhonchi. Heart sounds suggest that the patient died from a right-sided tension
were distant and regular; no murmur, rub, or gallop was
pneumothorax.
heard. The abdomen was soft and not distended. The
Unexpectedly, the right upper lobe remained inflated
extremities were not edematous.
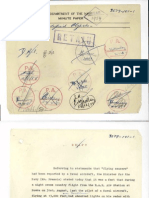
when the anterior chest wall was removed (Figure). No
The patient was intubated because of his impending
respiratory failure, using an orotracheal approach and obstructing endobronchial lesion or pleural scarring was
topical anesthesia. A chest radiograph showed the endo- found to account for this finding. Air trapped in large,
tracheal tube in satisfactory position, a normal mediastinal noncommunicating buflae was responsible for the persis-
contour, a left perihilar infiltrate, and bullous changes in tent expansion of the right upper lobe.
both upper lung fields. An ECG revealed sinus tachycar-
dia without ischemic changes. An arterial blood gas, DISCUSSION
drawn before intubation when the patient was breathing The classic findings of tension pneumothorax--tracheal
100% oxygen, returned with a pH of 7.04; CO 2, 105 mm deviation, hyperresonant hemithorax, and unilaterally
Hg; oxygen, 95 mm Hg; and HCO3,26 mEq/L.
decreased breath sounds--are useful to suggest the diag-
After intubation, the patient became more alert and
nosis, but they are not always present.l,2, 4 In patients
was able to follow commands. However, ten minutes later
with chronic obstructive pulmonary disease, the diagnosis
he suddenly became unresponsive, profoundly hypoten-
sire, and, within seconds, pulseless. The rhythm on the of tension pneumothorax can be especially subtle.
monitor remained sinus tachycardia. Physical signs are often absent or overlooked because
CPR and volume resuscitation were begun. IV epine- their underlying disease already may have produced
phrine and bicarbonate were administered as empiric diminished chest wall motion, decreased breath sounds,
treatment for electromechanical dissociation. The endo- and hyperresonance to percussion. 2 Similarly, distended
tracheal tube position was verified. Distant breath sounds neck veins, which are suggestive of tension pneumothorax
still were heard symmetrically over both lung fields, and in patients without underlying cardiopulmonary disease,
the trachea was midline. When the patient did not are nonspecific in this population because they are
respond to these initial measures, a 1&gauge over-the- observed frequently during an exacerbation of chronic
needle catheter connected to water seal was inserted into obstructive pulmonary disease.
the left chest in the second intercostal space, midclavicu-
lar line. Air bubbled continuously through the water seal, Figure.
and a spontaneous pulse returned. A 28F thoracostomy Autopsy photograph of the
tube was inserted in the midaxillary line, fifth intercostal thoracic structures after the
space. As the tube was being secured, the patient again anterior chest wall was
removed. Although the right
became tachycardic and then pulseless. CPR was restarted. middle and lower lobes
Patency of the chest tube was confirmed by a persistent (arrow 1) are collapsed as
air leak. expected, the right upper
Because there was now a strong suspicion for a contra- lobe (arrow 2) is still
lateral tensio n pneumothorax, thoracentesis of the right inflated because of air
trapped in bullae. A chest
chest was attempted, in the same high anterior position tube is present in the left
as had been used on the left. There was no efflux of air hemithorax.
through the needle. Pericardiocentesis was performed
using a left subxiphoid approach, yielding 2 mL of yellow
fluid, without clinical improvement. Shortly afterward,
1 3 4/864 ANNALS OF EMERGENCY MEDICINE 22:5 MAY 1993
TENSION PNEUMOTHORAX
Mines & Abbuhl
Besides physical findings, the clinical setting may suggest Reviewing the medical literature since 1966, we could
the diagnosis of tension pneumothorax. Positive-pressure identify no study that quantitated the sensitivity of needle
ventilation, through a bag-valve system or a mechanical thoracostomy in diagnosing tension pneumothorax. Several
ventilator, increases the risk of tension pneumothorax, authorities2,5, 6 who advocate needle thoracostomy to
particularly when there is coexistent pulmonary disease. 1-3,5 empirically diagnose this condition do not mention its
Both risk factors were present in the index case. limitations, implying that it is virtually 100% sensitive.
When a tension pneumothorax is suspected clinically Ross 1 mentioned that in performing thoracentesis using
and the patient is unstable, time does not permit a radio- the anterior approach, a loculated simple pneumothorax
graphic diagnosis. Instead, empiric needle or catheter can be missed. To our knowledge, this case report is the
thoracentesis is indicated. 1-3 If a tension pneumothorax first description of a false-negative result of needle thora-
is present, one expects to see the "the rapid efflux of air costomy in a tension pneumothorax that was confirmed
through the needle during both inspiration and expiration" at autopsy
along with clinical improvement. 1 Needle thoracostomy is Our case also shows that an entire lung need not be
thus a quick diagnostic and therapeutic maneuver, which collapsed for tension physiology to exist. This observation
needs to be followed by a more definitive tube thoracostomy is consistent with results of a controlled study of tension
Most authorities1,6, r recommend needle decompres- pneumothorax in animals. 9 In this experiment, air was
sion using a high anterior approach in the second or introduced into the pleural cavities of mechanically venti-
third intercostal space at the midclavicular line. McEwen 2 lated sheep. Cardiac output decreased as the degree of
favored empiric placement of the needle in the fourth or pneumothorax increased, even before the entire lung was
collapsed and before mediastinal shift was seen on chest
fifth intercostal space, anterior axillary line, but Ross 1
believed that the lateral approach is less safe. He argued radiograph. In another report, radiographically small pneu-
mothoraces resulted in severe cardiopulmonary compro-
that because free air in the pleural space theoretically rises
mise in mechanically ventilated patients with adult respira-
to the high anterior chest, the lateral approach presents a
tory distress syndrome, lo Tension physiology developed in
greater risk of lung injury if a large pneumothorax is not
some of these patients despite a functioning ipsilateral chest
present. Also, one is more likely to encounter pleural
tube because the pneumothoraces were loculated.
adhesions using the lateral approach because they are
more prevalent in dependent areas of the thorax.
SUMMARY
Empiric needle decompression of the chest is not with-
out risks. At best, if a tension pneumothorax is present, A patient with chronic obstructive pulmonary disease was
thoracentesis converts the injury to a simple pneumotho- intubated because of acute respiratory failure and soon suf-
tax. On the other hand, if the diagnosis is wrong and the fered cardiovascular collapse. A left-sided tension pneu-
lung is inflated normally, thoracentesis actually can pro- mothorax was diagnosed and treated quickly, but a subse-
duce a pneumothorax. This outcome can be minimized quent right-sided tension pneumothorax was missed
by attaching the needle to a water seal or syringe. Even if because needle thoracostomy did not vent air under pres-
it does not create a simple pneumothorax, thoracentesis sure. An autopsy suggested that the needle thoracostomy
produces a tiny pleural puncture wound that, in concert was falsely negative because it sampled air from a noncom-
with positive-pressure ventilation, can result in a tension municating bulla rather than from the pleural space.
pneumothorax. For this reason, in intubated patients, In intubated patients, tension physiology can exist with
tube thoracostomy is the preferred technique to empiri- only localized collapse of a lung, and diagnostic needle
cally exclude tension pneumothorax when time permits, t thoracostomy can be falsely negative. When a high index
The case described here also shows that needle thora- of suspicion for tension pneumothorax is present in very
costomy is not a perfectly sensitive test to detect tension unstable patients, empiric tube thoracostomy is a reason-
able first step and a mandatory second step if initial
pneumothorax. Moreover, it illustrates an important point
thoracentesis does not yield expected results.
about clinical reasoning. A single negative diagnostic test
result that does not concur with a strong clinical suspicion
should make the physician question whether this is a false- REFERENCES
1, RossDS: Thoracentesis,in RobertsJR, HedgesJR (eds): ClinicalProceduresin Emergency
negative result> In retrospect, it would have been reason- Medicine, ed 2. Philadelphia, WB Saunders, 1991, p 114-117.
able for the physicians here to proceed with a right-sided 2. McEwenJl: Pleural disease, in RosenP, Barkin RM (eds): EmergencyMedicine: Conceptsand
tube thoracostomy despite the negative thoracentesis. Clinical Practice, ed 3. Philadelphia, MosbyYear Book,1992, p 1121-1131.
MAY 1993 22:5 ANNALS OF EMERGENCY MEDICINE 86 5 / 1 3 5
TENSION PNEUMOTHORAX
M~nes & Abbuhl
I II
3. Vukich DJ. Markovchick V: Thoracic trauma, in RosenP, 8arkin RM (eds): EmergencyMedicine: The authors are grateful to Lawrence Kenyon, MD, for the autopsy photograph.
Concepts and Clinical Practice, ed 3. Philadelphia, Mosby Year Book, 1992, p 434-436.
4. Rojas R, Wasserberger J, BalasubramaniamS: Unsuspectedtension pneumethoraxas a
Address for reprints:
hidden cause of unsuccessful resuscitation (letter). Ann EmargMad 1983;12:411-412.
5. Oalbec DL, Krome RL: Thoracostomy.EmergMad Clin North Am 1986;4:441-457. Daniel Mines, MD
6. Vukich DJ: Pneumothorax,hemothorax, and other abnormalities of the pleural space. Emerg Emergency Department, Ground Silverstein
Mad Clin North Am 1983;1:431-444. Hospital of the University of Pennsylvania
7. American College of SurgeonsCommittee on Trauma: Advanced TraumaLife Support Course 3400 Spruce Street
Student Manual. Chicago,ACS, 1989, p 93.
Philadelphia, Pennsylvania 19104-4283
8. KassirerJP, KopelmanBl: Learning Clinical Reasoning.Baltimore, Williams & Wilkins, 1991.
9. Bitto T, Mannien JD, StephensonLW, et al: Pneumothoraxduring positive-pressure
mechanical ventilation. J ThoracCardiovascSurg 1985;89:585-591.
10. Gobien RP, Reines HD, Schabel SI: Localizedtension pneumethorax:Unrecognizedform of
barotrauma in adult respirator,/distress syndrome. Radiology 1982;142:15-19.
1 3 6 / 866 ANNALS OF EMERGENCY MEDICINE 22:5 MAY 1993
You might also like
- Constellations A PlayDocument88 pagesConstellations A PlayMora Gabaroni89% (18)
- Tension PneumothoraxDocument19 pagesTension PneumothoraxRupita SitanggangNo ratings yet
- MG II Sem 20 - Limba EnglezaDocument12 pagesMG II Sem 20 - Limba EnglezaMădălina Stănășel0% (1)
- Guitar Lesson PlansDocument13 pagesGuitar Lesson PlansjamieholroydNo ratings yet
- Chest Trauma Pneumothorax - TensionDocument5 pagesChest Trauma Pneumothorax - Tensionmita susantiNo ratings yet
- PneumothoraxDocument13 pagesPneumothoraxRex NamudNo ratings yet
- Chest Trauma Pneumothorax - TensionDocument4 pagesChest Trauma Pneumothorax - TensionAndi HakimNo ratings yet
- Tension PneumothoraxDocument5 pagesTension PneumothoraxKay BristolNo ratings yet
- Class 1 ED (Pneumothorax Paper)Document31 pagesClass 1 ED (Pneumothorax Paper)Shafiq KadirNo ratings yet
- Partial Lobar Collapse of Lung in Young Adult: A Case ReportDocument3 pagesPartial Lobar Collapse of Lung in Young Adult: A Case ReportGusti Ngurah PNo ratings yet
- Gambaran Emergensi ThoraxDocument15 pagesGambaran Emergensi Thoraxsteven hkNo ratings yet
- Young Man With Cardiac Arrest Secondary To Undiagnosed Mediastinal MassDocument4 pagesYoung Man With Cardiac Arrest Secondary To Undiagnosed Mediastinal MassPxPPxH ChanNo ratings yet
- Pneumothora X: Oleh: Dela Oktarini, S.Ked Pembimbing: Dr. Amran Sinaga, SP.BDocument20 pagesPneumothora X: Oleh: Dela Oktarini, S.Ked Pembimbing: Dr. Amran Sinaga, SP.BSafira Amilia RamadaniNo ratings yet
- Chest Trauma SeminarDocument45 pagesChest Trauma Seminarha9719199No ratings yet
- Chapter 4: Thoracic Trauma ObjectivesDocument29 pagesChapter 4: Thoracic Trauma ObjectivesDeborah Anasthasia PakpahanNo ratings yet
- 150+ Cases in Chest XrayDocument21 pages150+ Cases in Chest XrayMuntadher KareemNo ratings yet
- Pneumothorax: Dr. Ibnu DharmajatiDocument16 pagesPneumothorax: Dr. Ibnu DharmajatiIbnu DharmajatiNo ratings yet
- Diagnosis of Pneumothorax in Critically Ill Adults: James J Rankine, Antony N Thomas, Dorothee FluechterDocument6 pagesDiagnosis of Pneumothorax in Critically Ill Adults: James J Rankine, Antony N Thomas, Dorothee FluechternovywardanaNo ratings yet
- Re Expansion Pulmonary EdemaDocument4 pagesRe Expansion Pulmonary EdemarendyjiwonoNo ratings yet
- Lecture 5 Pneumonia and SepsisDocument9 pagesLecture 5 Pneumonia and Sepsishenlo hiNo ratings yet
- PneumothoraxDocument36 pagesPneumothoraxEira Lopez50% (6)
- Clinical Aspects of PneumothoraxDocument3 pagesClinical Aspects of PneumothoraxelisabethNo ratings yet
- Surgery TCVS SGD Guide KKDocument7 pagesSurgery TCVS SGD Guide KKFu Xiao ShanNo ratings yet
- Learning Objectives: Niken Rahmatia 1418011152Document17 pagesLearning Objectives: Niken Rahmatia 1418011152Taro RahmatiaNo ratings yet
- TENSION PNEUMOTHORAX (Malav Shah)Document66 pagesTENSION PNEUMOTHORAX (Malav Shah)Sharath PsNo ratings yet
- NAME: Neema Tamang Roll No:-20 Subject:-Surgery Assignment Topic:-Pneumothorax Faculty: HA 2Document9 pagesNAME: Neema Tamang Roll No:-20 Subject:-Surgery Assignment Topic:-Pneumothorax Faculty: HA 2Shreekrishna BudhathokiNo ratings yet
- Atrial Septal Defect Presenting As Recurrent Amoebic Lung AbscessDocument2 pagesAtrial Septal Defect Presenting As Recurrent Amoebic Lung AbscessBill RajagukgukNo ratings yet
- Pneumothorax: Xie Can Mao 1st Affiliated Hospital of Sun Yat-Sen UniverstyDocument95 pagesPneumothorax: Xie Can Mao 1st Affiliated Hospital of Sun Yat-Sen UniverstySalman HabeebNo ratings yet
- PneumothoraxDocument95 pagesPneumothoraxYan Sheng HoNo ratings yet
- Main Strem BroncusDocument2 pagesMain Strem BroncusSri BayaniNo ratings yet
- Bilateral Tension Pneumothorax Following Equipment ImprovisationDocument6 pagesBilateral Tension Pneumothorax Following Equipment ImprovisationIlvita MayasariNo ratings yet
- Adenotonsillar Hypertrophy As A Cause of Pulmonary HypertensionDocument4 pagesAdenotonsillar Hypertrophy As A Cause of Pulmonary HypertensionRozadila EsrianaNo ratings yet
- PneumothoraxDocument43 pagesPneumothoraxSravani KanchiNo ratings yet
- Tension Pneumothorax: History and PhysicalDocument5 pagesTension Pneumothorax: History and PhysicalKenneth AndayaNo ratings yet
- Prof. M. A. Wahab Department of Medicine Holy Family Red Crescent Medical College HospitalDocument6 pagesProf. M. A. Wahab Department of Medicine Holy Family Red Crescent Medical College Hospitalram krishnaNo ratings yet
- Clinical Review - FullDocument5 pagesClinical Review - FullAhmad SaifuddinNo ratings yet
- Simultaneous Bilateral Primary Spontaneous Pneumothorax (2019)Document7 pagesSimultaneous Bilateral Primary Spontaneous Pneumothorax (2019)sandi_prawira_yudhaNo ratings yet
- Pneumothorax: From Definition To Diagnosis and Treatment: Review ArticleDocument5 pagesPneumothorax: From Definition To Diagnosis and Treatment: Review ArticleRiani NazilaNo ratings yet
- Trauma Thorax: Disusun Oleh: Uray Ria ApriniDocument22 pagesTrauma Thorax: Disusun Oleh: Uray Ria ApriniUray RiaNo ratings yet
- Tension Pneumothorax Following Open Cholecystectomy Under General AnaesthesiaDocument2 pagesTension Pneumothorax Following Open Cholecystectomy Under General AnaesthesiaIndra NasutionNo ratings yet
- Knapp-Seltzer1979 Article UnilateralPulmonaryOedemaACaseDocument3 pagesKnapp-Seltzer1979 Article UnilateralPulmonaryOedemaACaseFandirisuNo ratings yet
- Pneumothorax: Narmada Kasuni Group 25 5 Year 1 SemesterDocument18 pagesPneumothorax: Narmada Kasuni Group 25 5 Year 1 SemesterNarmada PemathilakaNo ratings yet
- Pneumothorax: Dr. Sivaraj KarriDocument50 pagesPneumothorax: Dr. Sivaraj KarriYamini ChowdaryNo ratings yet
- Pneumothorax FinalDocument62 pagesPneumothorax FinalmithramuruganNo ratings yet
- Subcutaneous Emphysema PDFDocument5 pagesSubcutaneous Emphysema PDFMarcella SaputraNo ratings yet
- Gambaran Radiologis Pada Kegawatan Paru: Farah Fatma WatiDocument42 pagesGambaran Radiologis Pada Kegawatan Paru: Farah Fatma WatisabariaNo ratings yet
- Pneumothorax, Tension and TraumaticDocument24 pagesPneumothorax, Tension and TraumaticSatria WibawaNo ratings yet
- Pneumothorax and AsthmaDocument8 pagesPneumothorax and AsthmaKyle FernandezNo ratings yet
- Case 12749: Spontaneous Pneumothorax: A Complication of TuberculosisDocument8 pagesCase 12749: Spontaneous Pneumothorax: A Complication of TuberculosisSanyuki KhoirunnisaNo ratings yet
- Articulo. Neumomediastino EspontaneoDocument3 pagesArticulo. Neumomediastino EspontaneoEdRooNo ratings yet
- Clinical Presentation and Diagnosis of PneumothoraxDocument49 pagesClinical Presentation and Diagnosis of PneumothoraxisahNo ratings yet
- Articulo Parcial 1 Urgencias Respiratorias Perros y GatosDocument23 pagesArticulo Parcial 1 Urgencias Respiratorias Perros y GatosYara Valentina Toledo ManriqueNo ratings yet
- Chest: Postgraduate Education CornerDocument8 pagesChest: Postgraduate Education CornerCristian LermaNo ratings yet
- Pneumothorax: David E. Manthey and Bret A. NicksDocument9 pagesPneumothorax: David E. Manthey and Bret A. NicksJha BhoenkNo ratings yet
- Dr. Dicky SP.P Materi Gawat Darurat ParuDocument41 pagesDr. Dicky SP.P Materi Gawat Darurat ParuYuni SaviraNo ratings yet
- Hafizah Hoshni PneumothoraxDocument47 pagesHafizah Hoshni PneumothoraxhafizahhoshniNo ratings yet
- Chest TraumaDocument39 pagesChest TraumaQuinnee VallejosNo ratings yet
- Bronchial Artery Pseudoaneurysm and Mediast - 2021 - Archivos de BronconeumologDocument2 pagesBronchial Artery Pseudoaneurysm and Mediast - 2021 - Archivos de BronconeumologMomoh GaiusNo ratings yet
- Nejm 200003233421207Document7 pagesNejm 200003233421207Ami DhaniaNo ratings yet
- 10 1097@SCS 0b013e31821d4dc9Document41 pages10 1097@SCS 0b013e31821d4dc9Sagar LodhiaNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- Anesthesia in Thoracic Surgery: Changes of ParadigmsFrom EverandAnesthesia in Thoracic Surgery: Changes of ParadigmsManuel Granell GilNo ratings yet
- MG II Sem 18 - Limba EnglezaDocument10 pagesMG II Sem 18 - Limba EnglezaMădălina StănășelNo ratings yet
- MG II Sem 19 - Limba EnglezaDocument13 pagesMG II Sem 19 - Limba EnglezaMădălina StănășelNo ratings yet
- Acl LINUXDocument13 pagesAcl LINUXMădălina StănășelNo ratings yet
- Can Tey 2016Document8 pagesCan Tey 2016Mădălina StănășelNo ratings yet
- A Novel Structural Risk Index For Primary Spontaneous Pneumothorax: Ankara Numune Risk IndexDocument5 pagesA Novel Structural Risk Index For Primary Spontaneous Pneumothorax: Ankara Numune Risk IndexMădălina StănășelNo ratings yet
- Buenaventura vs. CA (G.R. No. 126376, November 20, 2003)Document7 pagesBuenaventura vs. CA (G.R. No. 126376, November 20, 2003)Stephen Neil Casta�oNo ratings yet
- Specimen Y9 Entrance ExamDocument7 pagesSpecimen Y9 Entrance ExamJayaletchumi MoorthyNo ratings yet
- Safety in Drilling ManualDocument151 pagesSafety in Drilling Manualstoianz100% (1)
- National Iron Plus Initiative Guidelines For Controlof IDADocument19 pagesNational Iron Plus Initiative Guidelines For Controlof IDAvvirumbi100% (1)
- Legal Theory LL.M.Document6 pagesLegal Theory LL.M.adv.abhimanyu.jadhavNo ratings yet
- Pozlaćena Fibula SirmiumDocument12 pagesPozlaćena Fibula SirmiumPero68No ratings yet
- File MP926-1 3079-101-1 3173603Document19 pagesFile MP926-1 3079-101-1 3173603heruassociates2555No ratings yet
- Lawrep 036 CSLJ JL 0245Document17 pagesLawrep 036 CSLJ JL 0245Jeckl100% (1)
- Booklet 1Document45 pagesBooklet 1Nora Beatriz DiazNo ratings yet
- Improving Access To Medicines For Non-Communicable Diseases in Rural India: A Mixed Methods Study Protocol Using Quasi-Experimental DesignDocument19 pagesImproving Access To Medicines For Non-Communicable Diseases in Rural India: A Mixed Methods Study Protocol Using Quasi-Experimental DesignNino AlicNo ratings yet
- Renacia Unit 2 Pretest and Activity 1Document3 pagesRenacia Unit 2 Pretest and Activity 1Erickajean Cornelio LabradorNo ratings yet
- Messiah - St. Bartholomew Episcopal Church The Nineteenth Sunday After PentecostDocument9 pagesMessiah - St. Bartholomew Episcopal Church The Nineteenth Sunday After PentecostIsaac BonneyNo ratings yet
- Kỳ Thi Chọn Học Sinh Giỏi Cấp TỉnhDocument17 pagesKỳ Thi Chọn Học Sinh Giỏi Cấp TỉnhNhok'ss Lì'ssNo ratings yet
- Maleficent Reaction PaperDocument1 pageMaleficent Reaction PaperShaina Baldemoro100% (3)
- Alcpt 21R (Script)Document18 pagesAlcpt 21R (Script)Matt Dahiam RinconNo ratings yet
- Evolution of MedicineDocument6 pagesEvolution of MedicineAssignmentLab.comNo ratings yet
- Transformation of Housing Policy in India - The Trend Towards Market MechanismsDocument8 pagesTransformation of Housing Policy in India - The Trend Towards Market MechanismsVaidish SumariaNo ratings yet
- EOs PDFDocument91 pagesEOs PDFArushee BhatnagarNo ratings yet
- Submission Deadline Marks and FeedbackDocument4 pagesSubmission Deadline Marks and Feedbackramanpreet kaurNo ratings yet
- CloseupDocument4 pagesCloseupWilliam DsouzaNo ratings yet
- United States v. Rodney Thompson, 4th Cir. (1999)Document6 pagesUnited States v. Rodney Thompson, 4th Cir. (1999)Scribd Government DocsNo ratings yet
- Review 1Document4 pagesReview 1Wei Yi100% (1)
- MTT 52 Hindi July 2023 January 2024Document23 pagesMTT 52 Hindi July 2023 January 2024Sujeet GuptaNo ratings yet
- Mathematical Logic in The Human BrainDocument23 pagesMathematical Logic in The Human BrainEugenia LupuNo ratings yet
- Which Sword Prophet Used Against His Enemies?Document152 pagesWhich Sword Prophet Used Against His Enemies?Moiz Uddin QidwaiNo ratings yet
- SCAFFOLDING Gibbons ChapterDocument29 pagesSCAFFOLDING Gibbons ChapterNeni WinartiNo ratings yet
- JSS 3 Sos 1ST Term ExamDocument11 pagesJSS 3 Sos 1ST Term ExamAmaraNo ratings yet
- Williams Diamond Mines of South Africa I High ResDocument463 pagesWilliams Diamond Mines of South Africa I High ResFarlangNo ratings yet