Professional Documents
Culture Documents
Hematological Profile and Pregnancy: A Review
Hematological Profile and Pregnancy: A Review
Uploaded by
dinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematological Profile and Pregnancy: A Review
Hematological Profile and Pregnancy: A Review
Uploaded by
dinaCopyright:
Available Formats
International Journal of Advances in Medicine
Kaur S et al. Int J Adv Med. 2014 Aug;1(2):68-70
http://www.ijmedicine.com pISSN 2349-3925 | eISSN 2349-3933
DOI: 10.5455/2349-3933.ijam20140804
Review Article
Hematological profile and pregnancy: a review
Simran Kaur1, Sabina Khan2*, Aruna Nigam3
1
Department of Physiology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India
2
Department of Pathology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India
3
Department of Obstetrics & Gynecology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New
Delhi, India
Received: 3 July 2014
Accepted: 19 July 2014
*Correspondence:
Dr. Sabina Khan,
E-mail: drsabina1@gmail.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Many physiological hematological changes occur during pregnancy to accommodate the demands of the developing
foetus. Infect, these changes may appear to be pathological in the non-pregnant state. Although physiological in
nature, but abnormal hematological profile does affect pregnancy and its outcome. One of the most important
underlying cause of maternal mortality is due to underlying hematological complications. This review deals with
thorough understanding of range of these haematological parameters during pregnancy.
Keywords: Hematological parameters, Physiology, Pregnancy
INTRODUCTION These changes revert back to normal after puerperium. 3
But, these changes are required to meet metabolic
Maternal mortality is defined as ‘the death of a woman demands of mother and also ensure adequate oxygen
while pregnant or within 42 days of the end of pregnancy, delivery to fetus.4 Depending upon the degree of change
from any cause related to or aggravated by the pregnancy in the hematological profile, the pregnancy outcome may
or its management, but not from accidental or incidental vary.5
cause’.1 Maternal mortality is the vital indicator with the
greatest disparity between developed and developing Thus, it becomes important to monitor hematological
countries. It is necessary to determine the cause of parameters during pregnancy, thereby improving its
maternal mortality for the prevention as well as making outcome.
the action plan for targeting the health goals.
CHANGES IN BLOOD VOLUME
According to World Health Organization, one woman
dies every minute from a pregnancy-related complication. Blood volume begins to increase as early as 6 weeks of
The main causes causing mortality are due to antepartum gestation and increases to more than 50% of the
and postpartum hemorrhage, unsafe abortion, eclampsia, prepregnant state.1,6 The change in plasma volume during
obstructed labour and infection2 .Thus, it is important to pregnancy is attributed to increased plasma renin activity
know variation in hematological profile during the entire and reduced atrial natriuretic peptide levels. The
course of pregnancy as well as delivery such that adverse hormonal changes are due to pregnancy induced systemic
incidents leading to maternal mortality can be minimized. vasodilatation and increased vascular capacitiance.3,7
After delivery the plasma volume gradually comes to
Many physiological hematological changes occur during prepregnant values as a result of diuresis.
pregnancy due to continuous development of fetus. 2
International Journal of Advances in Medicine | July-September 2014 | Vol 1 | Issue 2 Page 68
Kaur S et al. Int J Adv Med. 2014 Aug;1(2):68-70
PHYSIOLOGICAL ANEMIA There is also evidence of bone marrow hyperplasia with
neutrophilic leukocytosis during last trimester of
There occur no change in the hemoglobin concentration pregnancy.24
till 16th week of gestation but thereafter, there is a steady
fall to reach the nadir in second trimester as a result of Leukocyte and neutrophil count increased significantly
expansion of plasma volume. A similar trend is seen in on day 1 but start decreasing until fifth day, when the
the PCV and the RBC count.8 The increase in red cell and value returns back to normal.25 This important finding
hemoglobin mass is reported to be maximum at 12-28 should always be kept in mind to avoid the unnecessary
weeks of pregnancy.9 There is little change in red blood use of antibiotic in the postpartum period.
cell indices during pregnancy. The underlying cause of
anemia during pregnancy is hemodilution i.e. rise in GESTATIONAL THROMBOCYTOPENIA
plasma volume more as compared to increase in the red
cell mass (40% vs. 20% respectively).3 This is also called Although the average platelet count decreases
as ‘physiological anemia of pregnancy’.10 It is advised to monotonically in pregnancy, there is an increase in
maintain the hemoglobin level at or above 11 g/dl and platelet aggregation especially during last 8 weeks of
should not be allowed to fall below 10.5 g/dl in any gestation.26 It has been reported that there can occur
trimester.11 significant fall in platelet count from 32 weeks gestation
onwards.27 Increased consumption of platelets as well as
These parameters are important to be kept above the decreased life span in the uteroplacental circulation has
reference levels as significantly poor positive correlations been suggested to be the explanation of the reduction in
were found between birth weight of newborns and the number of circulating platelets during pregnancy.27
maternal serum hemoglobin, hematocrit and MCV Platelet count as well as other hemostatic factors return to
levels.12 Haemoglobin showed a positive correlation with normal after 6 weeks of delivery.28
newborn length and did not correlate with weight
probably because length is more stable than weight.13 It is After anemia, most common hematological abnormality
seen that, haemoglobin and haematocrit increases on day during pregnancy is thrombocytopenia.29 Especially, as
1 after delivery, reduced on days 3 and 5 then started we call it ‘gestational thrombocytopenia’ which is partly
rising such that by day 42, the normal haemoglobin in due to hemodilution and partly due to increased platelet
non-pregnant women was achieved.14 activation and accelerated clearance.27 Gestational
thrombocytopenia requires no specific treatment and
CHANGES IN WBC COUNT corrects itself spontaneously after delivery but the other
etiologies must be excluded i.e. megaloblastic anemia,
The other prominent change in the hematological profile immune thrombocytopenia, thrombotic microangiopathy
during pregnancy is leukocytosis which is due to syndromes, eclampsia and liver disorders before labeling
physiological stress. This rise occur early in pregnancy the patient as gestational thrombocytopenia.29
and remain elevated throughout pregnancy.15 There WBC
count during healthy pregnancy vary from 6 × 10 9-16 × CONCLUSION
109/L which further increases to 9 × 109-25 × 109/L hours
after delivery.16 It takes 4 weeks time for WBC count to Hematological parameters are the routinely performed
come back to normal after delivery.17 investigations during pregnancy and after delivery. Thus
it is important to know the normal variation in all the
The leukocytosis is due to increased inflammatory parameters throughout the pregnancy and puerperium and
response during normal pregnancy, which can be as a reason behind them. The proper interpretation of this
consequence of selective immune tolerance, routinely performed parameters help in early recognition
immunosuppression and immunomodulation of fetus. 18 of impending antepartum and postpartum complications
However one study proposes that this increase in The physiological leukocytosis should always be kept in
leucocyte count is seen only after normal spontaneous mind while using antibiotics during postpartum period so
delivery.19 Tzur et al. has shown that leukocytosis during as to minimize its unnecessary use.
first trimester is associated with complications during
pregnancy.20 Thus it is important to interpret and correlate Funding: No funding sources
the clinical findings with leukocyte count throughout Conflict of interest: None declared
pregnancy and puerperium. Ethical approval: Not required
Amongst leucocytes, there is preponderance of the REFERENCES
neutrophils on differential counts which is due to
impaired neutrophilic apoptosis in pregnancy. 21,22 1. Datta D, Datta P. Maternal mortality in india:
Neutrophil counts during pregnancy can double up twice problems and strategies. Asian J Med Res.
to its postpartum values. The monocytosis occurs during 2013;2(1):31-5.
pregnancy but the other cells in differential count i.e. 2. Chandra S, Tripathi A, Mishra S, Amzarul M.
lymphocyte, eosinophil and basophil decline in number. 23 Physiological changes in hematological parameters
International Journal of Advances in Medicine | July-September 2014 | Vol 1 | Issue 2 Page 69
Kaur S et al. Int J Adv Med. 2014 Aug;1(2):68-70
during pregnancy. Indian J Hematol Blood Transfus. normal pregnancy. Eur J Obstet Gynecol Reprod
2012;28(3):144-6 Biol. 2008;136(1):16-9.
3. Dennen F, Ocaña J, Karasik S, Egan L, Paredes N, 16. Wadsworth GR. Blood-volume: a commentary.
Flisser A, et al. Comparison of hemodynamic, Singapore Med J. 2002;43(8):426-31.
biochemical and hematological parameters of 17. Ramsay M. Changes in WBC count. In: Sue Pavord,
healthy pregnant women in the third trimester of Beverley Hunt, eds. Obstetric Hematology Manual.
pregnancy and the active labor phase. BMC London: Guy’s and St. Thomas’ NHS Foundation
Pregnancy Childbirth. 2011;11:33. Trust and King’s College; 2010: 92-98.
4. Salas SP, Rosso P, Espinoza R, Robert JA, Valdes 18. Osonuga IO, Osonuga OA, Onadeko AA, Osonuga
G, Donoso E. Maternal plasma volume expansion A, Osonuga AA. Hematological profile of pregnant
and hormonal changes in women with idiopathic women in southwest of Nigeria. Asian Pac J Trop
fetal growth retardation. Obstet Gynecol. Dis. 2011;1:232-4.
1993;81:1029-33. 19. Delgado I, Neubert R, Dudenhausen W. Changes in
5. Akinbami AA, Ajibola SO, Rabiu KA, Adewunmi white blood cells during parturition in mothers and
AA, Dosunmu AO, Adediran A, et al. newborn. Gynecol Obstet Invest. 1994;38:227-35
Hematological profile of normal pregnant women in 20. Tzur T, Weintraub AY, Sergienko R, Sheiner E.
Lagos, Nigeria. Int J Women’s Health. Can leukocyte count during the first trimester of
2013;5(1):227-32 pregnancy predict later gestational complications?
6. Lind T. Hematologic system. Maternal physiology. Arch Gynecol Obstet. 2013 Mar;287(3):421-7.
Washington: CREOG. 1985;25:7-40. 21. Konijnenberg A, Stokkers E, Vander Post J, Schaap
7. Bernstein IM, Ziegler W, Badger GJ. Plasma M, Boer K, Bleker O, et al. Extensive platelet
volume expansion in early pregnancy. J Obstet activation in preeclampsia compared with normal
Gynecol. 2001;97:669 pregnancy: enhanced expression of cell adhesion
8. DeMayer EM, Tegman A. Prevalence of anaemia in molecules. Am J Obstet Gynecol. 1997;176(2):461-
the world. WHO Qlty. 1998;38:302-16. 9.
9. Whittaker PG, Macphail S, Lind T. Serial 22. Gatti L, Tinconi PM, Guarneri D, Bertuijessi C,
haematological changes and pregnancy outcome. Ossola MW, Bosco P, et al. Hemostatic parameters
Obstet Gynecol. 1996;88(1):33-9. and platelet activation by flow-cytometry in normal
10. James TR, Reid HL, Mullings MA. Are published pregnancy: a longitudinal study. Internat J Clin Lab
standards for hemtological indices in pregnancy Res. 1994;24(4):217-9
applicable across populations: an evaluation in 23. Pitkin RM, Witte DL. Platelet and leukocyte counts
healthy pregnant Jamacian women. BMC Pregnancy in pregnancy. JAMA. 1979;242(24):2696-8.
Childbirth. 2008;8:8. 24. Verma A, Chaudhary H. Study of hematological
11. Sharma P, Nagar R. Hematological profile of parameters in advanced pregnancy. Int J Recent
anemic pregnant women attending antenatal Trends Sci Technol. 2013;7(1):16-9.
hospital. IOSR J Nurs Health Sci. 2013;1(4):11-5. 25. Onwukeme KE. Puerperal haematological indices in
12. Mwinga K, Vermund S, ChenY, Mwatha A, Read J, the Nigerian. Afr J Med Med Sci. 1992;21(2):51-5.
Urassa W, et al. Selected hematologic and 26. Fay RA, Hughes AO, Farron NT. Platelets in
biochemical measurements in African HIV-infected pregnancy: hyperdestruction in pregnancy. Obstet
and uninfected pregnant women and their infants: Gynecol. 1983;61:238-40.
the HIV prevention trials network 024 protocol. 27. Ahmed Y, van Iddekinge B, Paul C, Sullivan MHF,
BMC Pediatrics. 2009;9:49. Elder MG. Retrospective analysis of platelet
13. Papadopol V, Damian O, Palimaru I, Adam C, numbers and volumes in normal pregnancy and pre-
Florescu N, Damaceanu D. Maternal hematological eclampsia. Br J Obstet Gynecol. 1993;100:216-20.
and biochemical parameters and pregnancy 28. Shehlata N, Burrows RF, Kelton JG. Gestational
outcome. J Prev Med. 2001;9(3):27-33. thrombocytopenia. Clin Obstet Gynecol.
14. Ramakers C, van der Woude DA, Verzijl JM, 1999;42:327-34
Pijnenborg JM, van Wijk EM. An added value for 29. Khellaf M, Loustau V, Bierling P, Michel M,
the hemoglobin content in reticulocytes (CHr) and Godeau B. Thrombocytopenia and pregnancy. Rev
the mean corpuscular volume (MCV) in the Med Intern. 2012 Aug;33(8):446-52.
diagnosis of iron deficiency in postpartum anemic
women. Int J Lab Hematol. 2012 Oct;34(5):510-6. DOI: 10.5455/2349-3933.ijam20140804
15. Lurie S, Rahamim E, Piper R, Golan A, Sadan O. Cite this article as: Kaur S, Khan S, Nigam A.
Total and differential leukocyte counts percentiles in Hematological profile and pregnancy: a review. Int J
Adv Med 2014;1:68-70.
International Journal of Advances in Medicine | July-September 2014 | Vol 1 | Issue 2 Page 70
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Jolly Grammar Programme P1-6Document8 pagesJolly Grammar Programme P1-6Mandy Whorlow100% (3)
- Non Aero Revenue - MBA ProjectDocument68 pagesNon Aero Revenue - MBA ProjectSuresh Kumar100% (2)
- GIDC Rajju Shroff ROFEL Institute of Management Studies: Subject:-CRVDocument7 pagesGIDC Rajju Shroff ROFEL Institute of Management Studies: Subject:-CRVIranshah MakerNo ratings yet
- LEARNING THEORIES Ausubel's Learning TheoryDocument17 pagesLEARNING THEORIES Ausubel's Learning TheoryCleoNo ratings yet
- Minimal Stimulation IVF Vs Conventional IVFDocument8 pagesMinimal Stimulation IVF Vs Conventional IVFpolygoneNo ratings yet
- Referee Report TemplateDocument2 pagesReferee Report TemplateAna Jufriani100% (1)
- Ethnomedical Knowledge of Plants and Healthcare Practices Among The Kalanguya Tribe in Tinoc, Ifugao, Luzon, PhilippinesDocument13 pagesEthnomedical Knowledge of Plants and Healthcare Practices Among The Kalanguya Tribe in Tinoc, Ifugao, Luzon, PhilippinesJeff Bryan Arellano HimorNo ratings yet
- Roger Dale Stafford, Sr. v. Ron Ward, Warden, Oklahoma State Penitentiary at McAlester Oklahoma Drew Edmondson, Attorney General of Oklahoma, 59 F.3d 1025, 10th Cir. (1995)Document6 pagesRoger Dale Stafford, Sr. v. Ron Ward, Warden, Oklahoma State Penitentiary at McAlester Oklahoma Drew Edmondson, Attorney General of Oklahoma, 59 F.3d 1025, 10th Cir. (1995)Scribd Government DocsNo ratings yet
- Piglia - Hotel AlmagroDocument2 pagesPiglia - Hotel AlmagroJustin LokeNo ratings yet
- Schedule CDocument273 pagesSchedule CAzi PaybarahNo ratings yet
- Web-2012-Allison 250-C18 T63-T700 Gas Turbine EngineDocument4 pagesWeb-2012-Allison 250-C18 T63-T700 Gas Turbine Enginekillerghosts666No ratings yet
- Test Method For DDF ProjectDocument13 pagesTest Method For DDF ProjectrantosbNo ratings yet
- OutDocument318 pagesOutBet HalNo ratings yet
- Human Resource Management PrelimsDocument2 pagesHuman Resource Management PrelimsLei PalumponNo ratings yet
- The Law of ParkinsonDocument5 pagesThe Law of Parkinsonathanassiadis2890No ratings yet
- If ملخص قواعدDocument2 pagesIf ملخص قواعدAhmed GaninyNo ratings yet
- Fped 07 00310Document6 pagesFped 07 00310Fariz HidayatNo ratings yet
- Dermatology TreatmentsDocument6 pagesDermatology TreatmentsMayar MostafaNo ratings yet
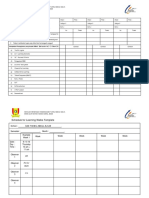
- Teacher Learning Walk Templates - 2017 - 1Document13 pagesTeacher Learning Walk Templates - 2017 - 1Zakaria Md SaadNo ratings yet
- DoomsdayDocument29 pagesDoomsdayAsmita RoyNo ratings yet
- Alaina Dauscher - Career Journal #01Document2 pagesAlaina Dauscher - Career Journal #01Alaina DauscherNo ratings yet
- Stones Unit 2bDocument11 pagesStones Unit 2bJamal Al-deenNo ratings yet
- 2020 Msce Practical Questions TargetDocument30 pages2020 Msce Practical Questions TargetspinyblessingNo ratings yet
- Commerce: Paper 7100/01 Multiple ChoiceDocument7 pagesCommerce: Paper 7100/01 Multiple Choicemstudy123456No ratings yet
- Case Study of A Condemned Boiler & Methods To Re-Establish ItDocument43 pagesCase Study of A Condemned Boiler & Methods To Re-Establish Its sivaNo ratings yet
- User Manual of CUBOIDDocument50 pagesUser Manual of CUBOIDshahinur rahmanNo ratings yet
- DS Masteri An PhuDocument174 pagesDS Masteri An PhuPhong PhuNo ratings yet
- ANALE - Stiinte Economice - Vol 2 - 2014 - FinalDocument250 pagesANALE - Stiinte Economice - Vol 2 - 2014 - FinalmhldcnNo ratings yet
- Sculpt Unbelievable Abs: Eight Potent Exercises That Zero in On Your AbdominalsDocument8 pagesSculpt Unbelievable Abs: Eight Potent Exercises That Zero in On Your Abdominalsjesus alamillaNo ratings yet
- A320 PedestalDocument14 pagesA320 PedestalAiman ZabadNo ratings yet