Professional Documents
Culture Documents
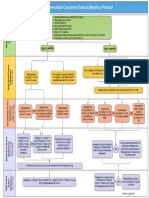
Clinical Asthma Pathway: ED Phase 1a: Initial Assessment - 1st Hour
Clinical Asthma Pathway: ED Phase 1a: Initial Assessment - 1st Hour
Uploaded by
d'Agung NugrohoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Asthma Pathway: ED Phase 1a: Initial Assessment - 1st Hour
Clinical Asthma Pathway: ED Phase 1a: Initial Assessment - 1st Hour
Uploaded by
d'Agung NugrohoCopyright:
Available Formats
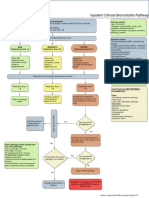
Clinical Asthma Pathway
For patients over two years without preexisting conditions.*
ED Phase 1a: Initial Assessment | 1st Hour Medication Dosing
ALL MEDICATIONS REQUIRE AN MD ORDER
RS 2-5:
Albuterol x1 **ED & Inpatient
RS 6-12: Albuterol dosing:
Reassess in 20-60 min
**Albuterol+ ipratropium <20 kg: 4 puff MDI or 2.5 mg nebulized
(max 3 doses)
RS 1: (max 3 doses); + prednisone, ≥20 kg: 8 puff MDI or 5 mg nebulized
*Consider steroids based on
Discharge with albuterol dexamethasone or
historical/clinical information Continuous albuterol via nebulizer:
methylprednisolone
*Consider ipratropium if more <20 kg: 10 mg/hr | ≥20 kg: 15 mg/hr
Consider adjunct therapies
than one dose of Albuterol Ipratropium bromide: 500 mcg nebulized
is needed. Prednisone or Prednisolone (oral):
1st dose: 2 mg/kg/day (max dose 60 mg/day)
Subsequently: 1-2 mg/kg/day
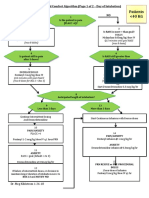
ED Phase 1b: Reassessment | 2nd Hour Dexamethasone: 0.3 mg/kg (max 10 mg)
Methylprednisolone:
RS 5-8: Admit RS 9-12: First dose: 2 mg/kg (max- 60mg)
Continuous albuterol Then: 1 mg/kg IV Q6h (max 125 mg/day)
RS 1-4: O2 sat <92% on 2LNC
O2 sat >92% on and Magnesium Indications for IV/IM steroids: Inability to tolerate PO or concern for
Discharge with or 40%FM:
2LNC or 40%FM: Consider BiPAP, magnesium Sulfate. Consider SQ/ inadequate (not adequate) GI absorption.
albuterol + steroid
Begin Phase 2 sulfate, chest X-ray, IM Terbutaline or
(if started in the ED) *Consider steroids if using albuterol q4 hours at home without
management continuous albuterol, Epinephrine, BiPAP, chest
clinical improvement or cough > 1 week
PICU consult X-ray, PICU consult.
Discharge/Home
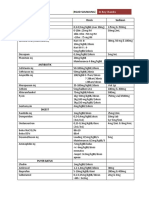
Inpatient: Phase 2 Albuterol dosing:
<20 kg: 2 puff MDI or 2.5 mg nebulized
≥20 kg: 4 puff MDI or 2.5 mg nebulized
Albuterol q2hrs; Respiratory score q2hrs; Initiate Discharge Plan (part of the asthma order set)
Adjunct Therapies
RS 1-4: RS 9-12: Magnesium sulfate IV: 50-75 mg/kg (max 2 gms) over 20 minutes
RS 5-8: (Consider administration of Normal Saline bolus)
Advance after one treatment Step back to previous phase or
Continue therapy in this phase
in this phase escalate care (see escalation box) Epinephrine (1:1000 = 1 mg/ml) or terbutaline (1 mg/ml):
0.01 ml/kg (max 0.4 ml) given SQ or IM q10-20min
Inpatient: Phase 3 *Exclusion
• Chronic lung disease (e.g. cystic fibrosis, restrictive lung disease,
Albuterol q3hrs; Respiratory score q3hrs bronchopulmonary dysplasia)
• Congenital and acquired heart disease
• Airway Issues (e.g. vocal cord paralysis, tracheomalacia,
RS 1-4: RS 9-12: tracheostomy dependent)
RS 5-8: • Medically complex children
Advance after one treatment Step back to previous phase or
Continue therapy in this phase • Immune disorders
in this phase escalate care (see escalation box)
• Sickle cell anemia
Consider alternate causes of hypoxia if oxygen saturation <94% when awake and <92% asleep (on room air) RN/RT to Notify MD
• For all phase transitions
Inpatient: Phase 4 •
•
Failure to advance on pathway after 12 hours in all inpatient phases
Persistent O2 requirement in Phase IV
• An increase in respiratory score
Albuterol q4hrs; Respiratory score q4hrs
Signs of Clinical Decline
RS 1-4: RS 9-12: • Drowsiness
RS 5-8: • Agitation
Discharge after one treatment Step back to previous phase or
Continue therapy in this phase • Confusion
in this phase escalate care (see escalation box)
• Silent chest exam
Notify MD and consider PMET activation
1. Completion of online education
2. Pharmacy education on use of spacer Escalation—Notify MD
3. Modification of home medications (if indicated) • Albuterol+Ipratromium bromide: 3 treatments q20mins over 1 hour
Discharge Plan 4. Asthma Action Plan • Magnesium sulfate
5. Appointment with PMD • Reassess after interventions
6. Appointment with subspecialty (if indicated) Consider PMET activation
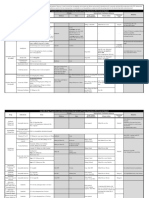
Respiratory Scoring Tool
Variable 0 Points 1 Point 2 Points 3 Points
RR
<2 months ≤60 61-69 ≥70
2-12 months ≤50 51-59 ≥60
13-23 months ≤40 41-44 ≥45
2-3 year ≤34 35-39 ≥40
4-5 year ≤30 31-35 ≥36
6-12 year ≤26 27-30 ≥31
>12 year ≤23 24-27 ≥28
3 of the following: subcostal,
2 of the following: subcostal, intercostal, substernal,
Retractions None Subcostal or intercostal intercostal, substernal OR nasal suprasternal, supraclavicular
flaring (infant) OR nasal flaring/head bobbing
(infant)
Dyspnea
1 of the following: difficulty 2 of the following: difficulty
Normal feeding, vocalizations Stops feeding, no vocalization,
0-23 months feeding, decreased vocalization feeding, decreased vocalization
and activity drowsy or confused
or agitated or agitated
1 of the following: decreased 2 of the following: decreased Stops eating or drinking,
Normal feeding, vocalizations
2-4 years appetite, increased coughing appetite, increased coughing stops playing, OR drowsy and
and play
after play, hyperactivity after play, hyperactivity confused
>4 years Counts to ≥10 in one breath Counts to 7-9 in one breath Counts to 4-6 in one breath Counts to ≤3 in one breath
Inspiratory and expiratory
Normal breathing, Expiratory wheeze only (greater
Auscultation End-expiratory wheeze only wheeze OR diminished breath
no wheezing present than end-expiratory wheeze)
sounds OR both
Adapted from: Liu LL, Gallaher MM, Davis RL, Rutter CM, Lewis TC, Marcuse EK. Use of a respiratory clinical score among different providers. Pediatr Pulmonol 2004;37(3):243-8.
You might also like
- Louis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFDocument2,424 pagesLouis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFPan50% (2)
- Common ICU DripsDocument1 pageCommon ICU DripsSunshine Willis100% (2)
- GMC Official PLAB 1 Question SampleDocument8 pagesGMC Official PLAB 1 Question Samplemuntaser100% (1)
- 2019 Practice of Anesthesia For Infants and ChildrenDocument2 pages2019 Practice of Anesthesia For Infants and ChildrenJavier GlezqNo ratings yet
- Nutrition Case StudyDocument30 pagesNutrition Case StudyCher BautistaNo ratings yet
- Dr. Rubi Li v. Spouses Reynaldo and Lina SolimanDocument2 pagesDr. Rubi Li v. Spouses Reynaldo and Lina Solimanralph_atmosferaNo ratings yet
- Medad TeamDocument18 pagesMedad TeamAxmed MaxamedNo ratings yet
- UNC ED Pediatric Asthma Protocol 1-29-15 KJRDocument2 pagesUNC ED Pediatric Asthma Protocol 1-29-15 KJRMax ImousNo ratings yet
- Drug Indications&DosagesDocument3 pagesDrug Indications&DosagesSAMWEL JOSIANo ratings yet
- Tablas de Dosificacion Kirk 9na EdDocument68 pagesTablas de Dosificacion Kirk 9na EdMarlieth Rosales HernandezNo ratings yet
- Dosis Obat AnakDocument3 pagesDosis Obat AnakhannaNo ratings yet
- Dosis Obat AnakDocument3 pagesDosis Obat Anakimam mulyadiNo ratings yet
- Ambulatory Care MedicineDocument26 pagesAmbulatory Care MedicineJustineValJadeLacabaNo ratings yet
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- Age 2 Months Age 2monthsDocument1 pageAge 2 Months Age 2monthsd'Agung NugrohoNo ratings yet
- FLCCC Alliance MATHplus Protocol ENGLISHDocument2 pagesFLCCC Alliance MATHplus Protocol ENGLISHBhanu Kumar100% (1)
- SDL Obat EmergencyDocument26 pagesSDL Obat EmergencyfarhantunichiaNo ratings yet
- Analgesia y Anestesia para ConejosDocument7 pagesAnalgesia y Anestesia para ConejosIgnacio Rosas TellezNo ratings yet
- 2015 Pain Management For PediatricDocument2 pages2015 Pain Management For Pediatricdiany astutiNo ratings yet
- AsthmaDocument2 pagesAsthmaAndrei MurariuNo ratings yet
- Igd RsudDocument6 pagesIgd RsudRidho FrihaNo ratings yet
- Drug Dosages KTHDocument20 pagesDrug Dosages KTHQazi Saadullah LatifNo ratings yet
- Picu NotesDocument65 pagesPicu NotesAhmed Mohammed100% (2)
- COVID19 - DexamethasoneDocument2 pagesCOVID19 - DexamethasoneLe Hoang TuanNo ratings yet
- Emrgency DrugsDocument4 pagesEmrgency Drugshacker ammerNo ratings yet
- FLCCC Alliance MATHplus Protocol ENGLISHDocument3 pagesFLCCC Alliance MATHplus Protocol ENGLISHJhonn BlackNo ratings yet
- Brief Outline Questions To Ask: Acute AsthmaDocument15 pagesBrief Outline Questions To Ask: Acute AsthmaLevina AudreyNo ratings yet
- Obtain 12 Lead ECG and Cardiology ConsultationDocument2 pagesObtain 12 Lead ECG and Cardiology ConsultationPauline ChanNo ratings yet
- FLCCC Alliance MATHplus Protocol ENGLISHDocument3 pagesFLCCC Alliance MATHplus Protocol ENGLISHfernandohNo ratings yet
- Station 3 LeafletDocument5 pagesStation 3 LeafletFelicianna Ashwinie StanleyNo ratings yet
- Pediatric IV Push Quick ED Reference TableDocument4 pagesPediatric IV Push Quick ED Reference TableTayyab RazaNo ratings yet
- Table 17-3 - Common Endotracheal Intubation Medication IndicatDocument1 pageTable 17-3 - Common Endotracheal Intubation Medication IndicatDragutin PetrićNo ratings yet
- 4 Drugs Used in GastrointestinalDocument13 pages4 Drugs Used in Gastrointestinalrajkumar871992No ratings yet
- Pediatric Medication Dosing GuildelinesDocument2 pagesPediatric Medication Dosing GuildelinesMuhammad ZeeshanNo ratings yet
- ICE DrugsDocument2 pagesICE DrugsRichelle FrondaNo ratings yet
- Recommended Doses of Medications To Treat Children With An Acute Asthma ExacerbaDocument3 pagesRecommended Doses of Medications To Treat Children With An Acute Asthma Exacerbaمعاذ الشريفNo ratings yet
- Hospital Treatment Protocol For Covid-19Document4 pagesHospital Treatment Protocol For Covid-19Adrian BoboceaNo ratings yet
- 04 Chapter Respiratory SystemDocument18 pages04 Chapter Respiratory SystemMSKCNo ratings yet
- Tuberculosis: Sudchaya Prasoetpan (R1 Silpakorn University Residency Program)Document56 pagesTuberculosis: Sudchaya Prasoetpan (R1 Silpakorn University Residency Program)moraceaebmNo ratings yet
- Poster On Epilepsy Management in CaninesDocument1 pagePoster On Epilepsy Management in Caninessai hemachandNo ratings yet
- Drug Therapy For PicuDocument32 pagesDrug Therapy For PicuNeethu Mariya MathewNo ratings yet
- QR Klinik Kesihatan Setting, by DR Gerard Loh DMDocument34 pagesQR Klinik Kesihatan Setting, by DR Gerard Loh DMlailatul husnaNo ratings yet
- ANTI-ARRHYTHMIC DRUGS Veterinary PharmacologyDocument5 pagesANTI-ARRHYTHMIC DRUGS Veterinary PharmacologyljramosNo ratings yet
- NICU Drugs GuideDocument49 pagesNICU Drugs GuideArhanNo ratings yet
- PCP Example 2Document15 pagesPCP Example 2Pau Joy EstarezNo ratings yet
- UVA Phenobarb Protocol Sdutta 8-4-21Document3 pagesUVA Phenobarb Protocol Sdutta 8-4-21Shourik DuttaNo ratings yet
- Doses de MedicamentosDocument1 pageDoses de MedicamentosSoraya Bio VetNo ratings yet
- Marik Covid Protocol Summary PDFDocument2 pagesMarik Covid Protocol Summary PDFJody VivasNo ratings yet
- Rsud Kabupaten Bengkayang Bidang Anestesi Anesthesia Medication DosagesDocument5 pagesRsud Kabupaten Bengkayang Bidang Anestesi Anesthesia Medication DosagesBonny ChristianNo ratings yet
- Paramedic Drugs: Drug Class Indications Dosage NameDocument14 pagesParamedic Drugs: Drug Class Indications Dosage NameIbrahem Al100% (7)
- Rsud Sijunjung Obat Dosis Sediaan: KejangDocument2 pagesRsud Sijunjung Obat Dosis Sediaan: KejangAprita SaparNo ratings yet
- Paediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Document14 pagesPaediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Nadia SalwaniNo ratings yet
- 40kg Fent - dex.InitialGoal Directed Comfort Algorithm 1 Page Less Than 40 KG - 01!26!2018Document2 pages40kg Fent - dex.InitialGoal Directed Comfort Algorithm 1 Page Less Than 40 KG - 01!26!2018Georgia DugaciNo ratings yet
- CalciumchannelalgorithmDocument1 pageCalciumchannelalgorithmLind YLNo ratings yet
- Bagan KejangDocument10 pagesBagan KejangNie' MKNo ratings yet
- Dose Modification GuidelinesDocument1 pageDose Modification GuidelinesAhmed Maged FadelNo ratings yet
- 1: Adhd: Scientific Name Dose CommentsDocument4 pages1: Adhd: Scientific Name Dose CommentsSadiq Abdo92No ratings yet
- Dilution Protocol For AdultsDocument23 pagesDilution Protocol For AdultsSharumathi ChandraNo ratings yet
- Dosis Puyer Sudah UrutDocument1 pageDosis Puyer Sudah UrutSvara SenjaNo ratings yet
- FLCCC Alliance MATHplus Protocol ENGLISHDocument3 pagesFLCCC Alliance MATHplus Protocol ENGLISHDavid GrayNo ratings yet
- Notes in Neonates محمد ابراهيم مستشفى قوص قنا.WhiteKnightLoveDocument77 pagesNotes in Neonates محمد ابراهيم مستشفى قوص قنا.WhiteKnightLoveMaRwa IbrahimNo ratings yet
- الأدوية والجرعاتDocument1 pageالأدوية والجرعاتsalehtaha1989No ratings yet
- Missed Doses of Long Acting InjectionsDocument5 pagesMissed Doses of Long Acting InjectionsAbdualaziz AlmalkiNo ratings yet
- Bronchiolitis Pathway InpatientDocument1 pageBronchiolitis Pathway Inpatientd'Agung NugrohoNo ratings yet
- Age 2 Months Age 2monthsDocument1 pageAge 2 Months Age 2monthsd'Agung NugrohoNo ratings yet
- Children's Hospital at Montefiore-IV Access Pathway: Predictor 0 Points 1 Point 2 PointsDocument1 pageChildren's Hospital at Montefiore-IV Access Pathway: Predictor 0 Points 1 Point 2 Pointsd'Agung NugrohoNo ratings yet
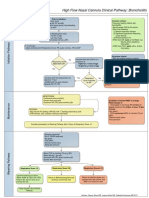
- High Flow Nasal Cannula Clinical Pathway: Bronchiolitis: Prior To Initiation: Inclusion CriteriaDocument1 pageHigh Flow Nasal Cannula Clinical Pathway: Bronchiolitis: Prior To Initiation: Inclusion Criteriad'Agung NugrohoNo ratings yet
- Bonus 2010 FA Step 1 Micro HIVDocument1 pageBonus 2010 FA Step 1 Micro HIVGabriel F. SotoNo ratings yet
- BT PTW GenogramDocument10 pagesBT PTW GenogramShashi YNNo ratings yet
- ArsenicDocument17 pagesArsenicChandrakumar Singh KhumukchambaNo ratings yet
- AMLS Mobile Reference GuideDocument6 pagesAMLS Mobile Reference GuideLim Jun Bin100% (1)
- Significance of Family History in Homoeopathic PrescribingDocument8 pagesSignificance of Family History in Homoeopathic PrescribingHomoeopathic Pulse50% (2)
- SSPL Product Brochure & Co Profile With Clients ListDocument12 pagesSSPL Product Brochure & Co Profile With Clients Listrohitagarwal_hlwNo ratings yet
- Neck DissectionDocument25 pagesNeck DissectionAdi SitaruNo ratings yet
- Standard Treatment Guidelines AND Essential Drugs List: Ministry of Health, Tonga-2007Document391 pagesStandard Treatment Guidelines AND Essential Drugs List: Ministry of Health, Tonga-2007Citra Ayu ApriliaNo ratings yet
- Serum Protein Electrophoresis and Immunofixation - BookFRev2web - PDF Oct 9, 2014Document19 pagesSerum Protein Electrophoresis and Immunofixation - BookFRev2web - PDF Oct 9, 2014mob3No ratings yet
- Askep Dalam Bahasa InggrisDocument6 pagesAskep Dalam Bahasa InggrisDhian Aji CandraNo ratings yet
- Vegetarianism: Sri Swami SivanandaDocument3 pagesVegetarianism: Sri Swami SivanandacusumanofrancNo ratings yet
- Management of Pregnant Patient in DentistryDocument10 pagesManagement of Pregnant Patient in DentistryVíctor Orduña LópezNo ratings yet
- Biotechnology Impact On SocietyDocument4 pagesBiotechnology Impact On SocietyEugeneKimANo ratings yet
- Pathophysiology of AppendicitisDocument2 pagesPathophysiology of AppendicitisDivine Jane Purcia67% (3)
- Schramm A., Gellrich N-C., Schmelzeisen R.-Navigational Surgery of The Facial Skeleton (2007)Document172 pagesSchramm A., Gellrich N-C., Schmelzeisen R.-Navigational Surgery of The Facial Skeleton (2007)Remus ChirciuNo ratings yet
- Product Monograph: (Clindamycin Phosphate Topical Solution USP)Document13 pagesProduct Monograph: (Clindamycin Phosphate Topical Solution USP)igunpharmNo ratings yet
- Thesis Statement About CigarettesDocument5 pagesThesis Statement About Cigarettesfexschhld100% (2)
- Ppz3o - Unit 1Document136 pagesPpz3o - Unit 1api-266151891No ratings yet
- Recurrent Pregnancy LossDocument211 pagesRecurrent Pregnancy LossGopal Kumar Das100% (1)
- Efusi Pleura & EmpyemaDocument47 pagesEfusi Pleura & EmpyemaArumLaksmitaDewiNo ratings yet
- Thyroid SwellingDocument8 pagesThyroid SwellingDn Ezrinah Dn Esham50% (2)
- Campus Map Building List PDFDocument1 pageCampus Map Building List PDFRicky Quizzagan MaguigadNo ratings yet
- NP 5Document28 pagesNP 5Trixia LivinaNo ratings yet
- Linear Quadratic (LQ) Model & Biological Based Treatment Planning - Dr. Manoj GuptaDocument60 pagesLinear Quadratic (LQ) Model & Biological Based Treatment Planning - Dr. Manoj GuptaSudhan Rajan100% (3)
- Maxillofacial Privileges QGHDocument4 pagesMaxillofacial Privileges QGHSanam FaheemNo ratings yet
- L 5 - Lungs PathologyDocument128 pagesL 5 - Lungs PathologyDiana Popovici100% (1)