Professional Documents
Culture Documents
Review: Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Review: Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Uploaded by
ellya theresiaCopyright:
Available Formats
You might also like
- KeNotes 2017 PDFDocument106 pagesKeNotes 2017 PDFDENTAL REVIEWER ONLY100% (3)
- Wilm's Tumor Pa Tho PhysiologyDocument1 pageWilm's Tumor Pa Tho Physiologya_yeLNo ratings yet
- Aaaq2 2015 Ir PresentationDocument45 pagesAaaq2 2015 Ir PresentationguerrezNo ratings yet
- The Duke Heart Failure ProgramDocument10 pagesThe Duke Heart Failure ProgramAnonymous PbAQxgw0No ratings yet
- 2012 Illinois Rules of The Road Review Course WorkbookDocument36 pages2012 Illinois Rules of The Road Review Course WorkbookmudkipzzzNo ratings yet
- OnQ Broadcast Intercom System ManualDocument2 pagesOnQ Broadcast Intercom System ManualJohn PallissardNo ratings yet
- Diabetes Conversation Maps: Journey To Better Diabetes EducationDocument1 pageDiabetes Conversation Maps: Journey To Better Diabetes EducationCenter for Managing Chronic DiseaseNo ratings yet
- IV Drug CompDocument5 pagesIV Drug CompWil Lester100% (1)
- Supportive & Preventive Medicine PDFDocument29 pagesSupportive & Preventive Medicine PDFhuong L100% (1)
- Daftar Nutrisi PERKECILDocument6 pagesDaftar Nutrisi PERKECILellya theresiaNo ratings yet
- 1117 FullDocument29 pages1117 FullElizabeth IB100% (1)
- Cardiovascular Outcomes Trials in Type 2 DiabetesDocument51 pagesCardiovascular Outcomes Trials in Type 2 Diabetes와라송이100% (1)
- Kathrine O Neal PP PDFDocument92 pagesKathrine O Neal PP PDFrezqNo ratings yet
- 1183 - The Global Burden of Heart Failure. - Martin COWIE (London, United Kingdom)Document21 pages1183 - The Global Burden of Heart Failure. - Martin COWIE (London, United Kingdom)Mulyani EdwarNo ratings yet
- A Randomized, Double-Blind, Controlled Trial Comparing Rifaximin Plus Lactulose With Lactulose Alone in Treatment of Overt Hepatic EncephalopathyDocument3 pagesA Randomized, Double-Blind, Controlled Trial Comparing Rifaximin Plus Lactulose With Lactulose Alone in Treatment of Overt Hepatic EncephalopathyYunita DNo ratings yet
- Dapa Brief Data (14271)Document24 pagesDapa Brief Data (14271)Adel SALLAM100% (1)
- 2002 GAO PDMP StudyDocument27 pages2002 GAO PDMP StudyKOMU NewsNo ratings yet
- Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy CREDENCE TrialDocument29 pagesCanagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy CREDENCE Trialgokulam0075028No ratings yet
- THURSDAY Salisbury AfsharDocument39 pagesTHURSDAY Salisbury AfsharNational Press Foundation100% (1)
- AIIMS June 2020 DR Siraj Ahmad PDFDocument4 pagesAIIMS June 2020 DR Siraj Ahmad PDFadiNo ratings yet
- SGLT 2 Inhibitors: Newer Paradigms in The Treatment of Heart Failure With Reduced Ejection FractionDocument4 pagesSGLT 2 Inhibitors: Newer Paradigms in The Treatment of Heart Failure With Reduced Ejection FractionIJAR JOURNALNo ratings yet
- Pharmacy PresentationDocument93 pagesPharmacy PresentationAira Abella100% (1)
- World Preview 2016 Outlook To 2022Document49 pagesWorld Preview 2016 Outlook To 2022Willy Pérez-Barreto MaturanaNo ratings yet
- Beyond Use DateDocument56 pagesBeyond Use DateDa Chan100% (1)
- ACC Handbook Ascvd Type 2 Diabetes: On andDocument10 pagesACC Handbook Ascvd Type 2 Diabetes: On andZH. omg sarNo ratings yet
- Pratley New Treatments For Type 2 DiabetesDocument85 pagesPratley New Treatments For Type 2 DiabetesMia DangaNo ratings yet
- Vanco & Ag PK 2018Document35 pagesVanco & Ag PK 2018Nguyen GeenNo ratings yet
- Aon Profile 2020Document16 pagesAon Profile 2020phanapa100% (1)
- SGLT 2 InhibitorDocument5 pagesSGLT 2 InhibitorAlimWijayaNo ratings yet
- PA 644 - M2 LecturesDocument735 pagesPA 644 - M2 LectureskatNo ratings yet
- The Filter, The Pump and The FilterDocument35 pagesThe Filter, The Pump and The FilterRenal Association MauritiusNo ratings yet
- AsdfgjkDocument14 pagesAsdfgjkMaria Frances Antoniette PerezNo ratings yet
- Slides Outcomes of Sglt2i in Diabetic Kidney Disease Is It All DiabetesDocument29 pagesSlides Outcomes of Sglt2i in Diabetic Kidney Disease Is It All DiabetesVaibhav DafaleNo ratings yet
- A Speech On PunctualityDocument2 pagesA Speech On PunctualityRrhayshelle Ahnne0% (1)
- HF2019Document24 pagesHF2019Sima Noviantika100% (2)
- New Pathways in Heart Failure TreatmentDocument34 pagesNew Pathways in Heart Failure TreatmentSwapnaNo ratings yet
- Journal Reading EMPEROR-ReducedDocument21 pagesJournal Reading EMPEROR-ReducedLolii Con Harhazyuku100% (1)
- Controlled Substances LawsDocument8 pagesControlled Substances LawsJames Lindon100% (1)
- Ultimate Reference DocumentDocument29 pagesUltimate Reference DocumentShellyza Moledina SajwaniNo ratings yet
- Illinois Pilot Program Act RoadmapDocument19 pagesIllinois Pilot Program Act RoadmapMPPNo ratings yet
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- SC PH 00389 - TRAJENTA Module 2020 1QDocument107 pagesSC PH 00389 - TRAJENTA Module 2020 1QJenny Calapati TorrijosNo ratings yet
- Introduction, Medicines Classification and Standard Operating ProceduresDocument14 pagesIntroduction, Medicines Classification and Standard Operating ProceduresAnkur SinghNo ratings yet
- AstraZeneca AR 2018 PDFDocument248 pagesAstraZeneca AR 2018 PDFChristian nelNo ratings yet
- Empagliflozin in Heart Failure With A Preserved Ejection FractionDocument11 pagesEmpagliflozin in Heart Failure With A Preserved Ejection Fractionsri wahyuniNo ratings yet
- Matching ActivityDocument26 pagesMatching Activityapi-661456802No ratings yet
- 02-05 2022 Pharm Pharmacokinetics 2022 R3Document38 pages02-05 2022 Pharm Pharmacokinetics 2022 R3Amira HelayelNo ratings yet
- Allaergic Conjunctivitis PathophysiologyDocument25 pagesAllaergic Conjunctivitis PathophysiologyRabiu Hassan MusaNo ratings yet
- Sharkbite® Metal Push-Fit Plumbing Solution: Technical InformationDocument36 pagesSharkbite® Metal Push-Fit Plumbing Solution: Technical InformationPubcrawlNo ratings yet
- CV 2021Document5 pagesCV 2021api-611973258No ratings yet
- Pharmacotherapy of DMDocument23 pagesPharmacotherapy of DMsalinaNo ratings yet
- Pearsonvue Exam of Pharmacy: - CasesDocument114 pagesPearsonvue Exam of Pharmacy: - Caseslina magdiNo ratings yet
- p2019b1 Sample PDFDocument22 pagesp2019b1 Sample PDFMaria PerezNo ratings yet
- All Types of InsulinDocument18 pagesAll Types of Insulinali mohammedNo ratings yet
- Peptic Ulcer DiseaseDocument41 pagesPeptic Ulcer DiseaseNneka Uchenna UkweNo ratings yet
- PharDose Chapter 1Document4 pagesPharDose Chapter 1Angelyka CabaloNo ratings yet
- Fellowship in DiabetesDocument2 pagesFellowship in DiabetesBenjamin NelsonNo ratings yet
- SPIRIVA HandiHaler InstructionsDocument9 pagesSPIRIVA HandiHaler InstructionssamyvnNo ratings yet
- CA Sitagliptin Vs Glipizide 1.1Document29 pagesCA Sitagliptin Vs Glipizide 1.1lordizzatNo ratings yet
- 8-22-16-Lecture Grand Rounds Drug Drug Interactions PDFDocument44 pages8-22-16-Lecture Grand Rounds Drug Drug Interactions PDFCastov Liubița100% (1)
- 3 Calculations PDFDocument31 pages3 Calculations PDFMisha Ptpm100% (1)
- A Narrative Review of New Treatment Options For Chronic Kidney Disease in Type 2 DiabetesDocument7 pagesA Narrative Review of New Treatment Options For Chronic Kidney Disease in Type 2 Diabetesjhoanna andrea portillaNo ratings yet
- Temporal Improvement of A COVID 19 Positive.31Document1 pageTemporal Improvement of A COVID 19 Positive.31ellya theresiaNo ratings yet
- 4 Prof. EAD Microbiome MAACI 2 19 JuniDocument25 pages4 Prof. EAD Microbiome MAACI 2 19 Juniellya theresiaNo ratings yet
- Jejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of LiteratureDocument6 pagesJejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of Literatureellya theresiaNo ratings yet
- Gastrointestinal Bleeding in Patients With Severe Sars-Cov-2Document3 pagesGastrointestinal Bleeding in Patients With Severe Sars-Cov-2ellya theresiaNo ratings yet
- Emerging Treatments For Crohn's Disease: Cells, Surgery, and Novel TherapeuticsDocument10 pagesEmerging Treatments For Crohn's Disease: Cells, Surgery, and Novel Therapeuticsellya theresiaNo ratings yet
- Peritoneal DialysisDocument17 pagesPeritoneal Dialysisellya theresiaNo ratings yet
- MR c1 Gastropati DMDocument27 pagesMR c1 Gastropati DMellya theresiaNo ratings yet
- Development of Treatment: How Do We Manage Antimicrobial Resistance?Document22 pagesDevelopment of Treatment: How Do We Manage Antimicrobial Resistance?ellya theresiaNo ratings yet
- Aki Rifle - Google SearchDocument1 pageAki Rifle - Google Searchellya theresiaNo ratings yet
- 6 PDFDocument2 pages6 PDFellya theresiaNo ratings yet
- WJG 25 5097Document9 pagesWJG 25 5097ellya theresiaNo ratings yet
- 01 Renal ModuleDocument71 pages01 Renal ModuleFatima AbduljalilNo ratings yet
- Newborn Physiology PathologyDocument99 pagesNewborn Physiology Pathologythev0206100% (1)
- PhysioEx Ex. 9 Act. 3Document4 pagesPhysioEx Ex. 9 Act. 3Juvy Anne LozanoNo ratings yet
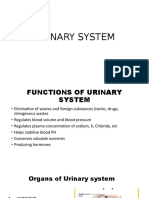
- Chapter 26 Urinary SystemDocument17 pagesChapter 26 Urinary SystemAmy Lalringhluani100% (1)
- System UriDocument48 pagesSystem UriStef FieNo ratings yet
- Urinary System PDFDocument27 pagesUrinary System PDFfiona100% (3)
- General Biology G11 WK13-16 A. TobiasDocument31 pagesGeneral Biology G11 WK13-16 A. TobiasKristine SantosNo ratings yet
- 13.3 Excretion in Humans IGCSE CIE Biology Ext Theory MS - LDocument7 pages13.3 Excretion in Humans IGCSE CIE Biology Ext Theory MS - LTaelo MasuNo ratings yet
- Excretion by Rakshita SinghDocument37 pagesExcretion by Rakshita SinghPurplet 7No ratings yet
- COMPLETE CS - Acute PyelonephritisDocument53 pagesCOMPLETE CS - Acute Pyelonephritisyasira100% (1)
- Excretory SystemDocument15 pagesExcretory Systemlaptop lenovoNo ratings yet
- Urinary SystemDocument28 pagesUrinary Systemgabanule brandonNo ratings yet
- Body Fluids & ElectrolytesDocument26 pagesBody Fluids & ElectrolytesMohamad Zekry Zuhairy100% (1)
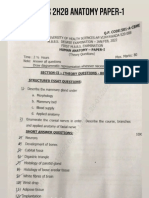
- NTRUHS 2k20 Batch Final PapersDocument24 pagesNTRUHS 2k20 Batch Final PapersLakshmidevi GaletiNo ratings yet
- PathoPhysiology of Renal Failure OverviewDocument7 pagesPathoPhysiology of Renal Failure Overviewnursing concept maps100% (1)
- RFT - Organ Function TestDocument28 pagesRFT - Organ Function TestRishita ChoubeyNo ratings yet
- Bolesti BubregaDocument6 pagesBolesti Bubregamedicinar85No ratings yet
- Histo NotesDocument19 pagesHisto Notesanas ishaqNo ratings yet
- Chapter 6 CMDocument14 pagesChapter 6 CMLeilani SablanNo ratings yet
- Csec HSB January 2011 p2Document19 pagesCsec HSB January 2011 p2Sachin Bahadoorsingh100% (1)
- Clinical Pharmacology and Forensic ToxicologyDocument107 pagesClinical Pharmacology and Forensic ToxicologySunilNo ratings yet
- Anatomi Fisiologi Sistem PerkemihanDocument65 pagesAnatomi Fisiologi Sistem PerkemihanMakkatul HikmahNo ratings yet
- Chapter 6 - Body Fluids, Water-Salt Balance RP1 PDFDocument77 pagesChapter 6 - Body Fluids, Water-Salt Balance RP1 PDFpizzaNo ratings yet
- A Level Biology NotesDocument6 pagesA Level Biology NotesMira AluedeNo ratings yet
- Acid-Base Disorders Fluid and ElectrolytesDocument13 pagesAcid-Base Disorders Fluid and ElectrolytesNicole BiduaNo ratings yet
- Pex 09 04Document4 pagesPex 09 04chaira nisaaNo ratings yet
- Artículo 2 - Fisiopatología de La PielonefritisDocument17 pagesArtículo 2 - Fisiopatología de La PielonefritisCAROLINA CHUMACERO BERMEONo ratings yet
- كتاب اسئلة جميلDocument401 pagesكتاب اسئلة جميلMohammadSAL-Rawashdeh100% (1)
Review: Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Review: Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Uploaded by
ellya theresiaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Review: Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Review: Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Uploaded by
ellya theresiaCopyright:
Available Formats
Review
New pharmacological strategies for protecting kidney
function in type 2 diabetes
Marcel H A Muskiet, David C Wheeler, Hiddo J L Heerspink
Type 2 diabetes is the leading cause of impaired kidney function, albuminuria, and renal replacement therapy globally, Lancet Diabetes Endocrinol 2018
thus placing a large burden on health-care systems. Current treatment strategies rely on intensive glucose lowering, Published Online
and strict blood pressure control targeting blockade of the renin–angiotensin–aldosterone system. Such approaches December 19, 2018
http://dx.doi.org/10.1016/
might slow decline in kidney function, but many patients progress to end-stage kidney failure despite optimal therapy.
S2213-8587(18)30263-8
In recent clinical trials, new-generation glucose-lowering drug classes, the sodium-glucose co-transporter-2 inhibitors
Diabetes Centre, Department
and agents that target the incretin pathway, have been shown to improve kidney outcomes in patients with type 2 of Internal Medicine, VU
diabetes. Other new approaches, which have been developed on the basis of an improved understanding of the University Medical Centre,
mechanisms that contribute to kidney damage in the context of diabetes, include use of drugs that block endothelin Amsterdam, Netherlands
(M H A Muskiet MD); Centre for
receptors (eg, atrasentan) and non-steroidal mineralocorticoid receptors (eg, finerenone). In this Review, we provide
Nephrology, University College
an overview of recent clinical data relevant to these new therapeutic approaches for management of kidney disease in London, London, UK
the context of type 2 diabetes. (Prof D C Wheeler MD); and
Department of Clinical
Introduction effective renoprotective strategy in patients with type 2 Pharmacy and Pharmacology,
University of Groningen,
Patients with type 2 diabetes who develop a reduction in diabetes in the early 2000s was a major step forward, but University Medical Centre
estimated glomerular filtration rate (eGFR) to less than was followed by several years without much progress.3 Groningen, Groningen,
60 mL/min per 1∙73 m², albuminuria (eg, urinary However, emerging data from clinical outcome trials Netherlands
(Prof H J L Heerspink PhD)
albumin-to-creatinine ratio [UACR] >3 mmol/mol), or suggest that new-generation glucose-lowering drug
Correspondence to:
both, sustained over at least 3 months, are considered to classes (sodium-glucose co-transporter-2 [SGLT2] inhibi
have chronic kidney disease according to current inter tors and certain incretin-based therapies) might protect Prof David C Wheeler, Centre for
Nephrology, University College
national guidelines.1 Chronic kidney disease identified the kidney through mechanisms not directly related to London, London NW3 2PF, UK
in the context of type 2 diabetes is usually referred to as glucose lowering.4,5 Furthermore, there are several novel d.wheeler@ucl.ac.uk
diabetic nephropathy or diabetic kidney disease, even pharmacological agents under development that target
when kidney histology has not been formally assessed newly identified mechanistic pathways underlying dia
by biopsy. The clinical assumption that kidney betic kidney disease (figure 1). In this Review, we
dysfunction is a consequence of diabetes might be re summarise current knowledge of the clinical benefits of
inforced by the presence of other diabetes complications new strategies that are either approved for clinical use or
(such as retinopathy) and by blood tests excluding other have shown promising efficacy and safety in advanced
causes of chronic kidney disease, such as systemic development programmes.
vasculitis or myeloma. A diagnosis of chronic kidney
disease in a person with type 2 diabetes has important Current treatment strategies in diabetic kidney
implications in terms of prognosis. Not only is the risk disease
of developing end-stage kidney disease increased, Recommended treatment strategies for patients with
potentially requiring renal replacement therapy (such as type 2 diabetes and chronic kidney disease are to initiate
dialysis or kidney transplantation), but patients with appropriate lifestyle changes (eg, weight management,
diabetes and chronic kidney disease are also at physical activity, dietary recommendations, and smoking
substantially increased risk of mortality and non-fatal cessation) and to target high blood pressure and poor
cardiovascular events compared with people with glycaemic control.
diabetes but without chronic kidney disease.2 The risk of
these adverse outcomes is further increased at lower Glycaemic control
levels of eGFR and higher levels of albuminuria.1 As the Optimisation of glycaemic control reduces the risk of
prevalence has increased, type 2 diabetes has emerged microvascular complications in diabetes, including the
as the leading cause of chronic kidney damage. onset and progression of albuminuria and, in post-hoc
Monitoring for the development and progression of follow-up analysis of the ADVANCE trial, the risk of end-
chronic kidney disease can be achieved through regular stage kidney disease.5,6 Yet reaching and maintaining
blood testing to allow estimation of glomerular filtration HbA1c targets can be more challenging in patients with
rate (GFR) and analysis of urine samples (preferably diabetic kidney disease because an eGFR lower than
early morning) for UACR. 60 mL/min per 1∙73 m² restricts the use, or dose, of
The aims of medical management in diabetic kidney several oral and injectable glucose-lowering drugs.7 For
disease are to reduce the level of albuminuria and prevent example, most guidelines recommend discontinuation
a progressive decline in eGFR. Identification of renin– of metformin when eGFR falls below 30 mL/min
angiotensin–aldosterone system (RAAS) inhibition as an per 1∙73 m² to reduce the risk of lactic acidosis, a rare but
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 1
Review
Classic renal risk factors
Obesity
SGLT2 inhibitors
and Hyperglycaemia
incretin-based therapies
Hypertension Endothelin ET-1 receptor antagonists
RAAS inhibitors
SGLT2 inhibitors Glomerular hyperfiltration RAAS
MRAs
Incretin-based therapies Dyslipidaemia
Metabolic and haemodynamic pathways
AGEs Reactive oxygen species
Kinase cascades, transcription factors
Chemokines Pro-inflammatory cytokines
Adhesion molecules Growth factors
Macrophage infiltration Extracellular matrix accumulation Podocyte injury
Inflammation
Tubulointerstitial damage Glomerulosclerosis and proteinuria
End-stage kidney disease
Figure 1: Pathophysiology of diabetic kidney disease and targets of promising renoprotective drugs in type 2 diabetes based on clinical trial data
SGLT2=sodium-glucose co-transporter-2. RAAS=renin–angiotensin–aldosterone system. ET-1=endothelin-1. MRAs=mineralocorticoid receptor antagonists.
AGEs=advanced glycation end products.
serious adverse effect.8 Accumulation of sulfonylureas albuminuria develops. Although most classes of anti
and their active metabolites because of reduced renal hypertensive medication can be used to control hyper
excretion increases the likelihood of hypoglycaemia, and tension in patients with type 2 diabetes and chronic
necessitates the avoidance of first-generation agents kidney disease, guide lines generally recommend in
(eg, tolbutamide) and dose restriction of some second- clusion of angiotensin recep tor blockers (ARBs) or
generation agents (eg, glimepiride) in patients with angiotensin-converting enzyme (ACE) inhibitors in the
chronic kidney disease.9 Largely because of these antihypertensive regimen, on the basis of evidence from
risks, arguments have been made for less stringent randomised controlled trials done almost two decades
HbA1c targets for patients with type 2 diabetes and low ago.5 These RAAS blockers reduce albuminuria, probably
eGFR levels by some experts.10 by reducing intraglomerular pressure, and might also
prevent renal inflammation and fibrosis. Although
Blood pressure control renoprotective in the longer term, their use might be
The best method to assess blood pressure in patients limited by acute reductions in eGFR or the development
with type 2 diabetes (eg, whether to use resting of hyperkalaemia. There are few studies directly com
office readings or 24 h assessment) is not universally paring ACE inhibitors with ARBs in diabetic kidney
agreed and guidelines differ in recommending target disease, but the available data suggest that the two classes
systolic and diastolic pressures.5,11 Lower targets (eg, have similar beneficial effects on kidney outcomes.12
<130/80 mm Hg) are generally considered appropriate to Declining kidney function is often associated with fluid
reduce cardiovascular risk and slow eGFR decline once retention, which exacerbates hypertension, resulting in
2 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
peripheral and pulmonary oedema. Loop diuretics are (DPP-4) inhibitors, and glucagon-like peptide-1 (GLP-1)
often used to offset volume expansion and treat associated receptor antagonists. Other new therapeutic approaches
symptoms but might have a detrimental effect on eGFR include mineralocorticoid receptor antagonists (MRAs;
as a result of intravascular volume depletion. figure 1).
Evidence-based renoprotective strategies SGLT2 inhibitors
The notion of specifically protecting the kidney in The kidneys have an important role in normal glucose
patients with type 2 diabetes arose largely from studies of homoeostasis through gluconeogenesis, use of glucose as
ARBs done in the late 1990s. In two clinical outcome a metabolic fuel, and re-absorption of most filtered glucose
trials reported in 2001, IDNT and RENAAL, the use of by the sodium-glucose co-transporters (SGLT1 and SGLT2)
irbesartan and losartan, respectively, reduced the likeli located in the luminal membrane of the proximal tubule.23
hood of adverse kidney outcomes by about 20% compared The majority (80–90%) of filtered glucose is reabsorbed
with conventional therapies.13,14 Data from previous by the high-capacity, low-affinity SGLT2 in the early
animal studies suggested that such renoprotective effects S1 segment of the proximal convoluted tubule, whereas
were due to reductions in intra glomerular pressure, the remaining 10–20% is reabsorbed by the low-capacity,
believed to result from the ability of these drugs high-affinity SGLT1 in the more distal S2/S3 segment.23,24
to selectively vasodilate the efferent arteriole of the In patients with poorly controlled diabetes, the maximum
glomerulus.15,16 This mechanism of action was thought to renal glucose reabsorptive capacity is increased compared
explain the acute reductions in eGFR observed in many with normal glucose-tolerant individuals, probably because
patients on initiation of these drugs, which need to be of upregulation of SGLT2.25,26 As such, inhibition of
considered in the context of their longer-term benefit on SGLT2 was identified as an attractive therapeutic target.
kidney function. Post-hoc analyses of these trials have Four SGLT2 inhibitors (canagliflozin, dapagliflozin,
lent support to the hypothesis that renoprotection was empagliflozin, and ertugliflozin) have been approved by
conferred as a result of RAAS blockade, rather than via the US Food and Drug Administration and the European
the effects on systemic blood pressure.17 Medicines Agency for use as glucose-lowering drugs in
patients with type 2 diabetes.23,27
The search for new therapies SGLT2 inhibitors dose-dependently increase urinary
Despite widespread use of RAAS inhibitors as part of the glucose excretion by about 70–80 g per day in healthy
antihypertensive regimen in clinical practice, there individuals without diabetes,27 and decrease HbA1c by
remains a high residual risk of progressive kidney dis 0∙5–0∙8% in patients with type 2 diabetes, depending on
ease, emphasising the need for new therapies.3,5 Follow baseline HbA1c and kidney function.28 SGLT2 inhibitors
ing RENAAL and IDNT, investigators tried to show that can be used in combination with other anti-hyper
maximising RAAS blockade by combination of an ARB glycaemic drugs and their glucose-lowering efficacy
with either an ACE inhibitor (VA NEPHRON-D)18 or the is not reduced when used as an adjunct to metformin,
direct renin inhibitor aliskiren (ALTITUDE)19 would have sulfonylureas, DDP-4 inhibitors, GLP-1 receptor agonists,
an additional benefit on kidney outcomes. Although or basal insulin.29 Glucose-lowering efficacy seems to
combination therapy led to greater reductions in albu be enhanced in patients with poor glycaemic con trol
minuria and blood pressure, these trials were stopped (HbA1c >8∙0%).28 Beyond glycaemic control, SGLT2
prematurely for safety and futility reasons, respectively. inhibitors have been shown to decrease bodyweight by
Alternative therapeutic approaches that have been tried 2–3 kg,5,23 partly as a direct consequence of a negative
unsuccessfully include administration of the glycos caloric balance due to increased urinary glucose excretion
aminoglycan sulodexide (Sun-MACRO),20 target ing of (1 g of glucose equates to 4 kcal). However, despite
the endothelin receptor with the antagonist avosentan ongoing glycosuria, weight loss does not usually continue
(ASCEND; see Endothelin receptor antagonists),21 and after 6 months, probably because of compensatory
activation of the nuclear factor erythroid 2-related factor 2 changes in metabolism and increased appetite and food
with bardoxolone methyl (BEACON).22 Despite such intake.30,31
setbacks, the growing prevalence of type 2 diabetes and As the reabsorption of glucose and sodium are coupled,
the increasing cost of managing the associated SGLT2 inhibition leads to a dose-dependent natriuresis.32
complications have driven the search for new therapies. Although the natriuretic effect of these drugs dissipates
Large-scale clinical trials have been required to prove after 2–3 days and sodium and fluid balance re-
cardiovascular safety (in addition to HbA1c lowering) of equilibrate, a reduction in plasma volume of about 7%,
new glucose-lowering drugs by regulatory agencies. along with an increase in haematocrit and reduction in
These cardiovascular outcome trials have not only systolic blood pressure of about 2–4 mm Hg, have been
indicated generally favourable adverse effect profiles of reported.28 The antihypertensive effects of SGLT2
newer drug classes, but have also identified potential inhibitors seem to be independent of concomitant
drug-specific renoprotective benefits associated with the antihypertensive medications (including diuretics and
use of some SGLT2 inhibit ors, dipeptidyl peptidase-4 RAAS inhibitors).33,34
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 3
Review
* Inhibition
SGLT2 inhibitors Stimulation
Insulin↑
ET-1 receptor antagonist
GLP-1 receptor agonists
Nitric oxide
ET-1↑ GLP-1 receptor agonists
Diabetes-related
Afferent arteriole Vasodilation glomerular Vasoconstriction Efferent arteriole
hyperfiltration
Ang-II↑
TGF↑
GLP-1 receptor agonists Ang-I↑
Proximal sodium reabsorption↑
Renin
SGLT1/2↑ NHE3↑ Glucagon↑ Amino acids↑
SGLT2 inhibitors GLP-1 receptor agonists Tubule SGLT2 inhibitors Angiotensinogen
Figure 2: Putative effects and mechanisms of novel drugs on renal haemodynamics in diabetes-related glomerular hyperfiltration
SGLT=sodium-glucose co-transporter. GLP-1=glucagon-like peptide-1. ET-1=endothelin-1. TGF=tubuloglomerular feedback. NHE3=sodium–hydrogen exchanger 3.
TGF= tubuloglomerular feedback. Ang-I=angiotensin-I. Ang-II=angiotensin-II. *SGLT2 inhibitors do not directly inhibit insulin action, but lead to a reduction in
concentration.
The beneficial effects of SGLT2 inhibitors on cardio an RAAS inhibitor.36–41 Despite these results, it is
renal outcomes have been established in three landmark important to realise that EMPA-REG OUTCOME,
placebo-controlled cardiovascular outcome trials, EMPA- CANVAS, and DECLARE were not designed to assess the
REG OUTCOME (empagliflozin),35 the CANVAS renoprotective effects of SGLT2 inhibitors.42 Dedicated
Program (canagliflozin), and the DECLARE-TIMI 58 kidney outcome trials (currently in progress) are required
trial.36–38 In EMPA-REG OUTCOME, which included before recommendations on the use of SGLT2 inhibitors
7020 patients with type 2 diabetes with established as a renoprotective drug can be included in updated
cardiovascular disease, empagliflozin reduced the risks clinical practice guidelines.4
of the composite primary outcome (major adverse The renoprotective benefits of SGLT2 inhibitors are
cardiovascular events [MACE]) by 14% (95% CI 1–26%; likely to be explained by several mechanisms. Like ACE
p=0∙04) relative to placebo after a median follow-up of inhibitors and ARBs, these drugs are believed to have
3∙1 years.35 Similarly, in the CANVAS Program, which favourable effects on renal haemodynamics (figure 2).
included 1042 patients with type 2 diabetes and high Their proximal natriuretic effect, possibly enhanced
cardiovascular risk, canagliflozin reduced the risk of the by functional blockade of the sodium–hydrogen
primary MACE outcome by 14% (95% CI 3–25%; p=0∙02) exchanger 3 (NHE3),43 increases sodium delivery to the
relative to placebo after a mean of 118∙2 weeks.36 In downstream juxtaglomerular apparatus.44 In turn, tubulo
DECLARE-TIMI 58, among 17 160 patients with type 2 glomerular feedback signalling is activated, resulting in
diabetes, including 10 186 without prior cardiovascular afferent arteriolar vasoconstriction and decreased renal
disease, dapagliflozin reduced the risk of cardiovascular blood flow, attenuating glomerular hyperfiltration, which
death or hospitalisation for heart failure by 17% but did is a characteristic of diabetic kidney disease.16 In long-
not result in a lower rate of MACE overall in this term trials, SGLT2 inhibitors consistently reduce eGFR
population. Importantly, all three SGLT2 inhibitors after treatment initiation over a wide range of baseline
slowed the progression of eGFR decline and reduced the values, with the reduction reversed after washout of the
risk of a composite renal outcome by approximately 40%. study drugs, collectively suggesting renal haemodynamic
These effects were achieved in all three studies, which actions.45 Such early reductions in eGFR predict a slower
enrolled patients with baseline eGFR greater than subsequent decline in kidney function on long-term
30 mL/min per 1.73 m² (creatinine clearance greater than treatment.16,23,46 SGLT2 inhibitors might also reduce renal
60 mL/min in DECLARE) who were already well hypoxia, which is typically observed in the kidneys of
managed, with about 80% of all participants prescribed people with diabetes.47 By reducing sodium and glucose
4 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
transport activity in the proximal tubule, energy and partly responsible for the roughly 70% amplification of
oxygen demands decrease, resulting in preservation of insulin secretion in the context of nutrient (particularly
tubular cell structural integrity and possibly function.47 glucose) ingestion—the so-called incretin effect.63 This
SGLT2 inhibitors are not currently licensed for use in finding was rapidly followed by the demonstration that
patients with diabetic kidney disease and an eGFR below the glucoregulatory actions of GLP-1 also include sup
45 mL/min per 1∙73 m² in most countries (table 1), since pression of glucagon secretion, inhibition of gastric
their efficacy in terms of glucose lowering is attenuated emptying rate and small bowel motility, and reduction in
in stages 3b–5 chronic kidney disease.51–53 However, the appetite and food intake, transduced by a single GLP-1
effects of the drugs in reducing bodyweight, blood receptor (GLP-1R) located in many organs including the
pressure, and albuminuria persist in these populations.54,55 kidney.59
Additionally, findings from subgroup analyses of EMPA- The incretin effect is severely reduced or absent in
REG OUTCOME and the CANVAS Program suggest patients with type 2 diabetes,63 which is regarded as a key
that the efficacy of SGLT2 inhibitors to reduce the risks of pathophysiological defect that contributes to glucose
cardiovascular and renal outcomes does not depend on intolerance.64 The insulinotropic and glucose-lowering
eGFR.36,56 In recognition of these findings, Health Canada response to exogenous GLP-1 is preserved in human type 2 For the Health Canada guidance
allows physicians to consider the use of SGLT2 inhibitors diabetes,65 suggesting that pharmacological efforts aimed see http://guidelines.diabetes.ca/
cpg/chapter13
when indicated for cardiovascular and renal protection at therapeutic amplification of GLP-1-induced glucose-
down to an eGFR of 30 mL/min per 1∙73 m². lowering in this population are worthwhile. However, the
The effects of SGLT2 inhibitors in slowing progressive GLP-1 peptide is unstable in vivo and continuous infusion
kidney function loss seem to be independent of glycaemic would be required to overcome this problem, limiting
control. In a secondary analysis of CANTATA-SU, clinical application. Circulating GLP-1 is rapidly inactivated
a 2-year, phase 3 registration trial comparing canagliflozin (<2 min), primarily by DPP-4, to a metabolite that
with the sulfonylurea glimepiride, the rate of kidney stimulates insulin secretion.48 These findings prompted
function decline was significantly lower in the two strategies to extend and maintain incretin activity in
canagliflozin group, whereas the glycaemic control was type 2 diabetes: first, the use of injectable GLP-1 receptor
similar between the two classes.57 Also, data from post- agonists that are resistant to DPP-4 cleavage and provide
hoc analyses of EMPA-REG OUTCOME and earlier supraphysiological concentrations of ligands to the GLP-1
phase 3 studies suggested that UACR lowering was receptor; and second, the use of oral DPP-4 inhibitors,
statistically independent of concomitant changes in which prevent de gradation of endogenously secreted
HbA1c.4,40 Collectively, these data suggest that reno GLP-1 and glucose-dependent insulinotropic polypeptide
protective effects are unlikely to be mediated by (also known as gastric inhibitory polypeptide, GIP),
improvements in glycaemic control, but rather by the another incretin hormone.48
other mechanisms outlined earlier. Renal outcome trials Several incretin-based drugs with different structures,
of SGLT2 inhibitors in patients with diabetic kidney modes of administration, and pharmacokinetic prop
disease are ongoing. One of these, CREDENCE erties (separating the GLP-1 receptor agonist class into
(canagliflozin; NCT02065791),58 was stopped early at short-acting [prandial] and long-acting compounds) have
the recommendation of the data safety monitoring been introduced as treatments for type 2 diabetes.59,63
committee, on the basis of achievement of prespecified GLP-1 receptor agonists reduce fasting glucose and
kidney efficacy criteria. Finally, since glomerular HbA1c levels by 0∙5–1∙3%, the reductions achieved
hyperfiltration is involved in the pathophysiology of depending on choice of agent, dose, baseline HbA1c, and
various kidney diseases beyond diabetic kidney disease, background therapy.48 Although less effective when
there is a rationale to extend the use of SGLT2 inhibitors compared with GLP-1 receptor agonists, DPP-4 inhibitors
in non-diabetic kidney disease such as chronic kidney promote reductions in HbA1c of 0∙6–0∙9%.48 Given their
disease induced by obesity, secondary focal segmental glucose-dependent mode of action, incretin-based drugs
glomerulosclerosis, or hypertensive nephrosclerosis.59 As are associated with low risk of hypoglycaemia, and they
such, a dedicated renal outcome trial of dapagliflozin are generally well tolerated.61,62,48
(DAPA-CKD; NCT03036150) is recruiting patients with As pharmacokinetic data and clinical experience with
chronic kidney disease with or without type 2 diabetes, GLP-1 receptor agonists in patients with type 2 diabetes
with an announcement for plans for a similar study and chronic kidney disease are scarce, caution or
assessing empagliflozin (EMPA-KIDNEY trial60). discontinuation is advised when kidney function is
severely impaired (table 1). DPP-4 inhibitors are well
Incretin-based therapies tolerated in stages 3b–5 chronic kidney disease,48
Glucagon-like peptide-1 (GLP-1) is secreted from gut although most manu facturers recom mend dose re
enteroendocrine L-cells at low tonic rates in the fasting ductions, with the exception of linagliptin, which is
and interprandial state. Circulating levels of this gut mainly eliminated through biliary excretion.65
hormone rise briskly within minutes of food intake.61,62 As with SGLT2 inhibitors, off-target effects of
Initial studies focused on its role as an incretin hormone, incretin-based drug classes might favourably modify the
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 5
Review
Brand name Approval Dosing Plasma Elimination route Use in patients with renal insufficiency
(agency half-life (h)
[year] or
year)
Mild Moderate Severe or ESRD
(CrCl 50–89 mL/min) (CrCl 30–50 mL/min) (CrCl <30 mL/min)
SGLT2 inhibitors
Dapagliflozin Forxiga (EU), EMA (2012), 5–10 mg once per day 12∙9 Renal 75%, faeces 21% No adjustment Not approved Not approved
Farxiga (USA) FDA (2014)
Canagliflozin Invokana 2013 100–300 mg once per day 10∙6–13∙1 Renal 34%, faeces 52% No adjustment Not approved Not approved
Empagliflozin Jardiance 2014 10–25 mg once per day 12∙4 Renal 54%, faeces 41% No adjustment Not approved Not approved
Ertugliflozin Steglatro 2017 5–15 mg once per day 11∙0–17∙0 Renal 50%, faeces 41% No adjustment Not approved Not approved
GLP-1 receptor agonists
Exenatide Byetta 2005 5–10 μg twice per day 2∙4 Mainly renal No adjustment Conservative Not recommended
(short-acting) (short-acting) dose escalation
Liraglutide Victoza EMA (2009), 0∙6–1∙2–1∙8 mg once 11∙6–13∙0 Peptidases, renal 6%, No adjustment No adjustment Not recommended
FDA (2010) per day (long-acting) faeces 5%
Exenatide Bydureon EMA (2011), 2 mg once per week Not specified* Mainly renal No adjustment Not recommended Not recommended
(long-acting) FDA (2012) (long-acting)
Lixisenatide Lyxumia (EU), EMA (2013), 10–20 μg once per day 3∙0 (short- Mainly renal No adjustment No adjustment Not recommended
Adlyxin (USA) FDA (2016) acting)
Albiglutide Eperzan (EU), 2014 30–50 mg once per week 120∙0 Peptidases, renal No adjustment No adjustment Not recommended
Tanzeum (USA) (long-acting)
Dulaglutide Trulicity 2014 0∙75–1∙5 mg once 112∙8 Peptidases, renal No adjustment No adjustment Not recommended
per week (long-acting)
Semaglutide Ozempic 2017 0∙5–1∙0 mg once per week 165∙0–184∙0 Peptidases, renal No adjustment No adjustment Not recommended
(long-acting)
DPP-4 inhibitors
Sitagliptin Januvia FDA (2006), 100 mg once per day 12∙4 Renal 87%, faeces 13% No adjustment Dose reduction Dose reduction
EMA (2007) (50 mg per day) (25 mg per day)
Vildagliptin Galvus 2007 50 mg twice per day 2∙0 Renal 85%, faeces 15% No adjustment Dose reduction Dose reduction
(50 mg per day) (50 mg per day)
Saxagliptin Onglyza 2009 5 mg once per day 2∙5 Renal 12–29%, faeces 22% No adjustment Dose reduction Dose reduction
(2∙5 mg per day) (2∙5 mg per day)
Linagliptin Trajenta (EU), 2011 5 mg once per day 12∙0 Renal ~5%, faeces ~80% No adjustment No adjustment No adjustment
Tradjenta (USA)
Alogliptin Nesina (USA) 2013 25 mg once per day 21∙0 Renal ~76%, faeces ~13% No adjustment Dose reduction Dose reduction
(12∙5 mg per day) (6∙25 mg per day)
CrCl=creatinine clearance. DPP-4=dipeptidyl peptidase-4. EMA=European Medicines Agency. ESRD=end-stage renal disease. EU=European Union. FDA=US Food and Drugs Administration. GLP-1=glucagon-like
peptide-1. SGLT2=sodium-glucose co-transporter-2. *The pharmacokinetic profiles of exenatide once per week and exenatide twice per day are similar, except that subcutaneous absorption is prolonged with the
once per week formulation. Data derived from SPCs and Muskiet et al,48 Tahrani et al,49 and Deacon.50
Table 1: Antihyperglycaemic drugs available in Europe and North America with dose reductions in chronic kidney disease
cardiorenal risk profile and effects on clinical outcomes (the putative gut–renal axis69), specifically by enhancing
beyond glycaemia.5 First, GLP-1-receptor-mediated re renal solute excretion in response to acute solute ingestion,
ductions in appetite and food intake result in a loss of forming a feed-forward loop between the gut and the
roughly 0∙8–1∙4 kg in bodyweight,66 albeit with much kidneys.48 GLP-1-receptors have been identified at various
variation in individual responses and within-class locations in the kidney, including preglomerular vascular
differences. DPP-4 inhibitors tend to have no effect on smooth muscle cells and proxi mal tubular cells,
bodyweight, as they do not induce satiety.48,67 Second, emphasising a potential physiological role of GLP-1 in
sustained GLP-1 receptor agonist treatment consistently kidney function.48 Administration of GLP-1 and GLP-1
reduces systolic blood pressure by about 2–3 mm Hg,5,48,68 receptor agonists induces natriuresis, diuresis, and urinary
whereas DPP-4 inhibitors have no uniform anti hyper alkalinisation in healthy men70,71 and people with type 2
tensive effect.5,66 Third, incretin-based therapies modestly diabetes, possibly mediated by inhibition of NHE3 in the
improve fasting and particularly postprandial lipid profiles.5 brush border of the proximal tubule.72–74 As with
Fourth, GLP-1 might modulate inflammation or fibrosis at SGLT2 inhibitors, such proxi mal natriuresis would be
multiple sites.48 Finally, GLP-1 has been implicated in the expected to stimulate tubuloglomerular feedback
enteroendocrine regulation of water and electrolyte balance (TGF) signalling, leading to afferent vasoconstriction and a
6 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
reduction in renal blood flow and GFR. However, in baseline and on-trial HbA1c and other traditional renal
patients with type 2 diabetes, mechanistic studies and risk factors.83 Both LEADER (liraglutide)84 and SUSTAIN-6
clinical trials have not identified (consistent) effects of (semaglutide)85 included a prespecified composite kidney
GLP-1 receptor agonists on renal haemodynamics72–75 or outcome, defined as progression to macroalbuminuria,
acute reductions in (estimated) GFR on initiation of doubling of serum creatinine, end-stage kidney disease
therapy.48 This finding might be explained by direct nitric (ESKD), or kidney death. The kidney composite outcome
oxide-dependent vasodilatory actions of GLP-1 receptor was reduced by 22% with liraglutide in 9340 patients after
agonists at the afferent arteriole, which might override or 3∙8 years83 and 36% by semaglutide in 3297 patients after
offset vasoconstriction induced by TGF (figure 2).71 Renal 104 weeks.86 Notably, in both trials, the effects were driven
response to DPP-4 inhibition might be even more by a 26−46% reduction in macroalbuminuria, rather than
complicated, as DPP-4 inhibitors induce natriuresis, at more clinically relevant kidney endpoints. In LEADER,
least partly independently of GLP-1.69, 76 the difference in kidney outcome was not altered by
Data from placebo-controlled phase 3 trials of adjustment for change in glycaemic control, bodyweight,
GLP-1 receptor agonists in patients with type 2 diabetes or systolic blood pressure.87 Finally, liraglutide modestly
have shown inconsistent effects on albuminuria and slowed eGFR decline by 2% compared with placebo after
generally no effect on eGFR. In the SCALE Diabetes trial, 36 months (−7∙44 vs −7∙82 mL/min per 1∙73 m²), the
56 weeks of liraglutide resulted in dose-dependent clinical relevance of which is uncertain.83,85
reductions in UACR,77 whereas the 26-week LIRA-RENAL In parallel to its finite effect on cardiovascular outcomes
trial in patients with type 2 diabetes and moderate-to- or mortality, DPP-4 inhibitor therapy might have, at best,
severe kidney impairment did not show reductions in a modestly beneficial effect on kidney endpoints in at-risk
UACR.78 In a small crossover trial in patients with type 2 patients with type 2 diabetes. In a pooled analysis of
diabetes and albuminuria who were on RAAS inhibitors, placebo-controlled trials, linagliptin reduced kidney disease
liraglutide given for 12 weeks reduced 24 h urinary events by 16%, driven by an 18% reduction in moderate
albumin excretion by 32% compared with placebo, albuminuria and a 14% reduction in severe albuminuria,
independent of HbA1c reductions and possibly driven with no effects on eGFR.88 Moreover, combined data from
by blood pressure lowering.77 Integrated data from randomised controlled trials including 217 patients with
nine registration trials of dulaglutide, which included type 2 diabetes and albuminuria suggested that linagliptin
6005 patients with type 2 diabetes, showed lower UACRs reduced UACR by 28%, independent of HbA1c or systolic
than with placebo (−16∙7% vs 10∙0%), insulin glargine blood pressure.89 However, MARLINA-T2D, which included
(−16.7% vs 3∙7%), and other active comparators 360 patients with type 2 diabetes on stable RAAS inhibition
(−20∙0% vs −12∙5%).79 Although no differences in serum and was sufficiently powered to test superiority of
creatinine levels were observed over 104 weeks, fewer linagliptin in reducing albuminuria, did not confirm these
patients receiving dulaglutide rather than insulin findings.90 Five cardio vascular outcome trials involving
glargine experienced a 40% decline in eGFR at any point DPP-4 inhibitors have provided data on kidney endpoints.
during a 1-year treatment period.80 In the AWARD-7 trial, In a secondary analysis of SAVOR-TIMI 53, which included
which included 577 patients with type 2 diabetes and 16 492 patients with type 2 diabetes at high risk of
moderate-to-severe chronic kidney disease, dulaglutide cardiovascular events, saxagliptin led to reclassification of
versus once-daily titrated insulin glargine (with similar patients into a lower UACR category, irrespective of
HbA1c reductions) resulted in a higher eGFR after baseline UACR.91 An overall mean reduction in UACR
52 weeks, and reduced UACR in patients with baseline of 34 mg/g was seen with saxagliptin, which was
macroalbuminuria.81 independent of HbA1c lowering, although the drug did not
Kidney outcome data have been collected as secondary affect other more clinically relevant kidney endpoints after
and exploratory endpoints in previous (table 2) and on 2∙1 years. In TECOS,92 which included 14 671 patients, there
going (table 3) cardiovascular safety trials of GLP-1 receptor was no clinically relevant difference in either eGFR or
agonists and DPP4 inhibitors in patients with type 2 UACR between the sitagliptin and placebo groups. In the
diabetes and high cardiovascular risk.48 In ELIXA, which MK-3102-018 cardiovascular outcome trial, which was
assessed the cardiovascular safety of lixisenatide versus terminated early in 2016 based on a business decision by
placebo in 6068 patients with type 2 diabetes and a the sponsor not to submit a marketing application, there
previous acute coronary event, the percentage change in were no clinically meaningful changes from baseline in
UACR showed a modest difference in favour of the eGFR at any timepoint between the once-weekly DPP-4
GLP-1 receptor agonist after 25 months of follow-up inhibitor omarigliptin and placebo in 4202 patients with
(24% vs 34%).82 However, in the total population, post-hoc type 2 diabetes and established cardiovascular disease after
adjustment for HbA1c levels attenuated the lixisenatide- a median follow-up of 96 weeks.93 Finally, in CARMELINA,
induced kidney benefit, suggesting some glucose linagliptin versus placebo did not significantly affect the
dependency. Nevertheless, in a recent exploratory analysis secondary kidney composite outcome (sustained >40%
of ELIXA, lixisenatide was associated with a lower risk of decrease in eGFR from baseline, ESKD or renal death) in
new-onset macroalbuminuria after adjustment for 6979 patients with type 2 diabetes at high cardiovascular
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 7
Review
Drug n Main Follow-up Mean Mean Mean Mean Baseline Renal outcome
inclusion (years) age type 2 baseline baseline albuminuria
criteria* (years) diabetes HbA1c eGFR status
duration (%) (mL/min
(years) per 1∙73 m²)
SGLT2 inhibitors
EMPA-REG Empagliflozin 7020 CVD history 3∙1 63∙1 57% >10 8∙1 74∙0 Micro 29%; Secondary: composite (macroalbuminuria, dSCr,
OUTCOME (2016) (median) macro 11% ESKD, renal death); HR 0∙61, 95% CI 0∙53–0∙70
CANVAS Program Canagliflozin 10 142 CVD risk or 3∙6 (mean) 63∙3 13∙5 8∙2 76∙5 Micro 22∙6%; Secondary: composite (macroalbuminuria, dSCr,
(2017) history macro 7∙6% ESKD, renal death); HR 0∙58, 95% CI 0∙50–0∙67
DECLARE-TIMI 58 Dapagliflozin 17 160 CVD risk or 4∙2 63∙8 11∙8 8∙3 86∙1 Micro: 23∙4%; Secondary: composite (>40% decrease in eGFR
(2018) history (median) macro 6∙8% to <60 ml/min per 1∙73 m2, ESKD, renal death)
HR 0∙53 (0∙43–0∙66)
GLP-1 receptor agonists
ELIXA (2015) Lixisenatide 6068 ACS <180 2∙1 60∙3 9∙3 7∙7 76∙0 Micro 19∙2%; Secondary: change in UACR; month 24,
days before (median) macro 6∙5% 34% vs 24%
start of trial
LEADER Liraglutide 9340 CVD risk or 3∙8 64∙3 12∙7 8∙7 80∙0 Micro 26∙3%; Secondary: composite (macroalbuminuria, dSCr,
(2016/2017) history (median) macro: 10∙5% ESKD, renal death); HR 0∙78, 95% CI 0∙67–0∙92
SUSTAIN-6 Semaglutide 3297 CVD risk or 2∙1 64∙6 13∙9 8∙7 NR NR Secondary: composite (macroalbuminuria, dSCr,
(2016) (subcutaneous) history (median) ESKD, renal death); HR 0∙64 95% CI 0∙46–0∙88
EXSCEL (2017) Exenatide 14 752 CVD risk 3∙2 62∙7 12∙0 8∙0 79∙0 NR NR
(long-acting) (median)
HARMONY Albiglutide 9463 CVD history 1∙6 64∙1 14∙1 8∙7 79∙0 NR Safety: eGFR difference: at 8 months: –1·11
Outcomes (2018) (median) (95% CI –1·84 to –0·39), at 16 months: –0·43
(–1·26 to 0·41)
DPP-4 inhibitors
EXAMINE (2013) Alogliptin 5380 ACS <90 1∙5 61∙0 7∙2 8∙0 71∙2 NR Secondary: change in eGFR mL/min per 1∙73 m²
days before (median) per eGFR subgroup for alogliptin and
start of trial placebo: eGFR >90 (–4∙5/−6∙7); 60–90 (1∙0/0∙6);
30–60 (2∙1/1∙1); <30 (1∙6/0∙2)
SAVOR-TIMI 53 Saxagliptin 16 492 CVD risk or 2∙1 65∙1 10∙3 8∙0 72∙6 Micro 28∙1%; Secondary: change in UACR 34∙3 mg/g; dSCr
(2013) history (median) macro 10∙4% HR 1·1, 95% CI 0∙89–1∙36; ESKD HR 0·90, 95% CI
0∙61–1∙32
TECOS (2015) Sitagliptin 14 671 CVD history 3∙0 65∙5 11∙6 7∙2 75∙1 Micro 23∙3%; Secondary: eGFR difference −1∙34 (95% CI
(median) macro 4∙8% −1∙76 to −0∙91); UACR difference −0∙18 mg/g
(95% CI −0∙35 to −0∙02)
MK-3102-018 Omarigliptin 4202 CVD history 1∙8 63∙7 12∙1 8∙0 86∙2 NR Safety: eGFR difference −2∙43 (95% CI
(2017) (median) −5∙36 to 0∙51)
CARMELINA Linagliptin 6979 CKD and 2∙2 65∙8 14∙7 7∙9 54∙6 Micro 41∙5%; Secondary: composite (≥40% eGFR reduction,
(2018) CVD history (median) macro 38∙6% ESKD, renal death) HR, 1∙04; 95% CI, 0∙89-1∙22.
or risk Exploratory: albuminuria progression HR 0∙86
(0∙78–0∙95)
ACS=acute coronary syndrome. CVD=cardiovascular disease. DPP-4=dipeptidyl peptidase-4. dSCr= doubling of serum creatinine concentration. eGFR=estimated glomerular filtration rate. ESKD=end-stage
kidney disease. GLP-1=glucagon-like peptide-1. HR=hazard ratio. NR=not reported. SGLT2=sodium-glucose co-transporter-2. UACR=urinary albumin-to-creatinine ratio. *All patients in all trials had type 2
diabetes.
Table 2: Effect of new-generation glucose-lowering drugs in completed cardiovascular outcome trials on secondary and exploratory renal outcomes in patients with type 2 diabetes and
high cardiovascular risk
and renal risk (ie, impaired eGFR and microalbuminuria (NCT01243424; comparing linagliptin and glimepiride)
or macroalbuminuria) after a median of 2∙2 years. In and GRADE (NCT01794143; comparing liraglutide,
exploratory renal analyses, the progression of the sitagliptin, glimepiride, and insulin glargine) are antici
albuminuria category occurred less frequently in the pated. However, by contrast with SGLT2 inhibitors, there
linagliptin group (hazard ratio [HR] 0∙86; 95% CI are no ongoing studies of incretin-based therapies
0∙78–0∙95).94 recruiting patients with diabetic kidney disease with a
Although incretin-based therapies (particularly primary objective of determining the effects of these
GLP-1 receptor agonists) might improve albuminuria in drugs on kidney endpoints.
type 2 diabetes, effects on more clinically relevant kidney
outcomes such as time to starting dialysis remain Endothelin receptor antagonists
uncertain. The results of active-comparator studies that The endothelin family comprises three endothelins
include secondary kidney endpoints such as CAROLINA (ET-1, ET-2, and ET-3) that bind to either the ETA or the
8 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
ClinicalTrials. Drug n Main inclusion Follow-up Mean Mean Mean Mean Baseline Trial status Renal outcome
gov (class) criteria (years) age type 2 baseline baseline albuminuria (expected
registration (years) diabetes HbA1c eGFR status completion
number duration (%) (mL/min date)
(years) per 1∙73 m2)
Renal outcome trials
SONAR NCT01858532 Atrasentan 5112 Type 2 diabetes, ~4 64∙8 16∙7 7∙8 43∙8 Macro 100% Terminated Primary:
(ETA receptor eGFR 25–75 mL/ (December, composite (dSCr,
antagonist) min per 1∙73 m², 2017) ESKD, renal death)
macroalbuminuria
CREDENCE NCT02065791 Canagliflozin 4401 Type 2 diabetes, Up to 5∙5 63∙0 15∙8 8∙3 56∙2 Macro 100% Terminated Primary:
(SGLT2 macroalbuminuria (July, 2018) composite (ESKD,
inhibitor) dSCr,
cardiovascular
death, renal death)
FIDELIO-DKD NCT02540993 Finerenone 4800 Type 2 diabetes, Up to 4 ∙∙ ∙∙ ∙∙ ∙∙ Macro 100% Ongoing Primary:
(MRA) macroalbuminuria, (April, 2020) composite (ESKD,
potassium ≥40% reduction in
≤4∙8 mmol/L eGFR, renal death)
DAPA-CKD NCT03036150 Dapagliflozin 4000 eGFR Up to 4 ∙∙ ∙∙ ∙∙ ∙∙ ∙∙ Ongoing Primary: composite
(SGLT2 25–75 mL/min per (November, (>50% reduction in
inhibitor) 1∙73 m², increased 2020) eGFR, ESKD,
albuminuria cardiovascular
death, renal death)
EMPA- NCT03594110 Empagliflozin 5000 eGFR 20-45 mL/ ~3∙1 Ongoing Primary: composite
KIDNEY (SGLT2 min per 1∙73 m² or (June, 2022) of kidney disease
inhibitor) 45-90 mL/min per progression (ESKD,
1∙73 m² with eGFR <10 mL/min
albuminuria per 1∙73 m², renal
death, or ≥40%
reduction in eGFR)
or cardiovascular
death
Cardiovascular outcome trials
FREEDOM- NCT01455896 Exenatide 4156 Type 2 diabetes, 2 NR NR NR NR NR Completed NR
CVO DUROS† CVD history (March,
(GLP-1 2016)
receptor
agonist)
REWIND NCT01394952 Dulaglutide 9901 Type 2 diabetes, 6.5 66∙2 10∙0 7∙3 77∙6 Micro/macro Completed Secondary:
(GLP-1 CVD risk or history 35∙3% (August, composite
receptor 2018) (retinopathy,
agonist) proteinuria, >30%
reduction in eGFR,
ESKD)
CAROLINA NCT01243424 Linagliptin* 6103 Type 2 diabetes, 8∙3 64∙0 6∙2 7∙2 77∙0 Micro 21∙2%; Completed Secondary:
(DPP-4 CVD risk or history macro 4∙3% (August, transition in
inhibitor) 2018) albuminuria
classes, change in
eGFR, change in
UACR
PIONEER-6 NCT02692716 Semaglutide 3183 Type 2 diabetes, Up to 1∙6 66∙1 14∙9 8∙2 74∙2 NR Completed NR
(GLP-1 CVD risk or history (September,
receptor 2018)
agonist
[oral])
VERTIS-CV NCT01986881 Ertugliflozin 8000 Type 2 diabetes, Up to 6∙1 .. .. .. .. .. Ongoing Secondary:
(SGLT2 CVD history (September, Composite (dSCr,
inhibitor) 2019) ESKD, renal death)
FIGARO-DKD NCT02545049 Finerenone 6400 Type 2 diabetes, Up to 4∙4 .. .. .. .. Macro 100% Ongoing Secondary:
(MRA) macroalbuminuria, (June, composite (ESKD,
potassium 2021) ≥40% reduction in
≤4∙8 mmol/L eGFR, renal death),
change in UACR
(Table 3 continues on next page)
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 9
Review
ClinicalTrials. Drug (class) n Main inclusion Follow-up Mean Mean Mean Mean Baseline Trial status Renal outcome
gov criteria (years) age type 2 baseline baseline albuminuria (expected
registration (years) diabetes HbA1c eGFR (mL/ status completion
number duration (%) min per date)
(years) 1∙73 m2)
(Continued from previous page)
Heart failure outcome trials
DAPA-HF NCT03036124 Dapagliflozin 4744 Type 2 diabetes, Up to 3 .. .. .. .. .. Ongoing Secondary:
(SGLT2 HFrEF (December, composite
inhibitor) (NYHA II–IV), 2019) (>50% reduction
LVEF ≤40%, high in eGFR, ESKD,
NT-proBNP renal death)
EMPEROR- NCT03057951 Empagliflozin 4126 HFpEF Up to 3∙2 .. .. .. .. .. Ongoing Secondary: eGFR
preserved (SGLT2 (NYHA II–VI), LVEF (June, slope, ESKD,
inhibitor) >40%, high 2020) or ≥40% reduction
NT-proBNP in eGFR
EMPEROR- NCT03057977 Empagliflozin 2850 HFrEF Up to 3∙2 .. .. .. .. .. Ongoing Secondary: eGFR
reduced (SGLT2 (NYHA II–VI), (June, slope, ESKD,
inhibitor) LVEF ≤40%, high 2020) or ≥40% reduction
NT-proBNP in eGFR
CKD=chronic kidney disease. CVD=cardiovascular disease. DPP-4=dipeptidyl peptidase-4. dSCr= doubling of serum creatinine concentration. eGFR=estimated glomerular filtration rate. ESKD=end-stage kidney
disease. ETA= endothelin A. GLP-1=glucagon-like peptide-1. SGLT2=sodium-glucose co-transporter-2. HFpEF=heart failure with preserved ejection fraction. HFrEF=heart failure with reduced ejection fraction.
LVEF=left ventricular ejection fraction. MRA=mineralocorticoid receptor antagonist. NR=not reported. NT-proBNP=N-terminal pro-B-type natriuretic peptide. NYHA=New York Heart Association. UACR=urinary
albumin-to-creatinine ratio. *Versus active comparator glimepiride. †The DUROS delivery system paired with exenatide (ITCA650) is a matchstick-sized, miniature osmotic pump that is inserted subcutaneously
to provide continuous and consistent treatment with exenatide therapy.
Table 3: Recently completed and ongoing clinical outcome trials assessing the effect of new drugs in type 2 diabetes on renal outcomes
ETB receptor. Generally, ETA receptor activation causes increase in effective renal blood flow and reduction in
vasoconstriction, matrix accumulation, and cell pro filtration fraction, suggesting that ET-1 causes vaso
liferation, whereas ETB receptor activation opposes constriction mediated by the efferent arteriole.101,102 In
these effects.95,96 The endothelin system also has an addition to haemodynamic effects, use of the ERA
important role in sodium and water regulation. atrasentan led to a reduction in albuminuria in one study,
Although ETB activation has a sodium and water re possibly through protection of the glycocalyx.103 Other
taining effect, ETA exerts a natriuresis effect, particularly potential mechanisms of ERA-induced renoprotection
via ETA receptors located in the collecting duct.97,98 involve preservation of podocyte morphology104 and
Pharmacological blockade of endothelin receptors is changes in production of growth factors and vaso
associated with sodium and water retention and this constrictors (eg, angiotensin II).105 Avosentan was the first
effect has made development of endothelin blockers ERA to be tested in a large, randomised, placebo-
challenging. controlled trial, which included 286 patients with diabetic
The endothelin system is believed to be involved in the kidney disease and macroalbuminuria. This 12-week trial
development and progression of diabetic kidney disease.99 showed a dose-dependent reduction in proteinuria, with
Patients with diabetic kidney disease generally have an optimal dose of 10 mg per day. Higher doses (≥25 mg
hyperglycaemia, insulin resistance, obesity, dyslipid per day) increased the risk of the main adverse outcome,
aemia, RAAS activation, endothelial dysfunction, and peripheral oedema (12%).106 Following this dose-finding
increased oxidative stress, all of which increase pro study, a large phase 3 trial assessing the effect of avosentan
duction of ET-1 in the kidney.99 Apart from its potent (at 25 and 50 mg per day) versus placebo on kidney
vasoconstrictive effects on the efferent renal vasculature, outcomes in 1392 patients with type 2 diabetes (ASCEND)
which can result in a reduction of renal blood flow and was undertaken, but was terminated early because of an
glomerular hyperfiltration,16 ET-1 might promote kidney excess of congestive heart failure and mortality associated
injury by activating pro-inflammatory and profibrotic with the ERA.21 These results show the narrow therapeutic
pathways.97,98 window of ERAs and the importance of careful dose
Data from multiple experimental and clinical selection to avoid adverse consequences of sodium and
mechanistic studies have supported the hypothesis that fluid retention.
endothelin blockade might delay the progression of Atrasentan, which has a higher ERA selectivity than
kidney disease in the long term. Endothelin receptor avosentan and might therefore exert less sodium
antagonists (ERAs) attenuate the vasoconstrictor effect of retention, has also been tested in diabetic kidney disease.
ET-1 and thereby reduce intraglomerular pressure and In a phase 2 trial (RADAR), atrasentan given at doses of
hyperfiltration (figure 2). In patients with hypertension 0∙75 mg or 1∙25 mg per day, reduced albuminuria versus
and chronic kidney disease, ERAs cause a significant placebo by 35% and 38%, respectively, in 211 patients
10 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
with diabetic kidney disease and overt proteinuria after
12 weeks, with the 1∙25 mg per day dose leading to Panel 1: Preventive measures to avoid hyperkalaemia in patients with diabetic
greater sodium retention.107 A large phase 3 confirmatory kidney disease receiving mineralocorticoid receptor agonist therapy*
outcome trial (SONAR), evaluating the effect of Monitoring serum K+ during MRA treatment
atrasentan in type 2 diabetes patients with chronic kidney Enables quick recognition of unusual changes in K⁺ levels, but optimal timing and
disease stage 2–4, which selected individual participants duration of K⁺ monitoring unknown
on the basis of their initial atrasentan response in terms
of albuminuria and bodyweight,108 was stopped Selection of patients on the basis of indices of mineralocorticoid activity (PRA,
prematurely because of a lower than expected number of urinary Na⁺:K⁺ ratio, FEK, or TTKG)
renal events (rather than safety concerns), with results More specific method of identifying risk of hyperkalaemia than exclusion of known
expected to be reported in 2019. common risk factors such as age, diabetes status, or eGFR, but indices are affected by diet
and GFR and methods are not validated
Mineralocorticoid receptor antagonists Dietary restriction of potassium intake and use of diuretics
The steroidal mineralocorticoid receptor (MR) has an Easy method to reduce risk of developing hyperkalaemia, but long-term compliance with
important role in the RAAS. Although traditionally dietary restriction is difficult to maintain
angiotensin II has been considered the key component
of the RAAS that mediates end-organ damage, it has Review of concomitant therapies (for example NSAIDs, β-blockers, and heparin)
become increasingly clear that aldosterone is at least as Easy method to prevent drug-related alterations in K⁺ homeostasis, but physicians are
important in driving cardiovascular and kidney injury, often unaware of all medications taken by the patient, and not all drugs with known
beyond the effects of renin and angiotensin II.109 Patients interaction can be safely discontinued
with diabetic kidney disease show increased activity of Reduce MRA dose
the MRs, which is probably driven by increased levels Reduced risk of developing hyperkalaemia, but possible reduced efficacy of MRAs
of circulating aldosterone, altered cortisol activity, or
increased local expression of the MR.110 MRA=mineralocorticoid receptor antagonist. PRA=plasma renin activity. FEK=fractional excretions of K⁺. TTKG=transtubular
potassium gradient. eGFR= estimated glomerular filtration rate. NSAIDs=non-steroidal anti-inflammatory drugs. *Derived
Clinically approved steroid-based MRAs, including from Roscioni et al.117
spironolactone and eplerenone, mimic the molecular
structure of the natural MR ligands. Findings from
clinical trials have shown that MRAs further reduce tested in ARTS-DN, a phase 2 clinical trial in patients with
albuminuria and blood pressure in patients with diabetic type 2 diabetes with diabetic kidney disease.120 823 patients
and non-diabetic kidney diseases when added to a RAAS were randomly assigned to receive once-daily doses of
inhibitor.111–113 Moreover, results from a prospective, open- finerenone (7∙5, 10, 15, or 20 mg) or placebo, as an adjunct
label study suggested that spironolactone might stabilise to RAAS inhibition. Finerenone decreased UACR in a
decline in kidney function in patients with proteinuric dose-dependent manner; a placebo-adjusted reduction of
kidney diseases.114 However, the use of MRAs is limited 21–38% was reported from baseline to 90 days. There
in clinical practice by adverse effects. Spironolactone is a were no differences in the incidence of the prespecified
poorly selective MRA and inhibits androgen and secondary outcome, an eGFR decrease of 30% or more,
progesterone receptors, increasing the likelihood of sex compared with placebo. Hyperkalaemia occurred in 12
hormone-related side-effects such as gynaecomastia, (1∙5%) out of 821 patients assigned to finerenone,
impotence, and menstrual irregularities, as well as compared with none of the 94 patients in the placebo
hyperkalaemia. Addition of both spiro no
lactone and group, although only patients with baseline potassium
eplerenone to RAAS inhibition increases the risk of levels of less than 4∙8 mmol/L were eligible and few
hyperkalaemia by three to eight times.115,116 This adverse patients with an eGFR less than 45 mL/min per 1∙73 m²
effect is particularly pronounced in older patients, and macroalbuminuria were included in the study. The
patients with diabetes, and those with chronic kidney efficacy and safety of finerenone in patients with diabetic
disease (ie, the population who might also gain the kidney disease is being tested in the ongoing FIDELIO-
greatest benefit from MRAs).117 Preventive measures to DKD (NCT02540993; expected study completion October,
avoid hyperkalaemia during MRA treatment are 2019) and FIGARO-DKD (NCT02545049; expected study
described in panel 1. completion February, 2020) trials.
In an attempt to more precisely target the MR, potent
MRAs that might exhibit less potassium retention— Future perspectives
specifically non-steroidal compounds such as Many of the new therapies described in the previous
finerenone—have been developed.118,119 In contrast with sections, which might improve outcomes for patients
spironolactone and eplerenone, which bind to the ligand with diabetic kidney disease, have already been granted
domain of the MR, finerenone induces a conformational marketing authorisation by regulatory agencies for non-
change within the MR complex, thereby ultimately renal indications, or are in advanced stages of develop
changing the stability and nuclear translocation of the ment. However, diabetic kidney disease is a multifactorial,
receptor.114 The efficacy and safety of finerenone has been heterogeneous disease comprising various complex
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 11
Review
Panel 2: Hurdles to the development of novel therapies to reduce the burden of Search strategy and selection criteria
diabetic kidney disease
We searched MEDLINE, PubMed, Google Scholar, and the
Several challenges are apparent for the development of new treatments or combinations Cochrane Library for English-language abstracts and full-text
of drugs for chronic kidney disease, including factors that must be considered in trial articles published up to Nov 30, 2018. We focused on new
design and the identification of appropriate endpoints and efficacy biomarkers. potentially renoprotective drugs in type 2 diabetes, with
Additionally, testing of novel therapies aimed at slowing the progression of diabetic kidney particular attention paid to sodium-glucose
disease must be done in patients with diabetes who are already receiving standard care, co-transporter-2 (SGLT2) inhibitors, incretin-based therapies,
including optimal risk factor control such as the use of renin–angiotensin– aldosterone endothelin receptor antagonists, and mineralocorticoid
system (RAAS) blockers. receptor antagonists. The keywords used included
“diabetic kidney disease”, “diabetic nephropathy”,
Diagnosis
“renoprotection”, “type 2 diabetes”, “sodium-glucose
• Disease awareness in patients with chronic kidney disease stages 1–3 is ~5%
cotransporter-2 inhibitor”, “SGLT2 inhibitor”, “incretin-based
• Physicians might neglect to inform patients that they have chronic kidney disease
therapy”, “glucagon-like peptide-1”, “GLP-1 receptor agonist”,
Clinical trial recruitment “dipeptidyl-peptidase-4 inhibitor”, “DPP-4 inhibitor”,
• Recruitment rates for diabetic kidney disease are ~0∙20 patients per site per month “endothelin receptor antagonist”, “mineralocorticoid
(~25% of the number of patients enrolled per month for a diabetes trial) receptor antagonist”, and “MRA”. These keywords were used
• Low rates delay timelines, increase costs, and negatively affect willingness of as single search terms and in combination. We also searched
pharmaceutical companies to invest the reference list of original articles, narrative reviews, clinical
• Clinical trial networks and patient registries could help to address this challenge guidelines, and systematic reviews and meta-analyses for
further relevant material. The evidence discussed in this
Patient selection
Review is mainly restricted to clinical studies, including
• Elimination of probable biological non-responders who decrease trial efficiency vs
cohort studies, randomised controlled trials, and
patient heterogeneity with respect to rate of renal function loss
meta-analyses of randomised clinical trials.
• Widespread use of RAAS blockers restricts recruitment of patients with high levels of
albuminuria and so-called rapid progressors
• Increasing numbers of patients with diabetic kidney disease who progress without as the diuretic properties of the SGLT2 inhibitor could
developing proteinuria; ~25% do not follow the classic paradigm mitigate the sodium and fluid retaining effects of the
• Development of novel biomarkers could supplement proteinuria in predicting ERA. Additionally, the renal haemodynamic benefits of
progression of renal disease SGLT2 inhibitors involves the afferent arteriole via TGF
Clinical endpoints signalling, whereas the ERAs reduce glomerular pressure
• Characterising the effect of a drug on renal markers (surrogates) vs parameters of by directly reducing efferent arteriolar resistance.
patient wellbeing and hard outcomes vs a composite of these Finally, although nearly all patients with type 2 diabetes
• Intermediate events and surrogates should match with the appropriate mechanisms will require multiple therapies to maintain glycaemic
of action of the drug (ie, acute reductions in renal function with RAAS blockers and control, no large-scale studies have provided definite data
sodium-glucose co-transporter-2 inhibitors) as to which are the best combinations to use. The ideal
• Using intermediate eGFR decrements (ie, 30%, or 40%, or eGFR slope) as surrogates of combination should correct multiple pathophysiological
accepted outcomes (ie, doubling of serum creatinine) defects in type 2 diabetes, while being well tolerated and
safe, easy to administer, and cost-effective. Based on their
different mechanisms of action in terms of reducing
phenotypes and it seems probable that not all patients glucose, bodyweight, blood pressure, and other cardio
will benefit from these drugs.121 Between-patient variation renal risk factors, combination therapy with an SGLT2
in underlying pathophysiology results in a wide diversity inhibitor and a GLP-1 receptor agonist might be expected
of individual drug responses, as described in more detail to fulfil (most of) these criteria.123 Hitherto, two trials have
elsewhere.122 This variation in individual drug response assessed this combination in patients with poorly
was addressed in the design of the SONAR trial described controlled type 2 diabetes and have shown useful
previously, which selected only responder patients reductions in glycaemic measures and additive effects on
(albuminuria reduction >30%) and excluded those who weight loss and lowering of blood pressure.117,118 Such
do not tolerate atrasentan.108 However, whether non- combination therapy might be even more powerful in
responders to atrasentan (in terms of albuminuria) slowing the progression of diabetic kidney disease beyond
might benefit from an SGLT2 inhibitor, an incretin-based either drug class used alone, but dedicated studies to
drug, or an MRA is an important question to be answered assess the effects of this combination on albuminuria and
in the future. kidney outcomes are needed to investigate this
It is also probable that future studies will start possibility.124,125 We believe that well designed mechanistic
combining new therapies to further slow the progression studies that aim to characterise individual drug responses
of diabetic kidney disease. Theoretically, the effect of an on the basis of phenotypic traits, as well as large-sized
SGTL2 inhibitor and an ERA would be complementary, prospective outcome trials that assess the cardiorenal
12 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
effects of different combinations of drugs, are necessary 7 Roussel R, Lorraine J, Rodriguez A, Salaun-Martin C. Overview of
to advance treatment approaches in patients with type 2 data concerning the safe use of antihyperglycemic medications in
type 2 diabetes mellitus and chronic kidney disease. Adv Ther 2015;
diabetes. Hurdles to overcome in the development of 32: 1029–64.
novel therapies to reduce the burden of diabetic kidney 8 Hung SC, Chang YK, Liu JS, et al. Metformin use and mortality in
disease and test combinations of drugs in patients with patients with advanced chronic kidney disease: national,
retrospective, observational, cohort study. Lancet Diabetes Endocrinol
type 2 diabetes are outlined in panel 2. 2015; 3: 605–14.
9 Scheen AJ. Pharmacokinetic considerations for the treatment of
Conclusions diabetes in patients with chronic kidney disease.
Expert Opin Drug Metab Toxicol 2013; 9: 529–50.
Several promising new approaches are emerging to 10 Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of
protect kidney function in patients with type 2 diabetes. hyperglycemia in type 2 diabetes, 2015: a patient-centered approach:
Such progress should offer hope to patients in whom update to a position statement of the American Diabetes
Association and the European Association for the Study of
a progressive loss of kidney function leads to ill health and Diabetes. Diabetes Care 2015; 38: 140–49.
reductions in quality of life. None of these new therapies 11 de Boer IH, Bakris G, Cannon CP. Individualizing blood pressure
have yet been adequately proven in large-scale randomised targets for people with diabetes and hypertension: comparing the
ADA and the ACC/AHA recommendations. JAMA 2018;
controlled trials assessing clinically relevant kidney 319: 1319–20.
endpoints such as 50% reduction in eGFR or the need to 12 Strippoli GF, Bonifati C, Craig M, Navaneethan SD, Craig JC.
initiate renal replacement therapy. Many such trials are Angiotensin converting enzyme inhibitors and angiotensin II
receptor antagonists for preventing the progression of diabetic
ongoing and several will be reported within the next kidney disease. Cochrane Database Syst Rev 2006; 4: CD006257.
3–5 years. Some of these agents, by virtue of their mode of 13 Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of
action, might also benefit patients with proteinuric kidney the angiotensin-receptor antagonist irbesartan in patients with
nephropathy due to type 2 diabetes. N Engl J Med 2001; 345: 851–60.
disease resulting from pathological processes other than
14 Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on
diabetic kidney disease. Bearing in mind the unmet need, renal and cardiovascular outcomes in patients with type 2 diabetes
clinicians will no doubt welcome these new therapies and and nephropathy. N Engl J Med 2001; 345: 861–69.
will be tempted to initiate them in patients with chronic 15 Brenner BM, Lawler EV, Mackenzie HS. The hyperfiltration theory:
a paradigm shift in nephrology. Kidney Int 1996; 49: 1774–77.
kidney disease for other indications (eg, to reduce
16 Tonneijck L, Muskiet MH, Smits MM, et al. Glomerular
cardiovascular risk) before kidney endpoint studies are hyperfiltration in diabetes: mechanisms, clinical significance,
completed. However, new risks might emerge in patients and treatment. J Am Soc Nephrol 2017; 28: 1023–39.
with chronic kidney disease. Whatever the specific 17 de Zeeuw D, Remuzzi G, Parving HH, et al. Proteinuria, a target
for renoprotection in patients with type 2 diabetic nephropathy:
findings of ongoing and future trials, we seem to be lessons from RENAAL. Kidney Int 2004; 65: 2309–20.
entering a new era in the management of patients with 18 Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin
chronic kidney disease in the context of type 2 diabetes. inhibition for the treatment of diabetic nephropathy. N Engl J Med
2013; 369: 1892–903.
Contributors 19 Parving HH, Brenner BM, McMurray JJ, et al. Cardiorenal end
All authors are fully responsible for all content, were involved at all points in a trial of aliskiren for type 2 diabetes. N Engl J Med 2012;
stages of writing and development of the Review, and have approved the 367: 2204–13.
final version. 20 Packham DK, Wolfe R, Reutens AT, et al. Sulodexide fails to
demonstrate renoprotection in overt type 2 diabetic nephropathy.
Declaration of interests
J Am Soc Nephrol 2012; 23: 123–30.
MHAM is a consultant for Eli Lilly & Co and Novo Nordisk (all honoraria
21 Mann JF, Green D, Jamerson K, et al. Avosentan for overt diabetic
paid to his employer). DCW has received honoraria or consultancy fees
nephropathy. J Am Soc Nephrol 2010; 21: 527–35.
from Akebia, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim,
22 de Zeeuw D, Akizawa T, Audhya P, et al. Bardoxolone methyl in
GlaxoSmithKline, Janssen, and Vifor Fresenius. HJLH is a consultant
type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med
for AbbVie, Astellas, AstraZeneca, Boehringer Ingelheim, Fresenius, 2013; 369: 2492–503.
Gilead, Janssen, and Merck (all honoraria paid to his employer).
23 Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ.
References Sodium glucose cotransporter 2 inhibitors in the treatment of
1 Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work diabetes mellitus: cardiovascular and kidney effects, potential
Group. KDIGO clinical practice guideline for the evaluation and mechanisms, and clinical applications. Circulation 2016; 134: 752–72.
management of chronic kidney disease. Kidney Int Suppl 2013; 24 Wright EM, Loo DD, Hirayama BA. Biology of human sodium
3: 1–150. glucose transporters. Physiol Rev 2011; 91: 733–94.
2 Fox CS, Matsushita K, Woodward M, et al. Associations of kidney 25 Freitas HS, Anhe GF, Melo KF, et al. Na+-glucose transporter-2
disease measures with mortality and end-stage renal disease in messenger ribonucleic acid expression in kidney of diabetic rats
individuals with and without diabetes: a meta-analysis. Lancet 2012; correlates with glycemic levels: involvement of hepatocyte nuclear
380: 1662–73. factor-1α expression and activity. Endocrinology 2008; 149: 717–24.
3 de Zeeuw D, Heerspink HJ. Unmet need in diabetic nephropathy: 26 Rahmoune H, Thompson PW, Ward JM, Smith CD, Hong G,
failed drugs or trials? Lancet Diabetes Endocrinol 2016; 4: 638–40. Brown J. Glucose transporters in human renal proximal tubular
4 Muskiet MHA, Heerspink HJL, van Raalte DH. SGLT2 inhibition: cells isolated from the urine of patients with non-insulin-dependent
a new era in renoprotective medicine? Lancet Diabetes Endocrinol diabetes. Diabetes 2005; 54: 3427–34.
2017; 5: 569–71. 27 van Bommel EJ, Muskiet MH, Tonneijck L, Kramer MH,
5 Muskiet MH, Tonneijck L, Smits MM, Kramer MH, Heerspink HJ, Nieuwdorp M, van Raalte DH. SGLT2 inhibition in the diabetic
van Raalte DH. Pleiotropic effects of type 2 diabetes management kidney—from mechanisms to clinical outcome.
strategies on renal risk factors. Lancet Diabetes Endocrinol 2015; Clin J Am Soc Nephrol 2017; 12: 700–10.
3: 367–81. 28 Zaccardi F, Webb DR, Htike ZZ, Youssef D, Khunti K, Davies MJ.
6 Wong MG, Perkovic V, Chalmers J, et al. Long-term benefits of Efficacy and safety of sodium-glucose co-transporter-2 inhibitors in
intensive glucose control for preventing end-stage kidney disease: type 2 diabetes mellitus: systematic review and network
ADVANCE-ON. Diabetes Care 2016; 39: 694–700. meta-analysis. Diabetes Obes Metab 2016; 18: 783–94.
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 13
Review
29 Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI. 48 Muskiet MHA, Tonneijck L, Smits MM, et al. GLP-1 and the kidney:
Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. from physiology to pharmacology and outcomes in diabetes.
Kidney Int 2018; 94: 26–39. Nat Rev Nephrol 2017; 13: 605–28.
30 Devenny JJ, Godonis HE, Harvey SJ, Rooney S, Cullen MJ, 49 Tahrani AA, Barnett AH, Bailey CJ. Pharmacology and therapeutic
Pelleymounter MA. Weight loss induced by chronic dapagliflozin implications of current drugs for type 2 diabetes mellitus.
treatment is attenuated by compensatory hyperphagia in Nat Rev Endocrinol 2016; 12: 566–92.
diet-induced obese (DIO) rats. Obesity (Silver Spring) 2012; 50 Deacon CF. Dipeptidyl peptidase-4 inhibitors in the treatment of
20: 1645–52. type 2 diabetes: a comparative review. Diabetes Obes Metab 2011;
31 Horie I, Abiru N, Hongo R, et al. Increased sugar intake as a form 13: 7–18.
of compensatory hyperphagia in patients with type 2 diabetes 51 Summary of product characteristics—dapagliflozin.
under dapagliflozin treatment. Diabetes Res Clin Pract 2018; http://www.ema.europa.eu/docs/en_GB/document_library/
135: 178–84. EPAR_-_Product_Information/human/002322/WC500136026.pdf
32 Komoroski B, Vachharajani N, Boulton D, et al. Dapagliflozin, (accessed Aug 21, 2018).
a novel SGLT2 inhibitor, induces dose-dependent glucosuria in 52 Summary of product characteristics—empagliflozin.
healthy subjects. Clin Pharmacol Ther 2009; 85: 520–26. http://www.ema.europa.eu/docs/en_GB/document_library/
33 Weber MA, Mansfield TA, Cain VA, Iqbal N, Parikh S, EPAR_-_Product_Information/human/002677/WC500168592.pdf
Ptaszynska A. Blood pressure and glycaemic effects of dapagliflozin (accessed Aug 21, 2018).
versus placebo in patients with type 2 diabetes on combination 53 Summary of product characteristics—canagliflozin.
antihypertensive therapy: a randomised, double-blind, http://www.ema.europa.eu/docs/en_GB/document_library/
placebo-controlled, phase 3 study. Lancet Diabetes Endocrinol 2016; EPAR_-_Product_Information/human/002649/WC500156456.pdf
4: 211–20. (accessed Aug 21, 2018).
34 Muskiet MHA, van Bommel EJ, van Raalte DH. Antihypertensive 54 Petrykiv S, Sjostrom CD, Greasley PJ, Xu J, Persson F,
effects of SGLT2 inhibitors in type 2 diabetes. Heerspink HJL. Differential effects of dapagliflozin on
Lancet Diabetes Endocrinol 2016; 4: 188–89. cardiovascular risk factors at varying degrees of renal function.
35 Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Clin J Am Soc Nephrol 2017; 12: 751–59.
cardiovascular outcomes, and mortality in type 2 diabetes. 55 Cherney DZI, Cooper ME, Tikkanen I, et al. Pooled analysis of
N Engl J Med 2015; 373: 2117–28. phase III trials indicate contrasting influences of renal function on
36 Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and blood pressure, body weight, and HbA1c reductions with
cardiovascular and renal events in type 2 diabetes. N Engl J Med empagliflozin. Kidney Int 2018; 93: 231–44.
2017; 377: 644–57. 56 Wanner C, Lachin JM, Inzucchi SE, et al. Empagliflozin and clinical
37 Perkovic V, Zeeuw D, Mahaffey KW, et al. Canagliflozin and renal outcomes in patients with type 2 diabetes mellitus, established
outcomes in type 2 diabetes: results from the CANVAS Program cardiovascular disease, and chronic kidney disease. Circulation 2018;
randomised clinical trials. Lancet Diabetes Endocrinol 2018; 137: 119–29.
6: 691–704 . 57 Heerspink HJ, Desai M, Jardine M, Balis D, Meininger G,
38 Wiviott DS, Raz I, Bonaca MP et al. Dapagliflozin and Perkovic V. Canagliflozin slows progression of renal function
cardiovascular outcomes in type 2 diabetes. N Engl J Med 2018; decline independently of glycemic effects. J Am Soc Nephrol 2017;
published online DOI:1056/NEJMoa1812389. 28: 368–75.
39 Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and 58 Jardine MJ, Mahaffey KW, Neal B, et al. The Canagliflozin and
progression of kidney disease in type 2 diabetes. N Engl J Med 2016; Renal Endpoints in Diabetes with Established Nephropathy Clinical
375: 323–34. Evaluation (CREDENCE) study rationale, design, and baseline
40 Cherney DZI, Zinman B, Inzucchi SE, et al. Effects of characteristics. Am J Nephrol 2017; 46: 462–72.
empagliflozin on the urinary albumin-to-creatinine ratio in patients 59 Dekkers CCJ, Gansevoort RT, Heerspink HJL. New diabetes
with type 2 diabetes and established cardiovascular disease: therapies and diabetic kidney disease progression: the role of
an exploratory analysis from the EMPA-REG OUTCOME SGLT-2 inhibitors. Curr Diab Rep 2018; 18: 27.
randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 60 Boehringer Ingelheim and Lilly announce an academic collaboration
2017; 5: 610–21. with University of Oxford to investigate the effects of empagliflozin
41 Neuen BL, Ohkuma T, Neal B, et al. Cardiovascular and renal in people with chronic kidney disease. https://www.boehringer-
outcomes with canagliflozin according to baseline kidney function: ingelheim.com/EMPA-KIDNEY (accessed Aug 21, 2018).
data from the CANVAS Program. Circulation 2018; published online 61 Drucker DJ. Mechanisms of action and therapeutic application of
June 25. DOI:10.1161/CIRCULATIONAHA.118.035901. glucagon-like peptide-1. Cell Metab 2018; 27: 740–56.
42 Muskiet MHA, van Baar MJB, Scholtes RA, van Raalte DH. 62 Smits MM, Tonneijck L, Muskiet MH, Kramer MH, Cahen DL,
Renal outcomes in CVOTs: keep calm and carry on. van Raalte DH. Gastrointestinal actions of glucagon-like
Lancet Diabetes Endocrinol 2018; 6: 674–76. peptide-1-based therapies: glycaemic control beyond the pancreas.
43 Pessoa TD, Campos LC, Carraro-Lacroix L, Girardi AC, Malnic G. Diabetes Obes Metab 2016; 18: 224–35.
Functional role of glucose metabolism, osmotic stress, 63 Nauck MA, Meier JJ. The incretin effect in healthy individuals and
and sodium-glucose cotransporter isoform-mediated transport on those with type 2 diabetes: physiology, pathophysiology, and
Na+/H+ exchanger isoform 3 activity in the renal proximal tubule. response to therapeutic interventions. Lancet Diabetes Endocrinol
J Am Soc Nephrol 2014; 25: 2028–39. 2016; 4: 525–36.
44 Cherney DZ, Perkins BA, Soleymanlou N, et al. Renal 64 Defronzo RA. From the triumvirate to the ominous octet: a new
hemodynamic effect of sodium-glucose cotransporter 2 inhibition paradigm for the treatment of type 2 diabetes mellitus. Diabetes
in patients with type 1 diabetes mellitus. Circulation 2014; 2009; 58: 773–95.
129: 587–97. 65 Nauck MA, Sauerwald A, Ritzel R, Holst JJ, Schmiegel W. Influence
45 Wanner C, Heerspink HJL, Zinman B et al. Empagliflozin and of glucagon-like peptide 1 on fasting glycemia in type 2 diabetic
kidney function decline in patients with type 2 diabetes: A slope patients treated with insulin after sulfonylurea secondary failure.
analysis from the EMPA REG OUTCOME trial. J Am soc Nephrol Diabetes Care 1998; 21: 1925–31.
2018; 29: 2755–69. 66 Sun F, Chai S, Li L, et al. Effects of glucagon-like peptide-1
46 Holtkamp FA, de Zeeuw D, Thomas MC, et al. An acute fall in receptor agonists on weight loss in patients with type 2 diabetes:
estimated glomerular filtration rate during treatment with losartan a systematic review and network meta-analysis. J Diabetes Res 2015;
predicts a slower decrease in long-term renal function. Kidney Int 2015: 157201.
2011; 80: 282–87. 67 Aaboe K, Knop FK, Vilsboll T, et al. Twelve weeks treatment with
47 Mudaliar S, Alloju S, Henry RR. Can a shift in fuel energetics the DPP-4 inhibitor, sitagliptin, prevent s degradation of peptide YY
explain the beneficial cardiorenal outcomes in the and improves glucose and non-glucose induced insulin secretion in
EMPA-REG OUTCOME study? A unifying hypothesis. patients with type 2 diabetes mellitus. Diabetes Obes Metab 2010;
Diabetes Care 2016; 39: 1115–22. 12: 323–33.
14 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
Review
68 Sun F, Wu S, Guo S, et al. Impact of GLP-1 receptor agonists on 88 Cooper ME, Perkovic V, McGill JB, et al. Kidney disease end
blood pressure, heart rate and hypertension among patients with points in a pooled analysis of individual patient-level data from
type 2 diabetes: a systematic review and network meta-analysis. a large clinical trials program of the dipeptidyl peptidase 4
Diabetes Res Clin Pract 2015; 110: 26–37. inhibitor linagliptin in type 2 diabetes. Am J Kidney Dis 2015;
69 Muskiet MH, Smits MM, Morsink LM, Diamant M. The gut-renal 66: 441–49.
axis: do incretin-based agents confer renoprotection in diabetes? 89 Groop PH, Cooper ME, Perkovic V, Emser A, Woerle HJ,
Nat Rev Nephrol 2014; 10: 88–103. von Eynatten M. Linagliptin lowers albuminuria on top of
70 Skov J, Dejgaard A, Frokiaer J, et al. Glucagon-like peptide-1 recommended standard treatment in patients with type 2 diabetes
(GLP-1): effect on kidney hemodynamics and and renal dysfunction. Diabetes Care 2013; 36: 3460–68.
renin-angiotensin-aldosterone system in healthy men. 90 Groop PH, Cooper ME, Perkovic V, et al. Linagliptin and its effects
J Clin Endocrinol Metab 2013; 98: E664–71. on hyperglycaemia and albuminuria in patients with type 2 diabetes
71 Muskiet MH, Tonneijck L, Smits MM, et al. Acute renal and renal dysfunction: the randomized MARLINA-T2D trial.
haemodynamic effects of glucagon-like peptide-1 receptor agonist Diabetes Obes Metab 2017; 19: 1610–19.
exenatide in healthy overweight men. Diabetes Obes Metab 2016; 91 Mosenzon O, Leibowitz G, Bhatt DL, et al. Effect of saxagliptin on
18: 178–85. renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care 2017;
72 Skov J, Pedersen M, Holst JJ, et al. Short-term effects of liraglutide 40: 69–76.
on kidney function and vasoactive hormones in type 2 diabetes: 92 Green JB, Bethel MA, Armstrong PW, et al. Effect of sitagliptin on
a randomized clinical trial. Diabetes Obes Metab 2016; 18: 581–89. cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;
73 Tonneijck L, Muskiet MHA, Smits MM, et al. Postprandial renal 373: 232–42.
haemodynamic effect of lixisenatide vs once-daily insulin-glulisine 93 Gantz I, Chen M, Suryawanshi S, et al. A randomized, placebo-
in patients with type 2 diabetes on insulin-glargine: an 8-week, controlled study of the cardiovascular safety of the once-weekly
randomised, open-label trial. Diabetes Obes Metab 2017; 19: 1669–80. DPP-4 inhibitor omarigliptin in patients with type 2 diabetes
74 Tonneijck L, Smits MM, Muskiet MHA, et al. Acute renal effects of mellitus. Cardiovasc Diabetol 2017; 16:112.
the GLP-1 receptor agonist exenatide in overweight type 2 diabetes 94 Rosenstock J, Perkovic V, Johansen OE et al. Effect of linagliptin vs
patients: a randomised, double-blind, placebo-controlled trial. placebo on major cardiovascular events in adults with type 2
Diabetologia 2016; 59: 1412–21. diabetes and high cardiovascular and renal risk: the CARMELINA
75 Tonneijck L, Smits MM, Muskiet MH, et al. Renal effects of randomized clinical trial. JAMA 2018; published online Nov 9.
DPP-4 inhibitor sitagliptin or GLP-1 receptor agonist liraglutide in DOI:10.1001/jama.2018.18269.
overweight patients with type 2 diabetes: a 12-week, randomized, 95 Barton M, Yanagisawa M. Endothelin: 20 years from discovery to
double-blind, placebo-controlled trial. Diabetes Care 2016; therapy. Can J Physiol Pharmacol 2008; 86: 485–98.
39: 2042–50. 96 Kohan DE, Rossi NF, Inscho EW, Pollock DM. Regulation of blood
76 Lovshin JA, Rajasekeran H, Lytvyn Y, et al. Dipeptidyl peptidase 4 pressure and salt homeostasis by endothelin. Physiol Rev 2011;
inhibition stimulates distal tubular natriuresis and increases in 91: 1–77.
circulating SDF-1α¹-⁶⁷ in patients with type 2 diabetes. Diabetes Care 97 Stuart D, Chapman M, Rees S, Woodward S, Kohan DE.
2017; 40: 1073–81. Myocardial, smooth muscle, nephron, and collecting duct gene
77 Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for targeting reveals the organ sites of endothelin A receptor antagonist
weight loss among patients with type 2 diabetes: the SCALE fluid retention. J Pharmacol Exp Ther 2013; 346: 182–89.
diabetes randomized clinical trial. JAMA 2015; 314: 687–99. 98 Stuart D, Rees S, Woodward SK, Koesters R, Strait KA, Kohan DE.
78 Davies MJ, Bain SC, Atkin SL, et al. Efficacy and safety of Disruption of the endothelin A receptor in the nephron causes mild
liraglutide versus placebo as add-on to glucose-lowering therapy fluid volume expansion. BMC Nephrol 2012; 13: 166.
in patients with type 2 diabetes and moderate renal impairment 99 Kohan DE, Barton M. Endothelin and endothelin antagonists in
(LIRA-RENAL): a randomized clinical trial. Diabetes Care 2016; chronic kidney disease. Kidney Int 2014; 86: 896–904.
39: 222–30. 100 Saleh MA, Pollock JS, Pollock DM. Distinct actions of endothelin
79 von Scholten BJ, Persson F, Rosenlund S, et al. The effect of A-selective versus combined endothelin A/B receptor antagonists in
liraglutide on renal function: a randomized clinical trial. early diabetic kidney disease. J Pharmacol Exp Ther 2011;
Diabetes Obes Metab 2017; 19: 239–47. 338: 263–70.
80 Tuttle KR, McKinney TD, Davidson JA, Anglin G, Harper KD, 101 Dhaun N, Ferro CJ, Davenport AP, Haynes WG, Goddard J,
Botros FT. Effects of once-weekly dulaglutide on kidney function in Webb DJ. Haemodynamic and renal effects of endothelin receptor
patients with type 2 diabetes in phase II and III clinical trials. antagonism in patients with chronic kidney disease.
Diabetes Obes Metab 2017; 19: 436–41. Nephrol Dial Transplant 2007; 22: 3228–34.
81 Tuttle KR, Lakshmanan MC, Rayner B, et al. Dulaglutide versus 102 Dhaun N, Macintyre IM, Melville V, et al. Blood
insulin glargine in patients with type 2 diabetes and pressure-independent reduction in proteinuria and arterial stiffness
moderate-to-severe chronic kidney disease (AWARD-7): after acute endothelin-a receptor antagonism in chronic kidney
a multicentre, open-label, randomised trial. disease. Hypertension 2009; 54: 113–19.
Lancet Diabetes Endocrinol 2018; 6: 605–17. 103 Boels MG, Avramut MC, Koudijs A, et al. Atrasentan reduces
82 Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in patients with albuminuria by restoring the glomerular endothelial glycocalyx
type 2 diabetes and acute coronary syndrome. N Engl J Med 2015; barrier in diabetic nephropathy. Diabetes 2016; 65: 2429–39.
373: 2247–57. 104 Barton M, Tharaux PL. Endothelin and the podocyte. Clin Kidney J
83 Muskiet MHA, Tonneijck L, Huang Y, et al. Lixisenatide and renal 2012; 5: 17–27.
outcomes in patients with type 2 diabetes and acute coronary 105 Barton M, Shaw S, d’Uscio LV, Moreau P, Luscher TF.
syndrome: an exploratory analysis of the ELIXA randomised, Angiotensin II increases vascular and renal endothelin-1 and
placebo-controlled trial. Lancet Diabetes Endocrinol. 2018; 6: 859–69. functional endothelin converting enzyme activity in vivo: role of
84 Mann JFE, Orsted DD, Brown-Frandsen K, et al. Liraglutide ETA receptors for endothelin regulation.
and renal outcomes in type 2 diabetes. N Engl J Med 2017; Biochem Biophys Res Commun 1997; 238: 861–65.
377: 839–48. 106 Wenzel RR, Littke T, Kuranoff S, et al. Avosentan reduces albumin
85 Hernandez, AF, Green, JB, Janmohamed, S, et al. Albiglutide and excretion in diabetics with macroalbuminuria. J Am Soc Nephrol
cardiovascular outcomes in patients with type 2 diabetes and 2009; 20: 655–64.
cardiovascular disease (Harmony Outcomes): a double-blind, 107 de Zeeuw D, Coll B, Andress D, et al. The endothelin antagonist
randomised placebo-controlled trial. Lancet 2018; 392: 1519–29. atrasentan lowers residual albuminuria in patients with
86 Marso SP, Bain SC, Consoli A, et al. Semaglutide and type 2 diabetic nephropathy. J Am Soc Nephrol 2014; 25: 1083–93.
cardiovascular outcomes in patients with type 2 diabetes. 108 Heerspink HJL, Andress DL, Bakris G, et al. Rationale and protocol
N Engl J Med 2016; 375: 1834–44. of the study of diabetic nephropathy with atrasentan (SONAR)
87 Mann JFE, Orsted DD, Buse JB. Liraglutide and renal outcomes in trial: a clinical trial design novel to diabetic nephropathy.
type 2 diabetes. N Engl J Med 2017; 377: 2197–98. Diabetes Obes Metab 2018; 20: 1369–76.
www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8 15
Review
109 Epstein M. Aldosterone as a mediator of progressive renal disease: 119 Barfacker L, Kuhl A, Hillisch A, et al. Discovery of BAY 94-8862:
pathogenetic and clinical implications. Am J Kidney Dis 2001; a nonsteroidal antagonist of the mineralocorticoid receptor for the
37: 677–88. treatment of cardiorenal diseases. ChemMedChem 2012;
110 Messaoudi S, Azibani F, Delcayre C, Jaisser F. Aldosterone, 7: 1385–403.
mineralocorticoid receptor, and heart failure. Mol Cell Endocrinol 120 Bakris GL, Agarwal R, Chan JC, et al. Effect of finerenone on
2012; 350: 266–72. albuminuria in patients with diabetic nephropathy: a randomized
111 Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF. clinical trial. JAMA 2015; 314: 884–94.
Aldosterone antagonists for preventing the progression of chronic 121 Tuomi T, Santoro N, Caprio S, Cai M, Weng J, Groop L. The many
kidney disease. Cochrane Database Syst Rev 2014; 4: CD007004. faces of diabetes: a disease with increasing heterogeneity. Lancet
112 Chrysostomou A, Becker G. Spironolactone in addition to ACE 2014; 383: 1084–94.
inhibition to reduce proteinuria in patients with chronic renal 122 de Zeeuw D, Heerspink HJL, Jardine M, Perkovic V. Renal trials in
disease. N Engl J Med 2001; 345: 925–26. diabetes need a platform: time for a global approach?
113 Epstein M, Williams GH, Weinberger M, et al. Selective aldosterone Lancet Diabetes Endocrinol 2018; 6: 356–58.
blockade with eplerenone reduces albuminuria in patients with 123 van Baar MJB, van Ruiten CC, Muskiet MHA, van Bloemendaal L,
type 2 diabetes. Clin J Am Soc Nephrol 2006; 1: 940–51. IJzerman van RG, Raalte DH. SGLT2 inhibitors in combination
114 Morales E, Millet VG, Rojas-Rivera J, et al. Renoprotective effects of therapy: from mechanisms to clinical considerations in type 2
mineralocorticoid receptor blockers in patients with proteinuric diabetes management. Diabetes Care 2018; 41: 1543–56.
kidney diseases. Nephrol Dial Transplant 2013; 28: 405–12. 124 Frias JP, Guja C, Hardy E, et al. Exenatide once weekly plus
115 Lazich I, Bakris GL. Prediction and management of hyperkalemia dapagliflozin once daily versus exenatide or dapagliflozin alone in
across the spectrum of chronic kidney disease. Semin Nephrol 2014; patients with type 2 diabetes inadequately controlled with
34: 333–39. metformin monotherapy (DURATION-8): a 28 week, multicentre,
116 Bomback AS, Kshirsagar AV, Amamoo MA, Klemmer PJ. Change double-blind, phase 3, randomised controlled trial.
in proteinuria after adding aldosterone blockers to ACE inhibitors Lancet Diabetes Endocrinol 2016; 4: 1004–16.
or angiotensin receptor blockers in CKD: a systematic review. 125 Ludvik B, Frias JP, Tinahones FJ, et al. Dulaglutide as add-on
Am J Kidney Dis 2008; 51: 199–211. therapy to SGLT2 inhibitors in patients with inadequately controlled
117 Roscioni SS, de Zeeuw D, Bakker SJ, Lambers Heerspink HJ. type 2 diabetes (AWARD-10): a 24-week, randomised, double-blind,
Management of hyperkalaemia consequent to placebo-controlled trial. Lancet Diabetes Endocrinol 2018; 6: 370–81.
mineralocorticoid-receptor antagonist therapy. Nat Rev Nephrol
2012; 8: 691–99. © 2018 Elsevier Ltd. All rights reserved.
118 Kolkhof P, Borden SA. Molecular pharmacology of the
mineralocorticoid receptor: prospects for novel therapeutics.
Mol Cell Endocrinol 2012; 350: 310–17.
16 www.thelancet.com/diabetes-endocrinology Published online December 19, 2018 http://dx.doi.org/10.1016/S2213-8587(18)30263-8
You might also like
- KeNotes 2017 PDFDocument106 pagesKeNotes 2017 PDFDENTAL REVIEWER ONLY100% (3)
- Wilm's Tumor Pa Tho PhysiologyDocument1 pageWilm's Tumor Pa Tho Physiologya_yeLNo ratings yet
- Aaaq2 2015 Ir PresentationDocument45 pagesAaaq2 2015 Ir PresentationguerrezNo ratings yet
- The Duke Heart Failure ProgramDocument10 pagesThe Duke Heart Failure ProgramAnonymous PbAQxgw0No ratings yet
- 2012 Illinois Rules of The Road Review Course WorkbookDocument36 pages2012 Illinois Rules of The Road Review Course WorkbookmudkipzzzNo ratings yet
- OnQ Broadcast Intercom System ManualDocument2 pagesOnQ Broadcast Intercom System ManualJohn PallissardNo ratings yet
- Diabetes Conversation Maps: Journey To Better Diabetes EducationDocument1 pageDiabetes Conversation Maps: Journey To Better Diabetes EducationCenter for Managing Chronic DiseaseNo ratings yet
- IV Drug CompDocument5 pagesIV Drug CompWil Lester100% (1)
- Supportive & Preventive Medicine PDFDocument29 pagesSupportive & Preventive Medicine PDFhuong L100% (1)
- Daftar Nutrisi PERKECILDocument6 pagesDaftar Nutrisi PERKECILellya theresiaNo ratings yet
- 1117 FullDocument29 pages1117 FullElizabeth IB100% (1)
- Cardiovascular Outcomes Trials in Type 2 DiabetesDocument51 pagesCardiovascular Outcomes Trials in Type 2 Diabetes와라송이100% (1)
- Kathrine O Neal PP PDFDocument92 pagesKathrine O Neal PP PDFrezqNo ratings yet
- 1183 - The Global Burden of Heart Failure. - Martin COWIE (London, United Kingdom)Document21 pages1183 - The Global Burden of Heart Failure. - Martin COWIE (London, United Kingdom)Mulyani EdwarNo ratings yet
- A Randomized, Double-Blind, Controlled Trial Comparing Rifaximin Plus Lactulose With Lactulose Alone in Treatment of Overt Hepatic EncephalopathyDocument3 pagesA Randomized, Double-Blind, Controlled Trial Comparing Rifaximin Plus Lactulose With Lactulose Alone in Treatment of Overt Hepatic EncephalopathyYunita DNo ratings yet
- Dapa Brief Data (14271)Document24 pagesDapa Brief Data (14271)Adel SALLAM100% (1)
- 2002 GAO PDMP StudyDocument27 pages2002 GAO PDMP StudyKOMU NewsNo ratings yet
- Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy CREDENCE TrialDocument29 pagesCanagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy CREDENCE Trialgokulam0075028No ratings yet
- THURSDAY Salisbury AfsharDocument39 pagesTHURSDAY Salisbury AfsharNational Press Foundation100% (1)
- AIIMS June 2020 DR Siraj Ahmad PDFDocument4 pagesAIIMS June 2020 DR Siraj Ahmad PDFadiNo ratings yet
- SGLT 2 Inhibitors: Newer Paradigms in The Treatment of Heart Failure With Reduced Ejection FractionDocument4 pagesSGLT 2 Inhibitors: Newer Paradigms in The Treatment of Heart Failure With Reduced Ejection FractionIJAR JOURNALNo ratings yet
- Pharmacy PresentationDocument93 pagesPharmacy PresentationAira Abella100% (1)
- World Preview 2016 Outlook To 2022Document49 pagesWorld Preview 2016 Outlook To 2022Willy Pérez-Barreto MaturanaNo ratings yet
- Beyond Use DateDocument56 pagesBeyond Use DateDa Chan100% (1)
- ACC Handbook Ascvd Type 2 Diabetes: On andDocument10 pagesACC Handbook Ascvd Type 2 Diabetes: On andZH. omg sarNo ratings yet
- Pratley New Treatments For Type 2 DiabetesDocument85 pagesPratley New Treatments For Type 2 DiabetesMia DangaNo ratings yet
- Vanco & Ag PK 2018Document35 pagesVanco & Ag PK 2018Nguyen GeenNo ratings yet
- Aon Profile 2020Document16 pagesAon Profile 2020phanapa100% (1)
- SGLT 2 InhibitorDocument5 pagesSGLT 2 InhibitorAlimWijayaNo ratings yet
- PA 644 - M2 LecturesDocument735 pagesPA 644 - M2 LectureskatNo ratings yet
- The Filter, The Pump and The FilterDocument35 pagesThe Filter, The Pump and The FilterRenal Association MauritiusNo ratings yet
- AsdfgjkDocument14 pagesAsdfgjkMaria Frances Antoniette PerezNo ratings yet
- Slides Outcomes of Sglt2i in Diabetic Kidney Disease Is It All DiabetesDocument29 pagesSlides Outcomes of Sglt2i in Diabetic Kidney Disease Is It All DiabetesVaibhav DafaleNo ratings yet
- A Speech On PunctualityDocument2 pagesA Speech On PunctualityRrhayshelle Ahnne0% (1)
- HF2019Document24 pagesHF2019Sima Noviantika100% (2)
- New Pathways in Heart Failure TreatmentDocument34 pagesNew Pathways in Heart Failure TreatmentSwapnaNo ratings yet
- Journal Reading EMPEROR-ReducedDocument21 pagesJournal Reading EMPEROR-ReducedLolii Con Harhazyuku100% (1)
- Controlled Substances LawsDocument8 pagesControlled Substances LawsJames Lindon100% (1)
- Ultimate Reference DocumentDocument29 pagesUltimate Reference DocumentShellyza Moledina SajwaniNo ratings yet
- Illinois Pilot Program Act RoadmapDocument19 pagesIllinois Pilot Program Act RoadmapMPPNo ratings yet
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- SC PH 00389 - TRAJENTA Module 2020 1QDocument107 pagesSC PH 00389 - TRAJENTA Module 2020 1QJenny Calapati TorrijosNo ratings yet
- Introduction, Medicines Classification and Standard Operating ProceduresDocument14 pagesIntroduction, Medicines Classification and Standard Operating ProceduresAnkur SinghNo ratings yet
- AstraZeneca AR 2018 PDFDocument248 pagesAstraZeneca AR 2018 PDFChristian nelNo ratings yet
- Empagliflozin in Heart Failure With A Preserved Ejection FractionDocument11 pagesEmpagliflozin in Heart Failure With A Preserved Ejection Fractionsri wahyuniNo ratings yet
- Matching ActivityDocument26 pagesMatching Activityapi-661456802No ratings yet
- 02-05 2022 Pharm Pharmacokinetics 2022 R3Document38 pages02-05 2022 Pharm Pharmacokinetics 2022 R3Amira HelayelNo ratings yet
- Allaergic Conjunctivitis PathophysiologyDocument25 pagesAllaergic Conjunctivitis PathophysiologyRabiu Hassan MusaNo ratings yet
- Sharkbite® Metal Push-Fit Plumbing Solution: Technical InformationDocument36 pagesSharkbite® Metal Push-Fit Plumbing Solution: Technical InformationPubcrawlNo ratings yet
- CV 2021Document5 pagesCV 2021api-611973258No ratings yet
- Pharmacotherapy of DMDocument23 pagesPharmacotherapy of DMsalinaNo ratings yet
- Pearsonvue Exam of Pharmacy: - CasesDocument114 pagesPearsonvue Exam of Pharmacy: - Caseslina magdiNo ratings yet
- p2019b1 Sample PDFDocument22 pagesp2019b1 Sample PDFMaria PerezNo ratings yet
- All Types of InsulinDocument18 pagesAll Types of Insulinali mohammedNo ratings yet
- Peptic Ulcer DiseaseDocument41 pagesPeptic Ulcer DiseaseNneka Uchenna UkweNo ratings yet
- PharDose Chapter 1Document4 pagesPharDose Chapter 1Angelyka CabaloNo ratings yet
- Fellowship in DiabetesDocument2 pagesFellowship in DiabetesBenjamin NelsonNo ratings yet
- SPIRIVA HandiHaler InstructionsDocument9 pagesSPIRIVA HandiHaler InstructionssamyvnNo ratings yet
- CA Sitagliptin Vs Glipizide 1.1Document29 pagesCA Sitagliptin Vs Glipizide 1.1lordizzatNo ratings yet
- 8-22-16-Lecture Grand Rounds Drug Drug Interactions PDFDocument44 pages8-22-16-Lecture Grand Rounds Drug Drug Interactions PDFCastov Liubița100% (1)
- 3 Calculations PDFDocument31 pages3 Calculations PDFMisha Ptpm100% (1)
- A Narrative Review of New Treatment Options For Chronic Kidney Disease in Type 2 DiabetesDocument7 pagesA Narrative Review of New Treatment Options For Chronic Kidney Disease in Type 2 Diabetesjhoanna andrea portillaNo ratings yet
- Temporal Improvement of A COVID 19 Positive.31Document1 pageTemporal Improvement of A COVID 19 Positive.31ellya theresiaNo ratings yet
- 4 Prof. EAD Microbiome MAACI 2 19 JuniDocument25 pages4 Prof. EAD Microbiome MAACI 2 19 Juniellya theresiaNo ratings yet
- Jejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of LiteratureDocument6 pagesJejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of Literatureellya theresiaNo ratings yet
- Gastrointestinal Bleeding in Patients With Severe Sars-Cov-2Document3 pagesGastrointestinal Bleeding in Patients With Severe Sars-Cov-2ellya theresiaNo ratings yet
- Emerging Treatments For Crohn's Disease: Cells, Surgery, and Novel TherapeuticsDocument10 pagesEmerging Treatments For Crohn's Disease: Cells, Surgery, and Novel Therapeuticsellya theresiaNo ratings yet
- Peritoneal DialysisDocument17 pagesPeritoneal Dialysisellya theresiaNo ratings yet
- MR c1 Gastropati DMDocument27 pagesMR c1 Gastropati DMellya theresiaNo ratings yet
- Development of Treatment: How Do We Manage Antimicrobial Resistance?Document22 pagesDevelopment of Treatment: How Do We Manage Antimicrobial Resistance?ellya theresiaNo ratings yet
- Aki Rifle - Google SearchDocument1 pageAki Rifle - Google Searchellya theresiaNo ratings yet
- 6 PDFDocument2 pages6 PDFellya theresiaNo ratings yet
- WJG 25 5097Document9 pagesWJG 25 5097ellya theresiaNo ratings yet
- 01 Renal ModuleDocument71 pages01 Renal ModuleFatima AbduljalilNo ratings yet
- Newborn Physiology PathologyDocument99 pagesNewborn Physiology Pathologythev0206100% (1)
- PhysioEx Ex. 9 Act. 3Document4 pagesPhysioEx Ex. 9 Act. 3Juvy Anne LozanoNo ratings yet
- Chapter 26 Urinary SystemDocument17 pagesChapter 26 Urinary SystemAmy Lalringhluani100% (1)
- System UriDocument48 pagesSystem UriStef FieNo ratings yet
- Urinary System PDFDocument27 pagesUrinary System PDFfiona100% (3)
- General Biology G11 WK13-16 A. TobiasDocument31 pagesGeneral Biology G11 WK13-16 A. TobiasKristine SantosNo ratings yet
- 13.3 Excretion in Humans IGCSE CIE Biology Ext Theory MS - LDocument7 pages13.3 Excretion in Humans IGCSE CIE Biology Ext Theory MS - LTaelo MasuNo ratings yet
- Excretion by Rakshita SinghDocument37 pagesExcretion by Rakshita SinghPurplet 7No ratings yet
- COMPLETE CS - Acute PyelonephritisDocument53 pagesCOMPLETE CS - Acute Pyelonephritisyasira100% (1)
- Excretory SystemDocument15 pagesExcretory Systemlaptop lenovoNo ratings yet
- Urinary SystemDocument28 pagesUrinary Systemgabanule brandonNo ratings yet
- Body Fluids & ElectrolytesDocument26 pagesBody Fluids & ElectrolytesMohamad Zekry Zuhairy100% (1)
- NTRUHS 2k20 Batch Final PapersDocument24 pagesNTRUHS 2k20 Batch Final PapersLakshmidevi GaletiNo ratings yet
- PathoPhysiology of Renal Failure OverviewDocument7 pagesPathoPhysiology of Renal Failure Overviewnursing concept maps100% (1)
- RFT - Organ Function TestDocument28 pagesRFT - Organ Function TestRishita ChoubeyNo ratings yet
- Bolesti BubregaDocument6 pagesBolesti Bubregamedicinar85No ratings yet
- Histo NotesDocument19 pagesHisto Notesanas ishaqNo ratings yet
- Chapter 6 CMDocument14 pagesChapter 6 CMLeilani SablanNo ratings yet
- Csec HSB January 2011 p2Document19 pagesCsec HSB January 2011 p2Sachin Bahadoorsingh100% (1)
- Clinical Pharmacology and Forensic ToxicologyDocument107 pagesClinical Pharmacology and Forensic ToxicologySunilNo ratings yet
- Anatomi Fisiologi Sistem PerkemihanDocument65 pagesAnatomi Fisiologi Sistem PerkemihanMakkatul HikmahNo ratings yet
- Chapter 6 - Body Fluids, Water-Salt Balance RP1 PDFDocument77 pagesChapter 6 - Body Fluids, Water-Salt Balance RP1 PDFpizzaNo ratings yet
- A Level Biology NotesDocument6 pagesA Level Biology NotesMira AluedeNo ratings yet
- Acid-Base Disorders Fluid and ElectrolytesDocument13 pagesAcid-Base Disorders Fluid and ElectrolytesNicole BiduaNo ratings yet
- Pex 09 04Document4 pagesPex 09 04chaira nisaaNo ratings yet
- Artículo 2 - Fisiopatología de La PielonefritisDocument17 pagesArtículo 2 - Fisiopatología de La PielonefritisCAROLINA CHUMACERO BERMEONo ratings yet
- كتاب اسئلة جميلDocument401 pagesكتاب اسئلة جميلMohammadSAL-Rawashdeh100% (1)