Professional Documents
Culture Documents
Effectiveness of Using Ursodeoxycholic Acid in Reducing Incidence of Gallstone Formation After Sleeve Gastrectomy
Effectiveness of Using Ursodeoxycholic Acid in Reducing Incidence of Gallstone Formation After Sleeve Gastrectomy
Uploaded by
vivianmtOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effectiveness of Using Ursodeoxycholic Acid in Reducing Incidence of Gallstone Formation After Sleeve Gastrectomy
Effectiveness of Using Ursodeoxycholic Acid in Reducing Incidence of Gallstone Formation After Sleeve Gastrectomy
Uploaded by
vivianmtCopyright:
Available Formats
International Surgery Journal
El Shenawy MSI et al. Int Surg J. 2019 Feb;6(2):403-408
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20185506
Original Research Article
Effectiveness of using ursodeoxycholic acid in reducing incidence of
gallstone formation after sleeve gastrectomy
Mahmoud Saad Ibrahim El Shenawy*, Mohamed Sabry Ammar,
Mahmoud Gamal Eldin Hagag
Department of General Surgery, Faculty of Medicine, Menoufia University, Menoufia, Egypt
Received: 11 December 2018
Revised: 20 December 2018
Accepted: 24 December 2018
*Correspondence:
Dr. Mahmoud Saad Ibrahim El Shenawy,
E-mail: drmahmoud394@yahoo.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Obese persons are at risk for cholesterol gallstones because of high saturation of cholesterol in their
bile. About 75% of gallstones are of cholesterol type. To reduce the risk for gallstone formation, policies of
prophylactic cholecystectomy are proposed. However, this is not widely accepted. A routine cholecystectomy during
bariatric surgery is recommended by some centers. Ursodeoxycholic acid enhances the conversion of cholesterol to
bile acids. It also enhances cholesterol transport as liquid crystals. Furthermore, it has an inhibitory action on the
prostaglandins and biliary glycoprotein, which is the possible explanation for its action on decreasing the saturation
index. The objective was the effectiveness of using Ursodeoxycholic Acid (UDCA) in reducing incidence of gallstone
formation after sleeve gastrectomy.
Methods: 50 morbid obese patients divided into 2 groups. Group A: 30 patients who received UDCA post-operative.
(5 male and 25 female) with mean age 34.8year. Patients had a body mass index (BMI) with mean BMI 46.9kg/m2.
Group B: 20 patients without receiving UDCA post-operative. (2 male and 18 female) with mean age 32.9year.
Patients had a mean of BMI 47.3kg/m2.
Results: Using UDCA has significant role in prophylaxis against development of gall stone formation. Patients who
received UDCA developed gall stones by a percentage 0% (0/30) while patients who hadn’t received UDCA
developed gall stones by a percentage 4.7% (3/20).
Conclusions: The use of UCDA effectively reduced the incidence of gall stone formation after laparoscopic sleeve
gastrectomy (LSG) in patient with morbid obesity.
Keywords: Gallstone formation, Morbid obesity, Sleeve gastrectomy, Ursodeoxycholic acid
INTRODUCTION bariatric surgery up to 6-8%.2 Obese persons are at risk
for cholesterol gallstones because of high saturation of
Obesity is now epidemic in the United States affecting cholesterol in their bile. About 75% of gallstones are of
more than 60million people, and the problem will worsen cholesterol type. The risk increases during rapid weight
in coming years as the incidence of childhood and loss using low-calorie diets and after bariatric surgery.
adolescent obesity rises.1 In the general population the The mechanism for gallstone formation during rapid
risk of cholelithiasis is 10-20%, compared with post- weight loss is not completely understood, several
bariatric patients where it is increased to 30-53% the mechanisms have been suggested including increased bile
overall prevalence of cholecystectomy in the general cholesterol saturation and gall bladder stasis, increased
population is 1-5%, which is slightly increased after secretion of mucin and calcium, and increased
International Surgery Journal | February 2019 | Vol 6 | Issue 2 Page 403
El-Shenawy MSI et al. Int Surg J. 2019 Feb;6(2):403-408
prostaglandins.3 Multiple approaches have been proposed Methods
and studied to prevent gall-stones after weight loss
surgery including concomitant cholecystectomy and • Clinical evaluation
prophylactic ursodeoxycholic acid (UDCA) treatment • Investigation
following surgery.4 The aim of this study is to define • Pre-operative preparation
effectiveness of the using of the ursodeoxycholic acid in • Pelvis-Abdominal Ultrasound pre-operative to
reducing incidence of gallstone formation after sleeve exclude existing gall stone or removed gall bladder.
gastrectomy operation.
Patients preparation
METHODS
All patients fasted for at least 8hours before performing
This prospective study had been conducted to patients abdominal ultra sound examination for regular checkup
admitted at General Surgery Department in Menoufia unless they develop symptoms like nausea, vomiting and
University Hospital. All patients admitted for Sleeve abdominal pain. Then, all data were statistically analyzed.
Gastrectomy Operation at General Surgery Department.
Eligible patients were between 20 and 60years of age and RESULTS
had a BMI of at least 40kg/m2 or BMI of at least 35kg/m2
with Co-Morbidity were included and the patients with This study had been conducted on 50 morbidly obese
history of cholecystectomy, presence of gallstones or patients and divided into 2 groups:
pregnancy were excluded.
• Group A includes 30 morbid obese patients who
Informed consent was obtained from each patient before received Ursodeoxycholic Acid (UDCA) post-
initiation of the study and hospital ethical committee operative for 6months.
approval was obtained for the protocol of the study. All • Group B includes 20 morbid obese patients without
patients were subjected to receiving Ursodeoxycholic Acid (UDCA) post-
operative.
• History taking: personal history, complain, history
of present illness, past history, family history. Then patients were grouped according to age, sex, body
• Full clinical evaluation mass index, initial body weight, percentage of weight
• Investigations. loss, presentation of gall stones. All procedures were
performed laparoscopically without conversions and no
Clinical evaluation: aimed at assessment of degree of mortalities.
obesity, preoperative clinical evaluation and detection of
different complications of morbid obesity (like In this study the mean age of group A was 34.8years with
hypertension, skeletal problems, diabetes, joint disease, ±SD 12.3years, minimum 20years and maximum 59years
obstructive sleep apnea and restrictive lung disease). and the mean age of group B was 32.9year with ±SD
10.8-years, minimum 20years and maximum 58years.
Investigations The P value of age was 0.594 which was insignificant
and indicates that age has no role in gall stones formation
• Laboratory investigations: CBC, FBS, renal after sleeve Gastrectomy.
functions, liver functions, coagulation profile and
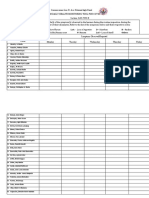
HbA1C for diabetic patients. Table 1: The age distribution of group A and group B.
• Abdomino-pelvic ultrasonography.
• Pulmonary evaluation: including chest X-ray and Group A Group B
pulmonary functions tests. (n-30) (n-20)
Age T-test P-value
• Cardiac assessment: ECG and echocardiography. (case (control
group) group)
Author divided patients randomly into two groups which Mean 34.8years 32.9 years 0.545 0.594(NS)
was group 1 includes 30 morbid obese patients underwent SD 12.3years 10.8 years
(LSG) laparoscopic sleeve gastrectomy with Min 20years 20years
postoperative prophylaxis using Ursodeoxycholic Acid Max 59years 58years
(UDCA) and group 2 includes 20 morbid obese patients
underwent LSG without postoperative prophylaxis using In this study, the sex of group A (n-30) 5 (16.66%) male
Ursodeoxycholic Acid (UDCA). patient and 25 (83.33%) female patient and group B (n-
20) 2 (10%) male patient and 18 (90%) female patient.
Treatments initiated 15days after surgery and continued The P value of sex was 0.51 which was insignificant and
for 6months or until gallstone development. Patients indicates that gender has no role in increasing risk of
agreed to take the trial medication for 6months or until development of gall stones. In this study, the mean BMI
gallstones developed. Medication compliance was of group A was 46.9kg/m2 with ±SD 4.3kg/m2, minimum
monitored at every visit.
International Surgery Journal | February 2019 | Vol 6 | Issue 2 Page 404
El-Shenawy MSI et al. Int Surg J. 2019 Feb;6(2):403-408
38kg/m2 and maximum 57kg/m2 and the mean BMI of patients free and 8 patients have joint disease in group B
group A was 47.3kg/m2 with ±SD 3.6kg/m2, minimum 37 (n-20) and 12 patients free. 4 patients have obstructive
kg/m2 and maximum 59kg/m2. sleep apnea in group A (n-30) and 26 patients free and 3
patients have obstructive sleep apnea in group B (n-20)
Table 2: The sex distribution of group A and group B. and 17 patients free. 5 patients have restrictive lung
disease in group A (n-30) and 25 patients free and 4
Sex Group A Group B Chi P-value patients have restrictive lung disease in group B (n-20)
Male 5 2 0.51 and 16 patients free.
0.44
Female 25 18 (NS)
The p value of this study of diabetes was 0.59 which was
The p value of BMI was 0.732 which was insignificant insignificant. The p value of this study of hypertension
and indicates that BMI has no role in increasing risk of was 0.236 which was insignificant. The p value of this
development of gall stones. In this study, the mean study of joint disease was 0.201 which was insignificant.
weight of group A was 134.9kg with ±SD 14.4kg, The p value of this study of obstructive sleep apnea was
minimum 103.5kg and maximum 171kg and the mean 0.868 which was insignificant. The p value of this study
weight of group A was 131kg with ±SD 13.1kg, of restrictive lung disease was 0.764 which was
minimum 112.5kg and maximum 171kg. The p value of insignificant.
weight was 0.26 which was insignificant and indicates
that initial weight has no role in increasing risk of Table 5: The height of group A and group B.
development of gall stones.
Height Group A Group B T-test P-value
Table 3: The BMI distribution of group A and Mean 170.9cm 167cm 1.36 0.194
group B. SD 10.4cm 9.8cm
MIN 150cm 150cm
BMI Group A Group B T-test P-value MAX 190cm 185cm
Mean 46.9kg/m2 47.3 kg/m2 0.361 0.732(NS)
SD 4.3 kg/m2 3.6 kg/m2 Table 6: The excess body weight distribution of group
Min 38 kg/m2 37 kg/m2 A and group B.
Max 57 kg/m2 59 kg/m2
Excess body
Group A Group B T-test P-value
In this study, the mean height of group A was 170.9cm weight
with ±SD 10.4cm, minimum 150cm and maximum Mean 66.7kg 65.4kg 0.39 0.69(NS)
190cm and the mean height of group B was 167cm with SD 10.7kg 11.3kg
SD. 9.8cm, minimum 150cm and maximum 185cm. The MIN 45kg 46kg
p value of height was 0.194 which was insignificant and MAX 86kg 86kg
indicates that the height has no role increasing risk of
development of gall stones. In this study the mean excess Table 7: The comorbidity distribution of group A
body weight of group A was 66.7kg with ±SD 10.7kg, and group B.
minimum 45kg and maximum 86kg and the mean excess
body weight of group B was 65.4kg with ±SD 11.3kg, Comorbidity Group A Group B chi P-value
minimum 46kg and maximum 86kg. The p value of Yes No Yes No
excess body weight was 0.69 which was insignificant and Diabetes 7 23 6 14 0.277 0.59 (NS)
indicates that excess body weight has no role in Hypertension 6 24 7 13 1.403 0.236 (NS)
increasing risk of development of gall stone.
Joint disease 8 22 8 12 1.638 0.201 (NS)
Obstructive
Table 4: The weight of group A and group B. 4 26 3 17 0.028 0.868 (NS)
sleep apnoea
Weight Group A Group B T-test P-value Restrictive
5 25 4 16 0.090 0.764 (NS)
lung disease
Mean 134.9kg 131kg 1.17 0.26(NS)
SD 14.4kg 13.1kg
The results had been found insignificant according to
Min 103.5kg 112.5kg
diabetes, hypertension, joint disease, obstructive sleep
Max 171kg 171kg
apnea and restrictive lung disease in this study and
indicate that diabetes, hypertension, joint disease,
In this study, diabetes in group A (n-30) 7 diabetic patient obstructive sleep apnea and restrictive lung disease have
and 23 patients free and in group B (n-20) 6 diabetic no role in increasing risk of gall stones formation after
patient and 14 patients free. 6 patients hypertensive in sleeve gastrectomy. In this study, the mean of the excess
group A (n-30) and 24 patients free and 7 patient body weight loss after one year of group A was 75.7%
hypertensives in group B (n-20) and 13 patients free. 8 with ±SD 9.8%, minimum 50% and maximum 90%.
patients have joint disease in group A (n-30) and 22
International Surgery Journal | February 2019 | Vol 6 | Issue 2 Page 405
El-Shenawy MSI et al. Int Surg J. 2019 Feb;6(2):403-408
Table 8: The comorbidity distribution of group A distribution of group A and group B were 0.216 which
and group B. was insignificant and indicates that the incidence of
symptomatic gall stone distribution of group A and group
Weight loss after B has no role in increasing risk of development of gall
1 year as % of Group Group T- stones formation after sleeve gastrectomy.
P-value
excess body A B test
weight DISCUSSION
Mean 75.7% 73.3% 1.51 0.15(NS)
SD 9.8% 7.8% Sleeve gastrectomy operation effective in providing
Min 50% 55% weight loss of large magnitude, correction of co-
Max 90% 95% morbidities, decreasing overall mortality and providing a
marked survival advantage. Development of gall stones
Table 9: The using of UDCA for 6months and the post sleeve gastrectomy operation became very common
incidence of gall stone formation for one year and many studies are done in order to discuss causes and
follow up. prophylaxis against its development.5
Gall stone Group A Group B Chi P-value Lithogenesis was modified following Laparoscopic
with withou Sleeve Gastrectomy Operation (LSG). Post bariatric
using t using modifications include cholesterol hyper-saturation of bile
UDCA UDCA (through cholesterol mobilization from fatty tissues
(n-30) (n-20) enhancing cholesterol crystallization, decreased secretion
+ve Gall stone of biliary acids (caloric restriction), increased mucin
0 3 4.787 0.029 (S) production (enhancing crystallization) and last,
formation
gallbladder hypo-motility (secondary to decreased
-ve Gall stone
30 17 cholecystokinin secretion related to the hypo-caloric diet,
Formation
or obesity related resistance to cholecystokinin, to
gastroduodenal exclusion, or due to intraoperative injury
Table 10: The incidence of symptomatic gall stone to the hepatic branches of the vagus nerves.6
distribution of group A and group B.
A prospective study, on 1398 patients with morbid
Symptomatic Group Group Chi P-value obesity found that around 8% of patients developed
gall stone A B
cholelithiasis (CL) and required cholecystectomy during
Yes 0 1 1.531 0.216 (NS) the first 6months after the primary bariatric procedure. 7
No 30 19 Based on the findings of several reports implying the
formation of gallstones after different bariatric
The mean of the excess body weight loss after one year procedures, the guidelines for perioperative nutritional,
of group B was 73.3% with ±SD 7.8%, minimum 55% metabolic, nonsurgical support of the bariatric surgery
and maximum 95%. The p value of the excess body patient. Now, recommended an ultrasound examination
weight loss after one year was 0.15 which was within the first 6months as a routine examination after
insignificant and indicates that the excess body weight bariatric surgery for the detection of gallstones.8
loss after one year has no role in increasing risk of
development of gall stones. In this study, the using of An estimated 10-25% of patients who lose weight
UDCA and the incidence of gall stone formation for one through very low-calorie dieting develop CL. In mal-
year follow up of group A (n-30) no patient has positive absorptive procedures, such as RYGB, CL develops due
gall stone formation. Group B (n-20) 3 (15%) have to changes in the composition of bile, with increases in
positive gall stone formation and 17 (85%) patient have the calcium and mucin contents leading to the formation
negative gall stone formation. of supersaturated or lithogenic bile that crystalizes,
deposits and eventually forms cholesterol gallstone.9
The p value of the using of UDCA and the incidence of
gall stone formation for one year follow up was 0.029 However, since LSG is a purely restrictive procedure
which was significant and indicate that UDCA has role in with an intact bowel transit and entero-endocrine system,
prophylaxis against development of gall stones formation the details of mechanism of CL development after SG
after sleeve gastrectomy. In this study, the incidence of remain unclear. It was assumed that the division of the
symptomatic gall stone formation for one year follow up lesser omentum during bariatric procedures may cause
of group A (n-30) no patient has develop symptoms like inadvertent injury to hepatic branch of the left vagus
nausea, vomiting and abdominal pain. Group B (n-20) 1 nerve, which controls the gallbladder motility.10 Motility
(5%) have develop symptoms like nausea, vomiting and dysfunction can thus supervene, resulting in stasis of bile
abdominal pain and 19 (95%) patient have negative and subsequently CL. Gallstone that form after LSG can
symptomatic gall stone formation. The p value of this remain asymptomatic and become detected only during
study of the incidence of symptomatic gall stone abdominal ultrasonography or they can present clinically
International Surgery Journal | February 2019 | Vol 6 | Issue 2 Page 406
El-Shenawy MSI et al. Int Surg J. 2019 Feb;6(2):403-408
with the classic symptoms of LC or even with 12months, 3% versus 22%, and 8% versus 30% at
complications as obstructive jaundice or pancreatitis.11 24months, cholecystectomy in 4.7% versus 12%,
respectively.15 It is also concordant with Abdallah E et al,
Reported that LSG and RYGB had comparable who conducted a study on a total of 406 patients (124
incidences of symptomatic and complicated gallstone males, 282 females) with a mean age of 32.1±9.4years
disease. Efforts have been made to prevent the formation were included. The mean baseline body mass index
of gallstone after bariatric procedures. Concomitant (BMI) was 50.1±8.3kg/m2.
cholecystectomy has been proposed but the added
morbidities as well as the prolongation of the operation Patients were subdivided into two groups which was
time and hospital stay have rendered this option group I, which did not receive prophylactic treatment
controversial.12 Found that concomitant cholecystectomy with UCDA after LSG and group II, which received
prolonged the operation time of LSG and resulted in UCDA therapy for 6months after LSG. Group I
unnecessary complication such as bile leakage. comprised 159 patients, and group II comprised 247
Prophylactic cholecystectomy with bariatric surgery patients. The two groups showed comparable
appeared to be an unnecessary procedure that should be demographics, % excess weight loss (EWL) and decrease
applied only in the presence of symptomatic gallstone as in BMI at 6 and 12months after LSG. Eight patients (5%)
advocated.13 developed CL in group I, whereas no patients in group II
did (P=0.0005).17
The use of UDCA has been advocated as prophylactic
measure against postoperative CL. The UDCA acts by Funding: No funding sources
inhibiting cholesterol secretion in bile, thereby preventing Conflict of interest: None declared
the super saturation of bile and cholesterol stone Ethical approval: The study was approved by the
formation.14 Daily oral administration of UDCA for Institutional Ethics Committee
6months was associated with a decreased rate of gallstone
formation after restrictive bariatric procedures.15 REFERENCES
Furthermore, a meta-analysis of randomized controlled
trials reported that the use of UDCA reduced the 1. Brethauer SA, Chand B, Schauer PR. Risks and
incidence of gallstone formation from 27.7% in placebo benefits of bariatric surgery: current evidence.
group to 8.8% in the treatment group including that Cleveland Clin J Med. 2006;73(11):993.
UDCA can effectively prevent CL after bariatric 2. Pineda O, Maydón HG, Amado M, Sepúlveda EM,
procedures.16 Guilbert L, Espinosa Oet al. A prospective study of
the conservative management of asymptomatic
However, despite the encouraging results found with preoperative and postoperative gallbladder disease
UDCA, it has not been widely applied as a routine in bariatric surgery. Obes Surg. 2017;27(1):148-53.
prophylactic measure against CL after bariatric surgery. 3. Elgamal A, Fawzy AT. Some risk factors of
This was likely due to the lack of distinct criteria that gallstone formation after laparoscopic sleeve
define the proper indication for UDCA based on gastrectomy and the role of ezetimibe versus
measurable risk factors and to the adverse effects of ursodeoxycholic acid in its prevention. Egypt J
UDCA including nausea, vomiting and diarrhea that Internal Med. 2014;26(2):75.
affect patient compliance.9 4. Adams LB, Chang C, Pope J, Kim Y, Liu P, Yates
A. Randomized, prospective comparison of
In this study, conducted on 50 patients divided into two ursodeoxycholic acid for the prevention of
groups after they met the inclusion criteria of this study. gallstones after sleeve gastrectomy. Obes Surg.
Group A received (UDCA) 500mg daily for 6months 2016;26(5):990-4.
15days postoperatively and Group B hadn’t received 5. Mechanick JI, Kushner RF, Sugerman HJ,
(UDCA). Results were collected regarding age, sex, BMI, Gonzalez-Campoy JM, Collazo-Clavell ML, Guven
initial body weight, excess weight loss. S, Spitz AF, et al. American association of clinical
endocrinologists, the obesity society and American
Results showed that using (UCDA) has significant role in society for metabolic and bariatric surgery medical
prophylaxis against development of gall stones, patients guidelines for clinical practice for the perioperative
who received (UDCA) developed gall stones by a nutritional, metabolic, and nonsurgical support of
percentage 0% (0/30) while patients who hadn’t received the bariatric surgery patient. Endocrine Prac.
(UDCA) developed gall stones by a percentage 4.78% 2008;14(1):1-83.
(3/20). Which was concordant with Miller K et al, who 6. Gustafsson U, Benthin L, Granström L, Groen AK,
reported that of 152 patients, 76 were randomized to Sahlin S, Einarsson C. Changes in gallbladder bile
placebo and 76 to 500mg of Ursodeoxycholic Acid daily composition and crystal detection time in morbidly
to assess the role of (UDCA) in prophylaxis against obese subjects after bariatric surgery. Hepatol.
development of gall stones after restrictive bariatric 2005;41(6):1322-8.
surgeries. Gall stone formation was significantly less 7. Tsirline VB, Keilani ZM, El Djouzi S, Phillips RC,
frequent with Ursodeoxycholic Acid than with placebo at Kuwada TS, Gersin K, et al. How frequently and
International Surgery Journal | February 2019 | Vol 6 | Issue 2 Page 407
El-Shenawy MSI et al. Int Surg J. 2019 Feb;6(2):403-408
when do patients undergo cholecystectomy after laparoscopic gastric bypass: a trend analysis of the
bariatric surgery?. Surg Obes Related Dis. nationwide inpatient sample from 2001 to 2008.
2014;10(2):313-21. Obes Surg. 2012;22(2):220-9.
8. Mechanick JI, Youdim A, Jones DB, Garvey WT, 14. Patel JA, Patel NA, Piper GL, Smith DE, Malhotra
Hurley DL, McMahon MM, et al. Clinical Practice G, Colella JJ. Perioperative management of
guidelines for the perioperative nutritional, cholelithiasis in patients presenting for laparoscopic
metabolic, and nonsurgical support of the bariatric Roux-en-Y gastric bypass: have we reached a
surgery patient. Obesity (Silver Spring). 2013 Mar; consensus?. Am Surg. 2009;75(6):470-6.
21(1):S1-27. 15. Miller K, Hell E, Lang B, Lengauer E. Gallstone
9. Manatsathit W, Leelasinjaroen P, Al-Hamid H, formation prophylaxis after gastric restrictive
Szpunar S, Hawasli A. The incidence of procedures for weight loss: a randomized double-
cholelithiasis after sleeve gastrectomy and its blind placebo-controlled trial. Ann Surg.
association with weight loss: A two-centre 2003;238(5):697.
retrospective cohort study. Inter J Surg. 2016;30:13- 16. Uy MC, Talingdan-Te MC, Espinosa WZ, Daez
8. ML, Ong JP. Ursodeoxycholic acid in the
10. Shaffer EA. Epidemiology of gallbladder stone prevention of gallstone formation after bariatric
disease. Best Prac Res Clin Gastroenterol. surgery: a meta-analysis. Obes Surg.
2006;20(6):981-96. 2008;18(12):1532-8.
11. Li VK, Pulido N, Fajnwaks P, Szomstein S, 17. Abdallah E, Emile SH, Elfeki H, Fikry M,
Rosenthal R. Predictors of gallstone formation after Abdelshafy M, Elshobaky A, et al. Role of
bariatric surgery: a multivariate analysis of risk ursodeoxycholic acid in the prevention of gallstone
factors comparing gastric bypass, gastric banding, formation after laparoscopic sleeve gastrectomy.
and sleeve gastrectomy. Surg Endoscopy. Surg Today. 2017;47(7):844-50.
2009;23(7):1640-4.
12. Raziel A, Sakran N, Szold A, Goitein D.
Concomitant cholecystectomy during laparoscopic Cite this article as: El Shenawy MSI, Ammar MS,
sleeve gastrectomy. Surg Endoscopy. Hagag MGE. Effectiveness of using ursodeoxycholic
2015;29(9):2789-93. acid in reducing incidence of gallstone formation
13. Worni M, Guller U, Shah A, Gandhi M, Shah J, after sleeve gastrectomy. Int Surg J 2019;6:403-8.
Rajgor D, et al. Cholecystectomy concomitant with
International Surgery Journal | February 2019 | Vol 6 | Issue 2 Page 408
You might also like
- Massey Bedside Swallowing ScreenDocument1 pageMassey Bedside Swallowing ScreenAngela SatitiNo ratings yet
- 2010 Brown. Reconstruction of The Maxilla and Midface. Introducing A New ClassificationDocument8 pages2010 Brown. Reconstruction of The Maxilla and Midface. Introducing A New ClassificationPablo Enrique Mejia PazNo ratings yet
- Edexcel Unit 1 Notes Cystic FibrosisDocument2 pagesEdexcel Unit 1 Notes Cystic FibrosisIllharm Sherrif100% (2)
- Family Planning: What Are The Advantages of A Contraceptive Injection?Document2 pagesFamily Planning: What Are The Advantages of A Contraceptive Injection?Adrian Clyde BautistaNo ratings yet
- Use of Ursodeoxycholic Acid As A Prophylaxis From Gall Stones After Bariatric Surgery: A Case Control StudyDocument5 pagesUse of Ursodeoxycholic Acid As A Prophylaxis From Gall Stones After Bariatric Surgery: A Case Control StudyFirdaus AldyNo ratings yet
- Manejo de SX Adherencial Con GastrografinDocument7 pagesManejo de SX Adherencial Con Gastrografinmanuel barrientosNo ratings yet
- Cholelithiasis: Causative Factors, Clinical Manifestations and ManagementDocument6 pagesCholelithiasis: Causative Factors, Clinical Manifestations and ManagementmusdalifahNo ratings yet
- PimpaleDocument6 pagesPimpaleMariano BritoNo ratings yet
- Dietary Intake and Ghrelin and Leptin Changes After SleeveDocument8 pagesDietary Intake and Ghrelin and Leptin Changes After Sleevea12345644321No ratings yet
- Initial Experience With Endoscopic Sleeve Gastroplasty in PolandDocument7 pagesInitial Experience With Endoscopic Sleeve Gastroplasty in PolandvictorNo ratings yet
- 10.1007@s11695 019 03862 ZDocument6 pages10.1007@s11695 019 03862 ZAzzeddine MustaphaNo ratings yet
- Apollo 2 Años 2017Document3 pagesApollo 2 Años 2017angelrullNo ratings yet
- Ianuarie 2017Document6 pagesIanuarie 2017Radu MiricaNo ratings yet
- Estudio Expo GastroDocument13 pagesEstudio Expo GastroIsaí VegaNo ratings yet
- 384 2013 Article 1807Document7 pages384 2013 Article 1807Arpit TandonNo ratings yet
- Laparoscopic Metabolic Surgery For The Treatment of Type 2 Diabetes in Asia: A Scoping Review and Evidence-Based AnalysisDocument10 pagesLaparoscopic Metabolic Surgery For The Treatment of Type 2 Diabetes in Asia: A Scoping Review and Evidence-Based AnalysisZulfadliNo ratings yet
- Association Between Body Mass Index Waist CircumfeDocument7 pagesAssociation Between Body Mass Index Waist CircumfeDzulRizkaNo ratings yet
- Pancreatic Cancerrelated Cachexia: Influence On Metabolism and Correlation To Weight Loss and Pulmonary FunctionDocument11 pagesPancreatic Cancerrelated Cachexia: Influence On Metabolism and Correlation To Weight Loss and Pulmonary FunctionLorelie AsisNo ratings yet
- Abstracts For The Website - pdf1441898071Document166 pagesAbstracts For The Website - pdf1441898071Radu MiricaNo ratings yet
- Annals of Medicine and SurgeryDocument4 pagesAnnals of Medicine and SurgeryRadu MiricaNo ratings yet
- Gallstone Formation After Gastrectomy For Adenocarcinoma of The StomachDocument5 pagesGallstone Formation After Gastrectomy For Adenocarcinoma of The StomachMuhammad Fuad MahfudNo ratings yet
- Prognostic Factors and Survival in Patients With Gastric Stump CancerDocument8 pagesPrognostic Factors and Survival in Patients With Gastric Stump Cancerd33aNo ratings yet
- EJMCM - Volume 10 - Issue 4 - Pages 893-903Document11 pagesEJMCM - Volume 10 - Issue 4 - Pages 893-903Junaid IwqNo ratings yet
- Jurnal 4Document7 pagesJurnal 4Ega Gumilang SugiartoNo ratings yet
- Diagnosis and Management of Klatskin Tumor: April 2010Document6 pagesDiagnosis and Management of Klatskin Tumor: April 2010Feby Kurnia PutriNo ratings yet
- Study 4Document6 pagesStudy 4angelrullNo ratings yet
- Health Outcomes of Gastric Bypass Patients Compared To Nonsurgical, Nonintervened Severely ObeseDocument10 pagesHealth Outcomes of Gastric Bypass Patients Compared To Nonsurgical, Nonintervened Severely ObesefseteteamNo ratings yet
- A Study of Clinical Presentations and Management oDocument4 pagesA Study of Clinical Presentations and Management oMaria AkulinaNo ratings yet
- Does Sleeve Shape Make A Difference in Outcomes?Document7 pagesDoes Sleeve Shape Make A Difference in Outcomes?JOTACENo ratings yet
- 01 HepatogastroDocument3 pages01 Hepatogastroyacine26No ratings yet
- Laparoscopic Sleeve Gastrectomy: Perioperative Outcomes, Weight Loss and Impact On Type 2 Diabetes Mellitus Over 2 YearsDocument5 pagesLaparoscopic Sleeve Gastrectomy: Perioperative Outcomes, Weight Loss and Impact On Type 2 Diabetes Mellitus Over 2 YearsYondri Mandaku TasidjawaNo ratings yet
- Billroth I & IIDocument5 pagesBillroth I & IIRoxieparkerNo ratings yet
- BSG Guidelines For The Management of Oesophageal and Gastric CancerDocument24 pagesBSG Guidelines For The Management of Oesophageal and Gastric CancergeorgeNo ratings yet
- Upper GI Malignancy - TutorDocument28 pagesUpper GI Malignancy - Tutoramoody95No ratings yet
- Laparoscopic Sleeve Gastrectomy For Super Super Obese Patients Bmigt60 KG 5151 PDFDocument5 pagesLaparoscopic Sleeve Gastrectomy For Super Super Obese Patients Bmigt60 KG 5151 PDFSuraj KurmiNo ratings yet
- Nin Research Paperon DiabetesDocument4 pagesNin Research Paperon DiabetesAvantikaNo ratings yet
- Per-Operative Conversion of Laparoscopic Cholecystectomy To Open Surgery: Prospective Study at JSS Teaching Hospital, Karnataka, IndiaDocument5 pagesPer-Operative Conversion of Laparoscopic Cholecystectomy To Open Surgery: Prospective Study at JSS Teaching Hospital, Karnataka, IndiaSupriya PonsinghNo ratings yet
- Prognostic Impact of Abdominal Adiposity, Waist Circumference and Body Mass Index in Patients With Intermediate-Risk Prostate Cancer Treated With RadiotherapyDocument7 pagesPrognostic Impact of Abdominal Adiposity, Waist Circumference and Body Mass Index in Patients With Intermediate-Risk Prostate Cancer Treated With RadiotherapyDani KusumaNo ratings yet
- Wjco 13 376Document13 pagesWjco 13 376Novia NadhillaNo ratings yet
- DiazVico-Elli2018 Article UtilityOfImmediatePostoperativDocument4 pagesDiazVico-Elli2018 Article UtilityOfImmediatePostoperativAndrei SarmientoNo ratings yet
- Tto de Ileo BiliarDocument5 pagesTto de Ileo BiliarnerisNo ratings yet
- Features of The Course of Cholelithis Disease in Elderly People With Diseases of The Internal Secretion GlandsDocument6 pagesFeatures of The Course of Cholelithis Disease in Elderly People With Diseases of The Internal Secretion GlandsCentral Asian StudiesNo ratings yet
- Ajphr 810041Document18 pagesAjphr 810041UsmleNo ratings yet
- CPG Ulcer enDocument24 pagesCPG Ulcer enAlina BotnarencoNo ratings yet
- Colonoscopi IndicationDocument26 pagesColonoscopi IndicationTony HardianNo ratings yet
- A Clinical Study of Etiology and Management of Acute Intestinal ObstructionDocument6 pagesA Clinical Study of Etiology and Management of Acute Intestinal ObstructionFalon PapalangiNo ratings yet
- Lu 2014Document6 pagesLu 2014Yanet FrancoNo ratings yet
- Sasjs 810 658-662 FTDocument5 pagesSasjs 810 658-662 FTrifa iNo ratings yet
- JurnalDocument9 pagesJurnalFrans 'cazper' SihombingNo ratings yet
- WJS GastrografinDocument12 pagesWJS Gastrografinkelly_ann23No ratings yet
- Article 1615981002 PDFDocument3 pagesArticle 1615981002 PDFMaria Lyn Ocariza ArandiaNo ratings yet
- Clinical Profile of Patients With Obstructive Jaundice: A Surgeon's PerspectivesDocument5 pagesClinical Profile of Patients With Obstructive Jaundice: A Surgeon's Perspectivessitoxpadang ceriaNo ratings yet
- OAGB v4.3Document27 pagesOAGB v4.3Muhamed sabryNo ratings yet
- S0301211519303719 Viscerale Aiuta Contro ChemioDocument23 pagesS0301211519303719 Viscerale Aiuta Contro Chemiomyname myselfNo ratings yet
- Metastatic Pancreatic Carcinoid Tumor With GOODocument10 pagesMetastatic Pancreatic Carcinoid Tumor With GOOMohamed HadzriNo ratings yet
- Palliative Stenting With or Without Radiotherapy For Inoperable Esophageal CarcinomaDocument7 pagesPalliative Stenting With or Without Radiotherapy For Inoperable Esophageal CarcinomaBella StevannyNo ratings yet
- PIIS2468125320301266Document12 pagesPIIS2468125320301266Putrisuci AndytichaNo ratings yet
- Accepted Manuscript: 10.1016/j.cgh.2015.12.030Document17 pagesAccepted Manuscript: 10.1016/j.cgh.2015.12.030lourdes marquezNo ratings yet
- Intestinal Ultrasound Detects An Increased Diameter and Submucosal Layer Thickness in The Appendix of Patients With Ulcerative Colitis Compared To Healthy Controls - A Prospective Cohort StudyDocument9 pagesIntestinal Ultrasound Detects An Increased Diameter and Submucosal Layer Thickness in The Appendix of Patients With Ulcerative Colitis Compared To Healthy Controls - A Prospective Cohort StudyСергей СадовниковNo ratings yet
- Gastroesophageal Junction Tumors: Overview and UpdatesDocument26 pagesGastroesophageal Junction Tumors: Overview and UpdatesDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Management Guidelines For Gallstone Pancreatitis ADocument6 pagesManagement Guidelines For Gallstone Pancreatitis AkartikapuspitNo ratings yet
- Association of Clinical Outcomes and Complications W - 2016 - Journal of The ChiDocument5 pagesAssociation of Clinical Outcomes and Complications W - 2016 - Journal of The ChiMor OB-GYNNo ratings yet
- Obesity Is Not A RiskDocument7 pagesObesity Is Not A Riskcarlos.alberto.palacios.serratNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Fistula Ani Guideline PDFDocument28 pagesFistula Ani Guideline PDFvivianmtNo ratings yet
- Fistula Ani Japanese GuidelineDocument7 pagesFistula Ani Japanese GuidelinevivianmtNo ratings yet
- Effect of Acupuncture On Post-Hemorrhoidectomy Pain: A Randomized Controlled TrialDocument8 pagesEffect of Acupuncture On Post-Hemorrhoidectomy Pain: A Randomized Controlled TrialvivianmtNo ratings yet
- Infections After Laparoscopic and Open Cholecystectomy: Ceftriaxone Versus Placebo A Double Blind Randomized Clinical TrialDocument6 pagesInfections After Laparoscopic and Open Cholecystectomy: Ceftriaxone Versus Placebo A Double Blind Randomized Clinical TrialvivianmtNo ratings yet
- Five-Year Follow-Up of Antibiotic Therapy For Uncomplicated Acute Appendicitis in The APPAC Randomized Clinical TrialDocument7 pagesFive-Year Follow-Up of Antibiotic Therapy For Uncomplicated Acute Appendicitis in The APPAC Randomized Clinical TrialvivianmtNo ratings yet
- HemoroidDocument2 pagesHemoroidvivianmtNo ratings yet
- Chemistry: Critical: (HH) (Ii)Document3 pagesChemistry: Critical: (HH) (Ii)Ahsen NaveedNo ratings yet
- Nephrology (Flashcards)Document3 pagesNephrology (Flashcards)Anthony BalaoingNo ratings yet
- Bridge Design Part Four Bridge Design, Part Four Aesthetic Enhancement For Anterior Fixed Bridge RestorationsDocument9 pagesBridge Design Part Four Bridge Design, Part Four Aesthetic Enhancement For Anterior Fixed Bridge Restorationsaziz2007No ratings yet
- J Cellular Molecular Medi - 2014 - Liu - The Multiple Functional Roles of Mesenchymal Stem Cells in Participating inDocument10 pagesJ Cellular Molecular Medi - 2014 - Liu - The Multiple Functional Roles of Mesenchymal Stem Cells in Participating indr. RiyanNo ratings yet
- DexamethasoneDocument4 pagesDexamethasoneMits Valencia Karlsson0% (2)
- Ivyx Z Fvbivm I Ivyx Z JVBF F VKWMB ..Document2 pagesIvyx Z Fvbivm I Ivyx Z JVBF F VKWMB ..Arafat RinkyNo ratings yet
- 3 Inflammation and RepairDocument14 pages3 Inflammation and RepaircedonuliNo ratings yet
- Classroom Daily Health Monitoring Tool For CovidDocument4 pagesClassroom Daily Health Monitoring Tool For CovidGenie Sina-on DadeaNo ratings yet
- Teaching Plan For Breast FeedingDocument4 pagesTeaching Plan For Breast FeedingKramSenarevolNo ratings yet
- Self Management SupportDocument8 pagesSelf Management SupportSetiyo Adi NugrohoNo ratings yet
- Multiple Sclerosis Pathology Diagnosis and Management PDFDocument178 pagesMultiple Sclerosis Pathology Diagnosis and Management PDFHari25885No ratings yet
- 4B CervixDocument87 pages4B CervixrubenNo ratings yet
- Gedesnii TugjrelDocument40 pagesGedesnii TugjrelSaibo BoldsaikhanNo ratings yet
- Shiloh Veterinary Hospital: Dell Kay Bertino, DVM Marci Cook, DVM Arielle Mansur, DVMDocument3 pagesShiloh Veterinary Hospital: Dell Kay Bertino, DVM Marci Cook, DVM Arielle Mansur, DVMyonasNo ratings yet
- Acute Kidney Injury in Children: Being AWAREDocument4 pagesAcute Kidney Injury in Children: Being AWAREIrkania PasangkaNo ratings yet
- 10 1016@j Blre 2019 100638 PDFDocument40 pages10 1016@j Blre 2019 100638 PDFHugo HectorNo ratings yet
- Broca's AphasiaDocument22 pagesBroca's Aphasiaعبدالله_عبدوNo ratings yet
- Complete Health HistoryDocument6 pagesComplete Health HistoryAIKA BAYANo ratings yet
- Personal HygieneDocument6 pagesPersonal Hygieneசிவா கிருஷ்ணா100% (1)
- Nursing Care CKDDocument17 pagesNursing Care CKDUlLfa Chii MuetmuethzNo ratings yet
- R3 Brochure EDDocument8 pagesR3 Brochure EDmohsin mazherNo ratings yet
- TanChart PeterBorten 2014 PDFDocument1 pageTanChart PeterBorten 2014 PDFAbd ar Rahman AhmadiNo ratings yet
- Pelod Vs Sofa Scoring in PediatricDocument6 pagesPelod Vs Sofa Scoring in PediatricAdrian KhomanNo ratings yet
- Gastrointestinal System: Anatomy Physiology &disordersDocument52 pagesGastrointestinal System: Anatomy Physiology &disordersprabha5050100% (1)
- SNAPPE-II Score For Neonatal Acute Physiology WithDocument3 pagesSNAPPE-II Score For Neonatal Acute Physiology WithwennyNo ratings yet