Professional Documents
Culture Documents
Drug Utilization Review (Dur) : Definition
Drug Utilization Review (Dur) : Definition
Uploaded by
somayya waliOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Utilization Review (Dur) : Definition
Drug Utilization Review (Dur) : Definition
Uploaded by
somayya waliCopyright:
Available Formats
CHAPTER # 03 DRUG UTILIZATION REVIEW
DRUG UTILIZATION REVIEW (DUR)
INTRODUCTION:
DEFINITION:
Drug utilization review (DUR) is defined as an authorized, structured, ongoing review of
prescribing, dispensing and use of medication.
Or
It is a quality assurance tool which monitors and evaluate drugs used against agreed criteria or
standards and if necessary advice on a change of practices to improve the quality, safety and
cost effectiveness.
EXPLANATION:
DUR/DUE is an ongoing, systematic process designed to maintain the appropriate and effective
use of medications. It involves a comprehensive review of a patient’s medication and health
history before, during, and after dispensing in order to attempt to achieve appropriate therapeutic
decision-making and positive patient outcomes. Pharmacists participating in DUR programs can
directly improve the quality of care for patients, individually and as populations, by striving to
prevent the use of unnecessary or inappropriate drug therapy, prevent adverse drug reactions and
improve overall drug effectiveness. DUR encompasses a drug review against predetermined
criteria that results in changes to drug therapy when these criteria are not met. As a quality
assurance measure, DUR programs provide corrective action, prescriber feedback and further
evaluations. DUR is not done for all drugs because it is tough job and required cost and time. It
is commonly done for those drugs having high cost, wide usage, changes in the dosage, known
or suspected inappropriate use, potential for improvement in patient cane and drug having two
therapeutic windows.
Other terms considered synonymous with DUR include drug use evaluation (DUE), medication
use evaluation (MUE), and medication use management. American Society of Health System
Pharmacists (ASHP) currently espouses the nomenclature medication use evaluation (MUE).
IMPORTANCE OF DRUG UTILIZATION REVIEW:
The importance of Drug utilization review is cleared from following points, these are;
1. DUR programs play a key role in helping managed health care systems understand,
interpret, evaluate and improve the prescribing, administration and use of medications.
2. DUR helps in improving quality of prescribing.
3. Employers and health plans find DUR programs valuable since the results are used to
foster more efficient use of scarce health care resources.
4. Pharmacists play a key role in this process because of their expertise in the area of
medication therapy management.
5. DUR identify areas of education.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
6. DUR affords the managed care pharmacist the opportunity to identify trends in
prescribing within groups of patients whether by disease-state such as those with asthma,
diabetes or high blood pressure, or by drug-specific criteria.
7. Pharmacists in collaboration with prescribers and other members of the health care team
can initiate action to improve drug therapy for patients.
8. It is helpful in development of formulary.
9. DUR allows the pharmacist to document and evaluate the benefit of pharmacy
intervention in improving therapeutic and economic outcomes while demonstrating the
overall value of the pharmacist.
10. It also helps in minimizing cost of treatment.
CLASSIFICATION OF DRUG UTILIZATION REVIEW:
DUR is classified in three categories:
1. Prospective
2. Concurrent
3. Retrospective
1. Prospective DUR: Prospective review involves evaluating a patient's planned drug therapy
before a medication is dispensed. Its main advantage is its preventive potential. It is used
when non-compliance with criteria will have the most serious consequences. The impact of
this approach is noticeable immediately. And physician may become accustomed to the
monitoring as a “double check”.
This process allows the pharmacist to identify and resolve problems before the patient has
received the medication. Pharmacists routinely perform prospective reviews in their daily
practice by assessing a prescription medications dosage and directions while reviewing
patient information for possible drug interactions or duplicate therapy. When part of an
online claims adjudication process, prospective DUR often relies on computerized algorithms
to perform key checks including drug interactions, duplications or contraindications with the
patient’s disease state or condition.
Identification of drug-drug interactions are a common outcome of a prospective DUR. For
example, a patient being treated with warfarin to prevent blood clots may be prescribed a
new drug by another specialist to treat arthritis. If taken together, the patient could experience
internal bleeding. Upon reviewing the patient's prescriptions, the pharmacist would note the
potential drug interaction and contact the prescriber to alert him/her to the problem.
Common problems Addressed by Prospective DUR:
These are;
a) Clinical abuse/misuse
b) Drug-disease contraindications (when a prescribed drug should not be used with certain
diseases).
c) Drug dosage modification.
d) Drug-drug interactions (when two or more different drugs interact and alter their intended
effects, often causing adverse events).
e) Drug-patient precautions (due to age, allergies, gender, pregnancy, etc.).
f) Formulary substitutions (e.g., therapeutic interchange, generic substitution).
g) Inappropriate duration of drug treatment.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
2. Concurrent DUR: Concurrent review is performed during the course of treatment. It also
involves the ongoing monitoring of drug therapy to foster positive patient outcomes. The
main difference is that with concurrent monitoring interventions are corrective. It presents
pharmacists with the opportunity to alert prescribers to potential problems and intervene in
areas such as drug-drug interactions, duplicate therapy, over or underutilization and
excessive or insufficient dosing. This type of review allows therapy for a patient to be altered
if necessary. As electronic prescribing becomes more widely adopted, the concurrent DUR
process may be performed by the prescriber at the time of prescription transmission to the
pharmacy, allowing interventions before the drug is dispensed. An important component of
DUR will require complete and current drug and allergy records for the patient, as well as
knowledge of appropriate therapeutic interchanges for individuals. As a safety net,
pharmacists will perform a similar role as prescribers on the dispensing side of these
transactions.
Concurrent DUR often occurs in institutional settings, where patients often receive multiple
medications. Periodic review of patient records can detect actual or potential drug-drug
interactions or duplicate therapy. It can also alert the pharmacist to the need for changes in
medications, such as antibiotics, or the need for dosage adjustments based on laboratory test
results. The key prescriber(s) must then be alerted to the situation so corrective action can be
taken.
Common problems Addressed by Concurrent DUR:
These are;
a) Drug-disease interactions.
b) Drug-drug interactions.
c) Drug dosage modifications.
d) Drug-patient precautions (age, gender, pregnancy, etc.).
e) Over and underutilization.
f) Therapeutic Interchange.
3. Retrospective DUR: A retrospective DUR reviews drug therapy after the patient has
received the medication. A retrospective review aims to detect patterns in prescribing,
dispensing or administering drugs. Based on current patterns of medication use, prospective
standards and target interventions can be developed to prevent recurrence of inappropriate
medication use or abuse. Outcomes of this review may aid prescribers in improving the care
of their patients, either individually or within a certain target population (e.g., patients with
diabetes, asthma, or high blood pressure). Retrospective DUR is used for identifying
prescribing frequency of a single drug or class of drugs. It can be also used for comparing
drug prescribing among physicians. It can be used for comparing prescribing drugs to
standard treatment guidelines. It can also used for monitoring the therapeutic use of high cost
drugs.
An example of a retrospective DUR may be the identification of a group of patients whose
therapy does not meet approved guidelines. For example, a pharmacist may identify a group
of patients with asthma, who according to their medical and pharmacy history, should be
using orally inhaled steroids. Using this information, the pharmacist can then encourage
prescribers to utilize the indicated drugs.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
Common problems Addressed by Retrospective DUR:
These are;
a) Appropriate generic use.
b) Clinical abuse/misuse.
c) Drug-disease contraindications.
d) Drug-drug interactions.
e) Inappropriate duration of treatment.
f) Incorrect drug dosage.
g) Use of formulary medications whenever appropriate.
h) Over and under utilization.
i) Therapeutic appropriateness and/or duplication.
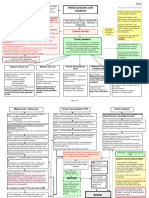
STEPS IN CONDUCTING A DRUG USE EVALUATION
Most authorities agree the following steps are essential when conducting any quality-related
DUR program. These are;
1) Selection of medicine or therapeutic area: In first step, medicine or therapeutic area of
drug utilization review is selected.
2) Identify or Determine Optimal Use (protocol of use): An organization’s established
criteria are defined to compare optimal use with actual use. The criteria should focus on
relevant outcomes within a delineated scope for DUR and identify the relevant drugs to
be monitored for optimal use in advance. For example, if the use of a drug class
prescribed to treat a patient with diabetes is being evaluated, then standards should be
determined to identify all drugs within the drug class and to evaluate each drug’s
effectiveness, such as a decrease in blood glucose or A1c (glycosylated hemoglobin)
levels to within normal limits.
3) Design method for data collection: A specific method is designed for data collection.
Then pilot that method before collection of data.
4) Data collection: This step is where data are gathered to measure the actual use of
medications. These data can be obtained from medical and prescription records or
electronic claim forms. It may require the organization to build an algorithm to identify
all members who fit the criteria.
5) Analyse and compare: Acceptable thresholds (percent of patients meeting the indicator)
should be determined prior to the comparison. This step involves applying the algorithm,
identifying members who meet the DUR criteria and the comparison between optimal or
appropriate and actual use. During this process, the evaluator determines causes for any
discrepancies and whether findings are expected. In this process, patterns or aberrations
can be identified and interpreted.
6) Intervene. This is the step where corrective action is implemented. Action should be
targeted to areas of concern such as prescribing patterns, medication misadventures, and
quality of drug therapy or economic consideration.
7) Evaluate the DUR Program. This step assesses the effectiveness of the DUR program.
Efforts should be made to evaluate the outcomes and document reasons for positive and
negative results. Implementing appropriate changes to the DUR program and continued
observation should be undertaken.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
8) Report the DUR findings. The final step is to report these findings to the appropriate
team within the organization (e.g., the pharmacy & therapeutics committee) and/or
individual prescribers when appropriate.
VALUE OF DUR PROGRAMS IN MANAGED HEALTH CARE:
Introduction:
Managed health care systems and pharmacy benefit management companies (PBMs) have the
responsibility of managing the medication use of anywhere from a few hundred thousand to
millions of patients. DUR programs play a key role in helping these organizations understand,
interpret and improve the prescribing, administration and use of medications. This is often
accomplished by using DUR programs to provide prescribers with feedback on their
performance and prescribing behaviors as compared to pre-set criteria or treatment protocols.
DUR information also allows prescribers to compare their approach to treating certain diseases
with their peers. The benchmarking generated by these comparisons is useful in stimulating
prescribers to change their prescribing habits in an effort to improve care. For example, many
health plans use DUR to encourage prescribers to use more generic drugs and to comply with
treatment guidelines established by national organizations such as the National Institutes of
Health or the American Heart Association by reporting prescriber adherence rates.
DUR information also assists managed health care systems and PBMs in designing educational
programs that improve rational prescribing, formulary compliance and patient compliance. These
educational programs might take the form of face-to-face education of prescribers and patients
by clinical pharmacists, telephone calls, letters, newsletters and educational symposia.
Role of the Health Care Practitioners:
Role of health care practitioners are discussed step wise according to the classes of DUR. These
are;
i. Prospective DUR: This process places responsibility on the health care practitioner to
conduct a review of the drug order when it is presented for filling and proactively resolve
potential drug patient problems. It affords the pharmacist or other health care practitioner
the opportunity to interact with patients and members of the health care team to work on a
treatment plan for each patient. In the retail and institutional settings, a pharmacist can
assess the prescription order at the time of dispensing and, using information from the
patient's medical and/or pharmacy record, determine the appropriateness of the drug therapy
prescribed. If the pharmacist identifies opportunities for improved patient care, he/she can
contact the prescriber to discuss treatment alternatives.
ii. Concurrent DUR: The pharmacist and other health care practitioners have the responsibility
in the concurrent DUR process to assess the ongoing therapy of the patient and, when
necessary, intervene to help modify the patient's treatment plan. When caring for those
patients with multiple diseases, case managers may become actively involved in the
management of the patient's condition. Through interaction with the prescriber, a health care
practitioner within a managed care organization can better understand the care plan the
prescriber would like to follow. Through patient counseling, health care practitioners can
offer education on the proper use of medications and determine if there are specific patient
needs.
iii. Retrospective DUR: Due to their expertise in drug therapy management, health care
practitioners play a leading role in describing the relationship between drug use and patient
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
outcomes using retrospective DUR. When addressing population-based retrospective DUR
issues rather than individual patient care, the managed care pharmacist has a primary role in
planning, organizing and implementing DUR activities. Pharmacists can educate health care
professionals regarding drug use, participate in decision making within the context of the
pharmacy and therapeutics (P&T) committee, and serve as members of DUR and other
committees where input concerning drug use and drug policy development is required.
Conclusion:
The process of DUR is still evolving. Using DUR information, managed care pharmacists can
identify prescribing trends in patient populations and initiate corrective action to improve drug
therapy for groups of patients as well as individuals. As the variety of health care professionals
(e.g., pharmacists, prescribers, nurses, optometrists, naturopaths, chiropractors) involved in the
medication use process expands, DUR will require a more multidisciplinary approach to
improving patient care. In addition, rapidly improving data systems will soon provide the
methodology for marrying medical and pharmacy data with patient outcome data. This will lead
to the next logical step, the evolution of DUR into a more comprehensive health care utilization
evaluation.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
PROTOCOL OF USE OF FEW LOW THERAPEUTIC INDEX DRUGS
VANCOMYCIN
JUSTIFICATION OF USE:
These are the situations in which vancomycin use is acceptable or appropriate.
a) Therapeutic use:
i. It is used for the treatment of serious infection caused by beta lactum resistance
gram positive micro-organisms (MRSA).
ii. Antibiotic associated colitis which fails to respond to metranidazole therapy or is
sever and potentially life threatening.
iii. Treatment of infections caused by gram positive organisms in patient who has
serious allergies to beta lactum antimicrobials.
b) Prophylactic use:
i. It is used as a prophylactic in endocarditis patients who is allergic to beta lactum
antimicrobial and clandamycine and those at high risk for endocarditis.
ii. It is used in surgical procedures like prosthetic materials or devices implantations
e.g. Hip joint replacement.
c) Empiric uses:
i. It is used for infection in critically ill patient related to line or catheter infections.
ii. It is used in febrile neutrophenic patients.
PROCESS INDICATORS:
Different process indicators are used such as;
1. Culture sensitivity test (CST): It is used before the therapy although not needed for
prophylactic and empirical use.
2. Base line serum creatinine: It is done at the time of therapy, if not normal then adjusts
the dose.
3. Base line complete blood count (CBC): e.g. neutrophils count. It is monitored at least
weekly, put increased for serve pats
4. Monitor for complications: e.g. toxicity, nephrotoxicity, neurotoxicity.
5. Red man syndrome: It is due to rapid I/V administration.
6. Serum drug monitoring: It means monitoring of serum drug concentration.
7. Monitor body temperature:
8. Dosage individualized with respect to disease condition, body weight, renal function etc.
DURATION OF THERAPY APPROPRIATE:
a) Therapeutic use: 7-14hrs (I/V 1-1.5gm infusion).
b) Prophylactic use: 24-72hrs (I/Vmg every 6hr for 10-14days orally).
c) Empiric use: 72hrs.
OUTCOME INDICATORS:
Temperature should come to normal within 3 days of administration.
CST test should be negative within 24 hours of stepping vancomycin.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
CIMETIDIN
JUSTIFICATION OF USE:
These are the situations in which Cimetidin use is acceptable or appropriate.
a) Therapeutic use:
i. It is used for the treatment of benign gastric and duodenal ulceration. Its dose is
300mg QID (or 800mg at bed time or 400BD) for 4 weeks.
ii. It is use in NSAID associated ulcer. Its dose is 300mg QID (or 800mg at bed time
or 400BD) for 8 weeks.
iii. It is used in gastric ulceration. Its dose is 300mg QID (or 800mg at bed time or
400BD) for 6 weeks.
iv. It is also justified in reflex oesophagitis. Dose is 400mg QID.
v. It is also justified in Zollinger-Ellision syndrome.
vi. It is used in gastric hyper secretion. Dose is P.O, IV, IM 300-600mg every 6
hours.
vii. It is used in short bowel syndrome too. Dose is 400mg BD.
b) Prophylactic use:
i. It is used in stress ulceration. Dose is 200-400mg every 4-6 hours.
ii. It is used prophylactically in prevention of upper GIT bleeding in critically ill
patients. Dose is 50mg per hour in continuous infusion.
iii. It is used as a acid aspiration in obstetric patients. Dose is 400mg, every 4-6
hours.
iv. It is also used in helicobacter pylori eradication. Dose is 400mg BD with
antibiotics.
PROCESS INDICATORS:
Different process indicators are used such as;
1. Monitor patients mental stat: Because it causes confusion.
2. Monitor patient for hyper sensitivity.
3. Monitor the significant D/s: e.g. warfarin, phenytoin.
4. Monitor the patient for complete blood count (CBC): Because cimetidin causes GIT
bleeding.
5. Monitor the pregnant and lactating patients.
6. Dose adjustment: It is usually done in renal and hepatic impairment.
7. Drug must be taken with food: Because proper pH is required.
DURATION OF THERAPY APPROPRIATE:
a) Therapeutic use: it is from 6 hours to 8 weeks
b) Prophylactic use: It is 200-400mg every 4-6 hours.
OUTCOME INDICATORS:
Active ulcer must be treated within 8 weeks.
GERD must be treated within 12 weeks.
AN EASY APPROACH TO CLINICAL PHARMACY
CHAPTER # 03 DRUG UTILIZATION REVIEW
PREDNISOLONE:
It belongs to steroids family (corticosteroid).
JUSTIFICATION OF USE:
These are the situations in which prednisolone use is acceptable or appropriate.
a) Therapeutic use:
i. It is used as a first line therapy in endocrine disorders, rheumatic disorders, acute
gouty arthritis and infiltrated inflammatory lesions of lichen plants.
ii. It is used in the treatment of steroid responsive inflammatory condition of
palpebral and bulbar conjunctive.
b) Prophylactic use:
i. It is used in allergic and inflammatory process.
PROCESS INDICATORS:
Different process indicators are used such as;
1. Dosage individualized: It is with respect to diseases i.e. herpes, chicken pox or other
viral diseases, diabetes, renal impairment.
2. Base line serum creatinine: It is done at the time of therapy, in order to adjusts the dose
and dosage.
3. Base line complete blood count (CBC) monitoring: e.g. leucocytes count, because it
decreases leucocytes count.
4. Monitor for complications: It is monitored for complications such as hypoglycemia,
hyperglycemia, hypocalcemia during treatment, delayed wound healing, menstrual
irregularities, fluid retention especially during pregnancy, GIT bleeding and moon face.
DURATION OF THERAPY APPROPRIATE:
a) P.O loading dose: 10-20 mg daily (60mg in severe cases) preferably in the morning time
after breakfast.
b) P.O maintenance dose: 2.5mg-15mg daily.
c) I/M prednisolone acetate): 25-100mg once or twice weekly.
WITHDRAWAL PROCEDURE:
The dose may be reduced rapidly down to physiological doses (7.5mg daily) and then reduce
more slowly.
Monitor for significant drug interactions, such as antichlinesterases, ambenonium, aspirin,
barbiturates, ritamplan, pyridostigmine, phenytoin, lectoconazole, hydantion, salicylates etc.
OUTCOME INDICATORS:
Inflammatory lesions should disappear.
The serum prednisolone level shall come to normal.
******************************************************************************
AN EASY APPROACH TO CLINICAL PHARMACY
You might also like
- 3 Spinal Cord Injury Nursing Care PlanDocument9 pages3 Spinal Cord Injury Nursing Care PlanCyrus De Asis88% (8)
- Biol 235 Assignment-3Document21 pagesBiol 235 Assignment-3Kiron GonidisNo ratings yet
- Praktikum Reproduksi 2Document46 pagesPraktikum Reproduksi 2Andika Tatag100% (1)
- Drug Utilization ReviewDocument5 pagesDrug Utilization ReviewWàrìs Ràfìqùé ßàlòçhNo ratings yet
- Drug Utilization ReviewsDocument7 pagesDrug Utilization ReviewsenoyNo ratings yet
- What Are Drug Utilization Reviews (Dur) : Why Durs Are ImportantDocument3 pagesWhat Are Drug Utilization Reviews (Dur) : Why Durs Are ImportantthegroovyNo ratings yet
- Drug Use EvaluationDocument27 pagesDrug Use Evaluationshanthi dasariNo ratings yet
- An Introduction To Pharmaco-EpidemiologyDocument21 pagesAn Introduction To Pharmaco-EpidemiologyMr.ShazNo ratings yet
- Drug Utilization Review (DUR)Document8 pagesDrug Utilization Review (DUR)Rinta MoonNo ratings yet
- Ward Round Participation & Drug Therapy MonitoringDocument20 pagesWard Round Participation & Drug Therapy MonitoringAman UpadhyayNo ratings yet
- Daily Activity of Clinical PharmacistDocument18 pagesDaily Activity of Clinical PharmacistŖÖŸÄĻ ŚÏVÄッNo ratings yet
- Medicine Use Evaluation: A Guide To ImplementationDocument26 pagesMedicine Use Evaluation: A Guide To ImplementationmrboredguyNo ratings yet
- DUR For PassingDocument24 pagesDUR For PassingAnne Paoad GambulaoNo ratings yet
- Drug Utilization ReviewDocument7 pagesDrug Utilization ReviewFaizaNadeemNo ratings yet
- Drug Utilization Review PDFDocument7 pagesDrug Utilization Review PDFDimas CendanaNo ratings yet
- Rational Drug Use NoteDocument14 pagesRational Drug Use NoteSteven A'Baqr EgiliNo ratings yet
- UNIT4 Clinical PharmacyDocument21 pagesUNIT4 Clinical PharmacyIsha AgarwalNo ratings yet
- Terms in ClinicalDocument10 pagesTerms in ClinicalZahraNo ratings yet
- Drug Therapy MonitoringDocument48 pagesDrug Therapy MonitoringPooja agarwalNo ratings yet
- ASHP Guidelines On Preventing Medication Errors in HospitalsDocument9 pagesASHP Guidelines On Preventing Medication Errors in HospitalsMedarabiaNo ratings yet
- Drug Therapy Monitoring and Pharmaceutical CareDocument48 pagesDrug Therapy Monitoring and Pharmaceutical CareHarsh Bhardwaj100% (1)
- Drug Therapy MonitoringDocument38 pagesDrug Therapy MonitoringSumanth100% (1)
- MedicationReview PracticeGuide2011Document29 pagesMedicationReview PracticeGuide2011Yusnia Gulfa MaharaniNo ratings yet
- Drug Utilization ReviewDocument7 pagesDrug Utilization ReviewArslan BashirNo ratings yet
- Drug Utilization Study in The Department of Medicine at A Teaching HospitalDocument11 pagesDrug Utilization Study in The Department of Medicine at A Teaching HospitalFaizan Ali UniqueNo ratings yet
- 4Document5 pages4Creepy PotatoesNo ratings yet
- Course: Patient Safety Solutions Topic:: Some DefinitionsDocument5 pagesCourse: Patient Safety Solutions Topic:: Some DefinitionsKian GonzagaNo ratings yet
- Drug Therapy MonitoringDocument13 pagesDrug Therapy MonitoringRaju Niraula100% (1)
- ASHP 5things List - 2022 UpdatesDocument3 pagesASHP 5things List - 2022 Updatesed seraficaNo ratings yet
- DurDocument18 pagesDurxtremist2001100% (2)
- Review of Pharmaceutical Care Services Provided by The PharmacistsDocument3 pagesReview of Pharmaceutical Care Services Provided by The PharmacistsellianaeyNo ratings yet
- The Assignment On Medication Errors in A Hospital & Some Examples of Adverse Reactions and Poisoning IncidencesDocument25 pagesThe Assignment On Medication Errors in A Hospital & Some Examples of Adverse Reactions and Poisoning IncidencesGroup Of Cheaters (ফাতরা)No ratings yet
- Pharamacology Notes 3Document7 pagesPharamacology Notes 3Martinet CalvertNo ratings yet
- Chapter 1Document23 pagesChapter 1Kuia AllardeNo ratings yet
- Introduction To Clinical PharmacyDocument32 pagesIntroduction To Clinical PharmacySuhail Ahmed SahitoNo ratings yet
- Clinical PharmacyDocument26 pagesClinical PharmacyboyapallymeghanaNo ratings yet
- Introduction To PharmacotherapeuticsDocument49 pagesIntroduction To PharmacotherapeuticsChandraprakash JadhavNo ratings yet
- ASHP Medication Use EvaluationDocument3 pagesASHP Medication Use EvaluationArslan BashirNo ratings yet
- Pharm Care 4 Chapter 1Document25 pagesPharm Care 4 Chapter 1MaraNagaSambarani100% (1)
- Adherence To MedicationDocument11 pagesAdherence To Medicationwillie2210100% (1)
- Rational Drug Use and PharmacistDocument4 pagesRational Drug Use and PharmacistJozef CherianNo ratings yet
- Standards of Practice For Clinical PharmacistsDocument4 pagesStandards of Practice For Clinical PharmacistsAIMANIBRAHIM82No ratings yet
- Lecture 3. General Guidelines For Clinical Pharmacy PracticeDocument22 pagesLecture 3. General Guidelines For Clinical Pharmacy Practicedaniya nadeem100% (1)
- Problems of Irrational Drug Use: Session GuideDocument22 pagesProblems of Irrational Drug Use: Session Guidearyo aryoNo ratings yet
- Addition and DeletionDocument10 pagesAddition and DeletionNikkaMontilNo ratings yet
- Hospital Formulary-Lecture NotesDocument7 pagesHospital Formulary-Lecture NotesPatras BhattiNo ratings yet
- Riazul LimonDocument25 pagesRiazul LimonGroup Of Cheaters (ফাতরা)No ratings yet
- Pharmacy CareDocument9 pagesPharmacy Caremysrsk100% (1)
- Role of Pharmacist Finale FatimaDocument5 pagesRole of Pharmacist Finale FatimafaramaNo ratings yet
- Org STP Harm CareDocument3 pagesOrg STP Harm CarelatemmaNo ratings yet
- Statements Pharmaceutical CareDocument3 pagesStatements Pharmaceutical CareDiegoAndrésYiZapataNo ratings yet
- 2.1 Pharmaceutics - IiDocument41 pages2.1 Pharmaceutics - Iiraukiraj37No ratings yet
- Pharmaceutical CareDocument7 pagesPharmaceutical Caresomayya waliNo ratings yet
- Drug Therapy CP A1Document6 pagesDrug Therapy CP A1Faizah KhalidNo ratings yet
- Phos 313 - Activity No 7 PhosDocument6 pagesPhos 313 - Activity No 7 PhosDIANA CAMILLE CARITATIVONo ratings yet
- Pharmacy CareDocument9 pagesPharmacy CareJoslin RozNo ratings yet
- Outpatient Pharmacy: Course Name: Hospital Training Course Code: PHD311 Date: 22 October 2020Document37 pagesOutpatient Pharmacy: Course Name: Hospital Training Course Code: PHD311 Date: 22 October 2020honeylemon.coNo ratings yet
- Adherence MedicationDocument12 pagesAdherence Medicationb.modNo ratings yet
- Chapter 38. Medication Reconciliation: BackgroundDocument14 pagesChapter 38. Medication Reconciliation: BackgroundnurhaidahNo ratings yet
- Dur and Due - 2016Document15 pagesDur and Due - 2016AriNo ratings yet
- Drug Utilisation ReviewDocument33 pagesDrug Utilisation ReviewkeerthanaNo ratings yet
- BPJ64 PolypharmacyDocument11 pagesBPJ64 PolypharmacyLimYouhokNo ratings yet
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Ethics and Pharmaceutical Industry: Presented by Seth KokoraDocument13 pagesEthics and Pharmaceutical Industry: Presented by Seth Kokorasomayya waliNo ratings yet
- ABH Sugar Troche (24 Troches) : Method of PreparationDocument1 pageABH Sugar Troche (24 Troches) : Method of Preparationsomayya waliNo ratings yet
- Define Communication. What Is The Importance of Communication in Business? HistoryDocument4 pagesDefine Communication. What Is The Importance of Communication in Business? Historysomayya waliNo ratings yet
- Pharmaceutical CareDocument7 pagesPharmaceutical Caresomayya waliNo ratings yet
- Diseases ClinicalDocument57 pagesDiseases Clinicalsomayya wali100% (1)
- Case Histo PDFDocument19 pagesCase Histo PDFsomayya waliNo ratings yet
- Accuracy, Precision, Mean and Standard Deviation: ICP Operations Guide: Part 14 by Paul Gaines, PH.DDocument3 pagesAccuracy, Precision, Mean and Standard Deviation: ICP Operations Guide: Part 14 by Paul Gaines, PH.Dsomayya waliNo ratings yet
- Detection of NoncomplianceDocument12 pagesDetection of Noncompliancesomayya waliNo ratings yet
- 10 Alkanes NomenclatureDocument29 pages10 Alkanes Nomenclaturesomayya waliNo ratings yet
- Meditation - Benefits of MeditationDocument2 pagesMeditation - Benefits of Meditationnavdeep2309No ratings yet
- Drug-Induced Nephrotoxicity: Cynthia A. Naughton, Pharmd, BCPS, North Dakota State University College of PharmacyDocument8 pagesDrug-Induced Nephrotoxicity: Cynthia A. Naughton, Pharmd, BCPS, North Dakota State University College of PharmacyAbdur Rachman Ba'abdullahNo ratings yet
- Hasler 2004 Prochaska Eating DisordersDocument7 pagesHasler 2004 Prochaska Eating Disordersandra_coralia9112No ratings yet
- Hopper 1975Document4 pagesHopper 1975egrdfgNo ratings yet
- Pengaruh Inisiasi Menyusu Dini Terhadap Waktu Pengeluaran Dan Perubahan Warna Mekonium Serta Kejadian Ikterik FisiologisDocument8 pagesPengaruh Inisiasi Menyusu Dini Terhadap Waktu Pengeluaran Dan Perubahan Warna Mekonium Serta Kejadian Ikterik FisiologisYESI NURMALA SARI SIANIPAR 1901015No ratings yet
- Diarrhea Drug StudyDocument12 pagesDiarrhea Drug StudyCeelin Robles0% (1)
- Caesarean SectionDocument32 pagesCaesarean SectionshravaniNo ratings yet
- Small Animals Ebook Collection-1Document48 pagesSmall Animals Ebook Collection-1Sanjay Kumar100% (4)
- Health Status QuestionaireDocument4 pagesHealth Status Questionaireapi-107381417No ratings yet
- DASS 21 in HealthcareDocument9 pagesDASS 21 in HealthcareRebecca SilaenNo ratings yet
- B.SC Nursing2018Question PapersFirst YearNursing Foundations FR 4firstDocument1 pageB.SC Nursing2018Question PapersFirst YearNursing Foundations FR 4firstJagdeesh PrasadNo ratings yet
- Travel Medicine: Health Quarantine 2021 Dr. Esther Meylina SipahutarDocument35 pagesTravel Medicine: Health Quarantine 2021 Dr. Esther Meylina SipahutarEsther Meyline XhypaNo ratings yet
- Ovarian Cancer: Presented By-Vaishnavi Saxena B.SC Nursing 3 YearDocument17 pagesOvarian Cancer: Presented By-Vaishnavi Saxena B.SC Nursing 3 YearVaishnavi Saxena100% (2)
- Monoclonal Antibodies: K. Prameela Department of Biotechnology Gitam UniversityDocument20 pagesMonoclonal Antibodies: K. Prameela Department of Biotechnology Gitam Universityanjanakaveri100% (1)
- AbtrascDocument2 pagesAbtrascbebo94No ratings yet
- Adult Headache GuidelinesDocument7 pagesAdult Headache Guidelinespallavi priyamNo ratings yet
- cv2018 HRDocument4 pagescv2018 HRLiliana SvetoslavovaNo ratings yet
- CHICKENPOXDocument36 pagesCHICKENPOXAlyssa Marie Pepito100% (1)
- Abnormal PsychologyDocument136 pagesAbnormal PsychologyMary Ye Ariola Magsino100% (3)
- Shekar Nethralaya: Complete Eye Care SolutionsDocument16 pagesShekar Nethralaya: Complete Eye Care SolutionsShubham MaheshwariNo ratings yet
- Shija IntroDocument27 pagesShija IntroHomeshori SoraishamNo ratings yet
- Kuesioner MenstruasiDocument7 pagesKuesioner MenstruasirerenNo ratings yet
- 24 Cerebral Blood FlowDocument31 pages24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Passing 3rd Year at University College London Medical SchoolDocument6 pagesPassing 3rd Year at University College London Medical Schoolkjb57No ratings yet
- Pmls Midterms ReviewerDocument10 pagesPmls Midterms ReviewerCute ni LeynesNo ratings yet
- NPH RadscaleDocument8 pagesNPH RadscaleLeChuckNo ratings yet
- D2 FC Mnchan 1Document24 pagesD2 FC Mnchan 1Keanu Win CatipayNo ratings yet