Professional Documents
Culture Documents
HAP Infographic Poster
HAP Infographic Poster
Uploaded by
wrnaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HAP Infographic Poster
HAP Infographic Poster
Uploaded by
wrnaCopyright:
Available Formats
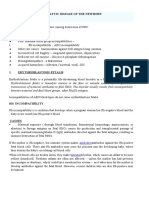
Predicting and Preventing Pre-eclampsia
THE CHALLENGE THE SOLUTION MAKING A DIFFERENCE
Definition: Pre-eclampsia
• A condition that affects 2–5% of pregnant women— Use risk factors plus biomarkers.
and as high as 8–12% in some countries in Africa—
usually from around 20 weeks
Includes high blood pressure + signs of damage to an
Four useful
•
1. Mean arterial pressure (MAP)
organ system, usually liver and kidneys Fight for • A key barrier to prevention of pre-eclampsia
biomarkers in LMICs is delayed first antenatal visit or
• High blood pressure (hypertension) and protein in 2. Serum placental growth factor comprehensive, contact with the health system
urine (proteinuria) for preterm (PLGF)
EARLY Convince women of the benefits of a first
pre-eclampsia
•
3. Uterine artery pulsatility index antenatal antenatal visit early in the first trimester
Pre-eclampsia is one of the leading causes of prediction at
maternal and perinatal morbidity and mortality.
(UTPI) visits for all • Remove barriers to antenatal care such
11–13+6 weeks’ as acceptability, affordability,
4. Serum pregnancy associated women: accessibility and quality
gestation: plasma protein-A (PAPP-A) Integrate pre-eclampsia risk assessment
Globally • Pre-eclampsia is associated with a variety of •
complications as an integral part of basic first trimester
76,000 • Most common cause of death in women with evaluation protocol
women die pre-eclampsia is intracranial haemorrhage
each year • Life expectancy of women who developed IDEAL PRE-ECLAMPSIA SOLUTION
preterm pre-eclampsia, requiring delivery at Push for • Prioritise provider education, consistent
from <37 weeks, is reduced on average by 10 years comprehensive
adherence to clinical guidelines and
Universal screening: improvement in referral pathways
pre-eclampsia • Women in low-resource countries are at a All pregnant women should be screened for universal • Workforce, availability of essential
higher risk of developing pre-eclampsia preterm pre-eclampsia at 11–13+6 weeks’
health drugs, information systems, governance
gestation using a combination of maternal risk and financing must be addressed
factors and biomarkers. The best model systems
Globally • Infants born to combines maternal risk factors + MAP, PLGF & approach:
mothers with
500,000 pre-eclampsia
UTPI. PAPP-A can be considered when PLGF &
UTPI cannot be measured.
babies die are at risk of being 1. Greater international attention is needed on
each year from born prematurely — pre-eclampsia and links between maternal health and non-
delivery is the communicable diseases (NCDs) as part of the SDGs agenda.
pre-eclampsia only cure. Where resources are limited:
Routine screening for preterm pre-eclampsia 2. All countries have an obligation to implement the best
by maternal risk factors and MAP should be pre-eclampsia testing and management practices
Maternal risk factors are associated done in all pregnancies. they can.
with the development of pre-eclampsia.
3. Skill development of primary health care providers on
risk assessment, accurate BP measurement, counselling, ensuring
Major Risk Factors: Minor Risk Factors: Treatment: aspirin availability and adherence to drug treatment and follow
Pre-existing chronic Advanced maternal age, nulliparity, Women identified at high risk should receive up makes the biggest difference to pre-eclampsia outcomes.
hypertension, renal disease, short and long inter-pregnancy intervals, aspirin prophylaxis at ~150 mg per night 4. Cost effectiveness of early pre-eclampsia prediction shows
autoimmune diseases, assisted reproductive technologies, commencing at 11–14+6 weeks’ gestation, substantial cost saving; prevention and treatment
previous history of obesity, ethnicity, family history of until 36 weeks gestation. saves lives.
pre-eclampsia pre-eclampsia
Download the FIGO pre-eclampsia guidelines at: www.figo.org/preeclampsia-guidelines
You might also like
- Prom Pprom SeminarDocument25 pagesProm Pprom Seminarizyanzati100% (1)
- Fixing - Nigeria (1) - 1 PDFDocument40 pagesFixing - Nigeria (1) - 1 PDFFlying Doctors Nigeria100% (1)
- Medical DisordersDocument225 pagesMedical DisordersWael GaberNo ratings yet
- Fetal DevelopmentDocument19 pagesFetal DevelopmentYemaya84No ratings yet
- AbortionDocument19 pagesAbortionAhmed SabryNo ratings yet
- Final Research Poster PDFDocument1 pageFinal Research Poster PDFapi-368247153No ratings yet
- MalpresentationDocument37 pagesMalpresentationLovely SarangiNo ratings yet
- HEMOLYTIC DISEASE OF THE NEWBORN - Docx PrintDocument6 pagesHEMOLYTIC DISEASE OF THE NEWBORN - Docx PrintJudy HandlyNo ratings yet
- Vasa PraeviaDocument14 pagesVasa Praeviakhadzx100% (2)
- Ectopic PregnancyDocument39 pagesEctopic PregnancyFecky Fihayatul IchsanNo ratings yet
- Rhesus Iso ImmunizationDocument12 pagesRhesus Iso Immunizationapi-3705046No ratings yet
- Jaundice in PregnancyDocument13 pagesJaundice in PregnancyAnonymous mvNUtwidNo ratings yet
- Factors Affecting Maternal Perception of Fetal MovementsDocument9 pagesFactors Affecting Maternal Perception of Fetal MovementsNoraNo ratings yet
- Mal Presentations Mal PositionsDocument4 pagesMal Presentations Mal PositionsMelissa Aina Mohd YusofNo ratings yet
- Shoulder DystociaDocument53 pagesShoulder DystociaMisganaw WorkuNo ratings yet
- Hepatitis B in PregnancyDocument17 pagesHepatitis B in PregnancysnazzyNo ratings yet
- Cervical EncirclageDocument8 pagesCervical EncirclageAnnapurna DangetiNo ratings yet
- Lower Respiratory InfectionDocument108 pagesLower Respiratory InfectionDewina Dyani Rosari IINo ratings yet
- Face and Brow Presentations in LaborDocument6 pagesFace and Brow Presentations in LabordenekeNo ratings yet
- Cardiotocograph (CTG) Interpretation and ResponseDocument23 pagesCardiotocograph (CTG) Interpretation and ResponseAndi Farid ANo ratings yet
- Malpresentation and Malposition: Supervision By: DR Ashjan Tarayra Directed By: DR Montaser AsafrahDocument53 pagesMalpresentation and Malposition: Supervision By: DR Ashjan Tarayra Directed By: DR Montaser AsafrahMahmoud Asafrah100% (1)
- Pregnancy and Labor at Fetal Malpresentations and Abnormal PelvisDocument40 pagesPregnancy and Labor at Fetal Malpresentations and Abnormal PelvisCoral Srinivasa Ramalu100% (1)
- Obg-13.4.20, After Noon Unit Xi, Effects of Drugs On Mother and FetusDocument22 pagesObg-13.4.20, After Noon Unit Xi, Effects of Drugs On Mother and FetusElakkiyaanu64 Elakkiyaanu64No ratings yet
- Constriction Band SyndromeDocument8 pagesConstriction Band SyndromesabistonNo ratings yet
- Abnormalities of Labour and Delivery and Their Management: Joó József GáborDocument44 pagesAbnormalities of Labour and Delivery and Their Management: Joó József GáborAnnisa Mutiara InsaniNo ratings yet
- 29 - Abnormal Uterine ActionDocument31 pages29 - Abnormal Uterine Actiondr_asaleh94% (18)
- Ginecologic ExaminationDocument24 pagesGinecologic ExaminationPeter HoNo ratings yet
- Ob-Gyn (Clinic/Office) Nurse: OB/GYN Nurses Provide A Variety of Functions Related To The Female Reproductive SystemDocument13 pagesOb-Gyn (Clinic/Office) Nurse: OB/GYN Nurses Provide A Variety of Functions Related To The Female Reproductive SystemJaclyn SarmientoNo ratings yet
- NSTDocument5 pagesNSTMarlisa YanuartiNo ratings yet
- Intrauterine Fetal Death: Prepared By: Roshni Adhikari Roshani Sunar Sabina Ranabhat Sadhana DevkotaDocument15 pagesIntrauterine Fetal Death: Prepared By: Roshni Adhikari Roshani Sunar Sabina Ranabhat Sadhana DevkotaRoshni SunarNo ratings yet
- CHEST PHYSIOTHERAPY IN NEONATES NotesDocument14 pagesCHEST PHYSIOTHERAPY IN NEONATES NotesAnu YadavNo ratings yet
- Breech Presentation:: EtiologyDocument16 pagesBreech Presentation:: Etiologyhussain AltaherNo ratings yet
- Ps of LaborDocument28 pagesPs of LaborErvina Luisa Delias CampusNo ratings yet
- Ovarian Cysts Overview: Menstrual Cycle Pregnancy UltrasoundDocument13 pagesOvarian Cysts Overview: Menstrual Cycle Pregnancy Ultrasoundzerocoolz123No ratings yet
- History TakingDocument26 pagesHistory TakingShauie CayabyabNo ratings yet
- DRTP Specialty Handbook Obstetrics and GynaecologyDocument48 pagesDRTP Specialty Handbook Obstetrics and GynaecologyAloah122346No ratings yet
- M.M. College of Nursing: Assignment ON Different Signs During PregnancyDocument4 pagesM.M. College of Nursing: Assignment ON Different Signs During PregnancyNadiya RashidNo ratings yet
- Ruptured Ectopic Pregnancy: by Lingga Lilianie Nur Safqi Guidance Dr. Reno YovialDocument31 pagesRuptured Ectopic Pregnancy: by Lingga Lilianie Nur Safqi Guidance Dr. Reno YoviallinggasafqiNo ratings yet
- ProlapseDocument51 pagesProlapsejijaniNo ratings yet
- Amniocentesis and CVS UHL Obstetric GuidelineDocument8 pagesAmniocentesis and CVS UHL Obstetric GuidelineGzz JoengNo ratings yet
- Birth Injuries in NeonatesDocument14 pagesBirth Injuries in NeonatessolecitodelmarNo ratings yet
- Deep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateDocument26 pagesDeep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateCristinaCaprosNo ratings yet
- Post Exposure Management Hepatitis B Hepatitis C and HivDocument39 pagesPost Exposure Management Hepatitis B Hepatitis C and HivQaiser ZamanNo ratings yet
- Active Management of Third Stage of Labour PracticDocument6 pagesActive Management of Third Stage of Labour PracticBhawna JoshiNo ratings yet
- Medical Diseases Complicating Pregnancy: by The Name of AllahDocument45 pagesMedical Diseases Complicating Pregnancy: by The Name of Allah'محمد علي' محمد لافيNo ratings yet
- Shoulder DystociaDocument37 pagesShoulder DystociaClaudia SanchezNo ratings yet
- Endocrine Disorders During Pregnancy 2006Document223 pagesEndocrine Disorders During Pregnancy 2006STEPHANIE TALILAHNo ratings yet
- 2) Normal & Abnormal Labor-1Document162 pages2) Normal & Abnormal Labor-1linaNo ratings yet
- Cryo SurgeryDocument8 pagesCryo SurgeryninroseNo ratings yet
- Assisting in Papanicolaou SmearDocument13 pagesAssisting in Papanicolaou SmearRika Mae100% (1)
- Risk of Post Partum Infections-1Document29 pagesRisk of Post Partum Infections-1gerryneutron100% (1)
- GTG 64b PDFDocument21 pagesGTG 64b PDFajeng larasati0% (1)
- Occiput Posterior Position Diagnosis VagDocument19 pagesOcciput Posterior Position Diagnosis VagMutianaUmminyaKhanzaNo ratings yet
- MK Fetal Lie and Presentation (OBGY)Document9 pagesMK Fetal Lie and Presentation (OBGY)Moses Jr KazevuNo ratings yet
- Benign Ovarian TumorsDocument38 pagesBenign Ovarian Tumorssimi yNo ratings yet
- Molar Pregnancy: Capitol Medical Center CollegesDocument38 pagesMolar Pregnancy: Capitol Medical Center CollegesDarlene Laude GoyaNo ratings yet
- 050 PPT - RetinoblastomaDocument61 pages050 PPT - RetinoblastomaAnastasia TjanNo ratings yet
- Clinical Tools and Biomarkers To Predict PreeclampsiaDocument10 pagesClinical Tools and Biomarkers To Predict PreeclampsiaZakkiyatus ZainiyahNo ratings yet
- Ijgo 12741Document5 pagesIjgo 12741zainabNo ratings yet
- Serum Uric Acid To Creatinine Ratio and Risk Of.14Document6 pagesSerum Uric Acid To Creatinine Ratio and Risk Of.14Familia Valdivia VilcaNo ratings yet
- FM9 0000000000000088Document6 pagesFM9 0000000000000088roboticsengineer.anttNo ratings yet
- Angel Summer Field Report (Max Hospital)Document50 pagesAngel Summer Field Report (Max Hospital)varshasharma05100% (1)
- Nursing Care Plan Neonatal Intensive Care Unit: All India Institute of Medical Sciences, RishikeshDocument14 pagesNursing Care Plan Neonatal Intensive Care Unit: All India Institute of Medical Sciences, RishikeshArchna Yadav100% (1)
- NRP 8 Edition in Canada: A Review of New Recommendations and Their RationaleDocument32 pagesNRP 8 Edition in Canada: A Review of New Recommendations and Their RationaleRavikiran Suryanarayanamurthy100% (1)
- Edit - HIL - Daily IGD 25.09.19Document30 pagesEdit - HIL - Daily IGD 25.09.19Inez WijayaNo ratings yet
- Breastfeeding and The Use of Human Milk: An Analysis of The American Academy of Pediatrics 2012 Breastfeeding Policy StatementDocument2 pagesBreastfeeding and The Use of Human Milk: An Analysis of The American Academy of Pediatrics 2012 Breastfeeding Policy StatementBayna Lestari LubisNo ratings yet
- Final Research Poster PDFDocument1 pageFinal Research Poster PDFapi-368247153No ratings yet
- Neonatal Respiratory Distress SyndromenhschoicesDocument6 pagesNeonatal Respiratory Distress SyndromenhschoicessehatkanNo ratings yet
- Trust Guideline For The Newborn and Infant Physical Examination (NIPE)Document37 pagesTrust Guideline For The Newborn and Infant Physical Examination (NIPE)Clara CarneiroNo ratings yet
- High Risk NewbornDocument10 pagesHigh Risk NewbornEmmy Flor ValmoriaNo ratings yet
- Drug StudyDocument2 pagesDrug StudyJohn Ronnel De GuiaNo ratings yet
- Obstetric ComplicationsDocument70 pagesObstetric ComplicationsNikhil TyagiNo ratings yet
- Breastcrawl PDFDocument41 pagesBreastcrawl PDFRyan AndarestaNo ratings yet
- NCM 102 - Lecture (PPP)Document245 pagesNCM 102 - Lecture (PPP)rhenier_ilado100% (3)
- The High Risk PregnancyDocument23 pagesThe High Risk Pregnancynursereview100% (3)
- The Role of Parity in The Mode of DeliveryDocument11 pagesThe Role of Parity in The Mode of DeliveryKanuyasa GekzNo ratings yet
- Asa 2016Document1,008 pagesAsa 2016dennyramdhanNo ratings yet
- The Grand MultiparaDocument5 pagesThe Grand MultiparaIndhumathiNo ratings yet
- Drug Use During Pregnancy and LactationDocument45 pagesDrug Use During Pregnancy and LactationSayli GoreNo ratings yet
- ACOG Guidelines For Exercise During PregnancyDocument13 pagesACOG Guidelines For Exercise During Pregnancypptscribid100% (1)
- Null 1Document8 pagesNull 1arpit kaushikNo ratings yet
- GemeliDocument11 pagesGemeliCacing UcilNo ratings yet
- NSVD Case Study FinalDocument60 pagesNSVD Case Study Finaljints poterNo ratings yet
- Significance of Non-Nutritive Sucking For Preterm InfantsDocument26 pagesSignificance of Non-Nutritive Sucking For Preterm Infantsapi-337349463No ratings yet
- Neonatal PneumoniaDocument11 pagesNeonatal PneumoniaKristine Joy Cadiz AgostoNo ratings yet
- Assisted Vaginal Delivery Using The Vacuum ExtractorDocument7 pagesAssisted Vaginal Delivery Using The Vacuum ExtractorAhmad MuhyiNo ratings yet
- Enfermedades Emergentes y Embarazo - EID - November 2006 - Volume CompletoDocument187 pagesEnfermedades Emergentes y Embarazo - EID - November 2006 - Volume CompletoRuth Vargas GonzalesNo ratings yet
- OB NotesDocument34 pagesOB NotesJillKellyNo ratings yet
- Patofizyoloji Based Management of PPHTDocument20 pagesPatofizyoloji Based Management of PPHTFunda TüzünNo ratings yet
- DDDDDocument58 pagesDDDDMARK JASON DIAZNo ratings yet