Professional Documents
Culture Documents
10 1001@jamaoncol 2019 0695
10 1001@jamaoncol 2019 0695
Uploaded by
Tantri SyahtiraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1001@jamaoncol 2019 0695
10 1001@jamaoncol 2019 0695
Uploaded by
Tantri SyahtiraCopyright:
Available Formats
Research
JAMA Oncology | Original Investigation
Body Composition and Cardiovascular Events
in Patients With Colorectal Cancer
A Population-Based Retrospective Cohort Study
Justin C. Brown, PhD; Bette J. Caan, DrPH; Carla M. Prado, PhD; Erin Weltzien, BA; Jingjie Xiao, PhD;
Elizabeth M. Cespedes Feliciano, ScD; Candyce H. Kroenke, ScD; Jeffrey A. Meyerhardt, MD
Invited Commentary
IMPORTANCE Patients with colorectal cancer (CRC) are up to 4-fold more likely than Supplemental content
individuals without a history of cancer to develop cardiovascular disease. Clinical care
guidelines recommend that physicians counsel patients with CRC regarding the association
between obesity (defined using body mass index [BMI] calculated as weight in kilograms
divided by height in meters squared) and cardiovascular disease risk; however, this
recommendation is based on expert opinion.
OBJECTIVE To determine which measures of body composition are associated with major
adverse cardiovascular events (MACEs) in patients with CRC.
DESIGN, SETTING, AND PARTICIPANTS Population-based retrospective cohort study of 2839
patients with stage I to III CRC diagnosed between January 2006 and December 2011 at an
integrated health care system in North America.
EXPOSURES The primary exposures were BMI and computed tomography–derived body
composition measurements (eg, adipose tissue compartments and muscle characteristics)
obtained at the diagnosis of CRC.
MAIN OUTCOMES AND MEASURES The primary outcome was time to the first occurrence of
MACE after diagnosis of CRC, including myocardial infarction, stroke, and cardiovascular
death.
RESULTS In this population-based cohort study of 2839 participants with CRC (1384 men and
1455 women), the average age (SD) was 61.9 (11.5) years (range, 19-80 years). A substantial
number of patients were former (1127; 40%) or current smokers (340; 12%), with
hypertension (1150; 55%), hyperlipidemia (1389; 49%), and type 2 diabetes (573; 20%).
The cumulative incidence of MACE 10 years after diagnosis of CRC was 19.1%. Body mass
index was positively correlated with some computed tomography-derived measures of body
composition. However, BMI was not associated with MACE; contrasting BMI categories of
greater than or equal to 35 vs 18.5 to 24.9, the hazard ratio (HR) was 1.23 (95% CI, 0.85-1.77;
P = .50 for trend). Visceral adipose tissue area was associated with MACE; contrasting the
highest vs lowest quintile, the HR was 1.54 (95% CI, 1.02-2.31; P = .04 for trend).
Subcutaneous adipose tissue area was not associated with MACE; contrasting the highest vs Author Affiliations: Pennington
Biomedical Research Center, Baton
lowest quintile, the HR was 1.15 (95% CI, 0.78-1.69; P = .65 for trend). Muscle mass was not Rouge, Louisiana (Brown); Stanley S.
associated with MACE; contrasting the highest vs lowest quintile, the HR was 0.96 (95% CI, Scott Cancer Center, Louisiana State
0.57-1.61; P = .92 for trend). Muscle radiodensity was associated with MACE; contrasting the University Health Sciences Center,
New Orleans (Brown); Kaiser
highest (ie, less lipid stored in the muscle) vs lowest quintile, the HR was 0.67 (95% CI,
Permanente Northern California,
0.44-1.03; P = .02 for trend). Oakland (Caan, Weltzien, Cespedes
Feliciano, Kroenke); University of
CONCLUSIONS AND RELEVANCE Visceral adiposity and muscle radiodensity appear to be risk Alberta, Edmonton, Alberta, Canada
(Prado, Xiao); Dana-Farber Cancer
factors for MACE. Body mass index may have limited use for determining cardiovascular risk Institute, Boston, Massachusetts
in this patient population. (Meyerhardt).
Corresponding Author: Justin C.
Brown, PhD, Pennington Biomedical
Research Center, 6400 Perkins Rd,
JAMA Oncol. doi:10.1001/jamaoncol.2019.0695 Baton Rouge, LA 70808 (justin.
Published online May 16, 2019. brown@pbrc.edu).
(Reprinted) E1
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 05/16/2019
Research Original Investigation Body Composition and Cardiovascular Events in Patients With Colorectal Cancer
C
olorectal cancer (CRC) is the fourth most common ma-
lignant neoplasm in the United States.1 Five-year sur- Key Points
vival for patients with CRC has increased by 33% over
Question Which measures of body composition are associated
the past 4 decades.2 Patients with CRC are now more suscep- with major adverse cardiovascular events in patients with
tible to competing causes of morbidity and mortality, such as colorectal cancer (CRC)?
those from cardiovascular disease (CVD).3,4 Patients with CRC
Findings In this population-based cohort study of 2839 patients
are 2-fold to 4-fold more likely than individuals without a his-
with CRC, body composition measured by visceral adiposity and
tory of cancer to develop CVD.5 Given the high risk of CVD in muscle radiodensity was associated with major adverse
patients with CRC, evidence is necessary to inform cardiovas- cardiovascular events, whereas body composition measured by
cular management in this susceptible population. body mass index was not associated with these events.
The American Cancer Society’s CRC survivorship care
Meaning Body composition measures collected using routine
guidelines recommend that physicians counsel patients with computed tomographic images, including visceral adiposity and
CRC regarding the association between obesity (defined using muscle radiodensity, can be used to assess cardiac risk in patients
body mass index [BMI], which is calculated as weight in kilo- with CRC; however, body mass index may have limited use for
grams divided by height in meters squared) and CVD risk, a rec- assessing cardiovascular risk in this patient population.
ommendation based exclusively on expert opinion.6 More-
over, uncertainty exists regarding the use of BMI for optimal review boards. Data analyses were performed from March 2018
cardiovascular risk management.7-9 At CRC diagnosis, pa- to September 2018.
tients undergo radiologic imaging with computed tomogra-
phy (CT) to characterize the disease stage. Using commer- Measures of Body Composition
cially available automated analysis methods, CT images can Height in meters and weight in kilograms were measured by
be used to quantify body composition, including visceral and medical assistants at the time of diagnosis. Body mass index
subcutaneous adiposity and muscle mass and radiodensity was calculated as weight in kilograms divided by height in me-
(a measure of lipid deposition into skeletal muscle).10 Quan- ters squared and categorized using the World Health Organi-
tification of body composition may improve prognostication zation classifications.12 Body composition was measured using
of overall and cancer-specific survival11; however, the incre- a single-slice transverse CT image of the third lumbar verte-
mental utility to guide CVD risk management is unknown. b r a a n d a n a l yze d w it h s l i c e O m at i c s o f t w a re V 5 .0
This study aimed to achieve 3 objectives using a popula- (TomoVision).13 Tissues were demarcated with a semiauto-
tion-based retrospective cohort of 2839 patients with CRC who mated procedure using Hounsfield unit thresholds of −29 to
were treated with curative intent. The first objective was to 150 for muscle, −150 to −50 for visceral adipose tissue, and −190
quantify the incidence of cardiovascular events up to 10 years to −30 for subcutaneous adipose tissue. Muscle radiodensity
after diagnosis of CRC. The second objective was to quantify quantifies the average radiation attenuation rate (in Houn-
the correlation between BMI and other measures of body com- sfield units) and is a radiologic measure of lipid deposition into
position. The third objective was to determine if specific BMI skeletal muscle.14 A randomly selected subsample of 50 CT im-
categories and CT-derived measures of body composition are ages were analyzed by 2 research staff members blinded to out-
risk factors for cardiovascular events independent of tradi- come (eFigure 1 in the Supplement), and the remaining CT im-
tional risk factors, including smoking, hypertension, hyper- ages were analyzed by a single trained research staff member
lipidemia, and type 2 diabetes. blinded to outcome.
Covariates
The KPNC EMR was used to obtain baseline information on age,
Methods
sex, self-reported race and ethnicity, and CVD risk factors, in-
Study Population and Design cluding smoking history, hypertension, hyperlipidemia, and
The Colorectal, Sarcopenia, Cancer And Near-term Survival type 2 diabetes.15 Cardiovascular disease risk factors were ob-
(C-SCANS) cohort was derived from the Kaiser Permanente tained using a 36-month lookback period from the time of CRC
Northern California (KPNC) cancer registry, with ascertain- diagnosis in the EMR. The KPNC cancer registry provided in-
ment of all patients aged 18 to 80 years who were diagnosed formation on the anatomical site of cancer, cancer stage, and
with stage I to III invasive CRC from 2006 to 2011 and under- the administration of chemotherapy and radiation. Covariate
went surgical resection for CRC (n = 4465). We excluded 693 data was 99.9% complete (2 missing observations for self-
patients without abdominal or pelvic CT images, 411 patients reported race and ethnicity and 3 missing observations for
without valid measures of body mass, 99 patients whose CT smoking history).
images were unreadable owing to poor image quality, and 423
patients who had a history of myocardial infarction or stroke Study Outcomes
documented in the electronic medical record (EMR) prior to The primary end point was defined as the time from cancer
CRC diagnosis. The final analytic sample included 2839 pa- diagnosis to the first occurrence of any component of the com-
tients. A waiver of written patient informed consent was ob- posite major adverse cardiovascular event (MACE) outcome,
tained by the study investigators, and this study was ap- including death from cardiovascular causes, nonfatal myocar-
proved by the KPNC and University of Alberta institutional dial infarction, or nonfatal stroke (3-component MACE). The
E2 JAMA Oncology Published online May 16, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 05/16/2019
Body Composition and Cardiovascular Events in Patients With Colorectal Cancer Original Investigation Research
3-component MACE is recommended by the US Food and Drug
Table 1. Baseline Characteristics of the Study Population
Administration for use in cardiovascular safety studies.16
Deaths were identified from the California State death regis- No. (%)a
Characteristic (n = 2839)
try, the National Death Index (using Social Security Adminis- Age, mean (SD), y 61.9 (11.5)
tration data), and KPNC electronic mortality files. Deaths were Sex
classified as cardiovascular specific if a cardiovascular cause
Male 1384 (49)
was documented as an underlying or contributing cause of
Female 1455 (51)
death on the death certificate through January 31, 2015. Vali-
Race/ethnicity
dated International Classification of Diseases codes were used
White 1828 (64)
to identify nonfatal myocardial infarction and nonfatal stroke
Black 201 (7)
in the EMR. 17,18 The end point event database was con-
Hispanic 320 (11)
structed by investigators blinded to BMI and body composi-
Asian and Pacific Islander 468 (17)
tion values.
Other 22 (1)
Cancer site
Statistical Analysis
Two time-to-event regression models were used to estimate Colon 1992 (70)
hazard ratios (HRs) and 95% CIs for each body composition Rectal 847 (30)
variable. The first regression model estimated the cause- Cancer stage
specific hazard using a Cox proportional hazards regression I 859 (30)
model. The cause-specific hazard is interpreted as the mag- II 891 (31)
nitude of the relative change in the instantaneous rate of the III 1089 (39)
occurrence of MACE in patients who are event free.19 The sec- Cancer treatment
ond regression model estimated the subdistribution hazard Chemotherapy 1501 (53)
using a Fine-Gray competing risk model.20 The subdistribu- Radiation 454 (16)
tion hazard is interpreted as the magnitude of relative change Smoking history
in the instantaneous rate of the occurrence of MACE in pa- Never 1389 (48)
tients who are event free or who have experienced a compet- Former 1127 (40)
ing event (eg, death from noncardiovascular causes, such as Current 340 (12)
CRC, which we previously reported is associated with body Cardiovascular risk factors
composition).21,22 Detailed comparisons of these 2 regres-
Hypertension 1150 (55)
sion models are described elsewhere.23,24 Contrasts were es-
Hyperlipidemia 1389 (49)
timated to test for trends across categories.
Type 2 diabetes 573 (20)
Covariates were chosen a priori and included age, sex, race,
Body composition measures, mean (SD)
ethnicity, cancer site, cancer stage, cancer treatment, smok-
Body mass, kg 80.8 (20.5)
ing history, hypertension, hyperlipidemia, and type 2 diabe-
Height, m 1.7 (0.1)
tes; analyses of CT-derived measures of body composition were
BMI 28.1 (6.0)
adjusted for patient height.25 One subgroup was specified a
Visceral adipose tissue area, cm2 151.7 (108.2)
priori, to test if sex modified any associations between BMI and
body composition with the risk of MACE. Effect modification Subcutaneous adipose tissue area, cm2 213.3 (121.2)
was examined by adding a statistical interaction term to the Muscle mass, cm2 140.5 (38.3)
regression model. Correlations between BMI and measures of Muscle radiodensity, HU 39.6 (9.8)
body composition were quantified using the Pearson correla- Abbreviations: BMI, body mass index (calculated as weight in kilograms divided
tion coefficient with 95% CI. by height in meters squared); HU, Hounsfield units.
a
Unless otherwise indicated, the number in parentheses is the percentage
of patients.
Results
Characteristics of the Study Cohort participants (12.9%). The cumulative incidence of MACE at 1,
Of 2839 participants, 1384 were men and 1455 were women 3, and 10 years after diagnosis was 3.4%, 5.9%, 19.1%, respec-
with an average (SD) age of 61.9 (11.5) years (range, 19-80 years). tively (Figure).
Many participants were former (n = 1127, 40%) or current smok-
ers (n = 340, 12%) and had hypertension (n = 1150, 55%), hy- Correlation Between BMI and Body Composition
perlipidemia (n = 1389, 49%), and type 2 diabetes (n = 573, Body mass index was positively correlated with visceral adi-
20%) (Table 1). pose tissue area (r = 0.61; 95% CI, 0.59-0.63), subcutaneous
Computed tomographic images were obtained at a adipose tissue area (r = 0.83; 95% CI, 0.82-0.85), and muscle
median of 6 days (interquartile range [IQR], 0-13) after results mass (r = 0.41; 95% CI, 0.38-0.44). Body mass index was nega-
of a biopsy confirmed diagnosis of CRC. By a median fol- tively correlated with muscle radiodensity (r = −0.33; 95% CI,
low-up of 6.8 years (IQR, 5.2- 8.3), MACE had occurred in 366 −0.37 to −0.30).
jamaoncology.com (Reprinted) JAMA Oncology Published online May 16, 2019 E3
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 05/16/2019
Research Original Investigation Body Composition and Cardiovascular Events in Patients With Colorectal Cancer
cantly associated with the risk of MACE whereas muscle
Figure. Cumulative Incidence Estimates of the Proportion of Participants
Experiencing a Major Adverse Cardiovascular Event
mass was not. These associations were independent of
other established cardiovascular risk factors, including
0.25 smoking, hypertension, hyperlipidemia, and type 2 diabe-
tes. Surprisingly, BMI was not associated with the risk of
MACE in this cohort.
Cumulative Incidence of MACE
0.20
Incident CRC and CVD share many risk factors, includ-
0.15 ing excess adiposity.26 Improvements in early cancer detec-
tion and chemotherapy efficacy have reduced the risk of
0.10
disease recurrence and cancer-specific mortality in CRC
survivors.27 However, the increasing burden of CVD in this
population may compromise improvements in overall
0.05
survival.28 Among 1966 Australian patients with CRC, the
3-year cumulative incidence of CVD after diagnosis of CRC
0
0 1 2 3 4 5 6 7 8 9 10 11 was 16%.29 Among 72 408 Medicare beneficiaries with CRC,
Time, y the 10-year cumulative incidence of CVD after diagnosis of
CRC was 57%.5 Physicians should be aware that patients
The solid line denotes the cumulative incidence function estimate accounting
diagnosed with CRC are not only at risk for cancer recur-
for competing risk. Shading around the line denotes the 95% CI. MACE
indicates major adverse cardiovascular event. rence but are at high risk of developing CVD at some point
during their survivorship trajectory. Furthermore, this CVD
risk is not described by BMI alone, and other body composi-
BMI, Body Composition, and Major Adverse tion measures should be considered to identify patients
Cardiovascular Events most in need of preventive cardiovascular care.
Body mass index was not associated with risk of MACE. For Visceral adipose tissue area and muscle radiodensity were
BMI categories greater than 35 vs 18.5 to 24.9, the HR was 1.23 identified as risk factors for MACE. The risk of MACE was higher
(95% CI, 0.85-1.77; P = .50 for trend) (Table 2). Contrasting the among patients in the highest quintile of visceral adiposity,
highest to lowest quintile of visceral adipose tissue area, the compared with those in the lowest quintile. These data are con-
multivariable-adjusted cause-specific HR for MACE was 1.54 sistent with observations that waist circumference (an anthro-
(95% CI, 1.02-2.31; P = .04 for trend) (eFigure 2 in the Supple- pometric proxy measure for visceral adipose tissue area) is in-
ment). Conversely, subcutaneous adipose tissue area was not dependently associated with CVD.30 A meta-analysis of 15
associated with risk of MACE. Contrasting the highest vs the studies with 258 114 participants demonstrated that each 1-cm
lowest quintile, the HR for MACE was 1.15 (95% CI, 0.78-1.69; increase in waist circumference increased the risk of a CVD
P = .65 for trend). Muscle mass was not associated with risk event by 2%.31
of MACE; comparing the highest vs lowest quintile, the HR for The risk of MACE was lower among patients in the high-
MACE was 0.96 (95% CI, 0.57-1.61; P = .92 for trend). Contrast- est quintile of muscle radiodensity (ie, less lipid stored in the
ing the highest (eg, less lipid stored in the muscle) to lowest skeletal muscle), compared with those in the lowest quintile.
quintile of muscle radiodensity, the multivariable-adjusted The exact mechanisms linking muscle radiodensity to MACE
cause-specific HR for MACE was 0.67 (95% CI, 0.44-1.03; are not clear. Muscle is an ectopic adiposity depot, and the ac-
P = .02 for trend). Sex did not modify the association be- cumulation of adiposity within skeletal muscle alters whole-
tween any body composition measure and risk of MACE body metabolism, manifesting in insulin resistance,14 im-
(results not shown). Effect estimates did not meaningfully dif- paired glucose tolerance, and type 2 diabetes.32 In addition,
fer when body composition measures were analyzed in their intermuscular adiposity is positively associated with a vari-
continuous form (eTable 1 and eFigure 3 in the Supplement), ety of proinflammatory mediators that are associated with CVD
when body composition measures were additionally risk, such as C-reactive protein, interleukin-6, and tumor ne-
adjusted for BMI (eTable 2 in the Supplement), or in a variety crosis factor.33 Further research is necessary to better under-
of sensitivity analyses (eTables 3-6 and eFigure 4 in the stand the mechanisms linking muscle radiodensity to MACE.
Supplement). In CRC survivors, we found no association between BMI
and the risk of MACE. Uncertainty exists regarding the use of
BMI as the optimal measure for c ardiovascular risk
stratification.34 In a nationally representative sample of 13 601
Discussion adults, obesity defined as a BMI category of 30 or more had a
In this population-based cohort, 1 of 5 patients experienced high sensitivity (≥95%) but poor specificity (36%-49%) in iden-
MACE within 10 years after CRC diagnosis. Visceral adipos- tification of obesity defined using percent body fat with bio-
ity but not subcutaneous adiposity was statistically signifi- electric impedance analysis.9 A meta-analysis of 10 studies
cantly associated with the risk of MACE. To our knowledge, demonstrated that anthropometric measures of visceral adi-
we are among the first to study muscle mass and muscle posity are superior to BMI in identifying cardiovascular risk fac-
radiodensity in relation to MACE in CRC; of these muscle tors, including hyperlipidemia, hypertension, and type 2
characteristics, muscle radiodensity was statistically signifi- diabetes.8
E4 JAMA Oncology Published online May 16, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 05/16/2019
Body Composition and Cardiovascular Events in Patients With Colorectal Cancer Original Investigation Research
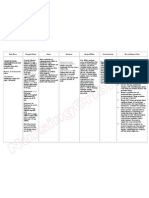
Table 2. Association Between Categorical Measures of Body Composition and Major Adverse Cardiovascular Events
P Value
for
Measure Body Composition Measurement Category Trend
BMI <18.5 18.5-24.9 25.0-29.9 30.0-34.9 ≥35.0
Mean (SD), kg/m2 17.3 (1.0) 22.5 (1.7) 27.3 (1.4) 32.2 (1.4) 40.0 (4.3)
No. events/No. at risk 4/52 114/888 133/1,016 68/551 47/332
Cause-specific hazard model,a 0.64 (0.23-1.74) 1 [Reference] 0.98 (0.76-1.27) 0.89 (0.65-1.22) 1.23 (0.85-1.77) .50
HR (95% CI)
Subdistribution hazard model,a 0.53 (0.19-1.53) 1 [Reference] 1.01 (0.78-1.31) 0.90 (0.65-1.24) 1.18 (0.81-1.71) .54
HR (95% CI)
Visceral Adipose Tissue Area, cm2 <53.9 53.9-106.2 106.3-163.6 163.7-238.0 ≥238.1
Mean (SD), cm2 26.0 (15.5) 79.2 (15.4) 135.0 (16.4) 199.1 (20.8) 319.7 (74.5)
No. events/No. at risk 41/568 62/570 72/566 83/568 108/567
Cause-specific hazard model,a 1 [Reference] 1.25 (0.84-1.86) 1.42 (0.96-2.10) 1.50 (1.01-2.23) 1.54 (1.02-2.31) .04
HR (95% CI)
Subdistribution hazard model,a 1 [Reference] 1.30 (0.87-1.94) 1.48 (1.00-2.21) 1.57 (1.05-2.35) 1.59 (1.06-2.40) .02
HR (95% CI)
Subcutaneous Adipose Tissue <117.3 117.4-163.0 163.1-214.1 214.2-294.9 ≥295.0
Area, cm2
Mean (SD), cm2 82.7 (26.9) 141.1 (13.1) 186.2 (14.9) 250.4 (23.8) 406.6 (101.1)
No. events/No. at risk 65/568 85/568 81/568 73/569 62/566
Cause-specific hazard model,a 1 [Reference] 1.21 (0.87-1.68) 1.20 (0.86-1.68) 1.12 (0.79-1.58) 1.15 (0.78-1.69) .65
HR (95% CI)
Subdistribution hazard model,a 1 [Reference] 1.28 (0.92-1.78) 1.26 (0.90-1.78) 1.16 (0.81-1.65) 1.16 (0.78-1.73) .65
HR (95% CI)
Muscle Mass, cm2 <105.3 105.4-123.9 124.0-147.8 147.9-174.6 ≥174.7
Mean (SD), cm2 93.6 (8.8) 114.1 (5.3) 135.3 (7.0) 161.1 (7.4) 198.8 (20.1)
No. events/No. at risk 79/570 63/566 71/568 80/571 73/564
Cause-specific hazard model,a 1 [Reference] 0.88 (0.63-1.25) 0.81 (0.54-1.20) 0.85 (0.53-1.35) 0.96 (0.57-1.61) .92
HR (95% CI)
Subdistribution hazard model,a 1 [Reference] 0.90 (0.63-1.27) 0.88 (0.60-1.30) 0.89 (0.56-1.43) 1.03 (0.62-1.73) .88
HR (95% CI)
Muscle Radiodensity, HU <31.5 31.5-37.5 37.6-42.5 42.6-48.0 ≥48.1
Mean (SD), HU 25.4 (4.9) 34.6 (1.7) 40.1 (1.5) 45.1 (1.6) 52.8 (4.3)
No. events/No. at risk 130/569 84/568 62/567 54/568 36/567
Cause-specific hazard model,a 1 [Reference] 0.68 (0.51-0.90) 0.58 (0.42-0.80) 0.68 (0.48-0.97) 0.67 (0.44-1.03) .02
HR (95% CI)
Subdistribution hazard model,a 1 [Reference] 0.71 (0.54-0.95) 0.61 (0.44-0.85) 0.72 (0.51-1.02) 0.70 (0.45-1.08) .04
HR (95% CI)
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided radiation, smoking history, hyperlipidemia, hypertension, type 2 diabetes, and
by height in meters squared); HR, hazard ratio; HU, Hounsfield units. height (the analysis of body mass index did not include height as a covariate).
a
Models are adjusted for age, sex, race/ethnicity, cancer stage, chemotherapy,
Limitations sue volume or changes in this volume are associated with
The main limitation of this study is the observational cardiovascular risk.
design, which precludes our ability to rule out residual con-
founding. The data used in our analysis were collected for
clinical care purposes. The reliance of this study on admin-
istrative codes within the EMR precluded our ability to
Conclusions
obtain information on patient behaviors such as physical Because patients with CRC are at a higher risk of developing CVD
activity, dietary patterns, and other behaviors or health con- than the general population, physicians may wish to refine car-
ditions that may influence body composition and the risk of diovascular risk management by integrating quantitative mea-
MACE. The measurement of physical activity was adopted sures of body composition that can be derived automatically from
across the KPNC health care system beginning in October CT scans that are routinely obtained during CRC diagnosis. This
2009. 35 Consequently, only 230 (8%) of our cohort had precision prevention approach to cardiovascular risk manage-
physical activity measures available at the time of CRC diag- ment may help to cost-effectively allocate limited resources such
nosis. Moreover, using administrative codes for the identifi- as dietary and physical activity counseling to patients who may
cation of CVD risk factors has high specificity (>0.95), but be most likely to benefit from lifestyle counseling. Our findings
low sensitivity (<0.76) compared with manual medical rec- suggest that body composition measures that are collected using
ord review.36 Measures of body composition were obtained routine CT images, including visceral adiposity and muscle ra-
at the third lumbar vertebrae at a solitary time point. diodensity, can be used to assess risk for MACEs in patients with
Although this anatomical region is correlated with whole- CRC, whereas BMI may have limited use for determining cardio-
body tissue volumes,13 it is not known how whole-body tis- vascular risk in this patient population.
jamaoncology.com (Reprinted) JAMA Oncology Published online May 16, 2019 E5
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 05/16/2019
Research Original Investigation Body Composition and Cardiovascular Events in Patients With Colorectal Cancer
ARTICLE INFORMATION 7. Kim SH, Després JP, Koh KK. Obesity and cardiovas- 23. Austin PC, Lee DS, Fine JP. Introduction to the
Accepted for Publication: February 11, 2019. cular disease: friend or foe? Eur Heart J. 2016;37(48): analysis of survival data in the presence of competing
Published Online: May 16, 2019. 3560-3568. doi:10.1093/eurheartj/ehv509 risks. Circulation. 2016;133(6):601-609. doi:10.1161/
doi:10.1001/jamaoncol.2019.0695 8. Lee CMY, Huxley RR, Wildman RP, Woodward M. CIRCULATIONAHA.115.017719
Author Contributions: Drs Brown and Weltzien had Indices of abdominal obesity are better discriminators 24. Dignam JJ, Zhang Q, Kocherginsky M. The use
full access to all the data in the study and take respon- of cardiovascular risk factors than BMI: a meta- and interpretation of competing risks regression
sibility for the integrity of the data and accuracy of the analysis. J Clin Epidemiol. 2008;61(7):646-653. doi: models. Clin Cancer Res. 2012;18(8):2301-2308. doi:
data analysis. 10.1016/j.jclinepi.2007.08.012 10.1158/1078-0432.CCR-11-2097
Study concept and design: Brown, Caan, Prado, 9. Romero-Corral A, Somers VK, Sierra-Johnson J, 25. Kronmal RA. Spurious correlation and the fallacy
Cespedes Feliciano, Kroenke. et al. Accuracy of body mass index in diagnosing of the ratio standard revisited. J R Stat Soc Ser A Stat
Acquisition, analysis, or interpretation of data: obesity in the adult general population. Int J Obes Soc. 1993;156(3):379-392. doi:10.2307/2983064
All authors. (Lond). 2008;32(6):959-966. doi:10.1038/ 26. Koene RJ, Prizment AE, Blaes A, Konety SH.
Drafting of the manuscript: Brown, Cespedes ijo.2008.11 Shared risk factors in cardiovascular disease and can-
Feliciano, Kroenke, Meyerhardt. 10. Prado CM, Heymsfield SB. Lean tissue imaging: cer. Circulation. 2016;133(11):1104-1114. doi:10.1161/
Critical revision of the manuscript for important a new era for nutritional assessment and intervention. CIRCULATIONAHA.115.020406
intellectual content: All authors. JPEN J Parenter Enteral Nutr. 2014;38(8):940-953. 27. Shi Q, Andre T, Grothey A, et al. Comparison of
Statistical analysis: Brown, Weltzien, Cespedes doi:10.1177/0148607114550189 outcomes after fluorouracil-based adjuvant therapy
Feliciano, Kroenke. for stages II and III colon cancer between 1978 to
11. Brown JC, Cespedes Feliciano EM, Caan BJ.
Obtained funding: Brown, Caan, Prado. 1995 and 1996 to 2007: evidence of stage migration
The evolution of body composition in oncology-
Administrative, technical, or material support: from the ACCENT database. J Clin Oncol. 2013;31
epidemiology, clinical trials, and the future of patient
Brown, Caan, Cespedes Feliciano. (29):3656-3663. doi:10.1200/JCO.2013.49.4344
care: facts and numbers. J Cachexia Sarcopenia Muscle.
Study supervision: Brown, Caan, Prado, 28. van Leersum NJ, Janssen-Heijnen ML, Wouters
2018;9(7):1200-1208. doi:10.1002/jcsm.12379
Meyerhardt. MW, et al. Increasing prevalence of comorbidity in
12. World Health Organization. Obesity: Preventing
patients with colorectal cancer in the South of the
Conflict of Interest Disclosures: Dr Brown reports and Managing the Global Epidemic. Geneva,
Netherlands 1995-2010. Int J Cancer. 2013;132(9):
grants from the National Cancer Institute (paid to his Switzerland: World Health Organization; 2000.
2157-2163. doi:10.1002/ijc.27871
institution). Dr Prado reports personal fees from Ab- 13. Shen W, Punyanitya M, Wang Z, et al. Total body
29. Hawkes AL, Lynch BM, Owen N, Aitken JF.
bott Nutrition outside the submitted work. skeletal muscle and adipose tissue volumes:
Lifestyle factors associated concurrently and
Dr Cespedes Feliciano reports grants from National estimation from a single abdominal cross-sectional
prospectively with co-morbid cardiovascular disease
Cancer Institute (K01-CA226155, R01CA175011) image. J Appl Physiol (1985). 2004;97(6):2333-2338.
in a population-based cohort of colorectal cancer
during the conduct of the study. No other disclosures doi:10.1152/japplphysiol.00744.2004
survivors. Eur J Cancer. 2011;47(2):267-276. doi:10.
were reported. 14. Aubrey J, Esfandiari N, Baracos VE, et al.
1016/j.ejca.2010.10.002
Funding/Support: Research reported in this publica- Measurement of skeletal muscle radiation attenua-
30. Pouliot MC, Després JP, Lemieux S, et al. Waist
tion was supported by the National Cancer Institute of tion and basis of its biological variation. Acta Physiol
circumference and abdominal sagittal diameter: best
the National Institutes of Health under award (Oxf). 2014;210(3):489-497. doi:10.1111/apha.12224
simple anthropometric indexes of abdominal visceral
numbers K99-CA218603, R01-CA175011, and R25- 15. Charlson M, Szatrowski TP, Peterson J, Gold J.
adipose tissue accumulation and related cardiovascu-
CA203650. Validation of a combined comorbidity index. J Clin
lar risk in men and women. Am J Cardiol. 1994;73(7):
Role of the Funder/Sponsor: The funder had no Epidemiol. 1994;47(11):1245-1251. doi:10.1016/0895-
460-468. doi:10.1016/0002-9149(94)90676-9
role in the design and conduct of the study; collection, 4356(94)90129-5
31. de Koning L, Merchant AT, Pogue J, Anand SS.
management, analysis, and interpretation of the data; 16. US Department of Health and Human Services,
Waist circumference and waist-to-hip ratio as
preparation, review, or approval of the manuscript; US Food and Drug Administration, Center for Drug
predictors of cardiovascular events: meta-regression
and decision to submit the manuscript for publication. Evaluation and Research. Guidance for industry:
analysis of prospective studies. Eur Heart J. 2007;28
Disclaimer: The content is solely the responsibility of diabetes mellitus—evaluating cardiovascular risk in
(7):850-856. doi:10.1093/eurheartj/ehm026
the authors and does not necessarily represent the new antidiabetic therapies to treat type 2 diabetes.
https://www.fda.gov/downloads/Drugs/Guidances/ 32. Goodpaster BH, Krishnaswami S, Resnick H, et al.
official views of the National Institutes of Health. Association between regional adipose tissue
ucm071627.pdf. Accessed April 2, 2019.
17. McCormick N, Bhole V, Lacaille D, Avina-Zubieta distribution and both type 2 diabetes and impaired
REFERENCES
JA. Validity of diagnostic codes for acute stroke in glucose tolerance in elderly men and women.
1. Siegel RL, Miller KD, Fedewa SA, et al. Colorectal
administrative databases: a systematic review. PLoS Diabetes Care. 2003;26(2):372-379. doi:10.2337/
cancer statistics, 2017. CA Cancer J Clin. 2017;67(3):
One. 2015;10(8):e0135834. doi:10.1371/journal.pone. diacare.26.2.372
177-193. doi:10.3322/caac.21395
0135834 33. Gustafson B, Smith U. Cytokines promote Wnt
2. Jemal A, Ward EM, Johnson CJ, et al. Annual report signaling and inflammation and impair the normal
to the nation on the status of cancer, 1975-2014, 18. McCormick N, Lacaille D, Bhole V, Avina-Zubieta
JA. Validity of myocardial infarction diagnoses in ad- differentiation and lipid accumulation in 3T3-L1
featuring survival. J Natl Cancer Inst. 2017;109(9). doi: preadipocytes. J Biol Chem. 2006;281(14):9507-9516.
10.1093/jnci/djx030 ministrative databases: a systematic review. PLoS One.
2014;9(3):e92286. doi:10.1371/journal.pone.0092286 doi:10.1074/jbc.M512077200
3. Baade PD, Fritschi L, Eakin EG. Non-cancer 34. Iliodromiti S, Celis-Morales CA, Lyall DM, et al.
19. Austin PC, Fine JP. Practical recommendations for
mortality among people diagnosed with cancer (Aus- The impact of confounding on the associations of
reporting Fine-Gray model analyses for competing
tralia). Cancer Causes Control. 2006;17(3):287-297. different adiposity measures with the incidence of
risk data. Stat Med. 2017;36(27):4391-4400. doi:10.
doi:10.1007/s10552-005-0530-0 cardiovascular disease: a cohort study of 296 535
1002/sim.7501
4. van Erning FN, van Steenbergen LN, Lemmens adults of white European descent. Eur Heart J. 2018;
20. Fine JP, Gray RJ. A proportional hazards model
VEPP, et al. Conditional survival for long-term 39(17):1514-1520. doi:10.1093/eurheartj/ehy057
for the subdistribution of a competing risk. J Am Stat
colorectal cancer survivors in the Netherlands: who 35. Coleman KJ, Ngor E, Reynolds K, et al. Initial
Assoc. 1999;94(446):496-509. doi:10.1080/
do best? Eur J Cancer. 2014;50(10):1731-1739. doi:10. validation of an exercise “vital sign” in electronic
01621459.1999.10474144
1016/j.ejca.2014.04.009 medical records. Med Sci Sports Exerc. 2012;44(11):
21. Caan BJ, Meyerhardt JA, Kroenke CH, et al.
5. Kenzik KM, Balentine C, Richman J, Kilgore M, Explaining the obesity paradox: the association 2071-2076. doi:10.1249/MSS.0b013e3182630ec1
Bhatia S, Williams GR. New-onset cardiovascular mor- between body composition and colorectal cancer 36. Birman-Deych E, Waterman AD, Yan Y, Nilasena
bidity in older adults with stage I to III colorectal can- survival. Cancer Epidemiol Biomarkers Prev. 2017;26 DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM
cer. J Clin Oncol. 2018;36(6):609-616. doi:10.1200/ (7):1008-1015. doi:10.1158/1055-9965.EPI-17-0200 codes for identifying cardiovascular and stroke risk
JCO.2017.74.9739 factors. Med Care. 2005;43(5):480-485. doi:10.1097/
22. Kroenke CH, Prado CM, Meyerhardt JA, et al.
6. El-Shami K, Oeffinger KC, Erb NL, et al. American 01.mlr.0000160417.39497.a9
Muscle radiodensity and mortality in patients with
Cancer Society colorectal cancer survivorship care colorectal cancer. Cancer. 2018;124(14):3008-3015.
guidelines. CA Cancer J Clin. 2015;65(6):428-455. doi: doi:10.1002/cncr.31405
10.3322/caac.21286
E6 JAMA Oncology Published online May 16, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 05/16/2019
You might also like
- 10 Qualities of An Effective Clinical PsychologistDocument6 pages10 Qualities of An Effective Clinical PsychologistShareena M R. Epres100% (2)
- CKD Case StudyDocument16 pagesCKD Case StudyLynne Cisquette100% (1)
- 10 1016@j Jaccao 2020 04 007Document10 pages10 1016@j Jaccao 2020 04 007ramangNo ratings yet
- The Joint Association of Fitness and Fatness On Cardiovascular Disease Mortality A Meta-AnalysisDocument27 pagesThe Joint Association of Fitness and Fatness On Cardiovascular Disease Mortality A Meta-AnalysisC F Morales OlearteNo ratings yet
- General Medicine: Open AccessDocument6 pagesGeneral Medicine: Open AccesssnNo ratings yet
- Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million AdultsDocument10 pagesAssociation of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million AdultsOscar DorantesNo ratings yet
- Jamaoncology Liu 2018 Oi 180081Document8 pagesJamaoncology Liu 2018 Oi 180081Bram KNo ratings yet
- Triple H NegativeDocument9 pagesTriple H NegativesamanNo ratings yet
- Aizer, Marital, Survival CancerDocument8 pagesAizer, Marital, Survival CancerFitri SetyawatiNo ratings yet
- Obesity and The Risk of Papillary Thyroid Cancer: A Pooled Analysis of Three Case-Control StudiesDocument9 pagesObesity and The Risk of Papillary Thyroid Cancer: A Pooled Analysis of Three Case-Control StudiesImam SuryaNo ratings yet
- Ioi70171 2461 2468Document8 pagesIoi70171 2461 2468jimmyneutron1337No ratings yet
- Genetic Risk, Adherence To A Healthy Lifestyle, and Coronary DiseaseDocument10 pagesGenetic Risk, Adherence To A Healthy Lifestyle, and Coronary DiseaseNurul Falah KalokoNo ratings yet
- Association Between Benign Thyroid Disease and Breast Cancer: A Single Center ExperienceDocument8 pagesAssociation Between Benign Thyroid Disease and Breast Cancer: A Single Center ExperiencelolaNo ratings yet
- Breast Cancer Subtype Distribution Is Different in Normal Weight, Overweight, and Obese WomenDocument7 pagesBreast Cancer Subtype Distribution Is Different in Normal Weight, Overweight, and Obese WomenValir HusleNo ratings yet
- Non Exercise Estimated Cardiorespiratory Fitness and All Cause Mortality in Cancer PatientsDocument7 pagesNon Exercise Estimated Cardiorespiratory Fitness and All Cause Mortality in Cancer PatientsAthenaeum Scientific PublishersNo ratings yet
- Tradução 3Document12 pagesTradução 3Ana AlineNo ratings yet
- Published EditionDocument10 pagesPublished EditionJames Dennis100% (2)
- 2016 Bradshaw Cardiovascular Disease Mortality Among BrCaDocument16 pages2016 Bradshaw Cardiovascular Disease Mortality Among BrCaAngélica Fernández PérezNo ratings yet
- ADN de Células Libres y Prevención de CA Colorectal. Estudio ECLIPSE. Chung. N Engl J Med 2024 390 973-83Document11 pagesADN de Células Libres y Prevención de CA Colorectal. Estudio ECLIPSE. Chung. N Engl J Med 2024 390 973-83ronaldNo ratings yet
- Warren 2016Document10 pagesWarren 2016Dwi AryanataNo ratings yet
- NIH Public AccessDocument10 pagesNIH Public AccessismuNo ratings yet
- Breast Cancer Screening Final Evidence SummaryDocument16 pagesBreast Cancer Screening Final Evidence SummaryzekeaispuroNo ratings yet
- Early Life Body Fatness and Risk of Colon CancerDocument17 pagesEarly Life Body Fatness and Risk of Colon CancerNilufar K.No ratings yet
- Rehabilitacion CardiacaDocument7 pagesRehabilitacion CardiacaAdrianGentileNo ratings yet
- Jama Usa TrendsDocument9 pagesJama Usa Trendsbrenda.rodriguezNo ratings yet
- J Jacc 2023 01 027Document11 pagesJ Jacc 2023 01 027ERIK EDUARDO BRICEÑO GÓMEZNo ratings yet
- Genética Clínica 2Document10 pagesGenética Clínica 2Victor MarquesNo ratings yet
- Magura HypercholesterolemiaProstateCancer 2008Document9 pagesMagura HypercholesterolemiaProstateCancer 2008zulfandana3No ratings yet
- Letters To The Editor: Association Between Recreational Cannabis Use and Cardiac Structure and FunctionDocument3 pagesLetters To The Editor: Association Between Recreational Cannabis Use and Cardiac Structure and Functionzionluis007No ratings yet
- 1 s2.0 S107814391500349X MainDocument7 pages1 s2.0 S107814391500349X Maintri1994No ratings yet
- Lack of Effect of Long-Term Supplementation With Beta Carotene On The Incidence of Malignant Neoplasms and Cardiovascular DiseaseDocument5 pagesLack of Effect of Long-Term Supplementation With Beta Carotene On The Incidence of Malignant Neoplasms and Cardiovascular DiseaseraisaNo ratings yet
- Primary Female Breast Sarcoma: Clinicopathological Features, Treatment and PrognosisDocument9 pagesPrimary Female Breast Sarcoma: Clinicopathological Features, Treatment and PrognosisSupriya PonsinghNo ratings yet
- 2074WJMH - WJMH 39 506Document10 pages2074WJMH - WJMH 39 506MSNo ratings yet
- Primary Female Breast Sarcoma Clinicopathological Features, Treatment and PrognosisDocument9 pagesPrimary Female Breast Sarcoma Clinicopathological Features, Treatment and PrognosisFrancesca Elize GuintoNo ratings yet
- 00006Document6 pages00006carlangaslaraNo ratings yet
- Dietary in Ammatory Potential and Risk of Cardiovascular Disease Among Men and Women in The U.SDocument13 pagesDietary in Ammatory Potential and Risk of Cardiovascular Disease Among Men and Women in The U.SRoxana CristeaNo ratings yet
- Relation Between Body Mass Index, Waist Circumference, and Death After Acute Myocardial InfarctionDocument10 pagesRelation Between Body Mass Index, Waist Circumference, and Death After Acute Myocardial InfarctionHydyrNo ratings yet
- Time To Initial Cancer Treatment in The United States and Association With Survival Over Time: An Observational StudyDocument15 pagesTime To Initial Cancer Treatment in The United States and Association With Survival Over Time: An Observational Studymrpaul giovaniNo ratings yet
- Midterm Second Activity (Journal) (Valdez Edmark, Moises) Bsn-4Document24 pagesMidterm Second Activity (Journal) (Valdez Edmark, Moises) Bsn-4Edmarkmoises ValdezNo ratings yet
- HCZ 186Document8 pagesHCZ 186charmantmayuwano4No ratings yet
- Metastasis Patterns and PrognoDocument17 pagesMetastasis Patterns and Prognosatria divaNo ratings yet
- Poorer Survival Outcomes For Male Breast Cancer Compared With Female Breast Cancer May Be Attributable To In-Stage MigrationDocument9 pagesPoorer Survival Outcomes For Male Breast Cancer Compared With Female Breast Cancer May Be Attributable To In-Stage MigrationabcdshNo ratings yet
- Triple Negative Breast Cancers: An Obsolete Entity?: ReviewDocument6 pagesTriple Negative Breast Cancers: An Obsolete Entity?: Reviewerikglu2796No ratings yet
- Cancer-Specific Survival Outcome in Early-Stage Young Breast Cancer: Evidence From The SEER Database AnalysisDocument10 pagesCancer-Specific Survival Outcome in Early-Stage Young Breast Cancer: Evidence From The SEER Database Analysismahmud.meftahNo ratings yet
- Weight Loss As A Predictor of Cancer in Primary Care A Systemati 2018Document12 pagesWeight Loss As A Predictor of Cancer in Primary Care A Systemati 2018devin mahendikaNo ratings yet
- Joc05039 1610 1616 PDFDocument7 pagesJoc05039 1610 1616 PDFDubster OneXNo ratings yet
- Geels 2000Document11 pagesGeels 2000NiaNo ratings yet
- Progression of Coronary Calcium and Incident Coronary Heart Disease EventsDocument9 pagesProgression of Coronary Calcium and Incident Coronary Heart Disease EventsJNo ratings yet
- Cardiac Radiation Dose Cardiac Disease and Mortlaity in Patients WTH Lung CancerDocument12 pagesCardiac Radiation Dose Cardiac Disease and Mortlaity in Patients WTH Lung Cancerromaana3540No ratings yet
- Left Sided Breast Cancer Is Associated With Aggressive Biology and Worse Outcomes Than Right Sided Breast CancerDocument9 pagesLeft Sided Breast Cancer Is Associated With Aggressive Biology and Worse Outcomes Than Right Sided Breast CancerMSNo ratings yet
- Canoy 2007Document11 pagesCanoy 2007Mariely PeñaNo ratings yet
- Nursing CourseDocument8 pagesNursing Coursepatel ravirajNo ratings yet
- ACR Lung-RADS v2022 Assessment Categories and Management RecommendationsDocument16 pagesACR Lung-RADS v2022 Assessment Categories and Management RecommendationsshokoNo ratings yet
- Features of Triple Negative Breast CancerDocument6 pagesFeatures of Triple Negative Breast CancermaleticjNo ratings yet
- Disparities in Outcomes Among Patients Diagnosed With Cancer in Proximity To An Emergency Department VisitDocument9 pagesDisparities in Outcomes Among Patients Diagnosed With Cancer in Proximity To An Emergency Department Visitevapruvost2No ratings yet
- 1101 FullDocument8 pages1101 FullAprilia R. PermatasariNo ratings yet
- Ioi80217 764 7730Document7 pagesIoi80217 764 7730kern tranhNo ratings yet
- The Predictive Value of Four Serum Biomarkers ForDocument8 pagesThe Predictive Value of Four Serum Biomarkers Forsebasags19No ratings yet
- HF 1Document14 pagesHF 1Galuh EkaNo ratings yet
- Rotter 2008Document6 pagesRotter 2008Benjamin SiglicNo ratings yet
- "Beat The Odds": Hugh D. Riordan, M.D., James A. Jackson, MT (ASCP) CLS, PH.D., and Ronald E. Hunninghake, M.DDocument2 pages"Beat The Odds": Hugh D. Riordan, M.D., James A. Jackson, MT (ASCP) CLS, PH.D., and Ronald E. Hunninghake, M.DFilipos ConstantinNo ratings yet
- Nutrisi SepsisDocument20 pagesNutrisi SepsisTantri SyahtiraNo ratings yet
- Fendo 09 00056Document7 pagesFendo 09 00056Tantri SyahtiraNo ratings yet
- Tiroid Heart DiseaseDocument23 pagesTiroid Heart DiseaseTantri SyahtiraNo ratings yet
- 10 1001@jamainternmed 2019 0392Document8 pages10 1001@jamainternmed 2019 0392Tantri SyahtiraNo ratings yet
- Ep171905 CRDocument6 pagesEp171905 CRTantri SyahtiraNo ratings yet
- Current Issues in Postoperative Pain Management PDFDocument12 pagesCurrent Issues in Postoperative Pain Management PDFikm fkunissulaNo ratings yet
- Ovarian CystsDocument29 pagesOvarian Cystspal_pal_palNo ratings yet
- Sewerage and Drainage EngineeringDocument3 pagesSewerage and Drainage EngineeringRenz PagcaliwaganNo ratings yet
- Rachel Carter Professional Disclosure StatementDocument5 pagesRachel Carter Professional Disclosure Statementapi-352566916No ratings yet
- EPM UK Workshop ManualDocument67 pagesEPM UK Workshop ManualMaisie RobertsNo ratings yet
- 08 PharmacoepidemiologyDocument61 pages08 PharmacoepidemiologyDrvinay Goud67% (3)
- Myasthenia Gravis. SURYADocument41 pagesMyasthenia Gravis. SURYANofilia Citra CandraNo ratings yet
- Anxiety Disorders: Treatment Considerations: Deborah Antai-Otong, MS, RN, CNS, NP, CS, FAANDocument10 pagesAnxiety Disorders: Treatment Considerations: Deborah Antai-Otong, MS, RN, CNS, NP, CS, FAANAmanda Marie Best OsbourneNo ratings yet
- CPG Management of Severe Childhood CariesDocument46 pagesCPG Management of Severe Childhood Cariesumiraihana1No ratings yet
- River BlindnessDocument3 pagesRiver BlindnessIlma Latansa100% (1)
- Uvr 03Document57 pagesUvr 03Shruti ShahNo ratings yet
- SteDis - HospWMDocument68 pagesSteDis - HospWMArvinth Guna SegaranNo ratings yet
- Rot 2 Darunday NCP Als 3Document10 pagesRot 2 Darunday NCP Als 3Ezra Miguel DarundayNo ratings yet
- Consent Hair TransplantationDocument4 pagesConsent Hair TransplantationKunda S100% (1)
- Concepts and Foundations of RehabilitationDocument13 pagesConcepts and Foundations of Rehabilitationamitesh_mpthNo ratings yet
- Morning Report: Chief ResidentsDocument35 pagesMorning Report: Chief ResidentsEssa Smj100% (1)
- Trimethoprim Sulfamethoxazole (TMP SMZ) Co TrimoxazoleDocument1 pageTrimethoprim Sulfamethoxazole (TMP SMZ) Co TrimoxazoleRenmico Aquino0% (1)
- Pilates: Jump To Navigation Jump To SearchDocument10 pagesPilates: Jump To Navigation Jump To SearchAsma HussainNo ratings yet
- NCP Depressive DisorderDocument3 pagesNCP Depressive Disorderluthercarl cachoNo ratings yet
- Clinical ToxicologyDocument6 pagesClinical ToxicologyGrace MarinoNo ratings yet
- Pharmacoepidemiology Pharmacoepidemiology At3: Studies Using Automated Databases GDocument27 pagesPharmacoepidemiology Pharmacoepidemiology At3: Studies Using Automated Databases GRuth Vargas GonzalesNo ratings yet
- 1B0DC46B-2D56-474B-81B5-AF1D9FA68F2FDocument2 pages1B0DC46B-2D56-474B-81B5-AF1D9FA68F2FJoelynMacalintalNo ratings yet
- ANEXO I ProvisionalDocument7 pagesANEXO I ProvisionalVidas probablesNo ratings yet
- Erythromycin: Bacteriostatic, Protein-Synthesis Inhibitors That Target RibosomeDocument3 pagesErythromycin: Bacteriostatic, Protein-Synthesis Inhibitors That Target RibosomeJubelle Sipalay100% (1)
- AIS Sports NutritionDocument3 pagesAIS Sports NutritionArnel VillasinNo ratings yet
- Testicular Torsion, Hydrocele & Fournier GangreneDocument41 pagesTesticular Torsion, Hydrocele & Fournier GangreneNur Insyirah100% (1)
- Patient Discharge Summary Form - 1390163 - 02-06-2022Document2 pagesPatient Discharge Summary Form - 1390163 - 02-06-2022ABHISHEK SINGHNo ratings yet
- Whocdscsreph200212 PDFDocument72 pagesWhocdscsreph200212 PDFIcaii InfotechNo ratings yet