Professional Documents
Culture Documents
Microhematuria Case Study: Medical Student Case-Based Learning
Microhematuria Case Study: Medical Student Case-Based Learning
Uploaded by
jenegne0 ratings0% found this document useful (0 votes)
5 views30 pagesA 75-year-old male presented with asymptomatic microhematuria and was found to have risk factors for urologic malignancy including age, smoking history, and weight loss. Imaging revealed a papillary lesion in the renal pelvis, and diagnostic ureteroscopy with biopsy demonstrated high-grade urothelial carcinoma. He underwent radical nephroureterectomy for treatment of upper tract urothelial carcinoma.
Original Description:
dufe
Original Title
NMSC-Microhematuria
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentA 75-year-old male presented with asymptomatic microhematuria and was found to have risk factors for urologic malignancy including age, smoking history, and weight loss. Imaging revealed a papillary lesion in the renal pelvis, and diagnostic ureteroscopy with biopsy demonstrated high-grade urothelial carcinoma. He underwent radical nephroureterectomy for treatment of upper tract urothelial carcinoma.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
5 views30 pagesMicrohematuria Case Study: Medical Student Case-Based Learning
Microhematuria Case Study: Medical Student Case-Based Learning
Uploaded by
jenegneA 75-year-old male presented with asymptomatic microhematuria and was found to have risk factors for urologic malignancy including age, smoking history, and weight loss. Imaging revealed a papillary lesion in the renal pelvis, and diagnostic ureteroscopy with biopsy demonstrated high-grade urothelial carcinoma. He underwent radical nephroureterectomy for treatment of upper tract urothelial carcinoma.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 30
Microhematuria Case Study
MEDICAL STUDENT CASE-
BASED LEARNING
Patient: Presentation
75-year-old Caucasian male referred for
asymptomatic (painless) microhematuria
What additional history would be
pertinent?
Patient: History & Physical Exam
• Denies gross hematuria, dysuria, irritative voiding symptoms, or difficulties
with urination
• No fevers, abdominal or flank pain
• Endorses 17 lb. weight loss over 10 months
• PMH: HTN. No prior GU history
• PSH: None
• Meds: Metoprolol, aspirin
• FHx: No known history of stones or malignancies
• SH: Retired veteran, 50 pack-year smoking history
• PE: No abdominal tenderness or distension, no costovertebral angle
tenderness bilaterally, normal phallus with orthotopic meatus
What is your differential diagnosis?
Differential Diagnosis
• Urolithiasis • UTI
• Malignancy • BPH
– Bladder cancer • Non-infectious cystitis
– Upper tract • Glomerulonephritis
urothelial carcinoma • Trauma
– Renal cell carcinoma • Strenuous exercise
What laboratory evaluation would be
appropriate?
Patient: Laboratory Evaluation
• Urinalysis: • Cr: 1.1
– Color: yellow
– SG: 1.015 • Hgb / Hct: 13.5 / 40.5
– pH: 5.5
– Nitrite: neg
– Leukocyte esterase: neg
– RBC: 3-5 / hpf (no RBC casts)
– WBC: 0-2 / hpf
– Protein: none
– Bacteria: none
– Squamous epithelial cells: none
Define microhematuria. How does this
differ from gross hematuria?
Types of Hematuria
Microhematuria Gross Hematuria
• >3 RBC/hpf on a single • Blood in the urine visible to
urinalysis the naked eye
• Not visible to the naked eye
Is a urine dipstick sufficient to
diagnose microhematuria?
No!
• Must obtain urinalysis with reflex microscopy to confirm
the presence of RBC’s
• False positives can occur with dipstick testing:
– Myoglobinuria
– Hemoglobinuria
– Povidone-iodine
• False negatives can also occur:
– Vitamin C ingestion
– Urine pH <5.1
– Prolonged exposure of dipstick to air prior to testing
What is the chance of malignancy in
the setting of hematuria?
Malignancy in Hematuria
• Likelihood of identifying malignancy depends
on type of hematuria:
– Microhematuria: 3-5% chance of malignancy
– Gross hematuria: 23% chance of malignancy
• Varies based on risk factors
What risk factors does the patient
have that would predispose him to
urologic malignancy?
Patient: Risk Factors/Clues for
Malignancy
• Older age
• Male gender
• History of cigarette smoking
• Weight loss
What would be your next step in
evaluating this patient’s hematuria?
Cystoscopy: Findings
• No urethral strictures
• Prostatic enlargement
• Orthotopic ureteral orifices with clear efflux of
urine bilaterally
• No abnormal lesions or tumors
• No active bleeding
• Cytology wash obtained: “atypical cells”
identified
Upper Tract Evaluation
• CT urography (CTU)
• What alternative modalities can be used to
evaluate the upper tracts (e.g. if Cr elevated or
patient allergic to iodine)?
– MR urography
– Retrograde pyelography with non-contrasted renal
imaging
Is the excretory phase really
necessary?
Can you see an abnormality (non-contrasted imaging)?
How about now (excretory phase)?
What would you do next?
Diagnostic Ureteroscopy
• Right-sided retrograde ureteroscopy was performed,
revealing large papillary-appearing protrusion into
the renal pelvis, which was biopsied
– Dx: high-grade urothelial carcinoma
• Tissue diagnosis can be obtained via retrograde or
antegrade ureteroscopy or via percutaneous
approaches if amenable
What is the incidence of upper tract
urothelial carcinoma (UTUC)?
What are some unique risk factors for
this disease?
UTUC
• Incidence: 2 new cases • Risk factors:
per 100,000 people – Tobacco use
– Cyclophosphamide exposure
• 5% of all urothelial – Phenacetin use
carcinomas – Aristolochic acid use
• Can occur in renal pelvis – Balkan nephropathy
– Lynch syndrome
or ureter
– Chronic inflammation
– History of bladder cancer
What is the surgical management of
non-metastatic UTUC?
Surgical Management
• Gold standard: radical nephroureterectomy
– Performed in index patient
• Nephron-sparing approaches: must be considered on
a case-by-case basis (e.g. tumor location,
multifocality, grade, renal function, comorbidities)
– Partial ureterectomy
– Endoscopic resection/fulguration
What principles are important in
surveillance of UTUC patients
following treatment?
Post-op Surveillance in UTUC
• Periodic cystoscopy
– Risk of metachronous bladder cancer: 22-47%
• Excretory urography of upper tracts (consider surveillance
ureteroscopies following nephron-sparing approaches)
– Risk of metachronous contralateral UTUC: 2-8%
• Monitor renal function
– After nephroureterectomy
– Following receipt of platinum-based chemotherapy
(nephrotoxic)
You might also like
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeFrom EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeNo ratings yet
- Addiction: The Process of AddictionDocument5 pagesAddiction: The Process of AddictionRaudel GlezNo ratings yet
- Disorders of PancreasDocument17 pagesDisorders of PancreasjonasNo ratings yet
- NMSC Gross HematuriaDocument41 pagesNMSC Gross HematuriaStoned PickleNo ratings yet
- UTUCDocument39 pagesUTUCShalini shreeNo ratings yet
- Eva Bolton Haematuria Presentation WebDocument52 pagesEva Bolton Haematuria Presentation WebereczkieNo ratings yet
- Hepatocellular Carcinoma and Other Hepatic MassesDocument59 pagesHepatocellular Carcinoma and Other Hepatic MassesIsaac MwangiNo ratings yet
- Prostate Cancer 111606Document31 pagesProstate Cancer 111606abd12medyNo ratings yet
- Hematuria: Ikobho A. DDocument28 pagesHematuria: Ikobho A. DPrincewill SeiyefaNo ratings yet
- HematuriaDocument15 pagesHematurianisaw_2No ratings yet
- TP Thyroid Nodules 1Document59 pagesTP Thyroid Nodules 1Meaw Thitirat SupasilNo ratings yet
- Cystic Diseases of The Kidney. Renal NeoplasmsDocument31 pagesCystic Diseases of The Kidney. Renal NeoplasmsFate ChanNo ratings yet
- Case Based Teaching - Urology: Haematuria & Renal TransplantDocument21 pagesCase Based Teaching - Urology: Haematuria & Renal Transplantamoody95No ratings yet
- The Paris System For Reporting Urinary CytopathologyDocument32 pagesThe Paris System For Reporting Urinary CytopathologyReymes BusterNo ratings yet
- Brad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Document36 pagesBrad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Cristian OrozcoNo ratings yet
- Testicular TumorsDocument35 pagesTesticular TumorsHafizur RashidNo ratings yet
- MS, Frcs (England), Frcs (Edinburgh), Frcs (Glasgow)Document52 pagesMS, Frcs (England), Frcs (Edinburgh), Frcs (Glasgow)Anis HospitalNo ratings yet
- Approach To Patient With Renal DiseaseDocument74 pagesApproach To Patient With Renal DiseaseSaja SaqerNo ratings yet
- Urology Sample Osce Exam e PDFDocument8 pagesUrology Sample Osce Exam e PDFLana LocoNo ratings yet
- Back To Basics - Urology - Dr. James Watterson 2009 - CompressedDocument171 pagesBack To Basics - Urology - Dr. James Watterson 2009 - CompressedDr Anais AsimNo ratings yet
- Evaluation and Management of HematuriaDocument26 pagesEvaluation and Management of Hematuriaoki777jxNo ratings yet
- Renal Cell Carcinoma: DR - Amit Gupta Associate Professor Dept. of SurgeryDocument20 pagesRenal Cell Carcinoma: DR - Amit Gupta Associate Professor Dept. of SurgeryvitelinductNo ratings yet
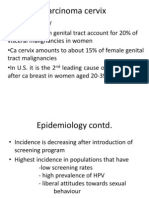
- Cervical CancerDocument36 pagesCervical CancerPro fatherNo ratings yet
- Hepatocellular CarcinomaDocument62 pagesHepatocellular CarcinomaWilliams Emmanuel AdeyeyeNo ratings yet
- Abnormal Cervical SmearDocument63 pagesAbnormal Cervical SmearAkhmal SidekNo ratings yet
- Urological TumoursDocument68 pagesUrological TumoursDr Anais AsimNo ratings yet
- HematuriaDocument31 pagesHematuriaSiti Zainab Bani PurwanaNo ratings yet
- Benign Prostatic HyperplasiaDocument36 pagesBenign Prostatic Hyperplasiamomodou s jallowNo ratings yet
- Imaging of Acute PancreatitisDocument53 pagesImaging of Acute PancreatitisLazar VučetićNo ratings yet
- Common Bile Duct Stones StrictureDocument48 pagesCommon Bile Duct Stones StrictureSyarif MalawatNo ratings yet
- Faiza Hashim Soomro PG-Gen SurgeryDocument47 pagesFaiza Hashim Soomro PG-Gen SurgeryFaiza Hashim SoomroNo ratings yet
- Gall Bladder CarcinomaDocument29 pagesGall Bladder CarcinomaUsman FarooqNo ratings yet
- Urothelial Tumors of The Upper Urinary Tract FixDocument25 pagesUrothelial Tumors of The Upper Urinary Tract FixAgung IndraNo ratings yet
- Liver BiopsyDocument4 pagesLiver BiopsyLouis Fortunato100% (1)
- Guidelines For UrologyDocument91 pagesGuidelines For UrologyAruna HarikrishnanNo ratings yet
- Colon CancerDocument41 pagesColon Cancervaishali TayadeNo ratings yet
- Renal Cell CarcinomaDocument9 pagesRenal Cell CarcinomaFabb NelsonNo ratings yet
- Tumors of The Kidney and Urinary BladerDocument76 pagesTumors of The Kidney and Urinary BladerTaufik Gumilar WahyudinNo ratings yet
- Faculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractDocument40 pagesFaculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractGalina LozovanuNo ratings yet
- Urogenital Cancers: - Renal Cell Ca - Bladder Ca - Renal Pelvis & Ureter - BPH & Prostate CaDocument17 pagesUrogenital Cancers: - Renal Cell Ca - Bladder Ca - Renal Pelvis & Ureter - BPH & Prostate CaAli Husain Abdul KadirNo ratings yet
- Surg 2 JaundicedDocument94 pagesSurg 2 Jaundicedapi-3728522No ratings yet
- Ca CervixDocument48 pagesCa CervixRanjita BainsNo ratings yet
- Radiologi Edit-1Document50 pagesRadiologi Edit-1Resi OfzanNo ratings yet
- Prof. Ziv Ben-Ari Liver Institute Rabin Medical CenterDocument62 pagesProf. Ziv Ben-Ari Liver Institute Rabin Medical CenterLigia Ariana BancuNo ratings yet
- Case StudiesDocument6 pagesCase StudiesPatricia CruzNo ratings yet
- RadiologiDocument54 pagesRadiologiresi silviaNo ratings yet
- Carcinomagallbladder PDFDocument61 pagesCarcinomagallbladder PDFZaki DhiifNo ratings yet
- HEPATOMADocument30 pagesHEPATOMASemestaNo ratings yet
- Topic 10Document10 pagesTopic 1089qqzp4yhkNo ratings yet
- Approach To The Patient With Hematuria: Paul D. Simmons, MD St. Mary's Family Medicine Residency Grand JunctionDocument41 pagesApproach To The Patient With Hematuria: Paul D. Simmons, MD St. Mary's Family Medicine Residency Grand JunctionMichael Spica RampangileiNo ratings yet
- Pancreaticcancer 150917114601 Lva1 App6891Document30 pagesPancreaticcancer 150917114601 Lva1 App6891enam professorNo ratings yet
- 9 Urinary and Male GenitalDocument31 pages9 Urinary and Male GenitalFlavia CatalinaNo ratings yet
- Seminar On Tumor of Genito-Urinary SystemDocument33 pagesSeminar On Tumor of Genito-Urinary SystemLakshay AroraNo ratings yet
- Squamous Cell CarcinomaDocument53 pagesSquamous Cell CarcinomaWacky BlankNo ratings yet
- HematuriaDocument4 pagesHematuriaArian SuryaNo ratings yet
- Abdominaltraumaanoverview-171025062135 4Document75 pagesAbdominaltraumaanoverview-171025062135 4Ion AndreeaNo ratings yet
- Liver TraumaDocument7 pagesLiver TraumanouradreamNo ratings yet
- 11 Prostate CancerDocument52 pages11 Prostate Cancerclaire yowsNo ratings yet
- Thrombophilia: Duha Alharbi, MD InternDocument30 pagesThrombophilia: Duha Alharbi, MD InternabrarNo ratings yet
- Hello PandaDocument1 pageHello PandajenegneNo ratings yet
- Hshshhshsben SNDocument3 pagesHshshhshsben SNjenegneNo ratings yet
- GFGFGFDocument5 pagesGFGFGFjenegneNo ratings yet
- Measurements in Femoro-Acetabular Impingement: How To Doit?Document33 pagesMeasurements in Femoro-Acetabular Impingement: How To Doit?jenegneNo ratings yet
- Nutrients: Use of An Extract of Annona Muricata Linn To Prevent High-Fat Diet Induced Metabolic Disorders in C57BLDocument22 pagesNutrients: Use of An Extract of Annona Muricata Linn To Prevent High-Fat Diet Induced Metabolic Disorders in C57BLjenegneNo ratings yet
- Measurements in Femoro-Acetabular Impingement: How To Doit?Document33 pagesMeasurements in Femoro-Acetabular Impingement: How To Doit?jenegneNo ratings yet
- Banadoz ® Cefpodoxime: CompositionDocument5 pagesBanadoz ® Cefpodoxime: CompositionjenegneNo ratings yet
- Journal of Clinical and Basic Cardiology: WWW - Kup.at/jcbcDocument6 pagesJournal of Clinical and Basic Cardiology: WWW - Kup.at/jcbcjenegneNo ratings yet
- 9164 62159 1 PBDocument12 pages9164 62159 1 PBjenegneNo ratings yet
- Overview of Viral MyositisDocument3 pagesOverview of Viral MyositisemirkurtalicNo ratings yet
- None C9efb7c9Document6 pagesNone C9efb7c9liana iwiwNo ratings yet
- Homeopathy Research Evidence Base 7-12-2017 PDFDocument214 pagesHomeopathy Research Evidence Base 7-12-2017 PDFGanesh ganguly GMNo ratings yet
- Nurse Practitioner Nurse in Philadelphia PA Resume Deborah StallworthDocument2 pagesNurse Practitioner Nurse in Philadelphia PA Resume Deborah StallworthDeborah StallworthNo ratings yet
- Abdominal Aortic AneurysmDocument44 pagesAbdominal Aortic AneurysmAkhilMuraleedharan100% (2)
- Applicable For Third & Fourth Year Subject Homoeopathic Materia MedicaDocument16 pagesApplicable For Third & Fourth Year Subject Homoeopathic Materia MedicaRahul MaliNo ratings yet
- Prophasedx Laboratory Phone: (855) 982-1100Document2 pagesProphasedx Laboratory Phone: (855) 982-1100ommanon15 aNo ratings yet
- High Risk NewbornDocument68 pagesHigh Risk NewbornjeshemaNo ratings yet
- Granulomatous InflammationDocument96 pagesGranulomatous InflammationIvonne Trujillo TorbiscoNo ratings yet
- Editorial Intro DR Jessica Rose-The Lies Vaccinologists Tell Themselves - VAERS Receives Due ScrutinyDocument3 pagesEditorial Intro DR Jessica Rose-The Lies Vaccinologists Tell Themselves - VAERS Receives Due ScrutinySY LodhiNo ratings yet
- Cardiovascular Examination FinalDocument28 pagesCardiovascular Examination FinalAllen Caine Taabbil100% (1)
- ICD-10 PodiatryDocument25 pagesICD-10 PodiatryAnonymous kdBDppigENo ratings yet
- Study Data Reviewer's Guide: LDCP, Inc. Study LDCP-0242-005Document15 pagesStudy Data Reviewer's Guide: LDCP, Inc. Study LDCP-0242-005anon_181306460No ratings yet
- Chapter 109. Nursing ServicesDocument10 pagesChapter 109. Nursing ServicesTarun SoniNo ratings yet
- The Effects of Active Break and Postural Shift Interventions On Recovery FromDocument8 pagesThe Effects of Active Break and Postural Shift Interventions On Recovery FromNiko TrogerNo ratings yet
- Please Stand by ..: © Business & Legal Reports, Inc. 1110Document37 pagesPlease Stand by ..: © Business & Legal Reports, Inc. 1110Johanamhy PanergoNo ratings yet
- Bear Cub 750 - Quick User GuideDocument2 pagesBear Cub 750 - Quick User GuideSn DayanidhiNo ratings yet
- Allergy - 2022 - Kallieri - RELIght A Two Year REal LIfe Study of Mepolizumab in Patients With Severe Eosinophilic AsTHmaDocument5 pagesAllergy - 2022 - Kallieri - RELIght A Two Year REal LIfe Study of Mepolizumab in Patients With Severe Eosinophilic AsTHmaRamon RondoNo ratings yet
- Ped CardioDocument18 pagesPed CardioIdioness100% (1)
- Assessment of The AbdomenDocument6 pagesAssessment of The Abdomenmalyn1218No ratings yet
- Bed Site Teaching: Ridwan Permana (712014027) Preceptor: Dr. Rizal Daulay, SP - OT.,MARSDocument21 pagesBed Site Teaching: Ridwan Permana (712014027) Preceptor: Dr. Rizal Daulay, SP - OT.,MARSRidwan PermanaNo ratings yet
- Cefoxitin Drug StudyDocument3 pagesCefoxitin Drug StudyBea Dela Cena100% (2)
- Health Informatics Exam AnswersDocument8 pagesHealth Informatics Exam Answersnajib TibizukaNo ratings yet
- Module 1 - IS-PEFRDocument7 pagesModule 1 - IS-PEFRRenea Joy ArruejoNo ratings yet
- IPX066 (Rytary) : A New Medication For Parkinson's Disease, Robert A. Hauser MDDocument8 pagesIPX066 (Rytary) : A New Medication For Parkinson's Disease, Robert A. Hauser MDRobert A. Hauser, MDNo ratings yet
- System 5000 Electrosurgical Unit (ESU)Document4 pagesSystem 5000 Electrosurgical Unit (ESU)George VlNo ratings yet
- Management of Chronic Hepatitis B in AdultsDocument76 pagesManagement of Chronic Hepatitis B in AdultsLan AllemNo ratings yet
- Buscopan - Medicine To Treat Stomach Cramps and IBS - NHSDocument9 pagesBuscopan - Medicine To Treat Stomach Cramps and IBS - NHSAdityaWijayaNo ratings yet