Professional Documents
Culture Documents
Thalassemic Mothers and Their Babies: Abstract
Thalassemic Mothers and Their Babies: Abstract
Uploaded by
Wahyu PermataCopyright:
Available Formats
You might also like
- Practice Bulletin No 144 Multifetal Gestations .40Document15 pagesPractice Bulletin No 144 Multifetal Gestations .40Jose Luis Morales Bautista100% (1)
- CHN Action PlanDocument9 pagesCHN Action PlanseeyarahNo ratings yet
- CM FrancisDocument229 pagesCM FrancisDrHassan Ahmed Shaikh50% (2)
- Pregnancy in Patients With B-Thalassemia Intermedia: Outcome of Mothers and NewbornsDocument4 pagesPregnancy in Patients With B-Thalassemia Intermedia: Outcome of Mothers and NewbornsIlham RamadhanisNo ratings yet
- Beta-Thalassemia Major and Pregnancy: Clinical StudyDocument3 pagesBeta-Thalassemia Major and Pregnancy: Clinical StudyherryNo ratings yet
- Fetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaDocument4 pagesFetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaMuhammad AdithiaNo ratings yet
- FTP PDFDocument4 pagesFTP PDFIzat FuadiNo ratings yet
- Referensi No 7Document5 pagesReferensi No 7Bagus Wanda HabibullahNo ratings yet
- Gestational Diabetes Mellitus in Teenage Pregnancy: A Case-Control StudyDocument3 pagesGestational Diabetes Mellitus in Teenage Pregnancy: A Case-Control StudySarly FebrianaNo ratings yet
- Prenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromaDocument5 pagesPrenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromawitaNo ratings yet
- Maternal and Obstetric Outcome of Women With Epilepsy 2009 SeizureDocument4 pagesMaternal and Obstetric Outcome of Women With Epilepsy 2009 Seizurebilal hadiNo ratings yet
- Ijrm 9 009 PDFDocument6 pagesIjrm 9 009 PDFWahyu PermataNo ratings yet
- Hum. Reprod.-2004-Carp-191-5Document5 pagesHum. Reprod.-2004-Carp-191-5venkayammaNo ratings yet
- Anemia MaternityDocument5 pagesAnemia MaternityBonaventura Ahardiansyah BoNo ratings yet
- Ojsadmin, 276Document6 pagesOjsadmin, 276komalvaid5No ratings yet
- The Association of Early-Onset Fetal Growth Restriction, Elevated Maternal Serum Alpha-Fetoprotein, and The Development of Severe Pre-EclampsiaDocument6 pagesThe Association of Early-Onset Fetal Growth Restriction, Elevated Maternal Serum Alpha-Fetoprotein, and The Development of Severe Pre-EclampsiaM.RautNo ratings yet
- Outcome of Pregnancy in Patients With Liver CirrhosisDocument7 pagesOutcome of Pregnancy in Patients With Liver CirrhosisSamirAyadNo ratings yet
- Vol93 No.6 661 5058Document6 pagesVol93 No.6 661 5058Titi Afrida SariNo ratings yet
- Maternal and Perinatal Outcome in Antepartum HemorrhageDocument5 pagesMaternal and Perinatal Outcome in Antepartum HemorrhagebayukolorNo ratings yet
- Spectrum of Grand MultiparityDocument4 pagesSpectrum of Grand MultiparityYoser ThamtonoNo ratings yet
- CD HAS ThaiDocument9 pagesCD HAS ThaiAlexandre RochaNo ratings yet
- Effect of PIH On Mothers and Babies PDFDocument3 pagesEffect of PIH On Mothers and Babies PDFAbdifatah AhmedNo ratings yet
- 60d587530e3c120210625article - PDF - FileStudy of Maternal and Perinatal OutcomDocument4 pages60d587530e3c120210625article - PDF - FileStudy of Maternal and Perinatal Outcommade dharmaNo ratings yet
- J of Obstet and Gynaecol - 2012 - Aksornphusitaphong - Risk Factors of Early and Late Onset Pre EclampsiaDocument5 pagesJ of Obstet and Gynaecol - 2012 - Aksornphusitaphong - Risk Factors of Early and Late Onset Pre EclampsiaDefi SelvianitaNo ratings yet
- Materials and MethodsDocument1 pageMaterials and MethodsImtihanamiseNo ratings yet
- Gong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Document21 pagesGong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Clarithq LengguNo ratings yet
- Hard Arson 2008Document7 pagesHard Arson 2008elda zulkarnainNo ratings yet
- Jcem 2587Document5 pagesJcem 2587Midwifery D4unisaNo ratings yet
- Thrombocytopenia at Different Stages of PregnancyDocument3 pagesThrombocytopenia at Different Stages of PregnancyInternational Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalDocument6 pagesSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenNo ratings yet
- Diabetic Placenta: Ultrastructure and Morphometry of The Term VilliDocument9 pagesDiabetic Placenta: Ultrastructure and Morphometry of The Term VilliklapouschakNo ratings yet
- Hum. Reprod.-2008-Bellver-278-84Document7 pagesHum. Reprod.-2008-Bellver-278-84Grigoriu RaduNo ratings yet
- First Trimester (NT-NB Scan) - Inverting The Antenatal PyramidDocument21 pagesFirst Trimester (NT-NB Scan) - Inverting The Antenatal PyramidKalpavriksha1974No ratings yet
- Correlation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesDocument6 pagesCorrelation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesstephaniedianNo ratings yet
- Chapter 3Document32 pagesChapter 3Vaibhav JainNo ratings yet
- Gim 20047Document4 pagesGim 20047Sabhina AnseliaNo ratings yet
- 2017 Article 784Document5 pages2017 Article 784Elena ZepedaNo ratings yet
- 2851-26. 31 Rasheed Eclampsia-1625840448Document3 pages2851-26. 31 Rasheed Eclampsia-1625840448Umair HasanNo ratings yet
- Endocrinology & Metabolic SyndromeDocument13 pagesEndocrinology & Metabolic SyndromeMayra PereiraNo ratings yet
- Maternal Serum Triglycerides in Women With Pre-Eclampsia: Original ArticleDocument5 pagesMaternal Serum Triglycerides in Women With Pre-Eclampsia: Original ArticleGladys SusantyNo ratings yet
- Compare The Histological Features Between The Normal and Hypertensive PlacentaDocument7 pagesCompare The Histological Features Between The Normal and Hypertensive PlacentaKamran AmeerNo ratings yet
- 140 140 1 PBDocument4 pages140 140 1 PBMina LelymanNo ratings yet
- Hellp Indicacion DexametasonaDocument6 pagesHellp Indicacion DexametasonaEyran AlfredoNo ratings yet
- Risk Factors Associated With Fetal Pleural Effusion in Prenatal Diagnosis: A Retrospective Study in A Single Institute in Southern ChinaDocument6 pagesRisk Factors Associated With Fetal Pleural Effusion in Prenatal Diagnosis: A Retrospective Study in A Single Institute in Southern Chinachristian roblesNo ratings yet
- Hyperglycemia in Pregnant Ladies and Its Outcome Out in The Opd, Labor Ward, Gynecology and Obstetrics, Lady Atichison Hospital, LahoreDocument7 pagesHyperglycemia in Pregnant Ladies and Its Outcome Out in The Opd, Labor Ward, Gynecology and Obstetrics, Lady Atichison Hospital, LahoreiajpsNo ratings yet
- Embarazo MultipleDocument15 pagesEmbarazo MultipleLina E. ArangoNo ratings yet
- 1 PB PDFDocument7 pages1 PB PDFAmanda Mustika AdiNo ratings yet
- Comparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.Document54 pagesComparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.prasadNo ratings yet
- Am. J. Epidemiol. 2007 Holzman 786 94Document9 pagesAm. J. Epidemiol. 2007 Holzman 786 94Sri AgustinaNo ratings yet
- Anti-Toxoplasma: Incidence of Antibodies in Women With High-Risk Pregnancy and Habitual AbortionsDocument5 pagesAnti-Toxoplasma: Incidence of Antibodies in Women With High-Risk Pregnancy and Habitual AbortionsFerdina NidyasariNo ratings yet
- Hamil AnggurDocument7 pagesHamil AnggurIchunx MelissaNo ratings yet
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 pagesPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08No ratings yet
- EG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderDocument6 pagesEG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderElena VisterniceanNo ratings yet
- tmp647F TMPDocument13 pagestmp647F TMPFrontiersNo ratings yet
- Analytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsDocument5 pagesAnalytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsNurvita WidyastutiNo ratings yet
- Karakteristik Penderita Preeklamsi Dan Eklamsi Yang Dirawat Inap Di Rumah Sakit Immanuel Bandung Periode Tahun 2006 - 2008Document6 pagesKarakteristik Penderita Preeklamsi Dan Eklamsi Yang Dirawat Inap Di Rumah Sakit Immanuel Bandung Periode Tahun 2006 - 2008Radi PdNo ratings yet
- Neonatal Sepsis in Low Birth Weight Infants in Dr. Soetomo General HospitalDocument4 pagesNeonatal Sepsis in Low Birth Weight Infants in Dr. Soetomo General HospitalMelati Nurul UtamiNo ratings yet
- Prevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksDocument4 pagesPrevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksTriponiaNo ratings yet
- Morbidity and Mortality Amongst Infants of Diabetic Mothers Admitted Into Soba University Hospital Khartoum SudanDocument7 pagesMorbidity and Mortality Amongst Infants of Diabetic Mothers Admitted Into Soba University Hospital Khartoum SudanAde Gustina Siahaan100% (1)
- Detection of Chromosome Aberrations in TheDocument3 pagesDetection of Chromosome Aberrations in TheSonia Delgado EspinozaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyFrom EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Ijrm 9 009 PDFDocument6 pagesIjrm 9 009 PDFWahyu PermataNo ratings yet
- Thalassaemia Syndromes and PregnancyDocument8 pagesThalassaemia Syndromes and PregnancyWahyu PermataNo ratings yet
- Beta-Thalassemia Major and Pregnancy: September 2013Document4 pagesBeta-Thalassemia Major and Pregnancy: September 2013Wahyu PermataNo ratings yet
- Scanned by CamscannerDocument5 pagesScanned by CamscannerWahyu PermataNo ratings yet
- 2 PBDocument9 pages2 PBWahyu PermataNo ratings yet
- Katarak PDFDocument6 pagesKatarak PDFWahyu PermataNo ratings yet
- Myelopathy: Clinical Clerkship of Neurology DepartmentDocument59 pagesMyelopathy: Clinical Clerkship of Neurology DepartmentWahyu PermataNo ratings yet
- Case Report Saraf RevisiDocument21 pagesCase Report Saraf RevisiWahyu PermataNo ratings yet
- Has Treetr Suhe L1L, RSL$: R$ Iry.RDocument1 pageHas Treetr Suhe L1L, RSL$: R$ Iry.RWahyu PermataNo ratings yet
- Uneb Primary Leaving Examination 2023 Integrated Science Questions With Answers Section A and Section BDocument13 pagesUneb Primary Leaving Examination 2023 Integrated Science Questions With Answers Section A and Section Bmarvinrukundo1No ratings yet
- Anjani Ayuningtyas KD NIM: 18.1422.S (4B)Document4 pagesAnjani Ayuningtyas KD NIM: 18.1422.S (4B)dilan mileaNo ratings yet
- Periodicity DentalGuideDocument52 pagesPeriodicity DentalGuideSalam BataienehNo ratings yet
- Abdominal Pain A Synthesis of Recommendations ForDocument11 pagesAbdominal Pain A Synthesis of Recommendations Forsakinah mawadahNo ratings yet
- Contract Proposal 6.23.17Document1 pageContract Proposal 6.23.17Ann DwyerNo ratings yet
- Jurnal Senam Hamil PDFDocument4 pagesJurnal Senam Hamil PDFrina astutiNo ratings yet
- Pilot Study FinalDocument65 pagesPilot Study FinalPriya SharmaNo ratings yet
- Upper Respiratory Tract Infection (Urti)Document2 pagesUpper Respiratory Tract Infection (Urti)wen_pilNo ratings yet
- Choose The Best Answers! Read The Following Text Carefully and Then Answer The Questions 1 To 5!Document9 pagesChoose The Best Answers! Read The Following Text Carefully and Then Answer The Questions 1 To 5!AbKholiqHSNo ratings yet
- TD Consent FormDocument2 pagesTD Consent FormMike Jonas GrabowskiNo ratings yet
- REFERENCE - Mental Health StigmasDocument9 pagesREFERENCE - Mental Health Stigmasgloria tolentinoNo ratings yet
- Consumer Understanding of Food Quality, Healthiness, and Environmental Impact: A Cross-National PerspectiveDocument20 pagesConsumer Understanding of Food Quality, Healthiness, and Environmental Impact: A Cross-National PerspectiveTeffi Boyer MontoyaNo ratings yet
- 3rd EXAM IN MAPEH-7Document4 pages3rd EXAM IN MAPEH-7Jim ValdezNo ratings yet
- VIVIAN2Document7 pagesVIVIAN2Emmanuel EliasNo ratings yet
- PR1 DuraDocument25 pagesPR1 DuraEigRa ArUdNo ratings yet
- PMLS 6 LABORATORY SAFETY Converted 1Document9 pagesPMLS 6 LABORATORY SAFETY Converted 1seaynNo ratings yet
- Global Health Initiatives: G14 Keisha Rianne T. Perez X-ST - AugustineDocument2 pagesGlobal Health Initiatives: G14 Keisha Rianne T. Perez X-ST - Augustineyixz 5dmNo ratings yet
- Pediatric Diagnosis and ProceduresDocument28 pagesPediatric Diagnosis and ProceduresRegine PanaliganNo ratings yet
- Managemen OMADocument8 pagesManagemen OMAHefieNo ratings yet
- Pharmaceuticals Export From BangladeshDocument3 pagesPharmaceuticals Export From BangladeshTanvir Mohammad ChyNo ratings yet
- Food Safety Enhancement Program ManualDocument86 pagesFood Safety Enhancement Program ManualSeyha L. AgriFoodNo ratings yet
- How Can Leadership Be Measured PDFDocument29 pagesHow Can Leadership Be Measured PDFNAASC Co.No ratings yet
- MDS SIC Blog - Mannitol Treatment For Parkinson's DiseaseDocument7 pagesMDS SIC Blog - Mannitol Treatment For Parkinson's DiseaseYanina Pérez de VillarrealNo ratings yet
- Eejay TemplatesDocument5 pagesEejay TemplatesanmaGirl8611No ratings yet
- Ra 10354 PDFDocument24 pagesRa 10354 PDFmarkkkkkkkheeessNo ratings yet
- Autoimmune Hemolytic Anemia in Children - Classification, Clinical Features, and Diagnosis - UpToDateDocument20 pagesAutoimmune Hemolytic Anemia in Children - Classification, Clinical Features, and Diagnosis - UpToDateNedelcu Miruna100% (1)
- Instituto Pima en Houston Texas - Buscar Con GoogleDocument1 pageInstituto Pima en Houston Texas - Buscar Con GoogleCesar Cruz CortezNo ratings yet
- Republic If The PhilippinesDocument3 pagesRepublic If The PhilippinesKirby C. CatulinNo ratings yet
Thalassemic Mothers and Their Babies: Abstract
Thalassemic Mothers and Their Babies: Abstract
Uploaded by
Wahyu PermataOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thalassemic Mothers and Their Babies: Abstract
Thalassemic Mothers and Their Babies: Abstract
Uploaded by
Wahyu PermataCopyright:
Available Formats
SOUTHEAST ASIAN J TROP MED PUBLIC HEALTH
THALASSEMIC MOTHERS AND THEIR BABIES
Somchai Insiripong1, Sunya Prabriputaloong2 and Nittaya Wisanuyothin3
1
Department of Medicine, 2Department of Obstetrics and Gynecology, 3Department of
Pediatrics, Maharat Nakhon Ratchasima Hospital, Nakhon Ratchasima, Thailand
Abstract. Thirty-two mothers with thalassemia, more than half of whom had hemo-
globin H disease with or without other forms of thalassemia or hemoglobinopathies
along with their 46 children were evaluated. The mean maternal hematocrit was 22.2%
and the mean maternal body mass index was 18.7. The majority of women were not
transfused during pregnancy. Eight point seven percent developed toxemia of preg-
nancy. All had spontaneous labor, 69.5% had a normal vaginal delivery and 23.9% had
a cesarean section. The mean infant birth weight was 2,542.2 grams. Low birth weight
was found in 34.7%; no extremely low birth weights occurred.
INTRODUCTION Women want to avoid the possibility of hav-
ing thalassemic babies. However, some
Thalassemia is a chronic genetic disease. women accept the risk and others never
Its main clinical manifestation is anemia knew they had thalassemia.
which can vary from asymptomatic to severe
The aim of this study was to describe
with death occurring during the first few
certain characteristics regarding thalassemic
hours of life depending on the type and com-
mothers and their babies.
bination of abnormality. Those with thalas-
semia major, besides having anemia, have
other manifestations of disease, including PATIENTS AND METHODS
chronic hypoxia, huge hepatosplenomegaly, Thalassemic mothers who delivered
bone changes due to hyperplasia of in- their babies at Maharat Nakhon Ratchasima
tramedullary hematopoietic tissue, hemo- Hospital between January 2003 and Decem-
chromatosis of the heart, short stature, de- ber 2007 were included in the study. They
layed puberty and a short life span (Benz, were interviewed using a group of questions
2008). Patients need transfusions. It is not consisting of maternal characteristics, such
only a health problem for the patient, but an as height and weight before pregnancy, age
economic burden on the family and the at first pregnancy. Some data were collected
country. When women with thalassemia be- from their medical records, namely, the type
come pregnant, they may have physical de- of thalassemia, sizes of the liver and spleen,
fects, anemia, short height and low body average hematocrit before pregnancy, num-
mass index as well as pass along the disease ber antenatal care (ANC) visits, number of
to their children (Deshmukh et al, 1998). transfusions during the pregnancy, mode of
Correspondence: Somchai Insiripong, Depart- delivery and infant characteristics, such as
ment of Medicine, Maharat Nakhon Ratchasima birth weight, sex and the number of other
Hospital, Nakhon Ratchasima 30000, Thailand. children. Most husbands did not have their
Tel: 081-9556993; Fax 66(0)44 293044 blood checked for thalassemia. Hemoglobin
E-mail: chaikorat@gmail.com typing of the babies was not explored either.
302 Vol 40 No. 2 March 2009
THALASSEMIC MOTHERS AND THEIR BABIES
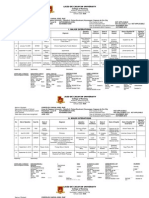
All parameters are expressed as means Table 1
and percentages. General maternal characteristics.
RESULTS Maternal characteristics Range Mean
Thirty-two thalassemic mothers were Age (years) 21-46 31.5
recruited and interviewed following a ques- Hematocrit (%) 13.6-30.3 22.2
tionnaire. Half became pregnant in spite of Liver size (cm) 0-7 1.65
Spleen size (cm) 2-8 4.0
strong encouragement to use birth control,
Height (cm) 146-165 153.1
while the other half were diagnosed with
Weight (kg) 35-55 44.1
thalassemia at the first ANC visit. The ages BMI (kg/km2) 15.5-20.8 18.7
of the women at their first pregnancy ranged
from 21 to 49 years (mean 31.9 years). The
average hematocrit, sizes of liver and/or
spleen, height, weight and body mass index Table 2
before pregnancy are shown in Table 1. Types of thalassemia in studied subjects.
All the women had anemia (mean he-
Type of thalassemia No. (%)
matocrit was 22.2%), the majority of them
had hepato- and/or splenomegaly, the mean Beta-thalassemia-Hb E 11 (34.3)
liver and spleen sizes were 1.6 and 3.0 cm, HbH with Constant-Spring (CS) 7 (21.8)
respectively below the costal margin. Five HbH disease 6 (18.7)
of 32 women (15.6%) had splenectomy dur- HbAEBart’s with CS 3 (9.3)
ing childhood for hypersplenism. No one HbEFBart’s 2 (6.2)
had regular blood transfusion before or dur- HbAEBart’s 1 (3.1)
ing their pregnancy. A minority of them were Unknown 2 (6.2)
Total 32
transfused because they experienced severe
anemic symptoms, such as fainting or severe
fatigue.
The types of maternal thalassemia are thalassemic women, half the infants were
shown in Table 2. One-third of women males. Thirty-two (69.5%) delivered their
(34.3%) had a severe form of beta-thalas- first baby, 13 (28.2%) their second and only
semia-hemoglobin E and nearly 2/3 (59.1%) 1 (2.1%) their third baby. No hydrops fetalis
had hemoglobin H or hemoglobin H plus cases or fetal deaths were recorded. Sixteen
others, such as hemoglobin Constant-Spring, babies (34.7%) had a low birth weight (de-
hemoglobin E or beta-thalassemia. fined as <2,500 grams); of these, one (2.1%)
Nine (28.1%) women attended the ANC had a very low (1,250 grams) birth weight
clinic, though irregularly, and received an (difined as <1,500 grams); nobody had an
occasional blood transfusion during preg- extremely low birth weight (defined as
nancy (1-4 units of packed red blood cells, <1,000 grams) (Papageorgiou et al, 2005). The
per person, a mean of 2 units/person. The birth weights (BW) of the babies born to
rest of the subjects did not attend the ANC thalassemic mothers are shown in Table 3.
clinic and never received a blood transfu- The majority of women had a blood
sion. Four mothers developed full blown transfusion during labor. Thirty-two of 46
toxemia of pregnancy. babies (69.5%) were born by normal vaginal
There were 46 babies born to these delivery. A minority needed some interven-
Vol 40 No. 2 March 2009 303
SOUTHEAST ASIAN J TROP MED PUBLIC HEALTH
Table 3
Birth weights of babies born to thalassemic mothers.
Range (grams) Mean(grams)
BW of all babies(N=46) 1,250-3,900 2,542.2
BW of babies of splenectomized mothers (N=5) 1,700-2,900 2,350.0
BW of babies from transfused mothers (N=7) 1,700-3,900 2,592.8
BW of babies from mothers with huge splenomegaly 1,550-3,500 2,400.0
(spleen ≥8 cm, below the costal margin, N=8)
tion: 11 cases had a cesarean section and 3 Table 4
had a vacuum extraction (Table 4). Modes of delivery in thalassemic mothers.
The indications for cesarean section
Mode of delivery Number (%)
were: 3 cases with toxemia, 2 with amnionitis
and 1 each for premature rupture of mem- Normal vaginal labor 32 (69.5)
branes, oligohydramnios, fetal distress and Cesarean section 11 (23.9)
breech position. One woman had repeat ce- Vacuum extraction 3 (6.5)
sarean section, the cause for the first cesar- Total 46
ean section was not clear.
DISCUSSION body mass index contributed to low birth
weight infants.
The 32 women delivered 46 infants. The
maternal abnormalities documented in- None of the infants had hepatospleno-
cluded anemia, short maternal stature, low megaly, pallor or hydrops fetalis in our
body mass index and hepatosplenomegaly, study.
in addition to thalassemia major. Sixteen The mean birth weight of the babies
babies (34.7%) had a low birth weight, which born to mothers who received occasional
is more common than the general popula- transfusion during pregnancy was not dif-
tion at our hospital varies between 11.8 and ferent from those born to non-transfused
14.0%. This is presumed to be due to mater- mothers. This may be because this women
nal anemia in combination with other ma- did not receive adequate transfusions to
ternal factors. In India, low birth weight was keep maintain adequate oxygenation of the
found in 30.3% of mothers with anemia, low fetus. The hemoglobin level should have
socioeconomic status, short birth interval, been kept above 11 g% (Singla et al, 1997).
short stature, tobacco exposure, low body Over half (69.8%) of the studied women had
mass index (Deshmukh et al, 1998) and low a normal vaginal delivery and 23.2% had a
non-pregnant weight (<40 kg) (Hirve and cesarean section, which is a much lower
Ganatra, 1994). Our findings are consistent sesarean section rate than in the women
with those of a previous study from Ghana without thalassemia who deliver at our hos-
(Geelhoed et al, 2006) as well as other stud- pital (41.6-43.3%). The indications for cesar-
ies (Bondevik et al, 2001; El Guindi et al, 2004) ean section in our study were toxemia of
which found that maternal anemia and low pregnancy, amnionitis, premature rupture of
304 Vol 40 No. 2 March 2009
THALASSEMIC MOTHERS AND THEIR BABIES
membranes, oligohydramanios, fetal disress moglobin H could not be calculated. These
and breech presentation, which are differ- infants will have hemoglobin typing carried
ent from those of the normal population out at 6 months after birth.
which mainly consist of a delayed second
stage of labor and previous cesarean section. REFERENCES
In a previous study (Jensen et al, 1995), the
Benz EJ. Clinical manifestations and diagnosis of
cesarean section in mothers with thalassemia
thalassemias 2008. [Cited 2008 Oct 20].
was primarily due to cephalopelvic dispro-
Available from: URL: www.uptodate.com
portion (10 out of 16, 62.5%). In our study,
Bondevik GT, Lie RT, Ulstein M, Kvåle G. Mater-
in spite of a low body mass index in moth- nal hematological status and risk of low
ers, transfusions were not adequate, result- birth weight and preterm delivery in Nepal.
ing in a decrease in low birth weights, there- Acta Obstet Gynecol Scand 2001; 80: 402-8.
fore no cases of CPD were diagnosed. Deshmukh JS, Motghare DD, Zodpey SP, Wadhva
Regarding the women who had a sple- SK. Low birth weight and associated ma-
nectomy, the birth weights of their infants ternal factors in an urban area. Indian Pediatr
were similar to those without a history of 1998; 35: 33-6.
splenectomy, although the sample size was El Guindi W, Pronost J, Carles G, et al. Severe
too small to draw any conclusions. It appears maternal anemia and pregnancy outcome.
a history of splenomegaly had no effect on Gynecol Obstet Biol Reprod (Paris) 2004; 33
(6 Pt 1): 506-9.
infant birth weight.
Geelhoed D, Agadzi F, Visser L, et al. Maternal
Four of 46 pregnancies (8.7%) were com- and fetal outcome after severe anemia in
plicated by toxemia of pregnancy which is pregnancy in rural Ghana. Acta Obstet
slightly higher than (3.1-7.1%) the general Gynecol Scand 2006; 85: 49-55.
obstetric population at our hospital. The Hirve SS, Ganatra BR. Determinants of low birth
causes(s) of this are unclear, but the anemia weight: a community based prospective co-
common in this group may have contributed hort study. Indian Pediatr 1994; 31: 1221-5.
to placental ischemia, one pathophysiologi- Jensen CE, Tuck SM, Wonke B. Fertility in beta
cal mechanism for toxemia of pregnancy. thalassemia major: a report of 16 pregnan-
This association needs to be explored further. cies, preconceptual evaluation and a review
Women with more severe thalassemia ba- of the literature. Br J Obstet Gynaecol 1995;
bies, such as found with alpha thalassemia 102: 625-9.
or Bart’s hemoglobin who developed hy- Papageorgiou A, Pelausa E, Kovacs L. The ex-
drops fetalis during pregnancy had a higher tremely low-birth-weight infant. In:
indicence of toxemia. There were no cases MacDonald MG, Mullett MD, Seshia MMK,
eds. Avery’s neonatology pathophysiology
of hydrops fetalis in our study in spite of the
and management of the newborn. 6th ed.
majority of mothers having hemoblobin H,
Philadelphia: Lippincott Williams and
including some with hemoglobin Constant- Wilkins, 2005: 459-89.
Spring.
Singla PN, Tyagi M, Kumar A, Dash D, Shankar
In our study, the hemoglobin type of the R. Fetal growth in maternal anemia. J Trop
fathers was not determined, therefore the ex- Ped 1997; 43: 89-92 [doi:10.1093/tropej/
pected frequency of hydrops fetalis or he- 43.2.89].
Vol 40 No. 2 March 2009 305
You might also like
- Practice Bulletin No 144 Multifetal Gestations .40Document15 pagesPractice Bulletin No 144 Multifetal Gestations .40Jose Luis Morales Bautista100% (1)
- CHN Action PlanDocument9 pagesCHN Action PlanseeyarahNo ratings yet
- CM FrancisDocument229 pagesCM FrancisDrHassan Ahmed Shaikh50% (2)
- Pregnancy in Patients With B-Thalassemia Intermedia: Outcome of Mothers and NewbornsDocument4 pagesPregnancy in Patients With B-Thalassemia Intermedia: Outcome of Mothers and NewbornsIlham RamadhanisNo ratings yet
- Beta-Thalassemia Major and Pregnancy: Clinical StudyDocument3 pagesBeta-Thalassemia Major and Pregnancy: Clinical StudyherryNo ratings yet
- Fetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaDocument4 pagesFetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaMuhammad AdithiaNo ratings yet
- FTP PDFDocument4 pagesFTP PDFIzat FuadiNo ratings yet
- Referensi No 7Document5 pagesReferensi No 7Bagus Wanda HabibullahNo ratings yet
- Gestational Diabetes Mellitus in Teenage Pregnancy: A Case-Control StudyDocument3 pagesGestational Diabetes Mellitus in Teenage Pregnancy: A Case-Control StudySarly FebrianaNo ratings yet
- Prenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromaDocument5 pagesPrenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromawitaNo ratings yet
- Maternal and Obstetric Outcome of Women With Epilepsy 2009 SeizureDocument4 pagesMaternal and Obstetric Outcome of Women With Epilepsy 2009 Seizurebilal hadiNo ratings yet
- Ijrm 9 009 PDFDocument6 pagesIjrm 9 009 PDFWahyu PermataNo ratings yet
- Hum. Reprod.-2004-Carp-191-5Document5 pagesHum. Reprod.-2004-Carp-191-5venkayammaNo ratings yet
- Anemia MaternityDocument5 pagesAnemia MaternityBonaventura Ahardiansyah BoNo ratings yet
- Ojsadmin, 276Document6 pagesOjsadmin, 276komalvaid5No ratings yet
- The Association of Early-Onset Fetal Growth Restriction, Elevated Maternal Serum Alpha-Fetoprotein, and The Development of Severe Pre-EclampsiaDocument6 pagesThe Association of Early-Onset Fetal Growth Restriction, Elevated Maternal Serum Alpha-Fetoprotein, and The Development of Severe Pre-EclampsiaM.RautNo ratings yet
- Outcome of Pregnancy in Patients With Liver CirrhosisDocument7 pagesOutcome of Pregnancy in Patients With Liver CirrhosisSamirAyadNo ratings yet
- Vol93 No.6 661 5058Document6 pagesVol93 No.6 661 5058Titi Afrida SariNo ratings yet
- Maternal and Perinatal Outcome in Antepartum HemorrhageDocument5 pagesMaternal and Perinatal Outcome in Antepartum HemorrhagebayukolorNo ratings yet
- Spectrum of Grand MultiparityDocument4 pagesSpectrum of Grand MultiparityYoser ThamtonoNo ratings yet
- CD HAS ThaiDocument9 pagesCD HAS ThaiAlexandre RochaNo ratings yet
- Effect of PIH On Mothers and Babies PDFDocument3 pagesEffect of PIH On Mothers and Babies PDFAbdifatah AhmedNo ratings yet
- 60d587530e3c120210625article - PDF - FileStudy of Maternal and Perinatal OutcomDocument4 pages60d587530e3c120210625article - PDF - FileStudy of Maternal and Perinatal Outcommade dharmaNo ratings yet
- J of Obstet and Gynaecol - 2012 - Aksornphusitaphong - Risk Factors of Early and Late Onset Pre EclampsiaDocument5 pagesJ of Obstet and Gynaecol - 2012 - Aksornphusitaphong - Risk Factors of Early and Late Onset Pre EclampsiaDefi SelvianitaNo ratings yet
- Materials and MethodsDocument1 pageMaterials and MethodsImtihanamiseNo ratings yet
- Gong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Document21 pagesGong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Clarithq LengguNo ratings yet
- Hard Arson 2008Document7 pagesHard Arson 2008elda zulkarnainNo ratings yet
- Jcem 2587Document5 pagesJcem 2587Midwifery D4unisaNo ratings yet
- Thrombocytopenia at Different Stages of PregnancyDocument3 pagesThrombocytopenia at Different Stages of PregnancyInternational Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalDocument6 pagesSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenNo ratings yet
- Diabetic Placenta: Ultrastructure and Morphometry of The Term VilliDocument9 pagesDiabetic Placenta: Ultrastructure and Morphometry of The Term VilliklapouschakNo ratings yet
- Hum. Reprod.-2008-Bellver-278-84Document7 pagesHum. Reprod.-2008-Bellver-278-84Grigoriu RaduNo ratings yet
- First Trimester (NT-NB Scan) - Inverting The Antenatal PyramidDocument21 pagesFirst Trimester (NT-NB Scan) - Inverting The Antenatal PyramidKalpavriksha1974No ratings yet
- Correlation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesDocument6 pagesCorrelation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesstephaniedianNo ratings yet
- Chapter 3Document32 pagesChapter 3Vaibhav JainNo ratings yet
- Gim 20047Document4 pagesGim 20047Sabhina AnseliaNo ratings yet
- 2017 Article 784Document5 pages2017 Article 784Elena ZepedaNo ratings yet
- 2851-26. 31 Rasheed Eclampsia-1625840448Document3 pages2851-26. 31 Rasheed Eclampsia-1625840448Umair HasanNo ratings yet
- Endocrinology & Metabolic SyndromeDocument13 pagesEndocrinology & Metabolic SyndromeMayra PereiraNo ratings yet
- Maternal Serum Triglycerides in Women With Pre-Eclampsia: Original ArticleDocument5 pagesMaternal Serum Triglycerides in Women With Pre-Eclampsia: Original ArticleGladys SusantyNo ratings yet
- Compare The Histological Features Between The Normal and Hypertensive PlacentaDocument7 pagesCompare The Histological Features Between The Normal and Hypertensive PlacentaKamran AmeerNo ratings yet
- 140 140 1 PBDocument4 pages140 140 1 PBMina LelymanNo ratings yet
- Hellp Indicacion DexametasonaDocument6 pagesHellp Indicacion DexametasonaEyran AlfredoNo ratings yet
- Risk Factors Associated With Fetal Pleural Effusion in Prenatal Diagnosis: A Retrospective Study in A Single Institute in Southern ChinaDocument6 pagesRisk Factors Associated With Fetal Pleural Effusion in Prenatal Diagnosis: A Retrospective Study in A Single Institute in Southern Chinachristian roblesNo ratings yet
- Hyperglycemia in Pregnant Ladies and Its Outcome Out in The Opd, Labor Ward, Gynecology and Obstetrics, Lady Atichison Hospital, LahoreDocument7 pagesHyperglycemia in Pregnant Ladies and Its Outcome Out in The Opd, Labor Ward, Gynecology and Obstetrics, Lady Atichison Hospital, LahoreiajpsNo ratings yet
- Embarazo MultipleDocument15 pagesEmbarazo MultipleLina E. ArangoNo ratings yet
- 1 PB PDFDocument7 pages1 PB PDFAmanda Mustika AdiNo ratings yet
- Comparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.Document54 pagesComparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.prasadNo ratings yet
- Am. J. Epidemiol. 2007 Holzman 786 94Document9 pagesAm. J. Epidemiol. 2007 Holzman 786 94Sri AgustinaNo ratings yet
- Anti-Toxoplasma: Incidence of Antibodies in Women With High-Risk Pregnancy and Habitual AbortionsDocument5 pagesAnti-Toxoplasma: Incidence of Antibodies in Women With High-Risk Pregnancy and Habitual AbortionsFerdina NidyasariNo ratings yet
- Hamil AnggurDocument7 pagesHamil AnggurIchunx MelissaNo ratings yet
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 pagesPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08No ratings yet
- EG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderDocument6 pagesEG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderElena VisterniceanNo ratings yet
- tmp647F TMPDocument13 pagestmp647F TMPFrontiersNo ratings yet
- Analytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsDocument5 pagesAnalytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsNurvita WidyastutiNo ratings yet
- Karakteristik Penderita Preeklamsi Dan Eklamsi Yang Dirawat Inap Di Rumah Sakit Immanuel Bandung Periode Tahun 2006 - 2008Document6 pagesKarakteristik Penderita Preeklamsi Dan Eklamsi Yang Dirawat Inap Di Rumah Sakit Immanuel Bandung Periode Tahun 2006 - 2008Radi PdNo ratings yet
- Neonatal Sepsis in Low Birth Weight Infants in Dr. Soetomo General HospitalDocument4 pagesNeonatal Sepsis in Low Birth Weight Infants in Dr. Soetomo General HospitalMelati Nurul UtamiNo ratings yet
- Prevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksDocument4 pagesPrevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksTriponiaNo ratings yet
- Morbidity and Mortality Amongst Infants of Diabetic Mothers Admitted Into Soba University Hospital Khartoum SudanDocument7 pagesMorbidity and Mortality Amongst Infants of Diabetic Mothers Admitted Into Soba University Hospital Khartoum SudanAde Gustina Siahaan100% (1)
- Detection of Chromosome Aberrations in TheDocument3 pagesDetection of Chromosome Aberrations in TheSonia Delgado EspinozaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyFrom EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Ijrm 9 009 PDFDocument6 pagesIjrm 9 009 PDFWahyu PermataNo ratings yet
- Thalassaemia Syndromes and PregnancyDocument8 pagesThalassaemia Syndromes and PregnancyWahyu PermataNo ratings yet
- Beta-Thalassemia Major and Pregnancy: September 2013Document4 pagesBeta-Thalassemia Major and Pregnancy: September 2013Wahyu PermataNo ratings yet
- Scanned by CamscannerDocument5 pagesScanned by CamscannerWahyu PermataNo ratings yet
- 2 PBDocument9 pages2 PBWahyu PermataNo ratings yet
- Katarak PDFDocument6 pagesKatarak PDFWahyu PermataNo ratings yet
- Myelopathy: Clinical Clerkship of Neurology DepartmentDocument59 pagesMyelopathy: Clinical Clerkship of Neurology DepartmentWahyu PermataNo ratings yet
- Case Report Saraf RevisiDocument21 pagesCase Report Saraf RevisiWahyu PermataNo ratings yet
- Has Treetr Suhe L1L, RSL$: R$ Iry.RDocument1 pageHas Treetr Suhe L1L, RSL$: R$ Iry.RWahyu PermataNo ratings yet
- Uneb Primary Leaving Examination 2023 Integrated Science Questions With Answers Section A and Section BDocument13 pagesUneb Primary Leaving Examination 2023 Integrated Science Questions With Answers Section A and Section Bmarvinrukundo1No ratings yet
- Anjani Ayuningtyas KD NIM: 18.1422.S (4B)Document4 pagesAnjani Ayuningtyas KD NIM: 18.1422.S (4B)dilan mileaNo ratings yet
- Periodicity DentalGuideDocument52 pagesPeriodicity DentalGuideSalam BataienehNo ratings yet
- Abdominal Pain A Synthesis of Recommendations ForDocument11 pagesAbdominal Pain A Synthesis of Recommendations Forsakinah mawadahNo ratings yet
- Contract Proposal 6.23.17Document1 pageContract Proposal 6.23.17Ann DwyerNo ratings yet
- Jurnal Senam Hamil PDFDocument4 pagesJurnal Senam Hamil PDFrina astutiNo ratings yet
- Pilot Study FinalDocument65 pagesPilot Study FinalPriya SharmaNo ratings yet
- Upper Respiratory Tract Infection (Urti)Document2 pagesUpper Respiratory Tract Infection (Urti)wen_pilNo ratings yet
- Choose The Best Answers! Read The Following Text Carefully and Then Answer The Questions 1 To 5!Document9 pagesChoose The Best Answers! Read The Following Text Carefully and Then Answer The Questions 1 To 5!AbKholiqHSNo ratings yet
- TD Consent FormDocument2 pagesTD Consent FormMike Jonas GrabowskiNo ratings yet
- REFERENCE - Mental Health StigmasDocument9 pagesREFERENCE - Mental Health Stigmasgloria tolentinoNo ratings yet
- Consumer Understanding of Food Quality, Healthiness, and Environmental Impact: A Cross-National PerspectiveDocument20 pagesConsumer Understanding of Food Quality, Healthiness, and Environmental Impact: A Cross-National PerspectiveTeffi Boyer MontoyaNo ratings yet
- 3rd EXAM IN MAPEH-7Document4 pages3rd EXAM IN MAPEH-7Jim ValdezNo ratings yet
- VIVIAN2Document7 pagesVIVIAN2Emmanuel EliasNo ratings yet
- PR1 DuraDocument25 pagesPR1 DuraEigRa ArUdNo ratings yet
- PMLS 6 LABORATORY SAFETY Converted 1Document9 pagesPMLS 6 LABORATORY SAFETY Converted 1seaynNo ratings yet
- Global Health Initiatives: G14 Keisha Rianne T. Perez X-ST - AugustineDocument2 pagesGlobal Health Initiatives: G14 Keisha Rianne T. Perez X-ST - Augustineyixz 5dmNo ratings yet
- Pediatric Diagnosis and ProceduresDocument28 pagesPediatric Diagnosis and ProceduresRegine PanaliganNo ratings yet
- Managemen OMADocument8 pagesManagemen OMAHefieNo ratings yet
- Pharmaceuticals Export From BangladeshDocument3 pagesPharmaceuticals Export From BangladeshTanvir Mohammad ChyNo ratings yet
- Food Safety Enhancement Program ManualDocument86 pagesFood Safety Enhancement Program ManualSeyha L. AgriFoodNo ratings yet
- How Can Leadership Be Measured PDFDocument29 pagesHow Can Leadership Be Measured PDFNAASC Co.No ratings yet
- MDS SIC Blog - Mannitol Treatment For Parkinson's DiseaseDocument7 pagesMDS SIC Blog - Mannitol Treatment For Parkinson's DiseaseYanina Pérez de VillarrealNo ratings yet
- Eejay TemplatesDocument5 pagesEejay TemplatesanmaGirl8611No ratings yet
- Ra 10354 PDFDocument24 pagesRa 10354 PDFmarkkkkkkkheeessNo ratings yet
- Autoimmune Hemolytic Anemia in Children - Classification, Clinical Features, and Diagnosis - UpToDateDocument20 pagesAutoimmune Hemolytic Anemia in Children - Classification, Clinical Features, and Diagnosis - UpToDateNedelcu Miruna100% (1)
- Instituto Pima en Houston Texas - Buscar Con GoogleDocument1 pageInstituto Pima en Houston Texas - Buscar Con GoogleCesar Cruz CortezNo ratings yet
- Republic If The PhilippinesDocument3 pagesRepublic If The PhilippinesKirby C. CatulinNo ratings yet