Professional Documents
Culture Documents
Postes de Fibra de Vidrio y Colados
Postes de Fibra de Vidrio y Colados
Uploaded by
Kathe ZapataCopyright:
Available Formats
You might also like
- Accelerated Fatigue Resistance of Thick CAD/CAM Composite Resin Overlays Bonded With Light - and Dual-Polymerizing Luting ResinsDocument8 pagesAccelerated Fatigue Resistance of Thick CAD/CAM Composite Resin Overlays Bonded With Light - and Dual-Polymerizing Luting ResinsTiago SpeziaNo ratings yet
- Unconsolidated UndrainedDocument9 pagesUnconsolidated UndrainedMohd Syafiq Akmal100% (2)
- Universiti Malaysia Sarawak: Faculty of EngineeringDocument22 pagesUniversiti Malaysia Sarawak: Faculty of EngineeringAyish Cehcter100% (1)
- Canam Purlins and Girts Catalogue CanadaDocument0 pagesCanam Purlins and Girts Catalogue CanadasaivanvalendezNo ratings yet
- CL 303-Assignment No.1Document2 pagesCL 303-Assignment No.1Vineeth Dasaraju0% (1)
- Limestone FGD ScrubbersDocument575 pagesLimestone FGD ScrubbersAnonymous Cxriyx9HIX100% (3)
- Bouillaguet 2003Document7 pagesBouillaguet 2003valperlunNo ratings yet
- Ari 15Document6 pagesAri 15mariaNo ratings yet
- 10 3290@j Jad A43609Document8 pages10 3290@j Jad A43609ilich sevillaNo ratings yet
- 1989 15557 2 PBDocument11 pages1989 15557 2 PBEduardo FernandezNo ratings yet
- 1 s2.0 S0022391310601114 Main PDFDocument9 pages1 s2.0 S0022391310601114 Main PDFPatty ChuNo ratings yet
- Bulk Fill Resin RestorationDocument18 pagesBulk Fill Resin RestorationNuningK93No ratings yet
- SEM Evaluation of The Cement Layer Thickness After Luting Two Different PostsDocument7 pagesSEM Evaluation of The Cement Layer Thickness After Luting Two Different PostsEdgar Pingo CampuzanoNo ratings yet
- Void and Gap Evaluation Using Microcomputed Tomography of Different Fiber Post Cementation TechniquesDocument5 pagesVoid and Gap Evaluation Using Microcomputed Tomography of Different Fiber Post Cementation TechniquesOskar OrtizNo ratings yet
- Dry-Bonding Etch-and-Rinse Strategy Improves Bond Longevity of A Universal Adhesive To Sound and Artificially-Induced Caries-Affected Primary DentinDocument9 pagesDry-Bonding Etch-and-Rinse Strategy Improves Bond Longevity of A Universal Adhesive To Sound and Artificially-Induced Caries-Affected Primary DentinRitter Adolfo OlivaresNo ratings yet
- Clinical Evaluation of Indirect Composite Resin Restorations Cemented With Different Resin CementsDocument9 pagesClinical Evaluation of Indirect Composite Resin Restorations Cemented With Different Resin CementsJoshua ValdezNo ratings yet
- Influence of Operator Experience On in Vitro Bond Strength of Dentin AdhesivesDocument5 pagesInfluence of Operator Experience On in Vitro Bond Strength of Dentin AdhesivesdanielaNo ratings yet
- Effect of Surface Treatment of Fiberglass Posts On Bond Strength To Root DentinDocument7 pagesEffect of Surface Treatment of Fiberglass Posts On Bond Strength To Root DentinKatherine Kelly Povis AresteguiNo ratings yet
- Does MTA Affect Fiber Post Retention in Repaired Cervical Root Canal PerforationsDocument7 pagesDoes MTA Affect Fiber Post Retention in Repaired Cervical Root Canal PerforationsAmanda Dos SantosNo ratings yet
- Pivoti 2011Document4 pagesPivoti 2011Carmen Breban CirțiuNo ratings yet
- Effect of Resin CementDocument7 pagesEffect of Resin Cementgerardo jimenezNo ratings yet
- BioDocument6 pagesBiomanar alsoltanNo ratings yet
- 10 3290@j Jad A42510Document9 pages10 3290@j Jad A42510Iván ForeroNo ratings yet
- Effect of Resin-Modified Glass-Ionomer Cement Lining and Composite Layering Technique On The Adhesive Interface of Lateral WallDocument6 pagesEffect of Resin-Modified Glass-Ionomer Cement Lining and Composite Layering Technique On The Adhesive Interface of Lateral WallAini Dwi HandiniNo ratings yet
- Effect of Irrigation Protocol During Post Space Preparation On The Dentin Adhesive Interface - An in Vitro StudyDocument9 pagesEffect of Irrigation Protocol During Post Space Preparation On The Dentin Adhesive Interface - An in Vitro StudyMayra Ortiz HerreraNo ratings yet
- Bond Strength of A Flowable Bulk-Fill Resin CompositeDocument7 pagesBond Strength of A Flowable Bulk-Fill Resin CompositeadzhanahadyanNo ratings yet
- Bulk Fill Case 2 PDFDocument6 pagesBulk Fill Case 2 PDFAnonymous SZqzD30YNo ratings yet
- Effect of Cementation Protocol On Push-Out Bond Strength of Fiber Posts To Root CanalDocument7 pagesEffect of Cementation Protocol On Push-Out Bond Strength of Fiber Posts To Root Canalgerardo jimenezNo ratings yet
- Effects of Fiber-Reinforced Composite Bases On Microleakage of Compos - Ite Restorations in Proximal LocationsDocument7 pagesEffects of Fiber-Reinforced Composite Bases On Microleakage of Compos - Ite Restorations in Proximal Locationsmaroun ghalebNo ratings yet
- Microtensile Bond Strength of Adhesive Systems in Different Dentin Regions On A Class II Cavity ConfigurationDocument8 pagesMicrotensile Bond Strength of Adhesive Systems in Different Dentin Regions On A Class II Cavity ConfigurationSinai AriasNo ratings yet
- Microleakage in Conventional and Bonded Amalgam Restorations: Influence of Cavity VolumeDocument7 pagesMicroleakage in Conventional and Bonded Amalgam Restorations: Influence of Cavity Volumegr_saini17768No ratings yet
- Joddd 12 140 PDFDocument6 pagesJoddd 12 140 PDFJessicaLisaNugrohoNo ratings yet
- The Effect of Immediate Dentin Sealing On The Marginal Adaptation and Bond Strengths of Total-Etch and Self-Etch AdhesivesDocument9 pagesThe Effect of Immediate Dentin Sealing On The Marginal Adaptation and Bond Strengths of Total-Etch and Self-Etch AdhesivesclaudiaNo ratings yet
- Microfiltracion en CarillasDocument6 pagesMicrofiltracion en CarillasCdjuan GnNo ratings yet
- In VivoDocument6 pagesIn Vivoo_eisa2002No ratings yet
- Effect of Tooth Substrate and Porcelain Thickness On Porcelain - Veneer Failure Loads in Vitro PDFDocument7 pagesEffect of Tooth Substrate and Porcelain Thickness On Porcelain - Veneer Failure Loads in Vitro PDFSgNo ratings yet
- Borzangy, 2019Document8 pagesBorzangy, 2019phaelzanonNo ratings yet
- Degradacion de Interfase 2Document25 pagesDegradacion de Interfase 2Sofía TrianaNo ratings yet
- 43Document9 pages43Fatimah DewiNo ratings yet
- Endo Article 1Document7 pagesEndo Article 1Alina AlexandraNo ratings yet
- Proenca 2007Document7 pagesProenca 2007valperlunNo ratings yet
- Effect of Different CAD-CAM Materials On The Marginal and Internal Adaptation of Endocrown Restorations: An in Vitro StudyDocument7 pagesEffect of Different CAD-CAM Materials On The Marginal and Internal Adaptation of Endocrown Restorations: An in Vitro StudyNetra TaleleNo ratings yet
- Evaluaci-N ÊÊdel ÊÊProtocoloÊ Êde ÊÊLimpieza ÊÊdelÊ ConductoÊ ÊRadicular Sobre La ÊÊResistencia ÊdeÊÊlaÊ ÊUni-n ÊÊdeÊ ÊPostes ÊdeÊ FibraÊÊde ÊÊVidriODocument7 pagesEvaluaci-N ÊÊdel ÊÊProtocoloÊ Êde ÊÊLimpieza ÊÊdelÊ ConductoÊ ÊRadicular Sobre La ÊÊResistencia ÊdeÊÊlaÊ ÊUni-n ÊÊdeÊ ÊPostes ÊdeÊ FibraÊÊde ÊÊVidriOjhompaz387No ratings yet
- Effect of Root Canal Sealers On Bond Strength of Fibreglass Posts Cemented With Self-Adhesive Resin CementsDocument7 pagesEffect of Root Canal Sealers On Bond Strength of Fibreglass Posts Cemented With Self-Adhesive Resin Cementswuhan lalalaNo ratings yet
- Jukka MatilanaDocument41 pagesJukka Matilanamilleny faizaNo ratings yet
- Comparison of Different Dentin Pretreatment Protocols On The Bond Strength of Glass Fiber Post Using Self-Etching AdhesiveDocument5 pagesComparison of Different Dentin Pretreatment Protocols On The Bond Strength of Glass Fiber Post Using Self-Etching AdhesivedrvenegascesfamromeralNo ratings yet
- Influence of Obturation Technique On Penetration Depth and AdaptationDocument13 pagesInfluence of Obturation Technique On Penetration Depth and AdaptationRaúl Jara CorvalánNo ratings yet
- 01 Mahidol Dental Journal 3 2020Document10 pages01 Mahidol Dental Journal 3 2020shafira zulvaNo ratings yet
- Effectiveness of Seven Types of Sealants Retention After One YearDocument6 pagesEffectiveness of Seven Types of Sealants Retention After One YearJoseph EneroNo ratings yet
- Effect of Etching The Coronal Dentin With The RubbDocument6 pagesEffect of Etching The Coronal Dentin With The Rubbmaroun ghalebNo ratings yet
- Reconstruction of Devital Teeth Using Direct Fiber-Reinforced Composite Resins: A Case ReportDocument7 pagesReconstruction of Devital Teeth Using Direct Fiber-Reinforced Composite Resins: A Case ReportAngga RanggaNo ratings yet
- 1-5 Sisteme AdeziveDocument10 pages1-5 Sisteme AdezivestuparusamiNo ratings yet
- Back To Back Composite RestorationsDocument10 pagesBack To Back Composite RestorationsAli AhmadNo ratings yet
- Effect of Composite Insertion Technique On Cuspal DeflectionDocument7 pagesEffect of Composite Insertion Technique On Cuspal DeflectionYaniuska ContrerasNo ratings yet
- Longevida Adhesivos-5Document25 pagesLongevida Adhesivos-5Camila Conejeros ArriagadaNo ratings yet
- Burbridge2007 NoDocument6 pagesBurbridge2007 NoKatherine VilchezNo ratings yet
- Effects of composite resin core level and periodontal pocket depth on crack propagation in endodontically treated teeth An extended finite element method studyDocument7 pagesEffects of composite resin core level and periodontal pocket depth on crack propagation in endodontically treated teeth An extended finite element method study李雲龍No ratings yet
- Fiber PostsDocument4 pagesFiber PostsNeha AroraNo ratings yet
- Shear Bond Strength of Porcelain Laminate Veneers To Enamel, Dentine and Enamel-Dentine Complex Bonded With Different Adhesive Luting Systems PDFDocument9 pagesShear Bond Strength of Porcelain Laminate Veneers To Enamel, Dentine and Enamel-Dentine Complex Bonded With Different Adhesive Luting Systems PDFLuis Alberto Carpio MorenoNo ratings yet
- TMP 67 ABDocument10 pagesTMP 67 ABFrontiersNo ratings yet
- ResilonDocument33 pagesResilonhasNo ratings yet
- Minimally Invasive Vertical Preparation Design For Ceramic VeneersDocument12 pagesMinimally Invasive Vertical Preparation Design For Ceramic VeneersdanielaNo ratings yet
- Fiber Posts Cementation TechniquesDocument4 pagesFiber Posts Cementation TechniquesAD TwentyOne Dental100% (1)
- Esthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsFrom EverandEsthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsRichard D. TrushkowskyNo ratings yet
- Chart Projections PDFDocument2 pagesChart Projections PDFSanjay WaghmodeNo ratings yet
- Reduction of Stress Concentration in Bolt Nut ConnectorsDocument6 pagesReduction of Stress Concentration in Bolt Nut ConnectorsjtorerocNo ratings yet
- Sample Birth Chart Analysis - Gann Astrononamy.336174811Document14 pagesSample Birth Chart Analysis - Gann Astrononamy.336174811Hitesh PatelNo ratings yet
- Blood RheologyDocument122 pagesBlood RheologyCharu MallNo ratings yet
- Computer Aided Analysis of The Structural Behaviour of Sloped Open Lattice Towers 1Document24 pagesComputer Aided Analysis of The Structural Behaviour of Sloped Open Lattice Towers 1Oladunni AfolabiNo ratings yet
- 371 ARMOX 370T Class1 UK Data SheetDocument2 pages371 ARMOX 370T Class1 UK Data SheetemregnesNo ratings yet
- Laboratory Specific Appendix I - SOP TemplateDocument13 pagesLaboratory Specific Appendix I - SOP TemplateBalachandar KumarNo ratings yet
- P Sheet 8 Linearization SolutionDocument3 pagesP Sheet 8 Linearization Solutionxtito2No ratings yet
- Pavagada Cengrs PagesDocument25 pagesPavagada Cengrs PagesswapneelkalraNo ratings yet
- Gas Laws Station KeyDocument5 pagesGas Laws Station Keyapi-332249032No ratings yet
- Bermuda and Dragon TriangleDocument2 pagesBermuda and Dragon TriangleSyed Mohsin Ali NaqviNo ratings yet
- Building Services - Iv Lighting and Electrical ServicesDocument19 pagesBuilding Services - Iv Lighting and Electrical ServicesankurNo ratings yet
- KSPedia XB1 PDFDocument156 pagesKSPedia XB1 PDFThe Lord Of The CraftNo ratings yet
- Lab For AP ChemistryDocument8 pagesLab For AP ChemistryCliff LiuNo ratings yet
- Design of Steel Structure 9084Document5 pagesDesign of Steel Structure 9084Shajit Kumar0% (1)
- Experiment 5 CreepDocument7 pagesExperiment 5 CreepRashedul IslamNo ratings yet
- Sci Pptq1 Wk1 Day 1-5Document68 pagesSci Pptq1 Wk1 Day 1-5Che LV100% (1)
- Direct Variation: Whatisitandhowdoiknowwheniseeit?Document23 pagesDirect Variation: Whatisitandhowdoiknowwheniseeit?saturnino corpuzNo ratings yet
- Ultrasonic 10Document5 pagesUltrasonic 10Mahade Hasan Dipu100% (1)
- UG 45 CalculationDocument7 pagesUG 45 CalculationnirgaNo ratings yet
- Wlt002-E-P-A00 - Well Data InterpretationDocument125 pagesWlt002-E-P-A00 - Well Data InterpretationSlim.BNo ratings yet
- RefrigeratorDocument6 pagesRefrigeratorChooi San LaiNo ratings yet
- Verification of ODOT's Load RatingDocument277 pagesVerification of ODOT's Load RatingVietanh Phung100% (1)
- DLL Science 8Document7 pagesDLL Science 8Mark Anthony Telan Pitogo0% (1)
- Internal Friction of Materials Anton PuskarDocument342 pagesInternal Friction of Materials Anton PuskarhezihilikNo ratings yet
Postes de Fibra de Vidrio y Colados
Postes de Fibra de Vidrio y Colados
Uploaded by
Kathe ZapataCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postes de Fibra de Vidrio y Colados
Postes de Fibra de Vidrio y Colados
Uploaded by
Kathe ZapataCopyright:
Available Formats
Effect of Resin Cement Mixing and Insertion Method into
the Root Canal on Cement Porosity and Fiberglass Post
Bond Strength
Natércia R. da Silvaa / Monise de Paula Rodriguesb / Aline A. Bicalhoc / Priscilla B. F. Soaresd /
Richard B. Pricee / Carlos J. Soaresf
Purpose: To evaluate the method of resin cement mixing and insertion into the root canal on resin cement porosity
and fiberglass-post push-out bond strength (PBS).
Materials and Methods: One hundred twenty human single-rooted teeth were sectioned to a length of 15 mm, endo-
dontically filled, and received a fiberglass post cemented with 3 self-adhesive resin cements (RelyX U200, seT,
Panavia SA) using 4 mixing methods/insertion techniques (handmix/endodontic file, handmix/Centrix syringe, auto-
mix/conventional tip, automix/endo tip). The samples were scanned using micro-CT. Two slices from the cervical,
middle, and apical thirds were submitted to push-out bond strength (PBS) testing, and failure modes were classified.
The PBS, volume of resin cement, and porosity data were analyzed using ANOVA and Tukey’s test.
Results: The porosity was lowest in the cervical third and highest in the apical third, irrespective of the resin ce-
ment. The porosity was lower in the the automix/endo tip group compared to the handmix/endodontic file group.
The use of Centrix or endo tip reduced the porosity and increased the PBS in the apical third compared with the use
of endodontic files. The root canal depth reduced the PBS for U200 and seT when handmix/endodontic files were
used. U200 and seT using the automix method increased the PBS, thus eliminating the effect of root region, irre-
spective of the insertion technique. In general, U200 showed higher PBS and Panavia lower PBS. Adhesive failure
between root dentin and resin cement was predominant.
Conclusions: Automixing the cement and using an endo tip produces fewer voids and increased the bond strengths.
Keywords: fiber post, insertion technique, micro-CT, porosity, root canal, resin cement.
J Adhes Dent 2019; 21: 37–46. Submitted for publication: 31.05.18; accepted for publication: 19.11.18
doi: 10.3290/j.jad.a41871
post-and-core has been not observed.12 Although it is very
F iberglass posts (FGP) are often used to provide retention
of the final restoration in endodontically treated teeth.26
The elastic modulus of the FGP is closer to that of dentin,
challenging to create mechanically homogenous units in the
root canal space,40 the efficacy of the bonding procedures
and the combination with dentin and resin cement allows when luting these posts plays an important role in the clinical
more uniform stress distribution and reduces the formation performance of composite-FGP restorations.26 A high, dura-
of vertical cracks in the root.9,33,37 However, the real benefit ble bond between resin cement and root dentin is required to
of reducing clinical fractures when compared with a cast provide a coronal seal and adequate retention of the FGP.26
a Dentist, Department of Operative Dentistry and Dental Materials, School of Den- e Professor, Department of Dental Clinical Sciences, Dalhousie University, Halifax,
tistry, Federal University of Uberlândia, Uberlândia, Minas Gerais, Brazil. Hypoth- Nova Scotia, Canada. Experimental design, contributed substantially to dis-
esis formulation, experimental design, wrote and proofread the manuscript. cussion, proofread the manuscript.
b PhD Student, Department of Operative Dentistry and Dental Materials, School f Professor and Chair, Department of Operative Dentistry and Dental Materials,
of Dentistry, Federal University of Uberlândia, Uberlândia, Minas Gerais, Brazil. School of Dentistry, Federal University of Uberlândia, Uberlândia, Minas Gerais,
Performed the experiments, wrote and proofread the manuscript. Brazil. Hypothesis formulation, experimental design, performed the statistical
c
analysis, wrote and proofread the manuscript.
Professor, Technical Health School, Federal University of Uberlândia, Minas
Gerais, Brazil. Performed the experiments, wrote and proofread the manuscript.
d Professor, Department of Periodontology and Implantology, School of Dentistry, Correspondence: Prof. Dr. Carlos José Soares, Av. Pará, 1720, Bloco 4L, Anexo A,
Federal University of Uberlândia, Uberlândia, Minas Gerais, Brazil. Experimen- Campos Umuarama, 38400-902 Uberlândia, Minas Gerais, Brazil.
tal design, performed the experiments, wrote and proofread the manuscript. Tel: +55-34-3225-8106; e-mail: carlosjsoares@ufu.br
Vol 21, No 1, 2019 37
da Silva et al
Due to the passive retention of FGP in root canals, their Therefore, the purpose of this study was to investigate
retention is mainly attributed to the resin cement and the the effect of resin cement type as well as the method by
cementation technique used.8 Cementing FGP into root ca- which the cement is mixed and inserted into the root canal
nals can be a clinical challenge due to complex cementa- on resin cement porosity and bond strength to the tooth.
tion techniques, the high level of technique sensitivity, and The null hypotheses tested were: 1) micro-CT analysis
the variability of the substrate.26 Simplifying luting proce- would not show any difference in the porosity due to differ-
dures would be helpful in overcoming technical problems ent cement manipulation and insertion techniques; 2) the
with multistep cements that may require enhanced mois- push-out bond strength (PBS) would not be affected by dif-
ture control or present chemical incompatibility between ferent cement mixing approaches and insertion techniques;
simplified adhesives and dual-curing methacrylate-based 3) the resin cement type and the root depth would not influ-
resin cements.4,41 Self-adhesive cements possess different ence the PBS.
chemical compositions to which different bonding mecha-
nisms may be inherent.22 This category of resin cement
requires no acid etching, priming, or bonding. These are all MATERIALS AND METHODS
are technique sensitive steps.10 The bonding mechanism
these cements represent an important difference when Sample Selection and Root Canal Preparation
compared with other resin cement that are micromechani- This study was approved by the local Ethics Committee
cally bonded to dental tissues.44 (Protocol 227/09). One hundred twenty single-, straight-
A homogeneous, sufficiently thick resin cement layer is rooted human adult maxillary central incisors with root
a prerequisite for retention of the FGP. Gaps in the resin lengths < 15 mm, of similar size and anatomic shape, were
cement or at the interfaces with FGP and root dentin may selected and stored in distilled water at 4°C until use.
negatively affect the mechanical properties of the resin Teeth with caries, cervical erosion, previous endodontic
and reduce the survival of the restorations.29 Defects treatment, a post or a crown were excluded. The specimens
within the cement can cause localized, highly concen- were decoronated by transversally sectioning the roots
trated stress in the root canal which could initiate crack 15 mm from the apex with a double-faced diamond disk (KG
propagation at relatively low loads. To ensure homogeneity Sorensen; Barueri, SP, Brazil) at low speed with air/water
of resin cement, the mode of cement delivery into the root spray coolant (Isomet 1000, Buehler; Lake Bluff, IL, USA).
canal should avoid the introduction of trapped air within The root canal was located using a 10 K-file (Dentsply
the cement layer.35 Improved delivery systems have re- Malleifer; Petrópolis, RJ, Brazil) that was introduced into
cently been developed to mix and provide a bubble-free the root canal until it was visible at the apical foramen.
paste-paste mixture.27 Moreover, it has also been re- The working length was set at 1.0 mm below the apical
ported that the self-adhesive cements have good flowabil- limit. The root canals were shaped using rotary instru-
ity under pressure. However, cement penetration into the ments (ProTaper system, Dentsply Malleifer) sequenced in
dentin substrate may be limited.24 The high viscosity, the order (SX, S1, S2, F1, F2, F3, F4), applying the crown-down
effects of neutralization generated by the setting reaction technique. One rotary kit was used to prepare 5 specimens
and buffering of the dentin, as well as the presence of a and then replaced. The root canals were irrigated with
secondary smear layer can negatively affect the ability of 2.5% sodium hypochlorite (Chlorine Rio; São José do Rio
the self-adhesive resin cement to demineralize and pene- Preto, SP, Brazil) using a syringe and a 27-gauge needle
trate into dentin.24 The relatively high viscosity of the resin throughout the series of file sizes. Final irrigation was per-
monomer may also be responsible for the reduced degree formed with 17% ethylene diamine tetra-acetic acid (EDTA,
of resin conversion.13 Ultimately, the materials used, as Biodynamics; Ibiporã, PR, Brazil) for 3 min, followed by 2.5%
well as the bonding interaction between the biological tis- NaOCl solution (Chlorine Rio) for 1 min, and 5 ml physio-
sues and the biomaterials, influence the outcome of the logic saline solution (LBS Labor; São Paulo, SP, Brazil) to
final restoration.16 remove the remaining debris. The instrumented root canals
Micro-computed tomography (micro-CT) is a noninvasive were dried with sterile paper points (Dentsply Malleifer),
3D analysis, and a powerful tool that can evaluate the resin then immediately obturated using a lateral condensation
matrix, internal structure, as well as mechanical properties, technique with a gutta-percha master cone (F4 ProTaper
and can also detect voids.9,20,27,32,42 Micro-CT also en- Universal, Dentsply Malleifer) as well as conventional
ables reconstruction and volumetric evaluation of the inter- gutta-percha accessory cones and calcium hydroxide based
nal and external structures, as a whole or separately, and cement (Sealer 26, Dentsply; Sao Paulo, SP, Brazil). The
overcomes the limitations of conventional methods that are root canal opening was sealed with resin-modified glass-
more invasive.18,39,42 The push-out strength test allows ac- ionomer cement (Vitremer, 3M Oral Care; St Paul, MN,
curate analysis of the overall bonding mechanism better USA). The endodontically treated roots were stored at 37°C
simulates clinical scenarios.2,15 Furthermore, analysis of and 100% relative humidity for 7 days.
possible correlations between the morphological character-
istics of the adhesive-root dentin interface and bond Post Space Preparation
strength might provide better explanations of the bonding A heated instrument (Paiva condenser, Golgran; São Paulo,
ability of resin cements to root dentin.9 SP, Brazil) was used to remove the gutta-percha to a depth
38 The Journal of Adhesive Dentistry
da Silva et al
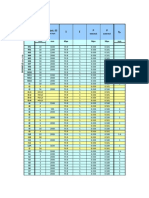
Table 1 Self-adhesive resin cements, batch number, manufacturer and composition
Material Manufacturer Batch number Composition
RelyX U200 3M Oral Care; 506742 Base paste: methacrylate monomers containing phosphoric acid groups,
St Paul, MN, USA methacrylate monomers, silanated fillers, initiator components, stabilizers,
rheological additives
Catalyst paste: methacrylate monomers, alkaline (basic) fillers, silanated fillers,
initiator components, stabilizers, pigments
Panavia SA Kuraray Noritake; 0070AA Paste A: 10-methacryloyloxydecyl dihydrogen phosphate (MDP), bisphenol A
Cement Osaka, Japan diglycidylmethacrylate (bis-GMA), triethyleneglycoldimethacrylate (TEG-DMA),
hydrophobic aromatic dimethacrylate 2-hydroxymethacrylate (HEMA), silanated
barium glass filler, silanated colloidal silica, dl-camphorquinone, peroxide,
catalysts, pigments
Paste B: hydrophobic aromatic dimethacrylate, hydrophobic aliphatic
dimethacrylate, silanated barium glass filler, surface treated sodium fluoride,
accelerators, pigments; inorganic filler 40 vol%. The particle size of inorganic
fillers ranges from 0.02 μm to 20 μm.
seT PP SDI; Bayswater, 61304011 35 wt% methacrylate ester, 65 wt% inorganic filler
Victoria, Australia
Information provided by manufacturers.
of 10 mm. The specimens were randomly assigned to y Handmix/Centrix (Fig 1b): resin cement was hand mixed,
12 groups (n = 10) according to the resin cement mixing then inserted into the canal using Centrix syringe (NOVA
and insertion technique (handmix/endodontic file; hand- DFL; Rio de Janeiro, RJ, Brazil) with AccuDose tips.
mix/Centrix syringe; automix/conventional tip; automix/ y Automix/conventional tip (Fig 1c): the resin cement was
endo tip) and the self-adhesive resin cement (Rely X U200 mixed through a dual-barrel syringe (mixing tip regular)
[3M Oral Care] control group; seT, SDI [Bayswater, Victoria, and dispensed directly into the canal using a dedicated
Australia]; Panavia SA Cement [Kuraray Noritake; Osaka, tip 24 mm long, larger diameter 3.8 mm, smaller diame-
Japan]). The resin cements are described in Table 1. ter 1.4 mm, according to the manufacturer’s instructions.
After post space preparation with a heated condenser y Automix/endo tip (Fig 1d): the cement was mixed
(Paiva condenser; Golgran) to 10 mm, a no. 5 Gates-Glid- through a dual-barrel syringe (18-mm mixing tip) and dis-
den drill was used at 8 mm. A bur specific to the post sys- pensed directly into the canal using a root canal tip
tem (White Post DC #3, FGM; Joinville, SC, Brazil) with di- (endo tip, 0.98 mm diameter) according to the manufac-
mensions similar to the glass-fiber post (height 20 mm, turer’s instructions.
upper and lower diameters 2.0 mm and 1.25 mm, respec-
tively) was used. The post space was cleaned by copious After 1 min, the excess cement was removed. Five min-
irrigation with distilled water. The canals were then dried utes after seating the post, the resin cement was light
with paper points (Dentsply Malleifer). cured at each coronal root surface (buccal, lingual, and oc-
clusal) for 40 s using a halogen curing lamp (Optilux 501,
Glass Fiber Post Cementation Kerr; Orange, CA, USA) that delivered irradiance of 1000
The post cementation protocol was the same for all resin mW/cm2 at the tip. The specimens were stored in 100%
cements tested. The glass-fiber post (White Post DC #3; humidity at 37°C for 7 days.
FGM) was etched with 24% hydrogen peroxide for 1 min,
and rinsed with distilled water,23 and then air dried. A si- Micro-CT Analysis
lane agent was subsequently applied to the post for 1 min Each specimen was air dried, mounted on a custom attach-
(Silano, Angelus; Londrina, PR, Brazil). All roots were dried ment and scanned using a high-resolution micro-CT system
with paper points and the fiber posts were cemented using (SkyScan 1272, Bruker; Kontich, Belgium). The scanner op-
four different techniques (Fig 1): erated at 100 kV and 100 mA (0.11-mm Cu filter). The
y Handmix/endodontic file, control group (Fig 1a): the self- resolution used was 1224/820 cross-sectional pixel size,
adhesive resin cement was dispensed and hand mixed and the intersection distances were 20 μm. This resulted in
for 20 s according to the manufacturer’s instructions. 380 transverse cross sections per specimen. The scanning
Then, the resin cement was introduced into the canal by parameters were: 180-degree rotation around the vertical
using a K-file, and the post portion was covered with ce- axis, a camera exposure time of 1000 ms, a rotation step
ment. The post was seated and held using finger pres- of 0.5 degrees, a frame average of 2, and random move-
sure for 5 min, the excess resin cement was removed, ment of 20. Each specimen was scanned for a total of
then light activation was performed for 40 s from the 35 min 41 s. Images of each specimen were reconstructed
buccal, lingual and incisal.30 using NRecon version 1.6.10.1 (Bruker). For each root, ap-
Vol 21, No 1, 2019 39
da Silva et al
a
Handmix/
endodontic file
b
Handmix/
Centrix
c
Automix/
conventional tip
d
Automix/
endo tip
Fig 1 Sequence of the sample preparation for each experimental group: (a) handmix group; (b) Centrix group; c. automix group; d. endo tip
group.
proximately 380 slices were made per specimen. CTAn measured using a stereomicroscope and digital micrometer
v.1.14.4.1 software (Bruker) was used for 3D quantitative digital camera (Mitutoyo; Tokyo, Japan) with an accuracy of
analysis (volume of resin cement in mm3 and volume of 0.01 mm. Each slice was subjected to push-out bond
porosity in %) of each root canal. The 3D analysis provided strength testing (DL500, EMIC; São José dos Pinhais, PR,
the quantitative porosity, which corresponds to the percent Brazil), with the load applied in the apical-coronal direction
(%) void volume within the resin cement layer. The influence at a crosshead speed of 0.5 mm/min. The maximum load
of the type of resin cement, cement mixing and insertion at failure was recorded in N and converted to MPa by divid-
method in the root canal, and different root section (apical, ing the load applied by the bonded area (A), calculated as
middle, and cervical slices) was analyzed. CTVol v.2.2.3.0 follows: A = 2π [(r + R)/2] h, where π is a constant of 3.14,
software (Bruker) was used for three-dimensional visualiza- r and R are the smallest and the largest radius, respec-
tion and qualitative evaluation of the specimens (Fig 2). tively, of the cross-sectioned tapered post, and h is the
thickness of the sectioned root with post.
Push-out Bond Strength Test
The restored teeth were fixed on a 20 mm x 20 mm acrylic Failure Mode Analysis
plate with cyanoacrylate (Super Bonder; Loctite, SP, Brazil), Failures were classified by a blinded, calibrated operator
and were sectioned transversely using the water-cooled low- using a stereomicroscope (Mitutoyo) at 40X magnification
speed diamond saw (Isomet 1000; Buehler). Two 1.0-mm- (Fig 3), according to these 5 categories: (I) adhesive failure
thick slices each were obtained from the apical, middle and between post and resin cement; (II) failure between resin
coronal root regions. Load indenter tips of 1.5 mm and cement and root dentin; (III) mixed failure, with resin ce-
2.5 mm base were used for the cervical and middle thirds, ment covering partially of the post surface; (IV) cohesive
and a smaller 1.0-mm tip and 2.0-mm base for the apical failure within the fiber post; and (V) cohesive failure within
third.47 The diameter and thickness of the specimens were the dentin.
40 The Journal of Adhesive Dentistry
da Silva et al
Fig 2 Micro-CT reconstruction of the root endodontically
treated with fiber post cemented using resin cement. a b c d
(a) handmix group; (b) Centrix group; (c) automix group;
(d) endo tip group.
Panavia SA
sET
RelyX U200
Statistical Analysis tion method (p = 0.134). The volume of porosity of the resin
The PBS data were statistically analyzed using 2-way ANOVA cements mixed and inserted using different methods in dif-
(resin cement and mixing/insertion method) with repeated ferent root regions are shown on Fig 5. ANOVA indicated a
measurement (root depth) and Tukey’s post-hoc multiple significant effect of the interaction between mixing and inser-
comparison test. The volume of resin cement and the vol- tion of resin cement method and root regions (p < 0.001).
ume of porosities were analyzed using 1-way ANOVA (mix- Tukey’s test demonstrated that the hand mixed resin ce-
ing/insertion method) with repeated measurement (root ment had lower porosity in the cervical third, followed by the
depth) and Tukey’s test. The chi-squared test was used to middle third, with the highest porosity found in the apical
analyze the failure modes. The significance level was set at third, irrespective of the resin cement. The lowest porosity
5%. All statistical analyses were performed using Sigma was found for resin cement mixed automatically and inserted
Plot 12.1 (Stata; College Station, TX, USA). into the root canal using the endo tip. The highest porosity
was found for resin cement mixed manually and inserted into
the root canal using the endodontic file. The use of a Centrix
RESULTS syringe reduced the porosity in the apical third for all resin
cements when compared with the hand-mixed group inserted
Micro-CT Analysis using the endodontic file. The resin cement automixed and
The volume of the resin cement calculated using micro-CT is inserted using the endo tip completely eliminated the effect
shown in Fig 4. Representative micro-CT images of the resin of root canal region on the porosity of the resin cement.
cement porosity produced by different mixing and insertion
methods are shown in Fig 2. ANOVA showed no significant Push-out Bond Strength Test
difference in the total volume occupied by resin cement and The bond strengths in MPa (mean and standard deviation)
voids in the root canal irrespective of manipulation and inser- according to resin cement, mixing and insertion methods,
Vol 21, No 1, 2019 41
da Silva et al
a 25 b 25 c 25
Panavia SA sET RelyX U200
Push-out bond strength – MPa
Push-out bond strength – MPa
Push-out bond strength – MPa
20 20 20
15 15 15
10 10 10
5 5 5
0 0 0
Cervical Middle Apical Cervical Middle Apical Cervical Middle Apical
Endotip Automix Centrix Handmix
d Panavia SA e sET f RelyX U200
Apical Apical Apical
Endotip
Endotip
Endotip
Middle Middle Middle
Cervical Cervical Cervical
Apical Apical Apical
Automix
Automix
Automix
Middle Middle Middle
Cervical Cervical Cervical
Apical Apical Apical
Centrix
Centrix
Centrix
Middle Middle Middle
Cervical Cervical Cervical
Apical
Handmix
Apical
Handmix
Apical
Handmix
Middle Middle Middle
Cervical Cervical Cervical
0% 20% 40% 60% 80% 100% 0% 20% 40% 60% 80% 100% 0% 20% 40% 60% 80% 100%
Fig 3 Bond strengths in MPa (mean and standard deviation) by resin cement, mixing/insertion methods and region for (a) Panavia; (b) seT
and (c) RelyX U200. Mean values labeled with different letters differ statistically signifcantly (Tukey’s test, p < 0.05). Upper-case letters
indicate comparison of the root region, and lower-case letters indicate comparison of mixing/insertion methods for each resin cement.
The failure mode distribution is shown in terms of the resin cement, mixing/insertion methods and region for (d) Panavia; (e) sET and
(f) RelyX U200. Categories of failure modes: (I) adhesive failure between post and resin cement; (II) failure between resin cement and root
dentin; (III) mixed failure, with resin cement partially covering the post surface; (IV) cohesive failure within the fiber post; (V) cohesive failure
within the dentin.
and root region for the experimental groups are shown in via resulted in lower bond strengths than did the other resin
Fig 3, a to c. ANOVA showed a statistically significant influ- cements tested.
ence of the interaction between the mixing/insertion The failure modes depending on resin cement, mixing
method and root region factors only for RelyX U200 and insertion methods, and root region for the experimental
(p = 0.002) and seT cement (p = 0.014). No difference was groups are shown in Fig 3, c to e. The chi-squared test
found for all factors for Panavia resin cement (p = 0.456). showed no statistically significant differences among failure
The root depth significantly reduced the bond strengths for modes, irrespective of root region and mixing/insertion
RelyX U200 and seT when manually mixed and inserted method (p = 0.456). Adhesive failure between root dentin
using endodontic files. The use of the Centrix syringe to in- and resin cement was the prevalent failure mode for all ex-
sert manually mixed resin cements statistically significantly perimental groups.
increased the bond strengths in the apical third compared
to insertion with endodontic files. Automatically mixing
RelyX U200 and seT resin cements increased the bond DISCUSSION
strengths eliminated the effect of the root region. The endo
tip resulted in bond strengths similar to the conventional tip The means by which resin cement is inserted into the root
for all resin cements. In general, RelyX U200 showed higher canal is one of the main factors influencing bonding quality
bond strengths than did the other resin cements, and Pana- to both the post and the root dentin walls.27 The voids pres-
42 The Journal of Adhesive Dentistry
da Silva et al
Fig 4 Resin cement volumes in mm3
5.0
(mean and standard deviation) by resin
Volume of resin cement – mm3
cement and mixing/insertion methods.
4.0
No statistically significant difference was
observed among them (Tukey’s test;
3.0
p < 0.05).
2.0
1.0
0.0
Automix
Centrix
Endotip
Handmix
Automix
Centrix
Endotip
Handmix
Automix
Centrix
Endotip
Handmix
Panavia SA sET RelyX U200
Fig 5 The porosity of resin cement
volumes in mm3 (mean and standard devia-
Volume of porosity – resin cement %
45%
tion) by mixing/insertion methods and root 40%
regions. Mean values followed by different
letters differ statistically significantly 35%
among them (Tukey’s test, p < 0.05). 30%
Upper-case letters indicate comparison of 25%
the mixing/insertion, and lower-case letters
20%
indicate comparison of root regions for
each resin cement. 15%
10%
5%
0%
Handmix
Centrix
Automix
Endtip
Handmix
Centrix
Automix
Endtip
Handmix
Centrix
Automix
Endtip
Panavia SA sET RelyX U200
Apical Medium Cervical
ent and their regional distribution were affected by the resin apical porosity for all resin cements, when compared with
cement mixing and insertion method.42 Delivery systems hand-mixed resin cements inserted using endodontic files.
that use a syringe to extrude the mixed cement through mix- Similar results were found in another study27 that observed
ing tips directly into the root canal should deliver a consis- a larger number of voids and bubbles when the conven-
tently bubble-free cement mixture.27 When using dual-sy- tional technique was used, vs application with a Centrix sy-
ringe-mixed resin cements, the mixing process does not ringe, which allowed a more homogeneous cement interface
generate voids, because neither catalyst nor base pastes for the self-adhesive luting materials tested. The injection
are in contact with air.42 Resin cement mixed manually and of resin cement into the root canal, particularly into the
inserted using a Centrix syringe presented greater void for- deeper root canal regions, obviated air retention in the root
mation than did automixed resin cement inserted using a canal (fewer bubbles). Additionally, the use of the specific
conventional or endo tip, demonstrating that the mixing endo tip associated with automixing significantly reduced
method influenced void formation in cement.11,42 Cements the porosity of all resin cements examined here. If the tip is
mixed manually have been shown to include several small thin enough to reach the bottom of the prepared root canal,
voids both during the mixing and while placing the post into hence enabling resin cement insertion from the apical to
the canal.42 the cervical thirds, much lower porosity is observed. This
In the present study, the use of a Centrix syringe to in- creates a more homogeneous cement layer along the entire
sert the manually mixed resin cement manually reduced the root surface and not only permits better bonding between
Vol 21, No 1, 2019 43
da Silva et al
resin cement and root dentin, it also results in better stress method used to mix and insert the resin cement into the
distribution along both post and dentin interface.9 Thus, the root canal may influence resin cement viscosity. The self-
use of a flexible root-canal-shaped application aid should adhesives do not have the ability to penetrate the smear
reduce the number of voids at the self-adhesive cement in- layer or dentin, and cannot form a hybrid layer as conven-
terface.27,45 The resin cement inserted using endodontic tional bonding agents do.1 Immediately after mixing the
files does not touch the entire root canal surface. Although base and catalytic pastes, the cements are able to flow
the Centrix syringe helps insert the resin cement into deep according to each material’s rheological properties7 when
areas of the root canal, it does not eliminate the bubbles delivering the resin cements. With RelyX U200, a simultane-
generated during hand mixing of resin cement. Automix in- ous neutralization effect occurs with the cement setting re-
sertion resembles that of the Centrix syringe, ie, bubbles action, due to buffering of the dentin and to chemical reac-
are not generated by the mixing process. Finally, the use of tions involving water release and alkaline filler that might
an endo tip helps to deliver the resin cement into the entire help increase the pH level.3 Resin infiltration is proportional
extension of the root canal, which explains the difference to the applied concentration, molecular weight or size, the
between groups. affinity of monomers for the substrate, and the time al-
The second and third null hypotheses were also rejected. lowed for penetration.25 Therefore, automixing and insertion
Automatically mixing RelyX U200 and seT resin cements using an endo tip may also promote time reduction, abbre-
increased the bond strengths and eliminated the effect of viating the viscosity increase. Additionally, Panavia SA con-
root region. Additionally, when these cements were manu- tains an acidic functional monomer, 10-methacryloxydecyl
ally mixed and inserted using endodontic files, the apical dihydrogen phosphate (10-MDP), which increases the bond
third exhibited significantly lower PBS. A negative effect was stability by bonding chemically to Ca2+ and building a na-
observed for void formation, as it reduced the bond noscale structure.6 Then for this resin cement, the porosity
strength by restricting the available area for cementation, at the interface may reduce the area in contact with root
which results in shorter survival time of the restoration.42 dentin, reducing the chemical interaction.
Greater push-out strengths were obtained for adhesive ce- Decreasing bond strength as a function of coronal-apical
ments when the endo tip was used.11 When sample de- direction can also be explained by inability of the dual-cur-
fects occupied more than 12% of the total transverse-sec- ing cements to reach a similar degree of conversion along
tion area of the endodontic cement layer, interfacial shear the entire extension of the root, where the curing light is
strengths were 70% lower than those found for samples unable to reach the apical areas.7,11,19 As the polymerizing
without defects. In contrast, those occupying less than 2% network develops further, the rate of radical propagation is
had a negligible effect on interfacial shear strength. 16 eventually limited by diffusion, and the polymerization rate
Greater porosity and higher stress concentration occurred decelerates, providing only limited conversio, even in the
at the cement-dentin interface, leading to lower bond presence of unreacted monomer and free radicals.17 There-
strength mainly at the apical region.9 Additionally, the fric- fore, the chemical-curing mechanism proceeds slowly under
tion between the cement and dentin plays an important role delayed photo-activation conditions. The cements are chem-
in push-out bond strength.14 A more homogeneous cement ically activated first and the polymerization reaction pro-
layer could improve this frictional retention, contributing to gresses slowly, especially in areas where the curing light is
higher PBS. unable to reach the material.31 However, it can be specu-
Push-out bond strength decreased as the apex was ap- lated that both the dynamic process in the acidity of the
proached, which may be due to several factors, including cements is progressively neutralized, as well as in the po-
numerous variables involved in root canal bonding tech- lymerization process itself, are influenced by the self-adhe-
nique, eg, moisture control, light penetration inside the root sive cement composition and the activation protocol.7
canal, and C-factor.28 It is rather difficult to achieve effec- Only self-adhesive resin cements were tested in this
tive bonding within the root canal due to its small size and study, as some studies report this type of resin cement to
inherent geometry, which make controlled application of the be the best option for post cementation.34,36 RelyX U200
several agents of the adhesive bonding system difficult. Vi- was considered the control group, because it has frequently
sual monitoring is almost impossible. Residue from post- shown higher and more uniform bond strength in the root
space preparation and conditioning may remain. Improved canal than conventional dual-curing resin cement.9,30 In this
bond strength of self-adhesive resin cements in the apical study, RelyX U200 generally showed higher bond strengths
third relies on the mixing and insertion method using a de- did than the other resin cements, and Panavia SA resulted
livery system (Centrix syringe) for handmix and mainly the in lower bond strengths than did the other resin cement
use of automixed resin cement inserted using an endo tip tested. Some authors suggest that the maintenance of a
to improve interaction with root dentin. The luting materi- low pH could have an adverse effect on the bond strength
als’s high viscosity negatively affects the demineralization of self-adhesive cements to root dentin.38 Acid monomers
and penetration potential into dentin of self-adhesive resin in simplified adhesives are known to promote the consump-
cements.46 A decrease in cement viscosity allows the tion of tertiary amines included in chemical paste of resin
monomer/comonomer systems to enhance diffusion of the cements, which results in incomplete polymerization and,
reactive species, leading to an increased rate of reticula- consequently, low bond strengths given a reduction in light
tion, especially in the initial stages of polymerization.5 The polymerization.41 RelyX U200 tends to increase the pH over
44 The Journal of Adhesive Dentistry
da Silva et al
24 h (from 2.8 to 7.0).28 The initially low pH of self-adhe- REFERENCES
sive cements or their residual unpolymerized acidic mono- 1. Aguiar TR, Andre CB, Arrais CAG, Bedran Russo AK, Giannini M. Micromor-
mers may cause exposure of coronal or radicular dentin phology of resin dentin interfaces using self-adhesive and conventional
collagen, allowing it to be degraded by the activation of ma- resin cements: a confocal laser and scanning electron microscope analysis.
Int J Adhes Adhes 2012;38:69–74.
trix metalloproteinases (MMPs) and cathepsins.21 Further- 2. Armstrong S, Geraldeli S, Maia R, Raposo LH, Soares CJ, Yamagawa J.
more, the smear layer and underlying dentin have been re- Adhesion to tooth structure: a critical review of “micro” bond strength
garded as solid buffers that probably rapidly buffer the test methods. Dent Mater 2010;26:50–62.
3. Cantoro A, Goracci C, Vichi A, Mazzoni A, Fadda GM, Ferrari M. Retentive
acidity of viscous solutions, thereby limiting the etching strength and sealing ability of new self-adhesive resin cements in fiber
ability of acidic monomers.45 Little information is also avail- post luting. Dent Mater 2011;27:197–204.
able on the resin cement seT. According to the manufac- 4. Carrilho MR, Carvalho RM, Tay FR, Pashley DH. Effects of storage media on
mechanical properties of adhesive systems. Am J Dent 2004;17:104–108.
turer (SDI), the cement establishes a chemical bond with
5. Charton C, Falk V, Marchal P, Pla F, Colon P. Influence of Tg, viscosity and
dental substrates.3 However, no details are provided on the chemical structure of monomers on shrinkage stress in light-cured dimeth-
functional acidic monomers and how they are activated in acrylate-based dental resins. Dent Mater 2007;23:1447–1459.
the absence of water.3 Microscopic observations of seT 6. Culhaoglu AK, Özcan E, Kilicarslan MA, Seker E. Effect of boric acid ver-
sus conventional irrigation solutions on the bond strength between fiber
specimens demonstrated that neither the cement-substrate post and root dentin. J Adhes Dent 2017;19:137–146.
interfaces nor the cement layer were gap-free, and the 7. D’Alpino PH, Silva MS, Vismara MV, Di Hipólito V, Miranda González AH, de
highly-filled cement was not able to penetrate the dentinal Oliveira Graeff CF. The effect of polymerization mode on monomer conver-
sion, free radical entrapment, and interaction with hydroxyapatite of com-
tubules. It should be considered that the absence of HEMA mercial self-adhesive cements. J Mech Behav Biomed Mater 2015;46:
might have limited the ability of the material to adequately 83–92.
wet the hydrophilic dental substrate.43 8. D’Arcangelo C, D’Amario M, Vadini M, Zazzeroni S, De Angelis F, Caputi
S. An evaluation of luting agent application technique effect on fibre post
Clinically, restoration longevity depends on numerous retention. J Dent 2008;36:235–240.
steps in the restorative process. The simplification of clini- 9. Da Silva NR, Aguiar GC, Rodrigues Mde P, Bicalho AA, Soares PB, Veríssimo
cal steps in terms of materials used is critical in restorative C, Soares CJ. Effect of resin cement porosity on retention of glass-fiber
posts to root dentin: an experimental and finite element analysis. Braz
procedures, because these many aspects need to be con- Dent J 2015;26:630–636.
sidered.7 Appropriate mixing and insertion methods of the 10. De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meer-
self-adhesive resin cement are important factors which can beek B. Bonding of an auto-adhesive luting material to enamel and dentin.
Dent Mater 2004;20:963–971.
improve the bond strength and reduce resin cement poros- 11. Durski MT, Metz MJ, Thompson JY, Mascarenhas AK, Crim GA, Vieira S,
ity, thus affecting restoration longevity. Use of a Centrix sy- Mazur RF. Push-out bond strength evaluation of glass fiber posts with dif-
ringe for hand-mixed resin-cement insertion into the root ferent resin cements and application techniques. Oper Dent 2016;41:
103–110.
canal and for auto-mixed cement employed with an endo tip
12. Figueiredo FE, Martins-Filho PR, Faria-E-Silva AL. Do metal post-retained
could potentially improve clinical results. However, more restorations result in more root fractures than fiber post-retained restora-
studies are necessary and the results of in vitro studies tions? A systematic review and meta-analysis. J Endod 2015;41:309–316.
should be carefully interpreted before being extrapolated to 13. Floyd CJ, Dickens SH. Network structure of Bis-GMA- and UDMA-based
resin systems. Dent Mater 2006;22:1143–1149.
a clinical context. 14. Goracci C, Fabianelli A, Sadek FT, Papacchini F, Tay FR, Ferrari M. The con-
tribution of friction to the dislocation resistance of bonded fiber posts.
J Endod 2005;31:608–612.
15. Goracci C, Grandini S, Bossù M, Bertelli E, Ferrari M. Laboratory assess-
CONCLUSIONS ment of the retentive potential of adhesive posts: a review. J Dent 2007;
35:827–835.
y Reducing the porosity of the resin cement, higher bond 16. Grassi FR, Pappalettere C, Di Comite M, Corsalini M, Mori G, Ballini A,
Crincoli V, Pettini F, Rapone B, Boccaccio A. Effect of different irrigating
strength between FGP and root dentin was obtained. solutions and endodontic sealers on bond strength of the dentin-post in-
y The use of automatically mixed cement inserted into the terface with and without defects. Int J Med Sci 2012;9:642–654.
root canal using an endo tip statistically significantly re- 17. Halvorson RH, Erickson RL, Davidson CL. Energy dependent polymeriza-
tion of resin-based composite. Dent Mater 2002;18:463–469.
duced resin cement porosity. When the resin cement
18. Keleş A, Alcin H, Kamalak A, Versiani MA. Oval-shaped canal retreatment
was mixed manually and inserted into the root canal with self-adjusting file: a micro-computed tomography study. Clin Oral In-
using an endodontic file, the greatest porosity and low- vestig 2014;18:1147–1153.
est bond strength were observed. 19. Kim YK, Kim SK, Kim KH, Kwon TY. Degree of conversion of dual-cured
resin cement light-cured through three fibre posts within human root canals:
y Automatic mixing increased the bond strength and elimi- an ex vivo study. Int Endod J 2009;42:667–674.
nated the effect of the root region. 20. Lorenzoni FC, Bonfante EA, Bonfante G, Martins LM, Witek L, Silva NR.
y In general, RelyX U200 showed hgher bond strengths MicroCT analysis of a retrieved root restored with a bonded fiber-rein-
forced composite dowel: a pilot study. J Prosthodont 2013;22:478–483.
than did the other resin cements tested. 21. Lührs AK, De Munck J, Geurtsen W, Van Meerbeek B. Does inhibition of pro-
teolytic activity improve adhesive luting? Eur J Oral Sci 2013;121:121–131.
22. Mazzitelli C, Monticelli F, Toledano M, Ferrari M, Osorio R. Effect of ther-
mal cycling on the bond strength of self-adhesive cements to fiber posts.
Clin Oral Investig 2012;16:909–915.
23. Menezes MS, Faria-e-Silva AL, Silva FP, Reis GR, Soares CJ, Stape TH,
Martins LR. Etching a fiber post surface with high-concentration bleaching
ACKNOWLEDGEMENTS agents. Oper Dent 2014;39:16–21.
24. Monticelli F, Osorio R, Mazzitelli C, Ferrari M, Toledano M. Limited decalcifi-
This study was supported by Research Support FAPEMIG, Founda- cation/diffusion of self-adhesive cements into dentin. J Dent Res 2008;
tion of the State of Minas Gerais, CNPq and CAPES. 87:974–979.
Vol 21, No 1, 2019 45
da Silva et al
25. Nakabayashi N, Pashley DH. Hybridization of dental hard tissues. Quint- 38. Stona P, Borges GA, Montes MA, Júnior LH, Weber JB, Spohr AM. Effect
essence: Tokyo, 1998. of polyacrylic acid on the interface and bond strength of self-adhesive
26. Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival eval- resin cements to dentin. J Adhes Dent 2013;15:221–227.
uation for glass-fiber-supported post endodontic restoration: a prospec- 39. Swain MV, Xue J. State of the art of Micro-CT applications in dental re-
tive observational clinical study. J Endod 2012;38:432–435. search. Int J Oral Sci 2009;1:177–188.
27. Pedreira AP, D’Alpino PH, Pereira PN, Chaves SB, Wang L, Hilgert L, Gar- 40. Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangi-
cia FC. Effects of the application techniques of self-adhesive resin ce- ble goal. J Endod 2007;33:391–8.
ments on the interfacial integrity and bond strength of fiber posts to 41. Tay FR, Suh BI, Pashley DH, Prati C, Chuang SF, Li F. Factors contributing
dentin. J Appl Oral Sci 2016;24:437–446. to the incompatibility between simplified-step adhesives and self-cured or
28. Pedreira AP, Pegoraro LF, de Góes MF, Pegoraro TA, Carvalho RM. Micro- dual-cured composites. Part II. Single-bottle, total-etch adhesive. J Adhes
hardness of resin cements in the intraradicular environment: effects of Dent 2003;5:91–105.
water storage and softening treament. Dent Mater 2009;25:868–876. 42. Uzun İH, Malkoç MA, Keleş A, Öğreten AT. 3D micro-CT analysis of void
29. Pereira JR, Lins do Valle A, Ghizoni JS, Lorenzoni FC, Ramos MB, Dos formations and push-out bonding strength of resin cements used for fiber
Reis Só MV. Push-out bond strengths of different dental cements used to post cementation. J Adv Prosthodont 2016;8:101–109.
cement glass fiber posts. J Prosthet Dent 2013;110:134–140. 43. Van Landuyt KL, Yoshida Y, Hirata I, Snauwaert J, De Munck J, Okazaki
30. Pereira RD, Valdívia AD, Bicalho AA, Franco SD, Tantbirojn D, Versluis A, M, Suzuki K, Lambrechts P, Van Meerbeek B. Influence of the chemical
Soares CJ. Effect of photoactivation timing on the mechanical properties structure of functional monomers on their adhesive performance. J Dent
of resin cements and bond strength of fiberglass post to root dentin. Res 2008;87:757–761.
Oper Dent 2015;40:206–221. 44. Van Meerbeek B, Dhem A, Goret-Nicaise M, Braem M, Lambrechts P,
31. Pereira SG, Fulgêncio R, Nunes TG, Toledano M, Osorio R, Carvalho RM. VanHerle G. Comparative SEM and TEM examination of the ultrastructure
Effect of curing protocol on the polymerization of dual-cured resin ce- of the resin-dentin interdiffusion zone. J Dent Res 1993;72:495–501.
ments. Dent Mater 2010;26:710–718. 45. Watzke R, Blunck U, Frankenberger R, Naumann M. Interface homogeneity
32. Rengo C, Spagnuolo G, Ametrano G, Juloski J, Rengo S, Ferrari M. Micro- of adhesively luted glass fiber posts. Dent Mater 2008;24:1512–1517.
computerized tomographic analysis of premolars restored with oval and 46. Yang B, Ludwig K, Adelung R, Kern M. Micro-tensile bond strength of
circular posts. Clin Oral Investig 2014;18:571–578. three luting resins to human regional dentin. Dent Mater 2006;22:45–56.
33. Santos AF, Meira JB, Tanaka CB, Xavier TA, Ballester RY, Lima RG, 47. Zanatta RF, Barreto B de C, Xavier TA, Versluis A, Soares CJ. Effect of
Pfeifer CS, Versluis A. Can fiber posts increase root stresses and reduce punch and orifice base sizes in different push-out test setups: stress dis-
fracture? J Dent Res 2010;89:587–591. tribution analysis. J Adhes Dent 2015;17:45–50.
34. Sarkis-Onofre R, Skupien JA, Cenci MS, Moraes RR, Pereira-Cenci T. The
role of resin cement on bond strength of glass-fiber posts luted into root
canals: a systematic review and meta-analysis of in vitro studies. Oper
Dent 2014;39:E31–44.
35. Shiratori FK, Valle AL, Pegoraro TA, Carvalho RM, Pereira JR. Influence
of technique and manipulation on self-adhesive resin cements used to
cement intraradicular posts. J Prosthet Dent 2013;110:56–60. Clinical relevance: The use of a Centrix syringe for hand-
36. Skupien JA, Sarkis-Onofre R, Cenci MS, Moraes RR, Pereira-Cenci T. A sys-
tematic review of factors associated with the retention of glass fiber posts.
mixed resin cement insertion into the root canal and
Braz Oral Res 2015;29. doi: 10.1590/1807-3107BOR-2015.vol29.0074. preferential use of an auto-mixed resin cement inserted
37. Soares CJ, Raposo LH, Soares PV, Santos-Filho PC, Menezes MS, with an endo tip can improve the bond strength and re-
Soares PB, Magalhães D. Effect of different cements on the biomechani-
cal behavior of teeth restored with cast dowel-and-cores-in vitro and FEA duce resin cement porosity.
analysis. J Prosthodont 2010;19:130–137.
46 The Journal of Adhesive Dentistry
Copyright of Journal of Adhesive Dentistry is the property of Quintessence Publishing
Company Inc. and its content may not be copied or emailed to multiple sites or posted to a
listserv without the copyright holder's express written permission. However, users may print,
download, or email articles for individual use.
You might also like
- Accelerated Fatigue Resistance of Thick CAD/CAM Composite Resin Overlays Bonded With Light - and Dual-Polymerizing Luting ResinsDocument8 pagesAccelerated Fatigue Resistance of Thick CAD/CAM Composite Resin Overlays Bonded With Light - and Dual-Polymerizing Luting ResinsTiago SpeziaNo ratings yet
- Unconsolidated UndrainedDocument9 pagesUnconsolidated UndrainedMohd Syafiq Akmal100% (2)
- Universiti Malaysia Sarawak: Faculty of EngineeringDocument22 pagesUniversiti Malaysia Sarawak: Faculty of EngineeringAyish Cehcter100% (1)
- Canam Purlins and Girts Catalogue CanadaDocument0 pagesCanam Purlins and Girts Catalogue CanadasaivanvalendezNo ratings yet
- CL 303-Assignment No.1Document2 pagesCL 303-Assignment No.1Vineeth Dasaraju0% (1)
- Limestone FGD ScrubbersDocument575 pagesLimestone FGD ScrubbersAnonymous Cxriyx9HIX100% (3)
- Bouillaguet 2003Document7 pagesBouillaguet 2003valperlunNo ratings yet
- Ari 15Document6 pagesAri 15mariaNo ratings yet
- 10 3290@j Jad A43609Document8 pages10 3290@j Jad A43609ilich sevillaNo ratings yet
- 1989 15557 2 PBDocument11 pages1989 15557 2 PBEduardo FernandezNo ratings yet
- 1 s2.0 S0022391310601114 Main PDFDocument9 pages1 s2.0 S0022391310601114 Main PDFPatty ChuNo ratings yet
- Bulk Fill Resin RestorationDocument18 pagesBulk Fill Resin RestorationNuningK93No ratings yet
- SEM Evaluation of The Cement Layer Thickness After Luting Two Different PostsDocument7 pagesSEM Evaluation of The Cement Layer Thickness After Luting Two Different PostsEdgar Pingo CampuzanoNo ratings yet
- Void and Gap Evaluation Using Microcomputed Tomography of Different Fiber Post Cementation TechniquesDocument5 pagesVoid and Gap Evaluation Using Microcomputed Tomography of Different Fiber Post Cementation TechniquesOskar OrtizNo ratings yet
- Dry-Bonding Etch-and-Rinse Strategy Improves Bond Longevity of A Universal Adhesive To Sound and Artificially-Induced Caries-Affected Primary DentinDocument9 pagesDry-Bonding Etch-and-Rinse Strategy Improves Bond Longevity of A Universal Adhesive To Sound and Artificially-Induced Caries-Affected Primary DentinRitter Adolfo OlivaresNo ratings yet
- Clinical Evaluation of Indirect Composite Resin Restorations Cemented With Different Resin CementsDocument9 pagesClinical Evaluation of Indirect Composite Resin Restorations Cemented With Different Resin CementsJoshua ValdezNo ratings yet
- Influence of Operator Experience On in Vitro Bond Strength of Dentin AdhesivesDocument5 pagesInfluence of Operator Experience On in Vitro Bond Strength of Dentin AdhesivesdanielaNo ratings yet
- Effect of Surface Treatment of Fiberglass Posts On Bond Strength To Root DentinDocument7 pagesEffect of Surface Treatment of Fiberglass Posts On Bond Strength To Root DentinKatherine Kelly Povis AresteguiNo ratings yet
- Does MTA Affect Fiber Post Retention in Repaired Cervical Root Canal PerforationsDocument7 pagesDoes MTA Affect Fiber Post Retention in Repaired Cervical Root Canal PerforationsAmanda Dos SantosNo ratings yet
- Pivoti 2011Document4 pagesPivoti 2011Carmen Breban CirțiuNo ratings yet
- Effect of Resin CementDocument7 pagesEffect of Resin Cementgerardo jimenezNo ratings yet
- BioDocument6 pagesBiomanar alsoltanNo ratings yet
- 10 3290@j Jad A42510Document9 pages10 3290@j Jad A42510Iván ForeroNo ratings yet
- Effect of Resin-Modified Glass-Ionomer Cement Lining and Composite Layering Technique On The Adhesive Interface of Lateral WallDocument6 pagesEffect of Resin-Modified Glass-Ionomer Cement Lining and Composite Layering Technique On The Adhesive Interface of Lateral WallAini Dwi HandiniNo ratings yet
- Effect of Irrigation Protocol During Post Space Preparation On The Dentin Adhesive Interface - An in Vitro StudyDocument9 pagesEffect of Irrigation Protocol During Post Space Preparation On The Dentin Adhesive Interface - An in Vitro StudyMayra Ortiz HerreraNo ratings yet
- Bond Strength of A Flowable Bulk-Fill Resin CompositeDocument7 pagesBond Strength of A Flowable Bulk-Fill Resin CompositeadzhanahadyanNo ratings yet
- Bulk Fill Case 2 PDFDocument6 pagesBulk Fill Case 2 PDFAnonymous SZqzD30YNo ratings yet
- Effect of Cementation Protocol On Push-Out Bond Strength of Fiber Posts To Root CanalDocument7 pagesEffect of Cementation Protocol On Push-Out Bond Strength of Fiber Posts To Root Canalgerardo jimenezNo ratings yet
- Effects of Fiber-Reinforced Composite Bases On Microleakage of Compos - Ite Restorations in Proximal LocationsDocument7 pagesEffects of Fiber-Reinforced Composite Bases On Microleakage of Compos - Ite Restorations in Proximal Locationsmaroun ghalebNo ratings yet
- Microtensile Bond Strength of Adhesive Systems in Different Dentin Regions On A Class II Cavity ConfigurationDocument8 pagesMicrotensile Bond Strength of Adhesive Systems in Different Dentin Regions On A Class II Cavity ConfigurationSinai AriasNo ratings yet
- Microleakage in Conventional and Bonded Amalgam Restorations: Influence of Cavity VolumeDocument7 pagesMicroleakage in Conventional and Bonded Amalgam Restorations: Influence of Cavity Volumegr_saini17768No ratings yet
- Joddd 12 140 PDFDocument6 pagesJoddd 12 140 PDFJessicaLisaNugrohoNo ratings yet
- The Effect of Immediate Dentin Sealing On The Marginal Adaptation and Bond Strengths of Total-Etch and Self-Etch AdhesivesDocument9 pagesThe Effect of Immediate Dentin Sealing On The Marginal Adaptation and Bond Strengths of Total-Etch and Self-Etch AdhesivesclaudiaNo ratings yet
- Microfiltracion en CarillasDocument6 pagesMicrofiltracion en CarillasCdjuan GnNo ratings yet
- In VivoDocument6 pagesIn Vivoo_eisa2002No ratings yet
- Effect of Tooth Substrate and Porcelain Thickness On Porcelain - Veneer Failure Loads in Vitro PDFDocument7 pagesEffect of Tooth Substrate and Porcelain Thickness On Porcelain - Veneer Failure Loads in Vitro PDFSgNo ratings yet
- Borzangy, 2019Document8 pagesBorzangy, 2019phaelzanonNo ratings yet
- Degradacion de Interfase 2Document25 pagesDegradacion de Interfase 2Sofía TrianaNo ratings yet
- 43Document9 pages43Fatimah DewiNo ratings yet
- Endo Article 1Document7 pagesEndo Article 1Alina AlexandraNo ratings yet
- Proenca 2007Document7 pagesProenca 2007valperlunNo ratings yet
- Effect of Different CAD-CAM Materials On The Marginal and Internal Adaptation of Endocrown Restorations: An in Vitro StudyDocument7 pagesEffect of Different CAD-CAM Materials On The Marginal and Internal Adaptation of Endocrown Restorations: An in Vitro StudyNetra TaleleNo ratings yet
- Evaluaci-N ÊÊdel ÊÊProtocoloÊ Êde ÊÊLimpieza ÊÊdelÊ ConductoÊ ÊRadicular Sobre La ÊÊResistencia ÊdeÊÊlaÊ ÊUni-n ÊÊdeÊ ÊPostes ÊdeÊ FibraÊÊde ÊÊVidriODocument7 pagesEvaluaci-N ÊÊdel ÊÊProtocoloÊ Êde ÊÊLimpieza ÊÊdelÊ ConductoÊ ÊRadicular Sobre La ÊÊResistencia ÊdeÊÊlaÊ ÊUni-n ÊÊdeÊ ÊPostes ÊdeÊ FibraÊÊde ÊÊVidriOjhompaz387No ratings yet
- Effect of Root Canal Sealers On Bond Strength of Fibreglass Posts Cemented With Self-Adhesive Resin CementsDocument7 pagesEffect of Root Canal Sealers On Bond Strength of Fibreglass Posts Cemented With Self-Adhesive Resin Cementswuhan lalalaNo ratings yet
- Jukka MatilanaDocument41 pagesJukka Matilanamilleny faizaNo ratings yet
- Comparison of Different Dentin Pretreatment Protocols On The Bond Strength of Glass Fiber Post Using Self-Etching AdhesiveDocument5 pagesComparison of Different Dentin Pretreatment Protocols On The Bond Strength of Glass Fiber Post Using Self-Etching AdhesivedrvenegascesfamromeralNo ratings yet
- Influence of Obturation Technique On Penetration Depth and AdaptationDocument13 pagesInfluence of Obturation Technique On Penetration Depth and AdaptationRaúl Jara CorvalánNo ratings yet
- 01 Mahidol Dental Journal 3 2020Document10 pages01 Mahidol Dental Journal 3 2020shafira zulvaNo ratings yet
- Effectiveness of Seven Types of Sealants Retention After One YearDocument6 pagesEffectiveness of Seven Types of Sealants Retention After One YearJoseph EneroNo ratings yet
- Effect of Etching The Coronal Dentin With The RubbDocument6 pagesEffect of Etching The Coronal Dentin With The Rubbmaroun ghalebNo ratings yet
- Reconstruction of Devital Teeth Using Direct Fiber-Reinforced Composite Resins: A Case ReportDocument7 pagesReconstruction of Devital Teeth Using Direct Fiber-Reinforced Composite Resins: A Case ReportAngga RanggaNo ratings yet
- 1-5 Sisteme AdeziveDocument10 pages1-5 Sisteme AdezivestuparusamiNo ratings yet
- Back To Back Composite RestorationsDocument10 pagesBack To Back Composite RestorationsAli AhmadNo ratings yet
- Effect of Composite Insertion Technique On Cuspal DeflectionDocument7 pagesEffect of Composite Insertion Technique On Cuspal DeflectionYaniuska ContrerasNo ratings yet
- Longevida Adhesivos-5Document25 pagesLongevida Adhesivos-5Camila Conejeros ArriagadaNo ratings yet
- Burbridge2007 NoDocument6 pagesBurbridge2007 NoKatherine VilchezNo ratings yet
- Effects of composite resin core level and periodontal pocket depth on crack propagation in endodontically treated teeth An extended finite element method studyDocument7 pagesEffects of composite resin core level and periodontal pocket depth on crack propagation in endodontically treated teeth An extended finite element method study李雲龍No ratings yet
- Fiber PostsDocument4 pagesFiber PostsNeha AroraNo ratings yet
- Shear Bond Strength of Porcelain Laminate Veneers To Enamel, Dentine and Enamel-Dentine Complex Bonded With Different Adhesive Luting Systems PDFDocument9 pagesShear Bond Strength of Porcelain Laminate Veneers To Enamel, Dentine and Enamel-Dentine Complex Bonded With Different Adhesive Luting Systems PDFLuis Alberto Carpio MorenoNo ratings yet
- TMP 67 ABDocument10 pagesTMP 67 ABFrontiersNo ratings yet
- ResilonDocument33 pagesResilonhasNo ratings yet
- Minimally Invasive Vertical Preparation Design For Ceramic VeneersDocument12 pagesMinimally Invasive Vertical Preparation Design For Ceramic VeneersdanielaNo ratings yet
- Fiber Posts Cementation TechniquesDocument4 pagesFiber Posts Cementation TechniquesAD TwentyOne Dental100% (1)
- Esthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsFrom EverandEsthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsRichard D. TrushkowskyNo ratings yet
- Chart Projections PDFDocument2 pagesChart Projections PDFSanjay WaghmodeNo ratings yet
- Reduction of Stress Concentration in Bolt Nut ConnectorsDocument6 pagesReduction of Stress Concentration in Bolt Nut ConnectorsjtorerocNo ratings yet
- Sample Birth Chart Analysis - Gann Astrononamy.336174811Document14 pagesSample Birth Chart Analysis - Gann Astrononamy.336174811Hitesh PatelNo ratings yet
- Blood RheologyDocument122 pagesBlood RheologyCharu MallNo ratings yet
- Computer Aided Analysis of The Structural Behaviour of Sloped Open Lattice Towers 1Document24 pagesComputer Aided Analysis of The Structural Behaviour of Sloped Open Lattice Towers 1Oladunni AfolabiNo ratings yet
- 371 ARMOX 370T Class1 UK Data SheetDocument2 pages371 ARMOX 370T Class1 UK Data SheetemregnesNo ratings yet
- Laboratory Specific Appendix I - SOP TemplateDocument13 pagesLaboratory Specific Appendix I - SOP TemplateBalachandar KumarNo ratings yet
- P Sheet 8 Linearization SolutionDocument3 pagesP Sheet 8 Linearization Solutionxtito2No ratings yet
- Pavagada Cengrs PagesDocument25 pagesPavagada Cengrs PagesswapneelkalraNo ratings yet
- Gas Laws Station KeyDocument5 pagesGas Laws Station Keyapi-332249032No ratings yet
- Bermuda and Dragon TriangleDocument2 pagesBermuda and Dragon TriangleSyed Mohsin Ali NaqviNo ratings yet
- Building Services - Iv Lighting and Electrical ServicesDocument19 pagesBuilding Services - Iv Lighting and Electrical ServicesankurNo ratings yet
- KSPedia XB1 PDFDocument156 pagesKSPedia XB1 PDFThe Lord Of The CraftNo ratings yet
- Lab For AP ChemistryDocument8 pagesLab For AP ChemistryCliff LiuNo ratings yet
- Design of Steel Structure 9084Document5 pagesDesign of Steel Structure 9084Shajit Kumar0% (1)
- Experiment 5 CreepDocument7 pagesExperiment 5 CreepRashedul IslamNo ratings yet
- Sci Pptq1 Wk1 Day 1-5Document68 pagesSci Pptq1 Wk1 Day 1-5Che LV100% (1)
- Direct Variation: Whatisitandhowdoiknowwheniseeit?Document23 pagesDirect Variation: Whatisitandhowdoiknowwheniseeit?saturnino corpuzNo ratings yet
- Ultrasonic 10Document5 pagesUltrasonic 10Mahade Hasan Dipu100% (1)
- UG 45 CalculationDocument7 pagesUG 45 CalculationnirgaNo ratings yet
- Wlt002-E-P-A00 - Well Data InterpretationDocument125 pagesWlt002-E-P-A00 - Well Data InterpretationSlim.BNo ratings yet
- RefrigeratorDocument6 pagesRefrigeratorChooi San LaiNo ratings yet
- Verification of ODOT's Load RatingDocument277 pagesVerification of ODOT's Load RatingVietanh Phung100% (1)
- DLL Science 8Document7 pagesDLL Science 8Mark Anthony Telan Pitogo0% (1)
- Internal Friction of Materials Anton PuskarDocument342 pagesInternal Friction of Materials Anton PuskarhezihilikNo ratings yet