Professional Documents
Culture Documents
Schizofrenia
Schizofrenia
Uploaded by
Chirita Elena0 ratings0% found this document useful (0 votes)
21 views2 pagesipoteza neurochimica
Original Title
schizofrenia
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentipoteza neurochimica
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
21 views2 pagesSchizofrenia
Schizofrenia
Uploaded by
Chirita Elenaipoteza neurochimica
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
Neurochemical Hypotheses
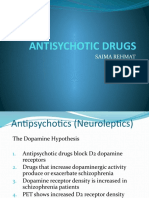
The Dopamine Hypothesis
The dopamine hypothesis postulates that the symptoms of schizophrenia result from
dysregulation of dopamine in the CNS. Four dopaminergic anatomical pathways are described
in this model. The mesolimbic pathway projects from the ventral tegmental area
(VTA) to limbic areas. Excessive mesolimbic dopamine may lead to positive symptoms of
schizophrenia, such as delusions and hallucinations. The mesocortical pathway projects
from VTA to cortex, particularly prefrontal cortex. Low mesocortical dopamine is proposed
to cause the negative symptoms and cognitive deficits of schizophrenia. The
nigrostriatal pathway, from the substantia nigra to the striatum, regulates movements;
low nigrostriatal dopamine leads to Parkinsonian motor symptoms. The tuberoinfundibular
pathway travels from the hypothalamus to the pituitary gland and inhibits prolactin secretion;
blockade of tuberoinfundibular dopamine leads to elevated prolactin and resultant
galactorrhea, amenorrhea, and decreased libido.
There remains some controversy over the role of excess mesolimbic dopamine in psychosis.
On the one hand, drug effects support this model: Dopamine agonists such as amphetamines
and cocaine provoke psychotic symptoms in normal subjects and those with
schizophrenia; likewise, effective antipsychotic drugs bind and block the D2 subtype of
dopamine receptors. Early studies showed increased dopamine metabolites and dopamine
receptors in schizophrenia. Positron emission tomography (PET) imaging studies confirm
increased synthesis of dopamine, increased levels of synaptic dopamine, and increased
dopamine release in response to stressors such as amphetamine challenge.
On the other hand, increased levels of mesolimbic dopamine and dopamine receptors
have not been consistently shown across studies and remain controversial. Furthermore,
many cases of schizophrenia are unresponsive to D2 blockade. Finally, some antipsychotic
drugs, such as the atypical agent clozapine, have relatively poor D2 binding,
which suggests that other neurotransmitters or receptors may be involved. On the whole,
current evidence appears to support a central role for striatal D2 receptors in acute psychosis.
The role of low mesocortical dopamine in negative and cognitive symptoms is also
controversial. On the one hand, a correlation has been shown between low levels of dopamine
metabolites in cerebrospinal fluid (CSF), low cortical dopamine, and the poor
performance on working memory tasks are seen in schizophrenia. Likewise, dopamine
agonists improve prefrontal activation and cognitive performance in schizophrenia. Yet
postmortem studies have not clearly shown altered dopamine receptor levels in prefrontal
cortex in patients with schizophrenia. PET studies have shown increased, decreased, or
unchanged receptor levels, depending on the radiotracer used. It has been proposed that
increases may actually reflect compensation for low prefrontal dopamine levels; this
would make the significance of either an increase or decrease unclear.
It is possible that the ongoing controversies over the role of dopamine in positive and
negative symptoms results in part from the crudeness of available measuring techniques.
Dopamine is thought to help define and “sharpen” cortical representations of sensation
and action, enhancing salient patterns and dampening nonsalient ones. Attempting to explain
brain dysfunction in terms of simple increases or decreases in dopamine may therefore
be as futile as trying to measure the accuracy of a drawing by how much ink it contains.
Subtle dysregulation of dopamine, whether in prefrontal cortex or striatum, could
cause major deficits in information processing without overall excess or lack of dopamine.
The Glutamate Hypothesis
The glutamate hypothesis proposes that dysfunction of the N-methyl-D-aspartate (NMDA)
glutamate receptor is the primary deficit underlying all the positive, negative, and cognitive
symptoms of schizophrenia. Glutamate is the major excitatory neurotransmitter in
the CNS. The NMDA receptor plays key roles in attention, perception, and cognition.
Importantly, this receptor also plays critical roles in developmental processes such as
axonal guidance, synaptic pruning, and plasticity, both in utero and during adolescence.
For these reasons, the NMDA receptor is an attractive target for schizophrenia research.
As with the dopamine hypothesis, the glutamate hypothesis originates in early findings
of low glutamate levels in the CSF of patients with schizophrenia, and in the observation
that the effects of NMDA antagonist drugs (ketamine, phencyclidine [PCP]) mimic
some of the positive, negative, and cognitive features of schizophrenia. Postmortem studies
show changes in the expression of NMDA receptors and their related proteins in
schizophrenia. Many genes conferring schizophrenia risk appear to interact with the
NMDA receptor in some way (such as GRM3, described earlier). Recent PET imaging
also suggests reduced hippocampal NMDA receptor binding in schizophrenia.
Glutamate models may be able to accommodate existing dopamine-centered hypotheses
on schizophrenia. In one model, reduced prefrontal glutamate neurotransmission
leads to reduced prefrontal activity. This results in decreased mesocortical activity, causing
negative and cognitive symptoms. It also results in a loss of regulation in the
mesolimbic projections. This pathway becomes hyperresponsive to stress or pharmacological
challenge, leading to acute episodes of psychosis. Of note here, cannabis reduces
corticostriatal glutamate release, while D2 receptor blockade increases glutamate release.
Dopamine–glutamate models may be able to explain how cannabis and dopamine
agonists provoke psychosis, and how D2 antagonists improve positive symptoms.
Glutamate-centered theories offer a potential means of unifying genetic, developmental,
neuropathological, and neurochemical understanding of schizophrenia. Lines of
supporting evidence for NMDA-related dysfunction in schizophrenia are beginning to
emerge. Research over the next few years should determine whether this trend continues,
and whether the glutamate hypothesis can inspire new approaches to treatment.
You might also like
- DOPAMINE SYN, TRAN, DEGR and ReceptorsDocument15 pagesDOPAMINE SYN, TRAN, DEGR and ReceptorsRaghuram MiryalaNo ratings yet
- Mechanism of Action of AriprazoleDocument5 pagesMechanism of Action of AriprazoleSiegfried CristoforNo ratings yet
- Neurotransmitters in Schizophrenia: Dr. Adel El SheshaiDocument47 pagesNeurotransmitters in Schizophrenia: Dr. Adel El SheshaielvinegunawanNo ratings yet
- McCutcheon Et Al-2020-World PsychiatryDocument19 pagesMcCutcheon Et Al-2020-World PsychiatryRob McCutcheonNo ratings yet
- Glutamate Neurotransmission in Psychotic Disorders and Substance AbuseDocument8 pagesGlutamate Neurotransmission in Psychotic Disorders and Substance AbuseLeanne MontgomeryNo ratings yet
- Dopamine Hypothesis of SchizophreniaDocument2 pagesDopamine Hypothesis of SchizophreniaCaspal OkeloNo ratings yet
- The Dopamine Hypothesis of SchizophreniaDocument8 pagesThe Dopamine Hypothesis of SchizophreniaRobert Selvin MNo ratings yet
- Ezqui y DopaDocument7 pagesEzqui y DopaJuanAmayaNo ratings yet
- Dopaminergic Pathways - LAGDocument30 pagesDopaminergic Pathways - LAGalvinbb100% (1)
- Write An Essay On Schizophrenia and The Drugs That Can Be Used To Treat It IIDocument4 pagesWrite An Essay On Schizophrenia and The Drugs That Can Be Used To Treat It IIscholifyNo ratings yet
- tmpFF8C TMPDocument11 pagestmpFF8C TMPFrontiersNo ratings yet
- The Neurochemistry in Schizophrenia, Bipolar and Major Depressive DisorderDocument1 pageThe Neurochemistry in Schizophrenia, Bipolar and Major Depressive DisorderMeenakshianandi KrishnanNo ratings yet
- Cure For Schizophrenia A Journey Can Biological Control Systems Be The Answer To Chemical Regulation?Document54 pagesCure For Schizophrenia A Journey Can Biological Control Systems Be The Answer To Chemical Regulation?Mushahid100% (1)
- Neurophysiology of SchizophreniaDocument14 pagesNeurophysiology of SchizophreniaShivan A.C.No ratings yet
- Schizophrenia DiseaseDocument6 pagesSchizophrenia DiseasemarkNo ratings yet
- Glutamatergic Theories of Schizophrenia: Daniel C. Javitt, MD, PHDDocument13 pagesGlutamatergic Theories of Schizophrenia: Daniel C. Javitt, MD, PHDlooolNo ratings yet
- WPS 15 03Document2 pagesWPS 15 03João Paulo AtidioNo ratings yet
- Testing The Glutamate Hypothesis of SchizophreniaDocument3 pagesTesting The Glutamate Hypothesis of SchizophreniaJohn000123No ratings yet
- Farmakologi ParkinsonsDocument12 pagesFarmakologi ParkinsonsAnisa DwiiNo ratings yet
- Schizophrenia: From Dopamine To Glutamate and Back: M.L. Carlsson, A. Carlsson and M. NilssonDocument11 pagesSchizophrenia: From Dopamine To Glutamate and Back: M.L. Carlsson, A. Carlsson and M. Nilssonbasit khanNo ratings yet
- Dopa RewardDocument8 pagesDopa RewardDenia Méndez ÁlvarezNo ratings yet
- Schizo CauseDocument2 pagesSchizo CauseNaum GrbicNo ratings yet
- AntipsychoticsDocument52 pagesAntipsychoticsNoor Ul AinNo ratings yet
- PHA3032 Notes: Theme 2: Pharmacology of Mood and BehaviourDocument45 pagesPHA3032 Notes: Theme 2: Pharmacology of Mood and BehaviourJoshuaWestNo ratings yet
- Neurotransmitters Safeya EffatDocument15 pagesNeurotransmitters Safeya Effatصالح الحديديNo ratings yet
- Biological FactorsDocument3 pagesBiological FactorsDEEPIKA PREMLAL 2170101No ratings yet
- Describing An Atypical Antipsychotic: Receptor Binding and Its Role in PathophysiologyDocument5 pagesDescribing An Atypical Antipsychotic: Receptor Binding and Its Role in PathophysiologyZulay BohorquezNo ratings yet
- DopamineDocument1 pageDopamineThe LullabyNo ratings yet
- Antisychotic Drugs: Saima RehmatDocument23 pagesAntisychotic Drugs: Saima RehmatSaima IftikharNo ratings yet
- Striatal Dopamine Synthesis Capacity in Autism Spectrum Disorder and Its Relation With Social Defeat: An (F) - FDOPA PET/CT StudyDocument10 pagesStriatal Dopamine Synthesis Capacity in Autism Spectrum Disorder and Its Relation With Social Defeat: An (F) - FDOPA PET/CT StudyAleksandra PanasikNo ratings yet
- Neurotransmitter DisturbancesDocument2 pagesNeurotransmitter DisturbancesNi'matul Muthmainnah SyariefNo ratings yet
- Neurotransmitter DisturbancesDocument2 pagesNeurotransmitter DisturbancesNi'matul Muthmainnah SyariefNo ratings yet
- Neuroleptics & AnxiolyticsDocument65 pagesNeuroleptics & AnxiolyticsAntonPurpurovNo ratings yet
- Serotonina y Depresioì N 1 PDFDocument8 pagesSerotonina y Depresioì N 1 PDFJenniferNo ratings yet
- Dopamin: Nur Fadhillah Khalid (P062181024) Mata Kuliah: NeurontrasmitterDocument27 pagesDopamin: Nur Fadhillah Khalid (P062181024) Mata Kuliah: Neurontrasmitternur fadhillah khalidNo ratings yet
- Faktor Neurobiologi: Qara Syifa Fachrani 1610211039Document22 pagesFaktor Neurobiologi: Qara Syifa Fachrani 1610211039Qara Syifa FNo ratings yet
- Targeting G Protein-Coupled ReceptorsDocument26 pagesTargeting G Protein-Coupled ReceptorsNorkelys ParraNo ratings yet
- Mechanism of Action of Ariprazole PDFDocument5 pagesMechanism of Action of Ariprazole PDFDio PattersonNo ratings yet
- Receptors Involved in Mental Disorders and The UseDocument17 pagesReceptors Involved in Mental Disorders and The Usedabafe4365No ratings yet
- Mood Disorders Short EssayDocument4 pagesMood Disorders Short EssayscholifyNo ratings yet
- MX Accion AdrenergecosDocument7 pagesMX Accion Adrenergecosetbriali84No ratings yet
- Imbalance of DopamineDocument1 pageImbalance of DopamineKayla EspositoNo ratings yet
- Schizophrenia: DR - RahmanDocument17 pagesSchizophrenia: DR - RahmanPineappleNo ratings yet
- Schizophrenia AdditionDocument2 pagesSchizophrenia Additionkatts4uNo ratings yet
- Neurophysiology of Depression and Bipolar Affective DisorderDocument17 pagesNeurophysiology of Depression and Bipolar Affective DisorderShivan A.C.No ratings yet
- Molecular NeurobiologyDocument17 pagesMolecular NeurobiologypairednursingNo ratings yet
- Antidepressant and AntimanicDocument60 pagesAntidepressant and Antimanictbuyinza21apNo ratings yet
- En 26 11Document14 pagesEn 26 11Mitchel Cordova LoaizaNo ratings yet
- Saliencia y Dopamina en Psicosis 2Document14 pagesSaliencia y Dopamina en Psicosis 2Julián PNo ratings yet
- Inhibitory NeurotransmittersDocument11 pagesInhibitory NeurotransmittersAi NeeriNo ratings yet
- Dopamine HypothesisDocument12 pagesDopamine HypothesisAndrew ThompsonNo ratings yet
- Anti Psychotic DrugsDocument67 pagesAnti Psychotic DrugsAhmed Osman100% (1)
- Neurological ControlDocument7 pagesNeurological ControlPrabha Amandari SutyandiNo ratings yet
- Overview CNS Chemical TransmissionDocument75 pagesOverview CNS Chemical TransmissionsaivasyaNo ratings yet
- Timmermann - Neurociencias y Aplicaciones Psicoterapéuticas en El Renacimiento de La Investigación Con PsicodélicosDocument8 pagesTimmermann - Neurociencias y Aplicaciones Psicoterapéuticas en El Renacimiento de La Investigación Con PsicodélicosNicolás BerasainNo ratings yet
- Chapter 4: Psychotropic Drugs: Structure and Function of The BrainDocument9 pagesChapter 4: Psychotropic Drugs: Structure and Function of The BrainciaraNo ratings yet
- Antipsychotic DrugsDocument18 pagesAntipsychotic DrugsJohn HolmesNo ratings yet
- A Critique of The Dopamine Hypothesis of Schizophrenia and PsychosisDocument12 pagesA Critique of The Dopamine Hypothesis of Schizophrenia and PsychosisXaviNo ratings yet
- Dopamine Pathways PDFDocument3 pagesDopamine Pathways PDFMuhammad Zul Fahmi AkbarNo ratings yet
- Politrauma - Rolul AtiDocument18 pagesPolitrauma - Rolul AtiChirita ElenaNo ratings yet
- Trauma Scor 1Document2 pagesTrauma Scor 1Chirita ElenaNo ratings yet
- Topic - 2 Initial Resuscitation of The Injured PatientDocument1 pageTopic - 2 Initial Resuscitation of The Injured PatientChirita ElenaNo ratings yet
- Bruce Lee Workout PDFDocument1 pageBruce Lee Workout PDFChirita ElenaNo ratings yet
- 90 Days of ActionDocument95 pages90 Days of ActionChirita ElenaNo ratings yet
- 0 For Mule Pen True LeviDocument4 pages0 For Mule Pen True LeviChirita Elena0% (1)
- Dezvoltarea CopiluluiDocument15 pagesDezvoltarea CopiluluiChirita ElenaNo ratings yet
- Ket 3xtDocument9 pagesKet 3xtMiXit LivesNo ratings yet
- CNS NeurotransmittersDocument30 pagesCNS Neurotransmittersdevanshi_582262183100% (2)
- Treatments For Schizophrenia: A Critical Review of Pharmacology and Mechanisms of Action of Antipsychotic DrugsDocument26 pagesTreatments For Schizophrenia: A Critical Review of Pharmacology and Mechanisms of Action of Antipsychotic DrugsMaria Jose CastañedaNo ratings yet
- Psicobiologia Del Aprendizaje y La Memoria, Fundamentos y AvancesDocument9 pagesPsicobiologia Del Aprendizaje y La Memoria, Fundamentos y AvancesErika AlvarezNo ratings yet
- Restoration of GABAA Receptor Function After Benzodiazepine Use - A Meta-AnalysisDocument19 pagesRestoration of GABAA Receptor Function After Benzodiazepine Use - A Meta-AnalysisLucasNo ratings yet
- Methamphetamine-Associated PsychosisDocument27 pagesMethamphetamine-Associated PsychosisJoyster Avila100% (1)
- NMA, NMDA and DAA ComparisonDocument9 pagesNMA, NMDA and DAA ComparisonAlfred FrancoNo ratings yet
- Case Study LFDocument35 pagesCase Study LFAlnah Debuque AlihuddinNo ratings yet
- Anestesia General Franks 2008 PDFDocument17 pagesAnestesia General Franks 2008 PDFPablo Lukacs CarmonaNo ratings yet
- Cell Death in Weaver Mouse Cerebellum: Amy B Harkins and Aaron P FoxDocument6 pagesCell Death in Weaver Mouse Cerebellum: Amy B Harkins and Aaron P FoxdupuytrenNo ratings yet
- Effects of Sodium Benzoate, A Commonly Used Food Preservative, On Learning, Memory, and Oxidative Stress in Brain of MiceDocument8 pagesEffects of Sodium Benzoate, A Commonly Used Food Preservative, On Learning, Memory, and Oxidative Stress in Brain of MiceBenson Ha.No ratings yet
- Neurotransmitters - 2016Document183 pagesNeurotransmitters - 2016AdminNo ratings yet
- Mechanisms of Action of Antiepileptic DrugsDocument7 pagesMechanisms of Action of Antiepileptic DrugsKenya Nicole CosteNo ratings yet
- Augmentation Strategies in Obsessive Compulsive DisorderDocument18 pagesAugmentation Strategies in Obsessive Compulsive DisorderLucijano Andreas SoftićNo ratings yet
- HHS Public Access: Molecular Mechanisms of Aluminum Neurotoxicity: Update On Adverse Effects and Therapeutic StrategiesDocument31 pagesHHS Public Access: Molecular Mechanisms of Aluminum Neurotoxicity: Update On Adverse Effects and Therapeutic Strategiesfajriana anggun putri amranNo ratings yet
- Brain Plasticity in Paediatric NeurologyDocument9 pagesBrain Plasticity in Paediatric NeurologySakinah A WandiraNo ratings yet
- Neuro - Synaptic TransmissionDocument74 pagesNeuro - Synaptic TransmissionSteve BlubaughNo ratings yet
- IBRO APRC Banasthali School Abstracts 2017Document25 pagesIBRO APRC Banasthali School Abstracts 2017International Brain Research OrganizationNo ratings yet
- The Missing Piece A Case For Microglia's Prominent Role in The Therapeutic Action of Anesthetics, Ketamine, and PsychedelicsDocument38 pagesThe Missing Piece A Case For Microglia's Prominent Role in The Therapeutic Action of Anesthetics, Ketamine, and PsychedelicsMoo GeeNo ratings yet
- The 100 Articles by Burhan ReadingDocument213 pagesThe 100 Articles by Burhan ReadingMD Sheikh SadiNo ratings yet
- Protocolos Pulsed PariedDocument13 pagesProtocolos Pulsed PariedAugusto ManoelNo ratings yet
- Intravenous Sub-Anesthetic Ketamine For Perioperative AnalgesiaDocument8 pagesIntravenous Sub-Anesthetic Ketamine For Perioperative AnalgesiaAraNo ratings yet
- Ketamine - New TricksDocument9 pagesKetamine - New TricksIftach HuebnerNo ratings yet
- Animal Models of Neuropsychiatric DisordersDocument18 pagesAnimal Models of Neuropsychiatric DisordersRodrigo CastroNo ratings yet
- Pediatrics in Review 1998 Stafstrom 342 51Document12 pagesPediatrics in Review 1998 Stafstrom 342 51Syafiq IshakNo ratings yet
- The Neurobiology of Addictive DisordersDocument8 pagesThe Neurobiology of Addictive DisordersDee DeeNo ratings yet
- Perinatal Asphyxia - Outline of Pathophysiology and Recent Trends in ManagementDocument31 pagesPerinatal Asphyxia - Outline of Pathophysiology and Recent Trends in Managementokwadha simionNo ratings yet
- Anasthesia Handout - Final-9awa3i8 PDFDocument148 pagesAnasthesia Handout - Final-9awa3i8 PDFNatosha MillerNo ratings yet
- Eervc 2019 Proceedings PDFDocument290 pagesEervc 2019 Proceedings PDFSmee VeselinovNo ratings yet
- 2017 Microwave Radiation and Brain Memory LossDocument14 pages2017 Microwave Radiation and Brain Memory LossPirate CeoNo ratings yet