Professional Documents
Culture Documents
Chapter 40-Oxygenation
Chapter 40-Oxygenation
Uploaded by
Haji Raji0 ratings0% found this document useful (0 votes)
258 views14 pagesThis document summarizes cardiovascular and respiratory physiology as it relates to oxygenation. It describes:
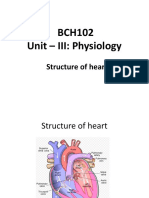
1) The structure and function of the heart including the coronary arteries, conduction system, and factors affecting stroke volume.
2) The structure and function of the respiratory system including ventilation, perfusion, gas exchange, and regulation of respiration.
3) How physiological factors like cardiac output, lung volumes, diffusion, and oxygen carrying capacity influence oxygen delivery to tissues.
Original Description:
Original Title
Chapter 40—Oxygenation
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes cardiovascular and respiratory physiology as it relates to oxygenation. It describes:
1) The structure and function of the heart including the coronary arteries, conduction system, and factors affecting stroke volume.
2) The structure and function of the respiratory system including ventilation, perfusion, gas exchange, and regulation of respiration.
3) How physiological factors like cardiac output, lung volumes, diffusion, and oxygen carrying capacity influence oxygen delivery to tissues.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
258 views14 pagesChapter 40-Oxygenation
Chapter 40-Oxygenation
Uploaded by
Haji RajiThis document summarizes cardiovascular and respiratory physiology as it relates to oxygenation. It describes:
1) The structure and function of the heart including the coronary arteries, conduction system, and factors affecting stroke volume.
2) The structure and function of the respiratory system including ventilation, perfusion, gas exchange, and regulation of respiration.
3) How physiological factors like cardiac output, lung volumes, diffusion, and oxygen carrying capacity influence oxygen delivery to tissues.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 14
Chapter 40—Oxygenation
Scientific Knowledge Base
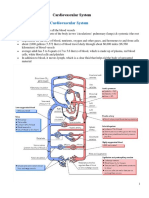
o Cardiovascular physiology
Structure and function
Myocardial pump
o Coronary artery disease (CAD) and cardiomyopathy
(enlarged heart) result in decreased pumping action and
a decrease in the volume of blood ejected from the
ventricles (stroke volume).
o Hemorrhage and dehydration cause a decrease in
circulating blood volume and a decrease in stroke
volume.
o Myocardial fibers have contractile properties allowing
them to stretch during filling. In a healthy heart this
stretch is proportionally related to the strength of
contraction. As the myocardium stretches, the strength
of the subsequent contraction increases; this is known
as Frank-Starling law of the heart.
Myocardial flow
o To maintain adequate blood flow to the pulmonary and
systemic circulation, myocardial blood flow must supply
sufficient oxygen and nutrients to the myocardium
itself.
o Blood flow through the heart is unidirectional.
Coronary artery circulation
o The coronary circulation is the branch of the systemic
circulation that supplies the myocardium with oxygen
and nutrients and removes waste.
o The coronary arteries fill during ventricular diastole.
o The left coronary artery, the most abundant blood
supply, feeds the left ventricular myocardium, which is
more muscular and does most of the heart’s work.
Systemic circulation
o The arteries and veins of the systemic circulation deliver
nutrients and oxygen to and remove waste from the
tissues.
Blood flow regulation
o The amount of blood ejected from the left ventricle
each minute is the cardiac output.
Normal is 4-6 L/min for 150 lb person
o The circulation volume of blood changes according to
the oxygen and metabolic needs of the body.
o Cardiac index (CI) more precise and takes into
consideration tissue perfusion and the client’s body
surface area (BSA).
Cardiac output / BSA; normal is 2.5-4L/min/m 2
o Stroke volumeamount of blood ejected from the left
ventricle with each contraction.
o The amount of blood in the left ventricle at the end
diastole (preload), the resistance to left ventricular
ejection (afterload), and myocardial contractility all
affect stroke volume.
o Some drugs increase the force of myocardial
contraction, such as digitalis preparations, epinephrine,
and sympathomimetic drugs (drugs that mimic effects
of SNS).
Conduction system
The heart’s conduction system generates the impulse needed to
initiate the electrical chain of events of a normal heartbeat.
Sympathetic nerve fibers, which increase the rate of impulse
generation and the speed of impulse transmission, innervate all
parts of the atria and ventricles. The parasympathetic fibers
originating form the vagus nerve decrease the rate and also
innervate all parts of the atria and ventricles as well as the SA
and AV nodes.
The conduction system originates with the SA node. In the right
atrium at an intrinsic rate b/w 60-100 bpm.
The AV node mediates impulses b/w atria and ventricles b/w 40
and 60 bpm.
o Assists atrial emptying by delaying the impulse before
transmitting it through the bundle of His and the
ventricular Purkinje network.
Intrinsic rate of the bundle of His and the ventricular Purkinje
network is b/w 20 and 40 bpm.
An ECG reflects the electrical activity of the conduction system.
It does not reflect the muscular work of the heart. Normal
sequence on ECG is normal sinus rhythm (NSR).
o Respiratory physiology
Structure and fuciton
The respiratory muscles, pleural space, lungs, and alveoli are
essential for ventilation, perfusion, and exchange of respiratory
gases.
Ventilation process of moving gases into and out of the lungs.
Perfusionrelates to the ability of the cardiovascular system to
pump oxygenated blood the tissues and return deoxygenated
blood to the lungs.
Diffusion is responsible for moving the respiratory gases to
another.
Work of breathing
o WOB is the effort required to expand and contract the
lungs.
o Inspiration active process, stimulated by chemical
receptors in the aorta.
o Expiration passive process that depends on the elastic
recoil properties of the lungs, requiring little or no
muscle work.
o Surfactant is a chemical produced in the lungs to
maintain the surface tension of the alveoli and keep
them from collapsing.
o Clients with advanced COPD lose the elastic recoil of the
lungs and thorax.
o Clients with COPD, especially emphysema, frequently
use accessory muscles of respiration to increase lung
volume.
Elevation of the clavicles during inspiration can
indicate ventilatory fatigue, air hunger, or
decreased lung expansion.
o Compliance is the ability of the lungs to distend or to
expand in response to increased intraalveolar pressure.
o Airway resistance is the pressure difference between
the mouth and alveoli in relation to the rate of flow of
inspired gas. Airway obstruction, asthma, and tracheal
edema increase airway resistance.
Lung volumes
o Spirometry measures the volume of air entering or
leavings the lungs.
Pulmonary circulation
o The primary function of the pulmonary circulation is to
move blood to and form the alveolar capillary
membrane for gas exchange.
o The pulmonary circulation also acts as a filter, removing
small thrombi before they reach vital organs.
Respiratory gas exchange
Diffusion of respiratory gases occurs at the alveolar capillary
membrane.
Increased thickness of the membrane impedes diffusion
because gases take longer to transfer across the membrane.
Oxygen transport
o Delivery depends on the amount of oxygen entering the
lungs (ventilation), blood flow to the lungs and tissues
(perfusion), rate of diffusion, and oxygen carrying
capacity.
o Three things influence the capacity of the blood to carry
oxygen: amount of dissolved oxygen in the plasma, the
amount of hemoglobin, and the tendency of
hemoglobin to bind with oxygen.
Carbon dioxide transport
o Reduced hemoglobin (deoxyhemoglobin) combines
with carbon dioxide, and the venous blood transports
the majority of carbon dioxide.
Regulation of respiration
Regulation of respiration is necessary to ensure sufficient
oxygen intake and carbon dioxide elimination to meet the
body’s demands.
Neural regulation includes the CNS control of respiratory rate,
depth, and rhythm.
Chemical regulation involves the influence of chemicals such as
carbon dioxide and hydrogen ions on the rate and depth of
respiration.
o Factors affecting oxygenation
Physiological factor any condition affecting the cardiopulmonary
functioning directly affects the body’s ability to meet oxygen demands.
Decreased oxygen-carrying capacity
o Anemia and inhalation of toxic substances decrease the
oxygen-carrying capacity of blood by reducing the
amount of available hemoglobin to transport oxygen.
o Carbon monoxide is the most common toxic inhalant
decreasing the oxygen-carrying capacity of blood.
Decreased inspired oxygen concentration
o Decreases in the fraction of inspired oxygen
concentration (FIO2) are caused by an upper or lower
airway obstruction limiting delivery of inspired oxygen
to alveoli; decreased environmental oxygen, such as at
high altitudes; or decreased inspiration, which occurs in
drug overdoses.
Hypovolemia
o With significant fluid loss, the body tries to adapt by
increasing the heart rate and peripheral
vasoconstriction to increase the volume of blood
returned to the heart and, in turn, increase the cardiac
output.
Increased metabolic rate
o Increased metabolic activity increases oxygen demand.
When body systems are unable to meet this demand,
the level of oxygenation declines.
Conditions affecting chest wall movement
Any condition reducing chest wall movement results in
decreased ventilation
Pregnancy: as fetus grows during pregnancy, the enlarging
uterus pushes abdominal contents upward against diaphragm.
In last trimester inspiratory capacity decreases causing dyspnea
on exertion and increased fatigue.
Obesity: clients morbidly obese have reduced lung volumes
from the heavy lower thorax and abdomen, particularly when
the recumbent and supine positions.
o Morbidly obese clients have reduction in compliance as
a result of encroachment of abdomen into chest,
increased work of breathing, and decreased lung
volumes.
o Obese client is susceptible to pneumonia after surgery
or an upper respiratory tract infection.
Musculoskeletal abnormalities: abnormal structural
configurations impairing oxygenation include those affecting the
rib cage, such as pectus excavatum, and the vertebral volume,
such as kyphosis, lordosis, or scoliosis.
Trauma: unstable chest wall allows the lung underlying the
injured area to contract on inspiration and bulge on expiration,
resulting in hypoxia.
Neuromuscular diseases: affect tissue oxygenation by
decreasing the client’s ability to expand and contract the chest
wall. Ventilation is impaired, and atelectasis, hypercapnia, and
hypoxemia occur.
CNS alterations: when medulla oblongata is affected, neural
regulation of respiration is damaged and abnormal breathing
patterns develop. When the phrenic nerve is damaged, the
diaphragm does not descend properly, thus reducing inspiratory
lung volumes and causing hypoxemia.
o Injury of C3-C5 results in paralysis of phrenic nerve.
o Alterations in cardiac functioning
Disturbances in conduction: electrical impulses that do not originate
from the SA node cause conduction disturbances. These rhythm
disturbances are called dysrhythmias, meaning a deviation from the
normal sinus heart rhythm.
Occur as a primary conduction disturbance, such as in response
to ischemia, valvular abnormality, anxiety, or drug toxicity; as a
result of caffeine, alcohol, or tobacco use; or as complications of
acid-base or electrolyte imbalance.
Ventricular tachycardia and ventricular fibrillation are life-
threatening rhythms that require immediate intervention.
Ventricular tachycardia is a life-threatening dysrhythmia
because of the decreased cardiac output and the potential to
deteriorate into ventricular fibrillation.
Altered cardiac output
Failure of myocardium to eject sufficient volume to systemic
and pulmonary circulations results in heart failure.
Left-sided heart failure
o Assessment findings include fatigue, breathlessness,
dizziness, and confusion as a result of tissue hypoxia
form the diminished cardiac output.
o As the left ventricle continues to fail, blood begins to
pool in the pulmonary circulation, causing pulmonary
congestion.
Right-sided heart failure
o Right-sided heart failure more commonly results from
pulmonary disease or as a result of long-term left sided
failure
o The primary pathological factor in right-sided failure is
elevated pulmonary vascular resistance (PVR).
o As the failure continues, the amount of blood ejected
from the right ventricle declines, and blood begins to
back up in the systemic circulation.
o Clinically the client has weight gain, distended neck
veins, hepatomegaly and splenomegaly, and dependent
peripheral edema.
Impaired valvular function
When stenosis occurs, the flow of blood through the valves is
obstructed.
Over time the stenosis causes the ventricle to hypertrophy, and
if the condition is untreated, left- or right sided heart failure
occurs.
When regurgitation occurs, there is a backflow of blood into an
adjacent chamber.
Myocardial ischemia
Results when the supply of blood to the myocardium from the
coronary arteries is insufficient to meet myocardial oxygen
demands.
Angina: angina pectoristransient imbalance between
myocardial oxygen supply and demand.
o This condition results in chest pain that is aching, sharp,
tingling, or burning, or that feels like pressure.
o Typically chest pain is left sided or substernal and often
radiates to the left or both arms, and to the jaw, neck
and back.
Pain usually lasts 1-15 minutes
Myocardial infarction
o Results from sudden decrease in coronary blood flow or
an increase in myocardial oxygen demand without
adequate coronary perfusion.
o Chest pain associated with MI in men is usually
described as crushing, squeezing, or stabbing.
o Pain occurs at rest or excretion and lasts more than 30
minutes.
o Most common initial symptom in women is angina, but
atypical symptoms of fatigue, indigestion, vasospasm,
SOB, or back or jaw pain are also present.
o Alterations in respiratory functioning
The goal of ventilation is to produce a normal arterial carbon dioxide
tension between 35-45 mm Hg (PaCO2) and maintain a normal arterial
oxygen tension (PaO2) between 95-100 mm Hg.
Hyperventilation
State of ventilation in excess of that required to eliminate the
carbon dioxide produced by cellular metabolism. Anxiety,
infections, drugs, or an acid-base imbalance induce
hyperventilation, as well as hypoxia associated with pulmonary
embolus or shock.
Salicylate (aspirin) poisoning causes excessive stimulation of the
respiratory center as the body attempts to compensate for
excess carbon dioxide.
Amphetamines also increase ventilation by raising CO 2
production.
Hypoventilation
Occurs when alveolar ventilation is inadequate to meet the
body’s oxygen demand or to eliminate sufficient carbon dioxide.
Atelectasiscollapse of alveoli, prevents normal exchange of
oxygen and carbon dioxide.
In clients with COPD, the administration of excessive oxygen
results in hypoventilation.
Their stimulus to breathe is a decreased arterial oxygen (PaO 2)
level.
Administration of oxygen greater than 24%-28% (1-3 L/min)
prevents the PaO2 from falling and obliterates the stimulus to
breathe, resulting in hypoventilation.
Hypoxia
Inadequate tissue oxygenation at the cellular level.
Causes include (1) decreased hemoglobin and lowered oxygen-
carrying capacity of the blood; (2) a diminished concentration of
inspired oxygen, which occurs at high altitudes; (3) the inability
of tissues to extract oxygen form the blood, as with cyanide
poisoning; (4) decreased diffusion of oxygen from the alveoli to
the blood, as in pneumonia; (5) poor tissue perfusion with
oxygenated blood, as with shock; and (6) impaired ventilation,
as with multiple rib fractures or chest trauma.
Nursing Knowledge Base
o Developmental factors
Infants and toddlers: are at risk for upper respiratory tract infections as
a result of frequent exposure to other children and exposure to
secondhand smoke.
School-age children and adolescents: exposed to respiratory infections
and respiratory risk factors such as secondhand smoke and cigarette
smoking.
Young and middle-age adults: exposed to multiple cardiopulmonary risk
factors: an unhealthy diet, lack of exercise, stress, and OTC and
prescription drugs not used as intended, illegal substances, and
smoking.
Older adults: changes include calcification of the heart valves, SA node,
and costal cartilages. The arterial system develops the atherosclerotic
plaques. Osteoporosis leads to changes in the size and shape of the
thorax.
The trachea and large bronchi enlarged form calcification of the
airways.
The alveoli enlarge, decreasing the surface area available for gas
exchange. The number of functional cilia is reduced, causing a
decrease in the effectiveness of the cough mechanism, putting
the older adult at increased risk for respiratory infections.
o Lifestyle factors
Risk factor modification is important and includes smoking cessation,
weight reduction, and a low-cholesterol and a low-sodium diet,
management of hypertension, and moderate exercise.
Nutrition: severe obesity decreases lung expansion, and increased body
weight increases tissue oxygen demands.
The malnourished client experiences respiratory muscle
wasting, resulting in decreased muscle strength and respiratory
excursion.
Client is at risk for retention of pulmonary secretions.
Cardioprotective nutrition includes diets rich in fiber; whole
grains; fresh fruits and vegetables; nuts; antioxidants; lean
meats; fish; and chicken; and omega-3 fatty acids.
Potatoes and citrus fruit juices are Cardioprotective in women,
but not men.
Exercise: people who exercise for 30-60 minutes daily have a lower
pulse rate and BP, decreased cholesterol level, increased blood flow,
and greater oxygen extraction by working muscles.
Smoking: inhaled nicotine causes vasoconstriction of peripheral and
coronary blood vessels, increasing blood pressure and decreasing blood
flow to peripheral vessels.
Women who take birth control pills and smoke cigarettes have
an increased risk for thombophlebitis and pulmonary emboli
Substance abuse: first, the person who chronically abuses substances
often has a poor nutritional intake.
Second, excessive use of alcohol and certain other drugs
depresses the respiratory center, reducing the rate and depth of
respiration and the amount of inhaled oxygen.
Stress: a continuous state of stress of severe anxiety increases the
body’s metabolic rate and the oxygen demand.
o Environmental factors
Incidence of pulmonary disease is higher in smoggy, urban areas than in
rural areas
Nursing Process—Assessment
o Nursing assessment cardiopulmonary functioning includes an in-depth history of
the client’s normal and present cardiopulmonary function, past impairments in
circulatory or respiratory functioning, and measures that the client uses to
optimize oxygenation.
o Nursing history: focuses on the clients’ ability to meet oxygen needs.
The nursing history for cardiac function includes pain and characteristic
of pain, dyspnea, fatigue, peripheral circulation, cardiac risk factors and
the presence of past or concurrent cardiac conditions.
The nursing history for respiratory function includes the presence of a
cough, SOB, wheezing, pain, environmental exposures, frequency of
respiratory tract infections, pulmonary risk factors, past respiratory
problems, current medication use, and smoking history or secondhand
smoke exposure.
Pain: presence of chest pain needs immediate thorough evaluation,
including location, duration, radiation, and frequency.
Pericardial pain results from inflammation of the pericardial sac,
occurs on inspiration, and does not usually radiate.
Pleuritic chest pain is peripheral and radiates to the scapular
regions.
Fatigue: fatigue in the client with cardiopulmonary alterations is often
an early sign of a worsening of the chronic underlying process.
Smoking: important to determine clients’ direct and secondary exposure
to tobacco.
Dyspnea: is a clinical sign of hypoxia. It is the subjective sensation of
difficult or uncomfortable breathing.
Is associated with exaggerated respiratory effort, use of the
accessory muscles of respiration, nasal flaring, and marked
increases in the rate and depth of respirations.
Orthopnea client uses multiple pillows when lying down or
must sit with the arms elevated and learning forward to
breathe.
Cough: coughing is a protective reflex to clear the trachea, bronchi and
lungs of irritants and secretions.
A productive cough results in sputum production, material
coughed up from the lungs that the client swallows or
expectorates.
If hemoptysis (bloody sputum) is present, determine if it is
associated with coughing and bleeding from the upper
respiratory tract, from sinus drainage, or from the GI tract
(hematemesis).
Wheezing: associated with asthma, acute bronchitis, or pneumonia.
Environmental or geographical exposures: most common exposures in
the home are cigarette smoke, carbon monoxide, and radon.
Respiratory infections: obtain information about the client’s frequency
and duration of respiratory tract infections.
On average, clients will have four colds per year.
Presentation with Pneumocystis carinii pneumonia (PCP) or
Mycoplasma pneumonia.
o Presentation with either indicates a significant
depression of the client’s immune system and
progression to AIDS.
Allergies: inquire about your client’s exposure to airborne allergens
Safe nursing practice also includes obtaining information about
food, drug, or insect sting allergies.
Health risks: determine familial risk factors, such as a family history of
lung cancer or cardiovascular disease.
Medications: clients taking warfarin (Coumadin) for blood thinning will
prolong the prothrombin time (PT)/international normalized ratio (INR)
results if they are taking gingko biloba, garlic, or ginseng with the
anticoagulation.
Clients need to recognize adverse reactions and be aware of the
dangers in combining prescribed medications with OTC drugs.
o Physical examination
Inspection: using inspection techniques perform a head-to-toe
observation of the client for skin and mucous membrane color, general
appearance, level of consciousness, adequacy of systemic circulation,
breathing patterns, and chest wall movement. (table 40-3)
Clubbed nails, obliteration of the normal angle between the
base of the nail and the skin often occur in clients with
prolonged oxygen deficiency, endocarditis, and congenital heart
defects.
Conditions such as emphysema, advancing age, and COPD cause
the chest to assume a rounded “barrel” shape.
Palpation: palpation of the extremities provides data about the
peripheral circulation, the presence and quality of peripheral pulses,
skin temperature, color, and capillary refill.
Auscultation: of the cardiovascular system include assessment for
normal S1 and S2 sounds, the presence of abnormal S3 and S4 sounds
(gallops), and murmurs or rubs.
Planning
o Goals and outcomes: clients with impaired oxygenation require a nursing care
plan directed toward meeting actual or potential oxygenation needs.
o Setting priorities: the client’s level of health, age, lifestyle, and environmental
risks affect the level of tissue oxygenation.
Implementation
o Health promotion
Prevention of respiratory infections is foremost in maintaining optimal
health.
Vaccinations: annual influenza vaccines are recommended for children
6-59 months, adults over 50, and clients with chronic illnesses.
Persons who should not be vaccinated include those with a
known hypersensitivity to eggs or other components of the
vaccine and adults with an acute febrile illness.
Healthy lifestyle behavior: encourage clients to eat a healthy low-fat,
high-fiber diet; monitor their cholesterol, triglyceride, HDL, and LDL
levels; reduce their stress; exercise; and maintain a body weight in
proportion to their height.
Elimination of cigarettes and other tobacco, reduction of
pollutants, monitoring of air quality, and adequate hydration
are additional healthy behaviors.
o During the hot summer months teach clients to limit
their activities to early in the day or late in the evening,
when temperatures are lower.
o Shoveling snow is especially risky and often precipitates
a cardiac event. Other events such as hanging holiday
lights and decorations in the extreme cold, will possibly
precipitate chest pain and bronchospasm.
o Acute care
Clients with acute pulmonary illnesses require nursing interventions
directed toward halting the pathological process.
Dyspnea management
Treat underlying process causing dyspnea, then add additional
therapies
Pharmacologic agents include bronchodilators, inhaled steroids,
muculytics, and low-dose antianxiety medications.
Airway maintenance: requires adequate hydration to prevent thick,
tenacious secretions
Suctioning, chest physiotherapy, and nebulizer therapy assist in
managing alterations in airway clearance.
Mobilization of pulmonary secretions: ability of a client to mobilize
pulmonary secretions makes the difference between a short-term
illness and a long recovery involving complications.
Humidification: process of adding water to gas
Air or oxygen with a high relative humidity keeps the airways
moist and helps loosen and mobilize pulmonary secretions.
Humidification is necessary for clients receiving oxygen therapy
at greater than 4 L/min.
Nebulization: adds moisture or medications to inspired air by mixing
particles of varying sizes with the air.
Humidification through Nebulization enhances mucociliary
clearance, the body’s natural mechanism for removing mucus
and cellular debris from the respiratory tract.
Chest physiotherapy: group of therapies used to mobilize pulmonary
secretions.
Chest physiotherapy is recommended for clients who produce
greater than 30 mL of sputum per day or heave evidence of
atelectasis by chest x-ray examination.
Suctioning techniques: suctioning is necessary when the client is unable
to clear respiratory secretions from the airways.
In most cases use sterile technique for suctioning because the
oropharynx and trachea are considered sterile.
Too-frequent suctioning puts the client at risk for development
of hypoxemia, hypotension, arrhythmias, and possible trauma
to the mucosa of the lungs.
Oropharyngeal and nasopharyngeal suctioning: is used when the client
is able to cough effectively but is unable to clear secretions by
expectorating or swallowing.
Orotracheal and nasotracheal suctioning: is necessary when the client
with pulmonary secretions is unable to manage secretions by coughing
and does not have an artificial airway present.
Tracheal suctioning: occurs through an artificial airway, such as an
endotracheal tube or tracheostomy tube.
Make sure the suction catheter is no greater than half of the
size of the internal diameter of the artificial airway.
Open suctioning involves a sterile catheter that is opened at the
time of suctioning.
o Wear sterile gloves during procedure
Closed suctioning involves a multiple-use suction catheter that
is encased in a plastic sheath
o Most often used on clients who require mechanical
ventilation to support their respiratory efforts, because
it permits continuous delivery of oxygen while suction is
performed, thus reducing the risk of oxygen
desaturation.
Artificial airways: for clients with decreased level of consciousness or
airway obstruction and aids in removal of tracheobronchial secretions.
Oral airway: simplest type of artificial airway, prevents obstruction of
the trachea by displacement of the tongue into the oropharynx.
Endotracheal and tracheal airway: presence of an artificial airway places
the client at high risk for infection and airway injury.
Endotracheal tubes (ETs) are short-term artificial airways to
administer mechanical ventilation, relieve upper airway
obstruction, protect against aspiration, or clear secretions.
Positioning: frequent changes of position are simple and cost-effective
methods for reducing stasis of pulmonary secretions and decreased
chest wall expansion, both of which increase the risk of pneumonia.
The 45-degree semi-Fowler’s position is the most effective
position.
This position uses gravity to assist in lung expansion and
reduces pressure from the abdomen on the diaphragm.
Incentive spirometry: encourages voluntary deep breathing by providing
visual feedback to clients about inspiratory volume.
Promotes deep breathing and prevents or treats atelectasis in
the postoperative client.
A postoperative inspiratory capacity ½- ¾ of the preoperative
volume is acceptable because of postoperative pain.
Chest tubes: a chest tube is a catheter inserted through the thorax to
remove air and fluids from the pleural space, to prevent air or fluid from
reentering the pleural space, or to reestablish normal intrapleural and
intrapulmonic pressures.
Mobile drains reduce the length of time needed for the chest
tube, improve ambulation, and decrease the length of time in
the hospital.
A pneumothorax is a collection of air in the pleural space.
A hemothorax is an accumulation of blood and fluid in the
pleural cavity between the parietal and visceral pleurae, usually
as a result of trauma.
o Produces a counterpressure and prevents the lung from
full expansion.
Special considerations: clamping a chest tube is contraindicated
when ambulating or transporting the client
o Will possibly result in a tension pneumothorax.
o Maintain the drainage device below the client’s chest.
Oxygen therapy: goal of oxygen therapy is to prevent or relive hypoxia.
Has dangerous side effects, such as atelectasis or oxygen
toxicity.
Safety precautions: although it does not spontaneously burn or cause an
explosion, it can easily cause a fire in a client’s room if it contacts a
spark from an open flame or electrical equipment.
Nasal cannula: is a simple, comfortable device used for oxygen delivery.
Two cannulas, about 1.5 cm long, protrude from the center of a
disposable tube and are inserted into the nares.
Be alert for skin breakdown over the ears and in the nares from
too tight an application of the nasal cannula.
Oxygen masks: device used to administer oxygen, humidity, or heated
humidity.
Simple face mask is used for short-term oxygen therapy
o Fits loosely and delivers oxygen concentrations form
30%-60%.
o Is contraindicated for clients with carbon dioxide
retention because retention can be worsened.
A plastic face mask with a reservoir bag and a Venturi mask are
capable of delivering higher concentrations of oxygen.
o When used as a nonrebreather, the plastic face mask
with a reservoir bag delivers from 60%-95% oxygen with
a flow rate of 6-10 L/min.
o The Venturi mask delivers oxygen concentrations of
24% to 60% with oxygen flow rates of 4-12 L/min.
Home oxygen therapy: indications for home oxygen therapy include an
PaO2 of 55 mm Hg or less or an SaO2 of 88% or less on room air at rest,
on exertion, or with exercise.
Restoration of cardiopulmonary functioning: if a client’s hypoxia is sever
and prolonged, cardiac arrest will result.
Permanent heart, brain, and other tissue damage occur within
4-6 min.
The ABCs of cardiopulmonary resuscitation are to establish an
Airway, initiate Breathing, and maintain Circulation.
The purpose of CPR is to circulate oxygenated blood to the brain
to prevent permanent tissue damage.
o Restorative and continuing care
Cardiopulmonary rehabilitationhelps the client to achieve and
maintain an optimal level of health through controlled physical exercise,
nutrition counseling, relaxation and stress management techniques, and
prescribed medications and oxygen.
Hydration: maintenance of adequate systemic hydration keeps
mucociliary clearance normal
The best way to maintain thin secretions is to provide a fluid
intake of 1500-200 mL/day unless contraindicated by cardiac
status.
Coughing techniques: coughing is effective for maintaining a patent
airway.
Permits the client to remove secretions from both upper and
lower airways.
Encourage clients with a large amount of sputum to cough
every hour while awake and every 2-3 hours while asleep until
the acute phase of mucus production has ended.
With the cascade cough, the client takes a slow, deep breath
and holds it for 2 seconds while contracting expiratory muscles.
The huff cough stimulates a natural cough reflex and is generally
effective only for clearing central airways.
The quad cough technique is for clients without abdominal
muscle control, such as those with SCI.
Respiratory muscle training: improves muscle strength and endurance,
resulting in improved activity tolerance
Prevents respiratory failure in clients with COPD
Breathing exercises
Pursed-lip breathing involves deep inspiration and prolonged
expiration through pursed lips to prevent alveolar collapse.
Diaphragmatic breathing is more difficult and requires the client
to relax intercostal and accessory respiratory muscles while
taking deep respirations.
Evaluation
o Evaluation of arterial blood gas levels, pulmonary function tests, vital signs, ECG
tracings, and physical assessment data provide objective measurement of the
success of therapies and treatments.
You might also like
- Circulatory System: A Tutorial Study GuideFrom EverandCirculatory System: A Tutorial Study GuideRating: 5 out of 5 stars5/5 (3)
- Chapter 012Document11 pagesChapter 012api-2813400240% (1)
- The Ketogenic Diet and BodybuildingDocument2 pagesThe Ketogenic Diet and BodybuildingHumphriesRasch39No ratings yet
- A. Fisiologi RespirasiDocument77 pagesA. Fisiologi RespirasiasriNo ratings yet
- Components of The Cardiovascular SystemDocument23 pagesComponents of The Cardiovascular SystemMr. DummyNo ratings yet
- Lecture 4 Properties of Myocardium and Cardiac Cycle 2020-2021Document43 pagesLecture 4 Properties of Myocardium and Cardiac Cycle 2020-2021badarbhai222No ratings yet
- Cardio Anapyhy Session1Document24 pagesCardio Anapyhy Session1Louise Anne Agnazata GayoNo ratings yet
- Body Fluids & CirculationDocument29 pagesBody Fluids & CirculationAyaan AshrafNo ratings yet
- CVS FullDocument32 pagesCVS FullLianne PalinsadNo ratings yet
- Cardiovascular SystemDocument9 pagesCardiovascular SystemMayim LouiseNo ratings yet
- Circulatory System TerminologiesDocument4 pagesCirculatory System TerminologiesavduqueNo ratings yet
- MF-local Circulation 2016Document61 pagesMF-local Circulation 2016OnSolomonNo ratings yet
- Blood VesselsDocument11 pagesBlood VesselsAndrea PeriguaNo ratings yet
- Blood CirculationDocument24 pagesBlood Circulationaanchal1203sharmaNo ratings yet
- Cardiac CycleDocument3 pagesCardiac CycleKhadijah HabeebahNo ratings yet
- Heart & Hemodynamics NotesDocument8 pagesHeart & Hemodynamics NotesBrandice BradleyNo ratings yet
- 1.2 The Circulatoy System: Prepared By: LING MEI TENGDocument13 pages1.2 The Circulatoy System: Prepared By: LING MEI TENGJuliet LingNo ratings yet
- Cardiovascular System - Lecture 3-2018-2019 PDFDocument27 pagesCardiovascular System - Lecture 3-2018-2019 PDFMary100% (1)
- Vascular Distensibility and Functions of The Arterial and 1Document83 pagesVascular Distensibility and Functions of The Arterial and 1gabby chaanNo ratings yet
- Circulatory System Edit OngoingDocument7 pagesCirculatory System Edit OngoingclintonbogololephojaneNo ratings yet
- Module 5 CardioVascular SystemDocument7 pagesModule 5 CardioVascular SystemWai KikiNo ratings yet
- Chapter 18 AHP215Document3 pagesChapter 18 AHP215gielduqueNo ratings yet
- Physiology of Circulation SystemDocument52 pagesPhysiology of Circulation SystemReni TeeWeeNo ratings yet
- (Lecture 7) The Cardiovascular, Respiratory and Lymphatic SystemDocument32 pages(Lecture 7) The Cardiovascular, Respiratory and Lymphatic SystemKasraSrNo ratings yet
- Cardiovascular DrugsDocument33 pagesCardiovascular DrugsKish Gabriel100% (1)
- CirculationDocument11 pagesCirculationRishikaphriya RauichandranNo ratings yet
- Circulation and Cardiovascular SystemDocument12 pagesCirculation and Cardiovascular SystemSatria MandalaNo ratings yet
- Structure and Function of The Cardiovascular System PDFDocument9 pagesStructure and Function of The Cardiovascular System PDFteuuuuNo ratings yet
- Circulation in Special AreasDocument48 pagesCirculation in Special AreasAninze ChideraNo ratings yet
- Topic 7: Transport in HumansDocument19 pagesTopic 7: Transport in HumansAmyrul Darwisy ZafranNo ratings yet
- Review of Anatomy and Physiology of Blood Vessels and BloodDocument9 pagesReview of Anatomy and Physiology of Blood Vessels and BloodDan Ataniel EnsaladaNo ratings yet
- 03 CVS PhysiologyDocument55 pages03 CVS PhysiologyMonenus KedirNo ratings yet
- Notes On Cardiovascular SystemDocument3 pagesNotes On Cardiovascular Systemmohamed waleedNo ratings yet
- Circulation NotesDocument2 pagesCirculation NotesBhkti MittalNo ratings yet
- 1.2 The Circulatoy System: Prepared By: LING MEI TENGDocument13 pages1.2 The Circulatoy System: Prepared By: LING MEI TENGJuliet LingNo ratings yet
- Topic 9 Cardiovascular SystemDocument36 pagesTopic 9 Cardiovascular SystemAlejandra CastilloNo ratings yet
- Pharma 6Document17 pagesPharma 6Cleo PizarrasNo ratings yet
- Special Regional CirculationDocument28 pagesSpecial Regional CirculationBenjamin SharonNo ratings yet
- Cardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryDocument73 pagesCardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryAparna RamachandranNo ratings yet
- THE HEART HandoutDocument61 pagesTHE HEART HandoutMitha PelangiNo ratings yet
- Human HeartDocument10 pagesHuman HeartRAHUL NISHADNo ratings yet
- Note On Pressure Flow and ResistanceDocument43 pagesNote On Pressure Flow and ResistanceSilver FestusNo ratings yet
- In Partial Fulfillment of The Requirements in Biological ScienceDocument11 pagesIn Partial Fulfillment of The Requirements in Biological ScienceGodfrey Loth Sales Alcansare Jr.No ratings yet
- Medical Surgical Nursing: Anatomy HeartDocument8 pagesMedical Surgical Nursing: Anatomy HeartRoyce Vincent TizonNo ratings yet
- Fundamentals - CH 40: Oxygenation/Gas Exchange: Nloa Sfe B.8 Situation - Care of Client With Problems in OxygenationDocument20 pagesFundamentals - CH 40: Oxygenation/Gas Exchange: Nloa Sfe B.8 Situation - Care of Client With Problems in OxygenationSOLEIL LOUISE LACSON MARBASNo ratings yet
- B.8 Situation - Care of Client With Problems in OxygenationDocument11 pagesB.8 Situation - Care of Client With Problems in OxygenationSOLEIL LOUISE LACSON MARBASNo ratings yet
- Exercise PhysiologyDocument24 pagesExercise PhysiologyMohammed AlharbiNo ratings yet
- Shock 2Document16 pagesShock 2brunoNo ratings yet
- Lecture Notes NCM 102: Union Christian College College of NursingDocument77 pagesLecture Notes NCM 102: Union Christian College College of Nursingnarswiponshistoryan100% (1)
- Mammalian CirculationDocument54 pagesMammalian Circulationron971No ratings yet
- Transe 3Document8 pagesTranse 3lija.medija.swuNo ratings yet
- Human Circulatory System - Study NotesDocument8 pagesHuman Circulatory System - Study NotesrockyajeetNo ratings yet
- A. MODUL PDP 8Document29 pagesA. MODUL PDP 8Suraya Eiman ZafiraNo ratings yet
- Cardiology: Patent LumenDocument5 pagesCardiology: Patent LumenDeepthi VallabhaneniNo ratings yet
- Blood Vessels NotesDocument5 pagesBlood Vessels NotesJan Vincent GoNo ratings yet
- BCH102 Unit - III: Physiology: Structure of HeartDocument17 pagesBCH102 Unit - III: Physiology: Structure of Heartdivya vajpayeeNo ratings yet
- Transport in HumansDocument6 pagesTransport in HumansJason Ng100% (5)
- Human Circulatory SystemDocument8 pagesHuman Circulatory SystemChelsea EdwardsNo ratings yet
- Cardiac Ana & DxticsDocument3 pagesCardiac Ana & Dxticsjames garciaNo ratings yet
- CirculationDocument10 pagesCirculationKezia JenniferNo ratings yet
- II. Blood Vessels Physiology By: Dr. Abdulrahman Aqra MD MSCDocument12 pagesII. Blood Vessels Physiology By: Dr. Abdulrahman Aqra MD MSCapi-290338101No ratings yet
- Renal TubuleDocument7 pagesRenal Tubulehurainsahar21No ratings yet
- Hypertension in Pregnancy: Margaret S. Hamilton, DNS, RNDocument33 pagesHypertension in Pregnancy: Margaret S. Hamilton, DNS, RNHaji RajiNo ratings yet
- Chapter 48 - Skin Integrity and Wound CareDocument13 pagesChapter 48 - Skin Integrity and Wound CareHaji Raji100% (1)
- Chapter 27 Self ConceptDocument7 pagesChapter 27 Self ConceptHaji RajiNo ratings yet
- Chapter 36 - Complementary and Alternatives TherapiesDocument6 pagesChapter 36 - Complementary and Alternatives TherapiesHaji RajiNo ratings yet
- ATI Psych ProctoredDocument6 pagesATI Psych Proctoredyoderjess425No ratings yet
- Take Away 2 - Airbus Hazard Prevention Handbook (Distribution Copy)Document41 pagesTake Away 2 - Airbus Hazard Prevention Handbook (Distribution Copy)UbernatorNo ratings yet
- Dav Public School, Pokhariput Investigatory Project of Chemistry OnDocument11 pagesDav Public School, Pokhariput Investigatory Project of Chemistry OnAnubhab SahuNo ratings yet
- Drug Study GuideDocument2 pagesDrug Study GuideAubrey SungaNo ratings yet
- PASCUAL, Jhigo V. REYES, Al Sebastian C. MEDINA, Chris Daniel J. PUSING, Daniel Joseph V. Documentation and Report Humss 11-3 Physical ScienceDocument2 pagesPASCUAL, Jhigo V. REYES, Al Sebastian C. MEDINA, Chris Daniel J. PUSING, Daniel Joseph V. Documentation and Report Humss 11-3 Physical ScienceJhigo Villar Franco PascualNo ratings yet
- Red and White Lesions of The Oral MucosaDocument32 pagesRed and White Lesions of The Oral MucosaBidisha BhattacharyyaNo ratings yet
- Bronchiectasis 2Document19 pagesBronchiectasis 2Liza FathiarianiNo ratings yet
- Medical Mnemonics 4 PrintDocument65 pagesMedical Mnemonics 4 Printanne0521100% (1)
- SYNTONICS Cheat Sheet 1Document1 pageSYNTONICS Cheat Sheet 1mavikNo ratings yet
- Prevalence of Nematode Contracaecum and Cestode Ligula Intestinalis Parasites Infection in Two Fish Species at Lake TanaDocument8 pagesPrevalence of Nematode Contracaecum and Cestode Ligula Intestinalis Parasites Infection in Two Fish Species at Lake TanaIJARP PublicationsNo ratings yet
- Antimicrobial Activity of Different Herbal Plants Extracts: A ReviewDocument38 pagesAntimicrobial Activity of Different Herbal Plants Extracts: A ReviewKima MadNo ratings yet
- HIT LLA Recaida en Pediatria 2020Document34 pagesHIT LLA Recaida en Pediatria 2020Nathalie Soler BarreraNo ratings yet
- Handouts Infectious Coryza Fall 2020Document3 pagesHandouts Infectious Coryza Fall 2020NabeelNo ratings yet
- Incredible 5-Second Water-Hack Kills Food CravingsDocument4 pagesIncredible 5-Second Water-Hack Kills Food CravingsSteeven MartínezNo ratings yet
- LOHMANN Brown Classic CageDocument48 pagesLOHMANN Brown Classic CageAram Nasih MuhammadNo ratings yet
- Oncology Nursing Trends and Issues 2Document6 pagesOncology Nursing Trends and Issues 2DaichiNo ratings yet
- Madison Health - Health Care Providers List 2023Document2 pagesMadison Health - Health Care Providers List 2023Sharik EssaNo ratings yet
- IPC Walk Rounds Final2019Document29 pagesIPC Walk Rounds Final2019AncyNo ratings yet
- Larazotide Acetate For Persistent Symptoms of Celiac Disease Despite A GlutenFree Diet A Randomized Controlled TrialDocument15 pagesLarazotide Acetate For Persistent Symptoms of Celiac Disease Despite A GlutenFree Diet A Randomized Controlled Trial-Yohanes Firmansyah-No ratings yet
- Isolation Room Fans PDFDocument8 pagesIsolation Room Fans PDFSandeep NairNo ratings yet
- Safe Injections - MCQDocument4 pagesSafe Injections - MCQSemo MezoNo ratings yet
- Frankenstein: Theme of IsolationDocument5 pagesFrankenstein: Theme of Isolationy.maungooNo ratings yet
- Classifying Giant Cell Lesions A Review.21Document5 pagesClassifying Giant Cell Lesions A Review.21shehla khanNo ratings yet
- Reyes vs. Magsaysay MitsuiDocument8 pagesReyes vs. Magsaysay MitsuiAldos Medina Jr.No ratings yet
- FOR AND AGAINST ESSAY: Advantages and Disadvantages of ComputersDocument3 pagesFOR AND AGAINST ESSAY: Advantages and Disadvantages of ComputersZerina DedićNo ratings yet
- Hypomineralised Second Primary Molars May Be Indicative of Future Molar Incisor Hypomineralisation PDFDocument6 pagesHypomineralised Second Primary Molars May Be Indicative of Future Molar Incisor Hypomineralisation PDFnha khoa NHƯ NGỌCNo ratings yet
- Project Utthaan: A Leprosy Awareness InitiativeDocument6 pagesProject Utthaan: A Leprosy Awareness InitiativeAmaayaNo ratings yet
- Fundus Fluorescein Angiography: Division of Clinical SciencesDocument5 pagesFundus Fluorescein Angiography: Division of Clinical SciencesPREM2KUMARNo ratings yet