Professional Documents
Culture Documents
Anemia Pada Kondisi CKD
Anemia Pada Kondisi CKD
Uploaded by
Niken DiazOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anemia Pada Kondisi CKD
Anemia Pada Kondisi CKD
Uploaded by
Niken DiazCopyright:
Available Formats
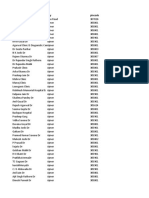
1.
Anemia
Penurunan Hb :
- Mengindikasikan anemia. Penurunan Hb selalu diikuti dengan penurunan
hematokrit dan RBC (red blood cell, sel darah merah), tetapi belum tentu diikuti
dengan abnormalitas nilai MCV, MCH dan MCHC. Pada kasus di atas anemia
terjadi karena pasien mengalami CKD. Salah satu hormon yang penting pada
proses eritropoiesis di sumsum tulang adalah eritropoeitin yang diproduksi oleh
kelenjar adrenal pada ginjal. CKD mengakibatkan gangguan kelenjar adrenal
sehingga terjadi penurunan produksi eritropoetin.
- Penanganan anemia pada pasien CKD dengan pemberian tranfusi PRC
(packed red cell) atau pemberian hormon eritropoeitin. Pada kasus ini, PRC
baru diberikan tgl 16/6 dan 17/6, seharusnya PRC/eritropoeitin sudah diberikan
pada saat tanggal 14/6. Juga tidak ada pemeriksaan darah lengkap (DL) lagi
untuk mengetahui apakah anemia masih terjadi setelah pemberian PRC.
GFR mL/menit:
(140 − 𝑢𝑠𝑖𝑎) × 𝐵𝐵 (𝑘𝑔)
× 0,85
72 × 𝑆𝑐𝑟
(140−55) × 50 (𝑘𝑔)
72×9,27
× 0,85 = 5,41
Anemia occurs in acute and chronic renal failure. The anemia is usually normocytic but may
be microcytic. In renal failure, anemia occurs in part because uremic metabolites decrease the
lifespan of circulating red blood cells and reduce erythropoiesis.
Anemia secondary to uremia is characterized by inappropriately low erythropoietin levels, in
contrast to the normal or high levels that occur with most other causes of anemia. To further
confuse the presentation, serum iron levels and the percentage of iron saturation are often
low, apparently because of negative acute-phase reactions.10 Furthermore, the serum
creatinine level and the degree of anemia may not correlate well.3
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3458456/?report=reader
As kidney disease progresses, anemia increases in prevalence, affecting nearly all patients with stage
5 CKD.2 Anemia in CKD is associated with reduced quality of life and increased cardiovascular
disease, hospitalizations, cognitive impairment, and mortality.2 Anemia in CKD is typically
normocytic, normochromic, and hypoproliferative. The demonstration of a circulating factor
responsible for stimulating erythropoiesis, and the kidney as the main source of erythropoietin (EPO)
in the 1950s3,4 engendered the hypothesis that EPO deficiency is a predominant cause Journal of
the American Society of Nephrology : JASN
American Society of Nephrology
Mechanisms of Anemia in CKD
Jodie L. Babitt and Herbert Y. Lin
Additional article information
Abstract
Anemia is a common feature of CKD associated with poor outcomes. The current
management of patients with anemia in CKD is controversial, with recent clinical trials
demonstrating increased morbidity and mortality related to erythropoiesis stimulating agents.
Here, we examine recent insights into the molecular mechanisms underlying anemia of CKD.
These insights hold promise for the development of new diagnostic tests and therapies that
directly target the pathophysiologic processes underlying this form of anemia.
Anemia was first linked to CKD over 170 years ago by Richard Bright.1 As kidney disease
progresses, anemia increases in prevalence, affecting nearly all patients with stage 5 CKD.2
Anemia in CKD is associated with reduced quality of life and increased cardiovascular
disease, hospitalizations, cognitive impairment, and mortality.2
Anemia in CKD is typically normocytic, normochromic, and hypoproliferative. The
demonstration of a circulating factor responsible for stimulating erythropoiesis, and the
kidney as the main source of erythropoietin (EPO) in the 1950s3,4 engendered the hypothesis
that EPO deficiency is a predominant cause of anemia in CKD.
You might also like
- Case 21Document45 pagesCase 21Mark GironNo ratings yet
- Chronic Kidney DiseaseDocument40 pagesChronic Kidney DiseasePaul SinsNo ratings yet
- Atrial FlutterDocument17 pagesAtrial FlutterEdRobertArnadNo ratings yet
- Jurnal AnastesiDocument12 pagesJurnal AnastesilissamariasianiparNo ratings yet
- Normocytic AnemiaDocument16 pagesNormocytic AnemiaPaula ArayaNo ratings yet
- Art:10.1007/s10741 008 9088 8 PDFDocument8 pagesArt:10.1007/s10741 008 9088 8 PDFShivangi IssarNo ratings yet
- Anemia of Chronic Disease and Kidney FailureDocument12 pagesAnemia of Chronic Disease and Kidney FailureMic HannaNo ratings yet
- Now Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelpDocument24 pagesNow Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelplicservernoidaNo ratings yet
- Anaemia of Chronic Renal DiseaseDocument9 pagesAnaemia of Chronic Renal DiseaseVitabuNo ratings yet
- Anemia For The Primary Care PhysicianDocument16 pagesAnemia For The Primary Care PhysicianAbdón Guerra FariasNo ratings yet
- Anemia in CKDDocument9 pagesAnemia in CKDM. Ryan RamadhanNo ratings yet
- Hematological Changes in Chronic Renal FailureDocument4 pagesHematological Changes in Chronic Renal FailurePriyank GuptaNo ratings yet
- Nephrotic Syndrome-1Document21 pagesNephrotic Syndrome-1Wondimu EliasNo ratings yet
- StudyDocument23 pagesStudyK'winetoy Ra'llavNo ratings yet
- Update On (Approach To) Anemia1 (Changes)Document39 pagesUpdate On (Approach To) Anemia1 (Changes)Balchand KukrejaNo ratings yet
- Influence of Progressive Renal Dysfunction in Chronic Heart FailureDocument6 pagesInfluence of Progressive Renal Dysfunction in Chronic Heart Failurenandhini raguNo ratings yet
- HemolysisDocument3 pagesHemolysisJoey JoseNo ratings yet
- 1191 2299 2 PB PDFDocument7 pages1191 2299 2 PB PDFTitis CresnaulanNo ratings yet
- Haematological Manifestationsin SLE PDFDocument21 pagesHaematological Manifestationsin SLE PDFLe DungNo ratings yet
- 857 1857 1 PBDocument4 pages857 1857 1 PBJesselle LasernaNo ratings yet
- Hemolytic Uremic SyndromeDocument2 pagesHemolytic Uremic SyndromeAndrea TeranNo ratings yet
- JR TA AnemiaDocument26 pagesJR TA AnemiaMohamad Ananto CNo ratings yet
- Anaemia and Red Blood CellDocument14 pagesAnaemia and Red Blood CelltomreneyoNo ratings yet
- Aki 6Document12 pagesAki 6WindaNo ratings yet
- Management: DiagnosisDocument6 pagesManagement: DiagnosisAhmed El-MalkyNo ratings yet
- Anemia of Chronic Kidney Disease (CKD)Document1 pageAnemia of Chronic Kidney Disease (CKD)Izzatul YazidahNo ratings yet
- Hematological Manifestations of Connective Tissue Disorders: Aymen OmerDocument69 pagesHematological Manifestations of Connective Tissue Disorders: Aymen OmeraymenNo ratings yet
- AntmiaDocument85 pagesAntmiafrendirachmadNo ratings yet
- Mon Anemia and CardiovascularDocument11 pagesMon Anemia and CardiovasculartyasNo ratings yet
- Decompensatedcirrhosis Andfluidresuscitation: Erin MaynardDocument6 pagesDecompensatedcirrhosis Andfluidresuscitation: Erin MaynardBruno MaiaNo ratings yet
- AnemiaFactSheet ANNADocument5 pagesAnemiaFactSheet ANNARahmad HidayatNo ratings yet
- Lec 2Document10 pagesLec 2fbbqbcht6yNo ratings yet
- Approach Considerations: Magnetic Resonance Imaging in Research SettingsDocument5 pagesApproach Considerations: Magnetic Resonance Imaging in Research SettingsLamyaa Ali HasanNo ratings yet
- Hematology L5Document22 pagesHematology L5Haibat Sultan StationeryNo ratings yet
- Anemia in CKD (B BATCH)Document16 pagesAnemia in CKD (B BATCH)Mayank SharmaNo ratings yet
- Anemia (: /Ə Ni Miə/ Also Spelled Greek Red Blood Cells HemoglobinDocument13 pagesAnemia (: /Ə Ni Miə/ Also Spelled Greek Red Blood Cells HemoglobinAryana BudiawanNo ratings yet
- Chronic Kidney DiseaseDocument17 pagesChronic Kidney Diseaseniken_rizkiNo ratings yet
- MEDSEM2LE4 Approach To AnemiaDocument19 pagesMEDSEM2LE4 Approach To AnemiaAndrea Ann MagpayoNo ratings yet
- Emergency Medicine Clinics of North America Volume Issue 2014 (Doi 10.1016 - J.emc.2014.04.007) Vieth, Julie T. Lane, David R. - AnemiaDocument16 pagesEmergency Medicine Clinics of North America Volume Issue 2014 (Doi 10.1016 - J.emc.2014.04.007) Vieth, Julie T. Lane, David R. - AnemiaJeffrey Stefan Pal RiveraNo ratings yet
- Erythrocyte Life Cycle: PathophysiologyDocument15 pagesErythrocyte Life Cycle: PathophysiologyYeniNo ratings yet
- Grade 7 Math ModuleDocument5 pagesGrade 7 Math ModuleAndre Labiste Aninon100% (2)
- Anemia Hip Pain Sickle Cell DiseaseDocument9 pagesAnemia Hip Pain Sickle Cell DiseasePerplexed CeleryNo ratings yet
- Nephrologi NotesDocument43 pagesNephrologi NotesSigit Harya HutamaNo ratings yet
- Anaemia: What Is Anemia?Document21 pagesAnaemia: What Is Anemia?Rashed ShatnawiNo ratings yet
- Hema - Guide Notes PDFDocument21 pagesHema - Guide Notes PDFVanessa Ladra100% (1)
- Chronic Kidney Disease (CKD) : By: Dr. Abiy WDocument48 pagesChronic Kidney Disease (CKD) : By: Dr. Abiy WyohannesNo ratings yet
- Management of Patients With Kidney DisordersDocument129 pagesManagement of Patients With Kidney DisordersJerome RarogalNo ratings yet
- Renalparenchymatous Hypertension: Vitebsk State Medical University, Internal Disease DepartmentDocument4 pagesRenalparenchymatous Hypertension: Vitebsk State Medical University, Internal Disease DepartmentSanduni WickramaratneNo ratings yet
- Inter'Medic CKDDocument31 pagesInter'Medic CKDMAHEJS HD100% (1)
- Acute Renal FailureDocument12 pagesAcute Renal FailureRifa Aprillia CahyaniNo ratings yet
- AnemiaDocument3 pagesAnemiaTwinkle Wong DevibarNo ratings yet
- Chronic Renal Failure Chapter 261 Pp. 1653-1663Document6 pagesChronic Renal Failure Chapter 261 Pp. 1653-1663Emil GulmaticoNo ratings yet
- AnemiaDocument9 pagesAnemiaAhmed MansourNo ratings yet
- Sindrom NefrotikDocument22 pagesSindrom NefrotikGyta Apriati100% (1)
- Acute Kidney Injury in HFDocument14 pagesAcute Kidney Injury in HFAnonymous NeRC5JYiSNo ratings yet
- crf03 1Document16 pagescrf03 1Aswin DamodaranNo ratings yet
- By DR - Vasudeva Chetty PakalaDocument97 pagesBy DR - Vasudeva Chetty Pakalaace forumNo ratings yet
- Wa0011.Document180 pagesWa0011.Mohamed AbdelmoniemNo ratings yet
- Doctors - 1 Lacs DataDocument64 pagesDoctors - 1 Lacs DataEconaur0% (1)
- Outpatient MedicineDocument0 pagesOutpatient Medicineclaragustin_53768590No ratings yet
- HemodialysisDocument19 pagesHemodialysissofi wardatiNo ratings yet
- Clinical Characteristic and Outcome of Acute Lower Respiratory Tract Infection in Children With Congenital Heart DiseaseDocument6 pagesClinical Characteristic and Outcome of Acute Lower Respiratory Tract Infection in Children With Congenital Heart DiseaseYenieMaciechESweteNo ratings yet
- Cardiac Oral Presentations - Program-Escvs 2017 PDFDocument32 pagesCardiac Oral Presentations - Program-Escvs 2017 PDFGhenadie BostanNo ratings yet
- Tracing:: ABILLAR, Rica MendozaDocument2 pagesTracing:: ABILLAR, Rica Mendozajzyryl abillarNo ratings yet
- Echo, ABPM and HolterDocument5 pagesEcho, ABPM and HolterLeo Anne BrazilNo ratings yet
- PDF Priscillax27s Medicine With Addon Final DDDocument166 pagesPDF Priscillax27s Medicine With Addon Final DDValsala BaskaranNo ratings yet
- Asuhan Keperawatan Kritis Dengan MCIDocument28 pagesAsuhan Keperawatan Kritis Dengan MCIsusi jNo ratings yet
- Lita SantosDocument3 pagesLita SantosMaye Arugay100% (1)
- Hahn - Internist Medical AutobioDocument32 pagesHahn - Internist Medical AutobiozipoliteNo ratings yet
- Cardiogenic Shock HandoutsDocument2 pagesCardiogenic Shock HandoutsAileenNo ratings yet
- Interpretation: L72 - Jammu (Lower Roop Nagar) CC H.No: 1, Sector-7, Ews Colonyjammu, JMK JammuDocument2 pagesInterpretation: L72 - Jammu (Lower Roop Nagar) CC H.No: 1, Sector-7, Ews Colonyjammu, JMK JammuSanjay GanjooNo ratings yet
- Full Download pdf of Cardiology Secrets, 6th Edition Glenn N. Levine - eBook PDF all chapterDocument63 pagesFull Download pdf of Cardiology Secrets, 6th Edition Glenn N. Levine - eBook PDF all chapterjinggomasito100% (6)
- Dipiro 9th MCQDocument380 pagesDipiro 9th MCQHaymanot AnimutNo ratings yet
- 8977 HiDocument6 pages8977 Hiwanwan_adongNo ratings yet
- (Physio A) ECG (Javier)Document4 pages(Physio A) ECG (Javier)AliNo ratings yet
- Intervento Di FontaneDocument3 pagesIntervento Di FontaneJ.c. ColussusNo ratings yet
- Electrical Diseases of The Heart PDFDocument982 pagesElectrical Diseases of The Heart PDFJavierPiñeiroAndradeNo ratings yet
- HYPERTENSION+QUESTIONNAIRE+ (Rev 1+2012) PDFDocument1 pageHYPERTENSION+QUESTIONNAIRE+ (Rev 1+2012) PDFZito Amora100% (1)
- Ischemic Heart Disease (IHD)Document37 pagesIschemic Heart Disease (IHD)Yowan SusantiNo ratings yet
- Speaker: Maj YS Swapna Sudha Chair Person: Maj Swapna Dharmaji Moderator: Col S.SenguptaDocument33 pagesSpeaker: Maj YS Swapna Sudha Chair Person: Maj Swapna Dharmaji Moderator: Col S.SenguptaSudha Kiran100% (1)
- Latihan Ekg KD A III 2016Document15 pagesLatihan Ekg KD A III 2016Syamsul PutraNo ratings yet
- IHD - JalalDocument46 pagesIHD - JalalMituran IshwarNo ratings yet
- Sally Aburumman Bushra SaleemDocument75 pagesSally Aburumman Bushra SaleemAbdulrahman AlsayyedNo ratings yet
- Tabel Severitas BPJS Tindakan JantungDocument9 pagesTabel Severitas BPJS Tindakan JantungTeduh ParamadinaNo ratings yet
- Ventricular Septal Defect VSD FactsheetDocument3 pagesVentricular Septal Defect VSD FactsheetArgolekso RatriNo ratings yet
- Acute Kidney Injury in Children: Being AWAREDocument4 pagesAcute Kidney Injury in Children: Being AWAREIrkania PasangkaNo ratings yet
- Cardiology Basic QuestionsDocument9 pagesCardiology Basic QuestionsSunita PooniaNo ratings yet