Professional Documents
Culture Documents
Pediatric Septic Shock
Pediatric Septic Shock
Uploaded by
Sugi DenyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatric Septic Shock
Pediatric Septic Shock
Uploaded by
Sugi DenyCopyright:
Available Formats
Pediatric Septic Shock 1
Section I: Scenario Demographics
Scenario Title: Pediatric Septic Shock
Date of Development: 09/06/2015 (DD/MM/YYYY)
Target Learning Group: Juniors (PGY 1 – 2) Seniors (PGY ≥ 3) All Groups
Section II: Scenario Developers
Scenario Developer(s): Kyla Caners
Affiliations/Institution(s): McMaster University
Contact E-mail (optional): kcaners@gmail.com
Section III: Curriculum Integration
Learning Goals & Objectives
Educational Goal: To allow learners to become more comfortable managing common issues associated
with pediatric resuscitation.
CRM Objectives: 1) Communicate effectively with team regarding orders and drug doses.
2) Allocate resources appropriately to manage a distraught parent.
Medical Objectives: 1) Recognize the need for early IO access in critically unwell child where iv
unsuccessful.
2) Initiate appropriate investigations and treatment for septic child. Specifically:
a. Check capillary blood glucose.
b. Administer IV antibiotics.
c. Prioritize IV fluid pushes then vasopressors
3) Recognize the need to intubate a septic child with altered LOC.
Case Summary: Brief Summary of Case Progression and Major Events
A 4 year-old girl is brought to the ED because she is “not herself.” She has had 3 days of fever and cough
and is previously healthy. She looks toxic on arrival with delayed capillary refill, a glazed stare, tachypnea
and tachycardia. The team will be unable to obtain IV access and will need to insert an IO. Once they have
access, they will need to resuscitate by pushing fluids. If they do not, the patient’s BP will drop. If a cap
sugar is not checked, the patient will seize. The patient will remain listless after fluid resuscitation and will
require intubation.
References
Marx, J. A., Hockberger, R. S., Walls, R. M., & Adams, J. (2013). Rosen's emergency medicine: Concepts and clinical practice. St. Louis: Mosby.
http://circ.ahajournals.org/content/132/18_suppl_2/S526
http://www.rch.org.au/clinicalguide/guideline_index/Intraosseous_access/
© 2015 EMSIMCASES.COM Page 1
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Pediatric Septic Shock 2
Section IV: Scenario Script
A. Scenario Cast & Realism
Patient: Pediatric Computerized Realism: Conceptual
Mannequin
Mannequin Select most Physical
Standardized Patient important Emotional/Experiential
Hybrid dimension(s) Other:
Task Trainer N/A
Confederates Brief Description of Role
Mother Can provide history. (To add a challenge for seniors, mother can become obstructive to
care or extremely distraught.)
RN To indicate when iv access cannot be established
B. Required Monitors
EKG Leads/Wires Temperature Probe Central Venous Line
NIBP Cuff Defibrillator Pads Capnography
Pulse Oximeter Arterial Line Other:
C. Required Equipment
Gloves Nasal Prongs Scalpel
Stethoscope Venturi Mask Tube Thoracostomy Kit
Defibrillator Non-Rebreather Mask Cricothyroidotomy Kit
IV Bags/Lines Bag Valve Mask Thoracotomy Kit
IV Push Medications Laryngoscope Central Line Kit
PO Tabs Video Assisted Laryngoscope Arterial Line Kit
Blood Products ET Tubes Other: masks, gowns, gloves for
droplet precautions
Intraosseous Set-up LMA Other:
D. Moulage
None required.
E. Approximate Timing
Set-Up: 3 min Scenario: 12 min Debriefing: 20 min
© 2015 EMSIMCASES.COM Page 2
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Pediatric Septic Shock 3
Section V: Patient Data and Baseline State
A. Clinical Vignette: To Read Aloud at Beginning of Case
A 4-year-old girl presents to your pediatric ED. Her mother states she is “not herself” and seems
“lethargic.” She’s had a fever and a cough for the last three days. Today she just seems different. She was
brought straight into a resus room and the charge nurse came to find you to tell you the child looks unwell.
B. Patient Profile and History
Patient Name: Rebecca Smythe Age: 4 Weight: 20kg
Gender: M F Code Status: Full
Chief Complaint: Lethargic
History of Presenting Illness: Fever and cough for last three days. Today, not as responsive. Doesn’t
seem interested in anything. Won’t eat or drink. Doesn’t look like herself. No known sick contacts, but she
does go to pre-kindergarten.
Past Medical History: Healthy Medications: None
IUTD
Term delivery, no issues.
Allergies: None.
Social History: Lives with mom and dad. Goes to pre-kindergarten class. Has a one year old brother.
Family History: Dad has asthma.
Review of Systems: CNS: Lethargic today. Sort of listless and uninterested.
HEENT: Nil.
CVS: Nil.
RESP: Cough for last three days.
GI: Nil.
GU: Mom doesn’t think she’s peed today.
MSK: Nil. INT: No rashes.
C. Baseline Simulator State and Physical Exam
No Monitor Display Monitor On, no data displayed Monitor on Standard Display
HR: 140/min BP: 82/44 RR: 40/min O2SAT: 91%
Rhythm: Sinus tach T: 39oC Glucose: 2.4 mmol/L
General Status: Looks toxic and unwell.
CNS: Glazed stare. Lethargic. PERLA.
HEENT: Normal TMs. PERLA. Glazed stare.
CVS: No murmur. Cap refill 5 seconds centrally. Eyes sunken.
RESP: GAEB. Rhonchi to R.
ABDO: Nil.
GU: Nil.
MSK: No hot joints. SKIN: No rashes.
© 2015 EMSIMCASES.COM Page 3
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Pediatric Septic Shock 4
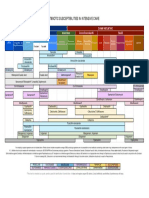
Section VI: Scenario Progression
Scenario States, Modifiers and Triggers
Patient State Patient Status Learner Actions, Modifiers & Triggers to Move to Next State
1. Baseline State Looks unwell. Learner Actions Modifiers
Rhythm: Sinus tach Cap refill 5 sec. - Attempt IV access (unable) Changes to patient condition based on
HR: 140/min Glazed stare. - Attempt IO access learner action
BP: 82/44 - Monitors - No push dose fluids after access,
RR: 40/min - Apply O2 no access by 2 min BP 75/35
O2SAT: 91% - Septic lab workup
T: 39oC - CXR Triggers
- Push fluids 20ml/kg x3 For progression to next state
(400ml per bolus) - No glucose check by 4 min
- Check glucose (2.4), replace 2. Seizure
with 2-4ml/kg of D25 (40-80ml) - Glucose checked, fluids given 3.
- Administer antibiotics Persistent hypotension
(ceftriaxone 50mg/kg iv) - 6 min 3. Persistent
- Take history from mother Hypotension
2. Seizure Nurse states “I Learner Actions Modifiers
think she’s - Check glucose (2.4), replace - Benzo given no change to
HR 155 seizing” and with 2-4ml/kg of D25 (40-80ml) seizure
BP 145/95 activates seizure. - Ensure staff wearing masks
(Optional: (meningitis risk) Triggers
mother to start - ± Add vancomycin for CSF - Glucose given 3. Persistent
panic “what do penetration Hypotension
you mean she’s - Delegate team member to - 8 min 3. Persistent
seizing??”) keep mother calm and informed Hypotension
3. Persistent Patient still Learner Actions Modifiers
Hypotension listless, poorly - Bolus up to total of 60ml/kg - 9 min (no pressor) BP 70/30
responsive. of fluid - 10 min (no pressor) BP 65/25
HR 130 - Start vasopressor (epi at 0.05
BP 75/35 mcg/kg/min or norepi at Triggers
0.05mcg/kg/min) - Pressor started 4. Poorly
- Consult ICU responsive
- Consider intubation - Intubation 5. Intubation
4. Poorly Responsive Patient not Learner Actions Modifiers
responsive at all. - Consider intubation - If not considering intubation
HR 120 BP/HR - Choose correct tube size (5 slowly decrease O2SATS to 85%
BP 85/45 stabilized, but uncuffed, 4.5 cuffed)
LOC worsening. - Ketamine or etomidate Triggers
- Paralytic - Intubate 5. Intubate
- Apneic oxygenation
5. Intubation Learner Actions Modifiers
- Intubate as above - Paralytics given RR 0
Unchanged - Post-intubation CXR
- Start sedation (midazolam) Triggers
- Insert OG - Intubation END CASE
- Call ICU - 12 min END CASE
© 2015 EMSIMCASES.COM Page 4
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Pediatric Septic Shock 5
Section VII: Supporting Documents, Laboratory Results, & Multimedia
Laboratory Results
No blood work required for this case.
Images (ECGs, CXRs, etc.)
CXR showing pneumonia:
CXR source: http://radiopaedia.org/articles/round-pneumonia-1
ECG showing sinus tachycardia:
ECG source: http://lifeinthefastlane.com/ecg-library/sinus-tachycardia/
© 2015 EMSIMCASES.COM Page 5
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Pediatric Septic Shock 6
Section VIII: Debriefing Guide
General Debriefing Plan
Individual Group With Video Without Video
Objectives
Educational Goal: To allow learners to become more comfortable managing common issues
associated with pediatric resuscitation.
CRM Objectives: 1) Communicate effectively with team regarding orders and drug doses.
2) Allocate resources appropriately to manage a distraught parent.
Medical Objectives: 1) Recognize the need for early IO access in critically unwell child where
iv unsuccessful.
2) Initiate appropriate investigations and treatment for septic child.
Specifically:
a. Check capillary blood glucose.
b. Administer IV antibiotics.
c. Prioritize IV fluid pushes then vasopressors
3) Recognize the need to intubate a septic child with altered LOC.
Sample Questions for Debriefing
1) How did it feel to perform a resuscitation with a distraught mother in the room? How do you feel the
team handled the situation? Do you have any suggestions for how to improve this?
2) How did the team approach drug dosing in this child? Did you all feel comfortable with how dosing
decisions were made and communicated? What are some ways to calculate weight and dosing when
you are uncertain?
3) Does everyone feel comfortable putting in an IO? What are the steps? Where you can put it?
4) How do you calculate glucose replacement in a child?
5) What considerations are required for a pediatric intubation as compared to an adult intubation?
Key Moments
Recognition of need for IO access.
Addressing needs of distraught mother.
Decision to start vasopressors and intubate.
© 2015 EMSIMCASES.COM Page 6
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
You might also like
- Sbar Mini Case StudiesDocument2 pagesSbar Mini Case Studiesapi-367705934No ratings yet
- 4melnyk Ebp Search For EvidenceDocument7 pages4melnyk Ebp Search For Evidenceapi-272725467No ratings yet
- Ely. Delirium SlidesDocument51 pagesEly. Delirium SlidesParvathy R NairNo ratings yet
- 2melnyk Ebp The Seven StepsDocument3 pages2melnyk Ebp The Seven Stepsapi-272725467100% (1)
- 51 To 100 Beded Hospital NormsDocument85 pages51 To 100 Beded Hospital NormsRAJU86% (7)
- StressDocument3 pagesStressabydlNo ratings yet
- Nutrition Management Premie NashDocument49 pagesNutrition Management Premie NashathaNo ratings yet
- Pediatric Assessment: General ImpressionDocument2 pagesPediatric Assessment: General ImpressionAghnia Nafila100% (1)
- 5P Handoff SheetDocument1 page5P Handoff SheetBarry SeeboNo ratings yet
- Ped All PatientDocument94 pagesPed All PatientRio Handi SanjayaNo ratings yet
- ABCDE Education SlidesDocument43 pagesABCDE Education SlidesEvangelina María C. PoliNo ratings yet
- SDPSC Icu Sedation Guidelines of Care Toolkit December 2009Document44 pagesSDPSC Icu Sedation Guidelines of Care Toolkit December 2009yonoNo ratings yet
- Pharmacology and The Nursing ProcessDocument28 pagesPharmacology and The Nursing ProcessEdralyn MatalangNo ratings yet
- Best Practice in ShockDocument30 pagesBest Practice in ShockFoungZanz D. LuffyzNo ratings yet
- Patient Satisfaction With The Health CareDocument15 pagesPatient Satisfaction With The Health CareEmna MahjoubiNo ratings yet
- Empirical Treatment of Sepsis in AdultsDocument11 pagesEmpirical Treatment of Sepsis in AdultsMarnia SulfianaNo ratings yet
- Anxiolytics and AntidepressantsDocument271 pagesAnxiolytics and AntidepressantsAmir PeljtoNo ratings yet
- Nursing Handover of Vital Signs at The Transition of Care Fromthe Emergency Department To The Inpatient Ward Anintegrative ReviewDocument12 pagesNursing Handover of Vital Signs at The Transition of Care Fromthe Emergency Department To The Inpatient Ward Anintegrative ReviewLilac SpaceNo ratings yet
- Chamberlain College of Nursing: Name: DateDocument6 pagesChamberlain College of Nursing: Name: DategabrielNo ratings yet
- Assessment Algorithm For Sedated Adult ICU Patients: No YesDocument18 pagesAssessment Algorithm For Sedated Adult ICU Patients: No YeshendraNo ratings yet
- Guide For Drug Level Monitoring of Commonly Used MedicationsDocument4 pagesGuide For Drug Level Monitoring of Commonly Used MedicationsMohamed HussienNo ratings yet
- Care Plan TemplateDocument12 pagesCare Plan TemplateemipNo ratings yet
- GNUR 383 LeadershipstudentDocument2 pagesGNUR 383 LeadershipstudentmerNo ratings yet
- A Nurse PractitionerDocument4 pagesA Nurse PractitionerN.DanielaNo ratings yet
- Pediatric EmergenciesDocument47 pagesPediatric EmergenciesahmedNo ratings yet
- Bsn-Rs-Careplan 2Document9 pagesBsn-Rs-Careplan 2api-520841770No ratings yet
- Board Certified Nurse Practitioner in Savannah GA Resume Michele StephensDocument4 pagesBoard Certified Nurse Practitioner in Savannah GA Resume Michele StephensMicheleStephens100% (1)
- The New Rapid ResponderDocument3 pagesThe New Rapid RespondersarahNo ratings yet
- CV ResidencyDocument5 pagesCV Residencyapi-355090691No ratings yet
- West Visayas State University: Nursing ProcessDocument4 pagesWest Visayas State University: Nursing ProcessPhylum Chordata100% (1)
- Ped Medications Chapter 11Document51 pagesPed Medications Chapter 11allisonNo ratings yet
- Sree Vasantham Hospital, Salem: 1. Er Protocol For Acute Intoxication (Poisoning)Document7 pagesSree Vasantham Hospital, Salem: 1. Er Protocol For Acute Intoxication (Poisoning)Elango MuthuNo ratings yet
- CCU Clinical GuidelinesDocument63 pagesCCU Clinical GuidelinesHAMMYER ALROKHAMINo ratings yet
- Clinical Placement Summary 2018 Barwon Health GeelongDocument9 pagesClinical Placement Summary 2018 Barwon Health Geelongapi-569029509No ratings yet
- Nursing Philosophy ReflectionDocument7 pagesNursing Philosophy Reflectionapi-480790431No ratings yet
- Outcomes of Ebp Process 2017Document3 pagesOutcomes of Ebp Process 2017api-272725467100% (1)
- Empirical Treatment of Sepsis in AdultsDocument15 pagesEmpirical Treatment of Sepsis in AdultsTaufik HakimNo ratings yet
- Handoffs - Implications For NursesDocument48 pagesHandoffs - Implications For Nursesaellenberg3755No ratings yet
- Conflict PresentationDocument19 pagesConflict Presentationapi-231905851No ratings yet
- Drugs in Cardiac EnmergenciesDocument94 pagesDrugs in Cardiac EnmergenciesVijayan VelayudhanNo ratings yet
- Virtual Simulation Undergraduate StudentsDocument9 pagesVirtual Simulation Undergraduate Studentskaren soliba0% (1)
- Think Nursing! ReportDocument20 pagesThink Nursing! ReportRobert Fraser RNNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- NomogramDocument2 pagesNomogramtammy_1025043737No ratings yet
- Calculation Skills For Paediatric NursingDocument19 pagesCalculation Skills For Paediatric NursingGovindaraju SubramaniNo ratings yet
- Head To Toe AssessmentDocument3 pagesHead To Toe Assessmentsandaman2225No ratings yet
- Pharmacology 2 NotesDocument14 pagesPharmacology 2 NotesNikko MabbayadNo ratings yet
- Guide To APRN RoleDocument4 pagesGuide To APRN RoleLaceyNo ratings yet
- Normal DIE CPP Calculations:: Increased Intracranial Pressure (Cerebral Perfusion Pressure)Document79 pagesNormal DIE CPP Calculations:: Increased Intracranial Pressure (Cerebral Perfusion Pressure)Nur SanaaniNo ratings yet
- Eportfolio Resume CVDocument4 pagesEportfolio Resume CVapi-577441503No ratings yet
- ICU Checklist For RoundingDocument1 pageICU Checklist For RoundingViolaNo ratings yet
- Elder Abuse and NelgectDocument10 pagesElder Abuse and Nelgectنادر القحطانيNo ratings yet
- Inserting A Nasogastric (NG) Tube Goal: The Tube Is Passed Into The Patient's Stomach CommentsDocument4 pagesInserting A Nasogastric (NG) Tube Goal: The Tube Is Passed Into The Patient's Stomach CommentsschniqueNo ratings yet
- ABCDEF Bundle WebcastDocument42 pagesABCDEF Bundle WebcastsoulstakersNo ratings yet
- Antibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeDocument1 pageAntibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeFaisal Reza AdiebNo ratings yet
- Nursing Code of EthicsDocument2 pagesNursing Code of EthicsClarissa HeatonNo ratings yet
- System Disorder ADDocument1 pageSystem Disorder ADSariahNo ratings yet
- Ventricular Tachycardia Bsn3b-Grp1Document35 pagesVentricular Tachycardia Bsn3b-Grp1Jessica RamosNo ratings yet
- Antiarrhytmics Treatable Antiarrhytmics: Atrial Fibrillation, Atrial Flutter, Vtach and PSVT Drugs MOA Indication S/E NotesDocument1 pageAntiarrhytmics Treatable Antiarrhytmics: Atrial Fibrillation, Atrial Flutter, Vtach and PSVT Drugs MOA Indication S/E Notesmonica leeNo ratings yet
- Devoir de Synthèse N°2 2011 2012 (Lycée Ali Bourguiba Bembla)Document4 pagesDevoir de Synthèse N°2 2011 2012 (Lycée Ali Bourguiba Bembla)ferchichi halimaNo ratings yet
- Leaflet - Clofazimine Tablets 100mgDocument1 pageLeaflet - Clofazimine Tablets 100mgdillah azhariNo ratings yet
- Public Health-Relevant Consequences of The COVID-19 Pandemic On Malaria in Sub-Saharan Africa: A Scoping ReviewDocument16 pagesPublic Health-Relevant Consequences of The COVID-19 Pandemic On Malaria in Sub-Saharan Africa: A Scoping ReviewM Franck MakongaNo ratings yet
- NCoV Corona Virus Template Slide PowerpointDocument30 pagesNCoV Corona Virus Template Slide PowerpointĐặng NamNo ratings yet
- PharmacologyDocument53 pagesPharmacologyapi-3743565No ratings yet
- Rife Frequency List For Rife Frequency GeneratorDocument18 pagesRife Frequency List For Rife Frequency GeneratorAttila Dudás100% (2)
- St. Joseph'S High School San Narciso, QuezonDocument22 pagesSt. Joseph'S High School San Narciso, QuezonDaphane Kate AureadaNo ratings yet
- Antepartum Fetal Assessment 2018Document39 pagesAntepartum Fetal Assessment 2018amena mahmoudNo ratings yet
- s41416 023 02233 XDocument7 pagess41416 023 02233 Xevita.irmayantiNo ratings yet
- Class XII PHY - EDDocument7 pagesClass XII PHY - EDsampoornaswayamNo ratings yet
- Journal Reading SinusitisDocument13 pagesJournal Reading SinusitisDiniEsfandiariNo ratings yet
- Journal EntryDocument2 pagesJournal EntryABDULJAMIR GAYAKNo ratings yet
- Sleep and RestDocument85 pagesSleep and RestJann ericka Jao100% (2)
- Prediksi Soal Utbk Bahasa Inggris 2022Document4 pagesPrediksi Soal Utbk Bahasa Inggris 2022Aulia Azhar0% (1)
- Laporan Obat Januari 21Document27 pagesLaporan Obat Januari 21PUSKESMAS PLANTUNGAN KDLNo ratings yet
- Liver CirrhosisDocument5 pagesLiver CirrhosisRLLTNo ratings yet
- Medical Devices PDFDocument38 pagesMedical Devices PDFDr D Alwin , VetNo ratings yet
- Healthcare Associated Infections in The Nicu PowerpointDocument21 pagesHealthcare Associated Infections in The Nicu Powerpointapi-489132887No ratings yet
- Initial Assessment and ManagementDocument13 pagesInitial Assessment and ManagementterriNo ratings yet
- CLCPDocument43 pagesCLCPeviltohuntNo ratings yet
- Pin Infection Grading SystemDocument1 pagePin Infection Grading SystemAlok SinghNo ratings yet
- Basic Maternity ConceptsDocument14 pagesBasic Maternity ConceptsDivine Grace Arreglo AbingNo ratings yet
- ExplanationDocument8 pagesExplanationmarisa dwilestariNo ratings yet
- 7.scope of NursingDocument33 pages7.scope of Nursingmaria jacobNo ratings yet
- SlicDocument3 pagesSlicapi-281774855No ratings yet
- Lithium Side-Effects ChecklistDocument2 pagesLithium Side-Effects ChecklistChalla Krishna VasanNo ratings yet
- Spinal ImmobilisationDocument34 pagesSpinal ImmobilisationGunther BielenNo ratings yet
- Neonatal Care Protocol For Hospital PhysiciansDocument648 pagesNeonatal Care Protocol For Hospital PhysiciansИван Мельник100% (2)
- Global Epidemiology of DementiaDocument9 pagesGlobal Epidemiology of DementiaMBNo ratings yet