Professional Documents
Culture Documents
Upper Gastrointestinal Toxicity Associated With Long-Term Aspirin Therapy: Consequences and Prevention
Upper Gastrointestinal Toxicity Associated With Long-Term Aspirin Therapy: Consequences and Prevention
Uploaded by
Saiful MukminOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Upper Gastrointestinal Toxicity Associated With Long-Term Aspirin Therapy: Consequences and Prevention
Upper Gastrointestinal Toxicity Associated With Long-Term Aspirin Therapy: Consequences and Prevention
Uploaded by
Saiful MukminCopyright:
Available Formats
Upper Gastrointestinal
Toxicity Associated With
Long-Term Aspirin Therapy:
Consequences and Prevention
Carl J. Lavie, MD, Colin W. Howden, MD,
James Scheiman, MD, and James Tursi, MD
Abstract: Antiplatelet therapy represents a fundamental
part of preventive management for patients who are at
risk of a secondary cardiovascular disease (CVD) event.
In most cases, the antiplatelet regimen is based on low-
dose aspirin, a drug that is highly effective in reducing the
incidence of CVD events, but is associated with a
substantial risk of gastrointestinal (GI) toxicity. The
dyspeptic symptoms, which can result from aspirin
administration, and which may occur with or without
associated ulceration and bleeding, may lead patients to
discontinue therapy, thus increasing their CVD risk. For
patients in whom aspirin is indicated and who are deemed
to be at increased risk of upper GI events, concomitant
therapy with a proton pump inhibitor (PPI) is currently
recommended. These agents are highly effective in
reducing the upper GI lesions associated with aspirin
therapy and have been associated with increased aspirin
adherence. However, widespread under-prescribing of
PPIs and potential noncompliance with their use means
that substantial numbers of patients are at unnecessary
risk of upper GI toxicity and—if aspirin therapy is
discontinued—CVD events. Provision of aspirin and
an immediate-release PPI as a coordinated-delivery
Conflict of interest: C.L., consultant and promotional speaker for Aralez Pharmaceuticals; C.W.H., consultant for
Takeda Pharmaceutical Company, Otsuka Pharmaceutical Company, Ironwood Pharmaceuticals, Aralez Pharma-
ceuticals, US WorldMeds, SynteractHCR; Expert witness for Allergan; co-editor, Alimentary Pharmacology &
Therapeutics; J.S.: consultant to Aralez Pharmaceuticals; and J.T.: employee, Aralez Pharmaceuticals R&D Inc.
Curr Probl Cardiol 2017;42:146–164.
0146-2806/$ – see front matter
http://dx.doi.org/10.1016/j.cpcardiol.2017.01.006
146 Curr Probl Cardiol, May 2017
combination tablet has been shown to both reduce the risk
of gastric ulcer formation and improve patient compli-
ance. This strategy, which may ultimately reduce the
incidence of CVD outcomes because of the associated
reduction in GI symptoms and the potential for greater
patient adherence to aspirin, warrants further investiga-
tion under both randomized controlled conditions
(explanatory trials), and in real-life settings (pragmatic
trials). (Curr Probl Cardiol 2017;42:146–164.)
Introduction
atients who survive a primary cerebrovascular or cardiovascular
P (CV) disease (CVD) event are at substantial risk of a subsequent
event.1,2 Secondary prevention is, therefore, of utmost importance
in the management of these patients. Antiplatelet therapy (APT) represents
a cornerstone of secondary prevention strategies,3,4 and aspirin is widely
recommended as the basis of APT in almost all patients who have had a
primary CVD event. For example, the American Heart Association (AHA)
and the American College of Cardiology Foundation (ACCF) recommend
the use of aspirin (75-162 mg/d) in all patients with coronary artery disease
(CAD), unless contraindicated (eg, allergy to nonsteroidal anti-
inflammatory drugs).3,5,6 The European Society of Cardiology (ESC)
recommends use of low-dose aspirin (75-150 mg/d) in all patients with
stable CAD.1 The AHA and the American Stroke Association recommend
the use of aspirin (50-325 mg/d) in patients who have had a stroke or
transient ischemic attack because of 50%-99% stenosis of a major
intracranial artery.4
These recommendations are based on evidence that aspirin significantly
reduces the risk of secondary CVD events. In the original Antithrombotic
Trialists’ Collaboration meta-analysis, administration of aspirin to patients
deemed to be at high risk of an occlusive vascular event (previous
occlusive event or other predisposing condition) was associated with a
23% reduction in the risk of having a serious CVD event (composite of
nonfatal myocardial infarction [MI], nonfatal stroke, or CVD death).7 In a
follow-up meta-analysis restricted to patients with previous MI, stroke, or
transient ischemic attack, aspirin therapy was associated with significant
reductions in the risks of major CAD events (rate ratio [aspirin vs control]
¼ 0.80), ischemic stroke (0.78), and serious CVD events (MI, stroke
Curr Probl Cardiol, May 2017 147
FIG 1. Effects of aspirin in the secondary prevention of cardiovascular disease.8 In secondary
prevention trials, aspirin reduces the incidence of all major cardiovascular events, but is
associated with an increase in the risk of hemorrhagic events. CHD, coronary heart disease; MI,
myocardial infarction. (Color version of figure is available online.)
[hemorrhagic or other], or CVD death) (0.81; absolute risk reduction,
1.49% per year) (Fig 1).8
Adverse Effects of Aspirin Therapy
Long-term low-dose (r325 mg) aspirin therapy is not, however,
without the potential for adverse effects. In addition to increasing the risk
of major gastrointestinal (GI) or cerebral bleeding,9 low-dose aspirin
therapy is associated with a significant increase in the risk of GI adverse
events.10 In a recent survey, 15% of patients receiving low-dose aspirin
experienced upper GI symptoms.11 Some of the most common GI
complaints reported by aspirin-treated patients are shown in Figure 2.12
The aspirin-treated patients who experience symptoms represent only a
minority of those who are adversely affected. Endoscopic surveys of
patients treated with r325 mg aspirin/d have reported the presence of
gastroduodenal ulcers in 11% of patients, 80% of whom were asympto-
matic,13 and either gastroduodenal ulcers or erosions or both in 48% of
asymptomatic patients.14 As gastric erosions predispose to gastric ulcer-
ation during aspirin therapy,15 these data suggest that a substantial
148 Curr Probl Cardiol, May 2017
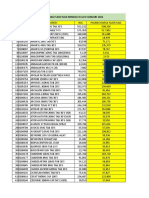
FIG 2. Gastrointestinal complaints experienced by low-dose aspirin-treated patients.12 Patients
whose physicians had recommended the use of low-dose aspirin for the secondary prevention of
cardiovascular (CV) events completed a questionnaire regarding the gastrointestinal problems
they had experienced. Data are shown for the total population of patients requiring CV
protection (n ¼ 437 [“CV protection”]), and the subset of patients who had taken deliberate
short-term breaks from their aspirin regimen (n ¼ 106 [“CV breaker”]). (Reprinted with
permission.)
proportion of asymptomatic patients is at increased risk of gastroduodenal
ulcer development if aspirin therapy is initiated or continued. Of those who
do develop peptic ulcers, approximately one-third have no prior symp-
toms.16,17 Therefore, aspirin-associated GI toxicity may progress to the
point of ulceration, with or without associated bleeding, before the patient
presents to a physician.
In observational studies, long-term low-dose aspirin is associated with
increased relative risks of upper and lower GI bleeding of 2.3 and 1.8,
respectively.18 These relative risks, which were derived from real-world
settings, concur with those from randomized trials,18 and are not mitigated
by the use of enteric-coated or buffered aspirin.19,20 Further, many of these
bleeding episodes occur without prior symptoms.
The adverse effects of aspirin on the GI tract are of sufficient frequency
and potential severity that it is important to balance the risks of GI and
CVD events when deciding on the advisability of prescribing aspirin to a
particular patient.21,22 This is particularly problematic in those at increased
CVD risk who have experienced a previous GI bleed.23 Importantly,
although cessation of aspirin therapy in patients at increased CVD risk who
have experienced peptic ulcer bleeding is associated with decreased risk of
recurrent ulcer bleeding, it is also associated with increased risk of all-
cause mortality.24
Curr Probl Cardiol, May 2017 149
FIG 3. Mechanisms by which aspirin injures the gastrointestinal mucosa. The adverse effects of
aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) on the upper gastrointestinal
(GI) tract mucosa are mediated by both direct and indirect mechanisms. Direct injury results from
trapping of high concentrations of aspirin within gastric epithelial cells. The indirect effects of
aspirin are mediated primarily via inhibition of cyclooxygenase and the resulting reduction in
prostaglandin synthesis. This leads to reductions in the secretion of bicarbonate and epithelial
mucus, mucosal blood flow, and mucosal proliferation necessary for repair. Aspirin also has
adverse effects on production of surface active phospholipids: changes to the hydrophobicity
reduce the acid barrier predisposing to mucosal injury. Other mechanisms of aspirin damage
may occur by microvascular injury with subsequent ischemia, free radical generation, and
cellular damage. The clinical significance of mucosal injury may be exacerbated by aspirin-
mediated inhibition of platelet aggregation, which predisposes to GI bleeding.25-29,78
(Reprinted with permission) (Color version of figure is available online.)
Mechanism for the Effect of Aspirin on the Upper GI
Mucosa
The adverse effects of aspirin on the upper GI tract mucosa are mediated
by both direct and indirect mechanisms (Fig 325-29). Direct topical injury
results from the ability of aspirin (a weak acid) to penetrate the mucous
layer that lines the gastric mucosa and to cross the plasma membrane of
gastric epithelial cells, whereupon the molecule dissociates, trapping
hydrogen ions within the cells.25 However, the main mechanism for its
toxic effects on the mucosa of the upper GI tract is systemic, through
inhibition of cyclooxygenase and consequent reduction in the synthesis of
prostaglandins.25,26 Prostaglandins are gastroprotective and these aspirin
effects lead to reductions in the secretion of bicarbonate and mucus by the
150 Curr Probl Cardiol, May 2017
gastric epithelium, impaired gastric mucosal blood flow, and reduced
epithelial cell proliferation.25,26 Consequently, the gastric mucosa becomes
more susceptible to injury by exogenous and endogenous substances (eg,
stomach acid and pepsin) and shows an impaired ability to repair itself.25,27
Moreover, the inhibition of platelet aggregation that forms the basis of
aspirin’s antithrombotic action will predispose to GI bleeding once
mucosal injury has occurred.27 From a clinical standpoint, the spectrum
of aspirin-induced GI toxicity induced by these mechanisms includes
superficial mucosal injury (subepithelial hemorrhage and erosions) and
mucosal ulceration; however, this may then lead to either hemorrhage or
perforation or both, which could lead to death.25
Risk Factors for Aspirin-Induced Upper GI Toxicity
A number of investigators have attempted to define risk factors for
adverse GI events in aspirin-treated patients. Among the most important
of these is prior peptic ulcer, a risk factor that is aggravated if there is a
history of associated bleeding.20,30 Risk meaningfully increases once
individuals reach the age of 60 years approximately, the increase in risk
showing a nonlinear relationship with rising age thereafter, and there is a
small increase in risk associated with male sex.20,30 Helicobacter pylori
infection is a major independent risk factor for peptic ulcer disease,31 and
one which increases the risk of duodenal ulcer among patients taking
low-dose aspirin.13 Additional risk factors for peptic ulcer disease
identified by Ruigomez et al,32 using data from almost 39,000 new users
of low-dose aspirin prescribed for the secondary prevention of CV
events, include concurrent use of nonsteroidal anti-inflammatory drugs,
anticoagulants, and oral steroids, as well as smoking, stress, depression,
anemia, and social deprivation. Knowledge of risk factors does not,
however, allow rapid quantification of risk for individual patients. In an
attempt to help physicians in routine clinical practice, Lanas et al22 generated
an algorithm that is designed to estimate the CV and GI risks of low-dose
aspirin administration in individual patients. Using data from 68 published
studies, they focused on increased age, male sex, and a history of previous
upper GI pain, dyspepsia, or peptic ulcers as significant risk factors.
Aspirin-Induced Upper GI Toxicity Leads to Poor
Adherence
Most patients who take low-dose aspirin do not experience serious
adverse events such as GI hemorrhage.18 However, less severe symptoms,
Curr Probl Cardiol, May 2017 151
which affect a greater proportion of patients,12 are a cause for concern
because of their association with reduced adherence.
Adherence to aspirin therapy is typically much worse than expected. A
systematic review of 32 studies has shown that, among patients who were
prescribed low-dose aspirin for prevention of CVD events, poor compli-
ance (the definition of which differed among studies) ranged from 10%-
50% and patient-initiated discontinuation of therapy occurred in up to 30%
of patients.33 The authors of this study noted the paucity of information
relating to reasons for poor compliance and discontinuation. However,
more recent data have shown that GI side effects are a prominent driver of
poor adherence to aspirin. In a study that investigated adherence to and
discontinuation of low-dose aspirin therapy prescribed for CV protection
in more than 1000 individuals, Moberg et al12 found that “stomach
problems” were among the most common reasons for lapses in therapy and
for patients taking deliberate short-term breaks. Other studies have also
found that upper GI symptoms are among the most common reasons for
discontinuing aspirin therapy.34
The risk of nonadherence is increased not only by the presence of GI
symptoms, but also by the GI symptom load,35 an association that was
noted in an observational, noninterventional study involving both French
and North American patients. In this study, those who experienced upper
GI symptoms, including gastroesophageal reflux disease-like and dyspep-
tic symptoms, on Z10% of days were significantly more likely to be
nonadherent with low-dose aspirin therapy than those who experienced
such symptoms on o10% of days (Fig 4).35
The clinical relevance of aspirin nonadherence lies in its significant
association with increased incidence of CVD events in patients at risk.36-38
The magnitude of the increase in risk is related to patients’ clinical
characteristics. Using data from 6 studies involving patients who required
aspirin for CAD or secondary prevention of CAD, those undergoing
coronary artery bypass grafting, and those with placement of drug-eluting
stents, Biondi-Zoccai et al36 found that, overall, aspirin discontinuation
was associated with a 3-fold increase in the risk of major adverse CVD
events. However, in patients with intracoronary stents, the increase in risk
was 90-fold.
These data highlight the importance of continuous aspirin therapy in
those patients in whom it is indicated. This includes those who have
experienced peptic ulcer bleeding who are at approximately 7-fold
increased risk of CVD events, and death if aspirin therapy is discon-
tinued.37 The ideal clinical scenario would, therefore, be to minimize the
prevalence of GI symptoms in aspirin-treated patients, thereby improving
152 Curr Probl Cardiol, May 2017
FIG 4. Relationship between symptom load and adherence in aspirin-treated patients.35 In a
multicenter, observational, noninterventional study, patients who were at risk of or who had
confirmed cardiovascular disease and for whom low-dose aspirin had been recommended,
completed an electronic diary for 3 months. The diary documented their aspirin use and any
upper gastrointestinal (GI) symptoms, including gastroesophageal reflux disease (GERD)-like
and dyspeptic symptoms. Among nonadherent patients (those who took o75% of their daily
aspirin doses), a significantly higher proportion reported a high GI symptom load (symptoms on
Z10% of diary days) than a low symptom load (symptoms on o10% of diary days). *P o 0.01.
(Reprinted with permission from Springer.)
patient quality of life, increasing adherence to aspirin, and reducing the
incidence of secondary CVD events.
Prevention of Aspirin-Induced Upper GI Toxicity
Before aspirin therapy is initiated, the benefits and risks should be
carefully weighed.22 Of paramount importance is the institution of
measures to mitigate risk and avoid complications in patients in whom
aspirin is indicated for CVD risk reduction.22 Aspirin dose is a prime
consideration. Low-dose aspirin appears to provide an effective antiplatelet
effect, but is associated with a 2- to 4-fold increase in upper GI event risk20
and a substantial risk of GI bleeding.39 For example, a 2013 meta-analysis
of 9 observational studies reported that the odds ratios (ORs) for upper GI
bleeding were 2.6 (95% CI: 1.9-3.7) and 3.6 (95% CI: 1.7-7.3) for aspirin
doses of r100 and 300-325 mg/d, respectively.40 Although these data
suggest a trend toward increased risk at higher aspirin doses, this is
Curr Probl Cardiol, May 2017 153
countered by the results of a meta-analysis of randomized controlled trials
that included 33,622 individuals treated with aspirin vs 32,365 placebo-
treated individuals. This analysis found that the risk of aspirin-associated
GI events increased at all doses studied (50-162.5 mg/d: OR ¼ 1.59, 95%
CI: 1.40-1.81; 162.5-1500 mg/d: OR ¼ 1.96, 95% CI: 1.58-2.43), with no
relationship between risk of GI hemorrhage and aspirin dose.41 However,
the association between aspirin and major bleeding dictates that the lowest
effective dose should be used for prevention of CVD events and, currently,
it is generally recommended that the daily dose should not exceed 150 mg
(ESC) or 162 mg (AHA/ACCF) in patients in whom aspirin is indicated
for secondary CVD prevention.1,3 The ongoing Aspirin Dosing: A
Patient-centric Trial Assessing Benefits and Long-term Effectiveness study
has been designed to compare the risk-benefit profiles of 81 or 325 mg/d
aspirin.42
The adverse effects of aspirin on the upper GI tract mucosa cannot be
reduced by changes to the drug formulation; neither buffering nor enteric
coating reduces the risk of major upper GI bleeding.19,20 Moreover, the
assumption that buffering and enteric coating would specifically reduce the
incidence of gastric (rather than duodenal) bleeding is not supported by the
results of a case-control study, which reported relative risks of gastric
bleeding for plain, buffered, and enteric-coated aspirin (o325 mg/d) vs
control of 2.6, 3.6, and 3.2, respectively.19 This supports the view that the
adverse effects of aspirin in the upper GI tract are due to its systemic effects
rather than its local, direct effects.19
The strategy that has proven most effective in reducing the incidence of
aspirin-associated GI adverse events is concomitant administration of
drugs that reduce gastric acid secretion. Proton pump inhibitors (PPIs)—
acid-activated prodrugs, which bind covalently to cysteine residues on the
luminal surface of the gastric Hþ/Kþ-ATPase, thereby inhibiting acid
secretion43—are currently the optimal approach.20,44 Numerous studies
have shown that these agents significantly reduce the risk of upper GI
adverse events in aspirin-treated patients.18,22,45-49 For example, meta-
analysis of data from 3 randomized controlled trials found that concomitant
administration of a PPI in patients receiving low-dose aspirin was
associated with an OR for major GI bleeding of 0.34 (95% CI: 0.21-
0.57),50 and other analyses have demonstrated risk reductions of similar or
greater magnitude.22 A multinational, randomized trial found that the
cumulative proportions of patients who developed peptic ulcers after
taking low-dose aspirin for 26 weeks were 1.5% and 1.1% in those who
took concomitant esomeprazole 40 and 20 mg/d, respectively, and 7.4% in
those who took placebo.47
154 Curr Probl Cardiol, May 2017
Gastric acid output can also be reduced by H2-receptor antagonists
(H2RAs), although to a much lesser extent than is seen with the PPIs.51
H2RAs preceded PPIs as the drug class of choice for suppression of acid
production,51 but these agents exhibit tachyphylaxis, which may reduce
clinical efficacy.52,53 Although a recent small study found no significant
difference between the H2RA, famotidine, and the PPI, rabeprazole, in the
incidence of recurrent upper GI bleeding and endoscopic ulcers in aspirin-
treated patients with a history of upper GI bleeding ulcers,54 superiority of
PPIs over H2RAs for the prevention of upper GI tract erosions, ulcers, and
bleeding related to the use of low-dose aspirin has been demonstrated in
numerous studies55,56 (Fig 5 57-63). Furthermore, the ACCF Task Force
recommends PPIs as the preferred option for prevention of aspirin-
associated upper GI tract adverse events (Fig 6).20 The effectiveness of
PPIs may lie, in part, in their ability to prevent ulcer formation in patients
who have gastric erosions before initiation of aspirin therapy: in a recent
study involving patients with this history, Goldstein et al15 found that
gastric ulcers developed in 13.0% of patients who received enteric-coated
aspirin alone and in 4.2% of those who received concomitant immediate-
release omeprazole (P ¼ 0.001). In this study, the aspirin and omeprazole
were delivered simultaneously, in a coordinated-delivery tablet, an
approach which has some advantages over separate administration of 2
drugs.64
FIG 5. Effects of H2-receptor antagonists vs proton pump inhibitors on low-dose aspirin-
associated gastrointestinal lesions.56-63 In a meta-analysis of randomized controlled trials in
which proton pump inhibitors (PPIs) were compared with histamine 2-receptor antagonists
(H2RAs) for the prevention of low-dose aspirin-related gastrointestinal erosion, ulceration, and
bleeding, PPIs were superior to H2RAs. (Reprinted with permission.) (Color version of figure is
available online.)
Curr Probl Cardiol, May 2017 155
FIG 6. ACCF Task Force recommendations for minimization of gastrointestinal bleeding in
patients who require antiplatelet therapy.20 The American College of Cardiology Foundation
(ACCF) Task Force recommends the use of proton pump inhibitors (PPIs) in patients for whom
antiplatelet therapy is indicated but who are at increased risk of gastrointestinal (GI) bleeding.
The cost-effectiveness of PPI therapy increases as the number of GI risk factors increases. GERD,
gastroesophageal reflux disease. (Reprinted with permission.) (Color version of figure is
available online.)
The value of coadministration of a PPI with aspirin lies not only in its
ability to reduce the incidence of upper GI tract adverse events but also in
its ability to reduce the risk of aspirin discontinuation.34,65,66 This has been
demonstrated in both randomized controlled trials and in real-world
observational studies. In 2 identically designed, randomized, double-
blind trials designed to compare the efficacy and safety of enteric-coated
aspirin and an enteric-coated aspirin and immediate-release omeprazole
coordinated-delivery tablet, Whellan et al66 found that there were
significantly fewer discontinuations due to prespecified upper GI adverse
events in the aspirin/PPI group (1.5% vs 8.2%; P o 0.001). Similar
findings have been reported from large patient groups, most notably, a
cohort of more than 35,000 patients with evidence of CVD who were new
users of low-dose aspirin, identified using the Health Improvement
Network primary care database in the United Kingdom.65 In this group,
compared with nonuse of PPIs, continuous PPI use was associated with
significantly lower risk of aspirin discontinuation among patients who
were considered to be at high risk of an upper GI tract adverse event at
156 Curr Probl Cardiol, May 2017
baseline (OR ¼ 0.83, 95% CI: 0.74-0.93).65 An apparent relationship
between PPI dose and risk of discontinuation in patients treated with low-
dose aspirin, as demonstrated in the OBERON study (esomeprazole
40 mg/d ¼ 0.24% of patients permanently stopped taking aspirin;
esomeprazole 20 mg/d ¼ 1.12%; and placebo ¼ 0.87%), requires further
investigation.47
In spite of the evidence supporting the concomitant use of aspirin and
PPIs, suboptimal prescribing of PPIs in patients who are taking aspirin has
been reported.67-69 The scale of this may be substantial. In a survey of more
than 3000 Dutch patients at increased GI risk for whom low-dose aspirin
had been prescribed, 36% did not receive a prescription for a PPI at all and
18% received prescriptions irregularly.67 In a retrospective drug use study
conducted in China, fewer than 3% of prescriptions for low-dose aspirin
were accompanied by a prescription for a PPI.68
This documented under-prescription of PPIs, combined with evidence
that continuous use of PPIs is associated with significantly lower risk of
upper GI tract events than intermittent use (P o 0.0001),70 suggests that
fixed-dose combinations of aspirin and a PPI may be advantageous. This
strategy has been explored using the enteric-coated aspirin (325 mg)/
immediate-release omeprazole (40 mg) coordinated delivery tablet dis-
cussed earlier. In a secondary CVD prevention population comprising
more than 1000 patients, all of whom had been taking aspirin 325 mg/d for
Z3 months and who were at risk of aspirin-associated gastric ulcers, this
fixed-dose aspirin and omeprazole combination was associated with a
significantly lower incidence of endoscopic gastric ulcers than enteric-
coated aspirin alone (3.2% vs 8.6%; P o 0.001).66
Although highly effective in the prevention of upper GI tract toxicity in
aspirin-treated patients, there are a number of possible adverse conse-
quences of long-term PPI use. These include bone fractures and bacterial
enteric infections, including those caused by Clostridium difficile.71 Recent
observational studies have also suggested potential increased risks of
dementia72 and chronic kidney disease73 after PPI use, although the
literature is divergent on these findings. Despite these proposed adverse
consequences of long-term PPI therapy,71 the quality of evidence has
generally been insufficient to establish causality, and multiple studies are
flawed due to residual confounding and channeling bias.74
In terms of CVD risk in PPI-treated patients, there have been
suggestions from a case-control study that PPIs may alter the platelet
response to aspirin,75 and from a retrospective registry study that
coadministration of a PPI may reduce aspirin’s protective effect in
patients with first time MI.76 However, a recent position paper from the
Curr Probl Cardiol, May 2017 157
ESC concluded that these data are not sufficiently robust to suggest that
PPIs adversely affect the CVD protective effects of aspirin.77 As a result,
the ESC continues to recommend the use of PPIs for the prevention of
gastric ulceration in aspirin-treated patients who are at risk of GI
bleeding,77 as do the ACCF Task Force and the Danish Society of
Gastroenterology and Hepatology.20,44 Moreover, the ESC’s 2013 expert
position paper suggests that concomitant PPI use may actually improve
patients’ CVD outcome because of improved compliance.49,77
Summary
Aspirin forms the basis of APT in most patients at increased CVD risk.
However, the risk of upper GI tract adverse events that accompanies
aspirin therapy is associated with reduced adherence, with a consequent
adverse effect on CVD risk. Concomitant administration of a PPI reduces
the incidence of upper GI tract symptoms and improves adherence with
aspirin. However, the widespread under-prescribing of PPIs means that
substantial numbers of patients are at unnecessary risk of upper GI tract
erosions, ulcers, and bleeding, as well as increased CVD risk if aspirin
therapy is discontinued. Provision of aspirin and a PPI as a coordinated-
delivery combination has been shown to reduce the risk of gastric ulcer
formation and to improve compliance in a clinical study. Such a strategy
would be expected to produce the same benefits in routine clinical practice.
Acknowledgments: The authors thank Janet Douglas, PhD, of MedVal
Scientific Information Services, LLC for medical writing and editorial
assistance, which was funded by Aralez Pharmaceuticals R&D Inc. This
article was prepared according to the International Society for Medical
Publication Professionals’ “Good Publication Practice for Communicating
Company-Sponsored Medical Research: The GPP3 Guidelines.”
REFERENCES
1. Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the
management of stable coronary artery disease: the task force on the management of
stable coronary artery disease of the European Society of Cardiology. Eur Heart J
2013;34:2949-3003.
2. Hong KS, Yegiaian S, Lee M, Lee J, Saver JL. Declining stroke and vascular event
recurrence rates in secondary prevention trials over the past 50 years and consequences
for current trial design. Circulation 2011;123:2111-9.
3. Smith SC, Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and
risk reduction therapy for patients with coronary and other atherosclerotic vascular
158 Curr Probl Cardiol, May 2017
disease: 2011 update: a guideline from the American Heart Association and American
College of Cardiology Foundation. Circulation 2011;124:2458-73.
4. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in
patients with stroke or transient ischemic attack: a guideline for healthcare profes-
sionals from the American Heart Association/American Stroke Association. Stroke
2011;42:227-76.
5. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/
STS Guideline for the diagnosis and management of patients with stable ischemic heart
disease: a report of the American College of Cardiology Foundation/American Heart
Association Task Force on Practice Guidelines, and the American College of
Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular
Nurses Association, Society for Cardiovascular Angiography and Interventions, and
Society of Thoracic Surgeons. J Am Coll Cardiol 2012;60:e44-164.
6. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on
duration of dual antiplatelet therapy in patients with coronary artery disease: a report of
the American College of Cardiology/American Heart Association Task Force on
Clinical Practice Guidelines. J Am Coll Cardiol 2016;134:e123-55.
7. Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of rando-
mised trials of antiplatelet therapy for prevention of death, myocardial infarction,
and stroke in high risk patients. Br Med J 2002;324:71-86.
8. Antithrombotic Trialists’ Collabortaion. Aspirin in the primary and secondary
prevention of vascular disease: collaborative meta-analysis of individual partic-
ipant data from randomised trials. Lancet 2009;373:1849-60.
9. De Berardis G, Lucisano G, D’Ettorre A, et al. Association of aspirin use with
major bleeding in patients with and without diabetes. J Am Med Assoc 2012;307:
2286-94.
10. Garcia Rodriguez LA, Hernandez-Diaz S, de Abajo FJ. Association between aspirin
and upper gastrointestinal complications: systematic review of epidemiologic studies.
Br J Clin Pharmacol 2001;52:563-71.
11. Cayla G, Collet JP, Silvain J, Thiefin G, Woimant F, Montalescot G. Prevalence and
clinical impact of upper gastrointestinal symptoms in subjects treated with low dose
aspirin: the UGLA survey. Int J Cardiol 2012;156:69-75.
12. Moberg C, Naesdal J, Svedberg LE, Duchateau D, Harte N. Impact of gastrointestinal
problems on adherence to low-dose acetylsalicylic acid: a quantitative study in patients
with cardiovascular risk. Patient 2011;4:103-13.
13. Yeomans ND, Lanas AI, Talley NJ, et al. Prevalence and incidence of gastroduodenal
ulcers during treatment with vascular protective doses of aspirin. Aliment Pharmacol
Ther 2005;22:795-801.
14. Niv Y, Battler A, Abuksis G, Gal E, Sapoznikov B, Vilkin A. Endoscopy in
asymptomatic minidose aspirin consumers. Dig Dis Sci 2005;50:78-80.
15. Goldstein JL, Scheiman JM, Fort JG, Whellan DJ. Aspirin use in secondary
cardiovascular protection and the development of aspirin-associated erosions and
ulcers. J Cardiovasc Pharmacol 2016;68:121-6.
Curr Probl Cardiol, May 2017 159
16. Barkun A, Leontiadis G. Systematic review of the symptom burden, quality of life
impairment and costs associated with peptic ulcer disease. Am J Med 2010;123:
358-66.
17. Wilcox CM, Clark WS. Features associated with painless peptic ulcer bleeding. Am J
Gastroenterol 1997;92:1289-92.
18. Garcia Rodriguez LA, Martin-Perez M, Hennekens CH, Rothwell PM, Lanas A.
Bleeding risk with long-term low-dose aspirin: a systematic review of observational
studies. PLoS One 2016;11:e0160046.
19. Kelly JP, Kaufman DW, Jurgelon JM, Sheehan J, Koff RS, Shapiro S. Risk of aspirin-
associated major upper-gastrointestinal bleeding with enteric-coated or buffered
product. Lancet 1996;348:1413-6.
20. Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus
document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use:
a report of the American College of Cardiology Foundation Task Force on Clinical
Expert Consensus Documents. Circulation 2008;118:1894-909.
21. Scheiman JM, Hindley CE. Strategies to optimize treatment with NSAIDs in patients at
risk for gastrointestinal and cardiovascular adverse events. Clin Ther 2010;32:667-77.
22. Lanas A, Polo-Tomas M, Casado-Arroyo R. The aspirin cardiovascular/gastro-
intestinal risk calculator—a tool to aid clinicians in practice. Aliment Pharmacol Ther
2013;37:738-48.
23. Sostres C, Lanas A. Should prophylactic low-dose aspirin therapy be continued in
peptic ulcer bleeding? Drugs 2011;71:1-10.
24. Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic
ulcer bleeding: a randomized trial. Ann Intern Med 2010;152:1-9.
25. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal
antiinflammatory drugs. N Engl J Med 1999;340:1888-99.
26. Wallace JL. Prostaglandins, NSAIDs, and gastric mucosal protection: why doesn’t the
stomach digest itself? Physiol Rev 2008;88:1547-65.
27. Fanaroff AC, Roe MT. Contemporary reflections on the safety of long-term aspirin
treatment for the secondary prevention of cardiovascular disease. Drug Saf 2016;39:
715-27.
28. Lichtenberger LM, Zhou Y, Jayaraman V, et al. Insight into NSAID-induced
membrane alterations, pathogenesis and therapeutics: characterization of interaction
of NSAIDs with phosphatidylcholine. Biochim Biophys Acta 2012;1821:994-1002.
29. Lichtenberger LM, Richards JE, Hills BA. Effect of 16,16-dimethyl prostaglandin E2
on the surface hydrophobicity of aspirin-treated canine gastric mucosa. Gastro-
enterology 1985;88:308-14.
30. Hernandez-Diaz S, Garcia Rodriguez LA. Cardioprotective aspirin users and their
excess risk of upper gastrointestinal complications. BMC Med 2006;4:22.
31. Rosenstock S, Jorgensen T, Bonnevie O, Andersen L. Risk factors for peptic ulcer
disease: a population based prospective cohort study comprising 2416 Danish adults.
Gut 2003;52:186-93.
32. Ruigomez A, Johansson S, Nagy P, Martin-Perez M, Rodriguez LA. Risk of
uncomplicated peptic ulcer disease in a cohort of new users of low-dose acetylsalicylic
160 Curr Probl Cardiol, May 2017
acid for secondary prevention of cardiovascular events. BMC Gastroenterol 2014;14:
205.
33. Herlitz J, Toth PP, Naesdal J. Low-dose aspirin therapy for cardiovascular prevention:
quantification and consequences of poor compliance or discontinuation. Am J
Cardiovasc Drugs 2010;10:125-41.
34. Martin-Merino E, Johansson S, Bueno H, Garcia Rodrigues LA. Discontinuation of
low-dose acetylsalicylic acid therapy in UK primary care: incidence and predictors in
patients with cardiovascular disease. Pragmat Obs Res 2012;3:1-9.
35. Pratt S, Thompson VJ, Elkin EP, Naesdal J, Sorstadius E. The impact of upper
gastrointestinal symptoms on nonadherence to, and discontinuation of, low-dose
acetylsalicylic acid in patients with cardiovascular risk. Am J Cardiovasc Drugs
2010;10:281-8.
36. Biondi-Zoccai GGL, Lotrionte M, Agostoni P, et al. A systematic review and meta-
analysis on the hazards of discontinuing or not adhering to aspirin among 50,279
patients at risk for coronary artery disease. Eur Heart J 2006;27:2667-74.
37. Derogar M, Sandblom G, Lundell L, et al. Discontinuation of low-dose aspirin therapy
after peptic ulcer bleeding increases risk of death and acute cardiovascular events. Clin
Gastroenterol Hepatol 2013;11:38-42.
38. Hamood H, Hamood R, Green MS, Almog R. Effect of adherence to evidence-based
therapy after acute myocardial infarction on all-cause mortality. Pharmacoepidemiol
Drug Saf 2015;24:1093-104.
39. Vaduganathan M, Bhatt DL, Cryer BL, et al. Proton-pump inhibitors reduce gastro-
intestinal events regardless of aspirin dose in patients requiring dual antiplatelet
therapy. J Am Coll Cardiol 2016;67:1661-71.
40. Valkhoff VE, Sturkenboom MC, Hill C, Veldhuyzen van Zanten S, Kuipers EJ. Low-
dose acetylsalicylic acid use and the risk of upper gastrointestinal bleeding: a meta-
analysis of randomized clinical trials and observational studies. Can J Gastroenterol
2013;27:159-67.
41. Derry S, Loke YK. Risk of gastrointestinal haemorrhage with long term use of aspirin:
meta-analysis. Br Med J 2000;321:1183-7.
42. Johnston A, Jones WS, Hernandez AF. The ADAPTABLE trial and aspirin dosing in
secondary prevention for patients with coronary artery disease. Curr Cardiol Rep
2016;18:81.
43. Shin JM, Sachs G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep
2008;10:528-34.
44. Laursen SB, Jorgensen HS, Schaffalitzky de Muckadell OB. National consensus on
management of peptic ulcer bleeding in Denmark 2014. Dan Med J 2014;61:B4969.
45. Yeomans N, Lanas A, Labenz J, et al. Efficacy of esomeprazole (20 mg once daily) for
reducing the risk of gastroduodenal ulcers associated with continuous use of low-dose
aspirin. Am J Gastroenterol 2008;103:2465-73.
46. Sylvester KW, Cheng JW, Mehra MR. Esomeprazole and aspirin fixed combination
for the prevention of cardiovascular events. Vasc Health Risk Manag 2013;9:245-54.
47. Scheiman JM, Devereaux PJ, Herlitz J, et al. Prevention of peptic ulcers with
esomeprazole in patients at risk of ulcer development treated with low-dose
Curr Probl Cardiol, May 2017 161
acetylsalicylic acid: a randomised, controlled trial (OBERON). Heart 2011;97:
797-802.
48. Lin KJ, Hernandez-Diaz S, Garcia Rodriguez LA. Acid suppressants reduce risk of
gastrointestinal bleeding in patients on antithrombotic or anti-inflammatory therapy.
Gastroenterology 2011;141:71-9.
49. Saini SD, Fendrick AM, Scheiman JM. Cost-effectiveness analysis: cardiovascular
benefits of proton pump inhibitor co-therapy in patients using aspirin for secondary
prevention. Aliment Pharmacol Ther 2011;34:243-51.
50. Lanas A, Wu P, Medin J, Mills EJ. Low doses of acetylsalicylic acid increase risk of
gastrointestinal bleeding in a meta-analysis. Clin Gastroenterol Hepatol 2011;9:762-8.
51. Garnett WR. History of acid suppression: focus on the hospital setting. Pharmaco-
therapy 2003;23:56S-60S.
52. McRorie JW, Kirby JA, Miner PB. Histamine2-receptor antagonists: rapid develop-
ment of tachyphylaxis with repeat dosing. World J Gastrointest Pharmacol Ther
2014;5:57-62.
53. Merki HS, Wilder-Smith CH. Do continuous infusions of omeprazole and ranitidine
retain their effect with prolonged dosing? Gastroenterology 1994;106:60-4.
54. Chan FK, Kyaw M, Tanigawa T, et al. Similar efficacy of proton-pump inhibitors vs
H2-receptor antagonists in reducing risk of upper gastrointestinal bleeding or ulcers in
high-risk users of low-dose aspirin. Gastroenterology 2017;152:105-10.
55. Lanas A, Garcia-Rodriguez LA, Arroyo MT, et al. Effect of antisecretory drugs and
nitrates on the risk of ulcer bleeding associated with nonsteroidal anti-inflammatory
drugs, antiplatelet agents, and anticoagulants. Am J Gastroenterol 2007;102:507-15.
56. Mo C, Sun G, Lu ML, et al. Proton pump inhibitors in prevention of low-dose
aspirin-associated upper gastrointestinal injuries. World J Gastroenterol 2015;21:
5382-92.
57. Guo M, Wang J, Zou YC, Weng Y. The clinical effect of esomeprazole in prevention
of low dose aspirin induced gastric mucosal injury. Chin J Dig 2012;29:
481-2. [article in Chinese].
58. Hu L, Zhou T, Xia YH. The effect of rabeprazole in prevention of low dose aspirin
induced gastric injury. MMJC 2012;14:100-1. [article in Chinese].
59. Ng FH, Wong SY, Lam KF, et al. Famotidine is inferior to pantoprazole in preventing
recurrence of aspirin-related peptic ulcers or erosions. Gastroenterology 2010;138:82-8.
60. Ng FH, Tunggal P, Chu WM, et al. Esomeprazole compared with famotidine in the
prevention of upper gastrointestinal bleeding in patients with acute coronary syndrome
or myocardial infarction. Am J Gastroenterol 2012;107:389-96.
61. Sun RR, He YQ, Li R. The effect of rabeprazole in prevention of low-dose aspirin
induced gastric mucosal injury in 40 elder patients. Chin J Mod Drug 2012;6:
79-80. [article in Chinese].
62. Wang J, Zhou G-K, Guo M. The efficacy in prevention of upper gastrointestinal injury
in patients of acute cornary syndrome with esomeprazole, famotidine and hydrotalcite.
Chin J Cardiovasc Res 2012;10:191-5. [article in Chinese].
63. Wang YP, Wang RJ. The clinical effect of lansoprazole in prevention of low dose aspirin
induced gastric mucosal injury. Strait Pharm J 2016;24:114-5. [article in Chinese].
162 Curr Probl Cardiol, May 2017
64. Gesheff MG, Franzese CJ, Bliden KP, et al. Review of pharmacokinetic and
pharmacodynamic modeling and safety of proton pump inhibitors and aspirin. Expert
Rev Clin Pharmacol 2014;7:645-53.
65. Martin Merino E, Johansson S, Nagy P, Garcia Rodriguez LA. Effect of baseline
gastrointestinal risk and use of proton pump inhibitors on frequency of discontinuation
of aspirin for secondary cardiovascular prevention in United Kingdom primary care.
Am J Cardiol 2013;112:1075-82.
66. Whellan DJ, Goldstein JL, Cryer BL, et al. PA32540 (a coordinated-delivery tablet of
enteric-coated aspirin 325 mg and immediate-release omeprazole 40 mg) versus
enteric-coated aspirin 325 mg alone in subjects at risk for aspirin-associated gastric
ulcers: results of two 6-month, phase 3 studies. Am Heart J 2014;168:495-502.
67. de Jong HJ, Korevaar JC, van Dijk L, Voogd E, van Dijk CE, van Oijen MG. Suboptimal
prescribing of proton-pump inhibitors in low-dose aspirin users: a cohort study in primary
care. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003044.
68. Zhu LL, Xu LC, Chen Y, Zhou Q, Zeng S. Poor awareness of preventing aspirin-
induced gastrointestinal injury with combined protective medications. World J
Gastroenterol 2012;18:3167-72.
69. Superceanu B, Veldhuyzen van Zanten S, Skedgel C, Shepherd M, Sketris I. The rate
of prescribing gastrointestinal prophylaxis with either a proton pump inhibitor or an
H2-receptor antagonist in Nova Scotia seniors starting nonsteroidal anti-inflammatory
drug therapy. Can J Gastroenterol 2010;24:481-8.
70. Hedberg J, Sundstrom J, Thuresson M, Aarskog P, Oldgren J, Bodegard J. Low-dose
acetylsalicylic acid and gastrointestinal ulcers or bleeding—a cohort study of the
effects of proton pump inhibitor use patterns. J Intern Med 2013;274:371-80.
71. Abramowitz J, Thakkar P, Isa A, Truong A, Park C, Rosenfeld RM. Adverse event
reporting for proton pump inhibitor therapy: an overview of systematic reviews.
Otolaryngol Head Neck Surg 2016;155:547-54.
72. Gomm W, von HK, Thome F, et al. Association of proton pump inhibitors with risk of
dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol 2016;73:410-6.
73. Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic
kidney disease. JAMA Intern Med 2016;176:238-46.
74. Vaezi MF, Yang Y-X, Howden CW. Complications of proton pump inhibitor therapy.
Gastroenterology 2017, in press.
75. Wurtz M, Grove EL, Kristensen SD, Hvas AM. The antiplatelet effect of aspirin is
reduced by proton pump inhibitors in patients with coronary artery disease. Heart
2010;96:368-71.
76. Charlot M, Grove EL, Hansen PR, et al. Proton pump inhibitor use and risk of adverse
cardiovascular events in aspirin treated patients with first time myocardial infarction:
nationwide propensity score matched study. Br Med J 2011;342:d2690.
77. Agewall S, Cattaneo M, Collet JP, et al. Expert position paper on the use of proton
pump inhibitors in patients with cardiovascular disease and antithrombotic therapy.
Eur Heart J 2013;34:1708-13b.
78. Scheiman JM. NSAIDs, gastrointestinal injury, and cytoprotection. Gastroenterol Clin
North Am 1996;25:279-98.
Curr Probl Cardiol, May 2017 163
Antiplatelet therapy is a very important component of the management of
patients who are at risk of secondary vascular disease. Low dose aspirin is the
most utilized antiplatelet therapy and it is the most effective. However, it has
been associated with risk of gastrointestinal toxicity, leading patients to
discontinue therapy and increasing their cardiovascular risk. In patients with
high risk of gastrointestinal events with aspirin, the use of proton pump
inhibitors is presently recommended.
In this issue of Current Problems in Cardiology, Lavie CJ et al review different
aspects of aspirin and gastrointestinal toxicity as well the utilization of a
coordinated delivery of aspirin and an immediate-release proton pump
inhibitor in a combination tablet.
Several clinical perspectives can be taken from this interesting review.
First, aspirin is the most common antiplatelet therapy utilized in the majority of
patients at higher risk of cardiovascular disease.
Second, the risk of gastrointestinal adverse events associated with aspirin
causes decrease in adherence to therapy. Concomitant administration of
proton pump inhibitors reduces the incidence of gastrointestinal symptoms
and improves adherence with aspirin.
Third, the main mechanism for aspirin toxic effects on the mucosa of the
gastrointestinal tract is systemic, through inhibition of cyclooxygenase and
the consequent decrease in the synthesis of prostaglandins.
Finally, the authors discuss the novel utilization of aspirin and a proton pump
inhibitor as a coordinated-delivery combination that reduces the risk of
gastric ulcer formation and improves compliance in a clinical study. Further-
more, this strategy may be beneficial to reduce cardiovascular risk and may
warrant further studies in both randomized controlled and pragmatic trials.
I want to thank the authors for a very interesting review of the novel
coordinated-delivery combination of aspirin and proton pump inhibitor and I
hope the authors will have more clinical information in the near future.
164 Curr Probl Cardiol, May 2017
You might also like
- Chemistry Investigatory Project Class 12 - Preparation of Aspirin From Acetyl Chloride.Document20 pagesChemistry Investigatory Project Class 12 - Preparation of Aspirin From Acetyl Chloride.Jenil M. Shah76% (37)
- Albumin Drug StudyDocument1 pageAlbumin Drug StudyMaine Concepcion100% (1)
- 1 s2.0 S0735109716003995 MainDocument2 pages1 s2.0 S0735109716003995 MaintopanNo ratings yet
- Aspirin Resistance: Is It Real and Does It Matter?: DR - Wai-Hong ChenDocument3 pagesAspirin Resistance: Is It Real and Does It Matter?: DR - Wai-Hong ChenPepo AryabarjaNo ratings yet
- Low Dose Aspirin and Mucoprotective Effects of Omeprazole and RanitidineDocument4 pagesLow Dose Aspirin and Mucoprotective Effects of Omeprazole and RanitidineIman HendriantoNo ratings yet
- s40256 023 00582 9Document12 pagess40256 023 00582 9laac5757No ratings yet
- AnatolJCardiol 7 2 27 30Document4 pagesAnatolJCardiol 7 2 27 30Chirac OanaNo ratings yet
- Aspirin To Prevent Future CVDDocument10 pagesAspirin To Prevent Future CVDAngelo DestaNo ratings yet
- 1.STRUKTUR KRISTAL (Kuliah)Document14 pages1.STRUKTUR KRISTAL (Kuliah)RatnaWulannNo ratings yet
- Aspirin Resistance or Treatment Non ComplianceDocument4 pagesAspirin Resistance or Treatment Non Compliancepinoi sufiNo ratings yet
- Combining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADocument7 pagesCombining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADrHellenNo ratings yet
- Aspirina en DiabeticosDocument5 pagesAspirina en DiabeticosgorinakNo ratings yet
- Aspirin Resistance2009Document10 pagesAspirin Resistance2009Stacey WoodsNo ratings yet
- 2007 Editorial NASPEAFDocument3 pages2007 Editorial NASPEAFpsoluopostimNo ratings yet
- Aspirin Resistance in Cardiovascular Disease A ReviewDocument10 pagesAspirin Resistance in Cardiovascular Disease A ReviewVioleta GrigorasNo ratings yet
- Jurnal AspirinDocument2 pagesJurnal AspirinNia SylvieniaNo ratings yet
- Aspirina Riesgos y Beneficios - Clev Clin J Med 2013Document9 pagesAspirina Riesgos y Beneficios - Clev Clin J Med 2013Ari JimenezNo ratings yet
- Aspirin For Primary Prevention of Cardiovascular Disease in The 21 Century: A Review of The EvidenceDocument8 pagesAspirin For Primary Prevention of Cardiovascular Disease in The 21 Century: A Review of The EvidenceForestier HsuNo ratings yet
- Aspirin Pregnancy WarningsDocument12 pagesAspirin Pregnancy Warnings'Prasada WedatamaNo ratings yet
- Acute Ischemic Stroke DrugsDocument45 pagesAcute Ischemic Stroke DrugsDamar TriutomoNo ratings yet
- 1 s2.0 S0735109716003983 MainDocument11 pages1 s2.0 S0735109716003983 MaintopanNo ratings yet
- Aspirin Benefits Vs RiskDocument9 pagesAspirin Benefits Vs RiskIsaac Aaron Enriquez MonsalvoNo ratings yet
- Articulo Aspirina en Prevencion Primaria - Aun Justificada Darla en Era de Estatinas (EDITORIAL) NEJMDocument3 pagesArticulo Aspirina en Prevencion Primaria - Aun Justificada Darla en Era de Estatinas (EDITORIAL) NEJMCarmen GonzálezNo ratings yet
- Update On Anti Platelet TherapyDocument4 pagesUpdate On Anti Platelet TherapyhadilkNo ratings yet
- Aspirin Kod KVBDocument7 pagesAspirin Kod KVBLukaNo ratings yet
- Aspirin, Clopidogrel, and Ticagrelor in Acute Coronary SyndromesDocument9 pagesAspirin, Clopidogrel, and Ticagrelor in Acute Coronary SyndromesJicko Street HooligansNo ratings yet
- Antiplatelet and Antithrombotic Therapy (Triple Therapy) Risk and Benefits (Am J Med 2014)Document7 pagesAntiplatelet and Antithrombotic Therapy (Triple Therapy) Risk and Benefits (Am J Med 2014)Eduardo MenaNo ratings yet
- Aspirin, Cyclooxygenase Inhibition and Colorectal Cancer: Carlos Sostres, Carla Jerusalen Gargallo, Angel LanasDocument11 pagesAspirin, Cyclooxygenase Inhibition and Colorectal Cancer: Carlos Sostres, Carla Jerusalen Gargallo, Angel LanasJNHRNo ratings yet
- 3ยา ต้องให้PPIDocument7 pages3ยา ต้องให้PPIChayagon MongkonsawatNo ratings yet
- 7265-Article Text-26197-1-10-20110314 PDFDocument4 pages7265-Article Text-26197-1-10-20110314 PDFzzzzNo ratings yet
- Bahan Bleeding 1Document6 pagesBahan Bleeding 1jalaludinsyahNo ratings yet
- Aspirin in The Primary Prevention of Cardiovascular Disease and CancerDocument16 pagesAspirin in The Primary Prevention of Cardiovascular Disease and CancerCARLOSNo ratings yet
- CPG3 Secondary Stroke PreventionDocument10 pagesCPG3 Secondary Stroke Preventionmochamad rizaNo ratings yet
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Document11 pagesEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazNo ratings yet
- Pharmaceuticals: Critical Overview On The Benefits and Harms of AspirinDocument16 pagesPharmaceuticals: Critical Overview On The Benefits and Harms of AspirinromyNo ratings yet
- Journal Reading Aspirin Resistance in Patients With Acute Ischemic StrokeDocument3 pagesJournal Reading Aspirin Resistance in Patients With Acute Ischemic StrokeBrigita De VegaNo ratings yet
- Managing Hypertension Using Combination Therapy - AAFPDocument18 pagesManaging Hypertension Using Combination Therapy - AAFPtorome4979No ratings yet
- Acute Coronary Syndrome Oral Anticoagulation in Medically Treated Patients - UpToDateDocument14 pagesAcute Coronary Syndrome Oral Anticoagulation in Medically Treated Patients - UpToDateBrian VianaNo ratings yet
- Avoiding The "Triple Whammy" in Primary Care:: ACE inhibitor/ARB + Diuretic + NSAIDDocument5 pagesAvoiding The "Triple Whammy" in Primary Care:: ACE inhibitor/ARB + Diuretic + NSAIDSintaNo ratings yet
- Information On Aspirin FormulationsDocument2 pagesInformation On Aspirin FormulationskookyinNo ratings yet
- J Ahj 2006 06 024Document7 pagesJ Ahj 2006 06 024Alexandra RosaNo ratings yet
- Antihypertensives in HDDocument6 pagesAntihypertensives in HDamanyNo ratings yet
- Aspirin PpiDocument10 pagesAspirin PpihermanfirdausNo ratings yet
- Australian PrescriberDocument3 pagesAustralian PrescriberMohamed OmerNo ratings yet
- Xtaiwan CancerDocument12 pagesXtaiwan CancerForestier HsuNo ratings yet
- Olsen 2005Document6 pagesOlsen 2005Amalia NandiaNo ratings yet
- Delaying or Halting Progression of Chronic Kidney DiseaseDocument9 pagesDelaying or Halting Progression of Chronic Kidney Diseasehannya manNo ratings yet
- ASCEND: Aspirin Doesn't Look Good For Primary CV Prevention in Diabetic PatientsDocument7 pagesASCEND: Aspirin Doesn't Look Good For Primary CV Prevention in Diabetic PatientsFernanda MenesesNo ratings yet
- Aspirin: Its Risks, Benefits, and Optimal Use in Preventing Cardiovascular EventsDocument9 pagesAspirin: Its Risks, Benefits, and Optimal Use in Preventing Cardiovascular EventsIrma Hanny Tri HartonoNo ratings yet
- MEFTAL P Suspension PIDocument10 pagesMEFTAL P Suspension PIpiyush patelNo ratings yet
- AspirinDocument7 pagesAspirinsamaneh shirkouhiNo ratings yet
- Association of Aspirin Use For Primary Prevention With Cardiovascular Events and Bleeding Eventsa Systematic Review and Meta-AnalysisDocument3 pagesAssociation of Aspirin Use For Primary Prevention With Cardiovascular Events and Bleeding Eventsa Systematic Review and Meta-AnalysismirzeroNo ratings yet
- Review of Medical Treatment of Stable Ischemic Heart DiseaseDocument11 pagesReview of Medical Treatment of Stable Ischemic Heart DiseaseSuci NourmalizaNo ratings yet
- ArticleDocument10 pagesArticleWahyu WijayantoNo ratings yet
- Stopp Start ToolkitDocument22 pagesStopp Start ToolkitRifky IlhamiNo ratings yet
- High-Dose Clopidogrel, Prasugrel or Ticagrelor: Trying To Unravel A Skein Into A Ball. Alessandro Aprile, Raffaella Marzullo, Giuseppe Biondi Zoccai, Maria Grazia ModenaDocument8 pagesHigh-Dose Clopidogrel, Prasugrel or Ticagrelor: Trying To Unravel A Skein Into A Ball. Alessandro Aprile, Raffaella Marzullo, Giuseppe Biondi Zoccai, Maria Grazia ModenaDrugs & Therapy StudiesNo ratings yet
- GI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyDocument11 pagesGI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyTony LeeNo ratings yet
- Concomitant Diabetes With Atrial Fibrillation andDocument9 pagesConcomitant Diabetes With Atrial Fibrillation and25515okeNo ratings yet
- Rapid Desensitization Protocols For Patients With Cardiovascular Disease and Aspirin Hypersensitivity in An Era of Dual Antiplatelet TherapyDocument7 pagesRapid Desensitization Protocols For Patients With Cardiovascular Disease and Aspirin Hypersensitivity in An Era of Dual Antiplatelet TherapyIfah 123No ratings yet
- Abraham 2015Document14 pagesAbraham 2015Luis Rafael Suárez U.No ratings yet
- Aspilets ECDocument5 pagesAspilets ECJerry SerapionNo ratings yet
- Acute Gastrointestinal Bleeding: Diagnosis and TreatmentFrom EverandAcute Gastrointestinal Bleeding: Diagnosis and TreatmentKaren E. KimNo ratings yet
- Dasha Lavana Dravakam PDFDocument9 pagesDasha Lavana Dravakam PDFDgbabu BabuNo ratings yet
- Filter Bag EnglishDocument32 pagesFilter Bag EnglishArun Gupta100% (1)
- ALIVE+Case+Study Cipla+Ascend+S1Document4 pagesALIVE+Case+Study Cipla+Ascend+S1Tanya SainiNo ratings yet
- DepressionDocument10 pagesDepressionsalfaciNo ratings yet
- Microencapsulation by Solvent Evaporation State of The Art For ProcessDocument15 pagesMicroencapsulation by Solvent Evaporation State of The Art For ProcessKaren SánchezNo ratings yet
- Precipitation TitrationDocument18 pagesPrecipitation TitrationRahul MalikNo ratings yet
- English For PharmacyDocument37 pagesEnglish For PharmacyBogdan Gavrilescu100% (2)
- Development and Validation of HPLC Method For Simultaneous Quantitation of Paracetamol and Dexketoprofen Trometamol in Bulk Drug and FormulationDocument4 pagesDevelopment and Validation of HPLC Method For Simultaneous Quantitation of Paracetamol and Dexketoprofen Trometamol in Bulk Drug and FormulationPaulo DantasNo ratings yet
- Pick-Up Station Request FormDocument2 pagesPick-Up Station Request FormJames LindonNo ratings yet
- Valid Sterisart-NF SLD5704-eDocument67 pagesValid Sterisart-NF SLD5704-esizhusyNo ratings yet
- Treatment of Clinical Mastitis: Jerry R. RobersonDocument18 pagesTreatment of Clinical Mastitis: Jerry R. Robersonika kurniawatiNo ratings yet
- Healthcare AnalyticsDocument9 pagesHealthcare AnalyticsRamyaNo ratings yet
- Veterinary Pharmacy, A Dismissed Necessity PDFDocument3 pagesVeterinary Pharmacy, A Dismissed Necessity PDFKelma TayebaNo ratings yet
- Update Pasang Flash Sale Minggu Iii SD Iv Januari 2022Document9 pagesUpdate Pasang Flash Sale Minggu Iii SD Iv Januari 2022riskaNo ratings yet
- AgomelatineDocument6 pagesAgomelatineI.m. DanielNo ratings yet
- Surface Tension Impact On Pharma ProductsDocument4 pagesSurface Tension Impact On Pharma ProductsOmar Alta'amerehNo ratings yet
- Biotechnology Analytical Development Director in CT Resume Shirish DhumeDocument5 pagesBiotechnology Analytical Development Director in CT Resume Shirish DhumeSharishDhumeNo ratings yet
- Enc 1102 Research ProposalDocument4 pagesEnc 1102 Research Proposalapi-317153884No ratings yet
- Solubility Enhancement of Poorly Water Soluble Drug by Using NanosuspensiontechnologyDocument8 pagesSolubility Enhancement of Poorly Water Soluble Drug by Using Nanosuspensiontechnologydini hanifaNo ratings yet
- MWC ModelDocument2 pagesMWC Modelrajwill1No ratings yet
- List of Centre Taxpayers SikkimDocument11 pagesList of Centre Taxpayers Sikkimudiptya_papai2007No ratings yet
- Reactii AdverseDocument8 pagesReactii AdverseEmanuela MerticariuNo ratings yet
- R&D ListDocument50 pagesR&D ListYashoda RaiNo ratings yet
- Prescribing Psychotropics: Perspective From Telepsychiatry Operational Guidelines 2020Document5 pagesPrescribing Psychotropics: Perspective From Telepsychiatry Operational Guidelines 2020ika nurul shofiyahNo ratings yet
- Assays For Controlling Host-Cell Impurities in BiopharmaceuticalsDocument5 pagesAssays For Controlling Host-Cell Impurities in BiopharmaceuticalsBabbooNo ratings yet
- AllDocument188 pagesAllpilotof1No ratings yet
- Far Eastern University Dr. Nicanor Reyes Medical Foundation: Reportable Events (Staff Nurse/Nursing Aide)Document3 pagesFar Eastern University Dr. Nicanor Reyes Medical Foundation: Reportable Events (Staff Nurse/Nursing Aide)Jupiter WhitesideNo ratings yet
- Product Knowledge (2) (26-8) 2-1Document38 pagesProduct Knowledge (2) (26-8) 2-1zeyad1234ali0No ratings yet