Professional Documents
Culture Documents
Women Heath
Women Heath
Uploaded by
Angelic khanCopyright:
Available Formats
You might also like
- Acog Practice Bulletin: Antepartum Fetal SurveillanceDocument12 pagesAcog Practice Bulletin: Antepartum Fetal SurveillanceMariana Hernandez100% (10)
- Case Simulation 118Document4 pagesCase Simulation 118Rica AvendañoNo ratings yet
- Electronic Fetal MonitoringDocument4 pagesElectronic Fetal MonitoringMauZungNo ratings yet
- Electrotherapy Evidence Based PracticeDocument401 pagesElectrotherapy Evidence Based PracticeAngelic khan50% (4)
- Handbook of Practical ElectrotherapyDocument164 pagesHandbook of Practical ElectrotherapyAngelic khan100% (2)
- Antepartum Fetal Well Being AssessmentDocument14 pagesAntepartum Fetal Well Being AssessmentIsrael WoseneNo ratings yet
- Left Tilt Manuever to Minimize HypotensionDocument5 pagesLeft Tilt Manuever to Minimize HypotensionAbdul Haseeb KhattakNo ratings yet
- ingemarsson1985Document7 pagesingemarsson1985Asela SubhasingheNo ratings yet
- Massagem Perineal em Trabalho de Parto e Prevenção de Trauma Perineal Ensaio Clínico RandomizadoDocument4 pagesMassagem Perineal em Trabalho de Parto e Prevenção de Trauma Perineal Ensaio Clínico RandomizadoSheila SilvaNo ratings yet
- Profil Biofisik High RiskDocument5 pagesProfil Biofisik High RiskbebekbebekNo ratings yet
- 0091-2182 2885 2990126-0 PDFDocument1 page0091-2182 2885 2990126-0 PDFParahmitaNo ratings yet
- Satoshi Dohi, Kiyotake Ichizuka, Ryu Matsuoka, Kohei Seo, Masaaki Nagatsuka, Akihiko SekizawaDocument6 pagesSatoshi Dohi, Kiyotake Ichizuka, Ryu Matsuoka, Kohei Seo, Masaaki Nagatsuka, Akihiko SekizawasandiNo ratings yet
- Ajacm 2009 4 (1) Acup Improve EndometrDocument7 pagesAjacm 2009 4 (1) Acup Improve EndometrdirkvandeweyerNo ratings yet
- Prospective Evaluation of Individual Cardiotocography Parameters in Predicting A Nonasphyxiated FetusDocument4 pagesProspective Evaluation of Individual Cardiotocography Parameters in Predicting A Nonasphyxiated FetusSanjay GoleNo ratings yet
- Partus LamaDocument4 pagesPartus LamaIntan PermataNo ratings yet
- Obestritic Anesthesia DNB Q & ADocument162 pagesObestritic Anesthesia DNB Q & Ahiwotbetesfa2123No ratings yet
- Does Exercise Training During Pregnancy Affect Gestational Age? A Randomised Controlled TrialDocument6 pagesDoes Exercise Training During Pregnancy Affect Gestational Age? A Randomised Controlled TrialTrnidad Moder GarvizoNo ratings yet
- Antepartum Fetal Surveillance ACOG Bulletin 2014 PDFDocument11 pagesAntepartum Fetal Surveillance ACOG Bulletin 2014 PDFDanNo ratings yet
- Archdischild 2023 326099.fullDocument5 pagesArchdischild 2023 326099.fullAlina1102No ratings yet
- Procedures ObgDocument12 pagesProcedures Obgraghuram reddyNo ratings yet
- The Effect of Hyoscine Butylbromide On The First Stage of Labour in Term PregnanciesDocument5 pagesThe Effect of Hyoscine Butylbromide On The First Stage of Labour in Term PregnanciesnephylymNo ratings yet
- NST CSTDocument9 pagesNST CSTNadiya RashidNo ratings yet
- Roy 2008Document4 pagesRoy 2008yenni anggrainiNo ratings yet
- Delayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleDocument11 pagesDelayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleManju KumariNo ratings yet
- p425Document4 pagesp425Adnan KhanNo ratings yet
- Chu 2018Document8 pagesChu 2018Nicholas PratamaNo ratings yet
- Co 713Document5 pagesCo 713larasNo ratings yet
- Preoperative Stabilisation in Congenital Diaphragmatic HerniaDocument3 pagesPreoperative Stabilisation in Congenital Diaphragmatic HerniaAgus PrimaNo ratings yet
- 2003-1050 KaminskiDocument10 pages2003-1050 KaminskichrisgochiroNo ratings yet
- 1298 4803 1 PBDocument6 pages1298 4803 1 PBshashikiran7920No ratings yet
- Fetal Well BeingDocument5 pagesFetal Well BeingCARL JOHN MANALONo ratings yet
- Delayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleDocument11 pagesDelayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleFatma ElzaytNo ratings yet
- Graphy) The Fetal Heartbeat (Cardio-) and The Uterine Contractions (-Toco-) DuringpregnancyDocument6 pagesGraphy) The Fetal Heartbeat (Cardio-) and The Uterine Contractions (-Toco-) DuringpregnancyHanna GustinNo ratings yet
- Benson Multicentre 1986Document4 pagesBenson Multicentre 1986Dian NovitasariNo ratings yet
- Jurnal Inter EDEMA 2Document4 pagesJurnal Inter EDEMA 2Edom LazarNo ratings yet
- 125 - Fetal Biophysical ProfileDocument5 pages125 - Fetal Biophysical ProfileYuly Andrea Marquez CastañedaNo ratings yet
- Medical Case Write UpDocument11 pagesMedical Case Write UpJang Abd MutalibNo ratings yet
- Reporte Especial Resicitacion NeonatalDocument17 pagesReporte Especial Resicitacion NeonatalAna León VigilNo ratings yet
- Students' Corner Protocols For Exercise During Pregnancy: AcknowledgementDocument4 pagesStudents' Corner Protocols For Exercise During Pregnancy: AcknowledgementMaria Quiza GeñosoNo ratings yet
- Effect of Single Low Dose Intrathecal Labor Analgesia On Maternal and Fetal OutcomeDocument6 pagesEffect of Single Low Dose Intrathecal Labor Analgesia On Maternal and Fetal OutcomeAnnaNo ratings yet
- Altered Uteroplacental Tissue PerfusionDocument5 pagesAltered Uteroplacental Tissue PerfusionArielle BajalaNo ratings yet
- Angle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundDocument5 pagesAngle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundNella SolanoNo ratings yet
- Timingyavas 2004Document10 pagesTimingyavas 2004Ramadhan AkmalNo ratings yet
- Referensi Nomor 6Document9 pagesReferensi Nomor 6audreynatalia777No ratings yet
- Supported By: None.: AbstractsDocument1 pageSupported By: None.: AbstractsFerry DimyatiNo ratings yet
- Uterine Blood Flow During Supine Rest and Exercise After 28 Weeks of GestationDocument9 pagesUterine Blood Flow During Supine Rest and Exercise After 28 Weeks of GestationMD Luthfy LubisNo ratings yet
- Objective Definition of Shoulder Dystocia: A Prospective EvaluationDocument4 pagesObjective Definition of Shoulder Dystocia: A Prospective Evaluationbahtiar bleachNo ratings yet
- Urban 2005Document5 pagesUrban 2005Miyyada AichaouiNo ratings yet
- AHA Guidelines On Neonatal ResuscitationDocument17 pagesAHA Guidelines On Neonatal ResuscitationVillia Damayantie100% (1)
- Effects of SP6 Acupuncture Point Stimulation On Labor Pain and Duration of LaborDocument8 pagesEffects of SP6 Acupuncture Point Stimulation On Labor Pain and Duration of LaborRismaAyuSaraswatiNo ratings yet
- +second Stage of Labor and Epidural Use A Larger.8Document9 pages+second Stage of Labor and Epidural Use A Larger.8Valentina AnastasNo ratings yet
- Does Regular Exercise in Pregnancy Influence Duration of Labor? A Secondary Analysis of A Randomized Controlled TrialDocument7 pagesDoes Regular Exercise in Pregnancy Influence Duration of Labor? A Secondary Analysis of A Randomized Controlled Trialana pintoNo ratings yet
- Ashrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarDocument4 pagesAshrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarWilliam AdiputraNo ratings yet
- Nursing Care Plan Cues Diagnosis Planning Implementation Rationale EvaluationDocument4 pagesNursing Care Plan Cues Diagnosis Planning Implementation Rationale EvaluationChrizley Shawn DeroniaNo ratings yet
- Do Zavanelli ModifDocument3 pagesDo Zavanelli ModifSAKAI69No ratings yet
- Persistence of Fetal Memory Into Neonatal LifeDocument5 pagesPersistence of Fetal Memory Into Neonatal LifeRodrigo LeãoNo ratings yet
- Friedman EA (2000) : Labor: Clinical Evaluation and Management, P 23, 2nd Ed. New York, Appleton-Century-CroftsDocument5 pagesFriedman EA (2000) : Labor: Clinical Evaluation and Management, P 23, 2nd Ed. New York, Appleton-Century-CroftsJuliane ItliongNo ratings yet
- Vagal Activity, Gastric Motility Masaje InfantilDocument6 pagesVagal Activity, Gastric Motility Masaje InfantilIsis SanzNo ratings yet
- NRP - Ima-IsaDocument55 pagesNRP - Ima-IsaPeter RamNo ratings yet
- BJVR - Volume 6 - Issue 2 - Pages 37-41Document5 pagesBJVR - Volume 6 - Issue 2 - Pages 37-41avijaymba808No ratings yet
- Suppression of Puerperal Lactation Using Jasmine Flowers (Jasminum Sambac)Document4 pagesSuppression of Puerperal Lactation Using Jasmine Flowers (Jasminum Sambac)Iara PachêcoNo ratings yet
- 1 s2.0 S1836955323001212 MainDocument8 pages1 s2.0 S1836955323001212 Mainfilipa reisNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Osteoporosis: Hani Abu DiehDocument24 pagesOsteoporosis: Hani Abu DiehAngelic khan100% (1)
- Prepared By: Ulfat Amin MSC Pediatric NursingDocument25 pagesPrepared By: Ulfat Amin MSC Pediatric NursingAngelic khanNo ratings yet
- Microbiology BcqsDocument16 pagesMicrobiology BcqsAngelic khanNo ratings yet
- Osteoarthritis 1583-170210113823Document34 pagesOsteoarthritis 1583-170210113823Angelic khanNo ratings yet
- Elbow Joint: Dr. Sharjeel Tasneem BSPT, (KU) MSPT, (KU) ADPT, (Ziauddin University)Document26 pagesElbow Joint: Dr. Sharjeel Tasneem BSPT, (KU) MSPT, (KU) ADPT, (Ziauddin University)Angelic khanNo ratings yet
- Arthritis: by DR Samra Tahseen Registrar, Radiology LNHDocument86 pagesArthritis: by DR Samra Tahseen Registrar, Radiology LNHAngelic khanNo ratings yet
- Pathology of The Respiratory SystemDocument57 pagesPathology of The Respiratory SystemAngelic khanNo ratings yet
- Et-Lec 14 Wax TherapyDocument64 pagesEt-Lec 14 Wax TherapyAngelic khanNo ratings yet
- Introduction To Medical SpirochaetalesDocument25 pagesIntroduction To Medical SpirochaetalesAngelic khanNo ratings yet
- Microbiology Medical MicrobiologyDocument40 pagesMicrobiology Medical MicrobiologyAngelic khanNo ratings yet
- Drugs Used in Current Physical Therapy PracticeDocument22 pagesDrugs Used in Current Physical Therapy PracticeAngelic khan100% (1)
- Drug Side EffectsDocument2 pagesDrug Side EffectsAngelic khanNo ratings yet
- Gene Therapy CartilageDocument15 pagesGene Therapy CartilageAngelic khanNo ratings yet
- Three Basic Types of Muscle ContractionsDocument2 pagesThree Basic Types of Muscle ContractionsAngelic khanNo ratings yet
- Presented by Yasha Ali Bangash & Pashmina Khan DPT Batch Ii Semester VDocument20 pagesPresented by Yasha Ali Bangash & Pashmina Khan DPT Batch Ii Semester VAngelic khanNo ratings yet
- Pharmacology of Central Nervous SystemDocument20 pagesPharmacology of Central Nervous SystemAngelic khan100% (1)
- Pharmacology of Central Nervous System Antipsychotic and Parkinson DiseaseDocument22 pagesPharmacology of Central Nervous System Antipsychotic and Parkinson DiseaseAngelic khanNo ratings yet
- GENE THERAPY For Musculoskeletal DisordersDocument20 pagesGENE THERAPY For Musculoskeletal DisordersAngelic khanNo ratings yet
- Therapeutic Exercise Foundation ConceptsDocument13 pagesTherapeutic Exercise Foundation ConceptsAngelic khanNo ratings yet
- ფიზიოლოგიური მშობიარობის მართვაDocument30 pagesფიზიოლოგიური მშობიარობის მართვაAchi BeridzeNo ratings yet
- Antenatal Fetal MonitoringDocument51 pagesAntenatal Fetal MonitoringCodillia Cheong100% (2)
- Fetal Monitoring Technology: Application NoteDocument8 pagesFetal Monitoring Technology: Application NoteCarlos MedikalNo ratings yet
- Figo Consensus Guidelines On Intrapartum Fetal Monitoring: Intermittent AuscultationDocument7 pagesFigo Consensus Guidelines On Intrapartum Fetal Monitoring: Intermittent AuscultationWilliam WongNo ratings yet
- Fetal Assessment and Wellbeing in Pregnancy (FetalDocument23 pagesFetal Assessment and Wellbeing in Pregnancy (Fetalapi-3705046100% (1)
- Labor DystociaDocument100 pagesLabor DystociaAnonymous kChMIy7tXNo ratings yet
- 344 PreprintDocument4 pages344 PreprintDii ScottouNo ratings yet
- IUFD AnitaDocument65 pagesIUFD AnitaarifuadNo ratings yet
- Antenatal Assssment Final @@Document46 pagesAntenatal Assssment Final @@Pragati BholeNo ratings yet
- Soal Bahasa Inggris Kelompok 8 DoneDocument5 pagesSoal Bahasa Inggris Kelompok 8 Doneputri dwi lailikaNo ratings yet
- FC1400 R4.0Document2 pagesFC1400 R4.0diniNo ratings yet
- Nursing Care Plan Cues and Evidences Nursing Diagnosis Objectives Interventions Rationale EvaluationDocument3 pagesNursing Care Plan Cues and Evidences Nursing Diagnosis Objectives Interventions Rationale EvaluationJoanne Therese ArbasNo ratings yet
- Labour Second StageDocument8 pagesLabour Second StageakankshaNo ratings yet
- Information Management Systems, ObstetricalDocument12 pagesInformation Management Systems, ObstetricalLee ThoongNo ratings yet
- SimMom Manual de UsoDocument50 pagesSimMom Manual de UsoHector ArellanoNo ratings yet
- Case Study For OligohydramniosDocument8 pagesCase Study For OligohydramniosKinjal Vasava100% (1)
- Cord ProlapseDocument17 pagesCord ProlapseRaihan RuzaidiNo ratings yet
- Conduct of Normal Labor and DeliveryDocument141 pagesConduct of Normal Labor and DeliveryRea Dominique CabanillaNo ratings yet
- Prolonged PregnancyDocument45 pagesProlonged PregnancyReshmi S ChellappanNo ratings yet
- 21 Non-Obstetric Surgery During PregnancyDocument5 pages21 Non-Obstetric Surgery During PregnancyAna-Maria CroitoruNo ratings yet
- Bahan Tugas Tokolitik Ulfadiya Putri 1Document25 pagesBahan Tugas Tokolitik Ulfadiya Putri 1hopa shopNo ratings yet
- ObstetricsDocument46 pagesObstetricsanaskabaha100% (3)
- M Vanguardia-McnpDocument11 pagesM Vanguardia-Mcnpmark OrpillaNo ratings yet
- Emergencias ReproductivasDocument24 pagesEmergencias ReproductivasYami SuperNo ratings yet
- Core Clinical Cases in ObstetricsDocument193 pagesCore Clinical Cases in Obstetricsshafijan100% (10)
- Sharon Treesa Antony Second Year M.SC Nursing Govt. College of Nursing KottayamDocument27 pagesSharon Treesa Antony Second Year M.SC Nursing Govt. College of Nursing KottayamNinaNo ratings yet
- Cardio To C OgraphyDocument6 pagesCardio To C OgraphyChinedu H. DuruNo ratings yet
- Assessment of Fetal Well-BeingDocument63 pagesAssessment of Fetal Well-BeingArhum Siddiqi100% (1)
Women Heath
Women Heath
Uploaded by
Angelic khanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Women Heath
Women Heath
Uploaded by
Angelic khanCopyright:
Available Formats
Fetal Heart Rate Response
to Maternal Exertion
Marshall W. Carpenter, MD; Stanley P. Sady, PhD; Bente Hoegsberg, MD; Mina A. Sady, MA; Barbara Haydon, BSN;
Eileen M. Cullinane, MS; Donald R. Coustan, MD; Paul D. Thompson, MD
Doppler monitoring of fetal heart rates during maternal exertion has suggested ments and distribution of brochures.
that fetal bradycardia occurs frequently during vigorous exercise, causing Women were excluded from the study if
concern for fetal safety. Doppler determination of fetal heart rate during vigorous they gave a history of medical problems
maternal effort is difficult. To avoid motion artifact, we observed fetal heart rate (such as asthma) or previous abnormal
using two-dimensional ultrasound and determined the incidence of fetal brady- pregnancies (such as preterm labor)
cardia in 45 pregnant women (age, 29.0\m=+-\3.7years [mean \m=+-\SD]; gestational that might compromise their ability to
age, 25.2 \m=+-\3.0 weeks) during 85 submaximal and 79 maximal cycle ergometer
complete the exercise test sessions. All
tests. Average fetal heart rate did not change during exercise. A single episode subjects provided written informed
consent following an orientation visit to
of fetal bradycardia (heart rate <110 beats per minute for \m=ge\10s) occurred the exerciselaboratory. The protocol
during submaximal exertion during a maternal vasovagal episode. Sixteen was approved by the institutional re¬
episodes of fetal bradycardia were noted within three minutes after cessation of view boards of all participating in¬
exercise, 15 of which followed maximal maternal effort. We conclude that brief stitutions.
submaximal maternal exercise up to approximately 70% of maximal aerobic Procedure
power (maternal heart rate \m=le\148beats per minute) does not affect fetal heart
rate. In contrast to submaximal maternal exertion, maximal exertion is common- Subjects were studied twice on sepa¬
ly followed by fetal bradycardia. This may indicate inadequate fetal gas ratedays, using an identical protocol
each time. Exercise tests were per¬
exchange. formed on an electrically braked cycle
(JAMA 1988;259:3006-3009) ergometer (Collins Pedal Mate, Brain-
tree, Mass). At each exercise test ses¬
sion, resting measurements were ob¬
VIGOROUS exertion in pregnant ewes rate decelerations are associated with
tained with subjects seated on the
reduces uterine blood flow and fetal ar¬ fetal hypoxia, such results raise concern ergometer for ten minutes (Fig 1). Sub¬
terial oxygen tension1,2 and may produce about fetal safety during vigorous exer¬ jects then cycled at 0, 30, and 60 W for
six minutes at each work load to obtain
significant fetal hypoxia. Recent human cise. Doppler measurement of fetal
submaximal exercise measurements.
studies using Doppler monitors to esti¬ heart rates during exercise is difficult,
mate fetal heart rate have reported pro¬
This was followed by five minutes of
however, because of artifact associated cool-down cycling against minimal re¬
longed fetal bradycardia even during with maternal motion.8'9 Consequently,
sistance and ten minutes of rest. The
low-intensity maternal exercise.3"5 Oth¬ we used two-dimensional ultrasonic im¬
maximal exercise session started with
ers have noted increased fetal heart rate aging to record the fetal heart rate re¬
immediately following cycling6 and run¬ sponse to maternal exercise. Our pur¬ approximately 60 W of resistance and
consisted of two-minute stages of incre¬
ning7 exercise. Since episodic fetal heart pose was to determine the effect of mental exertion until subjects were un¬
submaximal and maximal maternal ex¬
ertion on fetal heart rate and the inci¬ able or unwilling to exercise further.
From the Department of Obstetrics and Gynecology, dence of fetal bradycardia. Subjects continued to cycle for five min¬
utes against minimal resistance. They
Women and Infants Hospital (Drs Carpenter, Hoegs-
berg, and Coustan and Ms Haydon), and the Depart- METHODS then assumed a semirecumbent position
ment of Medicine, Miriam Hospital (Drs Sady and for an additional seven minutes of ultra¬
Thompson and Mss Sady and Cullinane), Brown Uni- Subjects sound observation followed by a non-
versity Program in Medicine, Providence, RI.
Reprint requests to Women and Infants Hospital, 101 Pregnant women were recruited into stress test. This latter test documents
Dudley St, Providence, RI 02905 (Dr Carpenter). the study through television announce- fetal heart rate acceleration in response
Downloaded From: http://jama.jamanetwork.com/ by a New York University User on 06/13/2015
three because of subject concerns about
100 fetal bradycardia. Consequently, 79
maximal and 85 submaximal exercise
tests among 45 subjects form the basis
of this report. Statistical tests were per¬
75
formed using Student's t test for inde¬
pendent means or the Wilcoxon rank-
sum test if a normal distribution was not
50 present. Fisher's exact test was used to
determine significant associations be¬
tween categorical variables.
25
RESULTS
Forty-five women were enrolled. The
mean age of the women was 29.2 ±3.7
Maximal years, and their mean gestation was
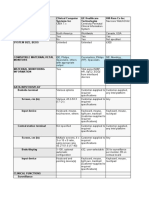
Resti Submaximal Exertion Rest 2 Exertion Rest 3 25.2 ±3.0 weeks (range, 20 to 34
-1t— weeks). All subjects had uncomplicated
10 16 22 28 33 43 ~53 —58
pregnancies. None smoked cigarettes
or took any medications except for pre¬
Exercise Period and Elapsed Time, min natal vitamins and iron. Twenty-one re¬
ported that they had exercised vigor¬
Fig 1.—Exercise protocol: duration of rest and exercise periods and associated percentage of maximal ously more than once a week prior to
aerobic power. pregnancy, and 16 reported that they
engaged in regular exercise during
pregnancy. Only three of the 16 exercis¬
Table 1.—Exercise Protocol Completion by Subjects ( =
45) ers performed prolonged exercise (96 to
112 km of running per week in one and
No. of Subjects >8 km per week of swimming in two).
Submaximal The others participated in recreational
and Maximal
Session Exertion
exercise of undetermined intensity.
1 42
Peak maternal oxygen uptake (V02)
2 37 among completed protocols averaged
25.9 ±4.2 mL-kg'-min' (mean ± SD)
(range, 18.0 to 39.0 mL-kg'-min"'), and
peak maternal heart rate was 180 ±8.6
to fetal movement. Such a response is observer (M.W.C.) who determined the beats per minute (range, 156 to 197
physiological and is accepted as exclud¬ fetal heart rate during each minute of beats per minute). In contrast, at the
ing fetal asphyxia.10 the exercise session. This was calcu¬ end of the submaximal portion of the
Maternal blood pressure was mea¬ lated from the elapsed time for the first protocol, the V02 was 17.2 ±2.4
sured with a mercury sphygmomanom- observed 20 cardiac cycles within each mL-kg~'-mnT' and maternal heart rate
eter at each work load and every minute minute of the protocol. Fetal bradycar¬ was 148 ± 16 beats per minute. This in¬
for the five minutes following maximal dia was defined as a heart rate below 110 dicates that during the submaximal por¬
exertion. Maternal heart rate and oxy¬ beats per minute for more than 10 s at tion of the protocol, subjects attained
gen uptake were measured during the any time during the testing session. VO2 values equaling 67.4% ±11.8% of
fourth and fifth minutes of each submax¬ Bradycardia duration was timed from their measured maximal aerobic power
imal exercise stage and during each onset to return of heart rate to pre- (V02max).
minute of the maximal exertion part of exercise values. Women who exercised regularly dur¬
the protocol. Maternal heart rate was To determine the reproducibility of ing pregnancy had a higher mean peak
measured using an electrocardiogram fetal heart rate estimations, we re¬ V02 (29.6±3.9 mL-kg'-min1) than less
(Marquette Instruments, Milwaukee). peated heart rate measurements ten active subjects (24.1 ± 3.2 mL-kg'-min ')
Oxygen uptake was determined using times on the same videotape segment (P<.01). In 57 maximal exercise ses¬
standard open-circuit spirometrie tech¬ for five randomly selected subjects at sions (72%), an increase in work rate
niques.11 Expired volume was measured each of the five rest and exercise peri¬ elicited less than a 150-mL/min increase
with a Fleisch pneumotach attached to a ods. The mean coefficient of variation in V02, thus meeting widely accepted
differential pressure transducer (Vali- was 2.2% or less for each period. criteria for maximum oxygen uptake
dyne MP-45, Northridge, Calif), and ex¬ Data
(Vo2 max).12 There was no difference in
pired gas concentrations were deter¬ Analysis peak V02 or peak maternal heart rate
mined with a mass spectrometer Satisfactory submaximal and maxi¬ between subjects who did and did not
(Perkin Elmer MGA 1100, Pomona, mal exercise data were obtained during satisfy this VOçjnax criterion (26.0 ±3.5
Calif). both exercise sessions in 37 subjects vs 25.7 ± 5.8 mL-kg'-min and 180 ± 8 vs
'
Fetal cardiac activity was continu¬ (Table 1). Three of the first sessions and 179 ± 9 beats per minute, respectively).
ously monitored and videotaped during three of the second sessions included This confirms that exercise effort was
exercise and rest periods using a linear only the submaximal portion of the pro¬ maximal or near maximal.
array two-dimensional ultrasound sys¬ tocol. Five subjects did not attempt a There were no significant differences
tem (Toshiba SLA-77A, Nasu, Japan). second exercise session: one because of in mean fetal heart rates between the
Videotapes were subsequently re¬ uterine contractions, one because of preexercise period and subsequent ex¬
viewed in entirety by an experienced exercise-associated hypotension, and ercise and rest periods (Table 2). Com-
Downloaded From: http://jama.jamanetwork.com/ by a New York University User on 06/13/2015
Table 2.—Mean Fetal Heart Rate During Rest and Table 3.—Exercise Variables in Sessions Where
Exercise Periods Fetal Bradycardia Was Present or Absent After
Maximal Exercise
No. of Average Fetal
Sessions Heart Rate,
Fetal
Completely Beats min,
Condition Recorded Mean ± SD Bradycardia, Mean ± SD
Resti 81 147±6 Present Absent
Exercise Variable (n 15)
=
(n=64)
OW 80 148±7 Peak maternal
30 W 80 148±7 heart rate,
60 W 80 148±8 beats/min 180.0 ±9.7 180.0 ±8.4
Rest 2 80 148±7 Peak maternal
Maximal oxygen uptake,
exercise 77 148 + 7
Rest 3 76 143±14 mL-kg-^min-1 29.0 ±5.3* 25.1 ±3.6
Duration of maximal
exercise period, min 7.4 ±2.5 6.9 ±1.8
Systolic pressure,
mm Hgt 39.0 ±18.7 36.0 ±15.6
parison of mean fetal heart rates during Diastolic pressure,
first and second exercise sessions for mm Hgt 18.0±21.8 10.0 ±12.0
Mean arterial
each subject also showed no significant pressure, mm Hgt 21.0±14.4 17.0 ±10.5
differences.
Eighteen episodes of fetal bradycar- *P<.01, unpaired r test.
tRefers to blood pressure at maximal exertion minus
dia were associated with the 85 exercise lowest pressure during recovery and includes 12 ses¬
test sessions, but only one episode oc¬ sions with and 58 without fetal bradycardia.
curred during exercise. This subject
sustained vasovagal hypotension dur¬
ing the second submaximal work load.
Two episodes of bradycardia in the same ute (range, 43 to 102 beats per minute).
fetus occurred on different exercise All episodes showed a rapid decelera¬
days; one prior to and one following the tion and most rapidly returned to base¬
submaximal portion of the exercise pro¬ line (Fig 2). Marked short-term varia¬
tocol. Therefore, 15 of 16 postexercise tion of heart rate characterized most
fetal bradycardias occurred after maxi¬ bradycardic episodes, although the two
mal maternal exertion, an incidence of episodes lasting greater than nine min¬
16.2% compared with 1.2% after sub- utes returned to baseline only slowly.
maximal exertion (P .0003).
=
Nevertheless, reactive nonstress tests
Peak maternal oxygen uptake was (fetal cardiac acceleration with fetal
higher during maximal exercise ses¬ movement) were observed within 30
sions that were followed by fetal minutes after conclusion of all exercise
bradycardia (29.0 ±5.3 vs 25.1 ±3.6 sessions.
mL-kg-'-min"1) (P .015).
=
Subjects Fetal bradycardia following maximal
achieved a plateau of oxygen uptake in a exertion occurred during both exercise
similar proportion of sessions (12/15 test sessions in three subjects, only dur¬
[80%] with and 44/63 [70%] without bra¬ ing the first session in seven subjects,
dycardia). Similarly, there were no dif¬ and only during the second session in
ferences in peak maternal heart rate two subjects. Three subjects, however, 12 3 4 5 6 7 8 9101112
between sessions with (180 ±8 beats elected not to perform a second maximal
per minute) and without (180 ± 10 beats test becuse of fetal bradycardia during Time, min
per minute) bradycardia. A maternal the initial session. Consequently, three
history of regular exercise during preg¬ of the seven subjects with bradycardia
Fig 2.—Fetal heart rate following maximal exertion
nancy was noted in 21 (33%) of 64 during the first exercise session who during 14 episodes of fetal bradycardia. Fetal heart
sessions without fetal bradycardia and exercised twice had a repeated episode rates were averaged over ten cardiac cycles every
in five (33%) of 15 sessions with after their second session. 30 s during postexercise period. One tape was lost.
bradycardia. Subjects gave birth at 40.0 ±0.8 Predeceleration baseline fetal heart rate and nadir
Maternal and fetal age did not differ weeks of gestation, and none had pre- fetal heart rate are noted for each deceleration. Zero
time equals time of cessation of maximal exertion.
in sessions with and without fetal brady¬ term labor or bleeding. Fetal bradycar¬
cardia (28.9 ±4.0 vs 29.4 ±3.8 years dia following maximal maternal exer¬
[P>.05] and 26.4 ±3.4 vs 25.9±3.0 tion did not predict future perinatal
weeks [P>.05], respectively). Similar¬ problems. By history from the attend¬ cell tumor of the brain and died at 5
ly, the duration of the maximal exercise ing obstetricians, there was only one weeks of age. A third child suffered sud¬
period, maternal blood pressure during abnormal fetal heart rate pattern intra- den infant death syndrome at 5 weeks of
exercise, and the fall in maternal blood partum, in an infant born with group age. None of these infants demonstrat¬
pressure after maximal exertion did not ß-hemolytic streptococcal sepsis who ed fetal bradycardia during this study.
differ between these groups (Table 3). died the day of birth. There were no
Fetal bradycardia occurred 96 ± 51 s reported cord entanglements. Forty- COMMENT
(range, 31 to 180 s) after maximal exer¬ three ofthe 45 infants had normal Apgar Renal13 and blood flow
splanchnic1,14
tion and lasted a median of 90 s (range, scores and normal physical examination decreases during exercise
in the non-
13 to 561 s). The lowest fetal heart rate results at birth. Of those with abnormal pregnant and pregnant animal. This re¬
during each postmaximal exertion bra¬ physical examination results, one was duction is proportional to the duration
dycardia determined from ten cardiac the infant with streptococcal sepsis, and and intensity of exercise and is medi¬
cycles averaged 73 ± 21 beats per min- the other had an undifferentiated germ ated by sympathetic vasoconstriction.15
Downloaded From: http://jama.jamanetwork.com/ by a New York University User on 06/13/2015
Pregnant ewes exercised to exhaustion less than the 30 minutes previously re¬ homeostatic mechanisms that previous¬
on a treadmill manifest a significant fall sulting in postexercise fetal tachycar¬ ly maintained fetal oxygen extraction.
in fetal oxygen tension without a de¬ dia.6,7 Our studies also contrast with pri¬ Consistent with this hypothesis are the
creased fetoplacental oxygen extraction or observations in finding no observations that moderate hypoxia
or net lactate production.2 Mild bicycle unexplained fetal bradycardia during produces vagally mediated bradycardia
exercise in humans in the supine posi¬ maternal exertion, despite work loads without antecedent tachycardia in un-
tion reduced sodium 24 washout from at or near maximal maternal oxygen anesthetized fetal and newborn lambs'8
the myometrium in one study,'6 sug¬ uptake. and our experience that most fetal bra¬
gesting a 25% reduction in perfusion. Subjects who had higher peak Vo2 dycardia occurred within two minutes
Heavy maternal exercise, therefore, during maximal voluntary exertion of exercise cessation. Vagai slowing of
may challenge fetal respiratory homeo- were more likely to demonstrate post- fetal heart rate may result from barore-
stasis and result in fetal hypoxia. exercise fetal bradycardia. This asso¬ ceptor responses as well as hypoxic
Studies of maternal exercise in ciation suggests that higher exercise stimulus of aortic and carotid chemore-
humans have examined changes in fetal capacity may predispose to fetal brady¬ ceptors. We assume that possible fetal
heart rate as an indicator of distur¬ cardia after maximal exertion. Subjects hypoxia after maternal exercise is mild
bances of fetal gas exchange. Fetal reporting frequent recreational exer¬ and transient, since all fetuses had nor¬
heart rate observations during and cise had no higher incidence than seden¬ mal nonstress test results within 30
after exercise have used Doppler moni¬ tary individuals, but we did not quantify minutes of exercise cessation.
tors of the type used with inactive the level of physical activity in subjects Our findings suggest that unex¬
women during labor. In some studies, outside the laboratory. Both maternal plained fetal bradycardia during mater¬
this technique has revealed increases in heart rate and Vo2 values among nal exertion of any intensity is rare.
fetal heart rate during maternal recov¬ subjects with and without postexercise Similarly, fetal bradycardia was rarely
ery following 30 minutes of submaximal fetal bradycardia indicate that both observed after maternal exercise re¬
exertion.6,7 Others, using Doppler moni¬ groups had peak efforts at or near their quiring an average of 67% of the
toring of women in the third trimester, VOjinax. mother's VOjinax or a mean maternal
have reported incidence of fetal bra¬
an The physiology of postexertional fetal heart rate of 148 beats per minute. Ma¬
dycardia during exercise of 11% to bradycardia must account for the ob¬ ternal exertion approaching maximal
100%, even at low work loads.3"5 served absence of fetal heart rate aerobic capacity, however, may be fol¬
We and others,58,9 however, have ob¬ changes during maternal exercise, the lowed by fetal bradycardia. The signifi¬
served that Doppler fetal heart rate prompt onset of fetal bradycardia fol¬ cance of this bradycardia is, as of yet,
monitoring during exercise is difficult lowing cessation of maximal maternal unknown. However, it seems prudent
because of artifact related to maternal effort, the steep slope of deceleration of to recommend that pregnant women
movement. Consequently, the inci¬ fetal heart rate, and the usually rapid limit their vigorous exercise to activi¬
dence of fetal bradycardia during ma¬ return of fetal heart rate to baseline ties requiring heart rates of 150 beats
ternal exercise and the risk of maternal values. A significant reduction in total per minute or less and conclude with a
exertion have been questioned.8,9 Two- uterine blood flow with heavy exertion gentle and continuous slowing of effort
dimensional ultrasound imaging, in con¬ has been observed.1,2 This reduction during recovery. Exercise in the pres¬
trast, appears to be accurate and may be exacerbated by the abrupt fall in ent study was brief, so we cannot com¬
reliable. maternal stroke volume found after ces¬ ment on the effect of exercise duration
In our study, we found the mean fetal sation of upright exercise late in human on the fetal heart rate response.
cardiac rate to be stable during and af¬ pregnancy.17 The combined effects of re¬
ter maternal exertion and independent duced uterine perfusion during vigor¬
of exercise intensity. The duration of ous exertion and the decrease in cardiac This study was supported by National Institutes
our exercise protocol, however, was output after exercise may compromise of Health grant P50HD11343.
References
1. Lotgering FK, Gilbert RD, Longo LD: Exercise rate reactivity before and after maternal jogging 13. Hohimer AR, Smith OA: Decreased renal
responses in pregnant sheep: Blood gases, tem- during the third trimester. Am J Obstet Gynecol blood flow in the baboon during mild dynamic leg
peratures, and fetal cardiovascular system. J Appl 1982;545-547. exercise. Am J Physiol 1979;236:H141-H150.
Physiol 1983;55:842-850. 8. Paolone AM, Shangold M: Artifact in the record- 14. Horvath SM: Review of energetics and blood
2. Clapp JF: Acute exercise stress in the pregnant ing of fetal heart rates during maternal exercise. J flow in exercise. Diabetes 1979;28(suppl 1):33-38.
ewe. Am J Obstet Gynecol 1980;136:489-494. Appl Physiol 1987;62:848-849. 15. Rowell LB: Human cardiovascular adjust-
3. Artal R, Romem Y, Paul RH, et al: Fetal brady- 9. O'Neill ME, Cooper KA, Hunyor SN, et al: ments to exercise and thermal stress. Physiol Rev
cardia induced by maternal exercise. Lancet 'Pseudo' fetal bradycardia during maternal exer- 1974;54:75-119.
1984;2:258-260. cise. J Appl Physiol 1987;62:849-850. 16. Morris N, Osborn SB, Wright HP, et al: Effec-
4. Jovanovic L, Kessler A, Peterson CM: Human 10. Keegan KA, Paul RH: Antepartum fetal heart tive uterine blood-flow during exercise in normal
maternal and fetal response to graded exercise. J rate testing: IV. The nonstress test as a primary and pre-eclamptic pregnancies. Lancet 1956;2:481\x=req-\
Appl Physiol 1985;58:1719-1722. approach. Am J Obstet Gynecol 1980;136:75-80. 484.
5. Artal R, Rutherford S, Romem Y, et al: Fetal 11. Wilmore JH, Costill DL: A semiautomated sys- 17. Morton MJ, Paul MS, Campos GR, et al: Exer-
heart rate responses to maternal exercise. Am J tems approach to the assessment of oxygen uptake cise dynamics in late gestation:Effects of physical
Obstet Gynecol 1986;155:729-733. during exercise. J Appl Physiol 1974;36:618-620. training. Am J Obstet Gynecol 1985;152:91-97.
6. Collings C, Curet LB: Fetal heart rate response 12. Taylor HL, Buskirk E, Henschel A: Maximal 18. Walker AM, Cannata JP, Dowling MH, et al:
to maternal exercise. Am J Obstet Gynecol oxygen uptake as an objective measure of cardio- Age-dependent pattern of autonomic heart rate
1985;151:498-501. respiratory performance. J Appl Physiol 1955;8: control during hypoxia in fetal and newborn lambs.
7. Hauth JC, Gilstrap LC, Widmer K: Fetal heart 73-80. Biol Neonate 1979;35:198-208.
Downloaded From: http://jama.jamanetwork.com/ by a New York University User on 06/13/2015
You might also like
- Acog Practice Bulletin: Antepartum Fetal SurveillanceDocument12 pagesAcog Practice Bulletin: Antepartum Fetal SurveillanceMariana Hernandez100% (10)
- Case Simulation 118Document4 pagesCase Simulation 118Rica AvendañoNo ratings yet
- Electronic Fetal MonitoringDocument4 pagesElectronic Fetal MonitoringMauZungNo ratings yet
- Electrotherapy Evidence Based PracticeDocument401 pagesElectrotherapy Evidence Based PracticeAngelic khan50% (4)
- Handbook of Practical ElectrotherapyDocument164 pagesHandbook of Practical ElectrotherapyAngelic khan100% (2)
- Antepartum Fetal Well Being AssessmentDocument14 pagesAntepartum Fetal Well Being AssessmentIsrael WoseneNo ratings yet
- Left Tilt Manuever to Minimize HypotensionDocument5 pagesLeft Tilt Manuever to Minimize HypotensionAbdul Haseeb KhattakNo ratings yet
- ingemarsson1985Document7 pagesingemarsson1985Asela SubhasingheNo ratings yet
- Massagem Perineal em Trabalho de Parto e Prevenção de Trauma Perineal Ensaio Clínico RandomizadoDocument4 pagesMassagem Perineal em Trabalho de Parto e Prevenção de Trauma Perineal Ensaio Clínico RandomizadoSheila SilvaNo ratings yet
- Profil Biofisik High RiskDocument5 pagesProfil Biofisik High RiskbebekbebekNo ratings yet
- 0091-2182 2885 2990126-0 PDFDocument1 page0091-2182 2885 2990126-0 PDFParahmitaNo ratings yet
- Satoshi Dohi, Kiyotake Ichizuka, Ryu Matsuoka, Kohei Seo, Masaaki Nagatsuka, Akihiko SekizawaDocument6 pagesSatoshi Dohi, Kiyotake Ichizuka, Ryu Matsuoka, Kohei Seo, Masaaki Nagatsuka, Akihiko SekizawasandiNo ratings yet
- Ajacm 2009 4 (1) Acup Improve EndometrDocument7 pagesAjacm 2009 4 (1) Acup Improve EndometrdirkvandeweyerNo ratings yet
- Prospective Evaluation of Individual Cardiotocography Parameters in Predicting A Nonasphyxiated FetusDocument4 pagesProspective Evaluation of Individual Cardiotocography Parameters in Predicting A Nonasphyxiated FetusSanjay GoleNo ratings yet
- Partus LamaDocument4 pagesPartus LamaIntan PermataNo ratings yet
- Obestritic Anesthesia DNB Q & ADocument162 pagesObestritic Anesthesia DNB Q & Ahiwotbetesfa2123No ratings yet
- Does Exercise Training During Pregnancy Affect Gestational Age? A Randomised Controlled TrialDocument6 pagesDoes Exercise Training During Pregnancy Affect Gestational Age? A Randomised Controlled TrialTrnidad Moder GarvizoNo ratings yet
- Antepartum Fetal Surveillance ACOG Bulletin 2014 PDFDocument11 pagesAntepartum Fetal Surveillance ACOG Bulletin 2014 PDFDanNo ratings yet
- Archdischild 2023 326099.fullDocument5 pagesArchdischild 2023 326099.fullAlina1102No ratings yet
- Procedures ObgDocument12 pagesProcedures Obgraghuram reddyNo ratings yet
- The Effect of Hyoscine Butylbromide On The First Stage of Labour in Term PregnanciesDocument5 pagesThe Effect of Hyoscine Butylbromide On The First Stage of Labour in Term PregnanciesnephylymNo ratings yet
- NST CSTDocument9 pagesNST CSTNadiya RashidNo ratings yet
- Roy 2008Document4 pagesRoy 2008yenni anggrainiNo ratings yet
- Delayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleDocument11 pagesDelayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleManju KumariNo ratings yet
- p425Document4 pagesp425Adnan KhanNo ratings yet
- Chu 2018Document8 pagesChu 2018Nicholas PratamaNo ratings yet
- Co 713Document5 pagesCo 713larasNo ratings yet
- Preoperative Stabilisation in Congenital Diaphragmatic HerniaDocument3 pagesPreoperative Stabilisation in Congenital Diaphragmatic HerniaAgus PrimaNo ratings yet
- 2003-1050 KaminskiDocument10 pages2003-1050 KaminskichrisgochiroNo ratings yet
- 1298 4803 1 PBDocument6 pages1298 4803 1 PBshashikiran7920No ratings yet
- Fetal Well BeingDocument5 pagesFetal Well BeingCARL JOHN MANALONo ratings yet
- Delayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleDocument11 pagesDelayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleFatma ElzaytNo ratings yet
- Graphy) The Fetal Heartbeat (Cardio-) and The Uterine Contractions (-Toco-) DuringpregnancyDocument6 pagesGraphy) The Fetal Heartbeat (Cardio-) and The Uterine Contractions (-Toco-) DuringpregnancyHanna GustinNo ratings yet
- Benson Multicentre 1986Document4 pagesBenson Multicentre 1986Dian NovitasariNo ratings yet
- Jurnal Inter EDEMA 2Document4 pagesJurnal Inter EDEMA 2Edom LazarNo ratings yet
- 125 - Fetal Biophysical ProfileDocument5 pages125 - Fetal Biophysical ProfileYuly Andrea Marquez CastañedaNo ratings yet
- Medical Case Write UpDocument11 pagesMedical Case Write UpJang Abd MutalibNo ratings yet
- Reporte Especial Resicitacion NeonatalDocument17 pagesReporte Especial Resicitacion NeonatalAna León VigilNo ratings yet
- Students' Corner Protocols For Exercise During Pregnancy: AcknowledgementDocument4 pagesStudents' Corner Protocols For Exercise During Pregnancy: AcknowledgementMaria Quiza GeñosoNo ratings yet
- Effect of Single Low Dose Intrathecal Labor Analgesia On Maternal and Fetal OutcomeDocument6 pagesEffect of Single Low Dose Intrathecal Labor Analgesia On Maternal and Fetal OutcomeAnnaNo ratings yet
- Altered Uteroplacental Tissue PerfusionDocument5 pagesAltered Uteroplacental Tissue PerfusionArielle BajalaNo ratings yet
- Angle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundDocument5 pagesAngle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundNella SolanoNo ratings yet
- Timingyavas 2004Document10 pagesTimingyavas 2004Ramadhan AkmalNo ratings yet
- Referensi Nomor 6Document9 pagesReferensi Nomor 6audreynatalia777No ratings yet
- Supported By: None.: AbstractsDocument1 pageSupported By: None.: AbstractsFerry DimyatiNo ratings yet
- Uterine Blood Flow During Supine Rest and Exercise After 28 Weeks of GestationDocument9 pagesUterine Blood Flow During Supine Rest and Exercise After 28 Weeks of GestationMD Luthfy LubisNo ratings yet
- Objective Definition of Shoulder Dystocia: A Prospective EvaluationDocument4 pagesObjective Definition of Shoulder Dystocia: A Prospective Evaluationbahtiar bleachNo ratings yet
- Urban 2005Document5 pagesUrban 2005Miyyada AichaouiNo ratings yet
- AHA Guidelines On Neonatal ResuscitationDocument17 pagesAHA Guidelines On Neonatal ResuscitationVillia Damayantie100% (1)
- Effects of SP6 Acupuncture Point Stimulation On Labor Pain and Duration of LaborDocument8 pagesEffects of SP6 Acupuncture Point Stimulation On Labor Pain and Duration of LaborRismaAyuSaraswatiNo ratings yet
- +second Stage of Labor and Epidural Use A Larger.8Document9 pages+second Stage of Labor and Epidural Use A Larger.8Valentina AnastasNo ratings yet
- Does Regular Exercise in Pregnancy Influence Duration of Labor? A Secondary Analysis of A Randomized Controlled TrialDocument7 pagesDoes Regular Exercise in Pregnancy Influence Duration of Labor? A Secondary Analysis of A Randomized Controlled Trialana pintoNo ratings yet
- Ashrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarDocument4 pagesAshrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarWilliam AdiputraNo ratings yet
- Nursing Care Plan Cues Diagnosis Planning Implementation Rationale EvaluationDocument4 pagesNursing Care Plan Cues Diagnosis Planning Implementation Rationale EvaluationChrizley Shawn DeroniaNo ratings yet
- Do Zavanelli ModifDocument3 pagesDo Zavanelli ModifSAKAI69No ratings yet
- Persistence of Fetal Memory Into Neonatal LifeDocument5 pagesPersistence of Fetal Memory Into Neonatal LifeRodrigo LeãoNo ratings yet
- Friedman EA (2000) : Labor: Clinical Evaluation and Management, P 23, 2nd Ed. New York, Appleton-Century-CroftsDocument5 pagesFriedman EA (2000) : Labor: Clinical Evaluation and Management, P 23, 2nd Ed. New York, Appleton-Century-CroftsJuliane ItliongNo ratings yet
- Vagal Activity, Gastric Motility Masaje InfantilDocument6 pagesVagal Activity, Gastric Motility Masaje InfantilIsis SanzNo ratings yet
- NRP - Ima-IsaDocument55 pagesNRP - Ima-IsaPeter RamNo ratings yet
- BJVR - Volume 6 - Issue 2 - Pages 37-41Document5 pagesBJVR - Volume 6 - Issue 2 - Pages 37-41avijaymba808No ratings yet
- Suppression of Puerperal Lactation Using Jasmine Flowers (Jasminum Sambac)Document4 pagesSuppression of Puerperal Lactation Using Jasmine Flowers (Jasminum Sambac)Iara PachêcoNo ratings yet
- 1 s2.0 S1836955323001212 MainDocument8 pages1 s2.0 S1836955323001212 Mainfilipa reisNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Osteoporosis: Hani Abu DiehDocument24 pagesOsteoporosis: Hani Abu DiehAngelic khan100% (1)
- Prepared By: Ulfat Amin MSC Pediatric NursingDocument25 pagesPrepared By: Ulfat Amin MSC Pediatric NursingAngelic khanNo ratings yet
- Microbiology BcqsDocument16 pagesMicrobiology BcqsAngelic khanNo ratings yet
- Osteoarthritis 1583-170210113823Document34 pagesOsteoarthritis 1583-170210113823Angelic khanNo ratings yet
- Elbow Joint: Dr. Sharjeel Tasneem BSPT, (KU) MSPT, (KU) ADPT, (Ziauddin University)Document26 pagesElbow Joint: Dr. Sharjeel Tasneem BSPT, (KU) MSPT, (KU) ADPT, (Ziauddin University)Angelic khanNo ratings yet
- Arthritis: by DR Samra Tahseen Registrar, Radiology LNHDocument86 pagesArthritis: by DR Samra Tahseen Registrar, Radiology LNHAngelic khanNo ratings yet
- Pathology of The Respiratory SystemDocument57 pagesPathology of The Respiratory SystemAngelic khanNo ratings yet
- Et-Lec 14 Wax TherapyDocument64 pagesEt-Lec 14 Wax TherapyAngelic khanNo ratings yet
- Introduction To Medical SpirochaetalesDocument25 pagesIntroduction To Medical SpirochaetalesAngelic khanNo ratings yet
- Microbiology Medical MicrobiologyDocument40 pagesMicrobiology Medical MicrobiologyAngelic khanNo ratings yet
- Drugs Used in Current Physical Therapy PracticeDocument22 pagesDrugs Used in Current Physical Therapy PracticeAngelic khan100% (1)
- Drug Side EffectsDocument2 pagesDrug Side EffectsAngelic khanNo ratings yet
- Gene Therapy CartilageDocument15 pagesGene Therapy CartilageAngelic khanNo ratings yet
- Three Basic Types of Muscle ContractionsDocument2 pagesThree Basic Types of Muscle ContractionsAngelic khanNo ratings yet
- Presented by Yasha Ali Bangash & Pashmina Khan DPT Batch Ii Semester VDocument20 pagesPresented by Yasha Ali Bangash & Pashmina Khan DPT Batch Ii Semester VAngelic khanNo ratings yet
- Pharmacology of Central Nervous SystemDocument20 pagesPharmacology of Central Nervous SystemAngelic khan100% (1)
- Pharmacology of Central Nervous System Antipsychotic and Parkinson DiseaseDocument22 pagesPharmacology of Central Nervous System Antipsychotic and Parkinson DiseaseAngelic khanNo ratings yet
- GENE THERAPY For Musculoskeletal DisordersDocument20 pagesGENE THERAPY For Musculoskeletal DisordersAngelic khanNo ratings yet
- Therapeutic Exercise Foundation ConceptsDocument13 pagesTherapeutic Exercise Foundation ConceptsAngelic khanNo ratings yet
- ფიზიოლოგიური მშობიარობის მართვაDocument30 pagesფიზიოლოგიური მშობიარობის მართვაAchi BeridzeNo ratings yet
- Antenatal Fetal MonitoringDocument51 pagesAntenatal Fetal MonitoringCodillia Cheong100% (2)
- Fetal Monitoring Technology: Application NoteDocument8 pagesFetal Monitoring Technology: Application NoteCarlos MedikalNo ratings yet
- Figo Consensus Guidelines On Intrapartum Fetal Monitoring: Intermittent AuscultationDocument7 pagesFigo Consensus Guidelines On Intrapartum Fetal Monitoring: Intermittent AuscultationWilliam WongNo ratings yet
- Fetal Assessment and Wellbeing in Pregnancy (FetalDocument23 pagesFetal Assessment and Wellbeing in Pregnancy (Fetalapi-3705046100% (1)
- Labor DystociaDocument100 pagesLabor DystociaAnonymous kChMIy7tXNo ratings yet
- 344 PreprintDocument4 pages344 PreprintDii ScottouNo ratings yet
- IUFD AnitaDocument65 pagesIUFD AnitaarifuadNo ratings yet
- Antenatal Assssment Final @@Document46 pagesAntenatal Assssment Final @@Pragati BholeNo ratings yet
- Soal Bahasa Inggris Kelompok 8 DoneDocument5 pagesSoal Bahasa Inggris Kelompok 8 Doneputri dwi lailikaNo ratings yet
- FC1400 R4.0Document2 pagesFC1400 R4.0diniNo ratings yet
- Nursing Care Plan Cues and Evidences Nursing Diagnosis Objectives Interventions Rationale EvaluationDocument3 pagesNursing Care Plan Cues and Evidences Nursing Diagnosis Objectives Interventions Rationale EvaluationJoanne Therese ArbasNo ratings yet
- Labour Second StageDocument8 pagesLabour Second StageakankshaNo ratings yet
- Information Management Systems, ObstetricalDocument12 pagesInformation Management Systems, ObstetricalLee ThoongNo ratings yet
- SimMom Manual de UsoDocument50 pagesSimMom Manual de UsoHector ArellanoNo ratings yet
- Case Study For OligohydramniosDocument8 pagesCase Study For OligohydramniosKinjal Vasava100% (1)
- Cord ProlapseDocument17 pagesCord ProlapseRaihan RuzaidiNo ratings yet
- Conduct of Normal Labor and DeliveryDocument141 pagesConduct of Normal Labor and DeliveryRea Dominique CabanillaNo ratings yet
- Prolonged PregnancyDocument45 pagesProlonged PregnancyReshmi S ChellappanNo ratings yet
- 21 Non-Obstetric Surgery During PregnancyDocument5 pages21 Non-Obstetric Surgery During PregnancyAna-Maria CroitoruNo ratings yet
- Bahan Tugas Tokolitik Ulfadiya Putri 1Document25 pagesBahan Tugas Tokolitik Ulfadiya Putri 1hopa shopNo ratings yet
- ObstetricsDocument46 pagesObstetricsanaskabaha100% (3)
- M Vanguardia-McnpDocument11 pagesM Vanguardia-Mcnpmark OrpillaNo ratings yet
- Emergencias ReproductivasDocument24 pagesEmergencias ReproductivasYami SuperNo ratings yet
- Core Clinical Cases in ObstetricsDocument193 pagesCore Clinical Cases in Obstetricsshafijan100% (10)
- Sharon Treesa Antony Second Year M.SC Nursing Govt. College of Nursing KottayamDocument27 pagesSharon Treesa Antony Second Year M.SC Nursing Govt. College of Nursing KottayamNinaNo ratings yet
- Cardio To C OgraphyDocument6 pagesCardio To C OgraphyChinedu H. DuruNo ratings yet
- Assessment of Fetal Well-BeingDocument63 pagesAssessment of Fetal Well-BeingArhum Siddiqi100% (1)