Professional Documents
Culture Documents
Chapter 19 Microbial Diseases of The Skin and Wounds
Chapter 19 Microbial Diseases of The Skin and Wounds
Uploaded by
GRACE MAR CABAHUGOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 19 Microbial Diseases of The Skin and Wounds
Chapter 19 Microbial Diseases of The Skin and Wounds
Uploaded by
GRACE MAR CABAHUGCopyright:
Available Formats
CHAPTER 19: MICROBIAL DISEASES OF THE SKIN AND WOUNDS
Functions of the skin • Cuts, scrapes, surgery, burns, bites, etc. Normal Microbiota of the Skin
• Allow microbes to infect the deeper tissues of the
• Prevents excessive water loss body Skin microbiota
• Regulates temperature • In most cases, other body defenses eliminate
• Involved in sensory phenomena infection • Made up of various microbes
• Assists in vitamin D formation • Can result in severe or fatal diseases o Yeast
• Barrier against microbial invaders Malassezia
Skin microbiota o Bacteria
Composed of two main layers Staphylococcus, Micrococcus,
• Normally harmless microbes present on the skin and the diphtheroids
• Dermis • Compete with potential pathogens for nutrients
• Epidermis and space May produce disease
• Cannot be completely removed through
Wounds cleansing • If penetrate epidermis or if immune system is
• Typically grow in moist areas of the skin suppressed
• Trauma to any tissue of the body
• Waste products cause body odor
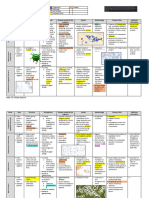
VIRAL DISEASES OF THE SKIN AND WOUNDS
Causative agent/ Pathogen and Diagnosis, treatment, and
Disease Gram Signs and symptoms Pathogenesis Epidemiology
Bacteria virulence factors prevention
Diagnosis
Isolation of Gram-
Infection of the hair
positive bacteria in
follicle S. epidermidis
grapelike clusters from
• Sty when it occurs Staphylococcus lacks virulence
pus
at the eyelid base transmitted via factors and
Treatment
Facultative • Spread of direct contact rarely causes
• Dicloxacillin
anaerobic; infection into or by fomites disease
Folliculitis Staphylococcus (semisynthetic penicillin)
+ cocci surrounding tissues Infection can S. aureus
(pimple) aureus is the drug of choice
arranged in can produce spread into the transiently
• Vancomycin is used to
clusters furuncles blood and colonizes the skin
treat resistant strains
• Carbuncles occur move to organs or mucous
Prevention
when multiple beyond the skin membranes of
• Hand antisepsis
furuncles grow most people
• Proper procedures in
together
hospitals to minimize
MRSA infections
Staphylococcal Skin becomes red Some No scarring Disease occurs Diagnosis
Scalded Skin Staphylococcus and wrinkled and Staphylococcus because dermis primarily in by characteristic
+
Syndrome aureus forms blisters aureus strains is unaffected infants sloughing of skin
(SSSS) Outer epidermis • One or two Death is rare Transmitted by Treatment
peels off in sheets different but may be due person-to-person Treated by
exfoliative toxins to secondary spread of administration of
cause SSSS infections bacteria antimicrobial drugs such
as Cloxacillin
Prevention
Widespread presence of
S. aureus makes
prevention difficult
• The bacteria Diagnosis
invade where • Transmitted by Impetigo: presence of
Impetigo: red the skin is person-to-person vesicles
Mostly:
Impetigo cocci patches form on Virulence factors: compromised contact or via Treatment
Staphylococcus
the face and limbs impetigo • Acute fomites Impetigo: Topical: Mupirocin
aureus
+ Erysipelas: • M protein glomerulonephr • Impetigo occurs Oral: Clindamycin or
Some:
infection spreads • Hyaluronic acid itis can result if most in children Amoxicillin
Streptococcus
to the lymph • Pyrogenic toxins infection • Erysipelas can Erysipelas: Penicillin
pyogenes coccus nodes spreads to the also occur in the Prevention
Erysipelas arranged in kidneys elderly Proper hygiene and
chains cleanliness
• Most cases are
caused by S.
pyogenes
Diagnosis
• Various
Early diagnosis is difficult
enzymes • S. pyogenes enters through breaks in
because symptoms are
Necrotizing Streptococcus facilitate the skin
+ nonspecific
fasciitis pyogenes invasion of • Usually spread person-to-person
Treatment
tissues
Clindamycin and Penicillin
• Exotoxin A and
Prevention
streptolysin S
damage cells
and tissues
• Diagnosed by visual
• Propionibacteria examination of the skin
are normal • Treated with antimicrobial
Rod- microbiota drugs and drugs that cause
Propionibacterium
Acne + shaped • Typically begins in exfoliation of dead skin cells
acnes
diptheroids adolescence but • Accutane is used to treat
can occur later in severe acne
life • Ultraviolet light is also used
to destroy bacteria
Cat Scratch Bartonella • Fever, malaise, • Endotoxin is the • Transmitted by cat bites or scratches Diagnosed with serological
- bacillus
Disease henselae localized swelling primary and by blood-sucking arthropods testing
at infection site virulence factor Antimicrobials: Rifampin,
Ciprofloxacin, Gentamicin
• Infection can Diagnosis can be difficult
occur in burn • Pyocyanin discoloration
victims indicates massive
• Found in soil, • Bacteria grow infection
• P. aeruginosa is
decaying under the • Treatment is difficult
• Blood infection inhabitant of
matter, moist surface of the because of multi-drug
causes fever, water and soil
environments burn resistance of P.
chills, and shock • Bacterium rarely
• VF: Fimbriae, • The bacteria aeruginosa;
Aerobic; • Blue-green color part of the
Pseudomonas Pseudomonas adhesins, kills cells, Simultaneous use of
- rod-shaped from the bacterial human
Infection aeruginosa capsule, toxins, destroys tissue, Penicillin and
bacterium pigment, microbiota
enzymes and triggers Aminoglycoside
pyocyanin, occurs • Can infect almost
• Rarely causes shock • P. aeruginosa is
in massive any organ or
disease despite • Debridement widespread, but
infections system once in
virulence of burn is infections typically don't
body
factors required for occur in healthy
topical individuals
antimicrobials
to be effective
Diagnosis
• R. rickettsii serological testing
• Nonitchy spotted • Rickettsias do does not Treatment
rash on trunk and not use glucose secrete any Severe: Rocky Mountain S.F.
• Transmitted via
Spotted Fever Intracellular appendages as a nutrient toxins Doxycycline/Chlorampheni
Rickettsia rickettsii - bite of infected
Rickettsiosis parasite • Organ failure can • Pathogen • Disease occurs col
tick
occur in severe avoids digestion from damage Prevention
cases in phagosome to blood use of tick repellents and
vessels avoidance of tick-infested
areas
Treatment
endospore- Characterized by Ciprofloxacin and
Cutaneous forming; an eschar postinfection immunization
Bacillus anthrasis + Prevention
Anthrax rod-shaped • Black, painless
bacterium ulcer control of the disease in
animals
Endospore- Death of muscle and • C. perfringens is Diagnosis
Clostridium - forming connective tissue most often Apperance
species bacilli • Blackening of isolated • Traumatic event must introduce Treatment
Gas gangrene Most isolated: rod- infected muscle • Bacterial endospores into dead tissue Rapid treatment is crucial
Clostridium shaped, and skin endospores • Mortality rate exceeds 40% • Surgical removal of
+
perfringens anaerobic, • Presence of gas survive harsh dead tissue
spore- bubbles conditions • Administration of
forming • Vegetative cells antitoxin and large
secrete 11 doses of intravenous
toxins Penicillin and
Clindamycin
Prevention
• proper cleaning of
wounds
Smallpox infection
Poxviruses are DNA occurs by • Variola virus
viruses inhalation of virus stocks are
• Produce various • Viruses spread maintained in U.S.
• Treatment requires
Diseases progress proteins that from the and Russian labs
immediate vaccination
Poxviruses through a series of interfere with the respiratory tract for research
• Vaccination discontinued
stages immune response throughout the • Monkeypox cases
in 1980s
• Orthopoxvirus body have increased
(variola virus) • Other poxviruses over the past
causes smallpox are spread by decade
direct contact
Orthopox virus Immunity: Cow pox virus
Smallpox
(variola) (vaccinia)
Diagnosis
Presence: lesions
• Spread between
Slow-spreading skin Immunoassay reveals
• Painful lesions mucous membranes
lesions presence of viral antigens
caused by of mouth and
• Herpetic Treatment
Produce various inflammation and genitals
Herpes Herpes virus 1 and gingivostomatitis, Acyclovir or its derivatives
proteins that act as cell death • Herpes infections in
infection 2 whitlow, herpes help control the disease but
virulence factors • Fusion of adults are not life
gladiatorum do not cure it
infected cells threatening
• Recurrence of Prevention
forms syncytia • Neonatal infections
lesions is common Health care workers can
can be fatal
wear gloves to limit
exposure
Diagnosis: observation
• Warts develop
• Transmitted via Treatment
• Benign epithelial several month
direct contact • Various techniques to
growths on the after infection
and fomites remove warts
skin or mucous Some strains trigger • Most warts are
• Individuals can • New warts can develop
Warts Papillomavirus membranes oncogenes in host harmless
spread viruses as a result of latent
• Can form on chromosome • Papillomavirus
among locations viruses
many body es may
on their own • Covered warts usually
surfaces precipitate
body diappear within 2
some cancers
months
• Highly contagious • Infection spreads Diagnosis
infectious disease from the characteristic lesions
• Characterized by respiratory tract to • Chickenpox occurs Treatment
lesions on the back the skin via blood mostly in children No treatment; Relief:
Chickenpox and trunk that spread and lymph • VZV infected 90% of Acetaminophen and
across body • Infected dermal children prior to antihistamines
• Virus becomes cells cause immunization Prevention
latent within sensory characteristic rash • Disease is more Vaccine available against
Varicella-zoster
nerves of chickenpox severe in adults chickenpox
virus (VZV)
• Occurs following • Chickenpox is • ~20% of people
reactivation of the usually a mild who have had
virus disease chickenpox develop
• Lesions are localized • Virus becomes shingles
Shingles Oral acyclovir
to skin along an latent in nerve • Risk of shingles
infected nerve ganglia increases with age
• Pain may last after • Reactivated VZV
lesions have healed causes shingles
• Infection spreads
from the
• Children develop a
respiratory tract
mild rash
throughout the Diagnosis
• Adults may develop
body via the observation of rash and
arthritis and • Spread by
Rubella virus blood serological testing
Rubella encephalitis respiratory secretions
(rubivirus) • The immune Treatment
• Congenital infection • Infects only humans
response to Prevention
can result in birth
infected cells Vaccination
defects or death of
contributes to the
fetus
disease severity in
adults
• Measles is highly Diagnosis
• Immune contagious based on signs of measles
• Characterized by response to • Spread via Treatment
• Adhesion and
Koplik's spots infected cells respiratory droplets Treatment involves
Measles Measles virus fusion proteins help
• Subacute sclerosing causes most • Humans are the administration of vitamin A,
(Rubeola) (morbillivirus) virus avoid immune
panencephalitis is rare symptoms only host antibodies against measles,
recognition
complication • Disease can be • Vaccination has and ribavirin;
fatal in children reduced spread of Prevention
the disease MMR vaccine
• Also referred to as fifth disease
Erythema B19 virus
• Respiratory disease that manifests as a rash
infectiosum (erythovirus)
• Adults may also develop anemia and joint pain
Human Herpes • Endemic disease of children
Roseola
Virus 6 • Characterized by a rose-colored rash
Mycoses of the Hair, Nails, and Skin • Subcutaneous • Hypo- or hyperpigmented patches of scaly skin
• In the hypodermis and muscles • Pathogens and virulence factors
• Mycoses are diseases caused by fungi • Caused by Malassezia furfur
• Systemic
• Most are opportunistic pathogens • Normal inhabitant of human skin
• Affect numerous systems
• Mycoses are classified by infection Wound Mycoses
location Superficial Mycoses
• Superficial • Some fungi grow in deep tissues but do
• Most common fungal infections
• Occur on the outer surfaces • Occur on the hair, nails, and outer skin layers not become systemic
• Cutaneous • Signs and symptoms • Fungi eventually grow into the epidermis
• Occur in the skin • Pityriasis versicolor to produce skin lesions
MYCOSES OF THE HAIR, NAILS, AND SKIN
Causative agent/ Pathogenesis Epidemiology Diagnosis, treatment, and Notes
Mycoses
Bacteria prevention
Diagnosis
Infected skin is pale green under
ultraviolet light
• Fungi produce keratinase, which dissolves keratin
microscopic examination
• Fungi are often transmitted via shared hair brushes
Superficial Mycoses Malassezia furfur Treatment
and combs
Topical: Ciclopirox
• Disease occurs most often in adolescents
Antifungal imidazole:
Ketoconazole shampoos
Prevention
Diagnosis
• Dermatophytes are among
• Dermatophytes • Clinical observation
the few contagious fungi Dermatophytoses
colonize skin, • KOH preparation of skin or nail
3 genera cause most • Dermatophytes classified by • Cutaneous lesions caused by
nails, and hair samples confirms diagnosis
dermatophytoses natural habitat some fungi that grow in the
• Use keratin as Treatment
• Microsporum o Anthropophilic: skin
Cutaneous Mycoses nutrient source • Topical: Terbinafine (1-4 weeks)
• Trichophyton associated with • Caused by dermatophytes
• Infection is rare • Chronic cases: Griseofulvin
• Epidermophyton humans • Cell-mediated immune
• Fungi must • Limited infections treated with
floccosum o Zoophilic: associated responses damage deeper
invade living topical agents
with animals tissues
layers of skin • Widespread infections treated
o Geophilic: soil fungi
with oral drugs
Wound Mycoses
four species of Diagnosis • Painless lesions form that
Chromoblastomycosis ascomycete fungi: Presence of golden brown bodies progressively worsen
• Fonsecaea in skin sample • People who work barefoot in
pedrosoi Treatment the soil are at risk
• F. compacta removal of infected tissues and
• Phialophora administration of antifungal drugs
verrucosa Prevention
• Cladophialophora Wearing shoes reduces number of
carrionii infections
Diagnosis
by observation of hyphae in skin
sample, biopsy material, or
• Acquired when spores enter wounds
over 30 genera of cerebrospinal fluid Disease is permanently
Phaeohyphomycosis • Disease is variable in presentation
fungi Treatment destructive to tissues
• Depends on site of fungal colonization
treated with itraconazole
Prevention
Diagnosis • Pricks and scrapes introduce
based on symptoms and presence fungi into people
of fungi in clinical samples • People who work barefoot in
some genera of soil Treatment soil most at riskT
Mycetomas
fungi surgical removal of mycetoma • umorlike lesions form on skin,
and antifungal therapy fascia, and bones
Prevention • Infections are prevalent in
countries near the equator
• Pricks and splinters introduce
fungi into humans
Diagnosis
• Occurs most often in
based on patient's history, clinical
gardeners and farmers
signs, and observation of fungi in
• Subcutaneous infection
clinical samples
usually limited to the arms
Treatment
Sporotrichosis Sporothrix schenckii and legs
Cutaneous lesions are treated with
• Fixed sporotrichosis remains
antifungal drugs
localized
Prevention
• Lymphocutaneous
wearing proper attire to avoid
sporotrichosis occurs when
inoculation of the fungus
the fungus enters the
lymphatic system
PARASITIC INFESTATIONS OF THE SKIN
Causative agent/ Signs and Pathogen and virulence factors Pathogenesis and Diagnosis, treatment, and
Disease symptoms prevention
Bacteria epidemiology
Cutaneous • Infected macrophages Diagnosis
• Produces • Protozoan transmitted by stimulate inflammatory microscopic identification of the
Leishmaniasis Leishmania
large, painless female sand flies responses protozoa
skin lesions • Leishmaniasis is endemic in Treatment
Mucocutaneous parts of the tropics and Antimicrobials are needed for
• Skin lesions subtropics severe infections
enlarge to Prevention
encompass reducing exposure to the
mucous reservoir host
membranes
Visceral
• Parasite is
spread by
macrophages
throughout
body
• Characterized
by intense Diagnosis
itching and observing mites, eggs, or fecal
rash at matter in skin samples or the
• Itching blisters occur where
infection site • The mite Sarcoptes scabiei is characteristic burrows
female mites lay eggs
• Lesions the causative agent Treatment
• Mites transmitted via
Scabies Sarcoptes scabiei common • Inflammation and damage to Treated with mite-killing lotions
prolonged body contact
between the nerve endings occur as the and cleaning of contaminated
• Epidemics occur in crowded
fingers, around mites burrow items
conditions
the genitalia, Prevention
and on the good personal hygiene
wrists, elbows,
and knees
You might also like
- L96 - Patna Lab II R K Estate (Opp. Igims Gate), Rajabazar PATNA-14 # 7632995990 & 0612-2295550 PatnaDocument3 pagesL96 - Patna Lab II R K Estate (Opp. Igims Gate), Rajabazar PATNA-14 # 7632995990 & 0612-2295550 PatnaAnkit AnandNo ratings yet
- Microbiology and Parasitology ReviewerDocument4 pagesMicrobiology and Parasitology ReviewerChrister Jon AcostaNo ratings yet
- Clinical Microbiology QuestionsDocument18 pagesClinical Microbiology QuestionsArianne Joy C. TamarayNo ratings yet
- Duffy - MalingeringDocument57 pagesDuffy - MalingeringNia Midford100% (1)
- 3.5 PHARMA ANTI MYCOBACTERIAL AGENTSpdfDocument18 pages3.5 PHARMA ANTI MYCOBACTERIAL AGENTSpdfJanet SantosNo ratings yet
- Digestive System Diseases TableDocument9 pagesDigestive System Diseases TableGRACE MAR CABAHUGNo ratings yet
- Fungal Infections of The Skin: by Bekele T. (BSC, MSC) 1Document109 pagesFungal Infections of The Skin: by Bekele T. (BSC, MSC) 1desuloveNo ratings yet
- Gram Negative Rods of Enteric TractDocument2 pagesGram Negative Rods of Enteric TractJohn TerryNo ratings yet
- Nematodes & Infections of The SkinDocument39 pagesNematodes & Infections of The SkinHannah LaputNo ratings yet
- Bacterial Cell StructureDocument6 pagesBacterial Cell StructureCasey StuartNo ratings yet
- Fungal InfectionsDocument42 pagesFungal InfectionsleenaloveuNo ratings yet
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterDocument4 pagesLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoNo ratings yet
- University of Santo Tomas Faculty of Pharmacy - Department of Medical TechnologyDocument5 pagesUniversity of Santo Tomas Faculty of Pharmacy - Department of Medical TechnologyWynlor AbarcaNo ratings yet
- Lecture 10 AutoimmunityDocument78 pagesLecture 10 AutoimmunitytimcarasNo ratings yet
- Superficial and Cutaneous MycosesDocument34 pagesSuperficial and Cutaneous MycosesPrincewill Seiyefa100% (1)
- MycosesDocument28 pagesMycosesAiman TymerNo ratings yet
- Clinpath - : Red Blood CellsDocument14 pagesClinpath - : Red Blood CellsYolanda Primrosa NurhanNo ratings yet
- Ricketsiae BacteriaDocument2 pagesRicketsiae BacteriaErnie G. Bautista II, RN, MDNo ratings yet
- Classification of Fungal InfectionsDocument26 pagesClassification of Fungal Infectionstev26100% (1)
- Gram Positive Cocci Sem 1 1Document45 pagesGram Positive Cocci Sem 1 1Charmaine Corpuz Granil100% (1)
- Chemical Examination of UrineDocument7 pagesChemical Examination of UrineStephen YorNo ratings yet
- ReviewersDocument1 pageReviewersRalph Renon CasamayorNo ratings yet
- LALA Megatable DermaDocument39 pagesLALA Megatable DermaJorelle MarquezNo ratings yet
- Medical MycologyDocument1 pageMedical MycologyHairul AnuarNo ratings yet
- Dermatology: Steps of Skin ExamDocument10 pagesDermatology: Steps of Skin Examtrina santiagoNo ratings yet
- MP 11 Cestodes NewDocument46 pagesMP 11 Cestodes NewGenelyn Marquez100% (1)
- Ex4 Frog EmbryoDocument20 pagesEx4 Frog EmbryoJan Leightton Laxamana100% (2)
- A. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusDocument8 pagesA. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusRuel MaddawinNo ratings yet
- Diagnostic Microbiology: CampylobacterDocument25 pagesDiagnostic Microbiology: Campylobacteranon_914901469No ratings yet
- Chapter 7 - NeoplasiaDocument23 pagesChapter 7 - NeoplasiaAgnieszka WisniewskaNo ratings yet
- MB Virology 5 & 6 HerpesvirusesDocument7 pagesMB Virology 5 & 6 HerpesvirusesUsman Ali AkbarNo ratings yet
- Bacterial and Viral GeneticsDocument52 pagesBacterial and Viral GeneticsPradeep Tomar100% (1)
- Pathogenesis of Bacterial InfectionDocument15 pagesPathogenesis of Bacterial InfectionMichaelJJordan100% (1)
- Microbiology - Bacteria Summary (Updated)Document26 pagesMicrobiology - Bacteria Summary (Updated)moZZeltovNo ratings yet
- Haemophilus SPPDocument109 pagesHaemophilus SPPJamie CañebaNo ratings yet
- Patient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansDocument21 pagesPatient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansMark Vincent JanoyogNo ratings yet
- Topic Outline: Elements of Parasitology (3P's) Types of Association of Living OrganismsDocument6 pagesTopic Outline: Elements of Parasitology (3P's) Types of Association of Living OrganismsJhunrick Corpuz TumpalanNo ratings yet
- Cervical Pathology 4Document104 pagesCervical Pathology 4Arie PratamaNo ratings yet
- (OS 217 - IDS) LEC 04 Diagnostic MycologyDocument6 pages(OS 217 - IDS) LEC 04 Diagnostic MycologyErtyWitalayaL.ToruanNo ratings yet
- 3 SEMR421 Bacteriology Part 3Document14 pages3 SEMR421 Bacteriology Part 3Micah Daniel TapiaNo ratings yet
- Valvular Heart Diseases Part 2 - Dr. BartolomeDocument9 pagesValvular Heart Diseases Part 2 - Dr. BartolomeMedisina101No ratings yet
- Micro para Questions 2004 2005Document6 pagesMicro para Questions 2004 2005DonnaBells Hermo LabaniegoNo ratings yet
- Mnemonic Normal Body FloraDocument2 pagesMnemonic Normal Body FloraZakir RashidNo ratings yet
- Different Types of HazardsDocument4 pagesDifferent Types of HazardsGNiqM100% (1)
- LesionsDocument16 pagesLesionsKevin NelsonNo ratings yet
- 11 Parasitology - Phasmids 4Document4 pages11 Parasitology - Phasmids 4maqmmNo ratings yet
- Mycobacteria: Nocardia, Rhodococcus, Tsukamurella and GordoniaDocument7 pagesMycobacteria: Nocardia, Rhodococcus, Tsukamurella and Gordonia20C – Gorospe, Rhai Chezka V.No ratings yet
- Ankur Vashishtha S Ubharti University MeerutDocument34 pagesAnkur Vashishtha S Ubharti University MeerutKana FajarNo ratings yet
- Micro-Para Practical Exam ReviewerDocument8 pagesMicro-Para Practical Exam ReviewerRA TranceNo ratings yet
- Psoriasis: Risk FactorsDocument9 pagesPsoriasis: Risk FactorsJohn Michael TaylanNo ratings yet
- MicrobiologyDocument49 pagesMicrobiologyinnyNo ratings yet
- Parasitology Lecture AmoebaDocument106 pagesParasitology Lecture AmoebaShanu KumariNo ratings yet
- Dracunculus MedinensisDocument1 pageDracunculus MedinensisEm KayNo ratings yet
- MalariaDocument5 pagesMalariaJessica Febrina WuisanNo ratings yet
- My Co BacteriumDocument15 pagesMy Co BacteriumPatrickNo ratings yet
- Mtap - Bacteriology FinalsDocument6 pagesMtap - Bacteriology FinalsMoira Pauline LibroraniaNo ratings yet
- Immuno SeroDocument80 pagesImmuno SeroDocAxi Maximo Jr AxibalNo ratings yet
- Is CompilationDocument75 pagesIs CompilationSophia AngNo ratings yet
- Mycology Bacteria Inducing Diseases NotesDocument5 pagesMycology Bacteria Inducing Diseases NotesEddy S.R.A/Eddy SaputraNo ratings yet
- NCM 112 Prefinal LectureDocument11 pagesNCM 112 Prefinal LectureRheeanne AmilasanNo ratings yet
- Normal Flora, Bacteria, and DiseaseDocument8 pagesNormal Flora, Bacteria, and DiseaseDeepbluexNo ratings yet
- A Fact A Day Wound Infection ManagementDocument2 pagesA Fact A Day Wound Infection ManagementSakti WNo ratings yet
- Chapter 18 CarbohydratesDocument136 pagesChapter 18 CarbohydratesGRACE MAR CABAHUG50% (2)
- LEC - 5 - Complexation and Protein BindingDocument50 pagesLEC - 5 - Complexation and Protein BindingGRACE MAR CABAHUGNo ratings yet
- Problem Set 2Document3 pagesProblem Set 2GRACE MAR CABAHUGNo ratings yet
- Digestive System Diseases TableDocument9 pagesDigestive System Diseases TableGRACE MAR CABAHUGNo ratings yet
- DDS Glycerin Supp PostlabDocument33 pagesDDS Glycerin Supp PostlabGRACE MAR CABAHUGNo ratings yet
- WHO 5th Edition Classification 2023Document57 pagesWHO 5th Edition Classification 2023mohamaed abbasNo ratings yet
- Filarial Nematodes: Wuchereria BancroftiDocument8 pagesFilarial Nematodes: Wuchereria BancroftiMegumi TadokoroNo ratings yet
- Quality Indicators in Blood BankDocument11 pagesQuality Indicators in Blood BankDr KalyanNo ratings yet
- The Use of Lipo-Flavonoid in The Management of TinnitusDocument16 pagesThe Use of Lipo-Flavonoid in The Management of TinnitusChristine JoyceNo ratings yet
- Ernest A Codman Patien Safety en MBEDocument2 pagesErnest A Codman Patien Safety en MBEClaudio M Cruz FierroNo ratings yet
- Drug-Study Hepa BDocument2 pagesDrug-Study Hepa BPauline Doronila100% (1)
- Solution Manual For Abnormal Psychology 18th Edition Jill M Hooley Matthew Nock James ButcherDocument29 pagesSolution Manual For Abnormal Psychology 18th Edition Jill M Hooley Matthew Nock James ButcherEricOrtegaizna98% (43)
- Laughter Is The Best Medicine - Docx Version 1Document2 pagesLaughter Is The Best Medicine - Docx Version 1Khelif AhmedNo ratings yet
- RAD 1015A Final Study GuideDocument4 pagesRAD 1015A Final Study GuideHelpGrowNo ratings yet
- 9577Document4 pages9577Kristina DewiNo ratings yet
- All About DiabetesDocument9 pagesAll About DiabetesArslan TariqNo ratings yet
- Cervical Cancer Thesis PDFDocument5 pagesCervical Cancer Thesis PDFWriteMyPersuasivePaperCanada100% (1)
- 356-Article Text-1309-1-10-20180924Document10 pages356-Article Text-1309-1-10-20180924wildan yogaNo ratings yet
- By I&C President Ryan Witt by I&C President Ryan WittDocument29 pagesBy I&C President Ryan Witt by I&C President Ryan WittryanwittNo ratings yet
- Intermittant Claudication FlowchartDocument2 pagesIntermittant Claudication FlowchartsilkofosNo ratings yet
- Earth Essence CBD GummiesDocument6 pagesEarth Essence CBD GummiesketsaadanNo ratings yet
- BariumDocument58 pagesBariummahammad makadaNo ratings yet
- Pedia Chapter 20Document22 pagesPedia Chapter 20CABARO NHORENo ratings yet
- Penelitian Epidemiologi Untuk Program Pencegahan Kanker ServiksDocument73 pagesPenelitian Epidemiologi Untuk Program Pencegahan Kanker ServiksIndonesian Journal of Cancer100% (1)
- 1515ec-1516ec-1517ec 2018-04Document74 pages1515ec-1516ec-1517ec 2018-04Pranish PradhanNo ratings yet
- Jurnal NeonatusDocument41 pagesJurnal NeonatusDesmiyati AdoeNo ratings yet
- PDF - How To Manage An Agitated Patient PDFDocument9 pagesPDF - How To Manage An Agitated Patient PDFAlexandr SocrovisciucNo ratings yet
- Female CondomsDocument2 pagesFemale Condomsapi-507694117No ratings yet
- CHAPTER 3: Toxic Effects of Drugs: Pharmacology Page 1Document1 pageCHAPTER 3: Toxic Effects of Drugs: Pharmacology Page 1Gabriel GonzagaNo ratings yet
- Asthma PhenotypesDocument55 pagesAsthma PhenotypesAnonymous so6ZnlKywNo ratings yet
- DTC3Document17 pagesDTC3camilaaedovNo ratings yet
- During The Holiday Weekend Second Home-Owners Are Allowed in Tahoe Tourists Are Still Not Allowed at This Time FINALDocument2 pagesDuring The Holiday Weekend Second Home-Owners Are Allowed in Tahoe Tourists Are Still Not Allowed at This Time FINALFOX40 NewsNo ratings yet
- PP Slides Ch19Document8 pagesPP Slides Ch19Jean SurigaoNo ratings yet