Professional Documents
Culture Documents
Diagnostic Accuracy of The Urinalysis For Urinary Tract Infections in Infants Less Than 3 Months of Age
Diagnostic Accuracy of The Urinalysis For Urinary Tract Infections in Infants Less Than 3 Months of Age
Uploaded by
Ivan DanindraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnostic Accuracy of The Urinalysis For Urinary Tract Infections in Infants Less Than 3 Months of Age
Diagnostic Accuracy of The Urinalysis For Urinary Tract Infections in Infants Less Than 3 Months of Age
Uploaded by
Ivan DanindraCopyright:
Available Formats
Diagnostic Accuracy of the Urinalysis
for Urinary Tract Infection in Infants
,3 Months of Age
Alan R. Schroeder, MDa, Pearl W. Chang, MDb, Mark W. Shen, MDc, Eric A. Biondi, MDd, Tara L. Greenhow, MDb
BACKGROUND:The 2011 American Academy of Pediatrics urinary tract infection (UTI) guideline abstract
suggests incorporation of a positive urinalysis (UA) into the definition of UTI. However,
concerns linger over UA sensitivity in young infants. Infants with the same pathogenic
organism in the blood and urine (bacteremic UTI) have true infections and represent
a desirable population for examination of UA sensitivity.
METHODS:We collected UA results on a cross-sectional sample of 276 infants ,3 months of
age with bacteremic UTI from 11 hospital systems. Sensitivity was calculated on infants
who had at least a partial UA performed and had $50 000 colony-forming units per milliliter
from the urine culture. Specificity was determined by using a random sample of infants
from the central study site with negative urine cultures.
The final sample included 245 infants with bacteremic UTI and 115 infants with
RESULTS:
negative urine cultures. The sensitivity of leukocyte esterase was 97.6% (95% confidence
interval [CI] 94.5%–99.2%) and of pyuria (.3 white blood cells/high-power field) was 96%
(95% CI 92.5%–98.1%). Only 1 infant with bacteremic UTI (Group B Streptococcus) and
a complete UA had an entirely negative UA. In infants with negative urine cultures, leukocyte
esterase specificity was 93.9% (95% CI 87.9 – 97.5) and of pyuria was 91.3% (84.6%–95.6%).
CONCLUSIONS:In young infants with bacteremic UTI, UA sensitivity is higher than previous
reports in infants with UTI in general. This finding can be explained by spectrum bias or by
inclusion of faulty gold standards (contaminants or asymptomatic bacteriuria) in previous
studies.
a
Department of Pediatrics, Santa Clara Valley Medical Center, San Jose, California; bDepartment of Pediatrics, WHAT’S KNOWN ON THIS SUBJECT: The
Kaiser Permanente Northern California, Oakland, California; cDepartment of Pediatrics, Dell Children’s Medical
Center, Austin, Texas; and dDepartment of Pediatrics, University of Rochester, Rochester, New York sensitivity of the urinalysis (UA) traditionally has
been considered suboptimal in young infants.
Dr Schroeder conceptualized and designed the initial study, coordinated data collection from all of
the sites, carried out the analysis and interpretation of data, and drafted the manuscript; Drs Shen, Whether the finding of a negative UA and
Chang, and Greenhow conceptualized and designed the initial study, coordinated or co-coordinated a positive urine culture represents a false-
data collection at each of their respective sites, and reviewed and revised the manuscript; negative UA versus a false-positive urine culture
Dr Biondi coordinated data collection for all of the participating Pediatric Research in the Inpatient
remains unclear.
Setting sites, and reviewed and revised the manuscript; and all authors approved the final
manuscript as submitted. WHAT THIS STUDY ADDS: In infants ,3 months
www.pediatrics.org/cgi/doi/10.1542/peds.2015-0012 with bacteremic urinary tract infection,
DOI: 10.1542/peds.2015-0012 a condition that represents true infection, the UA
Accepted for publication Mar 2, 2015 sensitivity is higher than previously reported for
Address correspondence to Alan R. Schroeder, MD, Department of Pediatrics, Santa Clara Valley urinary tract infection in general, suggesting that
Medical Center, 751 S. Bascom Ave, San Jose, CA 95128. E-mail: Alan.Schroeder@hhs.sccgov.org. the UA is reliable even in young infants.
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2015 by the American Academy of Pediatrics
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
PEDIATRICS Volume 135, number 6, June 2015 ARTICLE
All sites had existing databases that differed from that used in this study,
The sensitivity of the urinalysis (UA)
included infants with bacteremic UTI. placement was determined by the
for the diagnosis of urinary tract
Each site obtained additional middle value in the reported range.
infection (UTI) in children generally
independent institutional review For example, 11–25 WBC/HPF was
has been reported to be 75% to
board approval for this study. placed in the 11–20 category and 3–5
85%.1–6 Because of this suboptimal
Informed consent was waived. WBC/HPF was placed in the 4–10
sensitivity, the urine culture is
category. The exceptions were 5
considered to be the gold standard Subjects patients with a result of 2–5 WBC/
for the diagnosis of UTI. However, the
Infants were included if they were HPF, which represented the second
findings of a positive urine culture in
a patient with a negative UA also may ,3 months of age and had the same lowest category for the reporting
pathogenic organism isolated from laboratory (0–1 WBC/HPF was the
reflect a false-positive urine culture
blood and urine. The primary aim of lowest). These results were placed in
due to asymptomatic bacteriuria or
the initial investigation was to the 4–10 WBC/HPF category.
contamination.7–10 The 2011
examine parenteral antibiotic Categories were also created for urine
American Academy of Pediatrics’
duration and outcomes. Therefore, culture CFU/mL (,10 000, 10–25
(AAP) UTI guideline suggests that the
diagnosis of UTI should require an infants were excluded if they had 000, 25–50 000, 50–100 000 and
abnormal UA in addition to a positive major comorbidities (defined as .100 000). Three infants had culture
urine culture.4 However, these neuromuscular conditions such as reports of 10 000–100 000 CFU/mL.
guidelines do not include infants spina bifida, previous urologic These results were placed in the
,2 months, and young infants with surgery other than circumcision, or 50 000–100 000 category.
a negative UA and a positive urine immunodeficiency), if they were The AAP recommendation to include
culture are generally considered to managed in the ICU, or if they had the UA to establish the diagnosis of
have UTI.11–13 indwelling urinary or central venous UTI suggests using pyuria and/or
catheters at the time the cultures bacteriuria. The suggested threshold
Bacteremic UTI represent a unique were drawn. For this secondary
and desirable condition in which to for pyuria is 5 WBC/HPF, but there is
analysis, infants were excluded if no no quantitative recommendation for
assess the sensitivity of the UA. UA was performed or if the urine
Infection with the same organism in bacteriuria. We therefore created 2
culture grew ,50 000 colony- definitions of a positive UA by using
the blood and urine renders forming units/milliliter (CFU/mL),
contamination or asymptomatic AAP criteria: (1) pyuria (.3 WBC/
the AAP threshold for UTI.4 However, HPF) and/or any bacteriuria on the
bacteriuria extremely unlikely, UA findings from this subgroup are
thereby minimizing the probability UA and (2) pyuria (.10 WBC/HPF)
presented. and/or any bacteriuria on the UA.
that the urine culture represents
a false positive. Data Collection and Variables The primary objective of the study
The aim of this study was to calculate was to assess the sensitivity of the UA
Bacteremic UTIs at each site were
the sensitivity of the UA in in this sample of infants with
originally identified by using existing
a multicenter sample of infants bacteremic UTI. However, to better
microbiology databases. Site
,3 months with bacteremic UTI. UA interpret the sensitivity of differing
investigators reviewed charts by
specificity was calculated by using thresholds of the various components
using a protocol specifically designed
a separate sample of similar-aged of the UA, we also assembled
for this study. Data on specific
infants with negative urine cultures. a sample of 115 similarly aged infants
components of the UA (white blood
with negative urine cultures to
cells/high-power field [WBC/HPF],
calculate UA specificity. These infants
METHODS bacteria, nitrites, leukocyte esterase
were randomly selected (1 in every
[LE]) were collected for each infant.
Setting 10 infants) from a microbiology
To avoid verification bias, infants
database at the central site of ∼1200
A multicenter database of infants with partial UA results were included.
infants ,90 days who underwent
,3 months with bacteremic UTI was Given that the terminology of UA
a workup for serious bacterial
assembled to analyze management results varied by hospital, we created
infection between 2005 and 2010.14
and outcomes for this condition. This a uniform categorization for the
investigation included 276 infants purposes of this study. For urinary Statistical calculations were
from 20 hospitals at 11 hospital WBC/HPF, the categories (0–3, 4–10, performed by using Stata 13 (Stata
systems (see Acknowledgments) 11–20, 21–50, and .50 WBC/HPF) Corp, College Station, TX). To
between 1998 and 2013. The central reflect an amalgamation of categories compare characteristics of the 2
site for the study was Santa Clara used at the participating hospitals. If samples, the Fisher’s exact test or x2
Valley Medical Center, in San Jose, CA. a UA WBC/HPF result category test were used, as appropriate, to
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
966 SCHROEDER et al
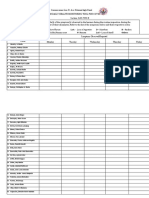
compare proportions, and the TABLE 1 Characteristics of Infants With Bacteremic UTI and Infants With Negative Urine Cultures
Wilcoxon rank sum test was used to Variable Bacteremic UTI, Negative Urine Culture, P
compare age. Given that the n = 245 n = 115
sensitivity and specificity of the UA Age, d, median (IQR) 37 (18–59) 37 (16–59) .48
were calculated in 2 separate samples Age #30 d, % 41.2 42.6 .80
of patients, likelihood ratios and Age #14 d, % 19.2 22.6 .45
predictive values would be Boys, % 60 50.4 .09
Urine collection method documented, % 75 96.5 ,.001
misleading and were not calculated, Urine collection method, if documented, % .003
and receiver operator characteristics Catheterization 98.1 91
curves were not created. Bag/clean catch 1.9 9
Organism — —
E coli 91.0
RESULTS Enterobacter spp 3.7
A total of 276 infants with bacteremic Klebsiella spp 2.5
Klebsiella+Pseudomonas 0.8
UTI were identified, from which 31 Enterococcus spp 0.8
(11%) were excluded: 12 infants had Group B Streptococcus 0.4
no UA performed and 19 infants Staphylococcus aureus 0.4
had urine cultures with ,50 000 Citrobacter 0.4
CFU/mL. Baseline characteristics of IQR, interquartile range; —, non-applicable.
the remaining 245 infants and the 115
infants with negative urine cultures 95% CI 98.5% –100%) and specificity Urine culture and UA results for the
are depicted in Table 1. For the 245 (87.8%, 95% CI 80.4%–93.2%) were 19 infants with bacteremia and urine
included infants with bacteremic UTI, both higher than those calculated culture growth ,50 000 CFU/mL are
35 had missing results for LE, 2 for by using the AAP definition of depicted in Table 4. All infants with
nitrites, 22 for WBC microscopy a positive UA (pyuria .3 WBC/HPF Escherichia coli had a positive UA but
(although WBC dipstick results were or bacteriuria), where sensitivity only 1 infant with a non–E coli
available for 13 of these infants) and was 98.3% (95% CI 95.2%–99.7%) organism had a positive UA.
45 for bacteria. Complete UA results but specificity was only 63.5%
were available for 178 infants. (54%–72.3%). An aggregate
Table 2 lists the results for the definition that included any positive DISCUSSION
various components of the UA in UA component was highly sensitive This study sheds new light on the
infants with bacteremic UTI and (99.4% in infants with complete UAs, diagnostic characteristics of the UA in
infants with negative urine cultures. 98.4% in infants with incomplete young infants. A definition of
Of the various individual UA UAs) but was less specific (60%, 95% a positive UA that includes pyuria
components, LE had the highest CI 50.4% –69%) than the aggregate of and/or positive LE was highly
sensitivity (97.6%, 95% confidence pyuria and/or LE. There was 1 infant sensitive and specific. All but 1 of 203
interval [CI] 94.5%–99.2%) and in the bacteremic group with infants with bacteremic UTI and
nitrites had the highest specificity a complete UA that was entirely recorded UA results for both LE and
(100%, 95% CI 96.8%–100%). Four negative. This infant was a 64-day old WBC/HPF were positive for 1 or both
infants with bacteremic UTI and girl who had Group B Streptococcus of these tests, and the one infant
4 infants with negative urine cultures (GBS) in the blood and urine with negative results for these
had “trace” LE. Categorizing “trace” (.100 000 CFU/mL). components was infected with an
results as negative reduced the LE UA performance did not differ organism (GBS) not commonly
sensitivity to 95.7% and increased significantly between infants # or described as a uropathogen. A
the specificity to 97.4%. For the .30 days of age (Table 3). For negative LE and the absence of pyuria
4 infants with bacteremic UTI with infants #30 days of age, all 82 who were also fairly specific (87.8%) in
“trace” LE, all 4 had bacteriuria on the had both LE and microscopy for infants with negative urine cultures.
UA, 3 had 4 to 10 WBC/HPF and WBC/HPF performed were positive UA bacteria, however, demonstrated
1 had 0 to 3 WBC/HPF. for 1 or both of these tests. UA poor specificity, suggesting that this
Table 3 reports the sensitivity and performance did not change component of the UA is not as useful
specificity of individual and aggregate significantly if infants with bag as LE or pyuria for ruling in a UTI.
UA components. Selecting an specimens were excluded: the UA There are 2 possible explanations for
aggregate definition of a positive UA sensitivity changed by ,0.5% and the near-perfect sensitivity of the UA
that includes pyuria (.3 WBC/HPF) the UA specificity changed by ,1% in infants with bacteremic UTI. One
and/or any LE, the sensitivity (99.5%, for each component of the UA. explanation is that the UA is in fact
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
PEDIATRICS Volume 135, number 6, June 2015 967
TABLE 2 Urinalysis Results in Infants With Bacteremic UTI and Infants With Negative Urine Several previous investigations
Cultures comparing clinical characteristics of
Urinalysis Component Bacteremic UTI Negative Urine Culture infants with UTI with and without
Leukocyte esterase, total n 210 115 bacteremia have demonstrated only
Negative 5 (2.4) 108 (93.9) minor or no differences between these
Trace, small, or 1+ 18 (8.6) 6 (5.2) 2 groups at presentation. In a sample
Moderate, positive, or 2+ 74 (35.2) 0 (0)
of 134 children (88 of whom were
Large or 3+ 113 (53.8) 1 (0.9)
Nitrites, total n 243 115 ,3 months) with bacteremic UTI
Negative 147 (60.5) 115 (100) matched with 134 children with UTI
Positive 96 (39.5) 0 (0) and no bacteremia, Honkinen et al16
WBC/HPF, total n 223 115 demonstrated that bacteremic patients
0–3 9 (4) 105 (91.3)
were more likely to have feeding
4–10 34 (15.3) 7 (6.1)
11–20 34 (15.3) 1 (0.9) problems (20% vs 10%, P = .02)
21–50 35 (15.7) 2 (1.7) and had higher C-reactive protein
.50 111 (49.8) 0 (0) concentrations (115 vs 76 mg/mL,
WBC, dip only, total n 13 — P , .01), but had no differences in
Negative 1 (7.7)
Small 1 (7.7)
highest temperature, duration of fever,
Moderate 6 (46.2) irritability, or serum WBC values.
Large 5 (38.5) Schnadower et al17 demonstrated
Bacteria, total n 200 115 that infants 29 to 60 days of age with
None 16 (8) 76 (66.1) UTI and bacteremia were more likely
Few, occasional, rare, small, trace, or 1+ 58 (29) 31 (37)
Moderate, present, or 2+ 60 (30) 7 (6.1) to have $1250 peripheral bands
Many or 3–4+ 66 (33) 1 (0.9) per microliter (adjusted odds ratio 3.8,
Unless otherwise noted, results are shown as n (%). —, non-applicable. 95% CI 2.3–6.2) or an absolute
neutrophil count of ,1500 cells/µL
(adjusted odds ratio 9.0, 95% CI
a highly sensitive test, and that contamination). The second
4.0–19.9) than infants with UTI and
previous reports of suboptimal UA explanation is spectrum bias:
negative blood cultures, but were
sensitivity have been flawed by screening tests are more sensitive
no more likely to appear clinically
a faulty gold standard (urine cultures when disease is severe.15
ill on presentation. Of note, the
that are positive because of Whether bacteremic UTI represents definition of UTI did not require
asymptomatic bacteriuria or a severe form of UTI is controversial. a positive UA in either of these studies.
Consequently, some of the patients
TABLE 3 Sensitivity and Specificity of Individual and Aggregate Components of the Urinalysis with nonbacteremic UTI may not
have had true UTI, which could
Urinalysis Component Sensitivitya (95% CI) Specificity (95% CI)
n = 115 account for these few reported
differences. In a prospective study
Individual components
Any LE, “trace” included 97.6 (94.5–99.2) 93.9 (87.9–97.5) by Newman et al,6 bacteremic and
Any LE, “trace” categorized as negative 95.7 (92.0–98.0) 97.4 (92.5–99.5) nonbacteremic infants ,3 months
+ for nitrites 39.5 (33.3–46) 100 (96.8–100) with UTI did not differ in clinical
Pyuria, .3 WBC/HPF 96 (92.5–98.1) 91.3 (84.6–95.6) appearance or maximum temperature.
Pyuria, .10 WBC/HPF 80.7 (74.9–85.7) 97.4 (92.6–99.5)
Finally, Hoberman et al18
Any bacteria 92 (87.3–95.4) 66.1 (56.7–74.7)
Aggregate componentsa demonstrated that patients with
Nitrites or LE, n = 209 97.6 (95.5–99.7) 93.9 (87.8–97.5) bacteremic UTI were younger than
Pyuria .3 WBC/HPF or any bacteriuria, n = 197 98.3 (95.2–99.7) 63.5 (54–72.3) those with nonbacteremic UTI, and
Pyuria .10 WBC/HPF or any bacteriuria, n = 197 97 (94.5–99.4) 65.2 (55.8–73.9) had slightly higher serum WBC
Pyuria .3 WBC/HPF or any LE, n = 203 99.5 (98.5–100) 87.8 (80.4–93.2)
findings (24.9 vs 20.3, P = .04), but
Any positive UA (pyuria $3 WBC/HPF), infants 99.4 (98.3–100) 60 (50.4–69)
with complete UA results only, n = 178 did not have significant differences in
Infants #30 d, n = 72 100 (95–199) 53.1 (38.3–67.5) highest temperature, duration of
Infants 31–92 d, n = 106 99.1 (94.9–100) 65.2 (52.4–76.5) fever before or after antibiotics, or
Any positive UA (pyuria $3 WBC/HPF), 98.4 (96.8–100) 60 (50.4–69) C-reactive protein values. Even if
entire sample, n = 245
bacteremic UTI is indeed a more
Infants # 30 d, n = 101 99 (94.6–100) 53.1 (38.3–67.5)
Infants 31–92 d, n = 144 97.9 (94–99.6) 65.2 (52.4–76.5) severe form of disease, it is reassuring
a Analyses performed for infants in whom results for each component were reported. The “n’s” refer to the denominator that the UA is highly reliable for
for the sensitivity calculations. severe UTIs.
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
968 SCHROEDER et al
TABLE 4 Urine Culture and UA Results in Infants With Bacteremia and Urine Culture Growth With still below the sensitivity found in our
,50 000 CFU/mL of the Same Organism investigation.12 Why the sensitivity
Organism n Urine Culture Growth, UA Result exceeded previous estimates in this
CFU/mL study is unclear. Like previous
,10K 10–25K 25–50K Pyuria .3 Any Any LE Any studies, however, the authors
WBC/HPF Bacteria Nitrites categorized infants with a negative
E coli 12 1 7 4 11/12 10/11a 12/12 2/12 UA and a positive urine culture as an
GBS 5 4 1 0 1/5 0/4a 0/5 0/5 initial “missed UTI.”
Enterococcus faecalis 1 1 0 0 0 ND 0 0
GAS 1 1 0 0 ND ND 0 0 We used the AAP-recommended
GAS, Group A Streptococcus; ND, not done. threshold of 50 000 CFU/mL for the
a Denominators reflect that not all infants had UA bacteria results. urine culture definition of UTI.
However, there were 19 infants in our
sample who had the same organism in
The alternative explanation for our Contaminated urine cultures are the blood and urine but ,50 000 CFU/
study findings (that the UA is indeed generally defined by growth of mL on urine culture (Table 4). All 12
highly reliable for all forms of UTI, nonpathogens or multiple organisms, of the infants with ,50 000 CFU/mL
and that previous reports of or growth of a pathogenic organism of E coli had a positive result for at
suboptimal UA sensitivity are biased with a low colony count.20 Given the least 1 component of the UA, indicating
by use of a flawed gold standard) is challenges in obtaining a clean urine that some infants with low bacterial
supported by several previous studies specimen from an infant, especially growth may have true UTIs. However,
on asymptomatic bacteriuria. a girl or an uncircumcised boy, the 7 infants with ,50 000 CFU/mL
Wettergren et al8,9 performed contaminated specimens are of non–E coli organisms had
screening bag urine cultures on 3581 common. In 1 study, 14% of urine unremarkable UAs, indicating that
asymptomatic infants at 3 separate cultures were contaminated. Age these infants may have had a primary
intervals during the first year of life, ,6 months, difficult catheterization, bacteremia with seeding into the urine.
beginning at 0.25 to 2 months. Infants and lack of circumcision were
with $50 000 CFU/mL from 2 The primary limitation of this study is
independent risk factors for
successive bag cultures underwent that spectrum bias might account for
contamination.20 Uncircumcised boys
the near-perfect sensitivity of the
suprapubic aspiration. Fifty (1.4%) of ,6 months of age had
the original cohort of 3581 infants had UA in infants with bacteremic UTI, as
a contamination rate of 43%.
growth from suprapubic aspiration discussed previously. Spectrum bias
Therefore, given that most estimates also may inflate the UA specificity,
(0.9% of girls and 2.5% of boys). Only
of UTI prevalence for a given given that the random sample had
2 of the 45 untreated infants were
condition (eg, febrile infant) rely negative urine cultures, which may
diagnosed with pyelonephritis within
exclusively on the urine culture, some represent the far end of the spectrum
2 weeks of detection of the
of these estimates may be inflated of nondisease. In addition, the urine
bacteriuria.9 Follow-up tests for renal-
due to asymptomatic bacteriuria or collection method was by bag in 4
concentrating capacity (a measure of
contamination, which in turn can infants and was not documented in
renal function) were done in 47 of 50
affect the apparent diagnostic approximately one-fourth of infants
children and were normal.8 In a study
performance of the UA. For example, in the bacteremic UTI group. Most of
by Hoberman et al,7 of 212 children
if the baseline prevalence of
,2 years of age with positive urine these undocumented cases came from
asymptomatic bacteriuria is 1% and 1 site where collection method was
cultures (.50 000 CFU/mL), 22
the reported prevalence of UTI in
patients had ,10 WBC/mm3 from an not routinely noted in the laboratory
a given population is 5%, then 20% of
enhanced UA (equivalent to ∼2 WBC/ reports, but where the standard of
the patients in that population do not care is to obtain urine by
HPF from an automated UA19).
have true UTIs, in which case even catheterization. Although bag
Dimercaptosuccinic acid scans were
a perfect screening test would not specimens have been demonstrated
performed on 15 of 22 of these
appear to have a sensitivity .80%. to have an increased risk of
patients and only 1 was positive,
and that patient had elevated In a recent study of 770 infants contamination, the fact that infants in
inflammatory markers and 8 WBC/mm3 ,90 days with UTI, the reported the bacteremic UTI group had the
on the UA. The authors concluded sensitivity of the UA dipstick (∼90%) same pathogenic organism in the
that asymptomatic bacteriuria and the combined dipstick + blood and urine lessens this concern,
was the likely explanation for microscopic analysis (∼95%) were and exclusion of infants with bag
these positive cultures without considerably higher than that specimens did not affect UA
pyuria. reported from previous studies but sensitivity. In the negative urine
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
PEDIATRICS Volume 135, number 6, June 2015 969
culture group, all of the specimens common serious bacterial infection. of this collaboration and for their
came from 1 site, which limits This diagnosis drives substantial ongoing dedication to research on
generalizability, and 9% of the interventions, including hospitalized children. We thank the
specimens were obtained by bag. hospitalization for prolonged following study collaborators who
Several studies have compared UA antibiotic therapy23 and follow-up participated in acquisition of data and
sensitivity and specificity in urinary imaging.24 Our study review of the manuscript: Michael
specimens obtained by bag versus highlights the need to further define Bendel-Stenzel, MD, Children’s
catheterization and have yielded the role of the UA in young infants Hospital and Clinics of Minnesota
mixed results, likely because of a lack with suspected UTI to minimize the (Minneapolis, MN); Clifford N. Chen,
of consistent and reliable gold possibility of harm and excessive MD, Children’s Medical Center of
standards.13,21 Although UA costs from overtreatment. Dallas (Dallas, TX); Rianna C. Evans,
specificity may be influenced slightly MD, Children’s Hospital of the King’s
by inclusion of bag specimens, CONCLUSIONS Daughters (Norfolk, VA); Jason French,
exclusion of infants with bag MD, Children’s Hospital Colorado
specimens had a very minimal impact The UA is highly sensitive in young (Denver, CO); Karen E. Jerardi, MD,
(change of ,1%) on the UA infants with bacteremic UTI. Although Cincinnati Children’s Hospital
specificity in our sample. this finding may reflect spectrum (Cincinnati, OH); Vivian Lee, MD,
bias, it is also consistent with Children’s Hospital Los Angeles (Los
Requiring a positive UA to make the previous studies, suggesting that the
diagnosis of UTI could have Angeles, CA); Matt Mischler, MD,
suboptimal sensitivity of the UA may Children’s Hospital of Illinois (Peoria,
important clinical implications. In be explained by urine culture results
a study of infants with bronchiolitis IL); Heidi Roman, MD, Santa Clara
that do not reflect true UTI. Valley Medical Center (San Jose, CA);
and fever, the risk of UTI was 1.1% if
a positive UA (using the 2011 AAP and Kelly E. Wood, MD, University of
UTI guidelines criteria) was ACKNOWLEDGMENTS Iowa Children’s Hospital (Iowa City, IA).
incorporated into the definition We thank the Pediatric Research in We thank Thomas B. Newman, MD
versus 6.1% if the definition relied on the Inpatient Setting network (http:// MPH and Kenneth B. Roberts, MD for
the urine culture alone.22 In young, www.prisnetwork.org/) for playing their review and critical appraisal of
febrile infants, UTI is the most an instrumental role in the formation this manuscript.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page 1126, and online at www.pediatrics.org/cgi/doi/10.1542/peds.2015-0884.
REFERENCES
1. Bachur R, Harper MB. Reliability of the management of the initial UTI in febrile 7. Hoberman A, Wald ER, Reynolds EA,
urinalysis for predicting urinary tract infants and children 2 to 24 months. Penchansky L, Charron M. Is urine
infections in young febrile children. Pediatrics. 2011;128(3):595–610 culture necessary to rule out urinary
Arch Pediatr Adolesc Med. 2001;155(1): 5. Shaw KN, McGowan KL, Gorelick MH, tract infection in young febrile
60–65 Schwartz JS. Screening for urinary tract children? Pediatr Infect Dis J. 1996;
2. Bonadio W, Maida G. Urinary tract infection in infants in the emergency 15(4):304–309
infection in outpatient febrile infants department: which test is best? 8. Wettergren B, Hellström M, Stokland E,
younger than 30 days of age: a 10-year Pediatrics. 1998;101(6). Available at: Jodal U. Six year follow up of infants with
evaluation. Pediatr Infect Dis J. 2014; www.pediatrics.org/cgi/content/full/101/ bacteriuria on screening. BMJ. 1990;
33(4):342–344 6/E1 301(6756):845–848
3. Hoberman A, Wald ER. Urinary tract 6. Newman TB, Bernzweig JA, Takayama JI, 9. Wettergren B, Jodal U. Spontaneous
infections in young febrile children. Finch SA, Wasserman RC, Pantell RH. clearance of asymptomatic bacteriuria
Pediatr Infect Dis J. 1997;16(1):11–17 Urine testing and urinary tract in infants. Acta Paediatr Scand. 1990;
4. Roberts KB; Subcommittee on Urinary infections in febrile infants seen in 79(3):300–304
Tract Infection, Steering Committee on office settings: the Pediatric Research 10. Roberts KB, Charney E, Sweren RJ, et al.
Quality Improvement and Management. in Office Settings’ Febrile Infant Study. Urinary tract infection in infants with
Urinary tract infection: clinical practice Arch Pediatr Adolesc Med. 2002;156(1): unexplained fever: a collaborative study.
guideline for the diagnosis and 44–54 J Pediatr. 1983;103(6):864–867
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
970 SCHROEDER et al
11. Lin DS, Huang SH, Lin CC, et al. Urinary 16. Honkinen O, Jahnukainen T, Mertsola J, specimens in febrile children. Pediatr
tract infection in febrile infants Eskola J, Ruuskanen O. Bacteremic Emerg Care. 2011;27(1):1–4
younger than eight weeks of age. urinary tract infection in children. 21. Schroeder AR, Newman TB, Wasserman
Pediatrics. 2000;105(2). Available at: Pediatr Infect Dis J. 2000;19(7): RC, Finch SA, Pantell RH. Choice of urine
www.pediatrics.org/cgi/content/full/ 630–634 collection methods for the diagnosis of
105/2/E20 17. Schnadower D, Kuppermann N, Macias urinary tract infection in young, febrile
12. Glissmeyer EW, Korgenski EK, Wilkes J, CG, et al; American Academy of infants. Arch Pediatr Adolesc Med. 2005;
et al. Dipstick screening for urinary tract Pediatrics Pediatric Emergency Medicine 159(10):915–922
infection in febrile infants. Pediatrics. Collaborative Research Committee. 22. Kaluarachchi D, Kaldas V, Roques E,
2014;133(5). Available at: www.pediatrics. Febrile infants with urinary tract Nunez R, Mendez M. Comparison of
org/cgi/content/full/133/5/e1121 infections at very low risk for adverse urinary tract infection rates among 2- to
13. McGillivray D, Mok E, Mulrooney E, events and bacteremia. Pediatrics. 2010; 12-month-old febrile infants with RSV
Kramer MS. A head-to-head comparison: 126(6):1074–1083 infections using 1999 and 2011 AAP
“clean-void” bag versus catheter 18. Hoberman A, Wald ER, Hickey RW, et al. diagnostic criteria. Clin Pediatr (Phila).
urinalysis in the diagnosis of urinary Oral versus initial intravenous therapy 2014;53(8):742–746
tract infection in young children. J for urinary tract infections in young 23. Averbuch D, Nir-Paz R, Tenenbaum A,
Pediatr. 2005;147(4):451–456 febrile children. Pediatrics. 1999;104(1 pt et al. Factors associated with bacteremia
14. Fielding-Singh V, Hong DK, Harris SJ, 1):79–86 in young infants with urinary tract
Hamilton JR, Schroeder AR. Ruling out 19. Shah AP, Cobb BT, Lower DR, et al. infection. Pediatr Infect Dis J. 2014;33(6):
bacteremia and bacterial meningitis in Enhanced versus automated urinalysis 571–575
infants less than one month of age: is 48 for screening of urinary tract infections 24. Schroeder AR, Abidari JM, Kirpekar R,
hours of hospitalization necessary? Hosp in children in the emergency et al. Impact of a more restrictive
Pediatr. 2013;3(4):355–361 department. Pediatr Infect Dis J. 2014; approach to urinary tract imaging after
15. Newman TB, Kohn MA. Evidence-Based 33(3):272–275 febrile urinary tract infection. Arch
Diagnosis. Cambridge, UK: Cambridge 20. Wingerter S, Bachur R. Risk factors for Pediatr Adolesc Med. 2011;165(11):
University Press; 2009 contamination of catheterized urine 1027–1032
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
PEDIATRICS Volume 135, number 6, June 2015 971
Diagnostic Accuracy of the Urinalysis for Urinary Tract Infection in Infants <3
Months of Age
Alan R. Schroeder, Pearl W. Chang, Mark W. Shen, Eric A. Biondi and Tara L.
Greenhow
Pediatrics 2015;135;965
DOI: 10.1542/peds.2015-0012 originally published online May 25, 2015;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/135/6/965
References This article cites 23 articles, 7 of which you can access for free at:
http://pediatrics.aappublications.org/content/135/6/965#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Evidence-Based Medicine
http://www.aappublications.org/cgi/collection/evidence-based_medic
ine_sub
Infectious Disease
http://www.aappublications.org/cgi/collection/infectious_diseases_su
b
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
Diagnostic Accuracy of the Urinalysis for Urinary Tract Infection in Infants <3
Months of Age
Alan R. Schroeder, Pearl W. Chang, Mark W. Shen, Eric A. Biondi and Tara L.
Greenhow
Pediatrics 2015;135;965
DOI: 10.1542/peds.2015-0012 originally published online May 25, 2015;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/135/6/965
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,
60007. Copyright © 2015 by the American Academy of Pediatrics. All rights reserved. Print
ISSN: 1073-0397.
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on September 17, 2019
You might also like
- Medical Emergencies in The Dental Office 6th Edition Malamed Test BankDocument2 pagesMedical Emergencies in The Dental Office 6th Edition Malamed Test BankKieranPenaNo ratings yet
- Case Study 8: Coronary Artery DiseaseDocument10 pagesCase Study 8: Coronary Artery Diseaseintrovoyz041100% (3)
- Chapter2 - Review of Related LiteratureDocument13 pagesChapter2 - Review of Related LiteratureDiana Laura Lei57% (7)
- Hepatitis A LetterDocument1 pageHepatitis A Letter10News WTSPNo ratings yet
- Peds 2023-061931Document8 pagesPeds 2023-061931Rene H. Framcisco, MDNo ratings yet
- Infection Urinaire 2019Document11 pagesInfection Urinaire 2019KhaoulapediatreNo ratings yet
- Kvitko-White Et Al-2013-Journal of Veterinary Internal MedicineDocument7 pagesKvitko-White Et Al-2013-Journal of Veterinary Internal MedicineCabinet VeterinarNo ratings yet
- Antimicrobial TutoringDocument3 pagesAntimicrobial TutoringmahapNo ratings yet
- JCM 00044-16Document7 pagesJCM 00044-16Renata PrimasariNo ratings yet
- Vesicoureteral Reflux: The RIVUR Study and The Way ForwardDocument3 pagesVesicoureteral Reflux: The RIVUR Study and The Way ForwardRohit GuptaNo ratings yet
- 1 s2.0 S1684118219301331 MainDocument9 pages1 s2.0 S1684118219301331 Mainyuwengunawan7No ratings yet
- Redefining Urinary Tract Infections by Bacterial Colony CountsDocument9 pagesRedefining Urinary Tract Infections by Bacterial Colony CountsindahdwitariNo ratings yet
- ITU e USG - Pediatrics-2014Document12 pagesITU e USG - Pediatrics-2014tfysksw6q8No ratings yet
- Articol Despre UTI in Paraplegic DogsDocument6 pagesArticol Despre UTI in Paraplegic DogsCristian FloreaNo ratings yet
- Absceso Hepático NeonatalDocument6 pagesAbsceso Hepático NeonatalNabila Peña ZapataNo ratings yet
- Pi Is 1875957219305261Document6 pagesPi Is 1875957219305261madimadi11No ratings yet
- Jurnal Anak IskDocument5 pagesJurnal Anak IskGintar Isnu WardoyoNo ratings yet
- A Controlled Study of Tuberculosis Diagnosis in HIV-Infected and Uninfected Children in PeruDocument17 pagesA Controlled Study of Tuberculosis Diagnosis in HIV-Infected and Uninfected Children in PeruEllyana PerwitasariNo ratings yet
- Clinical Therapy of UTI in Children Under The Age of Five Varies WidelyDocument21 pagesClinical Therapy of UTI in Children Under The Age of Five Varies WidelyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 611-Main Article Text (Blinded Article File) - 1200-1!10!20171212Document4 pages611-Main Article Text (Blinded Article File) - 1200-1!10!20171212Ramot Tribaya Recardo PardedeNo ratings yet
- Analysis of Clinical Characteristics and Genetic Testing in Patients With Acute Fatty Liver of Pregnancy: A Retrospective StudyDocument7 pagesAnalysis of Clinical Characteristics and Genetic Testing in Patients With Acute Fatty Liver of Pregnancy: A Retrospective StudyCharlotte FloresNo ratings yet
- Cit230 PDFDocument4 pagesCit230 PDFJoyBoyXNo ratings yet
- Lactobacillus Therapy For Acute Infectious Diarrhea in Children A Meta-AnalysisDocument9 pagesLactobacillus Therapy For Acute Infectious Diarrhea in Children A Meta-AnalysisfahrunisaNo ratings yet
- Study of Clinical Etiological and Radiological Profile of UTI CasesDocument8 pagesStudy of Clinical Etiological and Radiological Profile of UTI CasesDebabrata MohapatraNo ratings yet
- NIH Public Access: Author ManuscriptDocument12 pagesNIH Public Access: Author ManuscriptadipurnamiNo ratings yet
- Acta Paediatrica - 2014 - Velasco - Using A Urine Dipstick To Identify A Positive Urine Culture in Young Febrile Infants IsDocument6 pagesActa Paediatrica - 2014 - Velasco - Using A Urine Dipstick To Identify A Positive Urine Culture in Young Febrile Infants IsCris FischerNo ratings yet
- Ejhs2503 0251Document6 pagesEjhs2503 0251Kiti AstutiNo ratings yet
- Nefro RaizaDocument6 pagesNefro Raizadayanita1221No ratings yet
- Fazelinia Et Al 2024 Stratification of Neurogenic Bladder Risk in Spina Bifida Using The Urinary PeptidomeDocument8 pagesFazelinia Et Al 2024 Stratification of Neurogenic Bladder Risk in Spina Bifida Using The Urinary PeptidomeCarolina LindsayNo ratings yet
- Urinary Tract Infections in Neonates With Unexplained Pathological Indirect Hyperbilirubinemia: Prevalence and SignificanceDocument5 pagesUrinary Tract Infections in Neonates With Unexplained Pathological Indirect Hyperbilirubinemia: Prevalence and SignificancePutri YingNo ratings yet
- CID Evaluation of Laboratory Methods For Diagnosis of VaricellaDocument10 pagesCID Evaluation of Laboratory Methods For Diagnosis of VaricellaK3 KoordinatorNo ratings yet
- Tamborini (2016) JVIM - Bacterial Cholangitis Cholecystitis or Both in DogsDocument10 pagesTamborini (2016) JVIM - Bacterial Cholangitis Cholecystitis or Both in DogsNick GoodyNo ratings yet
- Clinical CharacteristicsDocument9 pagesClinical CharacteristicsManusama HasanNo ratings yet
- Efficacy and Safety of Fluconazole Prophylaxis in Extremely Low Birth Weight Infants: Multicenter Pre-Post Cohort StudyDocument10 pagesEfficacy and Safety of Fluconazole Prophylaxis in Extremely Low Birth Weight Infants: Multicenter Pre-Post Cohort StudyAnry UmarNo ratings yet
- Does This Child Have Appendicitis?: The Rational Clinical ExaminationDocument14 pagesDoes This Child Have Appendicitis?: The Rational Clinical ExaminationTrys RobledoNo ratings yet
- Originalresearch: ABO-incompatible Platelets Are Associated With Increased Transfusion Reaction RatesDocument9 pagesOriginalresearch: ABO-incompatible Platelets Are Associated With Increased Transfusion Reaction Ratesmy accountNo ratings yet
- Jurnal YuliaDocument8 pagesJurnal YuliaRayantiNo ratings yet
- Akbari2013 PDFDocument8 pagesAkbari2013 PDFyakoub bensaadaNo ratings yet
- Etiology and Risk Factors of Acute Gastroenteritis in A Taipei Emergency Department: Clinical Features For Bacterial GastroenteritisDocument8 pagesEtiology and Risk Factors of Acute Gastroenteritis in A Taipei Emergency Department: Clinical Features For Bacterial GastroenteritisakhmadNo ratings yet
- Diagnosis and Treatment of Urinary Tract Infections in ChildrenDocument7 pagesDiagnosis and Treatment of Urinary Tract Infections in ChildrenmahendraNo ratings yet
- The Clinical Spectrum of Chronic Diarrhea in ChildrenDocument15 pagesThe Clinical Spectrum of Chronic Diarrhea in ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Blood Culture With CAPDocument10 pagesBlood Culture With CAPKaye Antonette AntioquiaNo ratings yet
- Performance of Xpert MTB RIF and Mycobacterial.88Document7 pagesPerformance of Xpert MTB RIF and Mycobacterial.88HanifNo ratings yet
- Clinical Predictors For Etiology of Acute Diarrhea in Children in Resource-Limited SettingsDocument14 pagesClinical Predictors For Etiology of Acute Diarrhea in Children in Resource-Limited SettingsMarcell KimNo ratings yet
- Fibrinogen-to-Albumin Ratio in Neonatal SepsisDocument8 pagesFibrinogen-to-Albumin Ratio in Neonatal SepsisRojas TerrazasNo ratings yet
- 001 The Society For Fetal Urology Consensus Statement On The Evaluation and Management of Antenatal HydronephrosisDocument20 pages001 The Society For Fetal Urology Consensus Statement On The Evaluation and Management of Antenatal HydronephrosisPaola ZuluagaNo ratings yet
- Diarrea en QuimioterapiaDocument6 pagesDiarrea en QuimioterapiaPaola DiazNo ratings yet
- Recurrent UtiDocument8 pagesRecurrent UtiRick Jeyrald AbagatNo ratings yet
- 523 FullDocument9 pages523 FullRodolfo Rodriguez CamposNo ratings yet
- Nej Mo A 1511812Document10 pagesNej Mo A 1511812anggiNo ratings yet
- 2016 Article 645Document10 pages2016 Article 645Betharia TriayuNo ratings yet
- Nej Mo A 1101549Document13 pagesNej Mo A 1101549P E R L A P I N KNo ratings yet
- Journal Reading AnakDocument19 pagesJournal Reading AnakPutra Priambodo WibowoNo ratings yet
- Article À CritiquerDocument10 pagesArticle À CritiquerAs MaaNo ratings yet
- 2011 Ispad NeumoníaDocument14 pages2011 Ispad NeumoníaAaron Nureña JaraNo ratings yet
- Aubron Et Al. 2014 Infecções UrináriasDocument10 pagesAubron Et Al. 2014 Infecções UrináriasLeandro FigueiraNo ratings yet
- tpmd170465 PDFDocument5 pagestpmd170465 PDFWaradhamma MatchimaNo ratings yet
- Yield of Blood Cultures in Children Presenting With Febrile Illness in A Tertiary Care HospitalDocument5 pagesYield of Blood Cultures in Children Presenting With Febrile Illness in A Tertiary Care Hospitalfaraz.mirza1No ratings yet
- 8.5 Case AnalysisDocument4 pages8.5 Case AnalysisMichal VillanuevaNo ratings yet
- Pharmaceutical Sciences: Finding of Organisms Causing Bacteriuria in Pregnant WomenDocument4 pagesPharmaceutical Sciences: Finding of Organisms Causing Bacteriuria in Pregnant WomeniajpsNo ratings yet
- Standard Article: R. Policelli Smith, J.L. Gookin, W. Smolski, M.F. Di Cicco, M. Correa, and G.S. SeilerDocument8 pagesStandard Article: R. Policelli Smith, J.L. Gookin, W. Smolski, M.F. Di Cicco, M. Correa, and G.S. SeilerAlejandro Estrada RiosNo ratings yet
- MAKALAH Keputusasan-1Document7 pagesMAKALAH Keputusasan-1ARINANo ratings yet
- Jurnal Ebm KedkelDocument5 pagesJurnal Ebm KedkelRifki Kholis PutraNo ratings yet
- Food Protein Induced Enterocolitis (FPIES): Diagnosis and ManagementFrom EverandFood Protein Induced Enterocolitis (FPIES): Diagnosis and ManagementTerri Faye Brown-WhitehornNo ratings yet
- Baguio City News On GuidelinesDocument2 pagesBaguio City News On GuidelinesLesly BriesNo ratings yet
- Fundoscopy: Learning OutcomesDocument6 pagesFundoscopy: Learning OutcomesSaraNo ratings yet
- C3.5 (C3.4) PEP and Needle Stick InjuryDocument8 pagesC3.5 (C3.4) PEP and Needle Stick Injuryvasthare phcNo ratings yet
- Hepatitis Assignment BioDocument2 pagesHepatitis Assignment BioAthira NairNo ratings yet
- Classroom Daily Health Monitoring Tool For CovidDocument4 pagesClassroom Daily Health Monitoring Tool For CovidGenie Sina-on DadeaNo ratings yet
- Diabetic FootDocument13 pagesDiabetic FootSafoora RafeeqNo ratings yet
- Kala-Azar (Leishmaniasis) Symptoms, Signs, DiagnosisDocument36 pagesKala-Azar (Leishmaniasis) Symptoms, Signs, Diagnosisatulbd2006No ratings yet
- Preventive OphthalmologyDocument2 pagesPreventive Ophthalmologysarguss14100% (1)
- Mathematical Model For Malaria Transmission Dynamics in Human and Mosquito Populations With Nonlinear Forces of InfectionDocument32 pagesMathematical Model For Malaria Transmission Dynamics in Human and Mosquito Populations With Nonlinear Forces of InfectionAshimi Blessing AyindeNo ratings yet
- H PyloriDocument7 pagesH PyloriBBD BBDNo ratings yet
- Bishaw Assigment of GI DisorderDocument98 pagesBishaw Assigment of GI DisorderRas Siko SafoNo ratings yet
- Test Bank For Frommers Radiology For The Dental Professional 10th Edition by Stabulas Savage DownloadDocument8 pagesTest Bank For Frommers Radiology For The Dental Professional 10th Edition by Stabulas Savage Downloadchristinedaughertyrwycgtpmxj100% (27)
- PSM Test Questions (5 Uni)Document14 pagesPSM Test Questions (5 Uni)Phyo MaungNo ratings yet
- Terapi Lesi Pra-Kanker Leher Rahim (Krioterapi)Document31 pagesTerapi Lesi Pra-Kanker Leher Rahim (Krioterapi)yulia gustiNo ratings yet
- Food Poisoning & Worm InfestationDocument13 pagesFood Poisoning & Worm InfestationPujani SenevirathnaNo ratings yet
- Reflection On MCN LECDocument12 pagesReflection On MCN LECLecery Sophia WongNo ratings yet
- Hayashi Treatment GuideDocument10 pagesHayashi Treatment GuideJames Deacon100% (3)
- PSM (Must Know)Document19 pagesPSM (Must Know)PranavNo ratings yet
- 2019 Evaluation and Management of The Febrile Young Infant in The Emergency DepartmentDocument31 pages2019 Evaluation and Management of The Febrile Young Infant in The Emergency DepartmentMonica ValderramaNo ratings yet
- The Immune System Game: (A Large Group Game That Resembles "Human Chess")Document5 pagesThe Immune System Game: (A Large Group Game That Resembles "Human Chess")kiki19841984No ratings yet
- OSCE OphthalmologyDocument15 pagesOSCE OphthalmologyHuzaifa Asif100% (2)
- Filariasis: Parasitic Disease Roundworms Filarioidea Black Ies Mosquitoes HelminthiasesDocument9 pagesFilariasis: Parasitic Disease Roundworms Filarioidea Black Ies Mosquitoes Helminthiasesadandiba06No ratings yet
- Hexyon LeafletDocument49 pagesHexyon LeafletEllaNo ratings yet
- CAT Jurnal Ortho IfaDocument10 pagesCAT Jurnal Ortho Ifaahmad iffa maududyNo ratings yet
- 8258 ID Mengembangkan Evidence Based Public Health Ebph Hiv Dan Aids Berbasis SurveilansDocument8 pages8258 ID Mengembangkan Evidence Based Public Health Ebph Hiv Dan Aids Berbasis SurveilansDamiriNo ratings yet
- Presentation Brain Metastasis CancerDocument26 pagesPresentation Brain Metastasis CancerAnugrah WulanNo ratings yet