Professional Documents
Culture Documents
Fetal Distress: Brenda A. Bucklin
Fetal Distress: Brenda A. Bucklin
Uploaded by
Rizki Amalia Wahid0 ratings0% found this document useful (0 votes)
25 views1 pageAn 18-year-old pregnant woman at 27 weeks gestation presents with severe preeclampsia necessitating induction of labor. During labor, the fetal heart rate monitor shows ominous changes. Fetal distress refers to a non-specific term for fetal heart rate abnormalities that could cause harm if not addressed. The diagnosis is challenging due to limitations of heart rate monitoring. Common risk factors include preeclampsia, diabetes, and growth restriction. Sustained hypoxia can lead to acidosis, neurological issues, and death if not resolved through emergency delivery.
Original Description:
fetal distress
Original Title
Fetal distress
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAn 18-year-old pregnant woman at 27 weeks gestation presents with severe preeclampsia necessitating induction of labor. During labor, the fetal heart rate monitor shows ominous changes. Fetal distress refers to a non-specific term for fetal heart rate abnormalities that could cause harm if not addressed. The diagnosis is challenging due to limitations of heart rate monitoring. Common risk factors include preeclampsia, diabetes, and growth restriction. Sustained hypoxia can lead to acidosis, neurological issues, and death if not resolved through emergency delivery.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
25 views1 pageFetal Distress: Brenda A. Bucklin
Fetal Distress: Brenda A. Bucklin
Uploaded by
Rizki Amalia WahidAn 18-year-old pregnant woman at 27 weeks gestation presents with severe preeclampsia necessitating induction of labor. During labor, the fetal heart rate monitor shows ominous changes. Fetal distress refers to a non-specific term for fetal heart rate abnormalities that could cause harm if not addressed. The diagnosis is challenging due to limitations of heart rate monitoring. Common risk factors include preeclampsia, diabetes, and growth restriction. Sustained hypoxia can lead to acidosis, neurological issues, and death if not resolved through emergency delivery.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 1
Fetal Distress
Brenda A. Bucklin
192
Case Synopsis
An 18-year-old, 150-kg primigravida presents at 27 weeks’ gestation with severe
preeclampsia. Her worsening condition necessitates induction of labor. During uterine
contractions, the electronic fetal heart rate monitor demonstrates ominous changes
(Fig. 192-1).
devoid of accelerations, variability, and even deceleration
PROBLEM ANALYSIS Abrupt and profound decreases in fetal oxygenation ofte
result in severe fetal bradycardia, usually less than 90 beats pe
Definition minute. Ominous signs suggesting that both fetal acidosis an
Fetal distress is a widely used clinical term that is imprecise hypoxia are present include the following:
and nonspecific. In 1998 the American College of ● Loss of fetal heart rate accelerations
Obstetricians and Gynecologists (ACOG) published a com- ● Increase in baseline fetal heart rate
mittee opinion that suggested replacing the term fetal distress ● Persistent absent variability, unresponsive to stimuli
with nonreassuring fetal heart rate tracing because the former ● Absent variability with late or variable decelerations
term has a low predictive value and is frequently associated
with the delivery of infants who turn out to be in good con- The challenge for obstetricians is to judiciously conside
dition. The ACOG went on to recommend that a nonreas- the electronic information within the clinical context t
suring fetal heart rate tracing be accompanied by a further ensure the best possible neonatal outcome. Emergenc
description of the findings (e.g., fetal bradycardia, repetitive cesarean delivery is indicated when the condition is lif
variable decelerations). Still, obstetricians continue to use threatening to the mother or fetus. In these situations, com
the term fetal distress to describe a wide range of fetal heart munication between obstetric and anesthesia care provider
rate abnormalities that, if not corrected or circumvented, is essential for maternal and fetal well-being.
will result in decompensation of physiologic responses and
cause permanent central nervous system or other damage or Risk Assessment
death. Anesthesiologists must consider the severity of the
fetal heart rate abnormality when determining the urgency The true incidence of fetal distress is difficult to quantif
of delivery and the type of anesthesia to be administered. largely because of the lack of clearly defined diagnostic cr
teria. However, it is a diagnosis that is likely overused b
physicians. In 1991 U.S. birth certificate statistics reveale
Recognition that fetal distress was a confounding factor in 4.3% of liv
Consistent, accurate diagnosis of true fetal distress (i.e., births. More recently, rates of cesarean delivery for fetal dis
intrauterine hypoxia or asphyxia) is a clinical challenge tress ranged from 2% to 8.7%.
because of the questionable reliability of electronic fetal Fetal distress may result from interference of oxyge
heart rate monitoring for predicting adverse neonatal out- transport at the level of the mother, the placenta, the umbi
comes. Still, electronic fetal heart rate monitoring is the pri- ical cord, or the fetus itself (Table 192-1). Sometimes th
mary screening tool. Additional support for the diagnosis cause is multifactorial, but more often a primary cause
may be obtained from the presence of meconium in the identifiable. Common high-risk obstetric conditions tha
amniotic fluid, deteriorating fetal acid-base status, lack of a increase the risk of fetal distress include the following:
fetal heart rate response to acoustic or scalp stimulation, and ● Preeclampsia or eclampsia and chronic hypertension
umbilical artery Doppler velocimetry. The most sensitive ● Diabetes mellitus
indicators of fetal cerebral oxygenation are heart rate ● Intrauterine growth retardation
variability or accelerations. ● Oligohydramnios
Gradual decreases in fetal oxygenation produce a variety ● Fetal prematurity or postmaturity
of fetal heart rate patterns (Fig. 192-2). Early signs of transient ● Chorioamnionitis
hypoxemia in a neurologically intact fetus may include tachy-
cardia, persistent sinusoidal fetal heart rate pattern, and peri-
odic changes consisting of late and variable decelerations. Implications
Although these changes alone do not preclude the delivery of
a healthy neonate, they should alert the clinician that the fetus Severe and sustained hypoxia in the fetus will eventually lea
is at risk. In extreme cases, the fetus will lose all central influ- to profound acidosis, neurologic sequelae (e.g., seizure
ence over its heart rate and develop a straight-line tracing coma, hypotonia), and ultimately, death.
770
You might also like
- The Sword of Kaigen by M. L. WangDocument6 pagesThe Sword of Kaigen by M. L. Wangdomojima0% (17)
- Emergencias ReumatologicasDocument15 pagesEmergencias ReumatologicasmizrapmNo ratings yet
- Yoga For Back PainDocument5 pagesYoga For Back PainaadityabuggascribdNo ratings yet
- Marginal Costing in Managerial Decision MakingDocument16 pagesMarginal Costing in Managerial Decision Makingyashashree_taori4443100% (4)
- Computer Network AnswersDocument4 pagesComputer Network Answersammad ahmadNo ratings yet
- Herrera 2016Document16 pagesHerrera 2016Farin MauliaNo ratings yet
- Gynec and Obs. Topic Fetal DistressDocument45 pagesGynec and Obs. Topic Fetal DistressRajdeep ParmarNo ratings yet
- Successful Management of Fetal Atrial Flutter at Term Pregnancy With PostnatalDocument5 pagesSuccessful Management of Fetal Atrial Flutter at Term Pregnancy With Postnatalaulia firdausNo ratings yet
- Kernicterus and The Healthy Term Newborn: Canadian Paediatric Surveillance ProgramDocument7 pagesKernicterus and The Healthy Term Newborn: Canadian Paediatric Surveillance ProgramFidelis OgonnaNo ratings yet
- Antenatal ProfileDocument6 pagesAntenatal ProfileSinchan GhoshNo ratings yet
- Post Term Pregnancy: Dr. M.C.BansalDocument31 pagesPost Term Pregnancy: Dr. M.C.BansalAnonymous ON3Qpn9ZNo ratings yet
- Intrapartal Diabetes MellitusDocument6 pagesIntrapartal Diabetes Mellitusapi-3797941No ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument6 pagesBest Practice & Research Clinical Obstetrics and GynaecologyElena ZepedaNo ratings yet
- Abarientos Con 2a Assignment 3 PDFDocument3 pagesAbarientos Con 2a Assignment 3 PDFjennielunay00No ratings yet
- PIIS0002937822003465Document14 pagesPIIS0002937822003465elizabethjenkinscoNo ratings yet
- Extremely Low Birth Weight (ELBW) InfantDocument48 pagesExtremely Low Birth Weight (ELBW) InfanthannanyusofNo ratings yet
- Preeklamsia Kasus ReportDocument7 pagesPreeklamsia Kasus ReportShofi FaizaNo ratings yet
- CAYABYAB Fetal-DistressDocument2 pagesCAYABYAB Fetal-DistressTrisha CayabyabNo ratings yet
- The Fetal DistressDocument28 pagesThe Fetal DistressPPDS Muhammad Fadli SyahdemaNo ratings yet
- Actualizacion en Monitoreo Fetal 2017Document10 pagesActualizacion en Monitoreo Fetal 2017Belmonte FerNo ratings yet
- Fetal Compromise in LabourDocument17 pagesFetal Compromise in LabourLAYLA AIZANo ratings yet
- Infants of Diabetic MothersDocument19 pagesInfants of Diabetic MothersGaby AldamaNo ratings yet
- Management of Fetal Distress: StephanieDocument16 pagesManagement of Fetal Distress: Stephanieyenni anggrainiNo ratings yet
- Archives of Gynecology and Obstetrics Volume 289 Issue 4 2014 (Doi 10.1007 - s00404-013-3072-9) Narang, Yum - Vaid, Neelam Bala - Jain, Sandhya - Suneja, Amita - Gu - Is Nuchal Cord JustifiDocument7 pagesArchives of Gynecology and Obstetrics Volume 289 Issue 4 2014 (Doi 10.1007 - s00404-013-3072-9) Narang, Yum - Vaid, Neelam Bala - Jain, Sandhya - Suneja, Amita - Gu - Is Nuchal Cord JustifiRaga ManduaruNo ratings yet
- ACOG Committee Opinion No 348 Umbilical Cord Blood Gas and Acid-Base AnalysisDocument4 pagesACOG Committee Opinion No 348 Umbilical Cord Blood Gas and Acid-Base AnalysisLina E. Arango100% (1)
- Jurnal Asfiksia PDFDocument14 pagesJurnal Asfiksia PDFditya.novianti06No ratings yet
- Predicting Fetal Outcome in Intrahepatic Cholestasis of Pregnancy: Is The Bile Acid Level Sufficient?Document2 pagesPredicting Fetal Outcome in Intrahepatic Cholestasis of Pregnancy: Is The Bile Acid Level Sufficient?Nicolae RusuNo ratings yet
- Uterine and Fetal Placental Doppler Indices Are Associated With Maternal Cardiovascular FunctionDocument8 pagesUterine and Fetal Placental Doppler Indices Are Associated With Maternal Cardiovascular FunctionMuhammad Pebri Nilhakim ZavbmNo ratings yet
- Zacharzewski 2019Document6 pagesZacharzewski 2019Ario DaniantoNo ratings yet
- PIIS0002937820311285Document17 pagesPIIS0002937820311285Jose Francisco Zamora ScottNo ratings yet
- Neonatal Resuscitation: Thomas E Wiswell MDDocument8 pagesNeonatal Resuscitation: Thomas E Wiswell MDm6000000No ratings yet
- JP 06020Document8 pagesJP 06020INDRINo ratings yet
- Seminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientDocument5 pagesSeminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientAsif KhanNo ratings yet
- NewbornEmergenices2006 PDFDocument16 pagesNewbornEmergenices2006 PDFRana SalemNo ratings yet
- Eclampsia OutputDocument5 pagesEclampsia OutputhailleyannNo ratings yet
- JP2011 848794Document8 pagesJP2011 848794ROSMEL VLADIMIR FABIAN LLAJARUNANo ratings yet
- Umbilical Cord ProlapseDocument5 pagesUmbilical Cord ProlapsesalamredNo ratings yet
- Update On Medical Disorders in Pregnancy An Issue of Obstetrics and Gynecology Clinics The Clinics Internal MedicineDocument217 pagesUpdate On Medical Disorders in Pregnancy An Issue of Obstetrics and Gynecology Clinics The Clinics Internal Medicinemeriatmaja100% (1)
- Seminars in Fetal & Neonatal Medicine: Michael P. NageotteDocument5 pagesSeminars in Fetal & Neonatal Medicine: Michael P. NageotteElena ZepedaNo ratings yet
- Gawat JaninDocument45 pagesGawat JaninNajla MasturaNo ratings yet
- NIH Public Access: Epidemiology of Preeclampsia: Impact of ObesityDocument14 pagesNIH Public Access: Epidemiology of Preeclampsia: Impact of ObesityHani FatimahNo ratings yet
- Physiological Changes in PregnancyDocument7 pagesPhysiological Changes in PregnancyFarid DjafarNo ratings yet
- Amniotic Fluid Embolism ArticleDocument3 pagesAmniotic Fluid Embolism ArticleShailesh JainNo ratings yet
- The Physiology of Intrapartum Fetal Compromise at Term: Sailesh. Kumar@mater - Uq.edu - AuDocument10 pagesThe Physiology of Intrapartum Fetal Compromise at Term: Sailesh. Kumar@mater - Uq.edu - AuseopyNo ratings yet
- Fetal Distress: PathogenesisDocument6 pagesFetal Distress: PathogenesisJulikrianto M. GultomNo ratings yet
- Fetal Distress: PathogenesisDocument6 pagesFetal Distress: PathogenesisWulid Lailah MagfirahNo ratings yet
- The Origins of Cerebral Palsy: John M. Keogh and Nadia BadawiDocument6 pagesThe Origins of Cerebral Palsy: John M. Keogh and Nadia BadawiC_DanteNo ratings yet
- Resusitasi IntrauterineDocument7 pagesResusitasi IntrauterineRizka AdiNo ratings yet
- Fetal Distres 1Document12 pagesFetal Distres 1mariah careyNo ratings yet
- Resuscitation in Pregnancy: Respiratory and Pulmonary ChangesDocument5 pagesResuscitation in Pregnancy: Respiratory and Pulmonary ChangesElle ReyesNo ratings yet
- Casestudy Makato 2nd Pre EclampsiaDocument7 pagesCasestudy Makato 2nd Pre EclampsiaRainier IbarretaNo ratings yet
- Postterm Pregnancy and IUFDDocument24 pagesPostterm Pregnancy and IUFDNejib M/AminNo ratings yet
- Seminars in Fetal & Neonatal Medicine: Michael P. NageotteDocument5 pagesSeminars in Fetal & Neonatal Medicine: Michael P. NageotteAnonymous 2KwbItVNo ratings yet
- Tool-Educational Sample Scenario 1 - Abruptio PlacentaeDocument2 pagesTool-Educational Sample Scenario 1 - Abruptio Placentaeanne marieNo ratings yet
- CP Neon EncepthDocument9 pagesCP Neon EncepthJuan Carlos HuanacheaNo ratings yet
- Neurosurgery in PregnancyDocument12 pagesNeurosurgery in PregnancyhkdawnwongNo ratings yet
- Resume Luar Negeri Dita FebriyantiDocument9 pagesResume Luar Negeri Dita FebriyantiDita FebriyantiNo ratings yet
- The Impact of Preeclampsia in Pregnancy: Original ArticleDocument4 pagesThe Impact of Preeclampsia in Pregnancy: Original ArticleAnonymous YYWsfmocYNo ratings yet
- Newborn With Respiratory Distress - Adam: KnowledgeDocument19 pagesNewborn With Respiratory Distress - Adam: KnowledgePeachesOrangesApplesNo ratings yet
- Congenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementFrom EverandCongenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDiva D. De León-CrutchlowNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Anesthesia and the FetusFrom EverandAnesthesia and the FetusYehuda GinosarNo ratings yet
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Dental Management of the Pregnant PatientFrom EverandDental Management of the Pregnant PatientChristos A. SkouterisNo ratings yet
- WahhabiDocument58 pagesWahhabiAt-Tarmizi CargasNo ratings yet
- Akritas Probability & Statistics With R For Engineers and ScientistsDocument256 pagesAkritas Probability & Statistics With R For Engineers and Scientistschristian neme schulNo ratings yet
- TSP Ee 21693Document21 pagesTSP Ee 21693popescu danielaNo ratings yet
- Fermat's Last TheoremDocument64 pagesFermat's Last Theoremtharaka1226No ratings yet
- EOM - LODSP - EOS Announcement For Huawei B2268H, B2268S, B2328-42, B5318-42, WBB Router B5328-155, B5328-58Document2 pagesEOM - LODSP - EOS Announcement For Huawei B2268H, B2268S, B2328-42, B5318-42, WBB Router B5328-155, B5328-58Lisanis PeruNo ratings yet
- Compact Modular Sulphur Recovery Solutions: Benoît Mares and Christian Streicher ProsernatDocument3 pagesCompact Modular Sulphur Recovery Solutions: Benoît Mares and Christian Streicher ProsernatnaeNo ratings yet
- Brushless DC Electric Motor Control by CPLDDocument6 pagesBrushless DC Electric Motor Control by CPLDIonela100% (3)
- Management and Theories of Management NotesDocument11 pagesManagement and Theories of Management NotesjosephNo ratings yet
- Probability Assignment 4Document3 pagesProbability Assignment 4Vijay KumarNo ratings yet
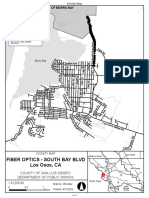
- Fiber Optics Installation ProjectDocument1 pageFiber Optics Installation ProjectKatherine WorshamNo ratings yet
- HESI Math and Science Answers Exam 2023Document4 pagesHESI Math and Science Answers Exam 2023Nelson MandelaNo ratings yet
- Educational Planning:: DefinitionDocument3 pagesEducational Planning:: DefinitionBasit AliNo ratings yet
- S S P J: Tructures OF Tory Roblems OINDocument10 pagesS S P J: Tructures OF Tory Roblems OINJuliana Marrey P. AgnoteNo ratings yet
- Multistate Licensure in NursingDocument11 pagesMultistate Licensure in Nursingapi-444163791No ratings yet
- Quarter 1 Lesson 1Document3 pagesQuarter 1 Lesson 1Lester EstoquiaNo ratings yet
- Control of HVDC Transmission System Based On MMC With Three-Level Flying Capacitor SubmoduleDocument22 pagesControl of HVDC Transmission System Based On MMC With Three-Level Flying Capacitor SubmoduleAnand Parakkat Parambil100% (1)
- Review Materials NTC LicenseDocument23 pagesReview Materials NTC Licensejoebanpaza194% (18)
- WE - Writing A Literature Review PDFDocument2 pagesWE - Writing A Literature Review PDFRonie Manic100% (1)
- An Introduction To Automatic Mesh Generation AlgorithmsDocument122 pagesAn Introduction To Automatic Mesh Generation AlgorithmsLinda FuNo ratings yet
- A Survey Analysis On CMOS Integrated Cir PDFDocument4 pagesA Survey Analysis On CMOS Integrated Cir PDFNK NKNo ratings yet
- SemioticsDocument4 pagesSemioticsPrincess MuskanNo ratings yet
- 2016 - Dairam N Et Al - Sucrose Losses Across GledhowDocument15 pages2016 - Dairam N Et Al - Sucrose Losses Across GledhowMaydolNo ratings yet
- Module 03 The DerivativeDocument10 pagesModule 03 The DerivativeEloisa SentillasNo ratings yet
- A Perspective of Braided Hairstyles PDFDocument9 pagesA Perspective of Braided Hairstyles PDFhumble happyNo ratings yet
- Reliability Blueprint PDFDocument30 pagesReliability Blueprint PDFFabioPaixao100% (1)
- What Is A Computer?: Programmable Data Abacus Slide Rule Input Process Output StorageDocument16 pagesWhat Is A Computer?: Programmable Data Abacus Slide Rule Input Process Output StorageAmoun AhmedNo ratings yet