Professional Documents
Culture Documents
SRK/T: Development of The Intraocular Lens Implant Power Calculation Formula
SRK/T: Development of The Intraocular Lens Implant Power Calculation Formula
Uploaded by
leviathan_brOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SRK/T: Development of The Intraocular Lens Implant Power Calculation Formula
SRK/T: Development of The Intraocular Lens Implant Power Calculation Formula
Uploaded by
leviathan_brCopyright:
Available Formats
Development of the SRK/T intraocular lens implant power calculation formula
John A. Retzlaff, M.D., Donald R. Sanders, M.D., Ph.D., Manus C. Kraff, M.D.
B TRA T
A ne, implant power calculation formula ( RKlT) .. as d eloped
u in the nonlin ar terms of the theOl'etical formulas a .it foundation
but empirical r gr ssion methodolog for optimization. Po toperati e
anterior chambel' depth prediction I'etinal thicknes a ial length
correction and corneal refracti e inde. .. ere tematieall and
interacti el optimized usin an iterati e p.-oce 's on fi e data ets
con. i ting
· of 1 677 post riOl' chamber lens ca e . The ne\ RKIT
fOl'mula perfOl'med ·Ii htl better than the Hollada RK II
Binkhorst and Hoffel' formula ,hieh wa. the e pected re ult a .an
fOl'mula pe.-forms supel"iorl ' \ ith the data f.-om, hich it wa deri ed,
omparati e accurae of thi. fOI"mula upon independent data set i
addl'e ed in a fo])ow-up report. The fOl'mula deri ed pro ide a
primal'il theoretical app.-oach undel' the R umbrella of formula
and has the added ad antage of bing calculable u ing either RK
-con tant that ha e been empirica]) deri ed 0 er the last nine
eal' or u in antel'iol" chamber depth e timate ,
Ke \Vord: A-con:tant, -scan, ant 'riorchamh rei pth a\iall('ngth ,
hiometr~, he ight fi)rmula, intraoculaJ' lens po" >1' calcula-
tion r gr', sion formula 'H , 'RK II, ' RKff, th oJ'eti-
'nl fi)J'm ula
Regression-derived lens implant power formulas that were empirically derived and individualized by
have an excellent accuracy record,l,8 Still, theoreti- manufacturers and surgeons over the last nine years.
cal formulas, because they are based on physiologic Many surgeons have expressed a desire to com-
optics, may be more accurate than regression for- pare regression formula results with theoretical
mulas when extended past a given database as in formula results for a given case and, if possible, have
unusually long or short eyes. some sort of definitive correlation between the
In addition to proven accuracy, regression for- regression A-constants and the theoretical anterior
mulas are simpler to derive and Vlanipulate than chamber depth (ACD) determinations. We decided,
theoretical formulas. 9 Residual error, due to sur- therefore, that it would be valuable to offer a
geon technique or intraocular lens (IOL) design, is theoretical approach to implant power calculation
combined into a single constant. In the SRK and under the SRK umbrella of formulas. We sought to
SRK II formulas, there are existing A-constants merge the theoretical and empirical approaches,
From the Department of Ophthalmology, University of Illinois at Chicago, and Medford, Oregon.
Analysis of the data performed in part by the Center for Clinical Research, which is funded by the American Society of Cataract and
Refractive Surgery and private donations.
Repdnt requests to Donald R. Sanders, M.D., Ph.D., 815 West Van Buren Street, Suite 300, Chicago, Illinois 60607.
J CATARACT REFRACT SURG- VOL 16, MAY 1990 333
using the best attributes of both, by combining the Table 1. SRKlT development data sets.
principles and methods of data analysis used for
development of the SRK formulas with the princi- Data Number
Set Company Style Source of Cases
ples and methods which have evolved in the devel-
opment of the theoretical formulas. This paper 1 3M PC 30 Multiple MDs 600
presents the SRKIf (SRKftheoretical) formula and 2 CooperVision JFIRLU Jaffe and Clayman 359
the methods used to derive it.
G70G
MATERIALS AND METHODS 3 IOLAB 707G Shearing 313
107G
Five formula derivation data sets, consisting of a
4 IOLAB G706 Kraff 305
total of 1,677 posterior chamber IOL cases , were
707G
used to optimize the constants in the formula
empirically. These data sources are detailed in Ta- 5 Surgidev B2020 Lindstrom 100
ble l. Each data source consisted of one or more
surgeon 's series of cases using a single posterior
chamber lens style. Cases with more than three
diopters (D) of postoperative astigmatism or with
postoperative visual acuity of worse than 20/40 were and interactively to create an empirical formula that
excluded. The database was meant to represent a uses the nonlinear terms of the theoretical formula
heterogeneous, real-world sample. For the most as its foundation. 16 Thus, the three steps listed were
part, applanation style A-scan units equipped with performed interdependently; changing anyone
oscilloscopes were used. Different brands of ker- changed the other two so several repetitions of each
atometers were used and K-readings were recorded optimization (iterations) were required to optimize
in diopters; radius of curvature was converted to all three interactively.
diopters using l.3375 refractive index. For example, if a corneal refractive index of 1.334
Analysis was performed on an IBM PC AT with a were chosen for trial, the calculated optical ACD for
8087 math coprocessor using the SPSS PC statisti- each case would be different than for any other
cal software. 10 refractive index so all ACDs would have to be
After developing the formula, the prediction recalculated. These new ACD values might require
accuracy was compared with that of the original and a different retina thickness correction factor which,
modified Binkhorst formulas, 11,12 the Holladay for- in turn, could change the ACD values.
mula,13 the Hoffer-Colenbrander formula, 14, 15 and
Predicting Postoperative ACD
the SRK 118 formula in the following way. The
To explore different ACD prediction methods, we
formulas were used as recommended by the authors;
algebraically rearranged the theoretical formula
ACD-constant and A-constant values were opti-
solving for postoperative ACD. (This required solu-
mized by iteration to obtain mean absolute errors
of zero. tion of a quadratic equation; we discovered , in
retrospect, that Holladay13 had used the same
Expected postoperative refraction was calculated
method earlier in his "reverse solution" of the
for each IOL case using each formula and compared
theoretical formula.) We then calculated, retrospec-
to the actual measured postoperative refraction.
tively, the theoretical optical ACD for each case in
Standard errors of the estimates, mean absolute
the five formula development data sets.
errors, standard errors of the mean deviations, and
Next, we devised and evaluated different methods
the distributions of the deviations were computed
and evaluated. of predicting this optical ACD; the relationship of
the axial length and corneal curvature to this ACD
value was exhaustively explored using many differ-
FORMULA DEVELOPMENT
ent regression models and the corneal height for-
Development of the final SRKff model consisted mula 17-21 in a variety of ways.
primarily of empirically optimizing (1) postoperative The simple linear regression equation proved to
ACD prediction, (2) retina thickness correction be as accurate a predictor of ACD as more complex
factor, and (3) corneal refractive index. regression models and was virtually as accurate as
Early refinements of the value assumptions of the the corneal height formula. The corneal height
various correction factors in the original theoretical formula , implemented as described , was chosen
formulas, for the most part , were developed concen- because it is more physiologic than the regression
trating on one factor at a time. We decided to explore line and might be expected to perform better in
each constant and procedural step systematically extreme cases.
334 J CATARACT RE F RACT SURG-VOL 16, MAY 1990
Axial Length Modificationsfor ACD Prediction in formula was presented by Fyodorov et al,l7,18 in
Very Long Eyes. Hoffer,14 Shammas,22 and Olsen 21 1967 and in 1975, examined by Bagan and Bru-
use no axial length correction for long eyes in their baker20 in 1980, and used by both Olsen21 and
prediction of postoperative ACD. Binkhorst 12 uses Holladay13 in their versions ofthe theoretical formula.
an abrupt upper limit of 26 mm in his ACD As Olsen 21 ,23 described, "the height formula
prediction, stating, "Beyond 26 mm the increase in regards the cornea as a section of a sphere the base of
axial length is believed to be mostly in the posterior which forms a plane at the level of the anterior iris,
segment." Holladay13 sets a cutoff at 25.3 mm for the calculated iris plane" (Figure 2). The height (H)
axial length modification and 48.31 D for corneal of the corneal dome is computed from the corneal
curvature. width (width) and the corneal curvature (r):
We tested the idea that very myopic eyes have H = r - Vr2 - (width/2)2
proportionally greater elongation of the posterior
Corneal Width. No white-to-white or other direct
than the anterior segment by comparing different
clinical estimate of corneal width was available in our
axial length corrections in long eyes. We reasoned
data, so it was necessary to devise a prediction of
that, if this phenomenon occurs at all, it might occur
corneal width (C w )' We found the linear formula
gradually with increasingly long eyes rather than
abruptly, so we tested curvilinear corrections as well C w = - 5.41 + 0.58412 x LCOR + 0.098 x K
as abrupt cutoff limits. The number of long eyes to be optimum.
among our 1,677 cases was insufficient to reach an Indirect evidence suggests that for use in the
absolute conclusion, but use of a correction for long corneal height formula, predicting corneal width in
eyes did appear warranted by the data. A parabolic this way may be more effective than using the white-
curve beginning at 24.2 mm appeared to give the to-white measurement.
most accurate prediction. Thus Intraocular Lens to Iris Plane Offset. The corneal
If L ::; 24.2, then LCOR = L
height formula hypothesis says that the intraocular
position of any given style IOL lies a constant
If L > 24.2, then LCOR = 3.446 + 1.715 xL - 0.237 X L2,
distance from the calculated iris plane in any
where L = axial length, LCOR = corrected axial length eye.l 7,18,21 Thus, the calculated iris plane serves as a
was adopted as part of the SRKfT ACD prediction reference point for IOL position (Figure 3). The
method. Figure 1 compares the SRKfT curvilinear constant distance from this plane to the optical plane
correction to abrupt corrections. We also tested axial of the specific IOL has been termed an offset by
length correction in short eyes and K-reading cor- Olsen 21 and the surgeon factor by' Holladay. 13 Holla-
rections in steep and flat eyes; these did not improve day's surgeon factor also includes a factor of 0.56 mm
accuracy of corneal height predictions so they were to account for corneal thickness.
not adopted. In our model the average eye calculated iris plane
Corneal Height Formula. The corneal height was 3.336 mm from the corneal vertex.
HOFFER
6.5
6.0
5.5
0
u 5.0 HOLLADAY
« Fig. 1. (Retzlaff) Graph showing post-
0
w 4.5 operative ACDs predicted by
f- BINKHORST II different formulas for different
U 4.0
0 length eyes for an IOL with an
W ACD-constant of 4.0. The kera-
0:::
a...
3.5 tometry value of 43 D was used
3.0 for SRKfT and Holladay calcula-
tions.
2.5
2.0
19 22 25 28 31 34 37
AXIAL LENGTH
J CATARACT REFRACT SURG- VOL 16. MAY 1990 335
Fig. 2. (Retzlaff) Diagram of the anterior segment showing Fig. 3. (Retzlaff) Diagram of the anterior segment with an
the height (H) of the corneal dome, computed by the IOL in place showing the offset from the calculated iris
height formula, and the location of the calculated iris plane to the optical plane of the IOL. The offset value,
plane. as calculated in this paper, also includes the corneal
thickness.
Computation of Offset and the Patient's Predicted Axial Length Correction Factor for Retinal
Postoperative ACD. The ACD-constant (ACDconst) Thickness
for a specific style IOL is the ACD of that IOL in an Many workers have theorized that physiologic
average eye. The difference between the average optical axial length is greater than ultrasonically
eye calculated iris plane and the AC D-constan t is the measured axial length by the distance from the
offset value for that IOL: vitreoretinal interface to the center retinal ele-
offset = ACDconst - 3.336 ments l (i.e., retinal thickness) (Figure 4).
Values from 0 to 0.5 mm have been used for the
The offset computed in this manner includes the
retinal thickness correction factor by various au-
corneal thickness dimension.
thors.I The Binkhorst formula uses 0.25 mm, the
In our data, the more complex linear form
Hoffer formula uses 0, and the Holladay formula
offset = ACDconst - b x 3.336 uses 0.20 mm.
was analyzed and the value for the b-constant (the In our model, retinal thickness axial length cor-
slope coefficient) was almost exactly 1, so the simpler rections from 0 through 0.5 mm were tested and
form can be used with no sacrifice in accuracy. found to be very nearly equivalent in accuracy.
The patient's postoperative ACD is predicted, However, we noted that in long eyes, smaller
then, by adding the computed corneal height for the correction values gave best accuracy and in short
patient's eye to the offset of the IOL to be implanted eyes, larger values gave best accuracy. This led us to
(see formulas (4), (5), and (6) in the formula appen-
dix). Table 2 compares predicted postoperative ACD
values for short, medium, and long eyes from
different formulas.
Optical Axial length
./
Table 2. Predicted postoperative ACDs for different length
eyes for an IOL with an ACD-constant of 4.0 mm.
i
Very Long
Short Medium Long
Formula 19 mm 23 mm 27 mm 31 mm 35 mm
SRKff 2.4 3.6 4.7 5.6 6.0
Holladay 2.7 3.8 4.7 4.7 4.7
Retina
Binkhorst II 3.2 3.9 4.4 4.4 4.4 Thickness
Factor
Hoffer 2.6 3.8 5.0 6.2 7.4
Keratometry value of 43 D used for SRKIT and Holladay Fig. 4. (Retzlaff) Diagram of the eye showing retinal thick-
formulas ness, ultrasonic axial length, and optical axial length.
336 J CATARACT REFRACT SURG-VOL 16, MAY 1990
evaluate different models for this axial length correc- Table 3. Axial length correction for different length eyes.
tion factor. We found the linear formula
Axial Length Retinal Thickness Correction
axial length correction = .65696 - 0.2029 XL
(mm) (mm)
gave a slightly more accurate prediction in everyone
18 0.29
of the five data sets used to develop the formula. We
speculate that vagaries of the ultrasound measure- 20 0.25
ment may account for this unexpected finding. 23 0.19
Hoffer (personal communication) suggested that our 26 0.13
finding may be partly because shorter eyes have 33 -0.01
faster average speed of sound than longer eyes
because the ultrasound travel distance through the
crystalline lens is a higher proportion of axial length
in shorter eyes. mulas are so sensitive to changes in ne that even this
We felt the consistency of this empirical correc- tiny difference results in expected refraction predic-
tion factor warranted our adopting it in the SRKff tion differences of 0.05 D to 0.06 D.
formula. Table 3 shows this correction for various
Relationship of A-Constants and ACD-Constants
axial lengths.
As noted, the ACD-constant (ACDeonst) for a
Corneal Refractive Index specific style IOL is the ACD of that IOL in an
The early theoretical IOL power calculation for- average eye. This value is a constant for a given IOL
mulas used a corneal refractive index (ne) of or IOUsurgeon and the term ACD-constant should
l.336. 18 ,24 Binkhorst chose the value of l.3 (413), be used when referring to this constant rather than
explaining, "The reduction in corneal power result- loosely referring to it as the ACD. By contrast, the
ing from this would seem justified to compensate for estimated postoperative ACD value (ACD est) is not a
a slight degree of postoperative Battening of the constant; it varies considerably from eye to eye
cornea."19 Retzlaff! later pointed out that studies being tailored for each patient's eye by all the
analyzing eyes in which multiple sutures were used modern theoretical formulas.
have shown surgically induced steepening of the The intraocular position of the five styles of
cornea. posterior chamber IOLs varied from quite anterior
Olsen 25 advocates a value of l.3315, based on a (uniplanar plano-convex IOL) to quite posterior
rather elegant analysis of corneal optics, and em- (ten-degree angulated biconvex IOL). The resultant
phatically points out, as have others before him, that wide range of optimal A-constants and ACD-con-
all these corneal refractive indices are fictitious in stants in these datasets facilitated effective explora-
that they "regard the cornea as a single refracting tion of the relationships of these values. As is often
surface whose curvature equals the front curva- the case, a simple linear regression equation (see
ture." formula 12) gave an excellent fit, providing a good
Holladay13 used the value 1.3 (413) in his formula, means of predicting ACD-constants from A-con-
choosing a lower value than 1.336 for reasons similar stants. Holladay13 reported similar findings. The
to Olsen's. relationship will be discussed further in a subse-
We approached this question heuristically, testing quent paper.
values from l.330 through l.338. Values from l.331
to l.334 yielded the most accurate predictions, RESULTS
about equal in accuracy across this range. The values
The formulas derived are shown in the formula
from l.331 to about l.332 resulted in seemingly
appendix.
unphysiologically shallow ACD values which were
In the five formula derivation data sets, the new
considerably less than manufacturers' generally rec-
SRKff formula performed slightly better than the
ommended ACD-constants for IOLs in this country.
Holladay and the SRK II formulas in all the data sets
Thus, we chose the value of 1.333, which gives ACD-
individ~ally (Table 4) and in the 1,677 cases as a
constant values in harmony with currently pub-
group (Table 5). This is the expected result because
lished ACD-constants, which is similar to the value
any formula performs superiorly with data from
used by Binkhorst and Holladay, and which empiri-
which it is derived.
cally is as accurate as any other corneal refractive
index value. The value l.333, which is a terminated
DISCUSSION
decimal number that can be precisely expressed in a
computer, is used in SRKff; l.3 (413) is used in the The first theoretical implant power formula was
Binkhorst and Holladay formulas. Theoretical for- presented by Fyodorov and Kolinko 17 in 1967. The
J CATARACT REFRACT SURG-VOL 16, l\IAY 1990 337
Table 4. Comparison of standard error of estimate of different formulas in five data sets.
Standard Error of Estimate
Data Hoffer!
Set N SRKIT SRK II Holladay Colenbrander Binkhorst Binkhorst II
1 600 .91 .94 .91 .95 1.02 .96
2 359 .77 .78 .77 .82 .88 .82
3 313 1.02 1.04 1.05 1.15 1.16 1.14
4 305 .63 .67 .65 .70 .77 .70
5 200 .94 .90 1.01 1.15 1.16 1.22
first English language publication was by Colen- Our goals were to (1) improve ease of use by
brander in 1973. 24 Other early theoretical models creating a theoretical formula under the SRK um-
were formulated by Thijssen,26 Van Der Heijde,27 brella that would use existing A-constant and optim-
and R.D. Binkhorst.l 9 All these formulas except ization methods and provide easy comparison of the
Fyodorov's used a constant value for estimated theoretical and regression approaches and (2), if
postoperative ACD. Early efforts to predict post- possible, improve on the accuracy of existing for-
operative ACD, mostly by using preoperative ACD mulas. This first point has been addressed in this
measurements, proved unsuccessful; thus, use of a paper; the second is addressed in a follow-up
fixed value remained standard practice until 1981 report.28
when Binkhorst recommended that estimated post-
REFERENCES
operative ACD be adjusted for different length
1. Retzlaff J. A new intraocular lens calculation formula. Am
eyes. 12 Shammas,22 Hoffer,14 Olsen,21 and Holla- Intra-Ocular Implant Soc J 1980; 6:148-152
d ay13 followed with their own methods of adjusting 2. Sanders DR, Kraff MC. Improvement of intraocular lens
estimated postoperative ACD. power calculation using empirical data. Am Intra-Ocular
We sought to enhance the accuracy of the theo- Implant Soc J 1980; 6:263-267
retical approach to implant power calculation by 3. Retzlaff J. Posterior chamber implant power calculation:
regression formulas. Am Intra-Ocular Implant Soc J 1980;
empirically and interactively optimizing the con- 6:268-270
stants in the formulas. The formula derived provides 4. Gills JP. Minimizing postoperative refractive error. Contact
a theoretical formula under the SRK umbrella that Intraocul Lens Med J 1980; 6:56-59
uses existing A-constants and optimization methods. 5. Sanders D, Retzlaff J, Kraff M, et al. Comparison of the
Software comparing the theoretical and regression accuracy of the Binkhorst, Colenbrander, and SRK™ im-
plant power prediction formulas. Am Intra-Ocular Implant
approaches has been developed for IBM personal Soc J 1981; 7:337-340
computers and compatibles and will be inbuilt in 6. Sanders DR, Retzlaff J, Kraff MC. Comparison of empiri-
most new A-scan units. cally derived and theoretical aphakic refraction formulas.
Table 5. Comparison of errors in prediction of implant power in 1,677 formula derivation cases.
Error in Power Prediction
(% of Cases)
Standard Error of
Formula Mean Absolute Error < 0.5 D <ID >2D Estimate*
SRKIT .64 50 80 3.3 .86
Holladay .65 50 80 3.5 .88
SRK II .67 48 77 3.6 .89
Hoffer .70 42 78 4.9 .94
Binkhorst II .70 47 78 4.8 .94
Binkhorst (old) .74 47 75 5.5 .99
*Standard error of estimate (in diopters) = '\hum (actual refraction - predicted refraction)2
N
338 J CATARACT REFRACT SURG- VOL 16, MAY 1990
Arch Ophthalmol 1983; 101:965-967 power of the intraocular lens. Vestn Oftalmoll967; 80(4):27-31
7. Thompson }T, Maumenee AE, Baker CC. A new posterior 18. Fyodorov SN, Galin MA, Linksz A. Calculation of the
chamber intraocular lens formula for axial myopes. Oph- optical power of intraocular lenses. Invest Ophthalmol
thalmology 1984; 91 :484-488 1975; 14:625-628
8. Sanders DR, Retzlaff}, Kraff MC . Comparison of the SRK 19. Binkhorst RD. The optical design of intraocular lens
II ™ formula and other second generation formulas. implants. Ophthalmic Surg 1975; 6(3):17-31
} Cataract Refract Surg 1988; 14:136-141 20. Bagan SM, Brubaker RF. Prediction of artiphakic anterior
9. Retzlaff}, Sanders DR, KraffM. A Manual ofImplant Power chamber depth. Ophthalmic Surg 1980; 11:768-770
Calculation , 2nd ed. Medford, Oregon, Retzlaff, Sanders, 21. Olsen T. Prediction ofintraocular lens pOSition after cataract
Kraff, 1988 extraction. } Cataract Refract Surg 1986; 12:376-379
10. SPSS Inc. SPSSIPC + and TRENDS, Chicago, Illinois, 22. Shammas H}F. The fudged formula for intraocular lens
1988. power calculations. Am Intra-Ocular Implant Soc J 1982;
11. Binkhorst RD. Intraocular lens power calculation manual. 8:350-352
New York, RD Binkhorst , 1978 23. Olsen T. Intraocular lens power calculation (letter to the
12. Binkhorst RD. Intraocular Lens Power Calculation Manual: editor). } Cataract Refract Surg 1988; 14:452
a Guide to the Author's TICC-40 Programs, 3rd ed. New 24. Colenbrander MC . Calculation of the power of an iris clip
York, RD Binkhorst, 1984 lens for distant vision. Br J Ophthalmol 1973; 57:735-740
13. Holladay}T, Praeger TC, Chandler TY, et al. A three-part 25. Olsen T. Theoretical approach to intraocular lens calcula-
system for refining intraocular lens power calculations. tion using Gaussian optics. J Cataract Refract Surg 1987;
} Cataract Refract Surg 1988; 14:17-24 13:141-145
14. Hoffer KJ. Preoperative cataract evaluation: intraocular lens 26. Thijssen JM. The emmetropic and iseikonic implant lens:
power calculation. Int Ophthalmol Clin 1982; 22(2):37-75 computer calculation of the refractive power and its accu-
15. Hoffer KJ. The effect of axial length on posterior chamber racy. Ophthalmologica 1975; 171:467-486
lenses and posterior capsule position. Curr Concepts Oph- 27. Van Del" Heijde GL. The optical correction of unilateral
thalmic Surg 1984; 1(1):20-22 aphakia. Trans Am Acad Ophthalmol Otolaryngol1976; 81:
16. Rasooly R, Merin S, BenEzra D. Empirical modification of 80-88
the theoretical IOL power formulas (letter to the editor). 28. Sanders DR, Retzlaff J, Kraff M, et al. Comparison of the
} Cataract Refract Surg 1988; 14:350-351 SRKIT formula and other theoretical and regression for-
17. Fedorov SN , Kolinko AI, Kolinko AI. Estimation of optical mulas. J Cataract Refract Surg 1990; 16:341-346
FORMULA APPENDIX
Postoperative ACD Computation
(1) Corneal radius of curvature, mm (r): r = 337.5/K
(2) Corrected axial length , mm (LCOR):
If L ~ 24.4, then LCOR = L
If L > 24.4, then LCOR = 3.446 + 1.716 X L - 0 0237
. X Lx L
(3) Computed corneal width, mm (C w )
C w = - 5.41 + 0.58412 x LCOR + 0.098 x K
(4) Corneal height ,f-m_m->-
(H-'.)_ _ __
H = r - Vr x r - ((C w x Cw )/4)'
(5) Offset for specific IOL to be implanted:
Offset = ACDeonst - 3.336
(6) Estimated postoperative ACD for patient:
ACD est = H + offset
Intraocular Lens Power Computations
(7) Constants:
V = 12; na = 1.336; ne = 1.333; nem1 = 0.333
(8) Retinal thickness, mm (RETHlCK) and optical axial length, mm (LOPT):
RETHICK = 0.65696 - 0 .02029 xL
LOPT = L + RETHICK
(9) Emmetropia IOL power, D (IOLemme):
IOLemme = 1000xnax (naX r-n o ml X LOPT)
(LOPT - ACD)X(n a Xr-n emlxACD)
(10) Ametropia IOL power, D (IOLamet ):
IOLamet = 1000XnaX (naX r-n cml x LOPT- .001 X REFTGTX (Vx (naX r-n o ml x LOPT) + LOPTxr))
(LOPT-ACD) x (na X r - ncm1 x ACD - .001 x REFTGT x (V x (na X r - n m o l x ACD) + ACD x r))
(11) Expected refraction, D (REFX):
REFX = 1000 X naX (n a X r-n c ml X LOPT)- IOL x (LOPT-ACD) X (naX r-n c ml X ACD)
na X(V X (n a X r -nam1 X LOYf) + LOPT x r) - .001 x IOL x (LOPT-ACD) x (V x (na x r - nom l XACD) + ACD x 1")
Determining ACD-Constant from the A-Constant
(12) ACDconst = 0.62467 x A - 68.747
J CATARACT REFRACT SURG-VOL 16, MAY 1990 339
Tailoring, Optimizing, the A-Collstant
(13) Refraction factor (RF):
If IOL > ..JS. then RF = 1.25 If IOL :S. 16, then RF = 1
(14) Short and long eye correction:
If L < 20, then C 3
"'
If 22 :S. L < 24, then C o
If 20 :S. L < 21, then C = 2 If L ~~then C -0,5
If 21 :S. L < 22, then C = 1
:J'I. s-
-
(15) Individual A-constant (Aindivl:
Aindiv = IOL + (REF X RF) + 2,5 X L + 0,9 X K - C ~'(...,J-
(The mean value of A-indiv for a data set is the personalized A-constant for that data set's IOUsurgeon)
VARIABLES
ACDeonst = constant used for anterior chamber depth in SRKIT formula for specific IOUsurgeon; can be computed from A-constant
ACD est = estimated postoperative anterior chamber depth for a given eye (mm)
A = constant used for SRKIT and SRK II
Aindiv = A-constant from postoperative values of an individual eye
C = short and long eye correction factor for SRK II
C w = corneal width computed from Land K (mm)
H = height of corneal dome (mm)
IOL = power of intended or implanted IOL (D)
IOLamet = power of IOL for given amount of ametropia, for a given REFTGT (D)
IOLemme = power of IOL for emmetropia (D)
K = averaged keratometry (D)
L = axial length measured ultrasonically (mm)
LOPT = "optical" axial length (mm) = L + RETHICK
LCOR = axial length with long eye correction; used in height formula
na = refractive index of aqueous and vitreous
ne = refractive index of the cornea
neml = ne minus 1, used in theoretical formula
offset = difference between corneal height of the average eye and the ACD-constant of a given IOL (see Figure 3)
r = averaged corneal radius of curvature (mm)
REF = actual postoperative refraction (D)
REFTGT = targeted or desired postoperative refraction (D)
REFX = expected postoperative refraction (D)
RETHICK = sensory retinal thickness (mm)
RF = refraction factor
340 J CATARACT REFRACT SURC- VOL 16, MAY 1990
You might also like
- A - Piper (D Major)Document5 pagesA - Piper (D Major)김소언No ratings yet
- Amore E MorteDocument5 pagesAmore E MorteAnastassia IvanovaNo ratings yet
- Hal Leonard Adult Piano Method - Book 1Document100 pagesHal Leonard Adult Piano Method - Book 1Jhonatan ViolinNo ratings yet
- Mercadante Il Giuramento Bella Adorata Incognita For Tenor in BB OperaDocument5 pagesMercadante Il Giuramento Bella Adorata Incognita For Tenor in BB OperaGiulia De SantisNo ratings yet
- Ave Maria by Luis BacaDocument8 pagesAve Maria by Luis BacaLucia AltenhofenNo ratings yet
- Pueri Hebraeorum (Palestrina)Document3 pagesPueri Hebraeorum (Palestrina)IkeNo ratings yet
- Amarilli D MollDocument4 pagesAmarilli D MollSvetlana AhmedovaNo ratings yet
- Un Amore Così Grande: Performed by Il Volo Arranged by Erbin BlackDocument2 pagesUn Amore Così Grande: Performed by Il Volo Arranged by Erbin BlackannalisaNo ratings yet
- Credea Misera in CDocument4 pagesCredea Misera in CJack GardnerNo ratings yet
- G.Donizzeti - Ah, Un Foco Insolito (DonPasquale)Document6 pagesG.Donizzeti - Ah, Un Foco Insolito (DonPasquale)Martynas ŽukauskasNo ratings yet
- Tosti Sogno in A Major For Voice and PianoDocument5 pagesTosti Sogno in A Major For Voice and PianoAnonimus CantatriceNo ratings yet
- Madrigal B MajorDocument3 pagesMadrigal B MajorChristian GomezNo ratings yet
- 내 주는 강한 성이요Document14 pages내 주는 강한 성이요onlybronze46100% (1)
- NezhnostDocument3 pagesNezhnostAlexander CheungNo ratings yet
- Rossini Gioacchino Adieux Vie Elegie Sur Une Seule Note 139997 PDFDocument8 pagesRossini Gioacchino Adieux Vie Elegie Sur Une Seule Note 139997 PDFPatricia ŽudetićNo ratings yet
- Fiel Espada ToledanaDocument5 pagesFiel Espada ToledanaCarlos D'OnofrioNo ratings yet
- Piero Piccioni Amore Mio Aiutami Sax e Piano MagnaniDocument2 pagesPiero Piccioni Amore Mio Aiutami Sax e Piano MagnaniFelixTVNo ratings yet
- Ombra Fedele Anch'io: "Idaspe"Document8 pagesOmbra Fedele Anch'io: "Idaspe"Jônatas Luís MonteiroNo ratings yet
- They Shall Be As Happy (In B, - 1)Document2 pagesThey Shall Be As Happy (In B, - 1)Jan FaltýnekNo ratings yet
- 1 Son Qual Nave in Ria Procella Leo1Document7 pages1 Son Qual Nave in Ria Procella Leo1José Emanuel Felix MendesNo ratings yet
- Conto DellaTerra-Partitura y PartesDocument7 pagesConto DellaTerra-Partitura y Partesisaias alvarezNo ratings yet
- PN VCL Panis Angelicus B DurDocument3 pagesPN VCL Panis Angelicus B DurWilliam Carvalhal100% (1)
- Ước Mơ Của Mẹ - Nhà Học ĐànDocument2 pagesƯớc Mơ Của Mẹ - Nhà Học ĐànHien HaNo ratings yet
- The Morning DewDocument2 pagesThe Morning DewAnonymous msJTXgNo ratings yet
- Schumann Robert Bist Wie Eine Blume 16948Document2 pagesSchumann Robert Bist Wie Eine Blume 16948Cameron KillickNo ratings yet
- Gia Mi Sembra - La Fedelta Premiata (Haydn) PDFDocument6 pagesGia Mi Sembra - La Fedelta Premiata (Haydn) PDFSandmanNo ratings yet
- Visione VenezianaDocument5 pagesVisione VenezianaCarlosIaquintaNo ratings yet
- Ciel Che Feci, Oberto Conte Di San BonifacioDocument4 pagesCiel Che Feci, Oberto Conte Di San BonifacioStefano StranoNo ratings yet
- Vieni Vieni in Questo Seno Fco. CavalliDocument2 pagesVieni Vieni in Questo Seno Fco. CavalliSahira BoranNo ratings yet
- Tosti Sogno in A Flat Major For Voice and PianoDocument5 pagesTosti Sogno in A Flat Major For Voice and PianoAnonimus CantatriceNo ratings yet
- The Soldier and The SailorDocument3 pagesThe Soldier and The SailorBrunoPancekNo ratings yet
- Pastyme ScoreDocument2 pagesPastyme ScoreMatthew JelfNo ratings yet
- Handel MyheartisInditing FullScoreDocument38 pagesHandel MyheartisInditing FullScoreANisNo ratings yet
- Franz Tunder: Ach Herr, Lass Deine Lieben EngeleinDocument5 pagesFranz Tunder: Ach Herr, Lass Deine Lieben EngeleinMonika ŁopuszyńskaNo ratings yet
- Senior Recital Program NotesDocument5 pagesSenior Recital Program NotesBrian HuppNo ratings yet
- Il Mio Bel Foco - High VoiceDocument6 pagesIl Mio Bel Foco - High Voicehw.rogozaNo ratings yet
- La Mia Letizia Infondere PDFDocument3 pagesLa Mia Letizia Infondere PDFDaniele100% (1)
- Canoni SpringDocument1 pageCanoni SpringMaria BandiniNo ratings yet
- Niksa Lendic: About The ArtistDocument7 pagesNiksa Lendic: About The Artist王馨妤No ratings yet
- Silent Night (Arr. Andrew Lumsden) - The Choir of Lichfield Cathedral & Robert Sharpe LyricsDocument4 pagesSilent Night (Arr. Andrew Lumsden) - The Choir of Lichfield Cathedral & Robert Sharpe LyricsAndrew TejowicaksonoNo ratings yet
- The Mission Gabriels Oboe Partitura Orchestrale PDFDocument3 pagesThe Mission Gabriels Oboe Partitura Orchestrale PDFJesus Hernandez100% (1)
- 13 Canons For Female Choir Op. 113 (Brahms) - IMSLP23157-PMLP52910Document28 pages13 Canons For Female Choir Op. 113 (Brahms) - IMSLP23157-PMLP52910Antonella RussoNo ratings yet
- Shelter Piano Score - BirdyDocument3 pagesShelter Piano Score - BirdyAllison ZavalaNo ratings yet
- Outlander Theme TranscriptionDocument3 pagesOutlander Theme TranscriptionOana Laura MuresanNo ratings yet
- Moon River (Completa) - Henry Mancini - Acordes 47 PDFDocument2 pagesMoon River (Completa) - Henry Mancini - Acordes 47 PDFConservatorio De Música A GuardaNo ratings yet
- IMSLP112459-PMLP229643-Franck - L Ange Gardien 2vvPfDocument7 pagesIMSLP112459-PMLP229643-Franck - L Ange Gardien 2vvPfMichelle Batacan Alexander100% (1)
- Paulus, Op.36 (Aria (Soprano) : Jerusalem, Die Du Todtest Die Propheten) : Full Score (Qty 2) (A3570) by Felix MendelssohnDocument8 pagesPaulus, Op.36 (Aria (Soprano) : Jerusalem, Die Du Todtest Die Propheten) : Full Score (Qty 2) (A3570) by Felix MendelssohnEm AnnaNo ratings yet
- Yes Sir That's My Baby PDFDocument4 pagesYes Sir That's My Baby PDFAndréas ForsmanNo ratings yet
- Triquet's AriaIMGDocument5 pagesTriquet's AriaIMGKevin William PrinaNo ratings yet
- Edm PDFDocument47 pagesEdm PDFSunil VadhvaNo ratings yet
- KV.341 Mozart Kyrie EleisonDocument7 pagesKV.341 Mozart Kyrie EleisonGhadeer Nasser AbeidohNo ratings yet
- N°5. "Giovinette, Che Fate All' Amore.": Duet and ChorusDocument6 pagesN°5. "Giovinette, Che Fate All' Amore.": Duet and ChorusAneliz RodriguezNo ratings yet
- John Dowland - Thinkst Thou Then by Thy FeigningDocument3 pagesJohn Dowland - Thinkst Thou Then by Thy FeigningdudubinhoNo ratings yet
- Coro A Bocca Chiusa PDFDocument5 pagesCoro A Bocca Chiusa PDFgabrielefabbri6No ratings yet
- browningsong 중앙Document115 pagesbrowningsong 중앙yooNo ratings yet
- 2013 Intraocular Lens Power Calculation in Eyes With Previous Hyperopic Laser in Situ KeratomileusisDocument6 pages2013 Intraocular Lens Power Calculation in Eyes With Previous Hyperopic Laser in Situ KeratomileusisHanna_RNo ratings yet
- Intraocular Lens Power Calculations in Eyes With Previous Corneal Refractive Surgery Review and Expert OpinionDocument41 pagesIntraocular Lens Power Calculations in Eyes With Previous Corneal Refractive Surgery Review and Expert OpinionFredericoGalvaniNo ratings yet
- A Combination of Newton-Raphson Method and HeuristDocument14 pagesA Combination of Newton-Raphson Method and Heuristpat juvNo ratings yet
- Intraoperative Refractive Biometry For Predicting Intraocular Lens Power Calculation After Prior Myopic Refractive SurgeryDocument5 pagesIntraoperative Refractive Biometry For Predicting Intraocular Lens Power Calculation After Prior Myopic Refractive Surgerymiranda vzlaNo ratings yet
- AML23-AR-00307AML Tud ACEDocument33 pagesAML23-AR-00307AML Tud ACEAnonymous UJFK2jk5gNo ratings yet
- Makalah IOL Sekunder Fani EmailDocument22 pagesMakalah IOL Sekunder Fani EmailaniemaniesNo ratings yet
- A Comprehensive Guide To Managing Astigmatism in The Cataract PatientDocument6 pagesA Comprehensive Guide To Managing Astigmatism in The Cataract PatientRaúl Plasencia SaliniNo ratings yet
- Alcon Centurion Operators Manual ScannedDocument197 pagesAlcon Centurion Operators Manual ScannedhernandezzNo ratings yet
- Sail Tech PapersDocument61 pagesSail Tech PapersRajiv RanjanNo ratings yet
- Werner 2010Document23 pagesWerner 2010Vanessa BuitragoNo ratings yet
- Galaxy FoldDocument9 pagesGalaxy Foldgan04eshNo ratings yet
- Medical Reabursement GONo.74Document19 pagesMedical Reabursement GONo.74gsreddy100% (1)
- Contrast Sensitivity and Glare in Cataract Using TDocument5 pagesContrast Sensitivity and Glare in Cataract Using TRaissaNo ratings yet
- Echoscan US-800Document68 pagesEchoscan US-800Eslam ElsayedNo ratings yet
- Biomaterials Science, Ratner (2ed.) - 13-21Document9 pagesBiomaterials Science, Ratner (2ed.) - 13-21LUIS ANTHONY SALAS ARISTANo ratings yet
- Penta CamDocument33 pagesPenta CamPrasoon MkNo ratings yet
- 12 DecDocument43 pages12 DecJayesh ThakkarNo ratings yet
- Adis Pasalic - Doktorat-EngDocument91 pagesAdis Pasalic - Doktorat-EngHariom ShuklaNo ratings yet
- A-SME Platinum Brochure (SST) 20180901 v1Document64 pagesA-SME Platinum Brochure (SST) 20180901 v1khamini dilly kannan100% (1)
- Medik FamiliDocument10 pagesMedik FamiliBig DaddyCoolNo ratings yet
- Latest CGHS Rate File979Document43 pagesLatest CGHS Rate File979Inder0% (1)
- Ijmrhs Vol 3 Issue 2Document281 pagesIjmrhs Vol 3 Issue 2editorijmrhsNo ratings yet
- Tecnis Eyhance SpecSheetDocument2 pagesTecnis Eyhance SpecSheetShripad BhawsarNo ratings yet
- Brochure Occular PentacamDocument15 pagesBrochure Occular PentacamLuisEsparzaAvitia100% (1)
- HRK 7000A enDocument2 pagesHRK 7000A enislamicfactsonline00No ratings yet
- Complication IntraoperativeDocument5 pagesComplication IntraoperativeizzatulhasanahNo ratings yet
- Yag Laser CapsulotomyDocument5 pagesYag Laser CapsulotomyinhaNo ratings yet
- Eye Essentials Cataract Assessment Classification and ManagementDocument245 pagesEye Essentials Cataract Assessment Classification and ManagementMaíra Dias100% (7)
- Brochure Iolmaster 700 ModfDocument11 pagesBrochure Iolmaster 700 ModfTT XNo ratings yet
- STAAR Surgical CRST Supplement 2016Document8 pagesSTAAR Surgical CRST Supplement 2016Andreea L. MihalceaNo ratings yet
- Postgraduate Ophthalmology Exams in IrelandDocument22 pagesPostgraduate Ophthalmology Exams in IrelandAna-Maria Misici100% (2)
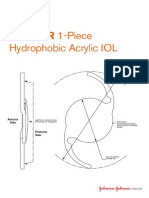
- Sensar 1 Piece - AAB00Document2 pagesSensar 1 Piece - AAB00rhymenNo ratings yet
- Value Focus: Tecnis Synergy Iols - A Breakthrough Innovation ThatDocument5 pagesValue Focus: Tecnis Synergy Iols - A Breakthrough Innovation ThatEnrique Ferrando BarbenaNo ratings yet
- Catalog P1-P10Document10 pagesCatalog P1-P10cncymzNo ratings yet
- اخطاء انكسار 4Document4 pagesاخطاء انكسار 4Hassan AljaberiNo ratings yet